Abstract
Objectives
To estimate trends in HIV testing, positivity and prevalence in UK primary care for 2000–2015 as part of a wider investigation into reasons for late diagnosis of HIV.
Design
Retrospective cohort study using the Clinical Practice Research Datalink (CPRD) which is derived from computerised clinical records produced during consultations in primary care.
Setting
404 general practices in England.
Participants
5 979 598 adults aged ≥16 years registered between 2000 and 2015 with 45 093 761 person years of observation.
Outcomes
Annual HIV testing rates, proportion of positive tests and prevalence of HIV-infected people recorded in primary care 2000–2015.
Results
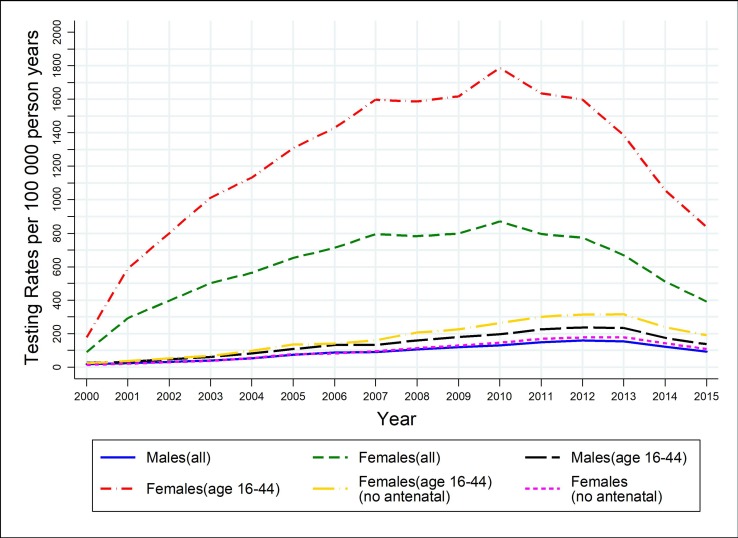
HIV testing in primary care increased from 2000 to 2010, but then declined. Testing was higher in females than in males and in those aged 16–44 years compared with older adults. Rates per 100 000 in women aged 16–44 years were 177 (95% CI 167 to 188); 1309 (95% CI 1282 to 1336); 1789 (95% CI 1757 to 1821) and 839 (95% CI 817 to 862) in 2000, 2005, 2010 and 2015, respectively, and for non-pregnant women: 22.5 (95% CI 19 to 26); 134 (95% CI 125 to 143); 262 (95% CI 250 to 275); 190 (95% CI 179 to 201). For men aged 16–44 years rates were: 26 (95% CI 22 to 29); 107 (95% CI 100 to 115); 196 (95% CI 185 to 206); 137 (95% CI 127 to 146). Over the study period, there were approximately two positive results per 1000 HIV tests. Men were eightfold more likely to test positive than women. The percentage of HIV diagnoses among adults recorded in CPRD may be as low as 55% in London and 67% in the rest of the UK.
Conclusions
HIV testing rates in primary care peaked in 2010 and subsequently declined. Access to testing was higher for women despite the prevalence of HIV being higher in men.
Implications and further research needed
Opportunities remain in primary care for increasing HIV testing to prevent costly late diagnoses and decrease HIV transmission. Interventions to improve targeting of tests and increase adherence to HIV testing guidelines are needed in primary care.
Keywords: primary care, HIV & AIDS, HIV testing, CPRD
Strengths and limitations of this study.
We investigated trends in HIV testing in primary care using high quality data from the Clinical Practice Research Datalink (CPRD) which is derived from computerised clinical records produced during consultations in primary care in England.
CPRD provided anonymised primary care records on patients registered between 2000 and 2015 in 404 primary care practices in England which is likely to be representative of the general patient population.
A limitation of the study is that not all general practices contribute data to CPRD and therefore we cannot know whether the sample was representative.
A major strength of the study was the large number of patients, nearly 6 million, which allowed us to contrast trends in HIV testing rates in primary care by sex, age, deprivation, rural/urban location and whether in London or not.
Data were available for 15 years of follow-up allowing us to show that HIV testing in primary care in England increased between 2000 and 2010, but then declined up to 2015.
Introduction
HIV testing in primary care is an important component of the strategy to diagnose HIV earlier and reduce transmission of HIV. In 2015 there were an estimated 89 800 (95% credible interval (CrI) 87 100 to 94 800) people living with HIV in England of whom approximately 15% (CrI 12%–19%) were unaware of their infection.1 Of those individuals newly diagnosed with HIV in 2015, 39% were diagnosed late, defined as having a CD4 count below 350 cells/mL within 3 months of diagnosis.2 An estimated 1 in 4 of newly diagnosed individuals experienced a missed opportunity for an earlier diagnosis within the healthcare system in the preceding year.3 Late diagnosis of HIV is associated with increased hospitalisations, decreased life expectancy4–7 and higher treatment and care costs to the National Health Service (NHS).8 Importantly, individuals with undiagnosed HIV are likely to be responsible for the majority of transmissions because successfully treated individuals are unlikely to infect others.9
Enhanced HIV testing is considered to be cost-effective in areas with a local diagnosed HIV prevalence that exceeds 2 per 1000 in adults aged 15–59 years.2 10 In these high HIV prevalence areas recommendations are an HIV test should be routinely offered to all new general practitioner (GP) registrations, those undergoing tests for other sexually transmitted infections or having blood tests for any reason, and all new hospital medical admissions.2 11 However, the majority of people with HIV seek medical care for a related condition several times prior to their HIV diagnosis.12 13 This may be presenting to general practice or hospital care. But without a high degree of clinical suspicion, the diagnosis is often missed.14 The British HIV Association(BHIVA) has published a list of indicator diseases that are more commonly found in those who are HIV positive than negative.15 HIV testing is recommended in these cases, but recent surveys suggest poor adherence to guidelines.16 17 Given the increase in HIV prevalence over time we would expect that there would be an increase in GP testing for HIV.
Evidence from systematic reviews shows that there are often many barriers to testing experienced by patients and equally by healthcare professionals (HCP).18–20 Patients presenting with clinical indicator conditions to their GP provide a valuable opportunity to diagnose HIV and avoid hospitalisations due to late diagnosis.21 Research has shown that the majority of patients (up to 75%) newly diagnosed with HIV had been seen in the healthcare system within the 12 months prior to their diagnosis resulting in a missed opportunity to test.12 14 22 23Opt out HIV testing has been shown to be feasible, acceptable and cost effective in eight pilot studies conducted in community, primary and secondary care settings in high prevalence areas across England.24 However, no recent evidence is available to know if HIV testing in primary care has been increasing and guidelines have been implemented over the country and not just in high risk areas.16 17
HIV testing in primary care has been reported only for the years 1995–2005 using data from the UK General Practice Research Database (GPRD).25 This study showed that testing in primary care remained low, but increased steadily. Our main objective was to analyse data from the same source collected between the years 2000 and 2015 to study if HIV testing trends continued to increase in primary care over this extended time period. In addition we investigated differences in HIV testing rates and HIV diagnosis by demographic characteristics and estimated the prevalence of HIV recorded in primary care and compared it with estimates from national surveillance.
Methods
Population and data
We used data from the Clinical Practice Research Datalink (CPRD), previously known as the GPRD, which is derived from computerised clinical records produced during consultations in primary care. The CPRD database contains information from GP practices in the UK using the Vision software system (roughly 9% of UK practices) who consent to data collection; the sample is broadly representative of the adult UK population.26 Only GP practices in England are eligible for linkage to other data sets such as hospital admissions and practices can opt out of linkage. CPRD provided anonymised primary care records and linked secondary care and mortality records on patients registered between 2000 and 2015 in 404 primary care practices in England. Data were available on nearly 6 million people aged over 16 years old. GPs enter data on tests, diagnoses and symptoms using Read codes that are a hierarchical alphanumeric system similar to, but more extensive than International Classification of Disease (ICD) codes. The list of Read codes used to identify (1) HIV tests25 (2) HIV diagnoses25 (3) pregnancy/delivery/abortion27 and (4) additional CPRD browser pregnancy medcodes is listed as appendices 1 to 4, respectively, in the online supplementary file. We used individual level quintiles of the Index of Multiple Deprivation (IMD), 2015.28 Practices were classified as rural, urban conurbation or city/town at lower super output level (a small area geographic boundary of around 1500 people) in England based on Office for National Statistics classifications, 2011,29 and as within or outside London. Ethnicity was grouped as Asian, Black African, Black Caribbean, Other, White and unknown based on linked Hospital Episode Statistics data.
bmjopen-2018-027744supp001.pdf (551.1KB, pdf)
We used national surveillance data from Public Health England (PHE) on testing in primary care derived from general practices that submit HIV tests to laboratories participating in the Sentinel Surveillance of Blood Borne Virus Testing (SSBBV). These practices cover 35% of England’s primary care population. HIV testing data are captured from 66% of the primary care population in extremely high prevalence areas (>5/1000), 37% within high prevalence areas (>2/1000) and 29% within low prevalence areas. These data exclude any point of care tests carried out by GPs, and tests carried out as part of antenatal screening. The latest data available on testing rates and positivity were for 2015.30 Data on HIV prevalence were derived from the HIV and AIDS Reporting System (HARS) and for earlier years the Survey of Prevalent HIV Infections Diagnosed (SOPHID) available from PHE.2 These data were available up to 2015.
Patient and public involvement
Public and patients were not involved in the design of this study. Patient data from general practices were contributed via CPRD and PHE surveillance as stated earlier.
Statistical methods
HIV testing rate, positivity and prevalence of HIV recorded in primary care
Using data from CPRD we estimated the HIV testing rates for each year between 2000 and 2015, overall and by patient demographics. Testing rates were estimated for males and females, for all ages and grouped by age (16–44,≥45 years, chosen to match the study by Evans et al25). We also estimated rates separately according to whether the practice was in London or not, and by type of location. For each calendar year, the denominator used to calculate the HIV testing rate was the number of patients who were in the CPRD cohort in that year satisfying the following inclusion criteria:
They were registered before 30 June of that year.
They did not transfer to another practice or die before 30 June of that year.
They were in the same practice for at least 6 months.
They had not previously tested positive for HIV.
The numerator was the number of HIV tests carried out within the relevant year. For each patient in the denominator, the number of tests was calculated, disregarding repeat tests that were within a 3-month period. Any test done or registered more than 90 days after the first recorded positive test was ignored.
As the majority of HIV tests in women are carried out as part of antenatal screening, analyses for females were repeated excluding these tests. We identified women who were pregnant using either delivery dates or Read codes as follows:
Delivery (birth) dates associated with the females in our data: An HIV test was considered antenatal if it occurred between 3 and 9 months before the recorded delivery date.
Read codes indicating any sign of pregnancy (antenatal): In this case an HIV test was considered antenatal if it occurred within 6 months from the day the Read code was recorded.
Read codes associated with the postpartum period: In this case the HIV test was considered antenatal if it occurred within 3–10 months before the corresponding record.
Read codes indicating any sign of miscarriage or abortion: An HIV test was recorded as antenatal if it occurred between 3 months prior to 3 months after the corresponding record.
The Read codes associated with pregnancy are listed in the online supplementary material. The antenatal HIV tests were excluded from the numerator and the corresponding patients were removed from the denominator for the related period as well.
We plotted the trends in HIV testing rates per 100 000 person years for 2000–2015 separately for men and women (including and excluding antenatal HIV tests) for all adults and restricted to those aged 16–44 years old. In addition, we calculated the annual proportion of HIV tests that were positive for each year to investigate whether testing improved in terms of targeting higher risk individuals during the later years.
For the years 2005, 2010 and 2015, we estimated and tabulated HIV testing rates and incidence rate ratios (IRRs) with 95% CI from Poisson models for males and females separately according to whether practice was in London or not, by age, ethnicity, IMD and by type of location. To validate our estimates of HIV testing rates recorded in CPRD, we compared them with those from national surveillance data collected by PHE for 2015.30 Finally, we estimated the prevalence of diagnosed HIV recorded in CPRD and compared this with estimated prevalence from national surveillance data collected by PHE using SOPHID and HARS to determine the proportion of all HIV diagnoses that were recorded in CPRD. Data analysis was performed using STATA V.14.
Results
Data were available on 5 979 598 distinct patients with 45 093 761 (males 22,155,768; females 22,937,630) person years of observation. The demographic characteristics of included individuals are shown in table 1. There were less males (48%) than females (52%). Practices (15%) and individuals (16%) in the most deprived quintile of IMD were under-represented in CPRD. The total number of HIV tests recorded in CPRD between 2000 and 2015 was 159 115 of which 357 (0.2%) were positive.
Table 1.
Patient and practice demographics
| Demographic variable |
Group | Frequency | Percentage (%) |
| Gender |
Males | 2 871 884 | 48.03 |
| Females | 3 107 562 | 51.97 | |
| Other/unknown | 152 | 0.00 | |
| Age (in 2015) |
16–44 | 2 684 443 | 44.89 |
| >44 | 3 295 155 | 55.11 | |
| Ethnicity |
Asian | 147 295 | 2.46 |
| Black African | 45 632 | 0.76 | |
| Black Caribbean | 28 558 | 0.48 | |
| Other | 118 934 | 1.99 | |
| White | 3 328 189 | 55.66 | |
| Unknown | 2 310 990 | 38.65 | |
| Region |
Outside London | 4 693 116 | 78.49 |
| London | 1 129 924 | 18.90 | |
| Unknown | 156 558 | 2.62 | |
| Urban/rural |
Urban (conurbation) | 2 134 497 | 35.70 |
| Urban (city/town) | 2 991 079 | 50.02 | |
| Rural | 697 452 | 11.66 | |
| Unknown | 156 558 | 2.62 | |
| Patient IMD (2015) 1=least deprived, …, 5=most deprived | Quintile 1 | 1 285 213 | 21.49 |
| Quintiles 2,3,4 | 3 564 936 | 59.62 | |
| Quintile 5 | 964 853 | 16.14 | |
| Unknown | 164 596 | 2.75 | |
| Practice IMD (2015) 1=least deprived, …, 5=most deprived | Quintile 1 | 1 249 293 | 20.89 |
| Quintiles 2,3,4 | 3 702 313 | 61.92 | |
| Quintile 5 | 871 434 | 14.57 | |
| Unknown | 156 558 | 2.62 |
IMD, Index of Multiple Deprivation.
Trends in HIV testing rates 2000–2015 in primary care
Figure 1 shows the trend in HIV testing rates per 100 000 person years for the period 2000–2015 by gender and age group, with and without inclusion of antenatal testing. The main reason for HIV testing among women of childbearing age was antenatal screening: the testing rates (per 100 000 person-years) in all women aged 16–44 increased from 177 (95% CI 167 to 188) in 2000 to 1789 (95% CI 1757 to 1821) in 2010 and then decreased to 839 (95% CI 817 to 862) in 2015, with the corresponding figures being 23 (95% CI 19 to 26), 262 (95% CI 250 to 275) and 190 (95% CI 179 to 201) when antenatal testing was excluded. For males the corresponding rates were 26 (95% CI 22 to 29), 196 (95% CI 185 to 206) and 137 (95% CI 127 to 146), which are lower than rates for females even when antenatal tests are excluded. HIV testing rates in primary care peaked in females in 2010 (figure 1) and have declined markedly since then. In men and women not tested antenatally, HIV testing rates increased until 2012–2013, but have declined since. Similar patterns were seen when data were restricted to those aged 16–44 years only, except that rates were much higher in younger adults compared with those aged 45 years and over (online supplementary table 1 all adults, online supplementary table 2 for those aged 16–44 years).
Figure 1.
Trend in HIV testing rates per 100 000 person years for the period 2000–2015 by gender and age group, with and without inclusion of antenatal testing.
bmjopen-2018-027744supp002.pdf (43.7KB, pdf)
Trends in positive HIV diagnosis in primary care
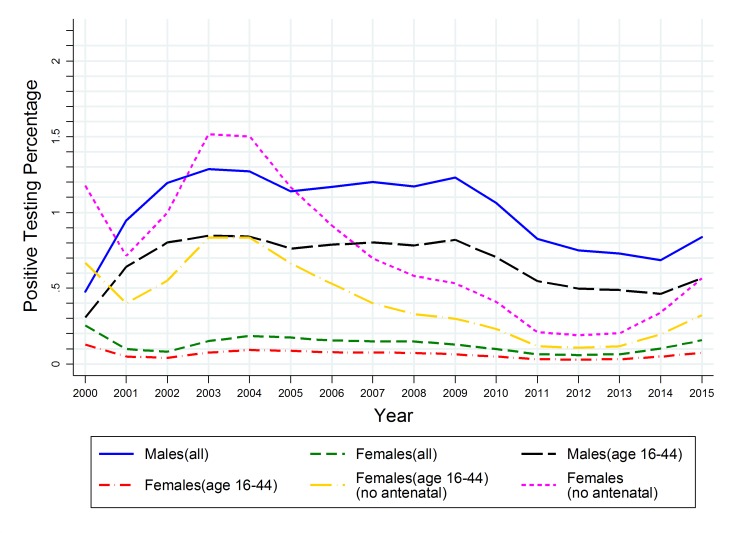
Although the number of HIV tests was much higher in women, more men tested positive: 196/20,328 (0.96%) men compared with 161/138,787 (0.12%) women. This was skewed by a very low rate of positive diagnoses in younger females who were screened antenatally. The smoothed trend in the percentage of tests that were positive for men and women of different ages is shown in figure 2 (plot of raw data is shown in online supplementary figure). Percentage positive (excluding antenatal tests) was similar in men and women before 2005, but declined more sharply in women thereafter. The percentage of tests that were positive peaked around 2003 and has fallen sharply since 2010, indicating that there is no evidence of better targeting of testing to individuals in later years.
Figure 2.
Trend in the percentage of HIV tests that were positive for the period 2000–2015 by gender and age group, with and without inclusion of antenatal testing.
bmjopen-2018-027744supp003.pdf (427.3KB, pdf)
HIV testing rates in practices within and outside London, by age and deprivation index
HIV testing rates were twofold higher in London compared with outside London for both men and women in 2005 and this differential increased in 2010 and 2015. Tables 2 and 3 give the testing rates for years 2005, 2010 and 2015 for males and females (excluding antenatal tests), respectively, stratified by whether the practices were in London or outside London. Data for all years between 2000 and 2015 are given for all adults (online supplementary table 1) and for adults aged 16–44 years (online supplementary table 2). In more recent years practices outside London but in conurbations had higher rates than those in cities or towns, which, in turn, had higher rates than rural practices. Although testing rates in men in London practices decreased between 2010 and 2015 overall from 273 (95% CI 251 to 295) to 246 (95% CI 225 to 266) per 100 000 person-years, there was evidence of a shift in targeting of testing since rates increased in older men from 151 (95% CI 127 to 176) to 180 (95% CI 154 to 206) per 100 000 person years and in the most deprived quintile from 415 (95% CI 351 to 480) to 565 (95% CI 487 to 643) per 100 000 person years. This targeting effect was also seen among women in London practices, but not in practices outside London. However, in 2015 in London it remained the case that older people were less likely to be tested: IRR for age ≥45 compared with 16–44 years was 0.59 (95% CI 0.50 to 0.71) for men and 0.46 (95% CI 0.38 to 0.55) in women. The corresponding IRRs for outside London were much lower: IRR for age ≥45 compared with 16–44 years was 0.37 (95% CI 0.32 to 0.43) in men and 0.18 (95% CI 0.16 to 0.21) in women. In contrast, by 2015 the most deprived group were two/threefold more likely to be tested than the least deprived, depending on gender and locality, with IRR for IMD quintile 5 versus 1 increasing markedly from 2005 to 2015 (table 2 (males) and table 3 (females)).
Table 2.
Testing rates (per 100 000 person years) for males and IRR with 95% CI for years 2005, 2010, 2015
| 2005 | 2010 | 2015 | |||||||
| Rate (95% CI) | IRR (95% CI) | P value | Rate (95% CI) | IRR (95% CI) | P value | Rate (95% CI) | IRR (95% CI) | P value | |
| London | |||||||||
| Overall | 133 (117 to 148) | — | — | 273 (251 to 295) | — | — | 246 (225 to 266) | — | — |
| Age | |||||||||
| 16–44 | 175 (151 to 198) | 1 | <0.0001 | 366 (333 to 400) | 1 | <0.0001 | 304 (272 to 336) | 1 | <0.0001 |
| >=45 | 75 (56 to 93) | 0.43 (0.33 to 0.56) | 151 (127 to 176) | 0.41 (0.34 to 0.50) | 180 (154 to 206) | 0.59 (0.50 to 0.71) | |||
| Ethnicity | |||||||||
| White | 102 (80 to 125) | 1 | <0.0001 | 240 (206 to 275) | 1 | <0.0001 | 222 (187 to 256) | 1 | <0.0001 |
| Asian | 152 (73 to 232) | 1.49 (0.85 to 2.62) | 329 (220 to 438) | 1.37 (0.95 to 1.96) | 167 (88 to 247) | 0.76 (0.47 to 1.22) | |||
| Black African | 669 (361 to 977) | 6.53 (3.93 to 10.85) | 1227 (849 to 1605) | 5.10 (3.63 to 7.18) | 919 (602 to 1236) | 4.15 (2.84 to 6.06) | |||
| Black Caribbean | 216 (432 to 389) | 2.11 (0.92 to 4.82) | 361 (148 to 574) | 1.50 (0.82 to 2.76) | 523 (267 to 779) | 2.36 (1.42 to 3.95) | |||
| Patient IMD (2015)* | |||||||||
| Quintile 1 | 160 (119 to 202) | 1 | 0.0912 | 207 (159 to 254) | 1 | <0.0001 | 200 (153 to 248) | 1 | <0.0001 |
| Quintiles 2,3,4 | 120 (102 to 139) | 0.75 (0.56 to 1.01) | 252 (226 to 279) | 1.22 (0.95 to 1.57) | 177 (155 to 198) | 0.88 (0.68 to 1.14) | |||
| Quintile 5 | 155 (114 to 195) | 0.96 (0.67 to 1.40) | 415 (351 to 480) | 2.01 (1.53 to 2.65) | 565 (487 to 643) | 2.82 (2.16 to 3.68) | |||
| Outside London | |||||||||
| Overall | 65 (60 to 70) | — | — | 106 (100 to 112) | — | — | 65 (60 to 69) | — | — |
| Age | |||||||||
| 16–44 | 95 (87 to 103) | 1 | <0.0001 | 161 (150 to 172) | 1 | <0.0001 | 100 (91 to 109) | 1 | <0.0001 |
| >=45 | 34 (29 to 39) | 0.36 (0.30 to 0.42) | 54 (48 to 60) | 0.34 (0.30 to 0.38) | 37 (32 to 42) | 0.37 (0.32 to 0.43) | |||
| Ethnicity | |||||||||
| White | 63 (57 to 69) | 1 | <0.0001 | 100 (92 to 108) | 1 | 63 (57 to 70) | 1 | ||
| Asian | 159 (89 to 229) | 2.52 (1.61 to 3.94) | 336 (245 to 427) | 3.36 (2.55 to 4.44) | 200 (135 to 266) | 3.16 (2.25 to 4.45) | |||
| Black African | 579 (221 to 937) | 9.17 (4.90 to 17.16) | 1321 (859 to 1783) | 13.24 (9.23 to 18.97) | 584 (289 to 878) | 9.22 (5.51 to 15.44) | |||
| Black Caribbean | 185 (37 to 366) | 2.93 (1.09 to 7.83) | 506 (156 to 856) | 5.06 (2.86 to 8.96) | 202 (25 to 379) | 3.19 (1.32 to 7.70) | |||
| Patient IMD (2015)* | |||||||||
| Quintile 1 | 60 (51 to 69) | 1 | 0.0002 | 98 (87 to 110) | 1 | <0.0001 | 61 (52 to 70) | 1 | <0.0001 |
| Quintiles 2,3,4 | 60 (54 to 66) | 1.0 (0.84 to 1.20) | 94 (87 to 101) | 0.96 (0.83 to 1.10) | 53 (48 to 59) | 0.87 (0.73 to 1.04) | |||
| Quintile 5 | 89 (75 to 104) | 1.49 (1.20 to 1.86) | 163 (145 to 182) | 1.66 (1.41 to 1.96) | 115 (99 to 131) | 1.89 (1.55 to 2.31) | |||
| Urban/rural class | |||||||||
| Conurbation | 65 (55 to 76) | 1 | 0.0045 | 144 (129 to 159) | 1 | <0.0001 | 91 (79 to 102) | 1 | <0.0001 |
| City/town | 69 (63 to 75) | 1.05 (0.88 to 1.26) | 100 (93 to 107) | 0.70 (0.61 to 0.79) | 60 (54 to 65) | 0.66 (0.56 to 0.77) | |||
| Rural | 47 (37 to 58) | 0.72 (0.55 to 0.95) | 75 (62 to 88) | 0.52 (0.43 to 0.64) | 49 (39 to 60) | 0.55 (0.43 to 0.70) | |||
*1=least deprived - 5=most deprived.
IMD, Index of Multiple Deprivation; IRR, incidence rate ratio.
Table 3.
Testing rates (per 100 000 person years) for females and IRR with 95% CI for years 2005, 2010, 2015 (antenatal testing excluded)
| 2005 | 2010 | 2015 | |||||||
| Rate (95% CI) | IRR (95% CI) | P value | Rate (95% CI) | IRR (95% CI) | P value | Rate (95% CI) | IRR (95% CI) | P value | |
| London | |||||||||
| Overall | 139 (123 to 155) | — | — | 309 (285 to 332) | — | — | 243 (223 to 264) | — | — |
| Age | |||||||||
| 16–44 | 216 (189 to 242) | 1 | <0.0001 | 479 (440 to 517) | 1 | <0.0001 | 327 (295 to 360) | 1 | <0.0001 |
| >=45 | 39 (26 to 52) | 0.18 (0.13 to 0.26) | 93 (74 to 112) | 0.19 (0.16 to 0.24) | 150 (127 to 173) | 0.46 (0.38 to 0.55) | |||
| Ethnicity | |||||||||
| White | 120 (100 to 140) | 1 | <0.0001 | 270 (239 to 301) | 1 | <0.0001 | 170 (144 to 195) | 1 | <0.0001 |
| Asian | 199 (117 to 280) | 1.65 (1.09,2.51) | 261 (183 to 339) | 0.97 (0.70 to 1.33) | 190 (126 to 254) | 1.12 (0.78 to 1.62) | |||
| Black African | 415 (234 to 596) | 3.46 (2.21 5.43) | 825 (602 to 1048) | 3.06 (2.29 to 4.08) | 728 (527 to 929) | 4.30 (3.13 to 5.87) | |||
| Black Caribbean | 248 (96 to 400) | 2.06 (1.15 to 3.72) | 438 (260 to 617) | 1.63 (1.06 to 2.48) | 399 (221 to 578) | 2.35 (1.50 to 3.70) | |||
| Patient IMD (2015)* | |||||||||
| Quintile 1 | 153 (112 to 194) | 1 | 0.0278 | 172 (130 to 215) | 1 | <0.0001 | 156 (115 to 197) | 1 | <0.0001 |
| Quintiles 2,3,4 | 125 (106 to 143) | 0.82 (0.60 to 1.10) | 284 (258 to 311) | 1.65 (1.27 to 2.14) | 195 (173 to 218) | 1.25 (0.95 to 1.66) | |||
| Quintile 5 | 183 (138 to 227) | 1.19 (0.84 to 1.71) | 539 (463 to 615) | 3.13 (2.37 to 4.14) | 520 (448 to 592) | 3.33 (2.50 to 4.46) | |||
| Outside London | |||||||||
| Overall | 67 (62 to 71) | — | — | 117 (111 to 123) | — | — | 83 (78 to 89) | — | — |
| Age | |||||||||
| 16–44 | 118 (108 to 127) | 1 | <0.0001 | 216 (204 to 229) | 1 | <0.0001 | 160 (148 to 171) | 1 | <0.0001 |
| >=45 | 21 (17,24) | 0.18 (0.15 to 0.21) | 34 (29 to 38) | 0.16 (0.14 to 0.18) | 29 (25 to 33) | 0.18 (0.16 to 0.21) | |||
| Ethnicity | |||||||||
| White | 67 (61 to 72) | 1 | <0.0001 | 117 (110 to 125) | 1 | <0.0001 | 77 (71 to 83) | 1 | <0.0001 |
| Asian | 188 (123 to 252) | 2.82 (2.01 to 3.95) | 357 (284 to 430) | 3.04 (2.46 to 3.77) | 207 (155 to 259) | 2.69 (2.07 to 3.50) | |||
| Black African | 515 (270,) | 7.33 (4.77 to 12.53) | 829 (563 to 1094) | 7.07 (5.13,9.73) | 432 (249 to 616) | 5.63 (3.71 to 8.53) | |||
| Black Caribbean | 235 (61 to 409) | 3.53 (1.68 to 7.44) | 778 (468 to 1087) | 6.63 (4.49 to 9.79) | 489 (257 to 721) | 6.36 (3.93 to 10.30) | |||
| Patient IMD (2015)* | |||||||||
| Quintile 1 | 64 (54 to 73) | 1 | 0.0001 | 95 (84 to 106) | 1 | <0.0001 | 71 (61 to 81) | 1 | <0.0001 |
| Quintiles 2,3,4 | 61 (55 to 67) | 0.97 (0.81 to 1.15) | 95 (88 to 102) | 1.00 (0.87 to 1.15) | 72 (65 to 78) | 1.01 (0.86 to 1.19) | |||
| Quintile 5 | 92 (77 to 107) | 1.45 (1.17 to 1.79) | 241 (218 to 265) | 2.54 (2.19 to 2.95) | 152 (134 to 170) | 2.15 (1.80 to 2.57) | |||
| Urban/rural class | |||||||||
| Conurbation | 54 (45 to 64) | 1 | 0.0078 | 165 (148 to 181) | 1 | <0.0001 | 120 (106 to 133) | 1 | <0.0001 |
| City/town | 72 (66 to 78) | 1.33 (1.10 to 1.60) | 108 (101 to 116) | 0.66 (0.59 to 0.74) | 77 (70 to 83) | 0.64 (0.56 to 0.74) | |||
| Rural | 62 (50 to 74) | 1.15 (0.89 to 1.47) | 85 (71 to 99) | 0.52 (0.43 to 0.62) | 60 (48 to 72) | 0.50 (0.40 to 0.62) | |||
*1=least deprived - 5=most deprived.
IMD, Index of Multiple Deprivation; IRR, incidence rate ratio.
HIV testing rates and positivity according to national surveillance data
For comparison, national surveillance data for 2015 estimated that general practices in extremely high prevalence areas (defined as greater than 5/1000 population, comparable with ‘London’ in our CPRD study) carried out the highest number of tests per practice population 860 per 100 000 person years. This was nearly double the coverage rate of general practices in high diagnosed prevalence areas (defined as greater than 2/1000 population), which was estimated at 440 per 100 000 person years, and ten times the coverage rate among general practices in low diagnosed prevalence areas, which was estimated at 90 per 100 000 person years. The estimates of HIV testing rates from surveillance were higher than our estimates from CPRD (tables 2 and 3). The proportion of positive tests among those tested in primary care estimated from SSBBV surveillance data was 0.4% in 2015.30 This varied from 0.5% in very high prevalence areas to 0.2% in low prevalence areas and was consistent with our estimated positivity (figure 2).
Prevalence of recorded HIV in CPRD and comparison with national surveillance estimates
In 2015 the prevalence of diagnosed HIV recorded in CPRD was 2.8 per 1000 adult patients in London practices and 0.8 per 1000 in the rest of the UK (table 4). According to PHE surveillance, in 2015 HIV prevalence in UK was estimated to be 1.6 per 1000, and excluding undiagnosed HIV was 1.3 per 1000 population.2 The HIV prevalence in London was estimated to be 4.7 per 1000, substantially higher than the rest of the UK at 1.1 per 1000. The corresponding observed prevalence, that is, excluding undiagnosed cases of HIV, was 4.2 and 0.9 per 1000 population in London and the rest of the UK, respectively.2 However, these percentages are likely to be overestimated as children aged <16 years were not included in the CPRD calculations of prevalence but were included in PHE data. In general practices in London, prevalence of HIV recorded in CPRD was higher for males, older individuals, Black African ethnicity and most deprived quintile (table 4) with a similar pattern in practices outside London except that prevalence did not vary by age.
Table 4.
Prevalence (with 95% CI) of diagnosed HIV recorded in CPRD (per 100 000 persons) by gender, age, ethnicity and patient IMD, for London and outside London
| Prevalence (95% CI) | |||
| 2005 | 2010 | 2015 | |
| London | |||
| All | 140 (129 to 151) | 230 (216 to 244) | 282 (267 to 297) |
| Gender | |||
| Males | 191 (172 to 209) | 294 (271 to 317) | 369 (344 to 395) |
| Females | 91 (78 to 103) | 170 (153 to 187) | 199 (181 to 217 |
| Age | |||
| 16–44 | 168 (152 to 184) | 234 (215 to 253) | 229 (210 to 249) |
| >44 | 103 (88 to 117) | 226 (205 to 247) | 341 (316 to 365) |
| Ethnicity | |||
| White | 127 (112 to 143) | 183 (164 to 202) | 224 (202 to 246) |
| Asian | 45 (17 to 72) | 84 (50 to 119) | 96 (60 to 131) |
| Black African | 1465 (1205 to 1726) | 2350 (2055 to 2646) | 2597 (2294 to 2899) |
| Black Caribbean | 195 (97 to 294) | 431 (291 to 572) | 538 (381 to 695) |
| Patient IMD (2015) | |||
| Quantile 1 | 32 (19 to 45) | 86 (65 to 107) | 121 (96 to 146) |
| Quantiles 2,3,4 | 136 (122 to 149) | 212 (195 to 228) | 256 (238 to 274) |
| Quantile 5 | 268 (230 to 306) | 444 (397 to 491) | 544 (492 to 596) |
| Outside London | |||
| All | 38 (36 to 41) | 64 (61 to 67) | 81 (77 to 85) |
| Gender | |||
| Males | 50 (46 to 54) | 81 (76 to 86) | 105 (99 to 110) |
| Females | 26 (23 to 29) | 48 (44 to 52) | 58 (54 to 62) |
| Age | |||
| 16–44 | 55 (51 to 59) | 78 (72 to 83) | 82 (76 to 87) |
| >44 | 22 (19 to 25) | 52 (48 to 56) | 80 (76 to 85) |
| Ethnicity | |||
| White | 29 (26 to 32) | 46 (43 to 50) | 60 (56 to 64) |
| Asian | 37 (16 to 59) | 40 (21 to 59) | 55 (34 to 76) |
| Black African | 2537 (2110 to 2964) | 3663 (3236 to 4091) | 3933 (3514 to 4353) |
| Black Caribbean | 135 (35 to 236) | 347 (195 to 499) | 484 (308 to 660) |
| Patient IMD (2015) | |||
| Quantile 1 | 19 (16 to 23) | 31 (26 to 35) | 42.58 (37 to 48) |
| Quantiles 2,3,4 | 35 (32 to 38) | 60 (56 to 65) | 77 (72 to 81) |
| Quantile 5 | 82 (72 to 91) | 132 (121 to 144) | 159 (146 to 172) |
IMD, Index of Multiple Deprivation.
Discussion
Statement of principal findings
Our analysis of CPRD data on GP consultations recorded on approximately 6 million people living in the UK over a 15-year period shows that the initial rise in HIV testing seen in primary care between 2000 and 2010 reversed with a significant drop in the testing rates for HIV in primary care from 2010. This is an unexpected finding as throughout this period prevalence of HIV has been increasing which should have engendered higher rates of testing in primary care, given the NICE recommendations on testing, which would increase with increased prevalence.31 32 HIV testing rates in primary care were higher in women than men throughout the study period, even when tests for antenatal screening were excluded, despite HIV prevalence being higher in men. This resulted in men being eightfold more likely to test positive than women in this setting. Over the 15-year period of the study, there were approximately two positive results per 1000 HIV tests. We did not find evidence of better targeting of HIV testing to individuals in more recent years as the percentage of tests that were positive peaked around 2003. Many individuals at high risk of HIV infection may choose to test in settings other than general practice, such as sexual health clinics, which might make it harder to target HIV testing among the population attending primary care.
The pattern of HIV testing has also changed over time. Testing was twofold higher in London than elsewhere and has increased in the groups and areas of high deprivation within London. This is reassuring as it also reflects the higher prevalence of HIV in these areas and indicates that HIV testing has become more geographically targeted. Overall, testing rates were higher in urban conurbations and cities than in rural areas reflecting the national prevalence figures.2 Younger people were more likely to be tested than those aged 45 years and over, which reflects the incidence pattern for HIV. However, our data show an increasing trend in the rate of testing among the older age group in London, but not elsewhere, which may have been driven by the recognition that among those with HIV infection the proportion diagnosed late is higher in older age groups.33
In 2015, the prevalence of HIV recorded in CPRD was over threefold higher in London than elsewhere, but overall was substantially lower than the prevalence of diagnosed HIV estimated from PHE surveillance.2 This may be due to HIV-positive individuals not using primary care or to non-disclosure of their HIV status to their GP, not recording of the diagnosis on GP systems, or to CPRD not including sufficient practices with high HIV prevalence. CPRD is broadly representative of primary care in the UK, but the UK HIV epidemic is concentrated in cities with approximately half of HIV-positive individuals living in London.2 The estimated percentage of HIV diagnoses among adults that were recorded in CPRD increased between 2005 and 2015 but was still substantially lower in London than elsewhere. This trend may reflect the ageing HIV population’s greater requirement of primary care services, decrease in stigma of disclosure, or better transfer and recording in primary care of positive results of HIV tests carried out in other settings in later years.
Strengths and weaknesses of the study
This study is very large with data from nearly six million patients followed over 15 years with detailed primary care records. This detailed coverage enabled us to accurately measure HIV testing rates according to the important factors of deprivation, urbanisation, gender, ethnicity and age. Records were collected prospectively and electronically over a significant time period; therefore, we were able to show clearly the trends that have occurred. Our analysis and the data collection may be biased by several factors. The CPRD only includes a sample of general practices, but this is broadly representative of primary care in the UK, and, given the large numbers, this is a sufficient sample size for estimates of testing rates to be accurate. We have shown the CPRD slightly under-represents deprivation, in both individuals and GP practices. While this may be the case, given the very large sample size, we think that we can still draw valuable conclusions from this data. This study can only show the composite rates of testing in primary care. We were not able to categorise the different indications for an HIV test. What is clear, given the number of HIV positive patients, is that many patients will have been diagnosed in other healthcare settings, for example, PHE estimated that in England during 2016 5.9% and 7.3% of new diagnoses in men and women, respectively, were made in primary care.34 This implies that estimates of the prevalence of diagnosed HIV based on diagnoses recorded in CPRD will be under-estimates for the UK which we have shown by comparing with surveillance data from PHE.
Strengths and weaknesses in relation to other studies, discussing important differences in results
HIV testing in primary care in the Netherlands also decreased between 2010 and 2015 despite similar guidelines encouraging more pro-active screening for HIV.35 Although HIV testing in primary care has declined, the rates of late diagnosis (CD4 count less than 350 cells/mL) have also declined from 50% in 2010 to 39% in 2015,36 indicating a discordancy between the testing in primary care and diagnosis. This indicates that increased testing has likely occurred in other settings. Earlier diagnosis may be due to better detection in secondary care, either from screening or testing those with indicator conditions, or through other routes such as sexual health clinics, insurance requests or specialist testing services. Moreover, if testing has become better targeted in primary care and incidence in the consulting population is decreasing then even without an increase in testing, those who get tested may be tested earlier in the course of HIV infection leading to reduced rates of late diagnoses. However, we have shown a significant decline in HIV testing in primary care since the previous analysis by Evans et al25 on testing up to 2005, and therefore we can look at increased testing in primary care as an option to improve early HIV detection rates.
Meaning of the study: possible explanations and implications for clinicians and policymakers
Since 2015, UK and international treatment guidelines37 for those diagnosed with HIV recommend immediate treatment with antiretroviral therapy due to findings from the START trial.38 This change, together with pre-exposure prophylaxis, has resulted in a decline in HIV infection rates for the last 2 years34. Nevertheless, there are still opportunities for diagnosing HIV earlier in primary care while testing rates remain very low. Current UK testing guidelines34 recommend people attending general practices in areas of high HIV prevalence should be offered an HIV test at registration or when having a blood test if they have not had an HIV test in the past 12 months. People newly diagnosed with an HIV indicator condition should also be offered an HIV test. The aim is to diagnose HIV earlier as late diagnosis of HIV is associated with increased morbidity and mortality.7 39 40 There are benefits for diagnosing HIV earlier both for the individual in terms of quality of life and life expectancy6 and a wider societal benefit of reduced transmission and lower NHS treatment costs.
Unanswered questions and future research
Although it is a public health imperative, and target, to increase HIV testing and diagnosis, it is unclear how this could be implemented in primary care. A literature review undertaken of public and HCP attitudes towards HIV testing in the UK showed that a proactive offer of an HIV test by the HCP was an important factor which could help increase testing rates.20 Reasons for low levels of HIV testing by the HCP include fear/concern of offending patients, inadequate knowledge/training on HIV, low awareness of current testing guidelines, underestimation of patient risk, insufficient time, competing priorities, perceived burdensome consent process and pre-test discussion.18–20 41 Studies indicate a need for education and training on HIV testing for HCP in primary care to overcome these barriers to testing.16 42 Adequate interventions are needed to address these barriers so individuals can receive a timely HIV test and with it the important treatment benefits and care if found to be HIV positive. Another literature review has provided evidence that HIV indicator conditions have the potential to be used more effectively as triggers for earlier HIV testing.43 Opt-out testing can facilitate increased HIV testing as has been evident from a trial in emergency care setting.44 When blood tests are carried out for any reason in primary care, there could also be an opt-out HIV test. Computer prompts based on risk algorithms are another strategy to support HIV testing45–49 which could be based on electronic health records such as those in CPRD.
Although the results shown here are for a UK-based population the methodology may be applicable to other healthcare systems. They provide accurate testing rates and detection rates in primary care which are measures of HIV testing that can be used for international comparisons. A key element for preventing transmission and late diagnosis of HIV is testing in primary care, based on a screening strategy or indicator conditions.50 These data inform us of the current situation on testing and will be useful in planning and evaluating interventions to improve this.
The data on the discrepancy between PHE and CPRD prevalence of HIV positive status being recorded are another finding of importance for planning. New testing strategies such as home test and rapid testing outside of standard healthcare settings may contribute to the decrease in testing in primary care. These need to have a strategy in their delivery to feed back to primary care to maximise the benefits to patients and their health networks.
Conclusions
HIV testing rates have declined in primary care in all age groups, although there has been a fall in late presentation. HIV testing rates are highest in London, and higher in urban areas than rural areas. Increased testing would likely increase the number of positive tests and help prevent late diagnosis. Further interventions to increase selectivity of testing (positive cases per test) may be required, either at the individual level using risk factors and HIV indicator conditions or at the practice level using knowledge of local HIV prevalence.
Supplementary Material
Acknowledgments
We would like to thank the following authors; Joni Jackson, Natalia V. Lewis, Gene S Feder, Penny Whiting, Timothy Jones, John Macleod and Maria Theresa Redaniel for sharing their medical codes to identify pregnancy, delivery and abortion used in our data analysis.
Footnotes
Contributors: MG and MM planned the research study and were responsible for study design. JM and TJ advised on study design. CD applied for ethics approval and did the literature search. TJ and CD obtained data from the CPRD and helped with coding and extracting data. SM was responsible for statistical analyses, tables and graphs. MM, SM and MG wrote the first draft of the paper. All authors contributed to writing and revising the paper and agreed to submission. MM acts as guarantor for the conduct of the study, had full access to the data and made decision to publish.
Funding: The study was supported by Research Capability Funding from North Bristol NHS Trust. This study is based in part on data from the Clinical Practice Research Datalink (CPRD) obtained under licence from the UK Medicines and Healthcare products Regulatory Agency. This report is independent research supported by the National Institute for Health Research (NIHR) Health Protection Research Unit in Evaluation of Interventions at University of Bristol in partnership with Public Health England. TJ’s time is supported by the NIHR Collaboration for Leadership in Applied Health Research and Care West at University Hospitals Bristol NHS Foundation Trust. MM is also supported by the NIHR Biomedical Research Centre at University Hospitals Bristol NHS Foundation Trust and the University of Bristol. However, the interpretation and conclusions contained in this report are those of the authors and not necessarily those of the National Health Service, the NIHR, the CPRD or the Department of Health.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: The protocol was submitted to and approved by the independent scientific advisory committee for the CPRD (protocol ISAC number 16_172A). The study was approved by the South West, Frenchay, Research Ethics Committee on 19 September 2016 (REC reference 16/SW/0286).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data relevant to the study are included in the article or uploaded as supplementary information.
References
- 1. Brown AE, Kirwan PD, Chau C, et al. Towards elimination of HIV transmission, AIDS and HIV-related deaths in the UK – 2017 report. London: Public Health England, 2017. [DOI] [PubMed] [Google Scholar]
- 2. Kirwan PC C, Brown AE, Delpech VC. HIV in the UK - 2016 report. London: Public Health England; 2016. [Google Scholar]
- 3. Ellis S, Curtis H, Ong ELC, et al. HIV diagnoses and missed opportunities. Results of the British HIV association (BHIVA) national audit 2010. Clin Med 2012;12:430–4. 10.7861/clinmedicine.12-5-430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chadborn TR, Delpech VC, Sabin CA, et al. The late diagnosis and consequent short-term mortality of HIV-infected heterosexuals (England and Wales, 2000-2004). AIDS 2006;20:2371–9. 10.1097/QAD.0b013e32801138f7 [DOI] [PubMed] [Google Scholar]
- 5. Girardi E, Sabin CA, Monforte Antonella D'Arminio. Late diagnosis of HIV infection: epidemiological features, consequences and strategies to encourage earlier testing. J Acquir Immune Defic Syndr 2007;46 Suppl 1:S3–8. 10.1097/01.qai.0000286597.57066.2b [DOI] [PubMed] [Google Scholar]
- 6. May M, Gompels M, Delpech V, et al. Impact of late diagnosis and treatment on life expectancy in people with HIV-1: UK Collaborative HIV cohort (UK chiC) study. BMJ 2011;343:d6016 10.1136/bmj.d6016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Croxford S, Kitching A, Desai S, et al. Mortality and causes of death in people diagnosed with HIV in the era of highly active antiretroviral therapy compared with the general population: an analysis of a national observational cohort. Lancet Public Health 2017;2:e35–46. 10.1016/S2468-2667(16)30020-2 [DOI] [PubMed] [Google Scholar]
- 8. Beck EJ, Mandalia S, Sangha R, et al. The cost-effectiveness of early access to HIV services and starting cART in the UK 1996-2008. PLoS One 2011;6:e27830 10.1371/journal.pone.0027830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rodger AJ, Cambiano V, Bruun T, et al. Sexual activity without condoms and risk of HIV transmission in Serodifferent couples when the HIV-positive partner is using suppressive antiretroviral therapy. JAMA 2016;316:171–81. 10.1001/jama.2016.5148 [DOI] [PubMed] [Google Scholar]
- 10. National Institute of Health and Care Excellence (NICE) HIV testing: increasing uptake among people who may have undiagnosed HIV. Economic assessment: resource impact of recommendations, 2016. Available: https://www.nice.org.uk/guidance/GID-PHG91/documents/economic-report [Accessed Jul 2016].
- 11. National Institute of Health and Care Excellence (NICE) HIV testing: increasing uptake among people who may have undiagnosed HIV, 2016. Available: niceorguk/guidance/ng60 [Accessed Sep 2017].
- 12. Read P, Armstrong-James D, Tong CYW, et al. Missed opportunities for HIV testing–a costly oversight. QJM 2011;104:421–4. 10.1093/qjmed/hcq236 [DOI] [PubMed] [Google Scholar]
- 13. Joore IK, Arts DL, Kruijer MJP, et al. Hiv indicator condition-guided testing to reduce the number of undiagnosed patients and prevent late presentation in a high-prevalence area: a case-control study in primary care. Sex Transm Infect 2015;91:467–72. 10.1136/sextrans-2015-052073 [DOI] [PubMed] [Google Scholar]
- 14. Burns FM, Johnson AM, Nazroo J, et al. Missed opportunities for earlier HIV diagnosis within primary and secondary healthcare settings in the UK. AIDS 2008;22:115–22. 10.1097/QAD.0b013e3282f1d4b6 [DOI] [PubMed] [Google Scholar]
- 15. British HIV Association UK national guidelines for HIV testing 2008, 2008. Available: http://www.bhiva.org/HIVtesting2008.aspx [Accessed Apr 2016].
- 16. Elmahdi R, Gerver SM, Gomez Guillen G, et al. Low levels of HIV test coverage in clinical settings in the U.K.: a systematic review of adherence to 2008 guidelines. Sex Transm Infect 2014;90:119–24. 10.1136/sextrans-2013-051312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hartney T, Kennedy I, Crook P, et al. Expanded HIV testing in high-prevalence areas in England: results of a 2012 audit of sexual health commissioners. HIV Med 2014;15:251–4. 10.1111/hiv.12099 [DOI] [PubMed] [Google Scholar]
- 18. Deblonde J, De Koker P, Hamers FF, et al. Barriers to HIV testing in Europe: a systematic review. Eur J Public Health 2010;20:422–32. 10.1093/eurpub/ckp231 [DOI] [PubMed] [Google Scholar]
- 19. Bolsewicz K, Vallely A, Debattista J, et al. Factors impacting HIV testing: a review – perspectives from Australia, Canada, and the UK. AIDS Care 2015;27:570–80. 10.1080/09540121.2014.986050 [DOI] [PubMed] [Google Scholar]
- 20. Davies C, Gompels M, May M. Public and healthcare practitioner attitudes towards HIV testing: review of evidence from the United Kingdom (UK). Int STD Res Rev 2015;3:91–122. 10.9734/ISRR/2015/18724 [DOI] [Google Scholar]
- 21. Scognamiglio P, Chiaradia G, De Carli G, et al. The potential impact of routine testing of individuals with HIV indicator diseases in order to prevent late HIV diagnosis. BMC Infect Dis 2013;13:473 10.1186/1471-2334-13-473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Goodall L, Leen C. Late diagnosis of HIV: could this be avoided? Scott Med J 2011;56:84–6. 10.1258/smj.2011.011032 [DOI] [PubMed] [Google Scholar]
- 23. Joore IK, Reukers DFM, Donker GA, et al. Missed opportunities to offer HIV tests to high-risk groups during general practitioners’ STI-related consultations: an observational study. BMJ Open 2016;6:e009194 10.1136/bmjopen-2015-009194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Health Protection Agency (HPA) Time to test for HIV: expanding HIV testing in healthcare and community services in England, 2011. Available: http://www.bhiva.org/documents/Publications/Time_to_test_final_report__Sept_2011.pdf [Accessed Sep 2017].
- 25. Evans HER, Mercer CH, Rait G, et al. Trends in HIV testing and recording of HIV status in the UK primary care setting: a retrospective cohort study 1995-2005. Sex Transm Infect 2009;85:520–6. 10.1136/sti.2008.034801 [DOI] [PubMed] [Google Scholar]
- 26. Herrett E, Gallagher AM, Bhaskaran K, et al. Data resource profile: clinical practice research Datalink (CPRD). Int J Epidemiol 2015;44:827–36. 10.1093/ije/dyv098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Jackson J, Lewis NV, Feder GS, et al. Exposure to domestic violence and abuse and consultations for emergency contraception: nested case-control study in a UK primary care dataset. Br J Gen Pract 2019;69:e199–207. 10.3399/bjgp18X700277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. National Statistics English indices of deprivation 2015. statistics on relative deprivation in small areas in England, 2015. Available: https://www.gov.uk/government/statistics/english-indices-of-deprivation-2015 [Accessed Apl 2016].
- 29. Rhodes SD, Vissman AT, Stowers J, et al. A CBPR partnership increases HIV testing among men who have sex with men (MSM): outcome findings from a pilot test of the CyBER/testing Internet intervention. Health Educ Behav 2011;38:311–20. 10.1177/1090198110379572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Public Health England (PHE) Health protection report. Annual report from the sentinel surveillance study of blood borne virus testing in England: data for January to December 2015, 2016. Available: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/540332/hpr2416_bbvs.pdf [Accessed Jul 2016].
- 31. National Institute for Health and Care Excellence (NICE) Increasing the uptake of HIV testing to reduce undiagnosed infection and prevent transmission among black African communities living in England. NICE Public Health guidance 33, 2011. Available: http//:niceorguk [Accessed Oct 2014].
- 32. National Institute for Health and Care Excellence (NICE) Increasing the uptake of HIV testing among men who have sex with men. NICE Public Health Guidance 34, 2011. Available: http//:niceorguk [Accessed Sep 2014].
- 33. Tavoschi L, Gomes Dias J, Pharris A, et al. New HIV diagnoses among adults aged 50 years or older in 31 European countries, 2004-15: an analysis of surveillance data. Lancet HIV 2017;4:e514–21. 10.1016/S2352-3018(17)30155-8 [DOI] [PubMed] [Google Scholar]
- 34. Nash SGF M, Gill ON, Connor N. HIV testing in England: 2017 report. London: Public Health England, 2017. [Google Scholar]
- 35. Joore IK, van Bergen JEAM, Ter Riet G, et al. Development and evaluation of a blended educational programme for general practitioners' trainers to stimulate proactive HIV testing. BMC Fam Pract 2018;19:36 10.1186/s12875-018-0723-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Public Health England (PHE) HIV: annual data tables. HIV surveillance data in the UK by demographic characteristics and geographical region, 2015. Available: https://www.gov.uk/government/statistics/hiv-annual-data-tables [Accessed Jul 2016].
- 37. World Health Organisation (WHO) Guideline on when to start antiretroviral therapy and on pre-exposure prophylaxis for HIV. Geneva: World Health organization, 2015. Available: http://www.who.int/hiv/pub/guidelines/earlyrelease-arv/en [Accessed Jul 2017]. [PubMed]
- 38. Lundgren JD, Babiker AG, Gordin F, et al. Initiation of antiretroviral therapy in early asymptomatic HIV infection. N Engl J Med 2015;373:795–807. 10.1056/NEJMoa1506816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Sabin C. Review of life expectancy in people with HIV in settings with optimal ART access: what we know and what we don't. J Int AIDS Soc 2012;15:18076 10.7448/IAS.15.6.18076 [DOI] [Google Scholar]
- 40. Nakagawa F, Lodwick RK, Smith CJ, et al. Projected life expectancy of people with HIV according to timing of diagnosis. AIDS 2012;26:335–43. 10.1097/QAD.0b013e32834dcec9 [DOI] [PubMed] [Google Scholar]
- 41. Hunter E, Perry M, Leen C, et al. HIV testing: getting the message across—a survey of knowledge, attitudes and practice among non-HIV specialist physicians. Postgrad Med J 2012;88:59–65. 10.1136/postgradmedj-2011-130031 [DOI] [PubMed] [Google Scholar]
- 42. Pillay TD, Mullineux J, Smith CJ, et al. Unlocking the potential: longitudinal audit finds multifaceted education for general practice increases HIV testing and diagnosis. Sex Transm Infect 2013;89:191–6. 10.1136/sextrans-2012-050655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Davies C, Gompels M, May M. Use and effectiveness of HIV indicator conditions in guiding HIV testing: a review of the evidence. Int STD Res Rev 2017;6:1–27. 10.9734/ISRR/2017/36373 [DOI] [Google Scholar]
- 44. Montoy JCC, Dow WH, Kaplan BC. Patient choice in opt-in, active choice, and opt-out HIV screening: randomized clinical trial. BMJ 2016;532:h6895 10.1136/bmj.h6895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Federman DG, Kravetz JD, Vasquez LS, et al. Improving human immunodeficiency virus testing rates with an electronic clinical reminder. Am J Med 2012;125:240–2. 10.1016/j.amjmed.2011.06.034 [DOI] [PubMed] [Google Scholar]
- 46. Schrantz SJ, Babcock CA, Theodosis C, et al. A targeted, conventional assay, emergency department HIV testing program integrated with existing clinical procedures. Ann Emerg Med 2011;58:S85–8. 10.1016/j.annemergmed.2011.03.031 [DOI] [PubMed] [Google Scholar]
- 47. Goetz MB, Hoang T, Bowman C, et al. A system-wide intervention to improve HIV testing in the Veterans health administration. J Gen Intern Med 2008;23:1200–7. 10.1007/s11606-008-0637-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Menza TW, Hughes JP, Celum CL, et al. Prediction of HIV acquisition among men who have sex with men. Sex Transm Dis 2009;36:547–55. 10.1097/OLQ.0b013e3181a9cc41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Sharghi N, Bosch RJ, Mayer K, et al. The development and utility of a clinical algorithm to predict early HIV-1 infection. J Acquir Immune Defic Syndr 2005;40:472–8. 10.1097/01.qai.0000164246.49098.47 [DOI] [PubMed] [Google Scholar]
- 50. Joore IK, Twisk DE, Vanrolleghem AM, et al. The need to scale up HIV indicator condition-guided testing for early case-finding: a case-control study in primary care. BMC Fam Pract 2016;17:161 10.1186/s12875-016-0556-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2018-027744supp001.pdf (551.1KB, pdf)
bmjopen-2018-027744supp002.pdf (43.7KB, pdf)
bmjopen-2018-027744supp003.pdf (427.3KB, pdf)