Background:
As guidelines and payers increasingly recommend use of patient decision aids (DAs), evidence about the comparative effectiveness of available DAs is critical for organizations interested in implementing them. The primary purpose of this study was to compare 2 DAs with regard to their ability to help patients become informed and receive their preferred treatment (that is, make an informed patient-centered decision), shared decision-making, surgical rates, and surgeon satisfaction.
Methods:
We performed a multisite factorial randomized trial enrolling patients with hip or knee osteoarthritis. Patients were randomly assigned to use a long, detailed DA (long DA) or short, interactive DA (short DA). Eight surgeons were randomly assigned to receive a patient preference report detailing the patient’s goals and treatment preferences or to administer usual care.
Results:
We distributed 1,636 pre-visit surveys, 1,220 of which were returned (75% response rate), and 1,124 post-visit surveys, 967 of which were returned (86% response rate). The patients in the sample had a mean age (and standard deviation) of 65 ± 10 years, 57% were female, 89% were white non-Hispanic, and 67% had knee osteoarthritis. The majority (67.2%) made informed patient-centered decisions, and the rate did not vary significantly between the DA groups (p = 0.97) or between the surgeon groups (p = 0.23). Knowledge scores were higher for the short-DA group (mean difference = 9%; p < 0.001). More than half of the sample (60.5%) had surgery within 6 months after the visit, and rates did not differ significantly by DA or surgeon group. Overall, the surgeons were highly satisfied and reported that the majority (88.7%) of the visits were of normal duration or shorter.
Conclusions:
The DECIDE-OA study is, to our knowledge, the first randomized comparative effectiveness study of 2 orthopaedic DAs. The short DA outperformed the long DA with regard to knowledge scores and was comparable with respect to other outcomes. The surgeons reported high satisfaction and normal visit duration with both DAs.
Clinical Relevance:
Surgeons need to ensure that patients with osteoarthritis are well-informed and have a clear preference regarding whether to undergo hip or knee replacement surgery. The DAs used in this study may help surgeons involve patients in elective surgery decisions and meet the requirements of informed consent.
Clinical guidelines for treatment of osteoarthritis emphasize the importance of informing patients about surgical and nonsurgical options and engaging patients in shared decision-making to determine the best treatment. Patient decision aids (DAs) are educational tools that support shared decision-making, and studies have shown that DAs reduce decisional conflict and improve knowledge scores compared with those associated with usual care1. Slover et al. discussed the importance of shared decision-making in orthopaedics and emphasized the need for more research into the best type and content of DAs, the feasibility of integration into practice, and surgeon acceptance2. Recently, the Washington State Health Care Authority certified DAs for selected conditions, including 3 for hip and knee osteoarthritis, and national certification efforts were under way3,4. The certified DAs vary in format, content, and level of interactivity. As DAs proliferate and efforts to integrate shared decision-making into routine care expand, understanding the comparative effectiveness of different interventions is critical.
A key goal of shared decision-making is aligning treatments to patients’ preferences5. However, studies have shown a very limited impact of DAs on this outcome1. Furthermore, studies suggest that surgeons do not meaningfully explore patients’ preferences6-8. Interventions may need to target both patients and surgeons to achieve fully shared decision-making9. To that end, patient and surgeon advisors helped design a surgeon intervention, called a patient preference report, to promote discussion of patients’ goals and treatment preferences.
The DECIDE-OA study was designed to evaluate the comparative effectiveness of 2 certified DAs (a long, linear DA compared with a short, interactive DA) with and without a surgeon-focused intervention (patient preference report versus usual care). Specifically, we tested the following hypotheses: (1) use of the long, detailed DA would result in more informed patient-centered decisions and higher knowledge scores than the short DA; (2) use of the short, interactive DA would result in more patients having a clear treatment preference than the long DA; and (3) surgeon intervention (instead of usual care) would increase the number of patients receiving their preferred treatment.
Materials and Methods
The reporting follows the CONsolidated Standards Of Reporting Trials (CONSORT) guidelines and Standards for UNiversal reporting of patient Decision Aid Evaluation (SUNDAE) guidelines10,11. The Partners Human Research Committee was the central institutional review board and approved all study activities. This study is registered in ClinicalTrials.gov (NCT02729831). Details on the design, interventions, and hypotheses are available in the published study protocol12.
Design
The multisite study was a 2 × 2 factorial randomized trial (see Table I for details on the study arms) at 3 sites with 8 surgeons. Surgeons at each site were assigned to 1 of 2 groups matched with regard to patient volume and years in practice. One group was randomly assigned to administer usual care and the other, to receive the patient preference report. Patients were randomly assigned to receive either the short DA or the long DA, stratified by site. Patients received the DA before the visit and were surveyed before the visit and after use of the DA (T1); at 1 week after the visit (T2); and 6 months later or, if they had surgery, 6 months postoperatively (T3). Surgeons who received the patient preference report did so before the visit. Neither the study participants nor the study staff were blinded to the interventions. The statistician conducting the analyses was blinded to the study arms.
TABLE I.
Four Study Groups in the 2 × 2 Factorial Trial
| Surgeon Group | ||
| Usual Care | Patient Preference Report | |
| DA group | ||
| Long | Group 1: patients receive long, detailed DA; surgeon does not receive report | Group 2: patients receive long, detailed DA; surgeon receives report |
| Short | Group 3: patients receive short, interactive DA; surgeon does not receive report | Group 4: patients receive short, interactive DA; surgeon receives report |
Whenever there was a post-randomization exclusion, the allocation was reassigned to the next available new patient to maintain the randomization sequence. The threat to validity was minimal since the process of identifying the next patient was based on the date of scheduled visits, which did not allow for human manipulation.
Setting and Participants
Participants were recruited from an academic medical center, community hospital, and orthopaedic specialty hospital from April 2016 through December 2017. Study staff screened all new patients of participating surgeons 2 weeks prior to their visit. Due to the limited data available before the visit, staff confirmed eligibility after the visit. Patients needed to be 21 years of age or older, read and speak English or Spanish, have a diagnosis of hip or knee osteoarthritis, and attend the visit with the surgeon. Criteria for exclusion were a DA in the prior 12 months, a joint replacement within the prior 5 years, a hip fracture or aseptic necrosis in the prior 12 months, a diagnosis of rheumatoid or psoriatic arthritis, cognitive impairment such that the patient was unable to consent to participate, or a non-osteoarthritis-related reason for the visit.
Interventions
The short DAs (Healthwise, 2016) were Knee Osteoarthritis: Is It Time to Think About Surgery? and Hip Osteoarthritis: Is It Time to Think About Surgery?”; these DAs are available as online interactive tools (which were used in this study) and can also be printed as 12-page brochures13,14. The long DAs (Health Dialog, 2016) were “Treatment Choices for Knee Osteoarthritis,” which is available as a 43-minute DVD and 52-page booklet, and “Treatment Choices for Hip Osteoarthritis,” which is available as a 45-minute DVD and 44-page booklet15. These DVDs and booklets were used in this study; the same content is available online. The patient preference report included patients’ responses to 3 items: (1) 3 activities that the patient wanted or needed to do but was unable to do because of knee or hip symptoms, (2) treatment preference, and (3) the main goal for the visit. A sample report is provided in the Appendix.
Outcome Measures
The primary outcome was the informed patient-centered decision, a binary variable derived from responses to the short version of the Hip/Knee Osteoarthritis Decision Quality Instrument16, which was administered after the patients used the DA and before they visited the surgeon (T1) and shortly after the surgeon visit (T2). The short version contains 5 decision-specific knowledge items and 1 treatment preference item (surgery, nonsurgical, or not sure). The knowledge items are summed into a knowledge score (0% to 100%). The informed patient-centered decision variable is the percentage of patients who have a knowledge score of ≥60% and who received their preferred treatment within 6 months after the visit. The informed patient-centered decision variable is a National Quality Forum (NQF)-endorsed measure that is associated with improved outcomes5. The treatment received—i.e., joint replacement surgery (within 6 months after the visit) or nonsurgical treatment—was self-reported by the patients or collected via chart review.
Secondary outcomes included shared decision-making, decisional conflict, overall and disease-specific quality of life, and surgical rates. The Shared Decision Making Process (SDMP) survey, administered at T2, is a 4-item survey that assesses discussion of nonsurgical options, pros and cons of surgery, and patient preferences17,18. The total score ranges from 0 to 4, with higher scores indicating more shared decision-making. The SDMP survey has been endorsed by the NQF as a measure of shared decision-making for elective surgery. Overall health status was measured at T1 with the EuroQol 5-Dimensions (EQ-5D) score, a 6-item summary measure with scores ranging from −0.11 (worst) to 1.0 (perfect) health19,20. At T1, the Knee injury and Osteoarthritis Outcome Score (KOOS), which has been used extensively to assess patients’ opinions about their knee, was completed as well19,21-25. Finally, the Harris hip score (HHS) was used at T1 to assess pain, function, range of motion, and deformity of each hip; scores range from 0 to 100, with higher scores indicating less dysfunction26-28.
Age, sex, race/ethnicity, comorbidity (Charlson comorbidity index), body mass index (BMI), insurance status, literacy (evaluated with the Single Item Literacy Screener29), and DA usage were collected via self-report and chart review.
Eight surgeons completed a short survey after the visit for a random sample of 30% of the enrolled patients. The survey included 7 items about the surgeon’s satisfaction with the visit, the duration of the visit, the treatment recommendation, and the surgeon’s perception of the patient’s treatment preference and of the patient’s satisfaction.
Analyses
Responders and non-responders were compared across groups to examine non-response bias. We also examined the balance of demographic and clinical characteristics across the arms of the study. For patient-reported measures, missing data were handled according to established protocols for the validated surveys.
The sample size calculations included consideration of potential interaction effects and clustering of patients within surgeons. The target sample of 280 in each of the 4 arms at T1 provided an 89% power to detect a difference in informed patient-centered decisions of 18%—i.e., the difference between 65% for patients using the short DA and 83% for those using the long DA.
There was no interaction between the DA and surgeon groups; therefore, separate analyses were conducted for each. For the comparisons of the surgeon groups, we performed regression modeling to adjust for imbalances in patient characteristics. No adjustments were needed for the DA groups. For the T1 outcomes (those assessed before any patient contact with the surgeon), patients were treated as independent observations. For the T2 outcomes, we used the generalized estimating equation (GEE) approach to account for clustering of patients within surgeons. We used the intention-to-treat approach in the testing of all hypotheses.
The heterogeneity of the treatment effect (HTE) analyses tested the interaction between interventions and different factors on study outcomes. Specific hypotheses regarding subgroups were explored, including the impact of age, literacy, DA use, and mode of delivery (online versus paper) on knowledge scores as well as the impact of age, sex, literacy, baseline symptom scores, DA use, and mode of delivery on treatment preferences, informed patient-centered decision rates, and surgical rates.
Exploratory analyses were performed using logistic regression with the GEE approach to examine the impact of prior experience with DA use, sex, age, literacy, DA use, and pre-visit treatment preference on surgeon satisfaction with the visit and perception of the duration of the visit.
All analyses were conducted with SAS version 9.4 (SAS Institute).
Results
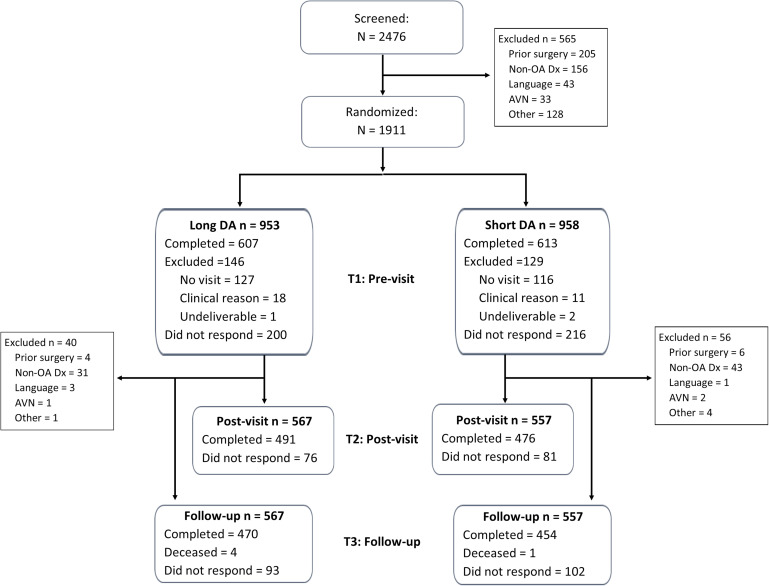
Figure 1 shows the flow of patients across the study. Of note, 275 subjects were excluded after randomization, mainly because they did not show up for their appointment (n = 243). Responders to the T1 survey were slightly younger than non-responders (mean age and standard deviation, 65 ± 10 compared with 66 ± 10 years; p = 0.02) and more likely to have knee osteoarthritis (66% compared with 58%; p = 0.007), but they did not differ by sex, mode of DA delivery, site, or study arm. Responders at T2 were slightly older (mean age, 65 ± 10 compared with 63 ± 10 years; p = 0.009) and more likely to have Medicare insurance (29% compared with 24%, p = 0.04) but did not differ with regard to any other factors.
Fig. 1.
Study CONSORT diagram. DA = decision aid, AVN = osteonecrosis, OA = osteoarthritis, and Dx = diagnosis.
Table II provides the sample characteristics of T1 responders. The sample was well balanced across the DA arms. Four factors (education, BMI, joint, and EQ-5D) were not balanced across the surgeon arms; however, the magnitudes of the differences were not clinically meaningful.
TABLE II.
Sample Characteristics
| Characteristic | Total | DA Group | Surgeon Group | ||
| Long | Short | Usual Care | Patient Preference Report | ||
| No. of patients | 1,124 | 567 | 557 | 574 | 550 |
| Age* (yr) | 65 ± 10 | 65 ± 10 | 65 ± 10 | 65 ± 10 | 65 ± 10 |
| Female (vs. male) | 57% | 56% | 58% | 58% | 57% |
| Race (white, non-Hispanic)† | 89% | 87% | 91% | 89% | 89% |
| Knee (vs. hip)‡ | 67% | 67% | 68% | 71% | 63% |
| Paper DA (vs. online) | 79% | 79% | 80% | 80% | 79% |
| High literacy (vs. low) | 86% | 86% | 85% | 84% | 87% |
| Education (≥college)‡ | 54% | 53% | 54% | 51% | 57% |
| Insurance | |||||
| Data missing | 26% | 25% | 26% | 18% | 34% |
| Medicare | 29% | 30% | 27% | 30% | 27% |
| Medicaid/dual eligible | 10% | 10% | 11% | 12% | 8% |
| Commercial | 36% | 35% | 36% | 40% | 31% |
| BMI*‡ (kg/m2) | 30.1 ± 6.5 | 30.3 ± 6.3 | 30.0 ± 6.7 | 31.1 ± 6.6 | 29.3 ± 6.4 |
| Charlson comorbidity index = 0 (vs. >0) | 73% | 74% | 73% | 74% | 73% |
| Quality of life (EQ-5D)*‡ | 0.64 ± 0.20 | 0.64 ± 0.20 | 0.64 ± 0.20 | 0.63 ± 0.20 | 0.65 ± 0.19 |
The values are given as the mean and standard deviation.
P < 0.05 for DA groups.
P < 0.05 for surgeon groups.
Informed Patient-Centered Decisions
Before the visit and after use of the DA, 40.7% of the patients met the criteria for informed patient-centered decisions and this did not vary by DA group (p = 0.38) or surgeon group (p = 0.24). After the visit, 67.2% of the sample met the criteria for informed patient-centered decisions, and again the rates were similar across the DA (p = 0.97) and surgeon (p = 0.23) groups. Exploratory analysis of HTE did not show any subgroup with a differential effect on informed patient-centered decisions.
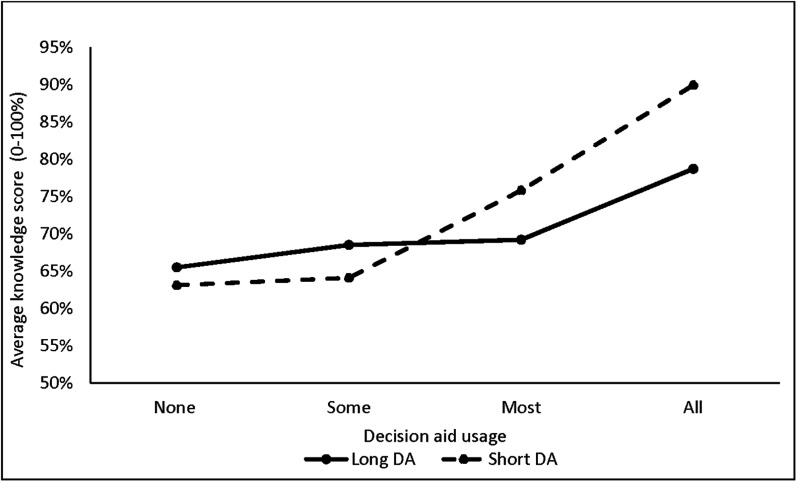
Examination of the individual components of the informed patient-centered decision variable showed that the patients who used the short DA had a higher mean knowledge score at T1 (mean difference = 9%, 95% confidence interval [CI] = 6% to 12%; p < 0.001) and T2 (mean difference = 7%, 95% CI = 3% to 10%; p < 0.001). In both DA groups, the knowledge scores were higher for patients who reported more DA usage (Fig. 2). HTE analyses showed a significant interaction between DA use and DA group (p < 0.001) with respect to knowledge at T1 and between age and DA group (p = 0.047) with respect to knowledge at T2 (Table III).
Fig. 2.
Pre-visit knowledge scores based on the amount of the DA that the patient reported reviewing.
TABLE III.
Key Findings from Analyses of Heterogeneity of Treatment Effects Assessing Impact of Intervention for Subgroups
| Subgroup | Outcome | DA Group | Surgeon Group | Interpretation | ||
| Short | Long | Patient Preference Report | Usual Care | |||
| DA use | T1 knowledge score | Mean score higher for short DA among those who reviewed all of it, but no difference among those who did not | ||||
| Patient reviewed all DA* | 90% | 79% | ||||
| Patient did not review all DA | 67% | 68% | ||||
| Age | T2 knowledge score | Mean score higher for short DA among those <65 but difference diminished among those ≥65 | ||||
| <65 yr† | 84% | 74% | ||||
| ≥65 yr | 82% | 78% | ||||
| DA mode of delivery | % patients with clear treatment preference at T2 | % with clear preference higher for short DA among those who used online version but no difference among those who used paper version | ||||
| Paper | 89% | 90% | ||||
| Online† | 93% | 89% | ||||
| Literacy | T2 SDMP score | Mean score higher for short DA among those with low literacy but no difference among those with high literacy | ||||
| Low† | 2.6 | 2.2 | ||||
| High | 2.5 | 2.5 | ||||
| Sex | T2 SDMP score | Mean score higher for patient-preference-report group among males but no difference among females | ||||
| Male† | 2.7 | 2.5 | ||||
| Female | 2.5 | 2.5 | ||||
P < 0.001 for testing interaction.
P < 0.05 for testing interaction.
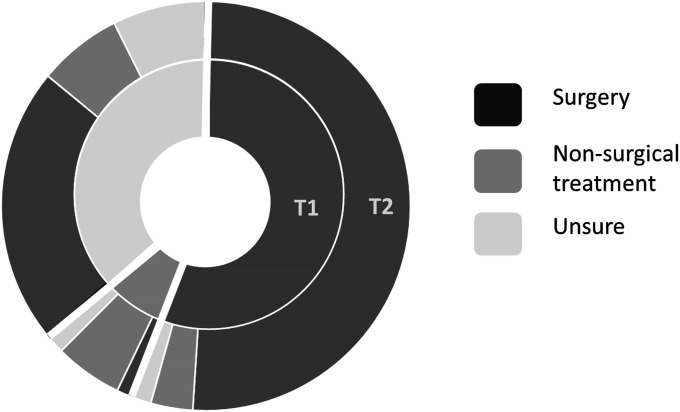
Figure 3 shows patients’ preferred treatment before and after the visit. More than one-third of the patients did not have a clear treatment preference at T1 (37.9% of those who used the long DA compared with 38.6% of those who used the short DA; p = 0.80). This percentage decreased considerably after the visit for both groups (10.5% and 10.4%, respectively, at T2; p = 0.99) (Table III).
Fig. 3.
Patient-reported treatment preference before (T1) and after (T2) the visit. The path across the circles indicates the preferences at each time point. The same color for both indicates no change in preference and a different color indicates those who changed their preference.
Most patients received the treatment that they had preferred at T2 (73.7% of those who used the long DA compared with 72.7% of those who used the short DA, p = 0.75; 73.5% in the usual-care surgeon group compared with 73.0% treated by a surgeon using the patient preference report, p = 0.34). In the entire sample, 15.7% (n = 150) preferred surgery but did not receive it (Table IV). Of those 150 respondents, 50 (33%) indicated that they had surgery scheduled in the future.
TABLE IV.
Concordance Between Patients’ Post-Visit Treatment Preference and Treatment Received
| Patient Preference | Treatment Received (no. [%]) | ||
| Surgery within 6 Mo | Nonsurgical Treatment | Total | |
| Preferred surgery | 558 (58%) | 150 (16%) | 708 (74%) |
| Preferred nonsurgical treatment | 6 (1%) | 142 (15%) | 148 (15%) |
| Not sure | 14 (1%) | 86 (9%) | 100 (10%) |
| Total | 578 (60%) | 378 (40%) | 956 (100%) |
SDMP
The overall SDMP scores were similar across the DA and surgeon groups (2.5 ± 1.1 compared with 2.5 ± 1.2 [p = 0.45] for the DA groups). Most patients reported discussion of surgery (90.2%), the reasons to have surgery (78.9%), and their treatment preference (79.9%). Less than half reported discussion of reasons not to have surgery (44.5%) or of nonsurgical treatments (44.5%). HTE analyses showed significant interactions between literacy and DA group and between patient sex and surgeon group for SDMP scores (Table III).
Surgical Rates
More than half of the sample (60.5%) had surgery within 6 months after the visit. Surgical rates did not differ across DA arms (62.5% in the long-DA group compared with 57.6% in the short-DA group; p = 0.07). There was also no difference in surgical rates between the surgeon groups (59.7% [patient preference report] compared with 60.5% [usual care]; p = 0.60). Exploratory analysis of HTE did not show any subgroup with a differential treatment effect.
Surgeon Satisfaction
We received 204 responses to 344 surveys given to the surgeons. Response rates varied significantly by site (9%, 87%, and 66%). Most surgeons were extremely or very satisfied with the visits (84.8%) and reported that the visit duration was either normal (68.6%) or shorter than normal (20.1%). These findings were consistent across DA and surgeon groups.
Surgeons with prior experience using DAs (n = 133) had a higher satisfaction rate than those at a site at which use of DAs was new (n = 71) (92.9% compared with 69.0% were extremely/very satisfied; p < 0.001) and were more likely to report normal or shorter-than-normal visit duration (96.1% compared with 77.5%; p < 0.001).
Discussion
This large, multisite randomized controlled trial provides important evidence on the comparative effectiveness of 2 certified DAs that vary in the amount of detail, level of interactivity, and use of patient narratives. Overall, both DAs performed well. The short DA was more effective in improving knowledge, particularly for younger patients, and it was also associated with higher reported shared decision-making for patients with low literacy. The surgeon intervention (patient preference report) did not have a measurable impact on outcomes. Participating surgeons reported high levels of satisfaction with both tools, and the majority did not perceive an increase in visit length with either.
The surgeon visit plays an important role in the decision-making process. Knowledge scores continued to be high after the visit, suggesting that the information in the DAs was reinforced by the surgeons and retained by the patients. Several studies of the long DA have demonstrated important benefits, including more patients making an informed choice30, higher knowledge, and lower decisional conflict17,31,32. This is the first study of which we are aware to examine the short DA, and contrary to our hypothesis it resulted in higher knowledge scores than the long DA.
The surgeon intervention (patient preference report) did not have a measurable impact on outcomes. Although the majority of the patient preference reports (494 [90%] of 550) were delivered to the surgeons for the patients who were intended to have that intervention, exit interviews with them suggest that it was not well-used during the visit. Rates of concordance between patient preferences and actual treatment were similar and high (about 73%) across the DA and surgeon arms. It may be difficult to increase these rates; however, for elective surgery decisions, ensuring that all patients receive their preferred treatment is important.
Concerns about reducing surgical rates and increasing visit duration are commonly cited barriers to DA use2,30. Prior trials have shown that use of the long DA resulted in lower surgical rates compared with the rates for those who received the usual care (no DA)1,17,33, although one study showed increased surgical rates with DA use in an underserved population34. In our sample, the DAs did not appear to dampen enthusiasm for surgery. In fact, a substantial minority of patients wanted surgery but did not have it (about 10% across these sites). Furthermore, a minority of visits felt longer than normal to the surgeon, even at the site at which the use of DAs was new.
There are several limitations of the study. First, there were many post-randomization exclusions, predominantly due to patients cancelling their appointments. The no-show rate was similar to that found in a prior study at one site before the use of DAs17 and did not appear to be impacted by the study. Second, the random assignment of surgeon clusters did not result in balanced patient groups, although the magnitude of the differences was not clinically relevant and not likely to have impacted the results. Third, the lack of a control group, the lack of blinding of staff and surgeons, and surgeons’ self-reported limited use of the patient preference report may have biased results. Training and integration into the electronic health record may improve the usage and impact of patient preference reports. Fourth, the surgeon satisfaction scores may not be generalizable as all surgeons agreed to participate in the study, 2 of the sites had previously used DAs, and the response rate was very low at 1 site.
Conclusions
We believe the DECIDE-OA study to be the first multisite randomized comparative effectiveness trial of certified DAs for hip and knee osteoarthritis. The short DA outperformed the long DA with regard to knowledge scores and was comparable with respect to other outcomes. The surgeons reported high satisfaction and normal visit duration with both DAs.
Appendix
Supporting material provided by the authors is posted with the online version of this article as a data supplement at jbjs.org (http://links.lww.com/JBJS/F425).
Acknowledgments
Note: The authors acknowledge the valuable contributions of their research staff Mahima Mangla, Sheila Mwangi, Susannah Daggett, and Abigail Ward and the members of the Health Decision Sciences Center’s Patient Advisory Committee.
Footnotes
Investigation performed at Massachusetts General Hospital, Boston, Massachusetts; Newton Wellesley Hospital, Newton, Massachusetts; and New England Baptist Hospital, Boston, Massachusetts
A commentary by Pablo Castañeda, MD, is linked to the online version of this article at jbjs.org.
Disclosure: The study was funded through a Patient-Centered Outcomes Research Institute (PCORI) Award (CDR#1503-28799). The funding agreement ensured the authors’ independence in designing the study, interpreting the data, and writing and publishing the report. On the Disclosure of Potential Conflicts of Interest forms, which are provided with the online version of the article, one or more of the authors checked “yes” to indicate that the author had a relevant financial relationship in the biomedical arena outside the submitted work (including with Healthwise, the developer of one of the decision aids in the study) (http://links.lww.com/JBJS/F424).
Disclaimer: The statements presented in the publication are solely the responsibility of the authors and do not necessarily represent the views of PCORI, its Board of Governors, or its Methodology Committee.
Data Sharing
A data-sharing statement is provided with the online version of the article (http://links.lww.com/JBJS/F426).
References
- 1.Stacey D, Légaré F, Lewis K, Barry MJ, Bennett CL, Eden KB, Holmes-Rovner M, Llewellyn-Thomas H, Lyddiatt A, Thomson R, Trevena L. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2017. April 12;4:CD001431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Slover J, Shue J, Koenig K. Shared decision-making in orthopaedic surgery. Clin Orthop Relat Res. 2012. April;470(4):1046-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Washington State Health Care Authority. Patient decision aids (PDAs). https://www.hca.wa.gov/about-hca/healthier-washington/patient-decision-aids-pdas. Accessed 2019 Jun 12. [Google Scholar]
- 4.Elwyn G, Burstin H, Barry MJ, Corry MP, Durand MA, Lessler D, Saigal C. A proposal for the development of national certification standards for patient decision aids in the US. Health Policy. 2018. July;122(7):703-6. Epub 2018 Apr 27. [DOI] [PubMed] [Google Scholar]
- 5.Sepucha KR, Atlas SJ, Chang Y, Freiberg A, Malchau H, Mangla M, Rubash H, Simmons LH, Cha T. Informed, patient-centered decisions associated with better health outcomes in orthopedics: prospective cohort study. Med Decis Making. 2018. November;38(8):1018-26. [DOI] [PubMed] [Google Scholar]
- 6.Mulley AG, Trimble C, Elwyn G. Stop the silent misdiagnosis: patients’ preferences matter. BMJ. 2012. November 8;345:e6572. [DOI] [PubMed] [Google Scholar]
- 7.Braddock C, 3rd, Hudak PL, Feldman JJ, Bereknyei S, Frankel RM, Levinson W. “Surgery is certainly one good option”: quality and time-efficiency of informed decision-making in surgery. J Bone Joint Surg Am. 2008. September;90(9):1830-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Braddock CH, 3rd, Edwards KA, Hasenberg NM, Laidley TL, Levinson W. Informed decision making in outpatient practice: time to get back to basics. JAMA. 1999. December 22-29;282(24):2313-20. [DOI] [PubMed] [Google Scholar]
- 9.Légaré F, Adekpedjou R, Stacey D, Turcotte S, Kryworuchko J, Graham ID, Lyddiatt A, Politi MC, Thomson R, Elwyn G, Donner-Banzhoff N. Interventions for increasing the use of shared decision making by healthcare professionals. Cochrane Database Syst Rev. 2018. July 19;7:CD006732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Altman DG, Schulz KF, Moher D, Egger M, Davidoff F, Elbourne D, Gøtzsche PC, Lang T. CONSORT GROUP (Consolidated Standards of Reporting Trials). The revised CONSORT statement for reporting randomized trials: explanation and elaboration. Ann Intern Med. 2001. April 17;134(8):663-94. [DOI] [PubMed] [Google Scholar]
- 11.Sepucha KR, Abhyankar P, Hoffman AS, Bekker HL, LeBlanc A, Levin CA, Ropka M, Shaffer VA, Sheridan SL, Stacey D, Stalmeier P, Vo H, Wills CE, Thomson R. Standards for UNiversal reporting of patient Decision Aid Evaluation studies: the development of SUNDAE Checklist. BMJ Qual Saf. 2018. May;27(5):380-8. Epub 2017 Dec 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mangla M, Bedair H, Chang Y, Daggett S, Dwyer MK, Freiberg AA, Mwangi S, Talmo C, Vo H, Sepucha K. Protocol for a randomised trial evaluating the comparative effectiveness of strategies to promote shared decision making for hip and knee osteoarthritis (DECIDE-OA study). BMJ Open. 2019. February 24;9(2):e024906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.The Ottawa Hospital. Decision aid summary. Arthritis: should I have knee replacement surgery? 2017. April 6 https://decisionaid.ohri.ca/Azsumm.php?ID=1191. Accessed 2018 Nov 15. [Google Scholar]
- 14.The Ottawa Hospital. Decision aid summary. Arthritis: should I have hip replacement surgery? 2017. April 6 https://decisionaid.ohri.ca/Azsumm.php?ID=1112. Accessed 2018 Nov 15. [Google Scholar]
- 15.Health Dialog. Health Dialog shared decision making video versions. 2017. November 30 https://www.healthdialog.com/sites/default/files/resources/Shared-Decision-Making-%20Video-%20Versions.pdf. Accessed 2018 Nov 15. [Google Scholar]
- 16.Sepucha KR, Stacey D, Clay CF, Chang Y, Cosenza C, Dervin G, Dorrwachter J, Feibelmann S, Katz JN, Kearing SA, Malchau H, Taljaard M, Tomek I, Tugwell P, Levin CA. Decision quality instrument for treatment of hip and knee osteoarthritis: a psychometric evaluation. BMC Musculoskelet Disord. 2011. July 5;12:149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sepucha K, Atlas SJ, Chang Y, Dorrwachter J, Freiberg A, Mangla M, Rubash HE, Simmons LH, Cha T. Patient decision aids improve decision quality and patient experience and reduce surgical rates in routine orthopaedic care: a prospective cohort study. J Bone Joint Surg Am. 2017. August 2;99(15):1253-60. [DOI] [PubMed] [Google Scholar]
- 18.Fowler FJ, Jr, Gerstein BS, Barry MJ. How patient centered are medical decisions?: results of a national survey. JAMA Intern Med. 2013. July 8;173(13):1215-21. [DOI] [PubMed] [Google Scholar]
- 19.Rabin R, de Charro F. EQ-5D: a measure of health status from the EuroQol Group. Ann Med. 2001. July;33(5):337-43. [DOI] [PubMed] [Google Scholar]
- 20.Jansson KÅ, Granath F. Health-related quality of life (EQ-5D) before and after orthopedic surgery. Acta Orthop. 2011. February;82(1):82-9. Epub 2010 Dec 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Roos EM, Toksvig-Larsen S. Knee Injury and Osteoarthritis Outcome Score (KOOS) - validation and comparison to the WOMAC in total knee replacement. Health Qual Life Outcomes. 2003. May 25;1:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rodriguez-Merchan EC. Knee instruments and rating scales designed to measure outcomes. J Orthop Traumatol. 2012. March;13(1):1-6. Epub 2012 Jan 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Collins NJ, Misra D, Felson DT, Crossley KM, Roos EM. Measures of knee function: International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, Knee Injury and Osteoarthritis Outcome Score (KOOS), Knee Injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS), Knee Outcome Survey Activities of Daily Living Scale (KOS-ADL), Lysholm Knee Scoring Scale, Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Activity Rating Scale (ARS), and Tegner Activity Score (TAS). Arthritis Care Res (Hoboken). 2011. November;63(Suppl 11):S208-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alviar MJ, Olver J, Brand C, Hale T, Khan F. Do patient-reported outcome measures used in assessing outcomes in rehabilitation after hip and knee arthroplasty capture issues relevant to patients? Results of a systematic review and ICF linking process. J Rehabil Med. 2011. April;43(5):374-81. [DOI] [PubMed] [Google Scholar]
- 25.Collins NJ, Roos EM. Patient-reported outcomes for total hip and knee arthroplasty: commonly used instruments and attributes of a “good” measure. Clin Geriatr Med. 2012. August;28(3):367-94. Epub 2012 Jun 22. [DOI] [PubMed] [Google Scholar]
- 26.Nilsdotter A, Bremander A. Measures of hip function and symptoms: Harris Hip Score (HHS), Hip Disability and Osteoarthritis Outcome Score (HOOS), Oxford Hip Score (OHS), Lequesne Index of Severity for Osteoarthritis of the Hip (LISOH), and American Academy of Orthopedic Surgeons (AAOS) Hip and Knee Questionnaire. Arthritis Care Res (Hoboken). 2011. November;63(Suppl 11):S200-7. [DOI] [PubMed] [Google Scholar]
- 27.Lawless BM, Greene M, Slover J, Kwon YM, Malchau H. Does age or bilateral disease influence the value of hip arthroplasty? Clin Orthop Relat Res. 2012. April;470(4):1073-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mahomed NN, Arndt DC, McGrory BJ, Harris WH. The Harris hip score: comparison of patient self-report with surgeon assessment. J Arthroplasty. 2001. August;16(5):575-80. [DOI] [PubMed] [Google Scholar]
- 29.Morris NS, MacLean CD, Chew LD, Littenberg B. The Single Item Literacy Screener: evaluation of a brief instrument to identify limited reading ability. BMC Fam Pract. 2006. March 24;7:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bozic KJ, Belkora J, Chan V, Youm J, Zhou T, Dupaix J, Bye AN, Braddock CH, 3rd, Chenok KE, Huddleston JI., 3rd Shared decision making in patients with osteoarthritis of the hip and knee: results of a randomized controlled trial. J Bone Joint Surg Am. 2013. September 18;95(18):1633-9. [DOI] [PubMed] [Google Scholar]
- 31.de Achaval S, Fraenkel L, Volk RJ, Cox V, Suarez-Almazor ME. Impact of educational and patient decision aids on decisional conflict associated with total knee arthroplasty. Arthritis Care Res (Hoboken). 2012. February;64(2):229-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Allen KD, Sanders LL, Olsen MK, Bowlby L, Katz JN, Mather RC, 3rd, Williams JW., Jr Internet versus DVD decision aids for hip and knee osteoarthritis. Musculoskelet Care. 2016. June;14(2):87-97. Epub 2015 Jul 29. [DOI] [PubMed] [Google Scholar]
- 33.Arterburn D, Wellman R, Westbrook E, Rutter C, Ross T, McCulloch D, Handley M, Jung C. Introducing decision aids at Group Health was linked to sharply lower hip and knee surgery rates and costs. Health Aff (Millwood). 2012. September;31(9):2094-104. [DOI] [PubMed] [Google Scholar]
- 34.Shue J, Karia RJ, Cardone D, Samuels J, Shah M, Slover JD. A randomized controlled trial of two distinct shared decision-making aids for hip and knee osteoarthritis in an ethnically diverse patient population. Value Health. 2016. June;19(4):487-93. Epub 2016 Jun 7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
A data-sharing statement is provided with the online version of the article (http://links.lww.com/JBJS/F426).