Abstract
Due to their potent immunomodulatory anti-inflammatory properties, synthetic glucocorticoids (GCs) are widely utilized in the treatment of chronic inflammatory disease. In this review, we examine our current understanding of how chronic inflammation and commonly used therapeutic GCs interact to regulate bone and muscle metabolism. Whilst both inflammation and therapeutic GCs directly promote systemic osteoporosis and muscle wasting, the mechanisms whereby they achieve this are distinct. Importantly, their interactions in vivo are greatly complicated secondary to the directly opposing actions of GCs on a wide array of pro-inflammatory signalling pathways that underpin catabolic and anti-anabolic metabolism. Several clinical studies have attempted to address the net effects of therapeutic glucocorticoids on inflammatory bone loss and muscle wasting using a range of approaches. These have yielded a wide array of results further complicated by the nature of inflammatory disease, underlying the disease management and regimen of GC therapy. Here, we report the latest findings related to these pathway interactions and explore the latest insights from murine models of disease aimed at modelling these processes and delineating the contribution of pre-receptor steroid metabolism. Understanding these processes remains paramount in the effective management of patients with chronic inflammatory disease.
Keywords: glucocorticoid, muscle wasting, osteoporosis
1. Glucocorticoids and Therapeutic Glucocorticoid Excess
Synthetic glucocorticoids (GCs), such as dexamethasone, prednisolone and hydrocortisone, are widely utilized in the treatment of chronic inflammatory diseases such as chronic obstructive pulmonary disease (COPD), inflammatory bowel disease (IBD) and rheumatoid arthritis (RA), with approximately 1% of the adult population in the U.K. and U.S. receiving this class of drugs. Their mechanisms of action are diverse, with GCs suppressing a range of pro-inflammatory pathways including p38-mitogen activated protein kinases (p38-MAPK), nuclear factor kappa-light-chain-enhancer (NF-κB) and activator protein (AP-1), in addition to inducing pro-resolving factors such as glucocorticoid induced leucine zipper (GILZ) and annexin-1 [1,2,3]. These significantly reduce leukocyte infiltration at sites of inflammation, suppress the production of pro-inflammatory cytokines and chemokines and support resolution of inflammation and tissue remodelling [4,5]. Despite the potent immune-modulatory anti-inflammatory actions of therapeutic GCs, their clinical application is limited due to severe systemic side effects. These occur in up to 70% of patients and can include muscle wasting and GC induced osteoporosis (GIO) [6,7,8,9,10]. The actions of GCs on bone and muscle metabolism are well established, but themselves complicated in the backdrop of chronic inflammation by separate inflammatory driven muscle wasting and bone loss. The inflammatory pathways that mediate bone and muscle loss in chronic inflammation are in turn suppressed by the anti-inflammatory actions of GCs, further complicating the prediction of their outcome on the musculoskeletal system. Understanding the complex interactions between GC and inflammatory regulation of bone and muscle metabolism remains paramount in the effective management of patients with chronic inflammatory disease. In this review, we explore how inflammatory drivers and therapeutic GCs interact to regulate bone and muscle metabolism and consider the role of local steroid metabolism in shaping these processes.
2. Glucocorticoid Signalling and Regulation of Inflammation
Lipophilic GCs readily diffuse across cell membranes, signalling through the cytoplasmic GC receptor (GR) superfamily, encoded by the NR3C1 gene. Classically, GC signalling and GR transactivation occur through ligand binding of the GRα homodimer. In its unbound state, GRα forms a multi-protein complex with chaperone proteins such as heat shock proteins (HSPs), HSPp-70, HSP90 and FK506 binding protein 52 that block their nuclear localization signal (NLS) and prevent translocation to the nucleus from the cytoplasm [11]. Upon GC binding, the GRα undergoes a conformational change, allowing dissociation of chaperone proteins. Homo-dimerization and exposure of the NLS are required for nuclear translocation of the ligand bound GR, where it can influence gene expression [12] (Figure 1). This is an oversimplified view of GC signalling, as several studies utilizing the GRdim mouse (possessing a mutation preventing GR dimerization) reveal that the anti-inflammatory properties of therapeutic GCs are mediated by both homo-dimeric GRα complexes and monomeric GRα to facilitate transactivation or transrepression of pro-inflammatory genes [5,13,14,15,16]. Whilst the mechanisms that underpin GR signalling have been reviewed extensively elsewhere, several key pathways are prominent in mediating the anti-inflammatory actions of GCs [17]. These include the direct GRα homodimer transactivation of anti-inflammatory genes such as secretory leukocyte protease inhibitor (SLPI), MAKP-1, GILZ and tristetraprolin (TTP), which suppress the NF-kB and p38-MAPK inflammatory pathways, in addition to the inhibition of pro-inflammatory transcription factors via their tethering to the GC bound GR [18,19,20,21]. In particular, GCs act via the GR to suppress the NF-κB and p38-MAPK inflammatory pathways and AP-1 pro-inflammatory pathways, which regulate the transcription of various genes relating to inflammation such as tumour necrosis factor-alpha (TNF-α) and interleukin-1 (IL-1β) and -6 [22]. Many of these inflammatory pathways considered are direct contributors to the process of inflammatory bone and muscle wasting and are themselves opposed by the actions of therapeutic GCs. This review will now consider how inflammation and GCs influence bone and muscle metabolism, both in isolation and in concert with one another.
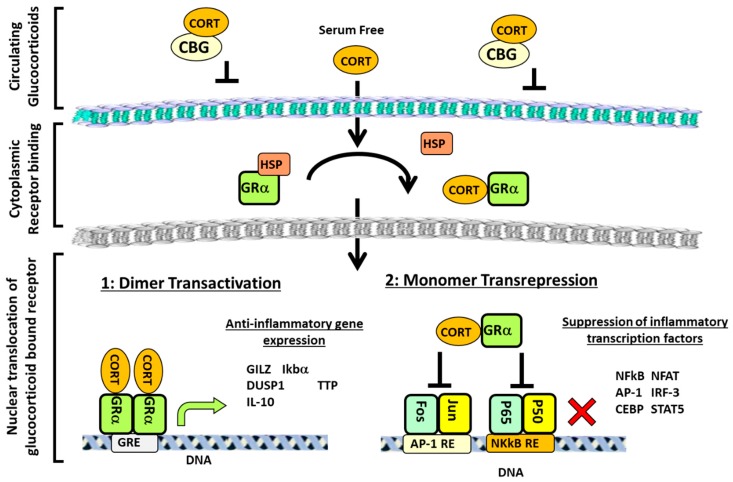
Figure 1.
Overview of glucocorticoid (GC) signalling pathways. The majority of glucocorticoids (GCs) in the circulation are bound by corticosteroid-binding globulin (CBG), which prevents diffusion across the membrane. However, free GCs can readily enter the cell, where they bind to the GR in the cytoplasm. This induces a conformational change in the glucocorticoid receptor (GR), which causes the dissociation of chaperone molecules, such as heat shock proteins (HSPs), to expose the nuclear localisation signal (NLS) and allow translocation of the GC/GR complex to the nucleus. Here, the GR can either dimerise to transactivate anti-inflammatory genes or signal as a monomer to inhibit pro-inflammatory transcription factors. Cortisol (CORT), nuclear factor of activated T-cells (NFAT), CCAAT-enhancer-binding proteins (or C/EBPs), nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB), p38 mitogen-activated protein kinases (p-38-MAPK), glucocorticoid induced leucine zipper (GILZ), secretory leukocyte protease inhibitor (SLPI), tristetraprolin (TTP), mitogen-activated protein kinase-1 (MKP-1), activator protein 1 (AP-1), signal transducer and activator of transcription 5 (STAT5), and response element (RE).
3. Bone Metabolism
Bone metabolism is a tightly regulated process that ensures homeostasis between bone resorption and bone formation. This process maintains a balance in calcium and phosphate mineral homeostasis, as well as allowing constant healthy remodelling to compensate for external loading stress and damage and requires the close interaction between osteocytes, bone lining cells, bone forming osteoblasts and bone resorbing osteoclasts [23]. Here, in quiescent bone, osteocytes produce factors such as transforming growth factor-β (TGF-β), sclerostin and dickkopf WNT signaling pathway inhibitor 1 (DKK-1), which inhibits osteoclast and osteoblast maturation and differentiation [24]. Signals such as bone matrix damage or immobilization result in osteocyte apoptosis, leading to a removal of the inhibitory signals and increases in factors that promote osteoclastogenesis, such as macrophage colony stimulating factor (M-CSF) and receptor activator of nuclear factor kappa-β ligand (RANKL) [25,26,27]. Together, these promote osteoclast differentiation from hematopoietic precursors and increase receptor activator of nuclear factor kappa-β (RANK) pathway activation, driving multinuclear polykaryon formation and the formation of mature osteoclasts that express osteoclast specific genes including tartrate-resistant acid phosphatase (TRAP) and cathepsin K [28,29,30]. Mature osteoclasts form tight integrin junctions on mineralized bone matrix, forming an acidified resorption compartment that facilitates the degradation of the inorganic hydroxyapatite component of the bone [31,32]. The organic component of bone can then be degraded by lysosomal enzymes, such as cathepsin K. In parallel to this process, a reduction in factors that suppress osteoblast differentiation (such as sclerostin and DKK-1) and an increase in factors that induce osteoblast differentiation (such as WNT, TGFβ and insulin-like growth factor 1 (IGF-1)) promote the formation of osteoblast pre-cursors from mesenchymal derived progenitors [33,34,35]. This process is tightly regulated through the master transcriptional regulator runt-related transcription factor 2 (RUNX2), mediating the expression of osteoblast specific genes such as osteocalcin, osteopontin and bone sialoprotein [36,37]. As osteoblasts continue to mature, RANKL levels (which maintain osteoclasts) decrease, whilst osteoprotegerin (OPG) (the dummy receptor for RANKL that suppresses RANK signalling) increases. Together with increasing TGFβ signalling, the decrease in RANK/RANKL signalling leads to reduced osteoclast differentiation, activity and survival [38]. The transition toward the reversal phase is characterised by an increase in mature osteoblasts at the vacated osteoclast lacunae site of bone resorption. One key cell type that appears to facilitate this transition appears to be a unique cell population known as reversal cells, which cover the eroded bone surface. Here, one study has revealed that the disruption of these cells results in a loss of the initiation of bone resorption, highlighting their importance in this process [39]. Mature osteoblasts then secrete factors required for osteoid formation including organic matrix rich in type 1 collagen, osteocalcin and bone sialoprotein (BSP) [40]. This is then mineralized via the deposition of hydroxyapatite crystals, created by the flux of calcium and phosphate ions within vesicles that are deposited as a mineralized nodule, in a process that has been shown to require the enzyme alkaline phosphatase to release phosphate ions [41,42]. Ultimately, bone formation ceases as osteoblasts undergo apoptosis or are incorporated into the osteocyte network.
4. Regulation of Bone Metabolism by Inflammation
In diseases such as RA, IBD and COPD, ongoing systemic inflammation results in inflammatory osteoporosis, with localized destruction of bone at sites of inflammation in diseases such as RA [43,44,45,46,47]. Systemic bone loss is characterized by a general decrease in bone mineral density (BMD) at the femoral neck, hip and spine in patients, resulting in increased fracture rates [47,48,49,50]. It is widely accepted that this inflammatory bone loss results from an imbalance in the bone remodelling cycle, shifting towards resorption and away from formation [51]. Studies exploring inflammatory bone loss are complicated by immobility in patients and the impact of concurrent anti-inflammatory drugs that can influence bone metabolism. However, significant insights have been derived from in vitro studies and clinical studies.
A prominent mechanism associated with a shift toward inflammatory bone loss is the interaction of the activated immune system with bone resorbing osteoclasts. Here, changes in the inflammatory cytokine profiles in patients with chronic inflammation result in increased levels of pro-osteoclastogenic mediators and a decrease in anti-osteoclastogenic mediators. Many of the pro-osteoclastogenic cytokines upregulated in chronic inflammation, including TNF-α, IL-1, IL-6, IL-8 and IL-17, mediate their actions via an upregulation of RANKL on fibroblasts and osteoblasts, which in turn promotes osteoclastic bone resorption [52,53,54,55]. In particular, combinations of cytokines including TNF-α, IL-1 and IL-6, act synergistically to increase RANKL in inflammation [56]. Activated Th17 and B cells also upregulate RANKL expression promoting resorptive bone lesions in patients and in vitro in a RANKL dependent manner [57,58,59]. A recent study identified a novel cytokine induced in response to TNF-α in T cells, known as secreted osteoclastogenic factor of activated T cells (SOFAT), which has the ability to cause osteoclastogenesis in a RANKL independent manner and may have implications in bone loss induced by chronic inflammatory disease [60].
Of particular interest, TNF-α also has effects on the bone forming ability of osteoblasts in inflammation. TNF-α treatment of osteoblasts’ precursors inhibits their differentiation by suppressing the DNA binding ability of RUNX2, leading to inhibition of alkaline phosphatase expression and matrix deposition [61]. The pro-apoptotic properties of TNF-α on osteoblasts has also been observed [62]. Similarly, IL-6 treatment of osteoblasts leads to reductions in alkaline phosphatase activity and in the expression of RUNX2 and osteocalcin, with mineralisation dramatically reduced in a dose dependent manner [63]. The prominent role of the inflammatory activation of osteoclastogenesis was derived from murine models using the TNF-tg mouse of chronic polyarthritis and inflammatory bone loss. Here, blockade of both the TNF-α and the RANKL/RANK signalling pathways using anti-TNF therapy in combination with anti-osteoclastic (OPG) was able to prevent inflammatory bone erosions [64]. Bone repair was then augmented through the addition of the pro-osteoblastic hormone parathyroid hormone (PTH). These results highlight the importance of bot inflammatory activation of osteoclasts and suppression of osteoblasts in mediating systemic and localized bone loss in chronic inflammation. Consequently, these results indicate that repair of bone erosions requires a therapy that simultaneously controls inflammation while also impacting both osteoclastic bone resorption and osteoblastic bone formation to shift the balance in bone homeostasis and promote normal repair and recovery of bone.
5. Effects of Glucocorticoids on Bone Metabolism
Whilst GCs are widely used in the treatment of chronic inflammation, they are themselves associated with an increased risk of fractures and osteoporosis at therapeutic doses resulting in GIO. GIO is the most common form of secondary osteoporosis with risk of fracture increasing dramatically within three to six months of starting GC therapy [65]. Interestingly, these changes are reversed rapidly upon cessation of GCs, indicating a rapid and acute nature of action at the cellular level. The mechanism that underpins this appears to be primarily mediated by a substantial inhibition of osteoblastic bone formation [66]. Under physiological conditions, GCs promote osteoblast maturation. However, at higher therapeutic doses, GCs downregulate WNT agonists and upregulate WNT inhibitors, which induce apoptosis and suppress osteoblast differentiating [67,68,69]. In one clinical study examining children receiving exogenous glucocorticoids, serum levels of the WNT signalling inhibitor DKK-1 were shown to be significantly elevated, suggesting it may play a key role in reduced bone formation in GIO [70]. In studies using transgenic mice with osteoblast targeted disruption of glucocorticoid signalling, GC signalling via the GR was shown to mediate reduced bone formation through the suppression of osteoblast differentiation via the WNT pathway and through inducing osteoblast apoptosis, with animals with GR signaling disruption being protected from GC induced bone loss [67,71].
The impact of GCs on osteoclasts is less clear. Studies have reported that GC treatment results in a decrease in osteoclast number, but an increase in osteoclast longevity, potentially mediated via a GC induced increase in M-CSF production [66,72,73]. In addition, studies have shown conflicting results on the expression of osteoclastic genes in response to GCs. One study showed that dexamethasone treatment of murine calvarial bones resulted in increased mRNA levels of Rank and Rankl, leading to increased markers of osteoclast activation [74]. Other studies showed that OPG levels are suppressed or reported no change at all in RANKL and OPG levels [72,75,76]. Some insight comes from one study in children receiving exogenous GCs, where serum levels of RANKL were elevated and OPG suppressed [77]. In these patients, spontaneous osteoclastogenesis in vitro was apparent in monocytic cell precursors. Certainly, one study utilizing a murine model of therapeutic GC delivery revealed that the targeting of osteoclasts using bisphosphonates was an effective strategy to prevent both cortical and trabecular bone loss [78]. There is some evidence to indicate that the responsiveness of osteoclasts to GCs is highly dependent on the stage of cell differentiation, but these findings require further investigation [79]. The variation in GC dose, the method of administration and the models employed may explain the variation in the results reported to date, whilst their interactions with inflammatory mediators in patients with chronic inflammation should also be taken into account when investigating their bone related effects.
6. Glucocorticoids, Inflammation and Bone Homeostasis
Glucocorticoids directly oppose a wide array of the pathways that drive inflammatory bone loss. Amongst these, their suppression of pro-inflammatory factors such as RANKL, TNF-α and IL-6 appears to be prominent in mediating their bone sparing effects in chronic inflammatory joint destruction, through the direct suppression of osteoclastogenesis and osteoclast activation [80] (Figure 2). In contrast, their potent suppression of anabolic bone formation by osteoblasts may synergize with the deleterious actions of inflammation on osteoblasts. Consequently, the net balance of GCs on bone metabolism in the context of chronic inflammation is less clear. Several clinical studies shed light on the balance between beneficial and detrimental actions of GCs on bone metabolism in chronic inflammation. These include a study reporting no differences in BMD loss in RA patients receiving therapeutic GCs in combination with traditional disease modifying anti-rheumatic drugs (DMARDS), relative to a matched control cohort [81]. Of particular interest were studies exploring whether GCs at lower therapeutic doses might promote positive anti-inflammatory actions without eliciting detrimental bone loss. These studies reported that low dose GC therapy in RA did not increase the risk of generalized osteoporosis at the spine and hip [82,83]. Another study found that patients receiving GCs in combination with anti-TNF therapy had a 2.5% increase in BMD at the femoral neck compared to a 0.7% decrease in BMD in those using anti-TNF alone, suggesting that GCs may increase bone metabolism in this context [84]. In contrast, two further studies found that GCs’ use was associated with decreased BMD in RA patients [43,85]. Similarly, in juvenile chronic arthritis (JCA), two studies found that GC treated patients had significantly less trabecular bone and higher risk of vertebral collapse than a matched control cohort [86,87]. These studies found strong links with the dose of steroid applied, but were further complicated by the application of GCs in the developing skeleton of younger patients, who may be more vulnerable to the anti-anabolic actions of GCs than adults. The conflicting nature of these results may stem from a variety of issues, including differences in disease pathophysiology, disease activity, duration and variations in the delivery and dose of GC therapy. In addition, concomitant use of alternative therapies such as anti-TNF treatments causes further complications, making it difficult to dissect the contribution of GCs to changes in bone metabolism in chronic inflammatory disease.
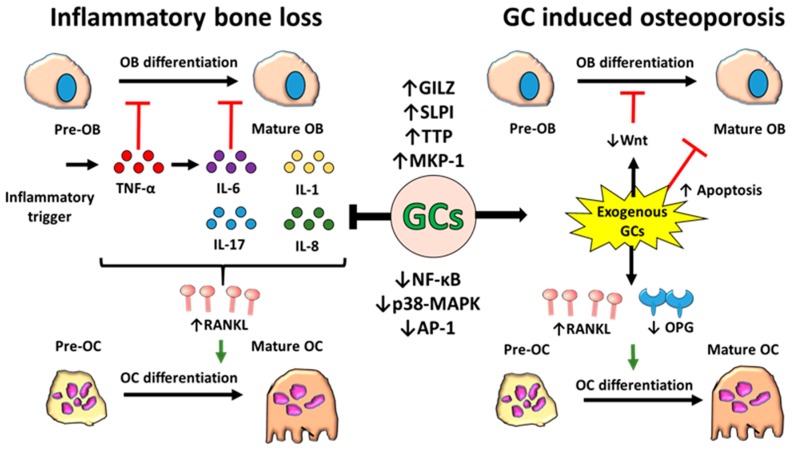
Figure 2.
Schematic representation of the effects of inflammation and glucocorticoids (GCs) on bone remodelling. During inflammation, elevated levels of pro-inflammatory cytokines, such as TNF-α and IL-6, inhibit the differentiation of bone forming osteoblasts from their precursors. These cytokines, along with other pro-inflammatory mediators including IL-1, IL-17 and IL-8, also upregulate the expression of receptor activator of nuclear factor kappa-Β ligand (RANKL), which binds to receptor activator of nuclear factor kappa-Β (RANK) on pre-osteoclasts and triggers their differentiation into mature bone resorbing osteoclasts. Overall, bone formation is decreased while bone resorption is increased, leading to a net loss of bone. Although GCs suppress inflammation via suppression of pro-inflammatory factors and induction of anti-inflammatory mediators, they can also independently drive bone loss by inhibiting differentiation and inducing apoptosis of osteoblasts whilst increasing osteoclast differentiation by stimulating expression of RANKL and decreasing its decoy receptor osteoprotegerin (OPG). Osteoblasts (OBs), p38 mitogen-activated protein kinases (p-38-MAPK), glucocorticoid-induced leucine zipper (GILZ), secretory leukocyte protease inhibitor (SLPI), tristetraprolin (TTP), mitogen-activated protein kinase-1 (MKP-1), activator protein 1 (AP-1), OC (osteoclast), canonical WNT signalling (WNT), and nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB).
7. Muscle Mass Related Metabolism
Similar to bone, muscle metabolism is tightly regulated to ensure a balance between anabolic and catabolic processes governing muscle mass. Its regulation is critical not only to facilitate mechanical locomotion, but also as a key site for whole body energy metabolism and homeostasis [88]. Several critical anabolic and catabolic signalling pathways determine muscle protein synthesis, muscle proteolysis and myogenesis as cellular processes in control of muscle mass.
IGF-1 has been identified as a critical factor mediating the regulation of anabolic and catabolic muscle homeostasis in adult myofibers. Produced primarily in the liver, its binding to the IGF-1 receptor (IGF1R) in skeletal muscle allows recruitment of the insulin receptor substrate 1 (IRS-1) and activation of phosphatidylinositol-3-kinase (PI3K) and phosphorylation of protein kinase B (nnown as AKT), [89,90]. Together, these result in the activation of the mammalian target of rapamycin (mTOR) signalling pathway, which results in suppression of proteolysis and activation of muscle protein synthesis. mTOR activation suppresses proteolytic, forkhead box class O family member proteins (FOXOs) and glycogen synthase kinase-3 beta (GSK-3β) pathways [91,92]. The activation of mTOR signalling promotes muscle protein synthesis through the downstream phosphorylation and inactivation of eIF4E-binding protein 1 (4E-BP1) and activation of the ribosomal protein S6 kinase beta-1 (p70S6K) [93,94,95]. When active, 4E-BP1 operates by suppressing the eukaryotic translation initiation factors (elF), which are a central rate limiting step in the regulation of protein synthesis in muscle. Here, eIF4F (a complex of initiation factors, eIF4e, eIF4G and eIF4A), promotes the translation of mRNA coding for muscle proteins by facilitating the cap dependent binding of messenger RNA to the 40S ribosomal subunit [96]. The repressor protein 4E-BP1 is a powerful negative regulator of eIF4F mediated protein translation, whilst its phosphorylation causes its dissociation from eIF4E and enables mRNA translation of anabolic muscle proteins. A second key stage in the regulation of anabolic protein metabolism in muscle occurs through the regulation of phosphorylated p70S6K by mTOR, which facilitates ribosomal biogenesis and translation capacity required for muscle protein anabolism [97]. An additional modulator of skeletal muscle mass downstream of the IGF-1/AKT pathway is GSK-3β. This protein kinase is a negative regulator of the translation initiation factor eIF2B and is phosphorylated and inactivated by AKT, allowing initiation of mRNA translation [98,99,100]. Together, the activation of these pathways by IGF-1 or insulin promote protein synthesis in muscle, favouring increased muscle mass.
The regulation of muscle catabolism shares many of these pathways and involves their inverse activation state. Proteolysis of skeletal muscle proteins through their targeted degradation by the ubiquitin-proteasome system (UPS) and autophagy pathways is under stringent control of the PI3K/AKT and mTOR signalling pathways [101]. Here, a reduction in anabolic factors such as IGF-1 or an increase in negative regulators such as myostatin, TGFβ or FGF results in a decrease of the PI3K/AKT and mTOR signalling. As AKT and mTOR kinase activity is responsible for inhibitory phosphorylation of the FOXOs, including FOXO1, FOXO3 and FOXO4 [102,103], the lack thereof allows their nuclear translocation. FOXO transcription factors bind to promoter and enhancer regions of target genes such as the E3 ligases, Atrogin-1 and muscle RING-Finger protein-1 (MURF-1) and the autophagy-related genes LC3 and Bnip3 [104,105,106,107]. In addition to FOXO, increased GSK-3β secondary to reduced IGF-1/AKT signalling has also been implicated in upregulating Atrogin-1 and MURF-1 [108].
The E3 ligases are the largest family of ubiquitination factors targeting muscle proteins for degradation by the UPS [109,110] and can be highly upregulated in catabolic conditions. These include the muscle specific F-box protein Atrogin-1 encoded by the FBXO32 gene and MURF-1 encoded by the TRIM63 gene [111,112]. Their expression is elevated in a plethora of skeletal muscle atrophy models, including immobilisation, denervation, cancer, starvation and diabetes [111,112,113]. Atrogin-1 has been shown to ubiquitinate desmin and vimentin, muscle proteins essential to sarcomere Z-disk architecture [114]. In addition, Atrogin-1 stimulates the degradation of transcription factor EIF3F, leading to impaired muscle protein synthesis [115]. This E3 ligase has also been shown to play a pivotal role in repressing myogenesis through the ubiquitination of myoblast determination protein 1 (MYOD) [116].
MURF-1 encodes a protein containing a RING finger domain, which is responsible for its ubiquitin-ligase activity [112,117]. MURF-1 ubiquitinates and catalyses the degradation of contractile proteins and thick filaments, such as myosin and troponin I, with the sparing of thin filaments such as actin [118,119]. Besides a role in the UPS, increased FOXO activation also upregulates protein degradation and clearance through the autophagy pathways [106]. In muscle, this appears to be mediated through the direct upregulation of autophagy genes such as LC3, BNIP3 and ATG through the FOXO pathway during muscular atrophy [120,121,122].
Postnatal myogenesis is an anabolic process important to the maintenance of muscle mass and integrity. Insulin-like growth factor 1 (IGF-1) has been shown to be a positive driver of myogenesis, whilst fibroblast growth factor (FGF), transforming growth factor β (TGF- β) and myostatin are potent inhibitors [123,124,125,126]. In addition, various secreted WNT signalling factors positively influence myogenesis. These are regulated by an array of stimuli, including exercise, nerve innervation and dietary protein intake, and are mediated through various gene regulatory networks including the T-box family, tbx6, ripply1 and mesp-ba in mesenchymal stem cell populations [127,128,129]. Ultimately, this drives the expression of myogenic regulatory factors (MRFs) such as myogenic differentiation 1 (MYOD), myogenic factor 5 (MYF5) and myogenin (MYOG), this process being in mesenchymal derived muscle progenitor cells called satellite cells [130,131,132,133]. Although some redundancy exists in their cellular function, MYF5 is mostly implicated in mediating the proliferation of satellite cells and MYOD in their differentiation into myoblasts, whilst downstream factors, including myogenin, initiate further differentiation of mature myocytes followed by the fusion and formation of mature myotubes [130,131,132] or mostly relevant for adult muscle, fusion with myofibers.
Below, we will describe how inflammation and glucocorticoids impact these regulatory processes of muscle mass metabolism, driving a shift towards anti-anabolic and catabolic protein metabolism, resulting in muscle wasting.
8. Effects of Inflammation of Muscle Metabolism
Inflammation is a well established driver of muscle wasting in preclinical models and strongly relates to poor prognostic outcome and increased morbidity and mortality in patients with chronic inflammatory diseases [134]. Pro-inflammatory cytokines such as TNFβα, IL-1β and IL-6, which are elevated in chronic inflammation, are themselves reported to drive proteolysis and autophagy and suppress myogenesis and protein synthesis in muscle [135,136,137,138]. Of these, TNF-α, at the apex of the inflammatory cytokine cascade in many chronic inflammatory diseases, is critical in regulating inflammatory muscle wasting. Here, its activation of the NF-kB and p-38 MAPK pathways directly induces muscle wasting through the increased expression of the E3 ligases, atrogin-1 and MURF-1 and activation of the UPS system [139,140,141,142,143]. In models of chronic inflammation, TNF-α also downregulates circulating levels of IGF-1 and the downstream PI3K/AKT/mTOR signalling pathways, whilst upregulating the catabolic FOXO pathway to suppress protein synthesis and myogenesis in muscle [141,142,144,145]. Another factor implicated in inflammatory muscle wasting is myostatin. This is also reported to be increased in chronic inflammation, where it positively correlates with markers of disease severity. Elevated myostatin downregulates PI3K/AKT/mTOR signalling, promoting muscle atrophy [146,147]. Of interest, several studies have reported elevated endogenous GC levels as being central mediators of inflammatory muscle wasting. Here, the inflammatory activation of the hypothalamic/pituitary/adrenal (HPA) axis in response results in an elevation of circulating cortisol to mediate muscle wasting [148,149,150,151]. Of note, the blockade of endogenous GC production or muscle GR signalling could reverse muscle wasting in some experimental models [152,153]. This indicates that in addition to a direct impact of inflammation on intra-cellular muscle mass regulatory processes, activation of the HPA axis as an evolutionarily conserved response to suppress systemic inflammation can result in GC driven muscle wasting as an indirect effect of inflammation on skeletal muscle.
9. Effects of Glucocorticoids on Muscle Metabolism
Extended exposure to therapeutic GCs results in the rapid onset of a GC induced muscle atrophy, characterised by a decrease in myogenesis and protein synthesis and an increase in proteolysis and atrophy of muscle fibres [9,154,155,156,157]. This leads to a significant decrease in muscle fibre size, with a greater degree of wasting apparent in fast-twitch or type II muscle fibres [158]. The shift towards greater catabolic loss of protein and decreased anabolic synthesis in muscle is elicited by GCs through a number of pathways, including a decrease in IGF-1 signalling and an increase in negative regulators of the mTOR pathways such as myostatin and the protein regulated in development and DNA damage response 1 (REDD1) [157,159]. Similarly, as with inflammatory pathway activation, GCs also activate the UPS and autophagy secondary to upregulation of the FOXO1 pathway [80,154,160]. In particular, the marked increase in degradation of contractile skeletal muscle proteins through the UPS system is believed to be central in GC induced muscle wasting in vivo. This is supported by several studies demonstrating the downregulation of the PI3K/AKT/mTOR signalling pathways and the upregulation of the E3 ligases Atrogin-1 and MURF-1 in response to GCs [112]. Several studies have also demonstrated a significant increase in 4E-BP1 and suppression of p70S6K in GC induced muscle atrophy, demonstrating a role for reduced protein synthesis and regeneration [157,159]. Of interest, the restoration of IGF-1 signalling can rescue GC induced myopathy in mice, demonstrating a crucial role for this growth factor in the process of GC-induced myopathy [9,154,155,156]. Glucocorticoid mediated muscle wasting has also been shown to be rescued through the in vivo deletion of myostatin, indicating that the negative regulation of the IGF-1 pathway may also be a crucial step in this process [161,162,163].
10. Interaction between Inflammation and Glucocorticoids in Muscle
As with bone, many of the central inflammatory pathways that induce muscle wasting, including the NF-kB and p38-MAPK pathways, are themselves suppressed by GC signalling, suggesting that therapeutic application may protect against the process of inflammatory muscle wasting. However, other elements of inflammatory muscle wasting such as the suppression of IGF-1 and induction of myostatin and FOXO1 pathway activation are common components in both inflammatory and GC induced muscle wasting (Figure 3). Understanding how these interact in vivo remains paramount in our understanding of how therapeutic GCs should be applied in the setting of chronic inflammatory disease. Some insights arise from clinical studies exploring these processes in patients with inflammatory disease receiving GCs. Of note, in inflammatory myopathies arising directly from muscle inflammation, such as with polymyositis and dermatomyositis, GCs are effective in controlling inflammation and protecting against inflammatory muscle wasting and associated weakness [164]. Similarly, therapeutic GCs are effective in preventing muscle wasting in patients with Duchenne muscular dystrophy (DMD), where progressive muscle necrosis mediates loss of muscle [165,166,167,168,169]. However, in other inflammatory diseases, where muscle wasting occurs secondarily to inflammation at a non-muscle site, the application of therapeutic GCs is strongly associated with rapid loss of muscle mass [170,171]. These findings may suggest that GCs can oppose the process of inflammatory muscle wasting when the active inflammation is confined to the muscle, but promote muscle wasting when used to manage other systemic chronic inflammatory diseases such as RA. As with GC induced osteoporosis in patients with chronic inflammatory disease, the interpretation of these findings in relation to muscle wasting is complicated by disease severity and duration and by concurrent DMARD therapies.
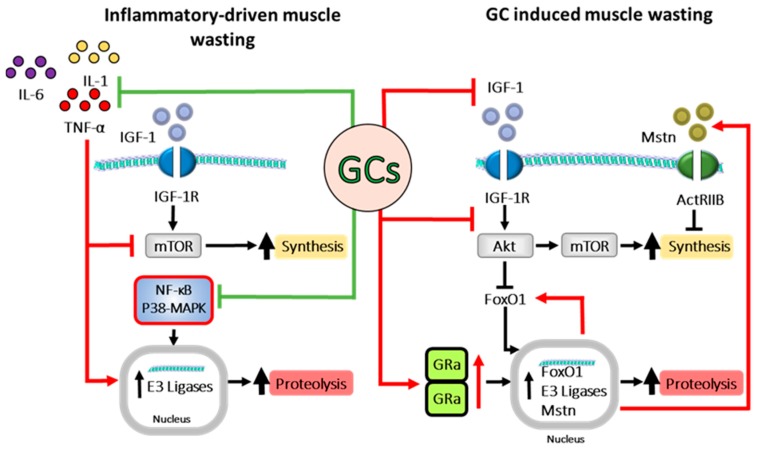
Figure 3.
Schematic representation of signalling pathways involved in both inflammatory driven and GC induced muscle wasting and their interactions. Inflammatory cytokines such as TNF-α and IL-1 inhibit mammalian target of rapamycin (mTOR) signalling, dampening muscle protein synthesis, whilst simultaneously inducing transcription of E3 ligases, leading to muscle proteolysis. Glucocorticoids (GCs) inhibit inflammatory signalling, including nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) signalling, and therefore decrease inflammatory driven muscle wasting. Despite this, GCs also drive muscle wasting through several pathways themselves, including suppression of the IGF-1/AKT/mTOR signalling cascade, leading to decreased protein synthesis and increased FOXO1 transcription. GR activation and dimerization induce the transcription of myostatin (MSTN), FOXO1 and other E3 ligases, leading to increased proteolysis and diminished protein synthesis. Forkhead box protein O1 (FOXO1), mammalian target of rapamycin (mTOR), insulin like growth factor (IGF-1), (p-38-MAPK), glucocorticoid induced leucine zipper (GILZ), secretory leukocyte protease inhibitor (SLPI), tristetraprolin (TTP), nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB), glucocorticoid receptor (GR), myostatin (MSTN), and IGF-1 receptor (IGF-1 R).
11. Insights from Murine Models of Chronic Inflammation Receiving Therapeutic Glucocorticoids
Additional insight has come from murine models of polyarthritis receiving therapeutic GCs. These are able to circumvent issues related to differences in disease activity between patients and complications arising from the various alternative anti-inflammatory drugs used to manage disease in patients. In one such study, we examined the role of the GC corticosterone, delivered as a monotherapy in the TNF-tg murine model of polyarthritis, on net bone and muscle metabolism [80]. This revealed that therapeutic doses of GCs, whilst effective at suppressing disease activity, also potently suppressed inflammatory osteoporosis and juxta articular bone loss. This confirmed that their capacity to suppress inflammatory pathways that mediate inflammatory bone loss outweighed their deleterious effects on bone metabolism. These bone sparing effects of GCs were mediated through the suppression of pro-inflammatory osteoclasts’ activation, both systemically and at sites of inflammation. However, whilst these treatments protected from inflammatory bone loss, we still observed a suppression of anabolic bone formation in all mice receiving GCs, suggesting that long term administration may still ultimately result in GIO.
Unlike bone, therapeutic GCs markedly exacerbated muscle wasting in mice with chronic inflammation. This was characterized by a marked activation of the catabolic FOXO1 and UPS pathways [80]. Similar findings had been reported in rats, where dexamethasone exacerbated inflammatory muscle wasting in models of sepsis [172]. These data indicate that the beneficial effects of inflammatory suppression by GCs in muscle were not sufficient to outweigh their deleterious actions on muscle metabolism. Whilst further work is required to better elucidate the actions of therapeutic GCs in the context of chronic inflammation, these data shed light on the potential strengths and weaknesses of their application in muscle and bone. In particular, they indicate that the management of side effects in muscle may need to be prioritised over those in bone, in patients with chronic inflammatory diseases receiving therapeutic GCs.
12. Pre-Receptor Regulation of Therapeutic GC Action to Protect against Side Effects
The pre-receptor metabolism of GCs by the 11β-hydroxysteroid dehydrogenase (11β-HSD) enzymes is recognised as a critical step in mediating GC signalling in many peripheral tissues. These are the 11β-HSD type 1 (11β-HSD1) and type 2 (11β-HSD2). 11β-HSD1 is expressed in many tissues, including the liver, bone, muscle and fat, where it converts inactive endogenous and therapeutic GCs (such as corticosterone and prednisone) to their active counterparts (such as cortisol and prednisolone), leading to a local accumulation and concentration of active GCs [173,174,175] (Figure 4). In contrast, 11β-HSD2 solely inactivates endogenous and therapeutic GCs within the kidney, providing circulating inactive GC substrate for the peripheral 11β-HSD1 enzyme and supporting renal clearance of GCs [175]. Several key studies have demonstrated a critical role for the pre-receptor activation of GCs by 11β-HSD1 in mediating the deleterious actions of therapeutic GCs in muscle and bone [176,177]. Here, animals with transgenic deletion of 11β-HSD1 are resistant to both exogenous GC induced muscle wasting and osteoporosis. This raises the exciting possibility that therapeutic 11β-HSD1 inhibitors, widely explored in the management of metabolic disease, may prevent bone loss and muscle wasting in patients with chronic inflammatory diseases receiving GCs [178,179]. Further studies lend strength to this concept, showing that 11β-HSD1 is potently upregulated within muscle cells and osteoblasts, where it is potently upregulated by circulating inflammatory cytokines such as TNF-α and IL-1β [174,180,181]. Despite this, caution should be applied in this context, given that systemic deletion of 11β-HSD1 can exacerbate disease activity in murine models of inflammation, secondary to a reduction in reactivation of endogenous GC at sites of inflammation [182,183]. Consequently, further studies are required to delineate the potential benefits and risks of 11β-HSD1 inhibition in chronic inflammatory disease.
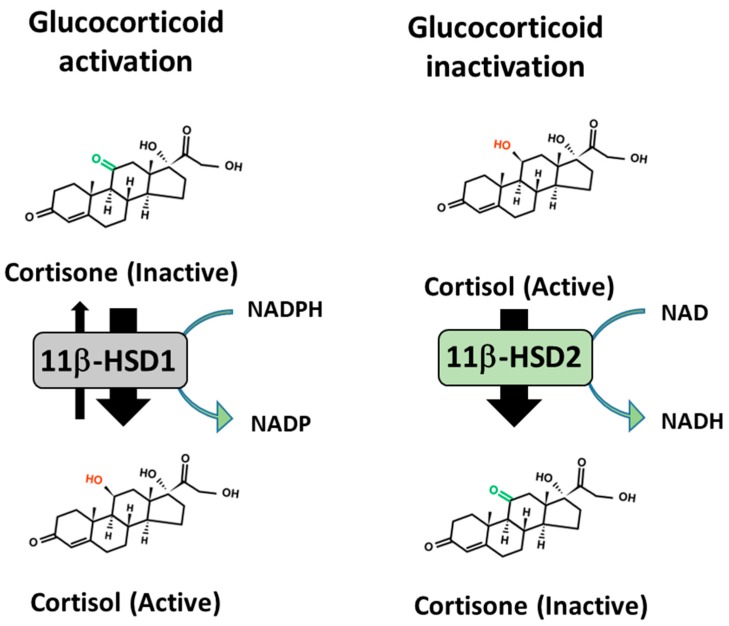
Figure 4.
Pre-receptor metabolism of GCs by 11β-HSD1. 11β-hydroxysteroid dehydrogenase (11β-HSD) type 1 is a bidirectional enzyme that predominantly reduces inactive GCs to their active counterparts in an NADPH dependent manner, whilst 11β-HSD type 2 is an NAD+ dependent unidirectional enzyme that converts active GCs to their inactive counterparts.
13. Conclusions
Both chronic inflammation and therapeutic GCs are potent drivers for systemic bone and muscle wasting resulting from an imbalance between anabolic and catabolic homeostasis. Whilst therapeutic GCs oppose many of the inflammatory pathways that drive bone and muscle wasting, they share common pathways that promote anti-anabolic and catabolic metabolism of bone and muscle and can drive or exacerbate these deleterious processes in chronic inflammatory disease. However, these relationships are invariably complicated by the nature of the inflammatory disease in which therapeutic GCs are utilized. Intriguingly, 11β-HSD1 inhibitors may possess the potential to prevent the deleterious actions of therapeutic GCs in the backdrop of chronic inflammation. However, further studies are required to assess their efficacy and safety in this context.
Acknowledgments
This review was supported by the Arthritis Research UK grant, Versus Arthritis: 20843.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Clayton S.A., Jones S.W., Kurowska-Stolarska M., Clark A.R. The role of microRNAs in glucocorticoid action. J. Biol. Chem. 2018;293:1865–1874. doi: 10.1074/jbc.R117.000366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Abraham S.M., Lawrence T., Kleiman A., Warden P., Medghalchi M., Tuckermann J., Saklatvala J., Clark A.R. Antiinflammatory effects of dexamethasone are partly dependent on induction of dual specificity phosphatase 1. J. Exp. Med. 2006;203:1883–1889. doi: 10.1084/jem.20060336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marco B.D., Massetti M., Bruscoli S., Macchiarulo A., Virgilio R.D., Velardi E., Donato V., Migliorati G., Riccardi C. Glucocorticoid-induced leucine zipper (GILZ)/NF-kappaB interaction: Role of GILZ homo-dimerization and C-terminal domain. Nucleic Acids Res. 2007;35:517–528. doi: 10.1093/nar/gkl1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Klint E.A., Grundtman C., Engström M., Catrina A.I., Makrygiannakis D., Klareskog L., Andersson U., Ulfgren A.K. Intraarticular glucocorticoid treatment reduces inflammation in synovial cell infiltrations more efficiently than in synovial blood vessels. Arthritis Rheum. 2005;52:3880–3889. doi: 10.1002/art.21488. [DOI] [PubMed] [Google Scholar]
- 5.Gilmour J.S., Coutinho A.E., Cailhier J.F., Man T.Y., Clay M., Thomas G., Harris H.J., Mullins J.J., Seckl J.R., Savill J.S., et al. Local amplification of glucocorticoids by 11 beta-hydroxysteroid dehydrogenase type 1 promotes macrophage phagocytosis of apoptotic leukocytes. J. Immunol. 2006;176:7605–7611. doi: 10.4049/jimmunol.176.12.7605. [DOI] [PubMed] [Google Scholar]
- 6.Fardet L., Flahault A., Kettaneh A., Tiev K.P., Généreau T., Tolédano C., Lebbé C., Cabane J. Corticosteroid-induced clinical adverse events: Frequency, risk factors and patient’s opinion. Br. J. Dermatol. 2007;157:142–148. doi: 10.1111/j.1365-2133.2007.07950.x. [DOI] [PubMed] [Google Scholar]
- 7.Feldstein A.C., Elmer P.J., Nichols G.A., Herson M. Practice patterns in patients at risk for glucocorticoid-induced osteoporosis. Osteoporos. Int. 2005;16:2168–2174. doi: 10.1007/s00198-005-2016-z. [DOI] [PubMed] [Google Scholar]
- 8.Strehl C., Bijlsma J.W., de Wit M., Boers M., Caeyers N., Cutolo M., Dasgupta B., Dixon W.G., Geenen R., Huizinga T.W., et al. Defining conditions where long-term glucocorticoid treatment has an acceptably low level of harm to facilitate implementation of existing recommendations: Viewpoints from an EULAR task force. Ann. Rheum. Dis. 2016;75:952–957. doi: 10.1136/annrheumdis-2015-208916. [DOI] [PubMed] [Google Scholar]
- 9.Löfberg E., Gutierrez A., Wernerman J., Anderstam B., Mitch W.E., Price S.R., Bergström J., Alvestrand A. Effects of high doses of glucocorticoids on free amino acids, ribosomes and protein turnover in human muscle. Eur. J. Clin. Investig. 2002;32:345–353. doi: 10.1046/j.1365-2362.2002.00993.x. [DOI] [PubMed] [Google Scholar]
- 10.Qi D., Pulinilkunnil T., An D., Ghosh S., Abrahani A., Pospisilik J.A., Brownsey R., Wambolt R., Allard M., Rodrigues B. Single-dose dexamethasone induces whole-body insulin resistance and alters both cardiac fatty acid and carbohydrate metabolism. Diabetes. 2004;53:1790–1797. doi: 10.2337/diabetes.53.7.1790. [DOI] [PubMed] [Google Scholar]
- 11.Wu B., Li P., Liu Y., Lou Z., Ding Y., Shu C., Ye S., Bartlam M., Shen B., Rao Z. 3D structure of human FK506-binding protein 52: Implications for the assembly of the glucocorticoid receptor/Hsp90/immunophilin heterocomplex. Proc. Natl. Acad. Sci. USA. 2004;101:8348–8353. doi: 10.1073/pnas.0305969101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barnes P.J. How corticosteroids control inflammation: Quintiles Prize Lecture 2005. Br. J. Pharmacol. 2006;148:245–254. doi: 10.1038/sj.bjp.0706736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reichardt H.M., Tuckermann J.P., Göttlicher M., Vujic M., Weih F., Angel P., Herrlich P., Schütz G. Repression of inflammatory responses in the absence of DNA binding by the glucocorticoid receptor. EMBO J. 2001;20:7168–7173. doi: 10.1093/emboj/20.24.7168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schäcke H., Schottelius A., Döcke W.D., Strehlke P., Jaroch S., Schmees N., Rehwinkel H., Hennekes H., Asadullah K. Dissociation of transactivation from transrepression by a selective glucocorticoid receptor agonist leads to separation of therapeutic effects from side effects. Proc. Natl. Acad. Sci. USA. 2004;101:227–232. doi: 10.1073/pnas.0300372101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Reichardt H.M., Kaestner K.H., Tuckermann J., Kretz O., Wessely O., Bock R., Gass P., Schmid W., Herrlich P., Angel P., et al. DNA Binding of the Glucocorticoid Receptor Is Not Essential for Survival. Cell. 1998;93:531–541. doi: 10.1016/S0092-8674(00)81183-6. [DOI] [PubMed] [Google Scholar]
- 16.Koenen M., Culemann S., Vettorazzi S., Caratti G., Frappart L., Baum W., Krönke G., Baschant U., Tuckermann J.P. Glucocorticoid receptor in stromal cells is essential for glucocorticoid-mediated suppression of inflammation in arthritis. Ann. Rheum. Dis. 2018;77:1610–1618. doi: 10.1136/annrheumdis-2017-212762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Scheschowitsch K., Leite J.A., Assreuy J. New Insights in Glucocorticoid Receptor Signaling-More Than Just a Ligand-Binding Receptor. Front. Endocrinol. 2017;8:16. doi: 10.3389/fendo.2017.00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Abbinante-Nissen J.M., Simpson L.G., Leikauf G.D. Corticosteroids increase secretory leukocyte protease inhibitor transcript levels in airway epithelial cells. Am. J. Physiol. 1995;268 Pt 1:L601–L606. doi: 10.1152/ajplung.1995.268.4.L601. [DOI] [PubMed] [Google Scholar]
- 19.Manetsch M., Ramsay E.E., King E.M., Seidel P., Che W., Ge Q., Hibbs D.E., Newton R., Ammit A.J. Corticosteroids and β₂-agonists upregulate mitogen-activated protein kinase phosphatase 1: In vitro mechanisms. Br. J. Pharmacol. 2012;166:2049–2059. doi: 10.1111/j.1476-5381.2012.01923.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang J.C., Derynck M.K., Nonaka D.F., Khodabakhsh D.B., Haqq C., Yamamoto K.R. Chromatin immunoprecipitation (ChIP) scanning identifies primary glucocorticoid receptor target genes. Proc. Natl. Acad. Sci. USA. 2004;101:15603–15608. doi: 10.1073/pnas.0407008101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smoak K., Cidlowski J.A. Glucocorticoids regulate tristetraprolin synthesis and posttranscriptionally regulate tumor necrosis factor alpha inflammatory signaling. Mol. Cell. Biol. 2006;26:9126–9135. doi: 10.1128/MCB.00679-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu T., Zhang L., Joo D., Sun S.-C. NF-κB signaling in inflammation. Signal Transduct. Target. Ther. 2017;2:17023. doi: 10.1038/sigtrans.2017.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Frost H.M. Skeletal structural adaptations to mechanical usage (SATMU): 2. Redefining Wolff’s law: The remodeling problem. Anat. Rec. 1990;226:414–422. doi: 10.1002/ar.1092260403. [DOI] [PubMed] [Google Scholar]
- 24.Burra S., Nicolella D.P., Francis W.L., Freitas C.J., Mueschke N.J., Poole K., Jiang J.X. Dendritic processes of osteocytes are mechanotransducers that induce the opening of hemichannels. Proc. Natl. Acad. Sci. USA. 2010;107:13648–13653. doi: 10.1073/pnas.1009382107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Verborgt O., Tatton N.A., Majeska R.J., Schaffler M.B. Spatial distribution of Bax and Bcl-2 in osteocytes after bone fatigue: Complementary roles in bone remodeling regulation? J. Bone Miner. Res. 2002;17:907–914. doi: 10.1359/jbmr.2002.17.5.907. [DOI] [PubMed] [Google Scholar]
- 26.Aguirre J.I., Plotkin L.I., Stewart S.A., Weinstein R.S., Parfitt A.M., Manolagas S.C., Bellido T. Osteocyte apoptosis is induced by weightlessness in mice and precedes osteoclast recruitment and bone loss. J. Bone Miner. Res. 2006;21:605–615. doi: 10.1359/jbmr.060107. [DOI] [PubMed] [Google Scholar]
- 27.Al-Dujaili S.A., Lau E., Al-Dujaili H., Tsang K., Guenther A., You L. Apoptotic osteocytes regulate osteoclast precursor recruitment and differentiation in vitro. J. Cell. Biochem. 2011;112:2412–2423. doi: 10.1002/jcb.23164. [DOI] [PubMed] [Google Scholar]
- 28.Takayanagi H., Kim S., Koga T., Nishina H., Isshiki M., Yoshida H., Saiura A., Isobe M., Yokochi T., Inoue J.I., et al. Induction and activation of the transcription factor NFATc1 (NFAT2) integrate RANKL signaling in terminal differentiation of osteoclasts. Dev. Cell. 2002;3:889–901. doi: 10.1016/S1534-5807(02)00369-6. [DOI] [PubMed] [Google Scholar]
- 29.Kukita T., Wada N., Kukita A., Kakimoto T., Sandra F., Toh K., Nagata K., Iijima T., Horiuchi M., Matsusaki H., et al. RANKL-induced DC-STAMP is essential for osteoclastogenesis. J. Exp. Med. 2004;200:941–946. doi: 10.1084/jem.20040518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wu H., Xu G., Li Y.P. Atp6v0d2 is an essential component of the osteoclast-specific proton pump that mediates extracellular acidification in bone resorption. J. Bone Miner. Res. 2009;24:871–885. doi: 10.1359/jbmr.081239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Väänänen H.K., Karhukorpi E.K., Sundquist K., Wallmark B., Roininen I., Hentunen T., Tuukkanen J., Lakkakorpi P. Evidence for the presence of a proton pump of the vacuolar H(+)-ATPase type in the ruffled borders of osteoclasts. J. Cell Biol. 1990;111:1305–1311. doi: 10.1083/jcb.111.3.1305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Blair H.C., Schlesinger P.H. Purification of a stilbene sensitive chloride channel and reconstitution of chloride conductivity into phospholipid vesicles. Biochem. Biophys. Res. Commun. 1990;171:920–925. doi: 10.1016/0006-291X(90)90771-E. [DOI] [PubMed] [Google Scholar]
- 33.Tang Y., Wu X., Lei W., Pang L., Wan C., Shi Z., Zhao L., Nagy T.R., Peng X., Hu J., et al. TGF-beta1-induced migration of bone mesenchymal stem cells couples bone resorption with formation. Nat. Med. 2009;15:757–765. doi: 10.1038/nm.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Xian L., Wu X., Pang L., Lou M., Rosen C.J., Qiu T., Crane J., Frassica F., Zhang L., Rodriguez J.P., et al. Matrix IGF-1 maintains bone mass by activation of mTOR in mesenchymal stem cells. Nat. Med. 2012;18:1095–1101. doi: 10.1038/nm.2793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Poole K.E., van Bezooijen R.L., Loveridge N., Hamersma H., Papapoulos S.E., Löwik C.W., Reeve J. Sclerostin is a delayed secreted product of osteocytes that inhibits bone formation. FASEB J. 2005;19:1842–1844. doi: 10.1096/fj.05-4221fje. [DOI] [PubMed] [Google Scholar]
- 36.Ducy P., Zhang R., Geoffroy V., Ridall A.L., Karsenty G. Osf2/Cbfa1: A transcriptional activator of osteoblast differentiation. Cell. 1997;89:747–754. doi: 10.1016/S0092-8674(00)80257-3. [DOI] [PubMed] [Google Scholar]
- 37.Roca H., Phimphilai M., Gopalakrishnan R., Xiao G., Franceschi R.T. Cooperative interactions between RUNX2 and homeodomain protein-binding sites are critical for the osteoblast-specific expression of the bone sialoprotein gene. J. Biol. Chem. 2005;280:30845–30855. doi: 10.1074/jbc.M503942200. [DOI] [PubMed] [Google Scholar]
- 38.Cao J., Venton L., Sakata T., Halloran B.P. Expression of RANKL and OPG correlates with age-related bone loss in male C57BL/6 mice. J. Bone Miner. Res. 2003;18:270–277. doi: 10.1359/jbmr.2003.18.2.270. [DOI] [PubMed] [Google Scholar]
- 39.Andersen T.L., Abdelgawad M.E., Kristensen H.B., Hauge E.M., Rolighed L., Bollerslev J., Kjærsgaard-Andersen P., Delaisse J.M. Understanding coupling between bone resorption and formation: Are reversal cells the missing link? Am. J. Pathol. 2013;183:235–246. doi: 10.1016/j.ajpath.2013.03.006. [DOI] [PubMed] [Google Scholar]
- 40.Cowles E.A., DeRome M.E., Pastizzo G., Brailey L.L., Gronowicz G.A. Mineralization and the expression of matrix proteins during in vivo bone development. Calcif. Tissue Int. 1998;62:74–82. doi: 10.1007/s002239900397. [DOI] [PubMed] [Google Scholar]
- 41.Weiner S. Organization of extracellularly mineralized tissues: A comparative study of biological crystal growth. CRC Crit. Rev. Biochem. 1986;20:365–408. doi: 10.3109/10409238609081998. [DOI] [PubMed] [Google Scholar]
- 42.Orimo H. The mechanism of mineralization and the role of alkaline phosphatase in health and disease. J. Nippon Med. Sch. 2010;77:4–12. doi: 10.1272/jnms.77.4. [DOI] [PubMed] [Google Scholar]
- 43.Haugeberg G., Orstavik R.E., Uhlig T., Falch J.A., Halse J.I., Kvien T.K. Bone loss in patients with rheumatoid arthritis: Results from a population-based cohort of 366 patients followed up for two years. Arthritis Rheum. 2002;46:1720–1728. doi: 10.1002/art.10408. [DOI] [PubMed] [Google Scholar]
- 44.Walker-Bone K. Recognizing and treating secondary osteoporosis. Nat. Rev. Rheumatol. 2012;8:480–492. doi: 10.1038/nrrheum.2012.93. [DOI] [PubMed] [Google Scholar]
- 45.Tack G.J., Verbeek W.H., Schreurs M.W., Mulder C.J. The spectrum of celiac disease: Epidemiology, clinical aspects and treatment. Nat. Rev. Gastroenterol. Hepatol. 2010;7:204–213. doi: 10.1038/nrgastro.2010.23. [DOI] [PubMed] [Google Scholar]
- 46.Graat-Verboom L., Spruit M.A., van den Borne B.E., Smeenk F.W., Martens E.J., Lunde R., Wouters E.F. Correlates of osteoporosis in chronic obstructive pulmonary disease: An underestimated systemic component. Respir. Med. 2009;103:1143–1151. doi: 10.1016/j.rmed.2009.02.014. [DOI] [PubMed] [Google Scholar]
- 47.Ding C., Parameswaran V., Udayan R., Burgess J., Jones G. Circulating levels of inflammatory markers predict change in bone mineral density and resorption in older adults: A longitudinal study. J. Clin. Endocrinol. Metab. 2008;93:1952–1958. doi: 10.1210/jc.2007-2325. [DOI] [PubMed] [Google Scholar]
- 48.Barbour K.E., Lui L.Y., Ensrud K.E., Hillier T.A., LeBlanc E.S., Ing S.W., Hochberg M.C., Cauley J.A. Study of Osteoporotic Fractures (SOF) Research Group. Inflammatory markers and risk of hip fracture in older white women: The study of osteoporotic fractures. J. Bone Miner. Res. 2014;29:2057–2064. doi: 10.1002/jbmr.2245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Barbour K.E., Boudreau R., Danielson M.E., Youk A.O., Wactawski-Wende J., Greep N.C., LaCroix A.Z., Jackson R.D., Wallace R.B., Bauer D.C., et al. Inflammatory markers and the risk of hip fracture: The Women’s Health Initiative. J. Bone Miner. Res. 2012;27:1167–1176. doi: 10.1002/jbmr.1559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pasco J.A., Kotowicz M.A., Henry M.J., Nicholson G.C., Spilsbury H.J., Box J.D., Schneider H.G. High-sensitivity C-reactive protein and fracture risk in elderly women. JAMA. 2006;296:1353–1355. doi: 10.1001/jama.296.11.1353. [DOI] [PubMed] [Google Scholar]
- 51.Hardy R., Cooper M.S. Bone loss in inflammatory disorders. J. Endocrinol. 2009;201:309. doi: 10.1677/JOE-08-0568. [DOI] [PubMed] [Google Scholar]
- 52.Wei S., Kitaura H., Zhou P., Ross F.P., Teitelbaum S.L. IL-1 mediates TNF-induced osteoclastogenesis. J. Clin. Investig. 2005;115:282–290. doi: 10.1172/JCI200523394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Palmqvist P., Persson E., Conaway H.H., Lerner U.H. IL-6, leukemia inhibitory factor, and oncostatin M stimulate bone resorption and regulate the expression of receptor activator of NF-kappa B ligand, osteoprotegerin, and receptor activator of NF-kappa B in mouse calvariae. J. Immunol. 2002;169:3353–3362. doi: 10.4049/jimmunol.169.6.3353. [DOI] [PubMed] [Google Scholar]
- 54.Yoshitake F., Itoh S., Narita H., Ishihara K., Ebisu S. Interleukin-6 directly inhibits osteoclast differentiation by suppressing receptor activator of NF-kappaB signaling pathways. J. Biol. Chem. 2008;283:11535–11540. doi: 10.1074/jbc.M607999200. [DOI] [PubMed] [Google Scholar]
- 55.Kotake S., Udagawa N., Takahashi N., Matsuzaki K., Itoh K., Ishiyama S., Saito S., Inoue K., Kamatani N., Gillespie M.T., et al. IL-17 in synovial fluids from patients with rheumatoid arthritis is a potent stimulator of osteoclastogenesis. J. Clin. Investig. 1999;103:1345–1352. doi: 10.1172/JCI5703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ragab A.A., Nalepka J.L., Bi Y., Greenfield E.M. Cytokines synergistically induce osteoclast differentiation: Support by immortalized or normal calvarial cells. Am. J. Physiol. Cell Physiol. 2002;283:C679–C687. doi: 10.1152/ajpcell.00421.2001. [DOI] [PubMed] [Google Scholar]
- 57.Kawai T., Matsuyama T., Hosokawa Y., Makihira S., Seki M., Karimbux N.Y., Goncalves R.B., Valverde P., Dibart S., Li Y.P., et al. B and T lymphocytes are the primary sources of RANKL in the bone resorptive lesion of periodontal disease. Am. J. Pathol. 2006;169:987–998. doi: 10.2353/ajpath.2006.060180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sato K., Suematsu A., Okamoto K., Yamaguchi A., Morishita Y., Kadono Y., Tanaka S., Kodama T., Akira S., Iwakura Y., et al. Th17 functions as an osteoclastogenic helper T cell subset that links T cell activation and bone destruction. J. Exp. Med. 2006;203:2673–2682. doi: 10.1084/jem.20061775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Takayanagi H., Ogasawara K., Hida S., Chiba T., Murata S., Sato K., Takaoka A., Yokochi T., Oda H., Tanaka K., et al. T-cell-mediated regulation of osteoclastogenesis by signalling cross-talk between RANKL and IFN-gamma. Nature. 2000;408:600–605. doi: 10.1038/35046102. [DOI] [PubMed] [Google Scholar]
- 60.Rifas L., Weitzmann M.N. A novel T cell cytokine, secreted osteoclastogenic factor of activated T cells, induces osteoclast formation in a RANKL-independent manner. Arthritis Rheum. 2009;60:3324–3335. doi: 10.1002/art.24877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Abbas S., Zhang Y.H., Clohisy J.C., Abu-Amer Y. Tumor necrosis factor-alpha inhibits pre-osteoblast differentiation through its type-1 receptor. Cytokine. 2003;22:33–41. doi: 10.1016/S1043-4666(03)00106-6. [DOI] [PubMed] [Google Scholar]
- 62.Jilka R.L., Weinstein R.S., Bellido T., Parfitt A.M., Manolagas S.C. Osteoblast Programmed Cell Death (Apoptosis): Modulation by Growth Factors and Cytokines. J. Bone Miner. Res. 1998;13:793–802. doi: 10.1359/jbmr.1998.13.5.793. [DOI] [PubMed] [Google Scholar]
- 63.Kaneshiro S., Ebina K., Shi K., Higuchi C., Hirao M., Okamoto M., Koizumi K., Morimoto T., Yoshikawa H., Hashimoto J. IL-6 negatively regulates osteoblast differentiation through the SHP2/MEK2 and SHP2/Akt2 pathways in vitro. J. Bone Miner. Metab. 2014;32:378–392. doi: 10.1007/s00774-013-0514-1. [DOI] [PubMed] [Google Scholar]
- 64.Redlich K., Görtz B., Hayer S., Zwerina J., Doerr N., Kostenuik P., Bergmeister H., Kollias G., Steiner G., Smolen J.S., et al. Repair of local bone erosions and reversal of systemic bone loss upon therapy with anti-tumor necrosis factor in combination with osteoprotegerin or parathyroid hormone in tumor necrosis factor-mediated arthritis. Am. J. Pathol. 2004;164:543–555. doi: 10.1016/S0002-9440(10)63144-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.van Staa T.P., Leufkens H.G., Cooper C. The epidemiology of corticosteroid-induced osteoporosis: A meta-analysis. Osteoporos. Int. 2002;13:777–787. doi: 10.1007/s001980200108. [DOI] [PubMed] [Google Scholar]
- 66.Weinstein R.S., Jilka R.L., Parfitt A.M., Manolagas S.C. Inhibition of osteoblastogenesis and promotion of apoptosis of osteoblasts and osteocytes by glucocorticoids. Potential mechanisms of their deleterious effects on bone. J. Clin. Investig. 1998;102:274–282. doi: 10.1172/JCI2799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zhou H., Mak W., Zheng Y., Dunstan C.R., Seibel M.J. Osteoblasts directly control lineage commitment of mesenchymal progenitor cells through Wnt signaling. J. Biol. Chem. 2008;283:1936–1945. doi: 10.1074/jbc.M702687200. [DOI] [PubMed] [Google Scholar]
- 68.Mak W., Shao X., Dunstan C.R., Seibel M.J., Zhou H. Biphasic glucocorticoid-dependent regulation of Wnt expression and its inhibitors in mature osteoblastic cells. Calcif. Tissue Int. 2009;85:538–545. doi: 10.1007/s00223-009-9303-1. [DOI] [PubMed] [Google Scholar]
- 69.O’Brien C.A., Jia D., Plotkin L.I., Bellido T., Powers C.C., Stewart S.A., Manolagas S.C., Weinstein R.S. Glucocorticoids act directly on osteoblasts and osteocytes to induce their apoptosis and reduce bone formation and strength. Endocrinology. 2004;145:1835–1841. doi: 10.1210/en.2003-0990. [DOI] [PubMed] [Google Scholar]
- 70.Brunetti G., Faienza M.F., Piacente L., Ventura A., Oranger A., Carbone C., Benedetto A.D., Colaianni G., Gigante M., Mori G., et al. High dickkopf-1 levels in sera and leukocytes from children with 21-hydroxylase deficiency on chronic glucocorticoid treatment. Am. J. Physiol. Endocrinol. Metab. 2013;304:E546–E554. doi: 10.1152/ajpendo.00535.2012. [DOI] [PubMed] [Google Scholar]
- 71.Rauch A., Seitz S., Baschant U., Schilling A.F., Illing A., Stride B., Kirilov M., Takacz A., Schmidt-Ullrich R., Ostermay S., et al. Glucocorticoids suppress bone formation by attenuating osteoblast differentiation via the monomeric glucocorticoid receptor. Cell Metab. 2010;11:517–531. doi: 10.1016/j.cmet.2010.05.005. [DOI] [PubMed] [Google Scholar]
- 72.Jia D., O’Brien C.A., Stewart S.A., Manolagas S.C., Weinstein R.S. Glucocorticoids act directly on osteoclasts to increase their life span and reduce bone density. Endocrinology. 2006;147:5592–5599. doi: 10.1210/en.2006-0459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Rubin J., Biskobing D.M., Jadhav L., Fan D., Nanes M.S., Perkins S., Fan X. Dexamethasone promotes expression of membrane-bound macrophage colony-stimulating factor in murine osteoblast-like cells. Endocrinology. 1998;139:1006–1012. doi: 10.1210/endo.139.3.5778. [DOI] [PubMed] [Google Scholar]
- 74.Swanson C., Lorentzon M., Conaway H.H., Lerner U.H. Glucocorticoid Regulation of Osteoclast Differentiation and Expression of Receptor Activator of Nuclear Factor-κB (NF-κB) Ligand, Osteoprotegerin, and Receptor Activator of NF-κB in Mouse Calvarial Bones. Endocrinology. 2006;147:3613–3622. doi: 10.1210/en.2005-0717. [DOI] [PubMed] [Google Scholar]
- 75.Hofbauer L.C., Gori F., Riggs B.L., Lacey D.L., Dunstan C.R., Spelsberg T.C., Khosla S. Stimulation of osteoprotegerin ligand and inhibition of osteoprotegerin production by glucocorticoids in human osteoblastic lineage cells: Potential paracrine mechanisms of glucocorticoid-induced osteoporosis. Endocrinology. 1999;140:4382–4389. doi: 10.1210/endo.140.10.7034. [DOI] [PubMed] [Google Scholar]
- 76.Humphrey E.L., Williams J.H., Davie M.W., Marshall M.J. Effects of dissociated glucocorticoids on OPG and RANKL in osteoblastic cells. Bone. 2006;38:652–661. doi: 10.1016/j.bone.2005.10.004. [DOI] [PubMed] [Google Scholar]
- 77.Faienza M.F., Brunetti G., Colucci S., Piacente L., Ciccarelli M., Giordani L., Del Vecchio G.C., D’Amore M., Albanese L., Cavallo L., et al. Osteoclastogenesis in children with 21-hydroxylase deficiency on long-term glucocorticoid therapy: The role of receptor activator of nuclear factor-kappaB ligand/osteoprotegerin imbalance. J. Clin. Endocrinol. Metab. 2009;94:2269–2276. doi: 10.1210/jc.2008-2446. [DOI] [PubMed] [Google Scholar]
- 78.Chen J., Yoon S.H., Grynpas M.D., Mitchell J. Pre-treatment with Pamidronate Improves Bone Mechanical Properties in Mdx Mice Treated with Glucocorticoids. Calcif. Tissue Int. 2019;104:182–192. doi: 10.1007/s00223-018-0482-5. [DOI] [PubMed] [Google Scholar]
- 79.Kim H.J., Zhao H., Kitaura H., Bhattacharyya S., Brewer J.A., Muglia L.J., Ross F.P., Teitelbaum S.L. Glucocorticoids suppress bone formation via the osteoclast. J. Clin. Investig. 2006;116:2152–2160. doi: 10.1172/JCI28084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Fenton C.G., Webster J.M., Martin C.S., Fareed S., Wehmeyer C., Mackie H., Jones R., Seabright A.P., Lewis J.W., Lai Y.C., et al. Therapeutic glucocorticoids prevent bone loss but drive muscle wasting when administered in chronic polyarthritis. Arthritis Res. Ther. 2019;21:182. doi: 10.1186/s13075-019-1962-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Güler-Yüksel M., Bijsterbosch J., Goekoop-Ruiterman Y.P.M., de Vries-Bouwstra J.K., Hulsmans H.M.J., de Beus W.M., Han K.H., Breedveld F.C., Dijkmans B.A.C., Allaart C.F., et al. Changes in bone mineral density in patients with recent onset, active rheumatoid arthritis. Ann. Rheum. Dis. 2008;67:823–828. doi: 10.1136/ard.2007.073817. [DOI] [PubMed] [Google Scholar]
- 82.Sambrook P.N., Cohen M.L., Eisman J.A., Pocock N.A., Champion G.D., Yeates M.G. Effects of low dose corticosteroids on bone mass in rheumatoid arthritis: A longitudinal study. Ann. Rheum. Dis. 1989;48:535–538. doi: 10.1136/ard.48.7.535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Sambrook P.N., Eisman J.A., Yeates M.G., Pocock N.A., Eberl S., Champion G.D. Osteoporosis in rheumatoid arthritis: Safety of low dose corticosteroids. Ann. Rheum. Dis. 1986;45:950–953. doi: 10.1136/ard.45.11.950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Wijbrandts C.A., Klaasen R., Dijkgraaf M.G.W., Gerlag D.M., van Eck-Smit B.L.F., Tak P.P. Bone mineral density in rheumatoid arthritis patients 1 year after adalimumab therapy: Arrest of bone loss. Ann. Rheum. Dis. 2009;68:373–376. doi: 10.1136/ard.2008.091611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Haugeberg G., Uhlig T., Falch J.A., Halse J.I., Kvien T.K. Bone mineral density and frequency of osteoporosis in female patients with rheumatoid arthritis: Results from 394 patients in the Oslo County rheumatoid arthritis register. Arthritis Rheum. 2000;43:522–530. doi: 10.1002/1529-0131(200003)43:3<522::AID-ANR7>3.0.CO;2-Y. [DOI] [PubMed] [Google Scholar]
- 86.Pereira R.M., Corrente J.E., Chahade W.H., Yoshinari N.H. Evaluation by dual X-ray absorptiometry (DXA) of bone mineral density in children with juvenile chronic arthritis. Clin. Exp. Rheumatol. 1998;16:495–501. [PubMed] [Google Scholar]
- 87.Varonos S., Ansell B.M., Reeve J. Vertebral collapse in juvenile chronic arthritis: Its relationship with glucocorticoid therapy. Calcif. Tissue Int. 1987;41:75–78. doi: 10.1007/BF02555248. [DOI] [PubMed] [Google Scholar]
- 88.Bergström J., Hermansen L., Hultman E., Saltin B. Diet, Muscle Glycogen and Physical Performance. Acta Physiol. Scand. 1967;71:140–150. doi: 10.1111/j.1748-1716.1967.tb03720.x. [DOI] [PubMed] [Google Scholar]
- 89.Coleman M.E., DeMayo F., Yin K.C., Lee H.M., Geske R., Montgomery C., Schwartz R.J. Myogenic vector expression of insulin-like growth factor I stimulates muscle cell differentiation and myofiber hypertrophy in transgenic mice. J. Biol. Chem. 1995;270:12109–12116. doi: 10.1074/jbc.270.20.12109. [DOI] [PubMed] [Google Scholar]
- 90.Lai K.M.V., Gonzalez M., Poueymirou W.T., Kline W.O., Na E., Zlotchenko E., Stitt T.N., Economides A.N., Yancopoulos G.D., Glass D.J. Conditional activation of akt in adult skeletal muscle induces rapid hypertrophy. Mol. Cell. Biol. 2004;24:9295–9304. doi: 10.1128/MCB.24.21.9295-9304.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Harwood A.J. Regulation of GSK-3: A Cellular Multiprocessor. Cell. 2001;105:821–824. doi: 10.1016/S0092-8674(01)00412-3. [DOI] [PubMed] [Google Scholar]
- 92.Schiaffino S., Mammucari C. Regulation of skeletal muscle growth by the IGF1-Akt/PKB pathway: Insights from genetic models. Skelet. Muscle. 2011;1:4. doi: 10.1186/2044-5040-1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Booth F.W., Tseng B.S., FlÜCk M., Carson J.A. Molecular and cellular adaptation of muscle in response to physical training. Acta Physiol. Scand. 1998;162:343–350. doi: 10.1046/j.1365-201X.1998.0326e.x. [DOI] [PubMed] [Google Scholar]
- 94.Pallafacchina G., Calabria E., Serrano A.L., Kalhovde J.M., Schiaffino S. A protein kinase B-dependent and rapamycin-sensitive pathway controls skeletal muscle growth but not fiber type specification. Proc. Nat. Acad. Sci. USA. 2002;99:9213–9218. doi: 10.1073/pnas.142166599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Brunn G.J., Hudson C.C., Sekulić A., Williams J.M., Hosoi H., Houghton P.J., Lawrence J.C., Abraham R.T. Phosphorylation of the Translational Repressor PHAS-I by the Mammalian Target of Rapamycin. Science. 1997;277:99. doi: 10.1126/science.277.5322.99. [DOI] [PubMed] [Google Scholar]
- 96.Gingras A.C., Raught B., Sonenberg N. eIF4 Initiation Factors: Effectors of mRNA Recruitment to Ribosomes and Regulators of Translation. Annu. Rev. Biochem. 1999;68:913–963. doi: 10.1146/annurev.biochem.68.1.913. [DOI] [PubMed] [Google Scholar]
- 97.Ma X.M., Blenis J. Molecular mechanisms of mTOR-mediated translational control. Nat. Rev. Mol. Cell Biol. 2009;10:307–318. doi: 10.1038/nrm2672. [DOI] [PubMed] [Google Scholar]
- 98.Hardt Stefan E., Tomita H., Katus Hugo A., Sadoshima J. Phosphorylation of Eukaryotic Translation Initiation Factor 2Bε by Glycogen Synthase Kinase-3β Regulates β-Adrenergic Cardiac Myocyte Hypertrophy. Circ. Res. 2004;94:926–935. doi: 10.1161/01.RES.0000124977.59827.80. [DOI] [PubMed] [Google Scholar]
- 99.Rommel C., Bodine S.C., Clarke B.A., Rossman R., Nunez L., Stitt T.N., Yancopoulos G.D., Glass D.J. Mediation of IGF-1-induced skeletal myotube hypertrophy by PI(3)K/Akt/mTOR and PI(3)K/Akt/GSK3 pathways. Nat. Cell Biol. 2001;3:1009–1013. doi: 10.1038/ncb1101-1009. [DOI] [PubMed] [Google Scholar]
- 100.Cross D.A., Alessi D.R., Cohen P., Andjelkovich M., Hemmings B.A. Inhibition of glycogen synthase kinase-3 by insulin mediated by protein kinase B. Nature. 1995;378:785–789. doi: 10.1038/378785a0. [DOI] [PubMed] [Google Scholar]
- 101.Latres E., Amini A.R., Amini A.A., Griffiths J., Martin F.J., Wei Y., Lin H.C., Yancopoulos G.D., Glass D.J. Insulin-like Growth Factor-1 (IGF-1) Inversely Regulates Atrophy-induced Genes via the Phosphatidylinositol 3-Kinase/Akt/Mammalian Target of Rapamycin (PI3K/Akt/mTOR) Pathway. J. Biol. Chem. 2005;280:2737–2744. doi: 10.1074/jbc.M407517200. [DOI] [PubMed] [Google Scholar]
- 102.Sandri M., Sandri C., Gilbert A., Skurk C., Calabria E., Picard A., Walsh K., Schiaffino S., Lecker S.H., Goldberg A.L. Foxo transcription factors induce the atrophy-related ubiquitin ligase atrogin-1 and cause skeletal muscle atrophy. Cell. 2004;117:399–412. doi: 10.1016/S0092-8674(04)00400-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Calnan D.R., Brunet A. The FoxO code. Oncogene. 2008;27:2276–2288. doi: 10.1038/onc.2008.21. [DOI] [PubMed] [Google Scholar]
- 104.Brunet A., Bonni A., Zigmond M.J., Lin M.Z., Juo P., Hu L.S., Anderson M.J., Arden K.C., Blenis J., Greenberg M.E. Akt Promotes Cell Survival by Phosphorylating and Inhibiting a Forkhead Transcription Factor. Cell. 1999;96:857–868. doi: 10.1016/S0092-8674(00)80595-4. [DOI] [PubMed] [Google Scholar]
- 105.Mammucari C., Milan G., Romanello V., Masiero E., Rudolf R., Del Piccolo P., Burden S.J., Di Lisi R., Sandri C., Zhao J., et al. FoxO3 Controls Autophagy in Skeletal Muscle In Vivo. Cell Metab. 2007;6:458–471. doi: 10.1016/j.cmet.2007.11.001. [DOI] [PubMed] [Google Scholar]
- 106.Sandri M. Autophagy in skeletal muscle. FEBS Lett. 2010;584:1411–1416. doi: 10.1016/j.febslet.2010.01.056. [DOI] [PubMed] [Google Scholar]
- 107.Stitt T.N., Drujan D., Clarke B.A., Panaro F., Timofeyva Y., Kline W.O., Gonzalez M., Yancopoulos G.D., Glass D.J. The IGF-1/PI3K/Akt pathway prevents expression of muscle atrophy-induced ubiquitin ligases by inhibiting FOXO transcription factors. Mol. Cell. 2004;14:395–403. doi: 10.1016/S1097-2765(04)00211-4. [DOI] [PubMed] [Google Scholar]
- 108.Evenson A.R., Fareed M.U., Menconi M.J., Mitchell J.C., Hasselgren P.O. GSK-3beta inhibitors reduce protein degradation in muscles from septic rats and in dexamethasone-treated myotubes. Int. J. Biochem. Cell Biol. 2005;37:2226–2238. doi: 10.1016/j.biocel.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 109.Glickman M.H., Ciechanover A. The Ubiquitin-Proteasome Proteolytic Pathway: Destruction for the Sake of Construction. Physiol. Rev. 2002;82:373–428. doi: 10.1152/physrev.00027.2001. [DOI] [PubMed] [Google Scholar]
- 110.Hershko A., Ciechanover A. The ubiquitin system. Annu. Rev. Biochem. 1998;67:425–479. doi: 10.1146/annurev.biochem.67.1.425. [DOI] [PubMed] [Google Scholar]
- 111.Gomes M.D., Lecker S.H., Jagoe R.T., Navon A., Goldberg A.L. Atrogin-1, a muscle-specific F-box protein highly expressed during muscle atrophy. Proc. Natl. Acad. Sci. USA. 2001;98:14440–14445. doi: 10.1073/pnas.251541198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Bodine S.C., Latres E., Baumhueter S., Lai V.K.M., Nunez L., Clarke B.A., Poueymirou W.T., Panaro F.J., Na E., Dharmarajan K., et al. Identification of ubiquitin ligases required for skeletal muscle atrophy. Science. 2001;294:1704–1708. doi: 10.1126/science.1065874. [DOI] [PubMed] [Google Scholar]
- 113.Polge C., Heng A.E., Jarzaguet M., Ventadour S., Claustre A., Combaret L., Béchet D., Matondo M., Uttenweiler-Joseph S., Monsarrat B., et al. Muscle actin is polyubiquitinylated in vitro and in vivo and targeted for breakdown by the E3 ligase MuRF1. FASEB J. 2011;25:3790–3802. doi: 10.1096/fj.11-180968. [DOI] [PubMed] [Google Scholar]
- 114.Lokireddy S., Wijesoma I.W., Sze S.K., McFarlane C., Kambadur R., Sharma M. Identification of atrogin-1-targeted proteins during the myostatin-induced skeletal muscle wasting. Am. J. Physiol. Cell Physiol. 2012;303:C512–C529. doi: 10.1152/ajpcell.00402.2011. [DOI] [PubMed] [Google Scholar]
- 115.Csibi A., Cornille K., Leibovitch M.P., Poupon A., Tintignac L.A., Sanchez A.M., Leibovitch S.A. The translation regulatory subunit eIF3f controls the kinase-dependent mTOR signaling required for muscle differentiation and hypertrophy in mouse. PLoS ONE. 2010;5:e8994. doi: 10.1371/journal.pone.0008994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Lagirand-Cantaloube J., Cornille K., Csibi A., Batonnet-Pichon S., Leibovitch M.P., Leibovitch S.A. Inhibition of atrogin-1/MAFbx mediated MyoD proteolysis prevents skeletal muscle atrophy in vivo. PLoS ONE. 2009;4:e4973. doi: 10.1371/journal.pone.0004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Centner T., Yano J., Kimura E., McElhinny A.S., Pelin K., Witt C.C., Bang M.L., Trombitas K., Granzier H., Gregorio C.C., et al. Identification of muscle specific ring finger proteins as potential regulators of the titin kinase domain. J. Mol. Biol. 2001;306:717–726. doi: 10.1006/jmbi.2001.4448. [DOI] [PubMed] [Google Scholar]
- 118.Kedar V., McDonough H., Arya R., Li H.H., Rockman H.A., Patterson C. Muscle-specific RING finger 1 is a bona fide ubiquitin ligase that degrades cardiac troponin I. Proc. Natl. Acad. Sci. USA. 2004;101:18135–18140. doi: 10.1073/pnas.0404341102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Cohen S., Brault J.J., Gygi S.P., Glass D.J., Valenzuela D.M., Gartner C., Latres E., Goldberg A.L. During muscle atrophy, thick, but not thin, filament components are degraded by MuRF1-dependent ubiquitylation. J. Cell Biol. 2009;185:1083. doi: 10.1083/jcb.200901052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Mizushima N., Yamamoto A., Matsui M., Yoshimori T., Ohsumi Y. In Vivo Analysis of Autophagy in Response to Nutrient Starvation Using Transgenic Mice Expressing a Fluorescent Autophagosome Marker. Mol. Biol. Cell. 2003;15:1101–1111. doi: 10.1091/mbc.e03-09-0704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Hanna R.A., Quinsay M.N., Orogo A.M., Giang K., Rikka S., Gustafsson A.B. Microtubule-associated protein 1 light chain 3 (LC3) interacts with Bnip3 protein to selectively remove endoplasmic reticulum and mitochondria via autophagy. J. Biol. Chem. 2012;287:19094–19104. doi: 10.1074/jbc.M111.322933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Masiero E., Agatea L., Mammucari C., Blaauw B., Loro E., Komatsu M., Metzger D., Reggiani C., Schiaffino S., Sandri M. Autophagy Is Required to Maintain Muscle Mass. Cell Metab. 2009;10:507–515. doi: 10.1016/j.cmet.2009.10.008. [DOI] [PubMed] [Google Scholar]
- 123.Yu M., Wang H., Xu Y., Yu D., Li D., Liu X., Du W. Insulin-like growth factor-1 (IGF-1) promotes myoblast proliferation and skeletal muscle growth of embryonic chickens via the PI3K/Akt signalling pathway. Cell Biol. Int. 2015;39:910–922. doi: 10.1002/cbin.10466. [DOI] [PubMed] [Google Scholar]
- 124.Florini J.R., Ewton D.Z., Magri K.A. Hormones, growth factors, and myogenic differentiation. Annu. Rev. Physiol. 1991;53:201–216. doi: 10.1146/annurev.ph.53.030191.001221. [DOI] [PubMed] [Google Scholar]
- 125.Thomas M., Langley B., Berry C., Sharma M., Kirk S., Bass J., Kambadur R. Myostatin, a negative regulator of muscle growth, functions by inhibiting myoblast proliferation. J. Biol. Chem. 2000;275:40235–40243. doi: 10.1074/jbc.M004356200. [DOI] [PubMed] [Google Scholar]
- 126.Rios R., Carneiro I., Arce V.M., Devesa J. Myostatin is an inhibitor of myogenic differentiation. Am. J. Physiol. Cell Physiol. 2002;282:C993–C999. doi: 10.1152/ajpcell.00372.2001. [DOI] [PubMed] [Google Scholar]
- 127.Windner S.E., Doris R.A., Ferguson C.M., Nelson A.C., Valentin G., Tan H., Oates A.C., Wardle F.C., Devoto S.H. Tbx6, Mesp-b and Ripply1 regulate the onset of skeletal myogenesis in zebrafish. Development. 2015;142:1159–1168. doi: 10.1242/dev.113431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Biolo G., Maggi S.P., Williams B.D., Tipton K.D., Wolfe R.R. Increased rates of muscle protein turnover and amino acid transport after resistance exercise in humans. Am. J. Physiol. 1995;268 Pt 1:E514–E520. doi: 10.1152/ajpendo.1995.268.3.E514. [DOI] [PubMed] [Google Scholar]
- 129.Phillips S.M. The science of muscle hypertrophy: Making dietary protein count. Proc. Nutr. Soc. 2011;70:100–103. doi: 10.1017/S002966511000399X. [DOI] [PubMed] [Google Scholar]
- 130.Rudnicki M.A., Schnegelsberg P.N.J., Stead R.H., Braun T., Arnold H.-H., Jaenisch R. MyoD or Myf-5 is required for the formation of skeletal muscle. Cell. 1993;75:1351–1359. doi: 10.1016/0092-8674(93)90621-V. [DOI] [PubMed] [Google Scholar]
- 131.Nabeshima Y., Hanaoka K., Hayasaka M., Esuml E., Li S., Nonaka I., Nabeshima Y.I. Myogenin gene disruption results in perinatal lethality because of severe muscle defect. Nature. 1993;364:532–535. doi: 10.1038/364532a0. [DOI] [PubMed] [Google Scholar]
- 132.Kassar-Duchossoy L., Gayraud-Morel B., Gomès D., Rocancourt D., Buckingham M., Shinin V., Tajbakhsh S. Mrf4 determines skeletal muscle identity in Myf5:Myod double-mutant mice. Nature. 2004;431:466–471. doi: 10.1038/nature02876. [DOI] [PubMed] [Google Scholar]
- 133.Tajbakhsh S., Rocancourt D., Cossu G., Buckingham M. Redefining the Genetic Hierarchies Controlling Skeletal Myogenesis: Pax-3 and Myf-5 Act Upstream of MyoD. Cell. 1997;89:127–138. doi: 10.1016/S0092-8674(00)80189-0. [DOI] [PubMed] [Google Scholar]
- 134.Roubenoff R., Roubenoff R.A., Ward L.M., Holland S.M., Hellmann D.B. Rheumatoid cachexia: Depletion of lean body mass in rheumatoid arthritis. Possible association with tumor necrosis factor. J. Rheumatol. 1992;19:1505–1510. [PubMed] [Google Scholar]
- 135.Londhe P., Guttridge D.C. Inflammation induced loss of skeletal muscle. Bone. 2015;80:131–142. doi: 10.1016/j.bone.2015.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Pedersen M., Bruunsgaard H., Weis N., Hendel H.W., Andreassen B.U., Eldrup E., Dela F., Pedersen B.K. Circulating levels of TNF-alpha and IL-6-relation to truncal fat mass and muscle mass in healthy elderly individuals and in patients with type-2 diabetes. Mech. Ageing Dev. 2003;124:495–502. doi: 10.1016/S0047-6374(03)00027-7. [DOI] [PubMed] [Google Scholar]
- 137.Jonsdottir I.H., Schjerling P., Ostrowski K., Asp S., Richter E.A., Pedersen B.K. Muscle contractions induce interleukin-6 mRNA production in rat skeletal muscles. J. Physiol. 2000;528:157–163. doi: 10.1111/j.1469-7793.2000.00157.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Goodman M.N. Interleukin-6 induces skeletal muscle protein breakdown in rats. Proc. Soc. Exp. Biol. Med. 1994;205:182–185. doi: 10.3181/00379727-205-43695. [DOI] [PubMed] [Google Scholar]
- 139.Cai D., Frantz J.D., Tawa N.E., Jr., Melendez P.A., Oh B.C., Lidov H.G., Hasselgren P.O., Frontera W.R., Lee J., Glass D.J., et al. IKKβ/NF-κB Activation Causes Severe Muscle Wasting in Mice. Cell. 2004;119:285–298. doi: 10.1016/j.cell.2004.09.027. [DOI] [PubMed] [Google Scholar]
- 140.Li Y.P., Chen Y., John J., Moylan J., Jin B., Mann D.L., Reid M.B. TNF-alpha acts via p38 MAPK to stimulate expression of the ubiquitin ligase atrogin1/MAFbx in skeletal muscle. FASEB J. 2005;19:362–370. doi: 10.1096/fj.04-2364com. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Guttridge D.C., Mayo M.W., Madrid L.V., Wang C.Y., Baldwin A.S., Jr. NF-kappaB-induced loss of MyoD messenger RNA: Possible role in muscle decay and cachexia. Science. 2000;289:2363–2366. doi: 10.1126/science.289.5488.2363. [DOI] [PubMed] [Google Scholar]
- 142.Layne M.D., Farmer S.R. Tumor necrosis factor-alpha and basic fibroblast growth factor differentially inhibit the insulin-like growth factor-I induced expression of myogenin in C2C12 myoblasts. Exp. Cell Res. 1999;249:177–187. doi: 10.1006/excr.1999.4465. [DOI] [PubMed] [Google Scholar]
- 143.Li Y.P., Reid M.B. NF-kappaB mediates the protein loss induced by TNF-alpha in differentiated skeletal muscle myotubes. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2000;279:R1165–R1170. doi: 10.1152/ajpregu.2000.279.4.R1165. [DOI] [PubMed] [Google Scholar]
- 144.Fernandez-Celemin L., Pasko N., Blomart V., Thissen J.P. Inhibition of muscle insulin-like growth factor I expression by tumor necrosis factor-alpha. Am. J. Physiol. Endocrinol. Metab. 2002;283:E1279–E1290. doi: 10.1152/ajpendo.00054.2002. [DOI] [PubMed] [Google Scholar]
- 145.Frost R.A., Lang C.H., Gelato M.C. Transient exposure of human myoblasts to tumor necrosis factor-alpha inhibits serum and insulin-like growth factor-I stimulated protein synthesis. Endocrinology. 1997;138:4153–4159. doi: 10.1210/endo.138.10.5450. [DOI] [PubMed] [Google Scholar]
- 146.Zhang L., Rajan V., Lin E., Hu Z., Han H.Q., Zhou X., Song Y., Min H., Wang X., Du J., et al. Pharmacological inhibition of myostatin suppresses systemic inflammation and muscle atrophy in mice with chronic kidney disease. FASEB J. 2011;25:1653–1663. doi: 10.1096/fj.10-176917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Brandt C., Nielsen A.R., Fischer C.P., Hansen J., Pedersen B.K., Plomgaard P. Plasma and muscle myostatin in relation to type 2 diabetes. PLoS ONE. 2012;7:e37236. doi: 10.1371/journal.pone.0037236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Lecker S.H., Solomon V., Mitch W.E., Goldberg A.L. Muscle protein breakdown and the critical role of the ubiquitin-proteasome pathway in normal and disease states. J. Nutr. 1999;129(Suppl. S1):227S–237S. doi: 10.1093/jn/129.1.227S. [DOI] [PubMed] [Google Scholar]
- 149.Hall-Angeras M., Angeras U., Zamir O., Hasselgren P.O., Fischer J.E. Effect of the glucocorticoid receptor antagonist RU 38486 on muscle protein breakdown in sepsis. Surgery. 1991;109:468–473. [PubMed] [Google Scholar]
- 150.Schakman O., Dehoux M., Bouchuari S., Delaere S., Lause P., Decroly N., Shoelson S.E., Thissen J.P. Role of IGF-I and the TNFalpha/NF-kappaB pathway in the induction of muscle atrogenes by acute inflammation. Am. J. Physiol. Endocrinol. Metab. 2012;303:E729–E739. doi: 10.1152/ajpendo.00060.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Lecker S.H., Jagoe R.T., Gilbert A., Gomes M., Baracos V., Bailey J., Price S.R., Mitch W.E., Goldberg A.L. Multiple types of skeletal muscle atrophy involve a common program of changes in gene expression. FASEB J. 2004;18:39–51. doi: 10.1096/fj.03-0610com. [DOI] [PubMed] [Google Scholar]
- 152.de Theije C.C., Schols A.M., Lamers W.H., Ceelen J.J., van Gorp R.H., Hermans J.R., Köhler S.E., Langen R.C. Glucocorticoid Receptor Signaling Impairs Protein Turnover Regulation in Hypoxia-Induced Muscle Atrophy in Male Mice. Endocrinology. 2018;159:519–534. doi: 10.1210/en.2017-00603. [DOI] [PubMed] [Google Scholar]
- 153.Smith I.J., Alamdari N., O’Neal P., Gonnella P., Aversa Z., Hasselgren P.O. Sepsis increases the expression and activity of the transcription factor Forkhead Box O 1 (FOXO1) in skeletal muscle by a glucocorticoid-dependent mechanism. Int. J. Biochem. Cell Biol. 2010;42:701–711. doi: 10.1016/j.biocel.2010.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Schakman O., Gilson H., de Coninck V., Lause P., Verniers J., Havaux X., Ketelslegers J.M., Thissen J.P. Insulin-like growth factor-I gene transfer by electroporation prevents skeletal muscle atrophy in glucocorticoid-treated rats. Endocrinology. 2005;146:1789–1797. doi: 10.1210/en.2004-1594. [DOI] [PubMed] [Google Scholar]
- 155.Tomas F.M., Munro H.N., Young V.R. Effect of glucocorticoid administration on the rate of muscle protein breakdown in vivo in rats, as measured by urinary excretion of N tau-methylhistidine. Biochem. J. 1979;178:139–146. doi: 10.1042/bj1780139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Hilton-Jones D. Diagnosis and treatment of inflammatory muscle diseases. J. Neurol. Neurosurg. Psychiatry. 2003;74(Suppl. 2):ii25–ii31. doi: 10.1136/jnnp.74.suppl_2.ii25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Gayan-Ramirez G., Vanderhoydonc F., Verhoeven G., Decramer M. Acute treatment with corticosteroids decreases IGF-1 and IGF-2 expression in the rat diaphragm and gastrocnemius. Am. J. Respir. Crit. Care Med. 1999;159:283–289. doi: 10.1164/ajrccm.159.1.9803021. [DOI] [PubMed] [Google Scholar]
- 158.Fournier M., Huang Z.S., Li H., Da X., Cercek B., Lewis M.I. Insulin-like growth factor I prevents corticosteroid-induced diaphragm muscle atrophy in emphysematous hamsters. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2003;285:R34–R43. doi: 10.1152/ajpregu.00177.2002. [DOI] [PubMed] [Google Scholar]
- 159.Wang H., Kubica N., Ellisen L.W., Jefferson L.S., Kimball S.R. Dexamethasone represses signaling through the mammalian target of rapamycin in muscle cells by enhancing expression of REDD1. J. Biol. Chem. 2006;281:39128–39134. doi: 10.1074/jbc.M610023200. [DOI] [PubMed] [Google Scholar]
- 160.Imae M., Fu Z., Yoshida A., Noguchi T., Kato H. Nutritional and hormonal factors control the gene expression of FoxOs, the mammalian homologues of DAF-16. J. Mol. Endocrinol. 2003;30:253–262. doi: 10.1677/jme.0.0300253. [DOI] [PubMed] [Google Scholar]
- 161.Artaza J.N., Bhasin S., Mallidis C., Taylor W., Ma K., Gonzalez-Cadavid N.F. Endogenous expression and localization of myostatin and its relation to myosin heavy chain distribution in C2C12 skeletal muscle cells. J. Cell. Physiol. 2002;190:170–179. doi: 10.1002/jcp.10044. [DOI] [PubMed] [Google Scholar]
- 162.Ma K., Mallidis C., Artaza J., Taylor W., Gonzalez-Cadavid N., Bhasin S. Characterization of 5′-regulatory region of human myostatin gene: Regulation by dexamethasone in vitro. Am. J. Physiol. Endocrinol. Metab. 2001;281:E1128–E1136. doi: 10.1152/ajpendo.2001.281.6.E1128. [DOI] [PubMed] [Google Scholar]
- 163.Ma K., Mallidis C., Bhasin S., Mahabadi V., Artaza J., Gonzalez-Cadavid N., Arias J., Salehian B. Glucocorticoid-induced skeletal muscle atrophy is associated with upregulation of myostatin gene expression. Am. J. Physiol. Endocrinol. Metab. 2003;285:E363–E371. doi: 10.1152/ajpendo.00487.2002. [DOI] [PubMed] [Google Scholar]
- 164.Ponyi A., Borgulya G., Constantin T., Vancsa A., Gergely L., Danko K. Functional outcome and quality of life in adult patients with idiopathic inflammatory myositis. Rheumatology. 2005;44:83–88. doi: 10.1093/rheumatology/keh404. [DOI] [PubMed] [Google Scholar]
- 165.Angelini C., Pegoraro E., Turella E., Intino M.T., Pini A., Costa C. Deflazacort in Duchenne dystrophy: Study of long-term effect. Muscle Nerve. 1994;17:386–391. doi: 10.1002/mus.880170405. [DOI] [PubMed] [Google Scholar]
- 166.Brooke M.H., Fenichel G.M., Griggs R.C., Mendell J.R., Moxley R.T., 3rd, Miller J.P., Kaiser K.K., Florence J.M., Pandya S., Signore L., et al. Clinical investigation of Duchenne muscular dystrophy. Interesting results in a trial of prednisone. Arch. Neurol. 1987;44:812–817. doi: 10.1001/archneur.1987.00520200016010. [DOI] [PubMed] [Google Scholar]
- 167.Fenichel G.M., Mendell J.R., Moxley R.T., 3rd, Griggs R.C., Brooke M.H., Miller J.P., Pestronk A., Robison J., King W., Signore L., et al. A comparison of daily and alternate-day prednisone therapy in the treatment of Duchenne muscular dystrophy. Arch. Neurol. 1991;48:575–579. doi: 10.1001/archneur.1991.00530180027012. [DOI] [PubMed] [Google Scholar]
- 168.Fenichel G.M., Florence J.M., Pestronk A., Mendell J.R., Moxley R.T., 3rd, Griggs R.C., Brooke M.H., Miller J.P., Robison J., King W., et al. Long-term benefit from prednisone therapy in Duchenne muscular dystrophy. Neurology. 1991;41:1874–1877. doi: 10.1212/WNL.41.12.1874. [DOI] [PubMed] [Google Scholar]
- 169.Griggs R.C., Moxley R.T., 3rd, Mendell J.R., Fenichel G.M., Brooke M.H., Pestronk A., Miller J.P. Prednisone in Duchenne dystrophy. A randomized, controlled trial defining the time course and dose response. Clinical Investigation of Duchenne Dystrophy Group. Arch. Neurol. 1991;48:383–388. doi: 10.1001/archneur.1991.00530160047012. [DOI] [PubMed] [Google Scholar]
- 170.Lemmey A.B., Wilkinson T.J., Perkins C.M., Nixon L.A., Sheikh F., Jones J.G., Ahmad Y.A., O’Brien T.D. Muscle loss following a single high-dose intramuscular injection of corticosteroids to treat disease flare in patients with rheumatoid arthritis. Eur. J. Rheumatol. 2018;5:160–164. doi: 10.5152/eurjrheum.2018.17148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Gibson J.N., Poyser N.L., Morrison W.L., Scrimgeour C.M., Rennie M.J. Muscle protein synthesis in patients with rheumatoid arthritis: Effect of chronic corticosteroid therapy on prostaglandin F2 alpha availability. Eur. J. Clin. Investig. 1991;21:406–412. doi: 10.1111/j.1365-2362.1991.tb01388.x. [DOI] [PubMed] [Google Scholar]
- 172.Tiao G., Fagan J., Roegner V., Lieberman M., Wang J.J., Fischer J.E., Hasselgren P.O. Energy-ubiquitin-dependent muscle proteolysis during sepsis in rats is regulated by glucocorticoids. J. Clin. Investig. 1996;97:339–348. doi: 10.1172/JCI118421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Gathercole L.L., Lavery G.G., Morgan S.A., Cooper M.S., Sinclair A.J., Tomlinson J.W., Stewart P.M. 11beta-hydroxysteroid dehydrogenase 1: Translational and therapeutic aspects. Endocr. Rev. 2013;34:525–555. doi: 10.1210/er.2012-1050. [DOI] [PubMed] [Google Scholar]
- 174.Hardy R.S., Doig C.L., Hussain Z., O’leary M., Morgan S.A., Pearson M.J., Naylor A., Jones S.W., Filer A., Stewart P.M., et al. 11beta-hydroxysteroid dehydrogenase type 1 within muscle protects against the adverse effects of local inflammation. J. Pathol. 2016;240:472–483. doi: 10.1002/path.4806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Bujalska I., Shimojo M., Howie A., Stewart P.M. Human 11 beta-hydroxysteroid dehydrogenase: Studies on the stably transfected isoforms and localization of the type 2 isozyme within renal tissue. Steroids. 1997;62:77–82. doi: 10.1016/S0039-128X(96)00163-8. [DOI] [PubMed] [Google Scholar]
- 176.Fenton C.G., Doig C.L., Fareed S., Naylor A., Morrell A.P., Addison O., Wehmeyer C., Buckley C.D., Cooper M.S., Lavery G.G., et al. 11beta-HSD1 plays a critical role in trabecular bone loss associated with systemic glucocorticoid therapy. Arthritis Res. Ther. 2019;21:188. doi: 10.1186/s13075-019-1972-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Morgan S.A., McCabe E.L., Gathercole L.L., Hassan-Smith Z.K., Larner D.P., Bujalska I.J., Stewart P.M., Tomlinson J.W., Lavery G.G. 11beta-HSD1 is the major regulator of the tissue-specific effects of circulating glucocorticoid excess. Proc. Nat. Acad. Sci. USA. 2014;111:E2482–E2491. doi: 10.1073/pnas.1323681111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Feig P.U., Shah S., Hermanowski-Vosatka A., Plotkin D., Springer M.S., Donahue S., Thach C., Klein E.J., Lai E., Kaufman K.D. Effects of an 11beta-hydroxysteroid dehydrogenase type 1 inhibitor, MK-0916, in patients with type 2 diabetes mellitus and metabolic syndrome. Diabetes Obes. Metab. 2011;13:498–504. doi: 10.1111/j.1463-1326.2011.01375.x. [DOI] [PubMed] [Google Scholar]
- 179.Rosenstock J., Banarer S., Fonseca V.A., Inzucchi S.E., Sun W., Yao W., Hollis G., Flores R., Levy R., Williams W.V., et al. The 11-beta-hydroxysteroid dehydrogenase type 1 inhibitor INCB13739 improves hyperglycemia in patients with type 2 diabetes inadequately controlled by metformin monotherapy. Diabetes Care. 2010;33:1516–1522. doi: 10.2337/dc09-2315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Ahasan M.M., Hardy R., Jones C., Kaur K., Nanus D., Juarez M., Morgan S.A., Hassan-Smith Z., Bénézech C., Caamano J.H., et al. Inflammatory regulation of glucocorticoid metabolism in mesenchymal stromal cells. Arthritis Rheum. 2012;64:2404–2413. doi: 10.1002/art.34414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Kaur K., Hardy R., Ahasan M.M., Eijken M., Van Leeuwen J.P., Filer A., Thomas A.M., Raza K., Buckley C.D., Stewart P.M., et al. Synergistic induction of local glucocorticoid generation by inflammatory cytokines and glucocorticoids: Implications for inflammation associated bone loss. Ann. Rheum. Dis. 2010;69:1185–1190. doi: 10.1136/ard.2009.107466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Coutinho A.E., Gray M., Brownstein D.G., Salter D.M., Sawatzky D.A., Clay S., Gilmour J.S., Seckl J.R., Savill J.S., Chapman K.E. 11beta-Hydroxysteroid dehydrogenase type 1, but not type 2, deficiency worsens acute inflammation and experimental arthritis in mice. Endocrinology. 2012;153:234–240. doi: 10.1210/en.2011-1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Hardy R.S., Fenton C., Croft A.P., Naylor A.J., Begum R., Desanti G., Buckley C.D., Lavery G., Cooper M.S., Raza K. 11 Beta-hydroxysteroid dehydrogenase type 1 regulates synovitis, joint destruction, and systemic bone loss in chronic polyarthritis. J. Autoimmun. 2018;92:104–113. doi: 10.1016/j.jaut.2018.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]