ABSTRACT
Background
Mexico's Prospera-Oportunidades-Progresa Conditional Cash Transfer Program (CCT-POP) included the distribution of fortified food supplements (FFS) for pregnant and lactating women and young children. Rigorous evaluations showed significant impacts on nutrition outcomes but also substantial gaps in addressing nutrition problems.
Objectives
To highlight the program design-related and implementation-related gaps and challenges that motivated further research and the eventual design and roll-out of a modified nutrition component for CCT-POP.
Methods
We used a program impact pathway approach to highlight the extent and quality of implementation of CCT-POP, and its impact on nutrition outcomes. We drew on previously published and new primary data, organized into 3 sources: impact evaluations, studies to inform reformulation of the FFS, and a longitudinal follow-up study using qualitative and quantitative methods to document FFS use and the dietary intake of women and children.
Results
Despite positive impacts, a high prevalence of malnutrition persisted in the population. Coverage and use of health services improved, but quality of care was lacking. Consumption of FFS among lactating women was irregular. Micronutrient intake improved among children who consumed FFS, but the pattern of use limited frequency and quantity consumed. Substantial diversity in the prevalence of undernutrition was documented, as was an increased risk of overweight and obesity among women.
Conclusions
Three key design and implementation challenges were identified. FFS, although well accepted for children, had limited potential to substantially modify the quality of children's diets because of the pattern of use in the home. The communications strategy was ineffective and ill-suited to its objective of motivating FFS use. Finally, the program with its common design across all regions of Mexico was not well adapted to the special needs of some subgroups, particularly indigenous populations. The studies reviewed in this paper motivated additional research and the eventual redesign of the nutrition component.
Keywords: fortified food supplements, dietary intake, pregnant and lactating women, infant and young child, program impact pathway, program impact
Introduction
Mexico's conditional cash transfer (CCT) program, initially named Progresa, later Oportunidades, then Prospera (referred to here as CCT-POP), began at pilot scale in 1997 in rural areas and was extended to urban areas in 2002. The program was 1 of the first CCTs (1) and has undergone rigorous impact evaluations for 20 y. The common features of all CCTs include targeting to low income subgroups and provision of cash on the condition of compliance with some type of conditionality. Most programs include conditionalities related to participation in preventive healthcare services, and incentives to send and keep children in school, but substantial variability in the specifics of those conditionalities exists among programs (1).
Several reviews of the impact of CCT programs on nutrition, health, and child development outcomes have been published (2–6). Authors have concluded that CCTs have a consistent positive impact on child anthropometry (height indicators), but mixed impact on other nutrition outcomes (6). The pathways by which these impacts have been achieved have been compared across several programs, with consistent positive results on the underlying determinants of malnutrition (e.g., poverty reduction, health service use, among others). However, information to assess the full pathway from underlying determinants to direct determinants (i.e., dietary intake and infectious disease) and ultimately improved child nutrition outcomes has been limited by a lack of data in several programs (6). Diversity among programs including the actual package of interventions implemented, and the extent to which conditionalities are enforced limits the utility of such reviews to inform CCT design. Such differences may substantially modify the potential for nutritional impacts, an aspect that has as yet been inadequately illustrated. For example, CCT-POP is 1 of the few programs that include distribution of fortified food supplements (FFS), Nutrivida for pregnant and lactating women (PLW), and Nutrisano for infants and young children (IYC).
As evaluators, we were continually asked by CCT-POP implementers whether the nutritional impacts were “sufficient” given program design and investment, and large enough to contribute to the achievement of the program's long-term goal, i.e., improved human capital. Nutritional supplements similar to Nutrivida and Nutrisano have resulted in improved growth of close to 3 cm in the short term under controlled field conditions (7), but this reference provides little basis for target setting in a complex program such as CCT-POP. This dialogue led to a series of analyses of the evaluation data and several complementary studies to explore in depth the quality of CCT-POP implementation and the adequacy of design for the context in various subgroups of the population, and to measure results for intermediate steps across the pathway to nutritional impacts. These studies sought to understand how impacts were achieved, identify the design and implementation factors that may limit greater impact, and to inform options to strengthen design and implementation. In this paper we provide an overview of the findings of these many studies, organized around the program's original intended impact pathway for nutrition. As part of this supplement, our specific objective is to highlight the program design-related and implementation-related gaps and challenges that motivated further research (8, 9) and the eventual design and roll-out of a modified nutrition component for CCT-POP (10, 11).
Methods
The impact pathway used for this analysis focuses on those aspects of the CCT-POP with potential to improve dietary intake among pregnant and lactating women and infants and young children, drawing on the known determinants of malnutrition (12). Evidence for progress across the pathway from published sources was identified through thorough search of program documents, reports, published and unpublished studies through the CCT-POP website, Pubmed, and National Institute of Public Health of Mexico (INSP) files.
For studies with primary data collection, the study protocols were reviewed and approved by the Biosecurity, Research, and Ethics Commissions of the INSP before commencement. Study participants for each were randomly selected from beneficiary lists maintained by the local primary health centers. For all studies, participation was entirely voluntary. The field teams were clearly identified as INSP staff without affiliation to the program to ensure that program beneficiaries did not feel compelled to participate if they did not desire to do so. All potential participants were provided with details of the study's objectives, procedures, risks, and benefits, and if in agreement, were asked to provide written consent.
Evidence was organized into 3 main data sources (Table 1) (13–21).
TABLE 1.
Overview of studies from which data have been used to analyze diverse objectives relevant for the impact pathway analysis of the CCT-POP in Mexico1
| Study short name | Primary objective | Design. Main statistical analyses used | Region | Year(s) | References |
|---|---|---|---|---|---|
| Data source 1: Impact evaluation studies | |||||
| Impact evaluation (rural) | Evaluate the impact of the program in rural areas on nutrition, health, education, poverty, and related outcomes | REE, then follow-up (repeat cross-sectional studies). Propensity score matching | Rural | REE: 1997, 2002 Follow-up: 2004, 2007 | (13) |
| Nutrition impact evaluation (rural) | Evaluate the impact of the program on growth and anemia in children in rural areas | REE (cohort). Random-intercept linear model and generalized estimating equations | Rural | 1999, 2000 | (14) |
| Impact evaluation (urban) | Evaluate the impact of the program in urban areas on nutrition, health, education, poverty, and related outcomes | Quasi-experimental effectiveness evaluation. Propensity score matching | Urban | 2002, 2003, 2004, 2006 | (13, 15) |
| Data source 2: Supplement reformulation studies | |||||
| Iron bioavailability | Compare the bioavailability of 3 forms of iron in the Nutrisano fortified complementary food | Randomized trial of bioavailability using isotopes. Correlations; chi-square and Student's t test | Laboratory | 2000 | (16) |
| Sensory evaluation | Compare the sensory properties of Nutrisano fortified complementary food with 3 forms of iron | Blind assessment with sensory experts. Chi-square test and analyses with logistic regression models | Laboratory | 2000 | (17) |
| Efficacy of the Nutrisano vs. syrup | Evaluate the effect of the Nutrisano fortified complementary food vs. syrup on iron status | Randomized efficacy trial. Chi-square, Student's t and Kruskal-Wallis tests | Small urban areas | 2000−2002 | (18) |
| Data source 3: Supplement acceptance, consumption, and dietary intake studies | |||||
| Supplement and dietary intake | Evaluate dietary intake and use and consume of the fortified supplements in children and women | Cohort of women and children. Repeated measures test using mixed models | Urban | 2003−2004 | (19) |
| Acceptance, facilitators, and barriers of supplement use | Determine and explore the sociocultural factors that facilitate or hinder the recommended intake of the nutritional supplement | Qualitative study. Framework analyses approach | Rural | 2002, 2003−2004 | (20) |
| Maternal knowledge and use of a supplement | Evaluate the efficacy of a behavioral change through communication intervention to improve supplement use | Efficacy study. Double-difference | Rural and urban | 2006 | (21) |
CCT-POP, Progresa-Oportunidades-Prospera Conditional Cash Transfer Program; REE, randomized effectiveness evaluation.
Impact evaluation studies
Impact evaluations were carried out in rural [randomized effectiveness trial with cross-sectional panels (13, 14)] and urban areas [quasi-experimental study with cross-sectional panels (15)]. Data collection was comprehensive and covered many topics. For this review we focused on impact for nutrition outcomes including intermediate outcomes, any information available related to Nutrivida/Nutrisano, and updates of the magnitude and distribution of nutrition issues in the population. We accessed results published in peer-reviewed journals and detailed reports publicly available on the CCT-POP site.
Studies with specific objective to inform reformulation of Nutrivida/Nutrisano
Nutrivida and Nutrisano are powdered milk-based products distributed monthly (or every second month, depending on the health center) by health staff. Women received Nutrivida from the first antenatal visit until 1 y postpartum and were instructed to consume it once daily as a beverage. Nutrisano is a porridge (papilla in Spanish) targeted at all children aged 4 mo to 23 mo and children aged 2−4 y identified during routine health visits as having low weight-for-age (this was modified in 2006 to target children aged 6 mo to 59 mo). Both products were developed in Mexico and fortified with age-appropriate and physiological status-appropriate amounts to contribute close to 100% of recommended daily intakes (22) of iron, zinc, folic acid, vitamin C, vitamin E, vitamin B-12, vitamin A (children only), and iodine (women only), as well as ∼20% of mean estimated energy requirements.
The small impact on anemia prevalence among IYC observed in the original rural impact evaluation (23) motivated a series of studies to determine whether the iron type and content should be modified. Three studies were carried out, 2 of which have been previously published (16, 17). The third study was a randomized efficacy trial to evaluate the impact of consumption of Nutrisano on children's iron status using micronutrient syrup as a reference (18). The trial was conducted in a small urban community in Puebla, Mexico in 2000. At that time, the program provided Nutrisano as of age 4 mo. Children aged 4−12 mo at baseline (the beneficiaries of the program) were recruited through the primary health centers. Parents of children were invited to participate, and written consent was sought. The study was not registered in a trial registry as this was not required by INSP at that time.
Individual children were randomly assigned using random number tables to receive Nutrisano or a micronutrient syrup containing iron in the form of ferrous sulfate. The syrup was available as an essential medical product in the health centers. Nutrisano was provided daily (6 d/wk) by project staff for 4 mo. Hemoglobin concentration was assessed in a venous blood sample using Hemocue. Serum ferritin and C-reactive protein were measured by nephelometry (Behring Nephelometer B-N 100 Analyzer) in samples collected at baseline and endline in the INSP laboratory in Cuernavaca, Mexico.
The results of this study and the analysis of the evaluation data raised several questions as to the acceptance and pattern of utilization of Nutrivida and Nutrisano, which motivated several additional studies.
Studies assessing Nutrivida/Nutrisano acceptance, consumption, and dietary intake
From July 2003 to May 2004 we recruited a cohort of lactating women and their infants and young children to assess dietary intake, and knowledge, acceptance, and use of Nutrivida and Nutrisano (19). Children aged 6−23 mo at baseline and their breastfeeding mothers (the beneficiaries of CCT-POP) were identified with support from health centers. Although Nutrivida was also provided to pregnant women and consumption patterns may differ during pregnancy, we chose to follow lactating women only for logistic reasons (i.e., mother/child pairs). A subset of 22 communities that had previously participated in the urban impact evaluation (13 intervention and 9 control) were randomly selected to be part of the follow-up. Data were collected approximately every 3 mo and included a single 24-h recall for each woman and child, and a detailed questionnaire of supplement use, preparation, and consumption pattern (i.e., 4 data points per child/women over a 12-mo period). Note that the population does not rely on subsistence farming and we did not anticipate major seasonal variation in the pattern of dietary intake with the exception of highly seasonable fruits such as mango. Height, weight, and hemoglobin concentration were measured at baseline and at 12-mo follow-up.
Total nutrient intake from home diet and Nutrivida/Nutrisano was assessed from 24-h recall data at each time point and averaged over the 4 measurements. Potential displacement of home diet with Nutrivida/Nutrisano consumption was assessed by comparing intake in intervention and control communities. We used the supplement consumption data to describe preparation and use pattern and intra-household sharing.
Additional studies during the same period used qualitative research methodologies to explore use and acceptance of the nutritional supplements (20, 21) and ethnographic research to gain insights into the social-cultural and other factors that might facilitate or impede use of the program generally, and the supplements specifically.
Results
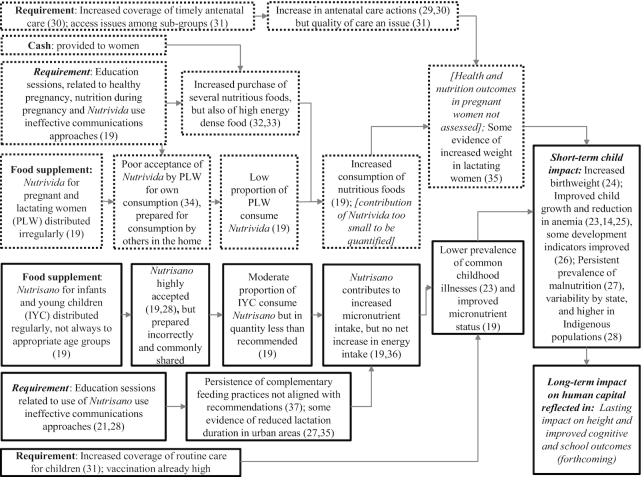
Results of the review are organized into 3 sections. First, we present a brief overview of what is known about the impact of CCT-POP on nutrition-related outcomes in women and infants and young children. We then present results across the intended impact pathway of the program as it was originally designed in 1997. The program sought to improve nutrition outcomes through actions directed to pregnant and lactating women (dotted lines in Figure 1), and to infants and young children (solid lines) (19, 21, 23–37). The arrows in Figure 1 show the intended pathway to impact and the content of each box provides a summary of what was learned through the impact evaluations and the studies described in Table 1.
FIGURE 1.
Overview of implementation and impact of the Progresa-Oportunidades-Prospera Conditional Cash Transfer Program (CCT-POP) in Mexico, using the impact pathway of its original design (1997). IYC, infants and young children; PLW, pregnant and lactating women.
Brief overview of the nutrition-related impact of CCT-POP
In the long term, the CCT-POP seeks to increase human capital among low-income families through improving health, nutrition, and education outcomes. Forthcoming evaluations will provide evidence of impacts of CCT-POP on adult height, and several education and cognition indicators after 20 y of implementation (study forthcoming: World Bank).
Several short-term impacts were assessed as part of evaluations in rural and urban areas. In rural areas, recall of birth weight was assessed among a single cross-sectional sample of women aged 15–49 y with a singleton live birth between 1997 and 2003. Program participation was associated with a 127.3 g higher birth weight (P = 0.02) and a 4.6% lower prevalence of low birth weight (P = 0.05) (24). Positive impacts in the short and medium term on nutritional status of children, particularly child growth and to a lesser extent anemia have been well documented (14, 25), as has impact on health status (23, 38), and for some indicators of child development (26).
The evaluation results illustrated that while the program used similar economic targeting criteria to identify beneficiary families in all regions of the country, the prevalence of undernutrition was substantially higher in rural than in urban areas (27) and among indigenous populations (28). For example, in rural areas only, the prevalence of stunting in the CCT-POP evaluation ranged from 17% to 38% across various states (28). This finding raised questions as to whether a single program design for the nutrition component was appropriate.
Improving pregnancy and lactation outcomes through better care and dietary intake
The program sought to achieve improved pregnancy and lactation outcomes (dotted lines in Figure 1) by improving women's health and nutrition during pregnancy and lactation. Timely and continual antenatal care was included as a conditionality required for continued receipt of program benefits. Cash provided to the female head of household was intended to empower women and lead to increased food purchase (6). Nutrivida was developed to fill dietary gaps of key micronutrients required during pregnancy. Messages related to both health and dietary intake, including the use of Nutrivida were delivered through education sessions, participation in which was part of the program requirements.
During the first years of implementation there were significant increases in the coverage of antenatal care among beneficiary pregnant women (e.g., 6% increase in 2000) (29, 31). The program successfully improved the timeliness and frequency of antenatal care, with a 16.7% increase in antenatal care during the first trimester, and 4.1% increase in the number of visits attended per woman (30). The quality of antenatal care, however, remains a challenge in the primary healthcare system (31), as does access for some women, particularly indigenous women (39). While participation in antenatal care is close to universal, in 2006 only 37.1% of pregnant or lactating women reported having received Nutrivida, slightly higher in rural (41.4%) than urban (28.6%) areas (40). Given the periodic and cross-sectional design of the impact evaluation surveys, there are insufficient data to assess the extent to which any improvement of pregnancy outcome was mediated through improved dietary intake during pregnancy and/or antenatal care. Some data are available, however, on food purchase and consumption. As intended by the program, the cash transfers increased household consumption (i.e., purchase) of total calories, and of several nutritious foods including fruits, vegetables, and animal-source foods (32). Evidence suggests that this did translate into increased consumption of these foods by PLW after 1 and 2 y of CCT-POP participation (33, 41), but full details of dietary patterns of women were not available.
This lack of information was part of the motivation for the detailed dietary studies (data source 3 in Table 1). Over the year-long follow-up period, we found that only 25% of lactating women reported consuming Nutrivida, of whom ∼60% prepared it according to recommendations (19). We did not go on to quantify nutrient intake from Nutrivida because of the very low reported quantities consumed. In a more in-depth study using qualitative research methods, women reported low acceptance of Nutrivida for their own consumption (34). Several reasons were reported including dislike of its texture, odor, and/or flavor, monotony of daily consumption, and concerns related to the time required for its preparation.
The prevalence of low weight among women was very low (<2%) and the prevalence of overweight and obesity high in all studies and all subgroups of the beneficiary population (19, 27, 28). For example, at the end of the year-long follow-up of beneficiary lactating women, the prevalence of overweight was 39.6% and obesity 24.3%, ∼3 percentage points higher than baseline (35). We therefore concluded that the diets of PLW were low in micronutrients but adequate or high in energy.
Improving child outcomes through better care, dietary practices, and intake
For IYC, the program sought to reduce childhood illness through prevention of malnutrition and early detection and treatment of illness (solid lines in Figure 1). Health was promoted through routine health care including vaccinations and through the health talks (a program requirement). The free provision of Nutrisano during those health visits, accompanied by talks related to its use were intended to improve dietary intake among infants and young children. As expected by the CCT-POP requirements, beneficiary women brought their children to routine health care appointments more often than their counterparts without the CCT-POP, translating into 25% lower prevalence of common childhood illness during the first 6 mo of life (23).
Despite the increased household-level consumption of several nutritious foods (32), the results demonstrated no change in dietary intake from home diet among beneficiary children aged 6−59 mo in rural areas of Mexico (42). In the rural impact evaluation sample, children who consumed Nutrisano had higher total dietary intakes of energy, iron, zinc, and vitamin A than nonconsumers (36). In an additional study in southern Mexico (19), over 90% of no longer breastfed children who consumed Nutrisano had adequate iron, zinc, vitamin A, and vitamin C intakes. In comparison, for no longer breastfed children who did not consume Nutrisano, only 44% had adequate iron intakes and 87% adequate intakes of vitamin A. This study and the year-long supplement consumption study in urban areas found that Nutrisano contributed to dietary adequacy of iron, zinc, and vitamins A and C but no net increase in energy intake (19).
Despite these findings, program evaluations revealed minimal impact on anemia (14, 25), and a persistently high prevalence of micronutrient deficiency (19). Both Nutrisano and Nutrivida were originally produced using reduced iron as fortificant and experts questioned the bioavailability of this iron form (43). The studies confirmed that the bioavailability of reduced iron was low, and that ferrous gluconate and ferrous sulfate provided substantially higher bioavailability (44). A technical report from the efficacy study described in Table 1 (18) showed that Nutrisano fortified with reduced iron had no impact on iron status or anemia after 4 mo follow-up compared with micronutrient syrup (Table 2). In parallel, studies confirmed that both ferrous sulfate and reduced iron resulted in greater changes to organoleptic properties of the foods than ferrous gluconate (45), which then replaced reduced iron as a fortificant.
TABLE 2.
Iron status, anemia, and iron deficiency in children aged 4−12 mo at baseline and 4 mo after supplementation, by study group1
| Study group | ||
|---|---|---|
| Fortified complementary food (Nutrisano) | Multiple micronutrient syrup | |
| Variables | (n = 98) | (n = 100) |
| Baseline | ||
| Hemoglobin, g/dL | 11.7 ± 1.2 | 11.8 ± 1.3 |
| Serum ferritin, ng/mL | 17.1 (9.7, 45.2) | 26.0 (13.2, 32.3) |
| Anemia,2 % | 26.7 | 17.0 |
| Iron deficiency,3 % | 28.1 | 25.0 |
| 4 mo | ||
| Hemoglobin, g/dL | 11.6 ± 1.3 | 11.8 ± 1.3 |
| Serum ferritin, ng/mL | 14.2 (8.5, 23.9) | 24.1 (16.9, 43.6)4 |
| Anemia, % | 29.2 | 17.6 |
| Iron deficiency, % | 37.7 | 12.54 |
Values are means ± SDs, medians (IQR), or prevalence (%).
Anemia defined as hemoglobin concentration < 11.0 g/dL.
Iron deficiency defined as serum ferritin < 12 ng/dL.
Significantly different (P < 0.01) than Nutrisano.
Despite high acceptance, coverage of Nutrisano was moderate. The proportion of children aged 6−24 mo who reported consuming Nutrisano regularly (≥4 times/wk) was 50% in rural areas and 33% in urban areas (19, 28). Even among those who did consume Nutrisano, the mean amount consumed during the longitudinal study across all ages was ∼20 g, just less than half the recommended daily dose of 44 g (28).
As part of that study we found that Nutrisano was consistently shared with other household members, mostly other children. On average, 2.5 family members consumed the Nutrisano that had been targeted to a single child aged 6−23 mo. Nutrisano in both rural and urban areas was commonly prepared as a beverage rather than a porridge, facilitating sharing but limiting nutrient density. The education component had only 1 session related to Nutrisano (and Nutrivida together). The qualitative and ethnographic studies (20, 21) concluded that this was insufficient to educate and motivate women to use the products appropriately. The session format was not conducive to learning, with women often standing for extended times in the heat/sun. Education was done in Spanish even in the predominantly indigenous communities where women may have limited Spanish fluency. Finally, the qualitative research illustrated that knowledge was often not the barrier to consumption. For example, women in rural and urban areas across all studies reported understanding well that Nutrisano was intended for a specific child. They did not, however, agree with this principle and shared with all children (19).
The impact evaluations also illustrated some potential concerns for child feeding. Breastfeeding initiation was very high (almost 95%) both in urban and in rural areas (27, 35), and no change was detected in the urban evaluation (not assessed in rural evaluations) (27). In urban areas, however, beneficiary women had shorter total breastfeeding duration (mean 14.0 mo) than women in the comparison communities (mean 16.3 mo) (27). We also found that the recommendation to begin distribution of Nutrisano at 6 rather than 4 mo was not fully embraced and implemented by some medical staff (21). Similarly, many medical staff prioritized distribution of Nutrisano to children with low weight regardless of age range (21).
Discussion
CCT-POP had positive impacts on child health and nutrition outcomes, 1 of the many factors that contributed to its continuity over 20 y (46). Generally, the program was well designed to influence the primary causes of childhood undernutrition – health and dietary intake (8). Coverage of antenatal and young childcare increased significantly. Nutrivida and Nutrisano were designed to address nutritional deficiencies in the population, and the health education component sought to increase knowledge and improve practices related to their use in addition to several health topics. The cash transfer enabled families to purchase more nutritious foods. Some program quality issues were identified and addressed early on and have been reported previously. For example, the reformulation of Nutrisano and Nutrivida with a more bioavailable form of iron and increased vitamin C content to favor iron absorption was adopted and implemented in 2005 after the results of the studies presented here (47). The age to begin distribution of Nutrisano was modified from 4 to 6 mo to avoid interference with breastfeeding and to ensure clear and consistent messages related to the recommended duration of exclusive breastfeeding (37, 47).
Through this review of the program impact pathway, however, we highlight several gaps in the appropriateness of design for subsets of the beneficiary population, and in the quality of implementation. First, Nutrivida and Nutrisano are high-quality products, well accepted by the population, with minimal distribution challenges in the case of children at least. Their use, however, was not aligned with recommendations, likely because of several factors including inadequate promotion, which relates directly to the second challenge, poor quality design and implementation of the communications component. Group sessions convened monthly covered many topics (25 in total), leaving little opportunity to cover any in detail (only 1 addressed Nutrisano and Nutrivida). Didactic methodology and physical location did not favor knowledge transfer and methods did not foster skills development and motivation. Finally, the CCT-POP beneficiary population is diverse, with substantial variability in the magnitude and severity of nutritional issues by geographic region and ethnic group. The identification of these gaps triggered several studies to inform potential alternatives to Nutrivida and Nutrisano, opportunities and approach to strengthen the communications component, and to improve understanding of sociocultural factors that may influence program acceptance and use.
At the time these studies were conducted (early 2000s) there was a growing body of evidence that micronutrient powders could provide an equally efficacious alternative to iron or micronutrient syrups to reduce anemia in children (48, 49), but there was no evidence on whether they were likely to have effects on functional outcomes such as child growth and development. We recommended a randomized trial to compare the impact of 2 alternatives to Nutrivida (micronutrient tablets and micronutrient powders) and Nutrisano (micronutrient syrup and micronutrient powders) on several nutrition outcomes among women and children, respectively (9).
The program requirements motivated more and timely health service use, creating opportunities for regular contact between the providers and program beneficiaries. The importance of health workers’ knowledge and communications skills for effective nutrition behavior change is well recognized (50). In CCT-POP, the central role of the healthcare professionals for implementation of the communications component was underappreciated in the initial design. Minimal training was provided for health professionals to deliver the program, and issues with quality of care were well documented (31). Bonvecchio et al. (10) report on several additional studies to explore programmatically feasible approaches to education that could meet the information and skill development needs of the beneficiary population.
Finally, the studies highlighted substantial diversity in the prevalence of malnutrition and in child feeding and related practices between rural and urban areas, and among indigenous and nonindigenous populations. The importance of context for the design of effective nutrition programs is well recognized (51). The design of a single approach has many advantages for ease of implementation in a program the size and complexity of CCT-POP. Yet in doing so, specific contextual factors that may impede program acceptance and use may not be adequately addressed. Theodore et al. will present results of several studies designed specifically to address this issue in CCT-POP (8).
Acknowledgments
The authors’ responsibilities were as follows—LMN: conceptualized the paper, developed the Program Impact Pathway; AB, FM-R, and RG-F: led data collection and in collaboration with JR-D interpreted many of the included studies and collaborated on the manuscript; AB, AG-G, and ACF-G: provided inputs for the Program Impact Pathway; AG-G, ACF-G, and LMN: wrote the manuscript and had primary responsibility for the final content; AB: gave key insights for the final manuscript; and all authors: read and approved the final manuscript.
Notes
Funds for the research reported here were provided by the National Coordination of the Progresa-Oportunidades-Prospera (now called Prospera Programa de Inclusión Social), Secretary of Social Development, Government of Mexico, Mexico City.
Author disclosures: AG-G, LMN, AB, ACF-G, FM-R, RG-F, and JR-D are all employed by INSP or GAIN, which provided funds to co-sponsor this supplement.
INSP, National Institute of Public Health of Mexico.
Publication costs for this supplement were defrayed in part by the payment of page charges. This article appears as part of the supplement “Implementation research for improvement of nutrition actions in an at-scale social protection program in Mexico,” sponsored by the National Institute of Public Health, Mexico (INSP), and the Global Alliance for Improved Nutrition (GAIN). The guest editors of the supplement, Lynnette M Neufeld and Anabelle Bonvecchio Arenas, have the following conflicts of interest: LMN is employed by GAIN, ABA is employed by INSP. The opinions expressed in this publication are those of the authors and are not attributable to the sponsors or the publisher, Editor, or Editorial Board of The Journal of Nutrition.
Abbreviations used: CCT-POP, Progresa-Oportunidades-Prospera Conditional Cash Transfer Program; FFS, fortified food supplement(s); INSP, National Institute of Public Health of Mexico; IYC, infants and young children; PLW, pregnant and lactating women.
References
- 1. Adato M, Hoddinott J. Conditional cash transfers in Latin America. International Food Policy Research Institute. Washington (DC): The Johns Hopkins University Press; 2010. Available from: http://www.ifpri.org/publication/conditional-cash-transfers-latin-america (Accessed April 24, 2019). [Google Scholar]
- 2. Segura-Pérez S, Grajeda R, Pérez-Escamilla R. Conditional cash transfer programs and the health and nutrition of Latin American children. Rev Panam Salud Publica. 2016;40(2):124–37. [PubMed] [Google Scholar]
- 3. de Walque D, Fernald L, Gertler P, Hidrobo M. Cash Transfers and Child and Adolescent Development. In: Bundy DAP, de Silva N, Horton S, Jamison DT, Patton GC, editors. Child and Adolescent Health and Development. 3rd edition Washington (DC): The International Bank for Reconstruction and Development / The World Bank, 2017, Chapter 23. [PubMed] [Google Scholar]
- 4. Mason JB, Saldanha LS, Ramakrishnan U, Lowe A, Noznesky EA, Girard AW, McFarland DA, Martorell R. Opportunities for improving maternal nutrition and birth outcomes: synthesis of country experiences. Food Nutr Bull. 2012;33(2 Suppl):S104–37. [DOI] [PubMed] [Google Scholar]
- 5. Owusu-Addo E, Cross R. The impact of conditional cash transfers on child health in low- and middle-income countries: a systematic review. Int J Public Health. 2014;59(4):609–18. [DOI] [PubMed] [Google Scholar]
- 6. Leroy JL, Ruel MT, Verhofstadt E. The impact of conditional cash transfer programmes on child nutrition: A review of evidence using a programme theory framework. J Dev Effect. 2009;1(2):103–29. [Google Scholar]
- 7. Habicht JP, Martorell R, Rivera FA. Nutritional impact of supplementation in the INCAP longitudinal study: analytic strategies and inferences. J Nutr. 1995;125(4 Suppl):1042S–50S. [DOI] [PubMed] [Google Scholar]
- 8. Theodore F, Bonvecchio A, García-Guerra A, Blanco-García I, Alvarado R, Rawlinson CJ, Neufeld LM, Pelto GH. Sociocultural influences on poor nutrition and program utilization of Mexico's conditional cash transfer program. J Nutr. 2019;149(Supplement_1):2290S–2301S. [DOI] [PubMed] [Google Scholar]
- 9. Neufeld ML, García-Guerra A, Quezada AD, Théodore F, Bonvecchio A, Domínguez Islas C, Garcia-Feregrino R, Hernandez A, Colchero A, Habicht JP. A fortified food can be replaced by micronutrient supplements for distribution in a Mexican social protection program based on results of a cluster randomized trial and costing analyses. J Nutr. 2019;149(Supplement_1):2302S–9S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bonvecchio A, González W, Théodore F, Lozada AL, Garcia-Guerra A, Alvarado R, Fernández-Gaxiola AC, Rawlinson CJ, Villa de la Vega A, Neufeld LM. Translating evidence-based program recommendations into action. The design, testing and scaling up of the behavior change strategy EsIAN in Mexico J Nutr. 2019;149(Supplement_1):2310S–22S. [DOI] [PubMed] [Google Scholar]
- 11. González W, Bonvecchio A, García-Guerra A, Vilar-Compte M, Villa de la Vega A, Quezada L, Rosas C, Lozada-Tequeanes AL, Hernández A. An iterative process for training design and implementation improved healthworkers knowledge for taking nutrition behavior change to scale. J Nutr. 2019;149(Supplement_1):2323S–31S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. United Nations Children Fund (UNICEF). Malnutrition: causes, consequences and solutions. The state of the world children 1998. UNICEF. Oxford University Press; 1998. [Google Scholar]
- 13. Instituto Nacional de Salud Pública. Nota técnica sobre el diseño muestral para la Encuesta de Evaluación Rural (ENCEL) 2007 [Technical note on the sampling design of the Rural Evaluation Survey (ENCEL) 2007]. Evaluación Externa del Programa de Desarrollo Humano Oportunidades 2007–2008. Centro de Investigación en Evaluación y Encuestas. Cuernavaca, México, 2007. Available from: https://evaluacion.prospera.gob.mx/es/wersd53465sdg1/eval_cuant/nota_tecnica_rur_muestra_final_2008.pdf (Accessed April 24, 2019). [Google Scholar]
- 14. Rivera JA, Sotres-Alvarez D, Habicht JP, Shamah T, Villalpando S. Impact of the Mexican program for education, health and nutrition (Progresa) on rates of growth and anemia in infants and young children: a randomized effectiveness study. JAMA. 2004;291:2563–70. [DOI] [PubMed] [Google Scholar]
- 15. Behrman JR, Todd PE, Hernández B, Urquieta J, Atanasio O, Angelucci M, Hernández M. Metodología de Evaluación de Oportunidades en Zonas Urbanas 2002–2004 y Rurales 1997–2003 [Methodology of the evaluation of Oportunidades in rural áreas 2002–2004 and rural areas 1997-2003]. In: Hernández-Padro B, Hernández-Ávilia M, Urquieta-Salomón JEeditors. Evaluación Externa del Programa de Desarrollo Humano Oportunidades 2006. Cuernavaca, México: Centro de Investigación en Evaluación y Encuestas; 2006Available from: https://evaluacion.prospera.gob.mx/es/wersd53465sdg1/docs/2006/insp_2006_tomo_iii_metodologico.pdf (Accessed April 24, 2019). [Google Scholar]
- 16. Pérez-Expósito AB, Villalpando S, Rivera JA, Griffin IJ, Abrams SA. Ferrous sulfate is more bioavailable among preschoolers than other forms of iron in a milk-based weaning food distributed by PROGRESA, a national program in Mexico. J Nutr. 2005;135(1):64–9. [DOI] [PubMed] [Google Scholar]
- 17. Morales J, Vargas F, Cassís L, Sánchez E, Villalpando S. Sensorial evaluation of nutritional supplements (PROGRESA) enriched with 3 different forms of iron in a rural Mexican community. J Food Sci. 2008;73(1):S1–S5. [DOI] [PubMed] [Google Scholar]
- 18. Neufeld ML, Rivera Dommarco J, Villalpando Hernández S, Shamah Levy T. The efficacy of the Progresa supplement and a multiple micronutrient supplement to improve nutritional status in Mexican women and infant. National Institute of Public Health, Cuernavaca, Morelos, Mexico, 2003, Available from: http://catalogoinsp.mx/files/tes/Doc2.pdf (Accessed April 23, 2019). [Google Scholar]
- 19. Neufeld LM, Sotres Alvarez D, Flores López M, Tolentino Mayo L, Jiménez Ruiz J, Rivera Dommarco J. Estudio sobre el consumo de los suplementos alimenticios Nutrisano y Nutrivida en niños y mujeres de zonas urbanas beneficiarios de Oportunidades [Study on the consumption of food supplements Nutrisano and Nutrivida among children and women beneficiaries of Oportunidades in urban areas]. In: Hernández-Prado B, Hernández-Ávila Meditors. Evaluación externa de impacto del Programa Oportunidades 2004. Tomo III. Alimentación. Cuernavaca, México: Instituto Nacional de Salud Pública, 2004, pp. 119–47.. Available from: https://evaluacion.prospera.gob.mx/es/wersd53465sdg1/docs/2004/insp_ciesas_2004_tomo_iii.pdf (Accessed April 23, 2019). [Google Scholar]
- 20. Escalante-Izeta E, Bonvecchio A, Théodore F, Nava F, Villanueva MA, Rivera-Dommarco JA. Facilitadores y barreras para el consumo del complemento alimentacio del Programa Oportunidades. Salud Publica Mex. 2008;50(4):316–24. [DOI] [PubMed] [Google Scholar]
- 21. Bonvecchio A, Pelto GH, Escalante E, Monterrubio E, Habicht JP, Nava F, Villanueva MA, Safdie M, Rivera JA. Maternal knowledge and use of a micronutrient supplement was improved with a programmatically feasible intervention in Mexico. J Nutr. 2007;137:440–6. [DOI] [PubMed] [Google Scholar]
- 22. Rosado JL, Rivera J, López G, Solano L. Development, production, and quality control of nutritional supplements for a national supplementation program in Mexico. Food Nutr Bull. 2000;21:30–4. [Google Scholar]
- 23. Gertler P. Do conditional cash transfers improve child health? Evidence from PROGRESA's control randomized experiment. Am Econ Rev. 2004;94(2):336–41. [DOI] [PubMed] [Google Scholar]
- 24. Barber SL, Gertler PJ. The impact of Mexico's conditional cash transfer programme, Oportunidades, on birthweight. Trop Med Int Health. 2008;13(11):1405–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Leroy JL, Garcia-Guerra A, Garcia R, Dominguez C, Rivera J, Neufeld LM. The Oportunidades program increases the linear growth of children enrolled at young ages in urban Mexico. J Nutr. 2008;138:793–8. [DOI] [PubMed] [Google Scholar]
- 26. Gertler P, Fernald L. The medium-term impact of Oportunidades on child development in rural areas. Final Report (Fourth Draft). Available from: https://sarpn.org/documents/d0001264/P1498-Child_dev_terminado_1dic04.pdf (Accessed April 20, 2019). [Google Scholar]
- 27. Neufeld LM, García-Guerra A, Leroy LJ, Flores-López ML, Fernández-Gaxiola AC, Rivera-Dommarco JA. Impacto del Programa Oportunidades en nutrición y alimentación en zonas urbanas de México [Impact of the Oportunidades program on nutrition and dietary intake in urban areas of Mexico]. In: Hernández-Prado B, Hernández-Ávila Meditors. Evaluación externa de impacto del Programa Oportunidades 2006. Tomo II, Alimentación. Cuernavaca, México: Instituto Nacional de Salud Pública, 2006. Available from: https://evaluacion.prospera.gob.mx/es/wersd53465sdg1/docs/2006/insp_2006_tomo_ii_alimentacion.pdf (Accessed April 20, 2019). [Google Scholar]
- 28. Neufeld LM, Mejía F, Fernández-Gaxiola AC, García-Guerra A, Méndez I, Domínguez CP. Diagnóstico situacional del estado nutricio de niños menores de dos años de edad y de sus madres, beneficiarios de Oportunidades en zonas rurales [Situation assessment of the nutritional status of children less than 2 years of age and their mothers, beneficiaries of Oportunidades in rural areas]. In: Bertozzi SM, González de la Rocha Meditors. Evaluación externa del Programa Oportunidades 2008. A diez años de intervención en zonas rurales (1997-2007). Tomo II, El reto de la calidad de los servicios: resultados en salud y nutrición. México, DF: Secretaría de Desarrollo Social, 2008, pp. 347–96.. Available from: https://evaluacion.prospera.gob.mx/es/wersd53465sdg1/docs/2008/2008_tomo_ii_calidad_servicios_salud_nutricion.pdf. (Accessed April 20, 2019). [Google Scholar]
- 29. Huerta MC, Hernández D. Algunos aspectos de la salud reproductiva de la población beneficiaria de Progresa [Some aspects of reproductive health of the beneficiary population of Progresa]. In: Gertler P.editor Evaluación de Resultados del Programa de Educación, Salud y Alimentación Salud 2000. Mexico DF: Evaluación Externa del Programa Progresa, 2000. Available from: https://evaluacion.prospera.gob.mx/es/wersd53465sdg1/docs/2000/ifpri_2000_salud.pdf. (Accessed April 20, 2019). [Google Scholar]
- 30. Orozco M, Soto H. Resultados de la operación de Progresa en la demanda de servicios de salud [Results of the implementation of Progresa in the demand for health services]. Evaluación de Resultados del Programa de Educación, Salud y Alimentación, primeros avances 1999. Mexico DF: Evaluación Externa del Programa Progresa, 1999. Available from: https://evaluacion.prospera.gob.mx/es/wersd53465sdg1/docs/1999/1999_libro_evaluacion.pdf. (Accessed April 20, 2019). [Google Scholar]
- 31. Gutiérrez JP, Leroy J, DeMaria L, Walker D, Campuzano JC, Moreno K, Serván E, Sosa Rubí SG, Bertozzi SM. Evaluación de la calidad de los servicios de atención a la salud asignados a la población beneficiaria de Oportunidades [Evaluation of the quality of attention in health services assigned to the beneficiary population of Oportunidades]. In: Bertozzi SM, González de la Rocha Meditors. Evaluación externa del Programa Oportunidades 2008. A diez años de intervención en zonas rurales (1997-2007). Tomo II, El reto de la calidad de los servicios: resultados en salud y nutrición. México, DF: Secretaría de Desarrollo Social, 2008. Available from: https://evaluacion.prospera.gob.mx/es/wersd53465sdg1/docs/2008/2008_tomo_ii_calidad_servicios_salud_nutricion.pdf (Accessed April 20, 2019). [Google Scholar]
- 32. Hoddinott J, Skoufias E. The impact of PROGRESA on food consumption. FCND Discussion Paper 150 Washington, DC: International Food Policy Research Institute (IFPRI), 2003. Available from: http://siteresources.worldbank.org/EXTLACREGTOPPOVANA/Resources/HoddinottSkoufiasimpactofprogresaonfoodconsumption.pdf. (Accessed April 20, 2019). [DOI] [PubMed] [Google Scholar]
- 33. Angelucci M, Attanasio O, Di Maro V. The impact of Oportunidades on consumption, savings and transfers. University College London, 2011. Available from: http://www.homepages.ucl.ac.uk/∼uctpjrt/Files/Angelucci%20Attanasio%20Di%20Maro%20-%20Oportunidades%20Consumption%20revised.pdf. (Accessed April 20, 2019). [Google Scholar]
- 34. Young S, Blanco I, Hernandez-Cordero S, Pelto G, Neufeld L. Organoleptic properties, ease of use, and perceived health effects are determinants of acceptability of micronutrients supplements among poor Mexican women. J Nutr. 2010;140:605–11. [DOI] [PubMed] [Google Scholar]
- 35. Neufeld ML, García-Guerra A, Fernández-Gaxiola AC, Rivera-Dommarco JA. Impacto de Oportunidades en alimentación y nutrición de niños y mujeres en zonas urbanas [Impact of Oportunidades on nutrition and dietary intake in children and women in urban areas]. In: González-Cossío T, Rivera-Dommarco J, López Acevedo G, Rubio Soto GMeditors. Banco Mundial y Secretaría de Desarrollo Social (SEDESOL), México D.F.: Nutrición y Pobreza, 2008, pp. 82–95. [Google Scholar]
- 36. Ramírez-Silva I, Rivera JA, Leroy JL, Neufeld LM. The Oportunidades program's fortified food supplement, but not improvements in the home diet, Increased the intake of key micronutrients in rural Mexican children aged 12–59 months. J Nutr. 2013;143:656–63. [DOI] [PubMed] [Google Scholar]
- 37. WHO. The optimal duration of exclusive breastfeeding. Report of an expert consultation. Geneva, WHO (document WHO/NHD/01.09, WHO WHO/FCH/CAH/01.24) March 2001. Available from: https://www.who.int/nutrition/publications/infantfeeding/WHO_NHD_01.09/en/. (Accessed May 6, 2019). [Google Scholar]
- 38. Gutiérrez JP, Bautista S, Gertler P, Hernández M, Bertozzi SM. Impacto de Oportunidades en la Morbilidad y el Estado de Salud de la Población Beneficiaria y en la Utilización de los Servicios de Salud. Resultados de Corto Plazo en Zonas Urbanas y de Mediano Plazo en Zonas Rurales [Impact of Oportunidades on mordibity and health status of the beneficiary population, and on utilization of health services. Results in the short-term in urban areas and medium term in rural areas]. [Internet] In: Hernández-Padro B, Hernández-Ávila Meditors. Evaluación Externa del Programa Oportunidades. Cuernavaca, México: Instituto Nacional de Salud Pública, 2004, pp. 19–69.. Available from: https://evaluacion.prospera.gob.mx/es/wersd53465sdg1/docs/2004/insp_ciesas_2004_tomo_ii.pdf (Accessed April 23, 2019). [Google Scholar]
- 39. Sosa-Rubi SG, Walker D, Servan E, Bautista-Arrendando S. Learning effects of a conditional cash transfer programme on poor rural women's selection of delivery care in Mexico. Health Policy Plan. 2011;26(6):496–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Instituto Nacional de Salud Pública (INSP). Componente de Oportunidades de la Encuesta Nacional de Salud y Nutrición (ENSANUT) 2006 [The Oportunidades component of the National Health and Nutrition Survey (ENSANUT 2006)]. Cuernavaca, México, 2006. Available from: https://evaluacion.prospera.gob.mx/es/wersd53465sdg1/docs/2006/insp_2006_ensanut.pdf (Accessed April 20, 2019). [Google Scholar]
- 41. Attanasio O, Di Mario V. Efectos de mediano plazo del Programa Oportunidades sobre el consumo de los hogares en zonas rurales [Medium-term effects of the Oportunidades programo on household consumption in rural areas]. In: Hernández-Prado B, Hernández-Ávila Meditors. Evaluación Externa de Impacto del Programa Oportunidades 2004, Tomo IV. Cuernavaca, México: Aspectos económicos y sociales, pp. 19–52.[cited2018; Dec 20]. Available from: https://evaluacion.prospera.gob.mx/es/wersd53465sdg1/docs/2004/insp_ciesas_2004_tomo_iv.pdf. (Accessed April 20, 2019). [Google Scholar]
- 42. Rivera-Dommarco JA, Shamah T, Villalpando S, Cuevas L, Mundo V, Morales Ruan C. El estado nutricional de la población en México: cambios en la magnitud, distribución y tendencias de mala nutrición de 1988 a 2006 [The nutritional status of the population in Mexico: changes in the magnitude, distribution and trends of malnutrition]. In: González-Cossío T, Rivera-Dommarco J, López Acevedo G, Rubio Soto GMeditors. Banco Mundial y Secretaría de Desarrollo Social (SEDESOL), México D.F.: Nutrición y Pobreza, 2008, pp. 1–22. [Google Scholar]
- 43. Hurrell RF. Fortification: overcoming technical and practical barriers. J Nutr. 2002;132(4 Suppl):806S–12S. [DOI] [PubMed] [Google Scholar]
- 44. Shamah-Levy T, Villalpando S, Rivera-Dommarco JA, Mundo-Rosas V, Cuevas-Nasu L, Jiménez-Aguilar A. Ferrous gluconate and ferrous sulfate added to a complementary food distributed by the Mexican nutrition program Oportunidades have a comparable efficacy to reduce iron deficiency in toddlers. J Pediatr Gastroenterol Nutr. 2008;47(5):660–6. [DOI] [PubMed] [Google Scholar]
- 45. Morales JC, Sánchez-Vargas E, García-Zepeda R, Villalpando S. Sensory evaluation of dairy supplements enriched with reduced iron, ferrous sulfate or ferrous fumarate. Salud Publica Mex. 2015;57(1):14–21. [DOI] [PubMed] [Google Scholar]
- 46. Levy S. Progress against poverty. Sustaining Mexico's Progresa-Oportunidades Program. Washington, D.C.: The Brookings Institution; 2006. [Google Scholar]
- 47. Neufeld L, Steta C, Rivera J, Martinez Valle A, Grados R, Uriega S, Lopez VH. Evaluation for program decision making: a case study of the Oportunidades program in Mexico. J Nutr. 2011; 141(11):2076–83. [DOI] [PubMed] [Google Scholar]
- 48. Zlotkin S, Arthur P, Antwi KY, Yeung G. Treatment of anemia with microencapsulated ferrous fumarate plus ascorbic acid supplied as sprinkles to complementary (weaning) foods. Am J Clin Nutr. 2001;74(6):791–5. [DOI] [PubMed] [Google Scholar]
- 49. Schauer C, Zlotkin S. Home fortification with micronutrient sprinkles—A new approach for the prevention and treatment of nutritional anemias. Paediatr Child Health. 2003;8(2):87–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Mbuya MN, Menon P, Habicht JP, Pelto GH, Ruel MT. Maternal knowledge after nutrition behavior change communication is conditional on both healthworkers’ knowledge and knowledge-sharing efficacy in rural Haiti. J Nutr. 2013;143(12):2022–8. [DOI] [PubMed] [Google Scholar]
- 51. Menon P, Covic NM, Harrigan PB, Horton SE, Kazi NM, Lamstein S, Neufeld L, Oakley E, Pelletier D. Strengthening implementation and utilization of nutrition interventions through research: a framework and research agenda. Ann N Y Acad Sci. 2014;1332:39–59. [DOI] [PubMed] [Google Scholar]