Abstract
BACKGROUND
To examine current patterns of hypertension (HTN) treatment in the United States, including blood pressure (BP) control, prevalence of different antihypertensive agents, and variations in treatment associated with patient and physician characteristics.
METHODS
We used data from the National Disease and Therapeutic Index (NDTI), a nationally representative physician survey produced by QuintilesIMS. We selected patients with a diagnosis of HTN and identified those prescribed antihypertensive therapies. We analyzed the type of antihypertensive agents prescribed. Extent of BP control, and associated patient and physician characteristics. We calculated 95% confidence intervals that accounted for the multistage NDTI sampling design.
RESULTS
Among those treated for HTN in 2014, BP control varied: systolic BP (SBP) ≥160 (15%) vs. SBP 150–159 (9%) vs. SBP 140–149 (19%) vs. SBP 130–139 (26%) vs. SBP <130 (32%). Of those treated for HTN, 29% used of angiotensin-converting enzyme inhibitors (ACEIs); 24%, thiazide-like diuretics; 22%, angiotensin receptor blockers (ARBs), 21%, calcium-channel blockers (CCBs); and 19% beta-blockers. Newer drugs had very limited uptake; no drugs approved after 2002 were used in more than 5% of patients. Selection of agents varied only modestly by patient and physician characteristics.
CONCLUSIONS
The treatment of HTN in 2014 predominantly involved older medications in 5 major classes of drugs: ACEIs, thiazide diuretics, ARBs, CCBs, and beta-blockers. Selection of antihypertensive agents showed limited variation by age, gender, race, and insurance type. Although 58% of treated patients had SBP <140, 24% had poorly controlled HTN with SBP ≥150, indicating the need for improved treatment.
Keywords: antihypertensive drugs, blood pressure, epidemiology, hypertension, prescribing pattern, prevalence
Hypertension (HTN) affects over 70 million individuals in the United States and is one of the major risk factors for cardiovascular disease (CVD).1,2 From 2011 to 2014, the prevalence of HTN was 30.0% among adult men and 28.1% among adult women, and the prevalence of HTN from 1999 to 2014 has remained stable over time.3–5 Annual cost of HTN is over $42.9 billion, with over $20.4 billion spent on prescription medications.6
Blood pressure (BP) increases the risk of CVD events independent of other risk factors, and higher BPs lead to greater risk of myocardial infarction, heart failure, stroke, and kidney disease.1 CVD is currently the leading cause of death in the United States and accounts for 17% of overall national health expenditures.7 HTN is present in 51.0% of adults with CVD, and 40.6% of CVD mortality has been attributable to HTN.8
BP-lowering treatments significantly reduce the risk of CVD and death in various patient populations—a 10 mm Hg reduction in systolic BP (SBP) has been shown to reduce the risk of major CVD events by 20%, coronary heart disease by 17%, stroke by 27%, heart failure by 28%, and all-cause mortality by 13%.9,10 While treatment rates for HTN have increased from 65% (2003–2004) to 75% (2011–2012), and adequate BP control has improved from 40% to 52%, detection, treatment, and control of HTN remains suboptimal.11 Healthy People 2020 goals include controlling 62% of all adults with HTN.12
Thiazide-like diuretics are the recommended initial therapy for most patients, either alone or in combination with one of the other classes.6 All classes of BP-lowering drugs have a similar effect in reducing coronary heart disease and stroke for a given reduction in BP, with the exception of the extra protective effect of beta-blockers shortly after a myocardial infarction, the effect of calcium-channel blockers (CCBs) in preventing stroke, and the effect of thiazides in preventing heart failure.13,14 Past estimates indicate that the medications prescribed for HTN in the United States have changed over time. From 1997 to 2012, angiotensin receptor blocker (ARB) use has increased from 3% to 18%, CCB use has decreased from 27% to 18%, diuretic use has been stable at 24–30%, and beta-blocker use has been stable at 14–16%.15
We used nationally representative audit data from U.S. office-based physicians to examine patterns of HTN treatment in 2014. These national data describe the population treated for HTN, define the medications used in treatment, and assess the adequacy of BP control.
METHODS
Data collection
Data were extracted from the National Disease and Therapeutic Index (NDTI), an ongoing nationally representative physician survey produced by QuintilesIMS (Plymouth Meeting, PA; formerly IMS Health). The NDTI is a quarterly audit of approximately 4,800 office-based physicians that provide information regarding patterns and treatment of disease in the United States. The physicians are selected from master lists of the American Medical Association and the American Osteopathic Association through random sampling stratified by specialty and geographic area. The universe of physicians from which samples are drawn includes physicians who are directly involved in office-based care, and therefore excludes specialties such as pathology, anesthesiology, and radiology. Participating physicians are surveyed for a 2-day period during each calendar quarter, and they complete an encounter form for each patient seen. For each encounter form, drug therapies are linked to the diagnosis specific 6-digit taxonomic codes representing diagnostic information (similar to ICD-9). The encounter form captures information on both newly prescribed and continued medications as well as nonprescription medications. In addition to diagnostic and drug information, the NDTI also provides information regarding patient characteristics (age, gender, race, insurance type, SBP, diastolic BP, etc.) as well as information regarding physician characteristics (specialty, region, etc.).
Information from this sample is then used to calculate representative national projections by assigning weights to each sample encounter. These weights account an independent estimate of total national encounters, the representativeness of specialties, and the number of visits sample by each physician. For example, visits to physicians who collect fewer visits would receive a larger weight compared to physicians who collect more visits.16–21
Using the data available within the NDTI, the ICD-9 code used to select for patients within our study with a diagnosis of HTN were 401.0 (malignant essential HTN), 401.1 (benign essential HTN), and 401.9 (unspecified essential HTN).22,23 These ICD-9 codes have been used in previous studies to define a diagnosis of HTN.24,25 Since the focus of the study involved national trends in the management of all severities of primary HTN, no clinical exclusion criteria were applied. Among the patients identified to have one of the above diagnoses of HTN from January 2014 through December 2014, prescribed antihypertensive therapies were identified using the 5-digit Uniform System of Classification (USC). For patients prescribed 2 or 3-drug combination medications, each chemical component was counted once as if they were separate. Data were stratified by different patient, provider, and visit characteristic groups.
Analysis
The percentage of each antihypertensive class prescribed was calculated by dividing the total number of each drug class prescribed by the total number of treatment visits for HTN. Patients taking a particular class were defined as the weighted national projection of the number of visits to patients with a diagnosis of HTN and treatment with that particular medication class. Total patients were defined as the national weighted projection of the number of visits by patients with a diagnosis of HTN and treatment with at least one antihypertensive medications.
Because many patients are taking more than one medication, the sum of these percentages is greater than 100%. To compare medication selection among different patient and physician strata, we calculated the proportional use by agent within each subpopulation (i.e., females prescribed angiotensin-converting enzyme inhibitors [ACEIs] divided by total number of females treated for HTN). To account for the small percentage of data reported as “N/A” or “unspecified”, these groups were redistributed into the other data groups based on weighted percentages. Ninety-five percent confidence intervals (CIs) were calculated using available tables of relative standard errors that account for the complex, multistage NDTI sampling design of each annual audit. Descriptive statistics were used to examine the prescribed antihypertensive agents and drug classes, as well as the patient and physician characteristics associated with particular antihypertensive agents. P values were calculated using a 2-tailed t-test.
RESULTS
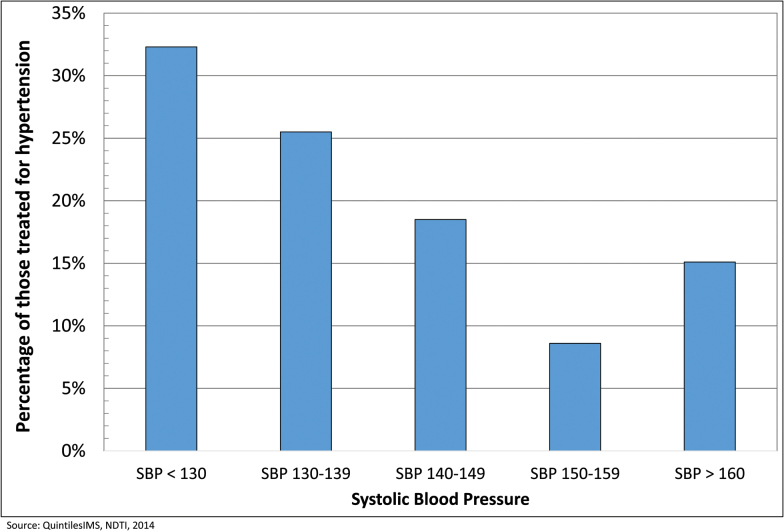
The total number of visits by patients with HTN in 2014 associated with antihypertensive treatment was 95.1 million (95% CI, 94.7–95.5). Among those treated for HTN, there were more patients age ≥ 60 (62%) vs. age <60 (38%), more White patients (68%) compared to Black (19%), Hispanic (6%), or Asian patients (5%) and more patients covered by Medicare (38%) and 3rd party insurance (32%) compared to HMO (17%) and Medicaid (5%) (Table 1). Most patients were treated by primary care physicians (75%) with 10% treated by cardiologists and 15% by a variety of other specialties. BP control widely varied among this medication-treated group of patients: SBP ≥160 (15%) vs. SBP 150–159 (9%) vs. SBP 140–149 (19%) vs. SBP 130–139 (26%) vs. SBP <130 (32%) (Figure 1).
Table 1.
Patient characteristics
| National projection in millions | Percentage among those treated for hypertension | |
|---|---|---|
| Age < 60 | 36.5 | 38.4% |
| Age ≥ 60 | 58.6 | 61.6% |
| Gender | ||
| Female | 48.1 | 50.5% |
| Male | 47.0 | 49.5% |
| Race | ||
| White | 64.8 | 68.2% |
| Asian | 4.6 | 4.8% |
| Black | 17.7 | 18.6% |
| Hispanic | 5.7 | 6.0% |
| Other/unspecified | 2.3 | 2.4% |
| Insurance | ||
| 3rd party | 30.2 | 31.8% |
| HMO | 16.5 | 17.4% |
| Medicare | 35.8 | 37.6% |
| Medicaid | 5.2 | 5.4% |
| Other | 7.4 | 7.8% |
| Patient SBP | ||
| SBP < 130 | 30.4 | 32.3% |
| SBP 130–139 | 24.0 | 25.5% |
| SBP 140–149 | 17.4 | 18.5% |
| SBP 150–159 | 8.1 | 8.6% |
| SBP ≥ 160 | 14.2 | 15.1% |
| Prescriber specialty | ||
| Cardiology | 9.9 | 10.4% |
| Primary carea | 71.5 | 75.2% |
| Other | 13.7 | 14.4% |
| Prescriber region | ||
| East | 22.7 | 23.9% |
| Midwest | 19.6 | 20.6% |
| South | 35.5 | 37.4% |
| West | 17.3 | 18.2% |
aPrimary care includes family practice, general practice, internal medicine, geriatrics.
Abbreviation: SBP, systolic blood pressure.
Source: QuintilesIMS, NDTI, 2014.
Figure 1.
Systolic blood pressure among those treated for hypertension. (Adapted from QuintilesIMS, NDTI, 2014.)
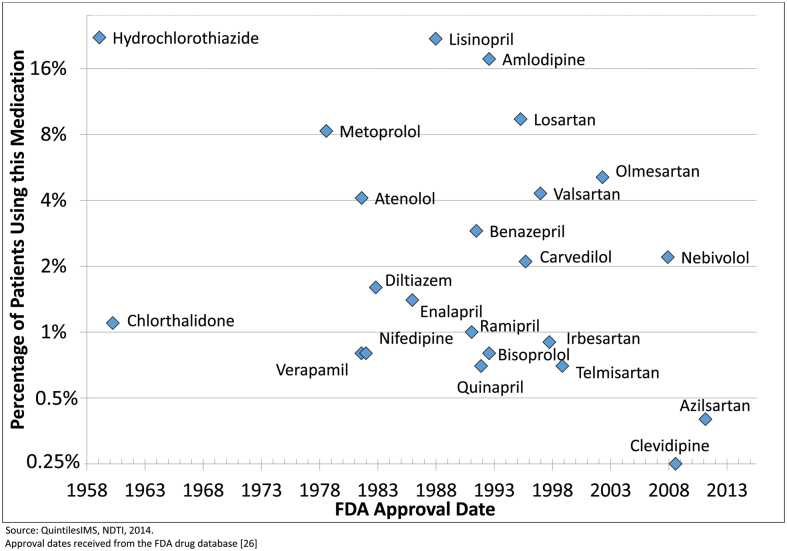
Of those treated for HTN, ACEIs were used in 28.5% (95% CI, 28.3–28.6%) followed by thiazide diuretics at 24.2% (95% CI, 24.0–24.4%), ARBs at 21.5% (95% CI, 21.3–21.6%), CCBs at 21.1% (95% CI, 21.0–21.3%), and beta-blockers at 18.7% (95% CI, 18.6–18.9%). Lisinopril was the most commonly prescribed ACEI (21.9% of all patients), followed by benazepril (2.9%), enalapril (1.4%), and ramipril (1.0%). Hydrochlorothiazide was the most commonly prescribed thiazide (22.2%), followed by chlorthalidone (1.1%). Losartan was the most commonly prescribed ARB (9.4%), followed by olmesartan (5.1%), and valsartan (4.3%). Amlodipine was the most commonly prescribed CCB (17.7%), followed by diltiazem (1.6%). Metoprolol was the most common beta-blocker (8.3%), followed by atenolol (4.1%), nebivolol (2.2%), and carvedilol (2.1%) (Table 2). The most commonly prescribed antihypertensive agents were approved over 2 decades ago. All antihypertensive agents prescribed to more than 5% of patients had an approval date of 2002 or earlier26 (Figure 2).
Table 2.
Drug class details among top 5 classes of antihypertensive drugs prescribed in 2014
| Drug name | National projection in millions | Percentage of treated patients on this medication |
|---|---|---|
| ACEIs | 27.1 | 28.5% |
| Lisinopril | 20.8 | 21.9% |
| Benazepril | 2.8 | 2.9% |
| Enalapril | 1.3 | 1.4% |
| Ramipril | 1.0 | 1.0% |
| Quinapril | 0.7 | 0.7% |
| Other | 0.5 | 0.5% |
| Thiazides | 23.0 | 24.2% |
| Hydrochlorothiazide | 21.1 | 22.2% |
| Chlorthalidone | 1.0 | 1.1% |
| Other | 0.9 | 0.9% |
| ARBs | 20.4 | 21.5% |
| Losartan | 9.0 | 9.4% |
| Olmesartan | 4.9 | 5.1% |
| Valsartan | 4.1 | 4.3% |
| Irbesartan | 0.8 | 0.9% |
| Telmisartan | 0.7 | 0.7% |
| Other | 1.0 | 1.0% |
| CCBs | 20.1 | 21.1% |
| Amlodipine | 16.8 | 17.7% |
| Diltiazem | 1.5 | 1.6% |
| Verapamil | 0.8 | 0.8% |
| Nifedipine | 0.8 | 0.8% |
| Other | 0.2 | 0.2% |
| Beta blockers | 17.8 | 18.7% |
| Metoprolol | 7.9 | 8.3% |
| Atenolol | 3.9 | 4.1% |
| Nebivolol | 2.1 | 2.2% |
| Carvedilol | 2.0 | 2.1% |
| Bisoprolol | 0.7 | 0.8% |
| Labetalol | 0.5 | 0.5% |
| Other | 0.6 | 0.7% |
| Nonthiazide diuretics | 4.1 | 4.3% |
| Triamterene | 2.0 | 2.1% |
| Furosemide | 1.0 | 1.0% |
| Other | 0.6 | 0.6% |
| Central acting agents | 1.4 | 1.5% |
| Clonidine | 1.3 | 1.4% |
| Other | 0.1 | 0.1% |
| Vasodilators | 0.7 | 0.7% |
| Hydralazine | 0.6 | 0.6% |
| Other | 0.0 | 0.1% |
Abbreviations: ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin receptor blocker; CCB, calcium-channel blockers.
Source: QuintilesIMS, NDTI, 2014.
Figure 2.
Original approval date of the antihypertensive drugs by prescribing prevalence. (Adapted from QuintilesIMS, NDTI, 2014. Approval dates received from the FDA drug database [26].)
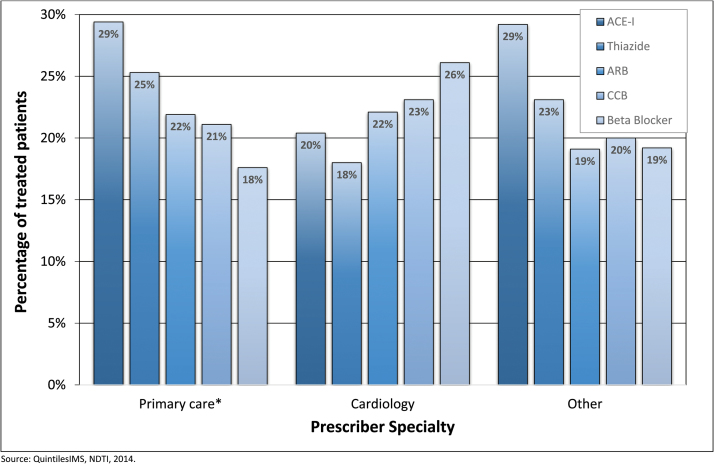
Selection of agents varied modestly among different patient groups. The proportional use of ACEIs was higher among those age <60 vs. age ≥60 (34% vs. 27%, P < 0.001), and use of thiazides was also higher (27% vs. 24%, P < 0.001). Use of ACEIs was higher among men vs. women (32% vs. 26%, P < 0.001) and use of beta-blockers was lower (18% vs. 21%, P < 0.001). Use of CCBs was higher among Blacks vs. Whites (27% vs. 20%, P < 0.001) and use of thiazides was also higher (28% vs. 23%, P < 0.001) whereas use of ACEIs was lower (24% vs. 30%, P < 0.001). Use of ARBs was higher among Asians vs. Whites (30% vs. 21%, P < 0.001). Use of ARBs was lower among those with Medicaid vs. those with 3rd party and PPO insurance (12% vs. 24%, P < 0.001), and use of thiazides was also lower (23% vs. 28%, P < 0.001) (Table 3). Primary care providers were more likely to prescribe ACEIs compared to cardiologists (29% vs. 20%, P < 0.001) as well as thiazides (25% vs. 18%, P < 0.001), whereas primary care providers were less likely to prescribe beta-blockers compared to cardiologists (18% vs. 26%, P < 0.001) (Figure 3).
Table 3.
Percentage of patients in each stratum taking a particular drug class
| ACEI | Thiazide | CCB | ARB | Beta blocker | Alpha blocker | Nonthiazide diuretics | Other | Total | |
|---|---|---|---|---|---|---|---|---|---|
| Total | 28.5% | 24.2% | 21.1% | 21.5% | 18.7% | 0.6% | 3.7% | 2.4% | 120.7% |
| Age | |||||||||
| Age < 60 | 33.9% | 27.2% | 20.2% | 22.7% | 16.7% | 0.3% | 3.2% | 2.5% | 126.7% |
| Age ≥ 60 | 26.5% | 23.5% | 22.8% | 21.8% | 20.9% | 0.8% | 4.2% | 2.5% | 123.0% |
| Gender | |||||||||
| Female | 26.0% | 25.5% | 20.9% | 21.7% | 20.5% | 0.4% | 4.6% | 2.9% | 122.5% |
| Male | 31.9% | 23.7% | 22.1% | 22.0% | 17.5% | 0.8% | 3.0% | 2.0% | 122.9% |
| Race | |||||||||
| White | 29.6% | 23.4% | 19.6% | 21.2% | 19.9% | 0.5% | 3.7% | 2.1% | 120.0% |
| Black | 24.3% | 27.8% | 27.4% | 19.8% | 15.5% | 0.7% | 4.7% | 4.1% | 124.2% |
| Hispanic | 30.5% | 27.6% | 16.5% | 22.3% | 16.8% | 1.2% | 2.0% | 2.6% | 119.6% |
| Asian | 23.9% | 19.9% | 25.2% | 29.5% | 17.9% | 0.4% | 2.5% | 1.9% | 121.2% |
| Other/unspecified | 31.3% | 19.2% | 20.4% | 24.2% | 17.7% | 0.5% | 2.9% | 1.1% | 117.3% |
| Insurance | |||||||||
| 3rd party and PPO | 29.7% | 27.5% | 19.9% | 24.4% | 17.2% | 0.5% | 3.6% | 2.1% | 124.9% |
| HMO | 30.6% | 24.5% | 20.3% | 23.1% | 17.1% | 0.7% | 3.1% | 1.4% | 120.8% |
| Medicare | 25.2% | 21.3% | 22.9% | 20.6% | 21.0% | 0.6% | 4.2% | 2.9% | 118.6% |
| Medicaid | 32.4% | 22.9% | 20.8% | 12.4% | 16.8% | 0.4% | 3.9% | 4.6% | 114.1% |
| Other | 31.6% | 25.1% | 19.9% | 16.3% | 19.0% | 0.6% | 3.0% | 3.0% | 118.6% |
| Old vs. new prescription | |||||||||
| Continued therapy | 31.1% | 26.1% | 22.7% | 22.8% | 20.5% | 0.5% | 4.0% | 2.2% | 129.9% |
| New therapy | 27.3% | 25.0% | 22.5% | 24.0% | 17.8% | 1.2% | 4.1% | 4.7% | 126.6% |
| Prescriber specialty | |||||||||
| Primary carea | 29.4% | 25.3% | 21.1% | 21.9% | 17.6% | 0.5% | 3.9% | 2.0% | 121.7% |
| Cardiology | 20.4% | 18.0% | 23.1% | 22.1% | 26.1% | 0.9% | 3.7% | 2.9% | 117.2% |
| Other | 29.2% | 23.1% | 20.0% | 19.1% | 19.2% | 0.5% | 2.9% | 4.5% | 118.4% |
| Prescriber region | |||||||||
| East | 24.8% | 23.9% | 22.9% | 24.6% | 19.9% | 0.4% | 5.9% | 2.2% | 124.5% |
| Midwest | 32.5% | 25.8% | 19.2% | 17.7% | 19.4% | 0.7% | 7.1% | 2.0% | 124.4% |
| South | 27.9% | 24.4% | 22.1% | 21.8% | 18.6% | 0.7% | 9.3% | 2.9% | 127.6% |
| West | 29.9% | 22.4% | 19.1% | 20.9% | 16.7% | 0.5% | 7.1% | 2.4% | 119.0% |
| SBP | |||||||||
| SBP < 130a | 31.1% | 25.1% | 20.0% | 21.1% | 20.4% | 0.3% | 3.8% | 2.0% | 123.9% |
| SBP 130–139a | 29.7% | 27.8% | 23.1% | 22.3% | 17.2% | 0.4% | 4.3% | 3.0% | 127.8% |
| SBP 140–149a | 27.7% | 24.7% | 23.7% | 22.5% | 17.8% | 1.0% | 4.0% | 3.1% | 124.5% |
| SBP 150–159a | 25.6% | 25.4% | 24.9% | 23.0% | 17.9% | 0.6% | 2.4% | 5.3% | 125.2% |
| SBP ≥ 160a | 25.4% | 26.0% | 26.0% | 20.5% | 20.6% | 0.8% | 3.2% | 9.4% | 131.8% |
Abbreviations: ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin receptor blocker; CCB, calcium-channel blockers; SBP, systolic blood pressure.
aPrimary care includes family practice, general practice, internal medicine, geriatrics.
Source: QuintilesIMS, NDTI, 2014.
Figure 3.
Prescribing patterns of antihypertensive therapy stratified by specialty—primary care, cardiology, and other. (Adapted from QuintilesIMS, NDTI, 2014.)
ACEI use was significantly more likely in patients with SBP <130 (31.1%) compared with those with BP ≥160 (25.4%). In contrast, the use of CCBs was less likely among those with SBP <130 (20.0%), but more likely among those with SBP ≥160 (26.0%) (Table 3).
DISCUSSION
Nationally representative data of office-based physicians from the NDTI was used to identify prescribing patterns for HTN in 2014. Compared to the U.S. general population, those treated for HTN in 2014 tended to be older (62% age ≥60 among those with treated HTN vs. 18% in the general population),27 were less likely to be White (68% among those with treated HTN vs. 77% in the general population), were more likely to be Black (19% among those treated with HTN vs. 13% in the general population).28 The majority of prescribers were primary care physicians (75.2%), and from the southern United States. Although 58% of patients being treated had SBP <140, many had SBP ≥140, including 9% with SBP 150–159 and 15% with SBP ≥160. Inadequate BP control in this setting is particularly concerning. All were accessing outpatient services and were reported to be on antihypertensive medications, thereby surmounting 2 common barriers to adequate HTN control.
The treatment of HTN in 2014 predominantly involved 5 major classes of drugs: ACEIs, thiazide diuretics, ARBs, CCBs, and beta-blockers. Selection of antihypertensive agents was generally consistent across patient subpopulations, but varied occasionally between age, gender, race, and insurance type. JNC 7 Guideline recommended use of thiazide-type diuretics for most patients as first-line therapy; however, thiazide diuretics were not the most prevalent drug class in 2014. This may reflect JNC 8 guideline equally emphasis on of thiazide, CCB, ACEI, or ARB as first-line agents in non-Black populations. An analysis of baseline data from SPRINT also found that thiazide prescription below expected levels—while 43% of the cohort was on a thiazide at baseline, the prevalence of thiazide prescription was only 16% among participants treated with a single agent, and over one third of patients taking ≥3 agents did not receive a thiazide.29
Use of ARBs was lower among those with Medicaid vs. all other insurance types, which may reflect the higher cost of most ARBs. Losartan, which became available as a generic in 2010, is the most commonly prescribed ARBs. Beta-blockers were more likely to be prescribed by cardiologists vs. primary care providers likely resulting from other cardiovascular indications that coexist with HTN, including atrial fibrillation, coronary artery disease, and congestive heart failure.
The predominance of ACEI, BB, CCB, thiazide-type diuretic, and ARB, also indicates that newer drugs with novel mechanisms of action, such as aliskiren and eplerenone, have been minimally adopted into practice. All prominently used medications were more than 12 years old.
We observed an association of ACEI use with better BP control and CCB with worse control. Although differences in drug effectiveness may contribute to these findings, other explanations may be possible, including the sequence by which drugs are selected and differences in the populations treated with these 2 drug classes (e.g., use of CCBs is more common in African Americans, who generally had worse control than other subpopulations).
There are several limitations that exist within our study. The sample analyzed may differ from the general population of Americans with HTN. Patient and physician characteristics collected on the survey are also limited. Additionally, patients making multiple visits in 2014 could have contributed more data to the national weighted projections, a potential bias that could have been reflected in our study results. We are also not able to identify other concomitant indications for antihypertensive medications such as chronic kidney disease, coronary heart disease, congestive heart failure, and atrial fibrillation, which could affect treatment indication and selection of drug class. The NDTI does not account patient adherence to medications, but represents the prescription orders generated by physicians. While more complicated patients may be over-represented among those seen in doctors’ offices, patients in this audit may show better BP control given their access to prescription medications and outpatient care.
In conclusions, the treatment of HTN in 2014 predominantly involved 5 major classes of drugs: ACEIs, thiazide diuretics, ARBs, CCBs, and beta-blockers with overwhelming use of older agents. Given the studied patients’ access to outpatient care and medications, observed BP control was suboptimal. Our findings indicate a need for focused efforts to improve BP control, particularly in the 24% of treated patients with SBP ≥150.
DISCLOSURE
Dr. Stafford was supported by a mid-career mentoring award (NIH K24 HL086703) and serves as an unpaid member of a QuintilesIMS scientific advisory committee. The other author declared no conflict of interest.
REFERENCES
- 1. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, Jones DW, Materson BJ, Oparil S, Wright JT, Jr, Roccella EJ; National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003; 289:2560–2572. [DOI] [PubMed] [Google Scholar]
- 2. Rosamond W, Flegal K, Furie K, Go A, Greenlund K, Haase N, Hailpern SM, Ho M, Howard V, Kissela B, Kittner S, Lloyd-Jones D, McDermott M, Meigs J, Moy C, Nichol G, O’Donnell C, Roger V, Sorlie P, Steinberger J, Thom T, Wilson M, Hong Y. Heart disease and stroke statistics: 2008 update at-a-glance. Dallas: American Heart Association, 2008. [DOI] [PubMed] [Google Scholar]
- 3. Vasan RS, Beiser A, Seshadri S, Larson MG, Kannel WB, D’Agostino RB, Levy D. Residual lifetime risk for developing hypertension in middle-aged women and men: The Framingham Heart Study. JAMA 2002; 287:1003–1010. [DOI] [PubMed] [Google Scholar]
- 4. Egan BM, Li J, Hutchison FN, Ferdinand KC. Hypertension in the United States, 1999 to 2012: progress toward Healthy People 2020 goals. Circulation 2014; 130:1692–1699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Yoon SS, Carroll MD, Fryar CD. Hypertension Prevalence and Control Among Adults: United States, 2011–2014. NCHS Data Brief. 2015;(220):1–8. [PubMed] [Google Scholar]
- 6. Davis K; Agency for Healthcare Research and Quality Medical Expenditure Panel Survey Expenditures for Hypertension among Adults Age 18 and Older, 2010: Estimates for the U.S. Civilian Noninstitutionalized Population <http://meps.ahrq.gov/mepsweb/data_files/publications/st404/stat404.shtml> 2013. Accessed 27 March 2016.
- 7. Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD, Finkelstein EA, Hong Y, Johnston SC, Khera A, Lloyd-Jones DM, Nelson SA, Nichol G, Orenstein D, Wilson PW, Woo YJ; American Heart Association Advocacy Coordinating Committee; Stroke Council; Council on Cardiovascular Radiology and Intervention; Council on Clinical Cardiology; Council on Epidemiology and Prevention; Council on Arteriosclerosis; Thrombosis and Vascular Biology; Council on Cardiopulmonary; Critical Care; Perioperative and Resuscitation; Council on Cardiovascular Nursing; Council on the Kidney in Cardiovascular Disease; Council on Cardiovascular Surgery and Anesthesia, and Interdisciplinary Council on Quality of Care and Outcomes Research Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation 2011; 123:933–944. [DOI] [PubMed] [Google Scholar]
- 8. Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Judd SE, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Mackey RH, Magid DJ, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER, 3rd, Moy CS, Mussolino ME, Neumar RW, Nichol G, Pandey DK, Paynter NP, Reeves MJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Wong ND, Woo D, Turner MB; American Heart Association Statistics Committee and Stroke Statistics Subcommittee Heart disease and stroke statistics–2014 update: a report from the American Heart Association. Circulation 2014; 129:e28–e292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, Chalmers J, Rodgers A, Rahimi K. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet 2016; 387:957–967. [DOI] [PubMed] [Google Scholar]
- 10. Neal B, MacMahon S, Chapman N; Blood Pressure Lowering Treatment Trialists’ Collaboration Effects of ACE inhibitors, calcium antagonists, and other blood-pressure-lowering drugs: results of prospectively designed overviews of randomised trials. Blood Pressure Lowering Treatment Trialists’ Collaboration. Lancet 2000; 356:1955–1964. [DOI] [PubMed] [Google Scholar]
- 11. Yoon SS, Gu Q, Nwankwo T, Wright JD, Hong Y, Burt V. Trends in blood pressure among adults with hypertension: United States, 2003 to 2012. Hypertension 2015; 65:54–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Egan BM, Li J, Hutchison FN, Ferdinand KC. Hypertension in the United States, 1999 to 2012: progress toward Healthy People 2020 goals. Circulation 2014; 130:1692–1699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ 2009; 338:b1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Rodeheffer RJ. Hypertension and heart failure: the ALLHAT imperative. Circulation 2011; 124:1803–1805. [DOI] [PubMed] [Google Scholar]
- 15. Zhou M, Daubresse M, Stafford RS, Alexander GC. National trends in the ambulatory treatment of hypertension in the United States, 1997–2012. PLoS ONE 2015; 10:e0119292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. IMS Health. NDTI Diagnosis Reference File, 2000 to 2014. Plymouth Meeting, PA: IMS Health, 2000 to 2014. [Google Scholar]
- 17. Zell ER, McCaig LF, Kupronis BA, Besser RE, Schuchat A. A comparison of the National Disease and Therapeutic Index and the National Ambulatory Medical Care Survey to evaluate antibiotic usage. Proceedings of the section on survey research methods, American Statistical Association Alexandria, VA: American Statistical Association; 2000; 840–845. [Google Scholar]
- 18. Stafford RS, Radley DC. National trends in ambulatory asthma treatment, 1997–2009. J Gen Intern Med 2011; 26:1465–1470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Stafford R, Radley D. The underutilization of cardiac medications of proven benefit, 1990 to 2002. J Am Coll Cardiol 2003; 41:56–61. [DOI] [PubMed] [Google Scholar]
- 20. Kirley K, Qato DM, Kornfield R, Stafford RS, Alexander GC. National trends in oral anticoagulant use in the United States, 2007 to 2011. Circ Cardiovasc Qual Outcomes 2012; 5:615–621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. IMS Health Incorporated. National Disease and Therapeutic Index. Plymouth Meeting, PA: IMS Health Incorporated, 2004. [Google Scholar]
- 22. Beckman KD. How to document and code for hypertensive diseases in ICD-10. Fam Pract Manag 2014; 21:5–9. [PubMed] [Google Scholar]
- 23. ICD-9-CM Official Guidelines for Coding and Reporting. Baltimore, MD: Centers for Medicare & Medicaid Services and National Center for Health Statistics. <https://www.cdc.gov/nchs/data/icd/icd9cm_guidelines_2011.pdf> 2011. Accessed 21 September 2016 [Google Scholar]
- 24. Ashman JJ, Rui P, Schappert SM. Age Differences in Visits to Office-Based Physicians by Adults With Hypertension: United States, 2013. NCHS Data Brief, No 263. Hyattsville, MD: National Center for Health Statistics, 2016. [PubMed] [Google Scholar]
- 25. Garrison GM, Oberhelman S. Screening for hypertension annually compared with current practice. Ann Fam Med 2013; 11:116–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Drugs@FDA: FDA Approved Drug Products. Drugs@FDA: FDA Approved Drug Products <http://www.accessdata.fda.gov/scripts/cder/drugsatfda/index.cfm> 2016. Accessed 21 September 2016.
- 27. U.S Department of Health and Human Services—Administration for Community Living. U.S. Population Totals by Age Group and Sex in the 2010 and 2000 Censuses. U.S. Administration on Aging, 2010. [Google Scholar]
- 28. US Census Bureau. United States 2010 Census <https://www.census.gov/2010census/about> 2011. Washington, DC. Accessed 20 October 2016.
- 29. Chang TI, Evans G, Cheung AK, Cushman WC, Diamond MJ, Dwyer JP, Huan Y, Kitzman D, Kostis JB, Oparil S, Rastogi A, Roumie CL, Sahay R, Stafford RS, Taylor AA, Wright JT, Jr, Chertow GM; SPRINT Study Research Group Patterns and correlates of baseline thiazide-type diuretic prescription in the Systolic Blood Pressure Intervention Trial. Hypertension 2016; 67:550–555. [DOI] [PMC free article] [PubMed] [Google Scholar]