Abstract
Background
Cancers escape immune surveillance via distinct mechanisms that involve central (negative selection within the thymus) or peripheral (lack of costimulation, receipt of death/anergic signals by tumor, immunoregulatory cell populations) immune tolerance. During the 1990s, moderate clinical benefit was seen using several cytokine therapies for a limited number of cancers. Over the past 20 years, extensive research has been performed to understand the role of various components of peripheral immune tolerance, with the co-inhibitory immune checkpoint molecules cytotoxic T-lymphocyte antigen 4 (CTLA-4), programmed death 1 (PD-1), and its ligand (PD-L1) being the most well-characterized at preclinical and clinical levels.
Patients and methods
We used PubMed and Google Scholar searches to identify key articles published reporting preclinical and clinical studies investigating CTLA-4 and PD-1/PD-L1, frequently cited review articles, and clinical studies of CTLA-4 and PD-1/PD-L1 pathway inhibitors, including combination therapy strategies. We also searched recent oncology congress presentations and clinicaltrials.gov to cover the most up-to-date clinical trial data and ongoing clinical trials of immune checkpoint inhibitor (ICI) combinations.
Results
Inhibiting CTLA-4 and PD-1 using monoclonal antibody therapies administered as single agents has been associated with clinical benefit in distinct patient subgroups across several malignancies. Concurrent blockade of CTLA-4 and components of the PD-1/PD-L1 system using various schedules has shown synergy and even higher incidence of durable antitumor responses at the expense of increased rates of immune-mediated adverse events, which can be life-threatening, but are rarely fatal and are reversible in most cases using established treatment guidelines.
Conclusions
Dual immune checkpoint blockade has demonstrated promising clinical benefit in numerous solid tumor types. This example of concurrent modulation of multiple components of the immune system is currently being investigated in other cancers using various immunomodulatory strategies.
Keywords: immuno-oncology, cytotoxic T-lymphocyte antigen 4, programmed death 1, peripheral immune tolerance, immune exhaustion, cancer
Introduction
Established cancers develop when they escape immune system regulation [1] and evolve into one of two cancer types. Inflamed cancers are usually immunogenic and rich in innate immune signals, chemokines for recruitment of T cells and other immune cell subsets, as well as tumor infiltration by various immune cell subsets [2]. Conversely, noninflamed cancers are often the end-product of poorly immunogenic transformed cells that have evolved when the host immune system has already eradicated highly immunogenic transformed cell clones. In noninflamed cancers, there are low or absent chemokine expression, lack of T-cell infiltration, potentially higher numbers of immunoregulatory populations (naturally occurring T-regulatory cells [Treg], myeloid-derived suppressor cells), and denser stroma. Noninflamed cancers comprise the majority of cancers, which, in part, explains the relatively low response rates seen with immunotherapies.
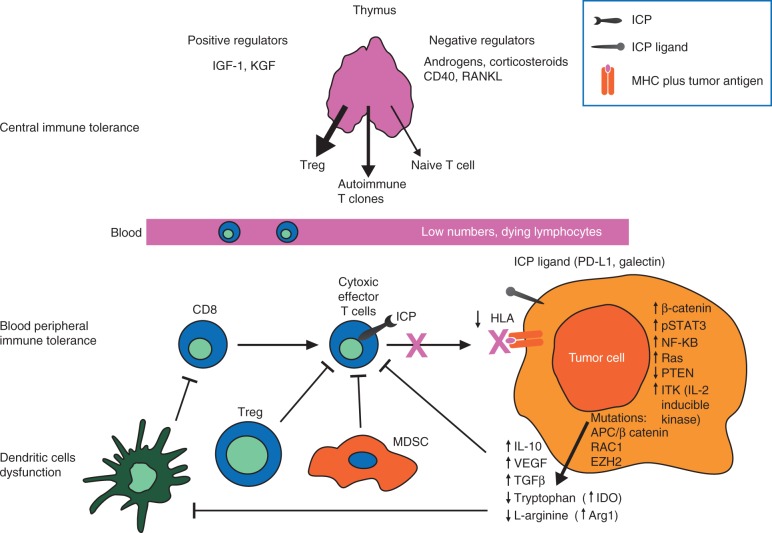
More recently, various mechanisms by which tumors escape immunosurveillance have been identified [3]. These mechanisms are usually induced by tumor cells themselves and/or the microenvironment, although primary or iatrogenic immunosuppression or inefficient activation of effector T cells may have a role (Figure 1 and supplementary Table S1, available at Annals of Oncology online). The lack of T cell effector function may be no different from other types of chronic inflammation, such as that seen in infections. More specifically, chronically stimulated effector T cells progressively lose effector function and eventually die. During this progressive decline, typically called exhaustion, immune checkpoint proteins (ICP) play important and dynamic roles. Immune cell death by exhaustion may account for the possibility that some cancers may be immunogenic, although low or absent immune cell infiltration within the tumor is observed [4].
Figure 1.
Mechanisms of immune tolerance. Immune tolerance involves a range of overlapping mechanisms that involve not only the periphery (e.g. tumor site), but also central lymphoid organs, especially thymus. They include intrathymic negative regulation (central), decreased costimulation, anergic signals from tumor cells, and immunoregulation (e.g. from Treg and MDSC [peripheral]). Arg1, arginase 1; HLA, human leukocyte antigen; ICP, immune checkpoint protein; IDO, indoleamine 2,3-dioxygenase; IGF-1, insulin-like growth factor; IL-10, interleukin 10; KGF, keratinocyte growth factor; MDSC, myeloid-derived suppressor cell; MHC, major histocompatibility complex; NF-κB, nuclear factor kappa-B; PD-L1, programmed death ligand 1; STAT, signal transducer and activator of transcription; RANKL, receptor activator of nuclear factor kappa-B ligand; TGF, transforming growth factor; Treg, regulatory T cells; VEGF, vascular endothelial growth factor.
Four issues are critical with respect to T-cell exhaustion in cancer. First, multiple ICPs can be simultaneously expressed [5]. Second, not all ICPs contribute equally to immune cell function and/or dysfunction. Among several co-inhibitory immune checkpoint systems, the CTLA-4/CD80/CD86 and PD-1/PD-L1/PD-L2 pathways have clinically significant roles in peripheral immune tolerance [6]. Third, the net effect on T-cell function is the sum of all co-stimulatory and co-inhibitory molecules simultaneously expressed in T cells. Fourth, T-cell exhaustion often coexists with other immunoregulatory mechanisms within the tumor (Figure 1) [7]. This may explain why single-agent immunotherapies have demonstrated variable efficacy across cancer types and why a combination approach, using agents targeting disease-specific mechanisms of immunosuppression, can be synergistic.
Various immunotherapies targeting distinct aspects of the immune system are either approved for clinical use or in development. This review provides an overview of novel single-agent and combination strategies that target the immune system. We will focus on the combination of CTLA-4 and PD-1 immune checkpoint inhibitors (ICIs), which has recently been approved in the USA for advanced melanoma and is currently being tested in other tumor types. We describe the rationale for this approach, the clinical data to date, and strategies for managing patients receiving combination ICP blockade.
Materials and methods
We used PubMed and Google Scholar searches to identify key articles published since 2004 reporting preclinical and clinical studies investigating CTLA-4 and PD-1/PD-L1, frequently cited review articles about ICPs and the immune system, and clinical studies of CTLA-4 and PD-1/PD-L1 pathway inhibitors, including combination therapy strategies. We also included recent congress presentations from international oncology meetings to cover the most up-to-date clinical trial data and searched the clinicaltrials.gov database to identify ongoing clinical trials of ICI combinations.
Peripheral immune tolerance: focus on the CTLA-4/CD80/CD86 and PD-1/PD-L1/PD-L2 pathways
ICPs are essential for maintaining peripheral self-tolerance during physiologic conditions. Different ICPs operate at various stages, anatomic locations, and impact distinct cell subsets of immune system activation (supplementary Table S2, available at Annals of Oncology online) [5]. Most co-inhibitory ICPs, such as CTLA-4 and PD-1, are upregulated in response to T-cell receptor activation as a physiologic response against unnecessary or prolonged immune system activation that may potentially damage normal tissues. CTLA-4 is upregulated early in this process and may induce T-cell inhibition by outcompeting with the costimulatory molecule CD28 for its ligands [8]. CTLA-4 is also required for the suppressive actions of Treg cells in secondary lymphoid organs or other peripheral tissues, including tumor sites [9]. Conversely, PD-1 is highly expressed on activated T cells after prolonged T-cell receptor stimulation [4]. Similar to CTLA-4, PD-1 is also required for their suppressive functions and for development of peripherally induced Treg cells [10, 11]. Therefore, treatment with CTLA-4 inhibitors expands the number of T-cell clones that recognize a broader number of tumor antigens [12], whereas treatment with PD-1 inhibitors preferentially increases the number of preexisting T-cell clones that recognize distinct tumor antigens [13, 14]. The ligands for PD-1, PD-L1 and PD-L2, are physiologically expressed by other immune cells as well as nonimmune cells. However, induction of PD-L1 expression can also be seen in peripheral tissues [8]. In malignancy, the expression of PD-L1 on cancer cells appears to be regulated in a complex set of interactions in part mediated by inflammatory cytokines. Preclinical melanoma models demonstrate an increase in PD-L1 expression in response to IFN-γ and suggest that this is driven by the presence of CD8+ T cells as part of a negative feedback loop [7, 15]. More recent work further highlights the underlying complexity in this system, suggesting specific genetic alterations in the GTPase RAC1 have the ability to modulate PD-L1 expression in melanoma cells [16]. Conversely, it is possible to have induction of PD-L1 that is independent from the presence of tumor-infiltrating lymphocytes (TILs) [17–22]. This observation is clinically relevant because PD-L1-positive, TIL-negative cancers may define a cancer type that may not be responsive to immunotherapies [23].
In summary, CTLA-4 and PD-1/PD-L1 exhibit distinct roles in regulating immune system activation. CTLA-4 limits T-cell activation and clonal expansion, and the PD-1/PD-L1/PD-L2 pathway limits T-cell function in the peripheral tissues, although the extent to which the PD-1 pathway is involved in early T cell priming in addition to modulation of effector function remains to be fully characterized. These spatiotemporal differences in the role of CTLA-4 and PD-1 provide the basis for combined blockade of CTLA-4 and PD-1 to increase effector T-cell response, discussed in further detail below.
Clinical development of inhibitors of CTLA-4 and the PD-1/PD-L1 pathway as single agents in cancers
Table 1 shows key clinical trials testing monoclonal antibodies targeting various ICPs [14, 24–54]. Ipilimumab, a monoclonal antibody against CTLA-4, was approved in the USA in 2011 for the treatment of patients with unresectable or metastatic melanoma on the basis of improved overall survival (OS) in two randomized, controlled phase III trials [24, 55]. In a recent pooled analysis of data from 10 prospective and 2 retrospective studies, including 2 phase III trials, ipilimumab demonstrated long-term OS in ∼20% of patients with advanced melanoma [56]. Although toxicities can be life-threatening, most serious adverse events (AEs) were reversible and treatable in clinical studies using established management algorithms [24, 55]. High-dose ipilimumab (10 mg/kg) has demonstrated increased recurrence-free survival (RFS) of 9 months versus placebo when administered in the adjuvant setting in patients at high risk for relapsing stage III melanoma, although the impact on OS is not yet known [57]. Based on the improvement in RFS, ipilimumab was recently approved by the FDA for this indication. In a randomized phase III trial in metastatic melanoma, tremelimumab, another monoclonal antibody to CTLA-4, was compared against physician’s choice chemotherapy, but failed to meet its primary OS endpoint. Post hoc analysis suggested that a considerable number of patients who were randomized to the control arm received standard-of-care ipilimumab following progression, potentially confounding the OS difference between these two groups [25].
Table 1.
Selected trials of single-agent immune checkpoint therapies
| Dose | Cancer type | Trial | Primary endpoint | Primary endpoint met (Y/N) | FDA approval status | |
|---|---|---|---|---|---|---|
| CTLA-4 | ||||||
| Ipilimumab | ||||||
| [24] | 3 mg/kg Q3W | Previously treated metastatic melanoma | Randomized phase III | OS | Y | Approved |
| Tremelimumab | ||||||
| [25] | 15 mg/kg Q90D | Treatment-naive, unresectable stage IIIc or IV melanoma | Open-label randomized phase III | OS | N | Not approved |
| PD-1 | ||||||
| Nivolumab | ||||||
| [26] | 3 mg/kg Q2W | Melanoma. Following ipilimumab, and a BRAF inhibitor, if BRAFV600+ | Open-label randomized phase III | ORR and OS | Y, ORR (OS pending) | Approved |
| [27] | 3 mg/kg Q2W | Melanoma. BRAF WT, treatment-naive | Randomized phase III | OS | Y | Approved |
| [28] | 3 mg/kg Q2W | Squamous-cell NSCLC. Following patient-based chemotherapy | Open-label randomized phase III | OS | Y | Approved |
| [29] | 3 mg/kg Q2W | Advanced RCC | Open-label randomized phase III | PFS | Y | Approved |
| [30] | 3 mg/kg Q2W | Nonsquamous-cell NSCLC. Following patient-based chemotherapy | Open-label randomized phase III | OS | Y | Approved |
| [31] | 3 mg/kg Q2W | Squamous cell carcinoma of the head and neck | Randomized phase III | OS | Y | Breakthrough designation |
| [32] | 3 mg/kg Q2W | Hodgkin’s lymphoma | Phase I | Safety | Y | Approved |
| Pembrolizumab | ||||||
| KEYNOTE-001 [14] | 2 or 10 mg/kg Q3W | Melanoma. Following ipilimumab, and a BRAF inhibitor, if BRAFV600+ | Phase Ib | ORR | Y | Yes, 2 mg/kg |
| KEYNOTE-006 [33] | 10 mg/kg Q2W or Q3W | Advanced melanoma | Randomized phase III | PFS and OS | Y | FDA approval in first-line setting |
| KEYNOTE-002 [34] | 2 mg/kg or 10 mg/kg Q3W | Melanoma. Following ipilimumab, and a BRAF inhibitor, if BRAFV600+ | Randomized phase III | PFS and OS | Y | Yes, following ipilimumab and, if BRAFV600+, a BRAF inhibitor |
| KEYNOTE-012 [35] | 10 mg/kg Q3W | Squamous cell carcinoma of the head and neck | Open-label phase I | Safety, ORR | Y | Approved |
| Pidilizumab | ||||||
| [36] | 1.5 mg/kg Q42D | Lymphoma (DLBCL) | Randomized phase II | PFS | Y | Ongoing |
| PD-L1 | ||||||
| Atezolizumab | ||||||
| [37] | 0.01–20 mg/kg Q3W | Metastatic urothelial bladder cancer | Phase I expansion | N/A | N/A | Approved |
| BMS-936559 | ||||||
| [38] | 0.3–10 mg/kg Q2W | Solid tumors | Phase I | Safety, MTD | N/A | Ongoing |
| Durvalumab | ||||||
| NCT02087423 [39] | Q2W | Solid tumors | Phase II | ORR | N/A | Ongoing |
| NCT01693562 [40] | Dose escalation/expansion Q2W, Q3W or Q4W | Solid tumors | Phase I/II | Safety, ORR | N/A | Ongoing |
| Avelumab | ||||||
| NCT02155647 [41] | Merkel cell carcinoma | Phase II | ORR | N/A | Ongoing | |
| PD-L2 | ||||||
| rHIgM12B7; NCT00658892 | Melanoma | Phase I | MTD | N/A | Ongoing | |
| CD137 | ||||||
| Urelumab | ||||||
| [42] | 1, 3, and 10 mg/kg Q3W | Advanced cancers | Phase I | Safety, DLT | N/A | Terminated |
| NCT01471210 | Advanced and/or metastatic solid tumors and relapsed/refractory B-cell NHL | Phase I | Safety, MTD, DLT | N/A | Ongoing | |
| KIR | ||||||
| Lirilumab | ||||||
| NCT01687387 | 0.1 mg/kg or 1 mg/kg Q4W | AML | Phase II | Leukemia-free survival | N/A | Ongoing |
| [43] | 0.015, 0.3, 1, 3, 6, and 10 mg/kg Q4W ×4 | Hematologic and solid tumors | Phase I | Safety and PK/PD | N/A | Ongoing |
| LAG-3 | ||||||
| IMP321 | ||||||
| [44] | 0.05, 0.25, 1.25, 6.25, and 30 mg Q2W | RCC | Phase I | Safety, MTD, PK, PD | N/A | Completed |
| BMS-986016 | 20, 80, 240 mg: 800 mg IV Q2W | CLL, HL, NHL, MM | Phase I | Safety, MTD, PK, PD | N/A | Ongoing |
| CD200 | ||||||
| Samalizumab | ||||||
| [45] | 50–500 mg/m2 Q4W | B-CLL, MM | Phase I/II | Safety, MTD, PK, PD | N/A | Completed |
| CD40 | ||||||
| CP-870,893 | ||||||
| [46] | 0.01–0.3 mg/kg | Advanced solid tumors | Phase I | MTD | N/A | Completed |
| [47] | 0.2 mg/kg weekly | Advanced solid tumors | Phase I | Safety, PD | N/A | Completed |
| Dacetuzumab (SGN-40) | ||||||
| [48] | Dose escalation | DLBCL | Phase II | ORR | N/A | Completed |
| [49] | Dose escalation | MM | Phase I | Safety | N/A | Completed |
| [50] | Dose escalation | NHL | Phase I | Safety, MTD, PK | N/A | Completed |
| ChiLob 7/4 | ||||||
| NCT01561911 | 50–500 mg/m2 Q4W | Solid tumors, lymphoma, B-cell NHL | Phase I | Safety, MTD | N/A | Completed |
| OX40 (CD134) | ||||||
| Anti-OX40 | ||||||
| NCT01644968 [51] | 0.1, 0.4, 2 mg/kg Q3W | Advanced solid tumors | Phase I | DLT | N/A | Ongoing |
| MEDI6383 | ||||||
| [52] | Dose escalation | Advanced solid tumors | Phase I | Safety | N/A | Ongoing |
| CD70 | ||||||
| ARGX-110 | ||||||
| [53] | 0.1, 1, 5, 10 mg/kg Q3W | Advanced solid and hematologic tumors | Phase I | DLT | N/A | Ongoing |
| SGN-CD70A | ||||||
| NCT02216890 | Nondisclosed | RCC, mantle-cell lymphoma, DLBCL, follicular lymphoma | Phase I | Safety | N/A | Ongoing |
| CD27 | ||||||
| CDX-1127 | ||||||
| [54] | 0.1, 0.3, 1.0, 3.0 or 10 mg/kg every 28 days | Advanced hematologic tumors | Phase I | Safety | N/A | Ongoing |
AML, acute myeloid leukemia; B-CLL, B cell chronic lymphocytic leukemia; CLL, chronic lymphocytic leukemia; CTLA-4, cytotoxic T-lymphocyte antigen 4; DLBCL, diffuse large B-cell lymphoma; DLT, dose-limiting toxicity; FDA, US Food and Drug Administration; HL, Hodgkin lymphoma; MM, multiple myeloma; MTD, maximum tolerated dose; N, no; N/A, not available; NHL, non-Hodgkin lymphoma; NSCLC, nonsmall cell lung cancer; ORR, objective response rate; OS, overall survival; PD, pharmacodynamics; PFS, progression-free survival; PK, pharmacokinetics; Q2/3/4W, every 2/3/4 weeks; Q42/90D, every 42/90 days; RCC, renal cell carcinoma; WT, wild type; Y, yes.
Nivolumab and pembrolizumab, two monoclonal antibodies against PD-1, were both approved in 2014 for the treatment of patients with unresectable stage III or distant metastatic melanoma and disease progression following ipilimumab and, if harboring a BRAFV600 mutation, a BRAF inhibitor [14, 58]. The indications for each agent were subsequently expanded to first-line therapy based on results from two separate studies: nivolumab demonstrated an improvement in OS compared with dacarbazine in patients with previously untreated metastatic melanoma without a BRAFV600 mutation [27] and pembrolizumab (at 10 mg/kg every 2 or 3 weeks) showed improved OS when compared to ipilimumab in advanced melanoma patients who had received at most one prior therapy [33]. Based on collective data supporting improved clinical efficacy, as well as reduced rates of toxicity, compared to ipilimumab, PD-1 therapy is established as an option for first-line therapy in patients with advanced melanoma [59]. Additionally, the indications for PD-1/PD-L1 based therapy continue to expand across many tumor types. Patients with advanced, previously treated squamous non-small cell lung cancer (NSCLC) who received nivolumab had a 41% lower risk of death compared to standard chemotherapy in a randomized phase III trial [28]. Similarly, the hazard ratio for death in patients with metastatic renal cell carcinoma who received nivolumab was 0.73 compared with everolimus in a randomized phase III trial [29] and was 0.70 compared with investigator’s choice in patients with squamous cell carcinoma of the head and neck [31]. Early investigation of pembrolizumab in NSCLC and of atezolizumab, a PD-L1 blocking antibody, in advanced urothelial cancer showed high antitumor responses in patients bearing tumors that express high levels of PD-L1 [37, 60]. In addition, pembrolizumab treatment in patients with squamous cell carcinoma of the head and neck resulted in an 18% and 25% ORR in HPV-positive and -negative patients, respectively [35]. Certain aspects of the tumor microenvironment have been associated with favorable immunotherapy responses, such as mutational burden [61–63] and virally driven cancers [64–66], offering insights to the spectrum of activity of co-inhibitory ICPs across more cancers.
Treatment combinations of peripheral ICIs and other strategies
Rationale for combinations other than inhibitors of CTLA-4 and PD-1
There are several barriers that limit responses to immunotherapies and to peripheral immune checkpoint inhibition, in particular. First, constitutive activation of several signaling pathways, such as the Wnt or the PI3K/Akt pathway, prevents influx of TILs [67, 68]. Second, several tumors may have low somatic mutation burden, which has been associated with resistance to immune checkpoint therapies, although this interaction is not completely understood as it is still possible to derive benefit from immunotherapy with a low mutational burden [63]. External beam irradiation has been studied in the context of a combination strategy, and while there are substantial preclinical data to suggest that radiation therapy may synergize with immune checkpoint blockade via various mechanisms, at this point the clinical data are more limited [13, 69]. Third, absolute lymphocyte counts are frequently low in patients with metastatic cancers, which is a result of spontaneous or tumor-cell-induced death [70]. This can occasionally be restored using immunotherapies that promote survival signals for T-cell growth and proliferation, such as high-dose bolus interleukin 2, a T-cell growth factor. Fourth, central (thymic) tolerance, a critical process to prevent autoimmunity, can restrict antitumor responses and limit the generation of tumor antigen-specific effector T cells [71]. Fifth, even within inflamed tumors there are variable degrees of both immunosuppression and peripheral immune tolerance. For example, tumor antigen-specific CD8+ cells that express high levels of two co-inhibitory ICP are more exhausted compared with those that express only one ICP [72], and T cell Ig ad ITIM domain is upregulated on tumor antigen-specific CD8+ cells and CD8+ tumor-infiltrating lymphocytes from patients with melanoma [73]. In addition, tumors may simultaneously contain various immunoregulatory cell types (Treg, myeloid-derived suppressor cells) and/or express high levels of enzymes that breakdown essential amino acids for T-cell growth (indoleamine 2,3-dioxygenase [IDO], arginase), in addition to high levels of ICP. In fact, there is now preclinical and early clinical evidence that targeting the PD-1/PD-L1 pathway in combination with IDO inhibition may be synergistic [74, 75]. Supplementary Table S3 and Table 2, available at Annals of Oncology online, show preclinical and clinical evidence, respectively, for combining peripheral ICI with other immunotherapies or treatment modalities [76–82].
Table 2.
Selected clinical trials testing the combination of peripheral ICI with other therapies
| Combination therapy | Study design | Cancer, stage | Study phase and trial number |
|---|---|---|---|
| Vaccines | |||
| gp100, MART-1, and NY-ESO-1+ nivolumab [76] | Vaccines+ nivolumab 1, 3, or 10 mg/kg, Q2W×12 | Melanoma, IIIC | Phase I, NCT01176461 |
| GM-CSF | |||
| Ipilimumab+ sargramostim [77] | Ipilimumab 10 mg/kg (day 1)+ sargramostim 250 μg (day 1–14) | Melanoma, III/IV | Phase II, NCT01134614 |
| Interferon | |||
| Ipilimumab+ peginterferon alfa-2b [78] | Ipilimumab 3 or 10 mg/kg, Q3W×12+ peginterferon alfa-2b | Melanoma, III/IV | Phase II, NCT01496807 |
| VEGF | |||
| Ipilimumab+ bevacizumab [79] | Ipilimumab 3 or 10 mg/kg+ bevacizumab 7.5 or 15 mg/kg Q3W | Melanoma, III/IV | Phase I, NCT00790010 |
| Small-molecule inhibitors | |||
| Atezolizumab+ vemurafenib or Atezolizumab+ vemurafenib+ cobimetinib | Atezolizumab 15–20 mg/kg Q3W, 800 mg Q2W or 1200 mg Q3W | Melanoma, III/IV | Phase Ib, NCT01656642 |
| Atezolizumab+ cobimetinib | Fixed doses of both or MPD fixed dose+ cobimetinib escalating doses | Solid tumors, metastatic | Phase I, NCT01988896 |
| Pembrolizumab+ dabrafenib+ trametinib | Pembrolizumab (days 1, 22)+ dabrafenib 150 mg/kg BID (day 1)+ trametinib 2 mg QD (day 1) | Melanoma, III/IV | Phase I/II, NCT02130466 |
| Dabrafenib+ ipilimumab+ trametinib [80] |
|
Melanoma, III/IV | Phase I, NCT01767454 |
| Durvalumab+ trametinib±dabrafenib [81] | Durvalumab 3 or 10 mg/kg Q2W+ dabrafenib 150 mg BID+ trametinib 2 mg QD or trametinib alone | Melanoma, III/IV | Phase I/II, NCT02027961 |
| IDO inhibitors | |||
| Pembrolizumab+ epacadostat (INCB024360) | Pembrolizumab 2 mg/kg Q3W+ epacadostat 25 mg BID | Solid tumors, metastatic melanoma | [64] |
| Ipilimumab+ epacadostat | Ipilimumab 3 mg/kg Q3W+ epacadostat 25 mg, 50 mg, 75 mg BID | Melanoma, metastatic or unresectable | Phase I/II, NCT01604889 |
| Ipilimumab+ indoximod | Ipilimumab 3 mg/kg Q3W+ indoximod 600 mg BID | Melanoma, metastatic | Phase I/II, NCT02073123 |
| Oncolytic virus | |||
| Pembrolizumab+ T-VEC | Pembrolizumab Q2W (Ib) Q3W (III)+ T-VEC intralesional Q2W (Ib) wk 0, 3, 5, 7 then Q3W | Melanoma, III/IV | Phase Ib/III, NCT02263508 |
| Chemotherapy | |||
| Pembrolizumab+ chemotherapy (gemcitabine, docetaxel, nab-paclitaxel, vinorelbine, irinotecan, doxorubicin) |
|
Breast cancer, sarcoma, pancreatic cancer, SCLC, metastatic | Phase I/II, NCT02331251 |
| Pembrolizumab+ chemotherapy (paclitaxel, carboplatin, bevacizumab, pemetrexed, erlotinib, gefitinib) or immunotherapy (ipilimumab) |
|
NSCLC | Phase I/II, NCT02039674 |
| Nivolumab±gemcitabine/cisplatin, pemetrexed/cisplatin, carboplatin/paclitaxel, bevacizumab maintenance, erlotinib or ipilimumab | Various doses and schedules | NSCLC | Phase I, NCT01454102 |
| Nivolumab+ chemotherapy (temsirolimus, irinotecan, irinotecan+ capecitabine) |
|
Pancreatic cancer, RCC, NSCLC, CRC | Phase I/II, NCT02423954 |
| Atezolizumab+ bevacizumab±FOLFOX [82] |
|
CRC | Phase I, NCT01633970 |
| Radiation therapy | |||
| Chemoradiation with or without sequential durvalumab | NSCLC | Phase III, NCT02125461 |
BID, twice daily; CRC, colorectal cancer; GM-CSF, granulocyte-macrophage colony-stimulating factor; ICI, immune checkpoint inhibitors; IDO, indoleamine 2,3-dioxygenase; MPD, myeloproliferative disease; NSCLC, nonsmall cell lung cancer; Q2/3W, every 2/3 weeks; QD, everyday; RCC, renal cell carcinoma; SCLC, small cell lung cancer; T-VEC, talimogene laherparepvec; VEGF, vascular endothelial growth factor.
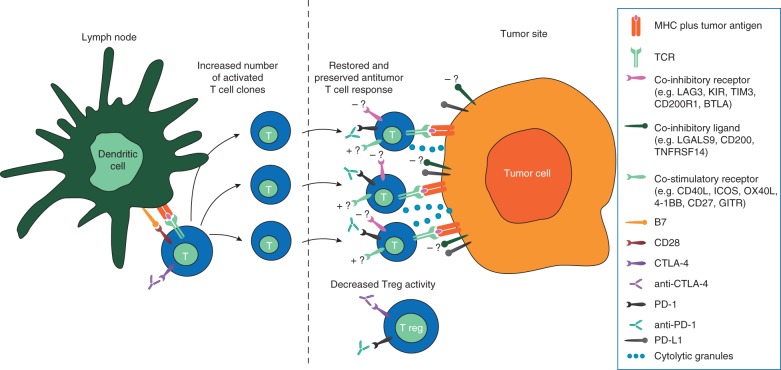
Rationale for CTLA-4 and PD-1 combination
CTLA-4 and PD-1/PD-L1 have complementary and synergistic roles in regulating activation via the T-cell receptor [83]. Blockade of CTLA-4 prevents the induction of tolerance and increases the number and repertoire of activated T cells [8, 12, 84]. PD-1 blockade restimulates previously primed T cells that have lost effector and proliferative function during the course of an immune response [4, 5, 12]. Concurrent PD-1 and CTLA-4 blockade restores ability of tumor-infiltrating CD8+ cells to produce IL-2 and therefore stimulates T cell growth, which may inhibit Treg-mediated suppression of antitumor responses [10, 13, 75, 85, 86]. Simultaneous blockade of both CTLA-4 and PD-1 should, therefore, increase the number of T cells participating in an antitumor response and prolong antitumor response by preventing PD-1:PD-L1-mediated downregulation and suppression by Tregs (Figure 2) [17, 87]. A recent study that tested the effects of anti-PD-1 or anti-CTLA-4 alone or in combination in patients’ blood and tumor tissue has shown that each treatment induces distinct immunologic effects and no overlapping changes in gene expression [88].
Figure 2.
Implications of CTLA-4 and PD-1 dual pathway blockade. Interruption of CTLA-4:B7 binding by T cells in lymph nodes via anti-CTLA-4 increases T-cell proliferation, activation, and survival, potentially leading to an increased number of activated T-cell clones that can respond to tumor antigens. Blockade of PD-1:PD-L1 binding at the tumor site via anti-PD-1 restores the activity of antitumor T cells that have become inactivated. CTLA-4 and PD-1 blockade may also reduce the suppressive effects of Tregs at the tumor site. Please note that T cells may express other (i.e. non-CTLA-4, non-PD-1, PD-L1) co-stimulatory (+?) as well as co-inhibitory immune checkpoint proteins (-?), whereas tumor cells upregulate almost exclusively co-inhibitory ICPs via genetic (gene amplification) [17] or epigenetic mechanisms (upregulation of PI3K) [87]. BTLA, B- and T-lymphocyte attenuator; CTLA-4, cytotoxic T-lymphocyte antigen 4; GITR, glucocorticoid-induced TNFR-related protein; ICOS, inducible costimulator; LAG-3, lymphocyte activation gene-3; LGALS9, lectin, galactoside-binding, soluble-9; KIR, killer-cell immunoglobulin-like receptor; PD-1, programmed death-1; PD-L1, programmed death ligand 1; TCR, T-cell receptor; TNFSRF, tumor necrosis factor receptor superfamily-14; Treg, regulatory T cells.
Clinical approaches and efficacy with CTLA-4 and PD-1 blockade
Efficacy of immune-checkpoint combinations
Based on the efficacy seen in preclinical studies, trials using combinations of anti-CTLA-4 and anti-PD-1 have been conducted in patients with melanoma and other cancers.
Phase I trial
A phase I trial evaluated ipilimumab plus nivolumab (I + N) in patients with unresectable stage III or IV melanoma [89]. Patients (n = 53) received escalating doses of concurrent nivolumab and ipilimumab for four cycles, followed by nivolumab monotherapy for four cycles. The regimen that consisted of nivolumab 1 mg/kg plus ipilimumab 3 mg/kg was selected for further investigation in phase II and III trials in metastatic melanoma. Across all concurrent cohorts, the objective response rate (ORR) was 40%, including early (i.e. within 12 weeks) and deep (i.e. ≥80% tumor shrinkage) responses that were unrelated to BRAFV600 mutation status. A recent long-term follow-up demonstrated 1-, 2-, and 3-year OS rates of 85%, 79%, and 68%, respectively [90]. The data from this study are encouraging and represent a dramatic shift from historical OS rates.
Phase II trial
A phase II randomized double-blind study showed significantly improved efficacy with combination I + N versus ipilimumab alone (Table 3) [91, 92]. Treatment-naïve patients with metastatic melanoma (n = 142) were randomized 2:1 to receive ipilimumab (3 mg/kg every 3 weeks [Q3W]) concurrently administered with either nivolumab (1 mg/kg Q3W) or placebo for four doses, followed by nivolumab (3 mg/kg) or placebo every 2 weeks (Q2W) until disease progression [91, 92]. Overall, ORR was significantly higher with I + N compared with ipilimumab monotherapy (59% versus 11%) [91]. At a minimum follow-up of 24.5 months, patients who received the combination had prolonged PFS compared with patients who received ipilimumab alone, and the 2-year OS rate for all randomized patients was 64% for the combination and 54% compared with ipilimumab monotherapy; median OS had not been reached in either group (hazard ratio 0.74, 95% CI 0.43‒1.26; P = 0.26) [92]. In the combination group, ORR was independent of tumor PD-L1 status (58% for PD-L1-positive and 55% for PD-L1-negative tumors). In the ipilimumab monotherapy group, a numerically higher ORR was observed among patients with PD-L1-positive compared with PD-L1-negative tumors (18% versus 4%). The results from this trial led to accelerated approval of the combination in the USA based on tumor response rate and durability of response.
Table 3.
Selected completed, ongoing, and planned studies with ICI combinations
| Immune checkpoints inhibited | Study design | Treatment | Study population | Primary endpoint(s) and key results (for completed trials) |
|---|---|---|---|---|
| Melanoma | ||||
| CTLA-4+PD-1 | ||||
| [93] | Phase III, randomized, placebo-controlled N=945 | Ipilimumab+nivolumab OR nivolumab versus ipilimumab (placebo-controlled) | Treatment-naïve, unresectable or metastatic melanoma |
|
| [91, 92] | Phase II, randomized, placebo-controlled N=142 | Ipilimumab+nivolumab versus ipilimumab (placebo-controlled) | Treatment-naïve, unresectable or metastatic melanoma |
|
| NCT02224781 | Phase III, randomized N=300 | Nivolumab+ipilimumab → dabrafenib+trametinib versus dabrafenib+trametinib→ nivolumab+ipilimumab | Advanced BRAFV600 mutant melanoma | 2-year OS rate |
| NCT02339571 | Phase II/III, randomized, open-label N=400 | Nivolumab+ipilimumab+GM-CSF induction → nivolumab+GM-CSF maintenance versus nivolumab+ipilimumab induction → nivolumab maintenance | Unresectable stage III/IV melanoma of known BRAF mutation status | OS |
| NCT01783938 [94] | Phase II, randomized, open-label N=140 | Ipilimumab → nivolumab versus nivolumab → ipilimumab (sequential treatment) | Unresectable stage III/IV melanoma | Incidence of treatment-related grade 3/5 AEs during induction |
| NCT02374242 | Phase II, randomized, open-label N=75 | Nivolumab monotherapy (cohorts 1 and 2, recruited in parallel) versus nivolumab+ipilimumab (cohort 3; randomized allocation versus cohort 1, once 6 patients treated safely in cohort 1) |
|
Intracranial response rate |
| NCT02320058 | Phase II, open-label N=148 | Nivolumab+ipilimumab induction → nivolumab monotherapy maintenance | Melanoma with measurable metastases in brain and extracranial compartments | CBR |
| NCT01621490 | Phase I, part-randomized, open-label biomarker study N=160 |
|
Unresectable stage III/IV melanoma | Changes from baseline in activated and memory T cells, IFN, IFN-inducible factors, and T-cell infiltration |
| NCT02186249 | Expanded access | Nivolumab+ipilimumab | Anti-CTLA-4 naïve, unresectable stage III/IV melanoma | Safety and tolerability |
| NCT02089685 [95] | Phase I/II, randomized, open-label N=343 | Pembrolizumab+IFN versus pembrolizumab+ipilimumab |
|
Safety, MTD and RP2D |
| Other tumor types | ||||
| CTLA-4+PD-1 | ||||
| NCT02231749 | Phase III, randomized, open-label N=1,070 | Nivolumab+ipilimumab versus sunitinib | Treatment-naïve, advanced or metastatic RCC | PFS, OS |
| NCT02210117 | Pilot, randomized, open-label N=45 | Nivolumab versus nivolumab+bevacizumab versus nivolumab+ipilimumab | Metastatic RCC eligible for cytoreductive surgery | Safety and tolerability of each combination |
| NCT01472081 [96] | Phase I, nonrandomized, open-label N=175 | Nivolumab+ipilimumab induction (3 different dosing arms)→ nivolumab monotherapy maintenance OR nivolumab+sunitinib OR nivolumab+pazopanib | Advanced or metastatic RCC |
|
| NCT02060188 | Phase II, dose-escalating, open-label N=96 | Nivolumab monotherapy OR nivolumab+ipilimumab (dose- escalation phase) | Recurrent and metastatic colon cancer | ORR in all MSI-H patients |
| NCT01454102 [97] | Phase I, randomized, open-label, multi-arm safety study N=412 | Nivolumab monotherapy OR nivolumab+ipilimumab OR nivolumab+bevacizumab maintenance OR nivolumab+erlotinib OR nivolumab+platinum-based doublet chemotherapy | Stage IIIB/IV NSCLC |
|
| NCT02039674 | Phase I/II N=308 |
|
Stage IIIB/IV NSCLC |
|
| NCT01592370 | Phase I, dose-escalation N=315 | Nivolumab (cohort 1) OR nivolumab+either ipilimumab or lirilumab | Relapsed or refractory lymphoma or multiple myeloma | Safety and tolerability of each combination |
| NCT02311920 | Phase I, randomized, open-label N=42 | Temozolomide and ipilimumab versus temozolomide and nivolumab versus temozolomide+nivolumab+ipilimumab | Newly diagnosed glioblastoma | Optimal dose of each combination |
| NCT01928394 [98] | Phase I/II, randomized, open-label N=1100 | Nivolumab versus nivolumab+ipilimumab | Advanced or metastatic triple-negative breast cancer, gastric cancer, pancreatic cancer, SCLC, or bladder cancer |
|
| NCT02017717 [99] | Phase I, open label, randomized N=100 (cohort 1) | Nivolumab monotherapy versus N+I | Grade IV malignant glioma |
|
| NCT02039674 | See Table 2 | |||
| PD-1+LAG-3 | ||||
| NCT01968109 | Phase I, dose-escalation, cohort expanding N=198 | BMS-986016 versus BMS-986016+nivolumab | Advanced solid tumors | Safety |
| PD-1+KIR | ||||
| NCT01714739 | Phase I, dose-escalation, cohort expanding N=162 |
|
Advanced solid tumors | Safety and tolerability |
| CTLA-4+KIR | ||||
| NCT01750580 | Phase I N=22 | Lirilumab+ipilimumab | Advanced solid tumors | Safety |
| PD-1+CD137 (4-1BB) | ||||
| NCT02179918 [100] | Phase I N=45 | Pembrolizumab+PF-05082566 | Advanced solid tumors | Dose-limiting toxicities |
| PD-L1+CTLA-4 | ||||
| NCT02352948 | Phase III, randomized, open-label N=900 |
|
|
OS and PFS |
| NCT02369874 | Phase III, randomized, open-label N=720 | Durvalumab+tremelimumab OR Durvalumab versus SOC | Recurrent or metastatic head and neck cancer | OS and PFS |
| NCT02261220 | Phase I, open-label N=233 | Durvalumab+tremelimumab | Advanced solid tumors | Safety |
| PD-1+PD-L1 | ||||
| NCT02118337 | Phase I, open-label N=196 | MEDI0680 (AMP-514)+Durvalumab | Advanced malignancies | Safety |
| PD-L1 or CTLA-4+OX-40 | ||||
| NCT02205333 | Phase Ib/II, open-label N=212 |
|
Advanced solid tumors or aggressive B-cell lymphomas | MTD and safety |
AE, adverse events; CBR, clinical benefit rate; CTLA-4, cytotoxic T-lymphocyte antigen 4; GM-CSF, granulocyte-macrophage colony-stimulating factor; ICI, immune checkpoint inhibitor; IFN, interferon; KIR, killer-cell immunoglobulin-like receptors; LAG-3, lymphocyte activation gene 3; mo, months; MSI-H, microsatellite-high; MTD, maximum tolerated dose; NSCLC, nonsmall cell lung cancer; OR, objective response; ORR, objective response rate; OS, overall survival; PD-1, programmed death-1; PD-L1, programmed death-1 ligand; PFS, progression-free survival; RCC, renal cell carcinoma; RP2D, recommended phase II dose; SCLC, small cell lung cancer; SOC, standard of care; WT, wild type.
Phase III trial
In the first phase III trial to evaluate the role of concurrent versus single-agent immune checkpoint blockade for the treatment of patients with metastatic melanoma (Table 3) [91–100], 945 treatment-naïve patients were randomized 1:1:1 to receive I + N at the phase II schedule or single-agent nivolumab 3 mg/kg Q2W plus placebo, versus single-agent ipilimumab Q3W plus placebo, until disease progression or unacceptable toxicity [93]. At a median follow-up of ∼12 months, both the I + N and nivolumab monotherapy groups demonstrated improved PFS and higher investigator-assessed ORR compared with ipilimumab alone, a benefit that was observed across predefined subgroups [101]. At a median follow-up of 20.7 months, OS data were too immature to analyze [102].
Although PFS for the combination was more prolonged compared with nivolumab alone (11.5 months versus 6.9 months, respectively), the study was not statistically powered to formally assess this difference. In patients whose tumors had at least 5% PD-L1 expression using the PD-L1 IHC 28-8 pharmDx immunohistochemical assay [103], PFS with the I + N combination was numerically higher compared with nivolumab monotherapy (11.2 months versus 5.3 months, respectively). Subset analysis in relation to PD-L1 expression suggests that patients bearing PD-L1-positive tumors who received the combination did not have significantly longer PFS compared with single-agent nivolumab. Accordingly, at this time PD-L1 should not be used for clinical management and making decisions between combination and single-agent anti-PD-1 therapy, based solely on these results.
Safety profile with dual CTLA-4 and PD-1 inhibition
ICI are associated with immune-related AEs that typically affect skin, gastrointestinal, hepatic, endocrine, pulmonary, and renal organ systems. Table 4 lists grade 3/4 treatment-related AEs reported in trials combining CTLA-4 and PD-1 inhibitors. Although the spectrum of AEs with I + N was similar to monotherapy, the incidence of serious (grade 3 or 4) AEs was higher in the I + N arm compared with monotherapy-treated patients (69% versus 44% and 56%, respectively) [91, 93, 104, 105]. Additionally, there is a suggestion that irAEs may occur early in the course of therapy with combination treatment, potentially after only one cycle [106, 107]. The safety profile across all phases was consistent, and treatment-related AEs were generally well-managed and resolved with established safety guidelines (supplementary Tables S4 and S5, available at Annals of Oncology online) [91, 93, 104]. Notably, although four deaths related to combination therapy were reported across the phase I and II studies, no treatment-related deaths were reported in the multicenter phase III trial (109 institutions, 21 countries) among patients receiving the combination regimen [91, 93, 104]. Towards identifying a concurrent I + N regimen with comparable efficacy but a better safety profile, different schedules that decrease frequency and dose of ipilimumab in melanoma and NSCLC may preserve efficacy but definitely reduce life-threatening adverse events [95, 101]. Of note, a recent analysis of 35 patients who discontinued I + N on the phase II study due to toxicity demonstrated a similar response rate (66%) to the overall study population (59%), with the potential for durable benefit [108], suggesting that continued observation may be a reasonable option for this patient cohort.
Table 4.
Rates of grade 3/4 treatment-related AEs reported in trials of concurrent CTLA-4 and PD-1 pathway blockade [91, 93, 104, 105]
| Grade 3/4 AEs (%) | |
|---|---|
| All treatment-related AEs | 51–64 |
| Colitis | 4–17 |
| Lipase increased | 9–15 |
| ALT increased | 8–12 |
| AST increased | 6–11 |
| Diarrhea | 7–11 |
| Rash | 5–9 |
| Amylase increased | ≤6 |
| Pyrexia | 0–3 |
| Fatigue | 1–5 |
| Dyspnea | ≤3 |
| Hypophysitis | ≤2 |
| Pneumonitis | ≤2 |
| Headache | ≤2 |
AE, adverse event; ALT, alanine aminotransferase; AST, aspartate aminotransferase; CTLA-4, cytotoxic T-lymphocyte antigen 4; PD-1, programmed death-1.
Clinical insights for managing patients receiving ICIs
Supplementary Table S5, available at Annals of Oncology online, provides an overview of immune-related AE management strategies, which emphasizes differential diagnoses, use of steroids, and a multidisciplinary approach. If a patient has a moderate to severe AE that is potentially immune-mediated, treatment should be delayed or discontinued. Steroids are typically used to reduce immune reactions [14, 91, 93]. In some instances, immune checkpoint therapy can be resumed following resolution of an AE; however, patients experiencing a severe AE should permanently discontinue therapy. In patients presenting with acute fatigue, weight loss, diarrhea, nausea, emesis, or arthralgia, a workup for endocrinopathies (in particular, hypophysitis) should be done. Prompt hormone replacement therapy ameliorates symptoms of endocrinopathies and may allow continued therapy with ICI in some cases [109].
As yet, there is insufficient evidence about whether the efficacy of I + N is adversely affected by corticosteroids. To date, pooled data from studies testing single-agent nivolumab or ipilimumab suggest that use of immune modulators to manage immune-related AEs does not significantly alter the efficacy to any of these agents [26, 110, 111].
Granulocyte-macrophage colony-stimulating factor (GM-CSF) has been studied in combination with ipilimumab. In a randomized multicenter study, ipilimumab (10 mg/kg) plus GM-CSF improved OS, though not PFS, and showed lower rates of serious AEs compared with ipilimumab alone [77]. The implications of reduced toxicity with combination treatment versus monotherapy may be worth exploring once more data are available.
Patient selection
From a safety standpoint, most studies have been conducted in patients with normal hepatic and renal function, although there are no absolute contraindications to therapy with ICI. Additionally, patients with a history of autoimmune disease (AID) have been excluded from clinical trials based on concerns of increased risk of developing immune-related AEs and possible diminished clinical benefit if patients are actively treated with systemic immune modulators [112–114]. It is the authors’ practice to consider therapy on an individual basis for patients with AID, after careful discussion of the risks and benefits, as clinical responses can be seen [115].
Development of biomarkers to assist in patient selection for therapy with ICI has trailed that of other therapies, such as small-molecule inhibitors. This may have significant economic implications due to the high cost of these agents over prolonged treatment periods [116]. This is especially likely if they are to be given in combination, either in cancers with low response rates to PD-1/PD-L1 pathway inhibitor studies; or even in cancers with high response rates (e.g. melanoma) but administered during earlier stages of cancer (e.g. adjuvant). Immunohistochemical expression of PD-L1 in tumor tissues seems to be the most promising biomarker so far and is currently used as an FDA-approved companion diagnostic test in patients with NSCLC who are considered for treatment with pembrolizumab [60]. Other tumor tissue-based tests that assess PD-L1 are likely to be FDA-approved as companion diagnostics in combination with other PD-L1 inhibitors [117].
Initial evidence suggested that patients with PD-L1-expressing tumors may have higher response rates and longer PFS to PD-1/PD-L1 pathway inhibitors than patients treated with anti-PD-1 monotherapy with low or negative PD-L1 expression [33, 118–120]. However, PD-L1 was not a predictive biomarker in phase III randomized trials in RCC and squamous cell NSCLC [121]. Moreover, patients with PD-L1 negative tumors still benefit from treatment with these agents when compared with other treatments [120]. This may be attributed to the fact that expression of PD-L1 is heterogeneous with respect to stage (primary versus metastatic), metastatic organs involved, and prior systemic or local treatment effects [122]. Screening for PD-L1 expression by immunohistochemistry, however, may be important in patients who would otherwise be considered for I + N as opposed to single-agent nivolumab, as the margin for PFS benefit to the combination therapy was greatest in patients with PD-L1-negative metastatic melanoma [93]. In the future, PD-L1 expression could factor into the complex decision-making involved with individualized patient treatment, however it has not yet been validated for this purpose at this time.
Analysis of pretreatment tumor tissues from patients who went on to receive pembrolizumab showed that preexisting high numbers of TILs in the vicinity of PD-L1- and PD-1-expressing cells had the greatest tumor response from pembrolizumab in metastatic melanoma [123]. ImmunoscoreTM is already a commercially available test (HalioDx) that accurately quantifies the density and distribution of TILs using standardized immunohistochemistry and computer imaging algorithms in formalin-fixed, paraffin-embedded tumor tissues with prognostic and predictive implications for therapy [124, 125]. It may likely assist in classifying cancers based on the tumor microenvironment and to facilitate prediction of response to ICI and other immuno-oncology agents [23, 126, 127]. Possibly, a combined tumor tissue biomarker that considers both immunoscore and PD-L1 expression is important [23], especially for patients who are considered for I + N therapy. Other predictive methodologies also continue to be investigated. Recently, multiparameter flow cytometry for PD-1 and CTLA-4 on freshly isolated mononuclear cells from tumor tissues was found to be a predictor of response to PD-1 monotherapy in metastatic melanoma [128]. Functionally, this T-cell subset demonstrated a partially exhausted phenotype. Interestingly, in a separate cohort of 24 patients treated with I + N, increased levels of PD-1 high/CTLA-4 high T cells were not predictive of benefit [129]. While it remains a critical question, the optimal biomarker to guide patient selection has yet to be defined.
Ongoing immune checkpoint combination studies in patients with advanced malignancies
Within melanoma the concurrent I + N regimen is FDA-approved for unresectable stage III or IV disease and is being evaluated in patients with active brain metastases (NCT02374242). Early data on the I + N regimen in other solid tumors suggest that combination treatment may have higher response rates compared with single-agent nivolumab on most occasions (Table 3). Ongoing studies are investigating other combinations of CTLA-4 and PD-1/PD-L1 pathway inhibitors in other tumor types (Table 3). The anti-PD-L1 agent durvalumab is also being combined with an anti-PD-1 agent (MEDI0680; AMP 514) in the first trial to target both the PD-1 receptor and its key ligand on the basis of preclinical data showing synergy [130]. This combination is being evaluated in patients with advanced malignancies, including melanoma (NCT02118337) (Table 3).
The success and promise of CTLA-4 and PD-1/PD-L1 pathway inhibitors has paved the way to investigate the therapeutic potential of other antibodies that target co-inhibitory or co-stimulatory ICP (Table 3). The list of prospective drug targets is large, and clinical trials testing antibodies against CD137, LAG-3, CD200, and KIR have offered early results of safety and activity. Clinical trials testing drugs against several other ICPs were recently opened to accrual or are ready to enroll patients (e.g. OX-40, CD40, CD27, Tim-3, GITR). Although the number of permutations for simultaneous targeting of these proteins is daunting, the most promising combinations will be ultimately defined by the cancer type-specific biology and in vivo testing in appropriate cancer-specific animal models.
Conclusion
The field of immuno-oncology is expanding rapidly, with the potential for broad application across multiple tumor types. ICIs are changing the treatment expectations for cancer patients, offering durable and deep responses for many patients. Combinations of immuno-oncology agents have shown improved response rates compared with single-agent therapy, although the high rate of grade 3/4 AEs remains a potential concern. This emphasizes the need for vigilance in AE identification, prompt management using established guidelines, appropriate risk stratification, and the need for better biomarkers of response that may rely on tumor biology and agent’s MOA (PD-L1 negative, immunoscore low/absent). Ongoing studies seek to refine patient selection and identify novel combination approaches, which may lead to safer and more effective treatments.
Key message
The combination of ipilimumab (anti-CTLA-4) and nivolumab (anti-PD-1), approved in the USA for advanced melanoma, has shown clinical benefit with manageable toxicity in other cancers. A better understanding of host immune response and predictive biomarkers may help identify patients who experience the most benefit to immune checkpoint blockade and those that are vulnerable to serious toxicities.
Supplementary Material
Acknowledgements
The authors take full responsibility for the content of this publication and confirm that it reflects their viewpoint and expertise. Professional medical writing assistance was provided by Britt Anderson, PhD and Dan Rigotti, PhD and professional editing assistance was provided by Artur Romanchuk at StemScientific, an Ashfield Company, and were funded by Bristol-Myers Squibb. Bristol-Myers Squibb generated the concept for this review article; however, the authors developed the content. Bristol-Myers Squibb reviewed a draft for medical accuracy only. Neither Bristol-Myers Squibb nor StemScientific influenced the content of the article, nor did the authors receive financial compensation for authoring the article.
Funding
This work was supported by Bristol-Myers Squibb. No grant number is applicable.
Disclosures
AKSS has served as a consultant for Bristol-Myers Squibb and her institution has received research funding from Bristol-Myers Squibb, Merck & Co., Genentech, Celldex, and Reata. SJM has served as a consultant for Prometheus Laboratories, Merck & Co., Genentech, Amgen, and Castle Biosciences. He has received a research grant from Merck & Co and Amgen.
References
- 1. Mittal D, Gubin MM, Schreiber et al. New insights into cancer immunoediting and its three component phases–elimination, equilibrium and escape. Curr Opin Immunol 2014; 27: 16–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Turley SJ, Cremasco V, Astarita JL. Immunological hallmarks of stromal cells in the tumour microenvironment. Nat Rev Immunol 2015; 15: 669–682. [DOI] [PubMed] [Google Scholar]
- 3. Vesely MD, Kershaw MH, Schreiber RD. et al. Natural innate and adaptive immunity to cancer. Annu Rev Immunol 2011; 29: 235–271. [DOI] [PubMed] [Google Scholar]
- 4. Wherry EJ. T cell exhaustion. Nat Immunol 2011; 12: 492–499. [DOI] [PubMed] [Google Scholar]
- 5. Pardoll DM. The blockade of immune checkpoints in cancer immunotherapy. Nat Rev Cancer 2012; 12: 252–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Topalian SL, Drake CG, Pardoll DM. Immune checkpoint blockade: a common denominator approach to cancer therapy. Cancer Cell 2015; 27: 450–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Spranger S, Spaapen RM, Zha Y. et al. Up-regulation of PD-L1, IDO, and T(regs) in the melanoma tumor microenvironment is driven by CD8(+) T cells. Sci Transl Med 2013; 5: 200ra116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fife BT, Bluestone JA. Control of peripheral T-cell tolerance and autoimmunity via the CTLA-4 and PD-1 pathways. Immunol Rev 2008; 224: 166–182. [DOI] [PubMed] [Google Scholar]
- 9. Qureshi OS, Zheng Y, Nakamura K. et al. Trans-endocytosis of CD80 and CD86: a molecular basis for the cell-extrinsic function of CTLA-4. Science 2011; 332: 600–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chen X, Fosco D, Kline DE. et al. PD-1 regulates extrathymic regulatory T-cell differentiation. Eur J Immunol 2014; 44: 2603–2616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Francisco LM, Salinas VH, Brown KE. et al. PD-L1 regulates the development, maintenance, and function of induced regulatory T cells. J Exp Med 2009; 206: 3015–3029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Robert L, Tsoi J, Wang X. et al. CTLA4 blockade broadens the peripheral T-cell receptor repertoire. Clin Cancer Res 2014; 20: 2424–2432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Twyman-Saint Victor C, Rech AJ, Maity A. et al. Radiation and dual checkpoint blockade activate non-redundant immune mechanisms in cancer. Nature 2015; 520: 373–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Robert C, Ribas A, Wolchok JD. et al. Anti-programmed-death-receptor-1 treatment with pembrolizumab in ipilimumab-refractory advanced melanoma: a randomised dose-comparison cohort of a phase 1 trial. Lancet 2014; 384: 1109–1117. [DOI] [PubMed] [Google Scholar]
- 15. Blank C, Brown I, Peterson AC. et al. PD-L1/B7H-1 inhibits the effector phase of tumor rejection by T cell receptor (TCR) transgenic CD8+ T cells. Cancer Res 2004; 64: 1140–1145. [DOI] [PubMed] [Google Scholar]
- 16. Vu HL, Rosenbaum S, Purwin TJ. et al. RAC1 P29S regulates PD-L1 expression in melanoma. Pigment Cell Melanoma Res 2015; 28: 590–598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Cancer Genome Atlas Network. Genomic classification of cutaneous melanoma. Cell 2015; 161: 1681–1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Velcheti V, Schalper KA, Carvajal DE. et al. Programmed death ligand-1 expression in non-small cell lung cancer. Lab Invest 2014; 94: 107–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Taube JM, Anders RA, Young GD. et al. Colocalization of inflammatory response with B7-h1 expression in human melanocytic lesions supports an adaptive resistance mechanism of immune escape. Sci Transl Med 2012; 4: 127ra37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lipson EJ, Vincent JG, Loyo M. et al. PD-L1 expression in the Merkel cell carcinoma microenvironment: association with inflammation, Merkel cell polyomavirus and overall survival. Cancer Immunol Res 2013; 1: 54–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. D’Angelo SP, Shoushtari AN, Agaram NP. et al. Prevalence of tumor-infiltrating lymphocytes and PD-L1 expression in the soft tissue sarcoma microenvironment. Hum Pathol 2015; 46: 357–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Schalper KA, Velcheti V, Carvajal D. et al. In situ tumor PD-L1 mRNA expression is associated with increased TILs and better outcome in breast carcinomas. Clin Cancer Res 2014; 20: 2773–2782. [DOI] [PubMed] [Google Scholar]
- 23. Teng MW, Ngiow SF, Ribas A. et al. Classifying cancers based on T-cell infiltration and PD-L1. Cancer Res 2015; 75: 2139–2145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hodi FS, O’Day SJ, McDermott DF. et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med 2010; 363: 711–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ribas A, Kefford R, Marshall MA. et al. Phase III randomized clinical trial comparing tremelimumab with standard-of-care chemotherapy in patients with advanced melanoma. J Clin Oncol 2013; 31: 616–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Weber JS, Antonia SJ, Topalian SL. et al. Safety profile of nivolumab (NIVO) in patients (pts) with advanced melanoma (MEL): a pooled analysis. J Clin Oncol 2015; 33: Abstr 9018. [Google Scholar]
- 27. Robert C, Long GV, Brady B. et al. Nivolumab in previously untreated melanoma without BRAF mutation. N Engl J Med. 2015; 372: 320–330. [DOI] [PubMed] [Google Scholar]
- 28. Brahmer J, Reckamp KL, Baas P. et al. Nivolumab versus docetaxel in advanced squamous-cell non-small-cell lung cancer. N Engl J Med 2015; 373: 123–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Motzer RJ, Escudier B, McDermott DF. et al. Nivolumab versus everolimus in advanced renal-cell carcinoma. N Engl J Med 2015; 373: 1803–1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Borghaei H, Paz-Ares L, Horn L. et al. Nivolumab versus docetaxel in advanced nonsquamous non-small-cell lung cancer. N Engl J Med 2015; 373: 1627–1639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ferris RL, Blumenschein GR, Fayette J. et al. Further evaluations of nivolumab (nivo) versus investigator’s choice (IC) chemotherapy for recurrent or metastatic (R/M) squamous cell carcinoma of the head and neck (SCCHN): CheckMate 141. J Clin Oncol 2016; 34: Abstr 6009. [Google Scholar]
- 32. Ansell SM, Lesokhin AM, Borrello I. et al. PD-1 blockade with nivolumab in relapsed or refractory Hodgkin’s lymphoma. N Engl J Med 2015; 372: 311–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Robert C, Schachter J, Long GV. et al. Pembrolizumab versus ipilimumab in advanced melanoma. N Engl J Med 2015; 372: 2521–2532. [DOI] [PubMed] [Google Scholar]
- 34. Ribas A, Puzanov I, Dummer R. et al. Pembrolizumab versus investigator-choice chemotherapy for ipilimumab-refractory melanoma (KEYNOTE-002): a randomised, controlled, phase 2 trial. Lancet Oncol 2015; 16: 908–918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Seiwert TY, Burtness B, Mehra R. et al. Safety and clinical activity of pembrolizumab for treatment of recurrent or metastatic squamous cell carcinoma of the head and neck (KEYNOTE-012): an open-label, multicentre, phase 1b trial. Lancet Oncol 2016; 17: 956–65. [DOI] [PubMed] [Google Scholar]
- 36. Armand P, Nagler A, Weller EA. et al. Disabling immune tolerance by programmed death-1 blockade with pidilizumab after autologous hematopoietic stem-cell transplantation for diffuse large B-cell lymphoma: results of an international phase II trial. J Clin Oncol 2013; 31: 4199–4206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Powles T, Eder JP, Fine GD. et al. MPDL3280A (anti-PD-L1) treatment leads to clinical activity in metastatic bladder cancer. Nature 2014; 515: 558–562. [DOI] [PubMed] [Google Scholar]
- 38. Brahmer JR, Tykodi SS, Chow LQ. et al. Safety and activity of anti-PD-L1 antibody in patients with advanced cancer. N Engl J Med 2012; 366: 2455–2465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Brahmer JR, Rizvi NA, Lutzky J. et al. Clinical activity and biomarkers of MEDI4736, an anti-PD-L1 antibody, in patients with NSCLC. J Clin Oncol 2014; 32: Abstr 8021. [Google Scholar]
- 40. Lutzky J, Antonia SJ, Blake-Haskins A. et al. A phase 1 study of MEDI4736, an anti–PD-L1 antibody, in patients with advanced solid tumors. J Clin Oncol 2014; 32: Abstr 3001. [Google Scholar]
- 41. Kaufman H, Hamid O, D’Angelo SP. et al. A phase II, open-label, multicenter trial to investigate the clinical activity and safety of avelumab (MSB0010718C) in patients with metastatic Merkel cell carcinoma. J Clin Oncol 2015; 33: Abstr TPS9086. [Google Scholar]
- 42. Sznol M. Phase I study of BMS-663513, a fully human anti-CD137 agonist monoclonal antibody, in patients (pts) with advanced cancer (CA). Presented at the American Society of Clinical Oncology annual meeting; May 30–June 3 2008; Chicago, IL, USA. Abstract 3007. [Google Scholar]
- 43. Vey N, Goncalves A, Karlin L. et al. A phase 1 dose-escalation study of IPH2102 (lirilumab, BMS-986015, LIRI), a fully human anti KIR monoclonal antibody (mAb) in patients (pts) with various hematologic (HEM) or solid malignancies (SOL). J Clin Oncol 2015; 33: Abstr 3065. [Google Scholar]
- 44. Brignone C, Escudier B, Grygar C. et al. A phase I pharmacokinetic and biological correlative study of IMP321, a novel MHC class II agonist, in patients with advanced renal cell carcinoma. Clin Cancer Res 2009; 15: 6225–6231. [DOI] [PubMed] [Google Scholar]
- 45. Mahadevan D, Lanasa MC, Whelden M. et al. First-in-human phase i dose escalation study of a humanized anti-CD200 antibody (samalizumab) in patients with advanced stage B cell chronic lymphocytic leukemia (B-CLL) or multiple myeloma (MM) [Abstract]. Presented at the 53rd ASH annual meeting; 10‒13 December 2011; San Diego, CA, USA. Abstract 2465.
- 46. Vonderheide RH, Flaherty KT, Khalil M. et al. Clinical activity and immune modulation in cancer patients treated with CP-870,893, a novel CD40 agonist monoclonal antibody. J Clin Oncol 2007; 25: 876–883. [DOI] [PubMed] [Google Scholar]
- 47. Rüter J, Antonia SJ, Burris HA. et al. Immune modulation with weekly dosing of an agonist CD40 antibody in a phase I study of patients with advanced solid tumors. Cancer Biol Ther 2010; 10: 983–993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. de Vos S, Forero-Torres A, Ansell SM. et al. A phase II study of dacetuzumab (SGN-40) in patients with relapsed diffuse large B-cell lymphoma (DLBCL) and correlative analyses of patient-specific factors. J Hematol Oncol 2014; 7: 44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Hussein M, Berenson JR, Niesvizky R. et al. A phase I multidose study of dacetuzumab (SGN-40; humanized anti-CD40 monoclonal antibody) in patients with multiple myeloma. Haematologica 2010; 95: 845–848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Advani R, Forero-Torres A, Furman RR. et al. Phase I study of the humanized anti-CD40 monoclonal antibody dacetuzumab in refractory or recurrent non-Hodgkin’s lymphoma. J Clin Oncol 2009; 27: 4371–4377. [DOI] [PubMed] [Google Scholar]
- 51. Hamid O, Thompson JA, Diab A. et al. First in human (FIH) study of an OX40 agonist monoclonal antibody (mAb) PF-04518600 (PF-8600) in adult patients (pts) with select advanced solid tumors: preliminary safety and pharmacokinetic (PK)/pharmacodynamics results. J Clin Oncol 2016; 34: Abstr 3079. [Google Scholar]
- 52. Bauer TM, Chae YK, Patel S. et al. A phase I study of MEDI6383, an OX40 agonist, in adult patients with select advanced solid tumors. J Clin Oncol 2015; 33: Abstr TPS3093. [Google Scholar]
- 53. Awada A, Rolfo CD, Rottey S. et al. A phase I, first-in-human study of ARGX-110, a monoclonal antibody targeting CD70, a receptor involved in immune escape and tumor growth in patients with solid and hematologic malignancies. J Clin Oncol 2014; 32: Abstr 3023. [Google Scholar]
- 54. Ansell SM, Northfelt DW, Flinn I. et al. Phase I evaluation of an agonist anti-CD27 human antibody (CDX-1127) in patients with advanced hematologic malignancies. J Clin Oncol 2014; 32: Abstr 3024. [Google Scholar]
- 55. Robert C, Thomas L, Bondarenko I. et al. Ipilimumab plus dacarbazine for previously untreated metastatic melanoma. N Engl J Med 2011; 364: 2517–2526. [DOI] [PubMed] [Google Scholar]
- 56. Schadendorf D, Hodi FS, Robert C. et al. Pooled analysis of long-term survival data from phase II and phase III trials of ipilimumab in unresectable or metastatic melanoma. J Clin Oncol 2015; 33: 1889–1894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Eggermont AM, Chiarion-Sileni V, Grob JJ. et al. Adjuvant ipilimumab versus placebo after complete resection of high-risk stage III melanoma (EORTC 18071): a randomised, double-blind, phase 3 trial. Lancet Oncol 2015; 16: 522–530. [DOI] [PubMed] [Google Scholar]
- 58. Weber JS, D’Angelo SP, Minor D. et al. Nivolumab versus chemotherapy in patients with advanced melanoma who progressed after anti-CTLA-4 treatment (CheckMate 037): a randomised, controlled, open-label, phase 3 trial. Lancet Oncol 2015; 16: 375–384. [DOI] [PubMed] [Google Scholar]
- 59. Panel chair. et al. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) Melanoma Version 1.2017. © 2016 National Comprehensive Cancer Network, Inc. Available at NCCN.org (18 September 2016, date last accessed).
- 60. Garon EB, Rizvi NA, Hui R. et al. Pembrolizumab for the treatment of non-small-cell lung cancer. N Engl J Med 2015; 372: 2018–2028. [DOI] [PubMed] [Google Scholar]
- 61. Snyder A, Makarov V, Merghoub T. et al. Genetic basis for clinical response to CTLA-4 blockade in melanoma. N Engl J Med 2014; 371: 2189–2199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Rizvi NA, Hellmann MD, Snyder A. et al. Cancer immunology. Mutational landscape determines sensitivity to PD-1 blockade in non-small cell lung cancer. Science 2015; 348: 124–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Van Allen EM, Miao D, Schilling B. et al. Genomic correlates of response to CTLA-4 blockade in metastatic melanoma. Science 2015; 350: 207–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Le DT, Uram JN, Wang H. et al. PD-1 blockade in tumors with mismatch-repair deficiency. N Engl J Med 2015; 372: 2509–2520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. El-Khoueiry AB, Melero I, Crocenzi TS. et al. Phase I/II safety and antitumor activity of nivolumab in patients with advanced hepatocellular carcinoma (HCC): CA209-040. J Clin Oncol 2015; 33: Abstr LBA101. [Google Scholar]
- 66. Nghiem P, Bhatia S, Daud A. et al. Activity of PD-1 blockade with pembrolizumab as first systemic therapy in patients with advanced Merkel cell carcinoma [Abstract]. Presented at the European Cancer Congress; 25‒29 September 2015; Vienna, Austria. Abstract 22LBA.
- 67. Spranger S., Bao R, Gajewski TF. Melanoma-intrinsic β-catenin signalling prevents anti-tumour immunity. Nature 2015; 523: 231–235. [DOI] [PubMed] [Google Scholar]
- 68. Peng W, Chen JQ, Liu C. et al. Loss of PTEN promotes resistance to T cell-mediated immunotherapy. Cancer Discov 2016; 6: 202–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Salama AK, Postow MA, Salama JK. Irradiation and immunotherapy: from concept to the clinic. Cancer 2016; 122: 1659–1671. [DOI] [PubMed] [Google Scholar]
- 70. Albers AE, Schaefer C, Visus C. Spontaneous apoptosis of tumor-specific tetramer+ CD8+ T lymphocytes in the peripheral circulation of patients with head and neck cancer. Head Neck 2009; 31: 773–781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Khan IS, Mouchess ML, Zhu ML. et al. Enhancement of an anti-tumor immune response by transient blockade of central T cell tolerance. J Exp Med 2014; 211: 761–768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Fourcade J, Sun Z, Pagliano O. et al. PD-1 and Tim-3 regulate the expansion of tumor antigen-specific CD8+ T cells induced by melanoma vaccines. Cancer Res 2014; 74: 1045–1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Chauvin JM, Pagliano O, Fourcade J. et al. TIGIT and PD-1 impair tumor antigen-specific CD8+ T cells in melanoma patients. J Clin Invest 2015; 125: 2046–2058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Gangadhar TC, Hamid O, Smith DC. et al. Preliminary results from a phase I/II study of epacadostat (incb024360) in combination with pembrolizumab in patients with selected advanced cancers. J Immunother Cancer 2015; 3(Suppl 2): O7. [Google Scholar]
- 75. Spranger S, Koblish HK, Horton B. et al. Mechanism of tumor rejection with doublets of CTLA-4, PD-1/PD-L1, or IDO blockade involves restored IL-2 production and proliferation of CD8(+) T cells directly within the tumor microenvironment. J Immunother Cancer 2014; 2: 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Gibney GT, Kudchadkar RR, DeConti RC. et al. Safety, correlative markers, and clinical results of adjuvant nivolumab in combination with vaccine in resected high-risk metastatic melanoma. Clin Cancer Res 2015; 21: 712–720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Hodi FS, Lee S, McDermott DF. et al. Ipilimumab plus sargramostim vs ipilimumab alone for treatment of metastatic melanoma: a randomized clinical trial. JAMA 2014; 312: 1744–1753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Kudchakar RR. A phase IB study of ipilimumab with peginterferon alfa-2b in patients with unresectable melanoma [Abstract]. Presented at the American Society for Clinical Oncology; May 31‒June 4 2013; Chicago, IL, USA. Abstract 9079. [DOI] [PMC free article] [PubMed]
- 79. Hodi FS, Lawrence D, Lezcano C. et al. Bevacizumab plus ipilimumab in patients with metastatic melanoma. Cancer Immunol Res 2014; 2: 632–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Minor DR, Puzanov I, Callahan MK. et al. Severe gastrointestinal toxicity with administration of trametinib in combination with dabrafenib and ipilimumab. Pigment Cell Melanoma Res 2015; 28: 611–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Ribas A, Butler M, Lutzky J. et al. Phase I study combining anti-PD-L1 (MEDI4736) with BRAF (dabrafenib) and/or MEK (trametinib) inhibitors in advanced melanoma. J Clin Oncol 2015; 33: Abstr 3003. [Google Scholar]
- 82. Bendell JC. Safety and efficacy of MPDL3280A (anti-PDL1) in combination with bevacizumab (bev) and/or FOLFOX in patients (pts) with metastatic colorectal cancer (mCRC). Presented at the American Society for Clinical Oncology Gastrointestinal Cancers Symposium; January 15‒17 2015; San Francisco, CA, USA. Abstract 704
- 83. Parry RV, Chemnitz JM, Frauwirth KA. et al. CTLA-4 and PD-1 receptors inhibit T-cell activation by distinct mechanisms. Mol Cell Biol 2005; 25: 9543–9553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Cha E, Klinger M, Hou Y. et al. Improved survival with T cell clonotype stability after anti-CTLA-4 treatment in cancer patients. Sci Transl Med 2014; 6: 238ra70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Selby M, Engelhardt J, Lu L-S. et al. Antitumor activity of concurrent blockade of immune checkpoint molecules CTLA-4 and PD-1 in preclinical models. J Clin Oncol 2013; 31: Abstr 3061. [Google Scholar]
- 86. Simpson TR, Li F, Montalvo-Ortiz W. et al. Fc-dependent depletion of tumor-infiltrating regulatory T cells co-defines the efficacy of anti-CTLA-4 therapy against melanoma. J Exp Med 2013; 210: 1695–1710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Atefi M, Avramis E, Lassen A. et al. Effects of MAPK and PI3K pathways on PD-L1 expression in melanoma. Clin Cancer Res 2014; 20: 3446–3457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Das R, Verma R, Sznol M. et al. Combination therapy with anti-CTLA-4 and anti-PD-1 leads to distinct immunologic changes in vivo. J Immunol. 2015; 194: 950–959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Wolchok JD, Kluger H, Callahan MK. et al. Nivolumab plus ipilimumab in advanced melanoma. N Engl J Med 2013; 369: 122–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Sznol M, Callahan MK, Kluger H. et al. Updated survival, response and safety data in a phase 1 dose-finding study (CA209-004) of concurrent nivolumab (NIVO) and ipilimumab (IPI) in advanced melanoma. Presented at the Society for Melanoma Research; 18‒21 November 2015; San Francisco, CA, USA.
- 91. Postow MA, Chesney J, Pavlick AC. et al. Nivolumab and ipilimumab versus ipilimumab in untreated melanoma. N Engl J Med 2015; 372: 2006–2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Hodi FS, Chesney J, Pavlick AC. et al. Combined nivolumab and ipilimumab versus ipilimumab alone in patients with advanced melanoma: 2-year overall survival outcomes in a multicentre, randomised, controlled, phase 2 trial. Lancet Oncol 2016; 17: 1558–1568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Larkin J, Chiarion-Sileni V, Gonzalez R. et al. Combined nivolumab and ipilimumab or monotherapy in untreated melanoma. N Engl J Med 2015; 373: 23–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Weber JS, Gibney G, Sullivan RJ. et al. Sequential administration of nivolumab and ipilimumab with a planned switch in patients with advanced melanoma (Checkmate 064): an open-label, randomised, phase 2 trial. Lancet Oncol 2016; 17: 943–955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Long GV, Atkinson V, Cebon JS. et al. Pembrolizumab (pembro) plus ipilimumab (ipi) for advanced melanoma: results of the KEYNOTE-029 expansion cohort [Abstract]. Presented at the American Society for Clinical Oncology; June 3‒June 7 2016; Chicago, IL, USA. Abstract 9506.
- 96. Hammers HJ, Plimack ER, Infante JR. et al. Expanded cohort results from CheckMate 016: a phase I study of nivolumab in combination with ipilimumab in metastatic renal cell carcinoma (mRCC). J Clin Oncol 2015; 33: Abstr 4516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Antonia SJ, Gettinger SN, Quan Man Chow L. et al. Nivolumab (anti-PD-1; BMS-936558, ONO-4538) and ipilimumab in first-line NSCLC: Interim phase I results. J Clin Oncol 2014; 32: Abstr 8023. [Google Scholar]
- 98. Antonia SJ, Bendell JC, Taylor MH. et al. Phase I/II study of nivolumab with or without ipilimumab for treatment of recurrent small cell lung cancer (SCLC): CA209-032. J Clin Oncol 2015; 33: Abstr 7503. [Google Scholar]
- 99. Sampson JH. Preliminary safety and activity of nivolumab and its combination with ipilimumab in recurrent glioblastoma (GBM): CHECKMATE-143. Presented at the American Society of Clinical Oncology; May 29‒June 2 2015; Chicago, IL, USA. Abstract 3010.
- 100. Tolcher AW, Sznol M, Hu-Lieskovan S. et al. Phase Ib study of PF-05082566 in combination with pembrolizumab in patients with advanced solid tumors. J Clin Oncol 2016; 34; Abstr 3002. [Google Scholar]
- 101. Rizvi NA, Gettinger SN, Goldman JW. et al. Safety and efficacy of first-line nivolumab and ipilimumab in non-small cell lung cancer [Abstract]. Presented at the World Conference on Lung Cancer; 6‒9 September 2015; Denver, CO, USA. Abstract ORAL02.05.
- 102. Wolchok JD, Chiarion-Sileni V, Gonzalez R. et al. Updated results from a phase III trial of nivolumab (NIVO) combined with ipilimumab (IPI) in treatment-naïve patients (pts) with advanced melanoma (MEL) (CheckMate 067). J Clin Oncol 2016; 34: Abstr 9505. [Google Scholar]
- 103. Phillips T, Simmons P, Inzunza HD. et al. Development of an automated PD-L1 immunohistochemistry (IHC) assay for non-small cell lung cancer. Appl Immunohistochem Mol Morphol 2015; 23: 541–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Kluger H, Sznol M, Callahan MK. et al. Survival, response duration, and activity by BRAF mutation status in a phase 1 trial of nivolumab (anti-PD-1, BMS-936558, ONO-4538) and ipilimumab concurrent or sequenced therapy in advanced melanoma. Presented at ESMO 2014.
- 105. Weber JS, Kudchadkar RR, Yu B. et al. Safety, efficacy, and biomarkers of nivolumab with vaccine in ipilimumab-refractory or -naive melanoma. J Clin Oncol. 2013; 31: 4311–4318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Friedman CF, Navid-Azarbaijani P, Shoushtari AN. et al. Toxicity associated with ipilimumab and nivolumab (Ipi+Nivo) combination therapy in melanoma patients (pts) treated at a single-institution under an expanded-access program (EAP). J Clin Oncol 2016; 34; Abstr 9519. [Google Scholar]
- 107. Hodi FS, Postow MA, Chesney JA. et al. Clinical response, progression-free survival (PFS), and safety in patients (pts) with advanced melanoma (MEL) receiving nivolumab (NIVO) combined with ipilimumab (IPI) vs IPI monotherapy in CheckMate 069 study [Abstract]. Presented at the American Society for Clinical Oncology; May 29‒June 2 2015; Chicago, IL, USA. Abstract 9004.
- 108. Hodi FS, Postow MA, Chesney JA. et al. Overall survival in patients with advanced melanoma (MEL) who discontinued treatment with nivolumab (NIVO) plus ipilimumab (IPI) due to toxicity in a phase II trial (CheckMate 069) [Abstract]. Presented at the American Society for Clinical Oncology; June 3‒June 7 2016; Chicago, IL, USA. Abstract 9518.
- 109. Ryder M, Callahan M, Postow MA. Endocrine-related adverse events following ipilimumab in patients with advanced melanoma: a comprehensive retrospective review from a single institution. Endocr Relat Cancer 2014; 21: 371–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Hoos A, Ibrahim R, Korman A. et al. Development of ipilimumab: contribution to a new paradigm for cancer immunotherapy. Semin Oncol 2010; 37: 533–546. [DOI] [PubMed] [Google Scholar]
- 111. Horvat TZ, Adel NG, Dang TO. et al. Immune-related adverse events, need for systemic immunosuppression, and effects on survival and time to treatment failure in patients with melanoma treated with ipilimumab at Memorial Sloan Kettering Cancer Center. J Clin Oncol 2015; 33: 3193–3198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Johnson DB, Sullivan RJ, Ott P. et al. Ipilimumab therapy in patients with advanced melanoma and preexisting autoimmune disorders. JAMA Oncol 2016; 2: 234–240. [DOI] [PubMed] [Google Scholar]
- 113. Kyi C, Carvajal RD, Wolchok JD, Postow MA. Ipilimumab in patients with melanoma and autoimmune disease. J Immunother Cancer 2014; 2: 35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Menzies AM, Johnson DB, Ramanujam S. et al. Anti-PD-1 therapy in patients with advanced melanoma and preexisting autoimmune disorders (AD) or major toxicity with ipilimumab (IPI) [Abstract]. Presented at the American Society for Clinical Oncology; June 3‒June 7 2016; Chicago, IL, USA. Abstract 9515.
- 115. Bostwick AD, Salama AK, Hanks BA. Rapid complete response of metastatic melanoma in a patient undergoing ipilimumab immunotherapy in the setting of active ulcerative colitis. J Immunother Cancer 2015; 3: 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Saltz L. Perspectives on Value [plenary lecture]. Presented at the American Society of Clinical Oncology; May 29‒June 2 2015; Chicago, IL, USA.
- 117. Herbst RS, Soria JC, Kowanetz M. et al. Predictive correlates of response to the anti-PD-L1 antibody MPDL3280A in cancer patients. Nature. 2014; 515: 563–567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Kefford R, Ribas A, Hamid O. et al. Clinical efficacy and correlation with tumor PD-L1 expression in patients (pts) with melanoma (MEL) treated with the anti-PD-1 monoclonal antibody MK-3475. Presented at the American Society of Clinical Oncology; May 30‒June 3 2014; Chicago, IL, USA. Abstract 3005.
- 119. Taube JM, Klein AP, Brahmer JR. et al. Association of PD-1, PD-1 ligands, and other features of the tumor immune microenvironment with response to anti-PD-1 therapy. Clin Cancer Res 2014; 20: 5064–5074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Topalian SL, Hodi FS, Brahmer JR. et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med 2012; 366: 2443–2454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Meng X, Huang Z, Teng F. et al. Predictive biomarkers in PD-1/PD-L1 checkpoint blockade immunotherapy. Cancer Treat Rev. 2015; 41: 868–876. [DOI] [PubMed] [Google Scholar]
- 122. Madore J, Vilain RE, Menzies AM. et al. PD-L1 expression in melanoma shows marked heterogeneity within and between patients: implications for anti-PD-1/PD-L1 clinical trials. Pigment Cell Melanoma Res 2015; 28: 245–253. [DOI] [PubMed] [Google Scholar]
- 123. Tumeh PC, Harview CL, Yearley JH. et al. PD-1 blockade induces responses by inhibiting adaptive immune resistance. Nature 2014; 515: 568–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Galon J, Mlecnik B, Marliot F. et al. Validation of the Immunoscore (IM) as a prognostic marker in stage I/II/III colon cancer: results of a worldwide consortium: final analysis of 1,336 patients. J Clin Oncol 2016; 34: Abstr 3500. [Google Scholar]
- 125. Mlecnik B, Church S, Berger A, Galon J. Immunoscore® as a predictor of response to chemotherapy in stage II and stage III colon cancer. Society for Immunotherapy of Cancer; 2015; National Harbor, MD. [Google Scholar]
- 126. Ascierto PA, Capone M, Urba WJ. et al. The additional facet of immunoscore: immunoprofiling as a possible predictive tool for cancer treatment. J Transl Med 2013; 11: 54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Galon J, Pagès F, Marincola FM. et al. The immune score as a new possible approach for the classification of cancer. J Transl Med 2012; 10: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Daud AI, Loo K, Pauli ML. et al. Tumor immune profiling predicts response to anti-PD-1 therapy in human melanoma. J Clin Invest 2016; 126: 3447–3452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Loo K, Tsai KK, Pauli M. et al. Novel T cell exhaustion marker to predict monotherapy PD-1 compared to combination CTLA-4 and PD-1 response in melanoma [Abstract]. Presented at the American Society for Clinical Oncology; June 3‒June 7 2016; Chicago, IL, USA. Abstract 9520.
- 130. Hamid O, Chow LQM, Tavakkoli F. et al. Phase I, open-label study of MEDI0680, an anti-programmed cell death-1 (PD-1) antibody, in combination with MEDI4736, an anti-programmed cell death ligand-1 (PD-L1) antibody, in patients with advanced malignancies. J Clin Oncol 2015; 33: Abstr TPS3087. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.