Abstract
Inflammatory bowel diseases (IBD), including Crohn’s disease and ulcerative colitis, are lifelong conditions that often begin in childhood. The implications of IBD are of particular importance in children because of the potential negative effects on growth, development, psychosocial function, and overall wellbeing. The key management strategy is to achieve sustained control of intestinal inflammation and monitor for potential complications of the disease and side effects of therapies. Overall, the evidence on the management of IBD in children is less extensive than in adults, but good quality multicenter studies and various guidelines and society consensus statements are available. This review summarizes the evidence on the pathophysiology, diagnosis, and approaches to management of children and adolescents with IBD.
Introduction
Crohn’s disease and ulcerative colitis are chronic relapsing conditions; Crohn’s disease involves the entire gastrointestinal tract from mouth to anus, whereas ulcerative colitis affects only the colon. The incidence and prevalence of inflammatory bowel diseases (IBD) is increasing, and 20-30% of cases present before the age of 20 years. IBD that starts in childhood is associated with more extensive disease, higher disease activity, and a more complicated course than adult onset IBD.1 2 3 The mean delay from onset to diagnosis is 11 months in new onset pediatric IBD (PIBD).4 Before 2000 the mainstay of treatment was anti-inflammatory drugs and corticosteroids, but now the armamentarium has expanded to immunomodulators and biologics. As the genotypic-phenotypic understanding of IBD advances, customized treatment for individual patients will be developed. Shortening the time to diagnosis and adherence to diagnostic and therapeutic guidelines should lead to improved clinical outcomes.5 The focus of management should be on controlling gut inflammation and optimizing nutrition, growth, and quality of life (QOL), while preventing disease related or treatment related complications.6 This review summarizes the evidence on disease presentation, diagnostic approach, and treatment options in children aged up to 18 with IBD.
Sources and selection criteria
We searched PubMed through December 2016 using the following terms alone and in combination: “inflammatory bowel disease”, “Crohn’s disease”, “ulcerative colitis”, “pathophysiology”, “epidemiology”, “diagnosis”, “disease management”, “complications”, and “child/children”. We also searched bibliographies of articles identified from relevant studies. Evidence came from articles in English that included randomized studies, cohort studies, observational studies, meta-analyses, and systematic reviews. Owing to the paucity of pediatric data, we also included retrospective studies and case series/reports. Most studies pertinent to the review were included, irrespective of the number of participants. We included the most recent articles named as “guidelines” or “clinical practice”. We also included some studies in adults when no pediatric data were available.
Epidemiology
Rates of PIBD are increasing worldwide, but accurate estimates are lacking.7Table 1 shows the incidence of PIBD worldwide. Ontario has one of the highest rates of childhood onset IBD, with an accelerated increase in incidence in younger children.23 Scotland has seen a 76% increase in diagnosis of PIBD since the mid-1990s, and the diagnosis was made at a younger age.24 People immigrating from low to high prevalence regions are at increased risk for developing IBD, particularly among first generation children.25 Australasian data indicate increasing incidence of PIBD, predominantly in children of European ancestry, with lower rates in indigenous populations.26 In a community based healthcare delivery system in northern California, the incidence of ulcerative colitis increased 2.7-fold over a period of 10 years. Hispanic and Asian children developed ulcerative colitis more often than Crohn’s disease.27 In British Columbia, South Asians had a threefold higher incidence of PIBD than non-South Asians.18 A population based study in Wisconsin found that the incidence of PIBD was similar in different ethnic groups, as well as in densely populated compared with sparsely populated counties.28 The relative risk for developing pediatric onset Crohn’s disease was higher in affluent areas, but this was not the case for ulcerative colitis.22 A higher prevalence with increasing latitudes has been noted for pediatric onset Crohn’s disease in Scotland and for ulcerative colitis in Finland,22 29 and an east-west gradient in IBD incidence was noted in Europe.30
Table 1.
Incidence rates for inflammatory bowel disease (IBD), Crohn’s disease (CD), and ulcerative colitis (UC) in children
| No of cases | Incidence per 100 000 | Country | ||
|---|---|---|---|---|
| IBD | CD | UC | ||
| CD 65; UC 398 | 7.6 | 4.6 | 2.8 | North eastern Slovenia |
| IBD 3409 | 0.47 | 0.27 | 0.2 | Saudi Arabia |
| IBD 99210 | 9.5 | 6.6 | 2.4 | Wisconsin, USA |
| CD 30; UC 211 | 11.4 | – | – | Singapore |
| CD 96; UC 293 | 12.8 | 9.2 | 2.8 | Stockholm County, Sweden |
| CD 44; UC 6112 | 5.6 | – | – | Iceland |
| EPIMAD registry13 | – | 6.7 | – | Northern France |
| CD 152; UC 5914 | 2.4 | 1.35 | 0.45 | Texas, USA |
| CD 92; UC 3615 | 2.16 | – | – | Kuwait |
| Population based7 | 11.8 | 6.2 | 4.4 | Ontario, Canada |
| CD 635; UC 81016 | 1.39 | – | – | Italy |
| CD 64; UC 7017 | 6.1 | 3.1 | 2.6 | Denmark |
| CD 36; UC 2518 | 15.9 | 6.41 | 6.7 | South Asian in BC, Canada |
| CD 203; UC 31719 | 7 | – | – | Finland |
| IBD 2520 | 5.7 | 3.64 | 2.05 | Norway |
| CD 22321 | 1.25 | – | – | Czech Republic |
| CD 383; UC 19722 | – | 2.3 | 1.2 | Scotland |
| CD 431; UC 2114 | 5.2 | – | – | Great Britain and Ireland |
Pathophysiology
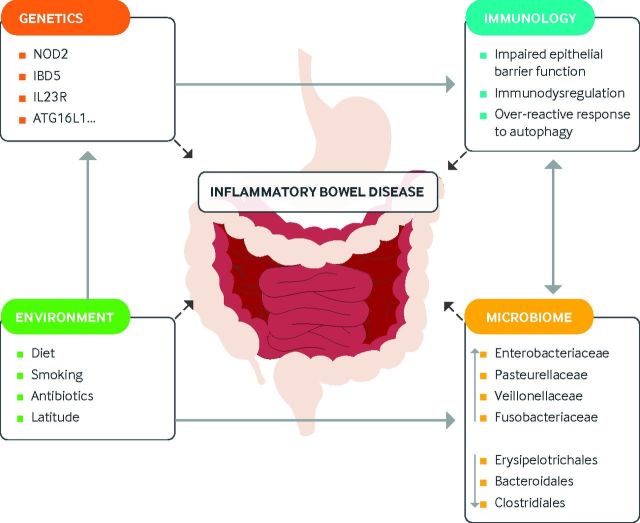
IBD is an immune mediated disease. In recent years, the specifics of the interaction of innate and adaptive responses to the disease process are becoming clearer. Genome-wide association studies have identified more than 200 genetic loci associated with IBD.31 These genes code for proteins involved in innate and adaptive immunity, autophagy, and mucosal barrier integrity and play a key role in immune homeostasis. Thus, a dysregulated immune response to commensal intestinal bacteria due to an underlying genetic predisposition is thought to be the trigger for chronic inflammation.32 33 34 Environmental factors likely influence many steps of the pathophysiology, such as the effect of diet and antibiotic use on epithelial barrier function and microbial diversity.35
The microbiome in Crohn’s disease has an increased abundance of specific bacterial families and a decrease of others.35 In PIBD and adult IBD, an increased load of entero-invasive Escherichia coli strains has been observed.36 However, no specific organism has been shown to cause IBD. Recently, interest has shifted to the role of the microbiome and environmental factors in the risk of development of autoimmune and inflammatory conditions, including IBD. The hygiene hypothesis theorizes that people raised under sanitary conditions have a higher risk of developing immune mediated diseases, such as IBD.37 A systematic review found an inverse association of several factors related to environmental hygiene and the risk of IBD, which is in alignment with the hygiene hypothesis.38Figure 1 summarizes the pathophysiology in IBD.
Fig 1.
Genetics
PIBD is familial in 19-41% of cases, compared with 5-10% in adults.31 A highly significant association was reported between Crohn’s disease and interleukin 23R in non-Jewish people of European ancestry with ileal Crohn’s disease; however, a coding variant of interleukin 23R was also found to confer a strong protective effect in a cohort of pediatric Crohn’s disease.41 42 A positive family history is often present when Crohn’s disease is diagnosed before 11 years of age.35 43 Genetic factors have only a modest role, and epigenetic factors may play a role in disease development. Different patterns of DNA methylation have been observed in treatment-naive PIBD, which supports the hypothesis of epigenetic factors playing a role in the pathophysiology.44
Evaluation and diagnosis
Clinical presentation
PIBD presents with wide variety of symptoms, both gastrointestinal and extra-intestinal. The initial presentation of ulcerative colitis is commonly abdominal pain and bloody diarrhea. This usually comes to medical attention sooner than the more varied and sometimes subtle presentation of Crohn’s disease. A child with Crohn’s disease may present with bloody diarrhea and abdominal pain when colitis is present or with vaguer symptoms such as non-bloody diarrhea, weight loss/growth failure, malaise, fatigue, anemia, or fever. Table 2 outlines characteristics of ulcerative colitis and Crohn’s disease in PIBD.3
Table 2.
Characteristics of Crohn’s disease and ulcerative colitis3
| Clinical features | Crohn’s disease | Ulcerative colitis |
|---|---|---|
| Sex distribution | Male > female | Male = female |
| Symptoms and signs | Abdominal pain, diarrhea, weight loss, anorexia, growth failure | Bloody diarrhea, abdominal pain |
| Location | Mouth to anus; involves all layers of gut: mucosa to serosa; most common: ileocolonic | Colon; involves only mucosa; most common: pancolonic |
| Endoscopic findings | Segmental distribution, aphthous ulcers, deep fissuring ulcers, cobblestoning, perianal disease, strictures, fistulas | Diffuse and continuous erythema, friability, granularity, loss of vascular pattern from rectum to variable extent |
| Histological findings | Pathognomonic non-caseating granulomas; patchy cryptitis, crypt abscesses, ileitis | Cryptitis, crypt abscesses, crypt architectural distortion, basal lymphocytosis, distal Paneth cell metaplasia |
| Radiologic findings | Rigid stenotic segments, skip areas, and sinus tracts or fistulas | Dilatation of colon in toxic megacolon |
Extra-intestinal manifestations may be the initial presentation of IBD and are more common in Crohn’s disease than in ulcerative colitis.16 They include erythema nodosum, pyogenic granuloma, uveitis, episcleritis, arthritis, and primary sclerosing cholangitis.
Two retrospective cohort studies (n=160 and n=153) found no differences in clinical presentation or subsequent hospital admission between younger and older children with PIBD.43 45 In a PIBD consortium registry (n=998), 9.9% of children with Crohn’s disease were 0-5 years of age, and children in this age group were more likely to present with rectal bleeding and be initially diagnosed as having ulcerative colitis46; they tended to have a more severe disease course and higher disease burden.45 Short stature, seen only in Crohn’s disease, occurred in about a fifth of the cases at presentation.4
Very early onset IBD is defined as the onset of IBD in children 6 years and younger. Very early onset IBD is still considered “polygenic” in nature, but a subgroup of very young patients, including neonates, may have one of the monogenic forms of the disease (XIAP deficiency, interleukin 10 signaling defects, IPEX-like), which have more severe presentations and will likely not respond to traditional treatment.47 48 The full spectrum of diagnostic testing and potential therapies for very early onset IBD will not be covered in this review.
Baseline tests
Baseline tests should include a complete blood count, liver enzymes, albumin, C reactive protein (CRP), and/or erythrocyte sedimentation rate (ESR).49 The sensitivity and specificity of anemia and increased ESR as predictors for IBD was 83% and 94% respectively (n=227, retrospective study).50 In children with intestinal or nutritional problems, anemia and thrombocytosis had a sensitivity of 90.8% and a specificity of 80% for ulcerative colitis and Crohn’s disease (n=103 IBD, 50 controls, screening test).51 Infectious causes should be excluded using stool nucleic acid amplification tests or culture.52 Fecal inflammatory markers such as calprotectin and lactoferrin can help in differentiating IBD from irritable bowel syndrome, but they can also be elevated in other inflammatory conditions. Calprotectin correlates significantly with mucosal inflammation in PIBD and can be used as a surrogate marker for inflammation; normalization indicates mucosal healing.53 A meta-analysis of 19 diagnostic studies in children with chronic gastrointestinal symptoms concluded that calprotectin, CRP, and albumin have potential clinical value to select children at low risk (negative calprotectin) or high risk (positive CRP or low albumin) for IBD (n=2806).54 Normal laboratory tests, however, may not always exclude IBD. In PIBD, normal platelets, ESR, albumin, or hemoglobin were found in 21% of mild Crohn’s disease cases, 54% of mild ulcerative colitis, and 4% of more severe Crohn’s disease or ulcerative colitis (n=392 CD, 134 UC; prospective multicenter study).55
Serology
Available serological markers are atypical perinuclear antineutrophil cytoplasmic antibody (pANCA), anti-saccharomyces cerevisiae antibody (ASCA), antibodies to Escherichia coli outer membrane porin, Pseudomonas fluorescens associated sequenceI2, and flagellin CBir1. In a retrospective study, the IBD Serology7 panel (Prometheus Laboratories, San Diego, CA), when compared with routine blood tests, had lower predictive value in screening for PIBD (n=394).56 A recent review concluded that the use of serum antibodies remains complementary in clinical practice.57 Serology may have a role in assessing prognosis. Children with Crohn’s disease who are ASCA IgA/IgG positive have a high prevalence of terminal ileal or ileocecal disease and are more likely to need surgery; in contrast, those with Crohn’s disease and positive pANCA are more likely to have pancolitis or left sided disease with sparing of the terminal ileum, and ileocecal resection is uncommon (n=139, retrospective cohort).58
Endoscopy
Colonoscopy including intubation of the terminal ileum and multiple biopsies for histology obtained from all segments of the lower intestinal tract is essential to differentiate Crohn’s disease from ulcerative colitis and identify localization and extent of disease.49 Isolated ileal inflammation may occur in the presence of a normal colon in up to 9% of children with Crohn’s disease, so ileal intubation should always be attempted.4 Unlike in adults, 10-34% of children with new onset ulcerative colitis lack histological features of chronic colitis at presentation.59
Esophagogastroduodenoscopy should be part of the first line investigation in all cases of suspected IBD. Absence of specific upper gastrointestinal symptoms does not preclude presence of upper gastrointestinal inflammation.60 In a retrospective study of 172 children with suspected IBD, the diagnosis was changed to Crohn’s disease on the basis of biopsies obtained at esophagogastroduodenoscopy.61 Data from a PIBD registry found that esophagogastroduodenoscopy helped to establish the final diagnosis in 10% of the children with IBD.62
The possibility of avoiding ionizing radiation and deep sedation/general anesthesia with capsule endoscopy makes it an appealing tool for diagnosis and monitoring in PIBD. In a meta-analysis of children undergoing capsule endoscopy (n=723), 65.4% had positive diagnosis, 69.4% had a new diagnosis, 68.3% had a change in treatment, and 2.6% had capsule retention.63 In a prospective cohort study (n=18), capsule endoscopy helped in diagnosing Crohn’s disease in 83.3%, affected medical decision making in 72.2%, and led to a change in medical management in 77.8% of the children.64 Capsule endoscopy was found to provide additional clinical information that affected management and improved outcomes in a tertiary PIBD center (n=66 established PIBD, 17 suspected; retrospective review).65 Nevertheless, because histology cannot be obtained with capsule endoscopy, it remains a complementary diagnostic tool.
Guidelines
The European Society for Paediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN) and the working group of the North American Society for Pediatric Gastroenterology Hepatology and Nutrition (NASPGHAN)/Crohn’s and Colitis Foundation of America recommend total colonoscopy with ileal intubation, upper endoscopy (esophagogastroduodenoscopy), multiple biopsies, and complete small bowel exploration as diagnostic procedures.49 66
Imaging
Cross sectional imaging techniques can depict subtle features of active inflammation such as fibrofatty proliferation and mesenteric hypervascularity, as well as extraluminal complications such as enteric fistula, intra-abdominal abscess, and free intraperitoneal air. The non-invasive nature of imaging makes it an ideal tool for serial assessment of disease activity and treatment response in patients receiving immunomodulators. A meta-analysis found no significant difference in the diagnostic accuracy of the various imaging modalities, so the choice of imaging should be based on their specific advantages and disadvantages (table 3).69
Table 3.
| Study | Advantages | Disadvantages |
|---|---|---|
| Small bowel follow-through | Low cost | Ionizing radiation |
| Long examination | ||
| Easily available | Poor bowel distension | |
| Variable interpretation | ||
| Computed tomography | Moderate cost | Ionizing radiation |
| Optimal bowel wall assessment | Need for intravenous iodine contrast | |
| Ideal in emergency setting | Inability to tolerate oral contrast | |
| Magnetic resonance imaging | No ionizing radiation | High cost |
| Cross sectional imaging in any plane | Prone to motion artifacts | |
| Differentiation of inflammatory versus fibrotic stricture/disease | Inability to tolerate oral contrast | |
| Less widely available | ||
| Bowel ultrasonography | No ionizing radiation | Operator dependent |
| Low cost | Inability to visualize entire gastrointestinal tract | |
| Easily available | Less reproducible | |
| Well tolerated in young children | ||
| Excellent depiction of bowel wall |
Barium small bowel follow-through is no longer the primary imaging modality in PIBD. However, it is still favored by some people as it is easy to perform, is widely available, and does not require sedation.67 68
Computed tomography can be used to stage IBD at diagnosis and assesses complications. Computed tomography is valuable in determining the cause of symptoms such as abdominal pain, vomiting, and fever in children with PIBD presenting to the emergency department.70 Ultrasonography is suitable for visualizing features of Crohn’s disease such as bowel thickness and dilatation, strictures, presence of fistulas, abscesses, or inflammatory changes in the mesentery.71 Small intestine contrast ultrasonography (SICUS) can be performed using oral anechoic contrast solution to enhance the sensitivity. In a study of 51 consecutive children with suspected or diagnosed Crohn’s disease, the sensitivity and specificity of SICUS were 100% and 100% respectively in patients without a previous diagnosis and 96% and 100% respectively in proven Crohn’s disease.72
Magnetic resonance enterography (MRE) has a higher specificity in children compared with a higher sensitivity in adults. A systematic review of 11 studies (n=496 children) concluded that MRE should supersede barium meal enteroclysis as the small bowel imaging technique in centers with appropriate expertise.73 Pelvic magnetic resonance imaging (MRI) is considered the gold standard for evaluating fistulas by identifying sinus tracts containing fluid with peripheral enhancement and abscesses, which appear as extraluminal focal fluid collections with a contrast enhanced rim.74 MRE is the imaging modality of choice in PIBD at diagnosis. It may detect small intestinal involvement and inflammatory changes in the intestinal wall and identify disease complications.74 75
Guidelines
The American College of Radiology (ACR) criteria for imaging of a child or young adult with suspected Crohn’s disease at initial presentation give equal weighting to computed tomography enterography and MRE. For imaging of children and young adults with known Crohn’s disease and an acute presentation (abdominal pain, fever, or leukocytosis), the ACR gives equal weighting to computed tomography of the abdomen and pelvis with contrast and MRE. The newer ACR recommendation for a child or young adult with known Crohn’s disease and stable non-acute mild symptoms on surveillance is to use MRE.71
Management
Treatment of IBD has evolved in the past decades to multiple available therapies.76 To decide which treatment will be most successful for a given patient, disease severity, location, phenotype, effect of the disease on growth and development, and the psychosocial status of the patient should all be considered.76 The approach to treating IBD has been classically described as either “top down” or “step up.” The step-up approach uses drugs such as aminosalicylates, antibiotics, or enteral therapy and escalates to immunomodulators, biologics, or surgical intervention if the disease worsens. In the top-down approach, treatment starts with drugs such as biologics on the basis of disease severity, with the hope that the therapy can be downgraded to “less aggressive” drugs.76 In reality, patients do not always go up or down the spectrum of available drugs used to treat IBD. Some phenotypes are predictive of a complicated course and therefore warrant early and ongoing aggressive treatment. De-escalating or trying the step-up approach could potentially prolong the course of active disease. In case of worsening disease, drugs may be added and not necessarily substituted, switching from monotherapy to combination therapy.77
Once diagnosis is established, two important decisions will need to be made: which treatment should be used for induction of remission and which for maintenance therapy. This decision should be individualized to each patient and clinical scenario. In many cases, more than one acceptable treatment strategy exists. The STRIDE (Selecting Therapeutic Targets in IBD) initiative proposed the “treat to target approach,” providing 12 recommendations including goals such as mucosal healing and improvement of QOL.78 In pediatrics, restoration of appropriate growth and pubertal development are also important goals.79Tables 4 and 5 outline the drugs used in PIBD, dosing, side effects, and screening tests.
Table 4.
| Drug | Dose | Side effects |
|---|---|---|
| Prednisone (oral) or methylprednisolone (intravenous) | 1-2 mg/kg daily, maximum 40-60 mg/day | Growth suppression, adrenal suppression, immunosuppression |
| Budesonide | 9 mg orally daily | Same as above but lower |
| 5-aminosalicylate | 50-80 mg/kg/day orally up to 4 g daily | May mimic acute exacerbation, interstitial nephritis |
| Azathioprine | 2-3 mg/kg/day orally | Immunosuppression, myelosuppression, pancreatitis, lymphoma |
| 6-mercaptopurine | 1-1.5 mg/kg/day orally | |
| Methotrexate | 15 mg/m2/day to maximum 25 mg/day | Nausea, hepatic fibrosis |
| Infliximab | 5 mg/kg intravenously at 0, 2, and 6 weeks, then every 8 weeks; dose can be increased to 10 mg/kg and interval be shortened to every 4-6 weeks | Immunosuppression, psoriasis, lymphoma |
| Adalimumab | Induction: 2.4 mg/kg (maximum 160 mg) at baseline, 1.2 mg/kg (maximum 80 mg) at week 2; maintenance: 0.6 mg/kg every other week |
Table 5.
Recommended tests before starting treatment with immunomodulators or biologics and for monitoring of treatment80 81 82 83
| Drug | Screening | Monitoring |
|---|---|---|
| Immunomodulators | Tuberculosis | Complete blood count and liver enzymes every 3 months |
| Pregnancy test before methotrexate* | ||
| Consider Epstein-Barr virus titers | ||
| Biologics | Tuberculosis† | Complete blood count and liver enzymes every visit (with infusions); tuberculosis screening annually |
| Varicella titers | ||
| Hepatitis B screening‡ | ||
| Imaging if suspected intra-abdominal or perianal abscess or fistula |
*Post-menarche female patients only.
†Consider screening for other infectious diseases, such as histoplasmosis, depending on region.
‡Recommend immunization accordingly.
Guidelines
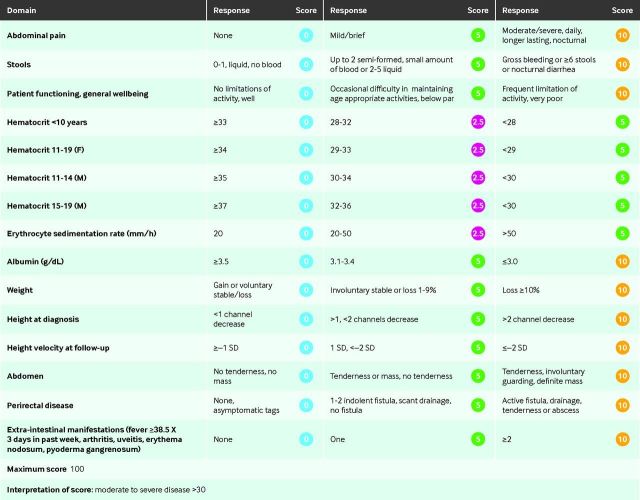
European Crohn’s and Colitis Organisation (ECCO)/ESPGHAN provide evidence based guidance on management of pediatric Crohn’s disease. Nutrition therapy is recommended as first line to induce remission in active Crohn’s disease.34 Nevertheless, this is not common practice in the US, mainly owing to acceptance by patients/families. The ESPGHAN consensus on management of acute severe ulcerative colitis in children provides a stepwise approach to escalating therapy based on Pediatric Ulcerative Colitis Activity Index (PUCAI) progression (fig 2).85 Clinical reports and consensus statements are also available from NASPGHAN for long term health supervision, management of pediatric Crohn’s disease with perianal manifestations and penetrating phenotype, and approach to infectious diseases in children receiving anti-tumor necrosis factor-α (TNF-α) drugs.86 87 88
Fig 2.
Pediatric Ulcerative Colitis Activity Index (PUCAI). Adapted from Turner et al84
Induction therapy
Exclusive enteral nutrition
Exclusive enteral nutrition (EEN) can be used for six to eight weeks to induce remission in patients with a new diagnosis or an acute flare of the disease. Evidence shows that elemental formulas are not superior to polymeric formulas, supporting the use of such formulas, which are less expensive and more palatable.34 Limited data from meta-analyses in 2000 and 2007 suggest that enteral nutrition has similar efficacy to corticosteroids in induction of remission in children with Crohn’s disease.89 90 EEN was shown to be superior to corticosteroids alone in treatment of active disease when the primary outcome was mucosal healing (n=37 children with Crohn’s disease; 19 polymeric diet, 18 steroids; randomized control, open label trial).91
Many theoretical explanations exist for how EEN works, but the mechanism is likely related to a diet induced modulation of intestinal microbiome.79 Partial enteral nutrition (PEN), when only a percentage of the total calorie intake is composed of a formula, has been shown to be ineffective in inducing remission in children with active Crohn’s disease (pediatric Crohn’s Disease Activity Index >20; see fig 3 for scoring).93 However, PEN can be used to improve nutritional status and maintenance of remission along with maintenance drugs.79
Fig 3.
Pediatric Crohn’s Disease Activity Index (PCDAI) adapted from Hyams et al.92
Corticosteroids
Systemic corticosteroids should be used only for induction of remission.34 When patients need steroids for a longer period than expected to achieve remission (>6-8 weeks) or, in other words, when there is steroid dependence, consideration should be given to step-up therapy or evaluation of the need for surgical intervention. Prednisone, or its equivalent, is recommended, and tapering should be gradual owing to the risk of adrenal insufficiency.34 Different available formulations of budesonide are modulated to be released in the ileum or throughout the colon and can be beneficial for induction of remission with lower systemic bioavailability and side effects.94
Antibiotics
Antibiotics such as metronidazole and ciprofloxacin can be used for inducing remission in perianal fistulizing disease. They are particularly beneficial when initiation of immunosuppressants has to be postponed owing to concomitant infection and need for surgical intervention.34 With the advantage of being minimally absorbed, rifaximin has also been shown to be of benefit in inducing remission of Crohn’s disease, particularly with colonic disease (n=402; phase II multicenter double blind placebo controlled trial).95
5-aminosalicylates
In mild to moderate ulcerative colitis, oral 5-aminosalicylates (5-ASAs) can be used for induction of remission but have little effect on severe disease.85 5-ASAs have also been used for induction of remission in very mild pediatric Crohn’s disease. However, a retrospective study of 43 children with Crohn’s disease (25 mild, 18 moderate-severe) treated with 5-ASA monotherapy compared with various combination therapies (steroids, enteral therapy, antibiotics, or immunomodulators) reported more exacerbations, shorter duration of first remission, and longer eventual duration of steroid use.96
Biologics
Anti-TNF treatment is recommended as induction therapy in severe PIBD.34 It is the preferred first choice for patients with perianal fistulizing disease, growth failure, or extra-intestinal manifestations.34 76 Two biologic drugs are approved for the treatment of PIBD: infliximab (25% murine/75% human monoclonal antibody) and adalimumab (100% human recombinant monoclonal antibody).
Maintenance therapy
5-aminosalicylates
Different oral preparations of 5-ASA differ in their location of action (table 6.) Rectal preparations can be used to treat distal disease and proctitis.76 The ESPGHAN consensus recommends that 5-ASA (oral or topical) should be stopped in the setting of an acute flare, owing to the potential for worsening diarrhea.85 A prospective observational study in 213 children with newly diagnosed ulcerative colitis and taking maintenance 5-ASAs found that 43% remained in steroid-free remission at one year.98 A placebo controlled randomized trial in 122 children with Crohn’s disease found that mesalamine was not an effective maintenance therapy (one year relapse 57% and 63% in treatment and placebo groups respectively).99 Prolonged use of 5-ASAs requires monitoring with yearly urinalysis for interstitial nephritis, a rare but severe side effect.97 100
Table 6.
Mesalamine formulations and their site of action97
| Formulation | Site of action |
|---|---|
| Asacol (Proctor and Gamble), Rowasa (Reid Rowell) | Terminal ileum, colon |
| Pentasa (Marion-Merrell-Dow) | Controlled release throughout small bowel |
| Balsalazide/Colazide (Astra Zeneca), balsalazide disodium/Colazal (Salix Pharmaceuticals) | Colon |
| Mesalamine/Lialda (Shire) | Colon |
Immunomodulators
Immunomodulators, such as thiopurines and methotrexate, are used as maintenance therapy and/or as combination therapy along with a biologic to decrease antibody formation against the anti-TNF in patients of all ages, thereby optimizing therapy.76 101 These drugs are slow acting and their effect may take two to three months to be optimal, assuming an appropriate dose.34 76
Thiopurines (6-mercaptopurine and azathioprine)—Thiopurines are effective drugs in maintenance therapy for PIBD. A multicenter placebo controlled randomized controlled trial (RCT) in 55 children newly diagnosed as having moderate to severe Crohn’s disease found a relapse rate of 9% in the group receiving steroids and 6-mercaptopurine compared with 47% in those receiving steroids and placebo (P<0.007).102 Important considerations are risk of myelosuppression and hepatotoxicity, warranting periodic monitoring (complete blood count and liver profile at least every three months on stable dosing and more frequently while the dose is being increased).34 Thiopurine S-methyltransferase is involved in azathioprine/6-mercaptopurine metabolism, and decreased/absent activity can lead to severe bone marrow suppression. Its activity should be measured before starting treatment; if it is undetectable, alternative treatment is needed. Patients with low to intermediate activity should be placed on a lower dose.34 103 104
Methotrexate can be used as maintenance therapy in patients with Crohn’s disease at risk for poor outcomes or failure of azathioprine/6-mercaptopurine, with remission rates of 23-53% at one year (based on a review of mainly retrospective studies in children from 1966 to August 2015).105 Methotrexate is contraindicated during pregnancy; if it is necessary in a female patient with potential for pregnancy, birth control methods should be provided. Methotrexate, although well tolerated, has potential for hepatotoxicity. A retrospective cohort study of 60 children with Crohn’s disease who were taking methotrexate reported transient elevation of liver enzymes in 27% and persistent elevation in 15%.106 Liver enzymes should be monitored.34 76
Biologics
Biologic (anti-TNF) therapy is indicated as induction and maintenance therapy in situations in which the patient has not responded to previous therapies or when the step-up approach is not likely to be successful.34 76 Recommendations for dosing and frequency of infliximab and adalimumab are available, but the doses and intervals should be adjusted on the basis of proactive monitoring of drug concentrations and antibody formation.34 76
The REACH study (randomized, multicenter, open label study) has shown the benefit of an every eight week regimen compared with every 12 weeks in children with moderate to severe Crohn’s disease (n=112). At 10 weeks, 88.4% (95% confidence interval 82.5% to 94.3%) of the children responded to infliximab.107 Children on the every eight weeks regimen did better than those on the every 12 weeks regimen, with rates of clinical remission of 55.8% and 23.5% respectively (P<0.001).107 Similar findings on efficacy and safety have been reported in an RCT of 60 children with moderate to severe ulcerative colitis taking infliximab and also in children with moderate to severe Crohn’s disease taking adalimumab (n=192; double blind maintenance dosing regimens following open label induction).108 109
Treatment failure with infliximab can be related to low trough drug concentrations resulting from inadequate dosing and/or formation of antibodies against the drug, which accelerates drug clearance.110 The recommended approach is proactive drug concentration monitoring to allow recognition of low drug concentrations and presence of antibody before the symptoms arise.111 Infliximab concentrations between 3 and 7 μg/mL were found to be associated with better clinical response.112 In pediatric Crohn’s disease, higher concentrations of infliximab during the induction phase predict a sustained response to the drug.113
Combination therapy: immunomodulators and anti-TNF
Immunomodulators such as azathioprine/6-mercaptopurine and methotrexate have recently been used in an attempt to restore response to an anti-TNF agent once the patient has developed antibodies against the drug (n=5, young adults).114 In a retrospective review of the PIBD Collaborative Research Group Registry, infliximab plus an immunomodulator was found to increase the chance that the patient would benefit from infliximab for five years (n=502).101
Surgery
Restorative proctocolectomy is a curative procedure in confirmed ulcerative colitis, although there is a risk for ongoing morbidity due to chronic pouchitis. In pediatric ulcerative colitis, surgery is reserved for patients with severe disease refractory to aggressive medical treatment.85 Between 8% and 26% of children with ulcerative colitis will need a colectomy in the first five years from diagnosis.115 116 117 Postoperative complications tend to be more common in children who have emergent colectomy compared with elective colectomy (n=30, retrospective review).118 The post-colectomy general health status and overall QOL in pediatric onset ulcerative colitis was found to be comparable to the that of normal population (n=52, controls=117; questionnaire survey).119
In Crohn’s disease, resection surgery can be an option to induce remission of localized disease, although it is not curative; this should be seen as a “surgically induced remission” and followed by initiation or optimization of maintenance therapy.34 In a Danish cohort (n=115 children with Crohn’s disease), the clinical recurrence rate after surgery was 50% at one year and 77% at 10 years.120 In a retrospective review (n=81 children), recurrence of Crohn’s disease was related to younger age at resection, and the likelihood of a second surgery was related to disease site and occurrence of operative complications at the initial surgery.121 Postoperative azathioprine did not decrease the rate of recurrence after surgery.120 In an open label randomized trial including patients with Crohn’s disease from 12 to 65 years of age (n=31), early intervention with infliximab monotherapy (compared with no infliximab) prevented clinical, serological, and endoscopic Crohn’s disease recurrence following ileocolic resection.122
Decision making regarding colectomy in children should take into consideration the toxicity of prolonged use of drugs, QOL, and self image, as well as functional outcomes and, in female patients, fertility after pouch procedures.123
Nutritional therapy
As previously discussed, EEN can be used for induction of remission. PEN can be used as adjuvant maintenance therapy along with drugs in selected patients.34
Many other dietary approaches have been discussed as potential adjuvant maintenance therapy for IBD, such as specific carbohydrate diet, anti-inflammatory diet, low FODMAP diet, and Paleolithic diet.124 No strong evidence exists to support any of these approaches, but it is encouraging to see research about potential mechanisms of action. Research efforts have been directed to studying how the microbiome composition affects the development and severity of IBD. The known dietary effect on microbiome composition makes it likely that dietary modifications can affect IBD. What dietary modifications should be made remains to be answered.124 125 126 127
Complications
Nutritional complications
Children with IBD are at risk for macronutrient and micronutrient deficiencies. Weight loss occurs in up to 70% of children with Crohn’s disease and in 34% with ulcerative colitis.128
Nutritional support in IBD is essential to long term survival and QOL. From ensuring appropriate calorie intake to monitoring bone health and micronutrients that can affect risks for thromboembolisms and malignancies, nutrition management should be taken as seriously as drug management of PIBD.129
Protein-energy malnutrition is more likely to be seen in severe, active disease, but a watchful approach to micronutrient deficiencies should be taken in the long term for all patients with IBD. Location of disease as well as history of surgical resection should guide the clinician to a proactive approach in terms of screening for specific micronutrient concentrations: vitamin B12 deficiency in the setting of terminal ileum resection or zinc loss in the setting of profuse diarrhea or high output fistula.129
Growth failure
Delayed skeletal maturation (which eventually leads to growth failure) is more common in Crohn’s disease than in ulcerative colitis and often leads to suboptimal linear growth and sometimes delayed puberty. Patients with Crohn’s disease are at risk for growth failure for many reasons including the inflammatory nature of the disease, the malabsorption of nutrients, and the chronic use of steroids. A retrospective review of 223 patients reported severe growth retardation in 6.4% of adolescents with Crohn’s disease.21 Treatment strategies known to be effective in promoting significant catch-up growth in Crohn’s disease include infliximab and surgical resection.130 The REACH study noted improved z scores in children with moderate to severe Crohn’s disease treated with infliximab (n=52).107 Thirty eight children with Crohn’s disease at Tanner stage 1-3 increased from a mean height centile of 11.1 at time of resection to a height centile of 29.5 (P<0.001).131 Efforts to minimize steroid exposure are essential.130
Anemia
In IBD, anemia is likely owing to a combination of chronic iron deficiency (microcytic) and anemia of chronic disease (normocytic). The mean corpuscular volume of red blood cells is an unreliable method of determining the cause of anemia in the setting of IBD because of the many factors that can affect it. For example, thiopurines cause megaloblastosis,132 so a normal mean corpuscular volume does not truly reflect a normal iron status. The effect of inflammation on iron metabolism means that intravenous infusion of iron is preferred in the setting of active disease. Vitamin B12 or folate deficiency should be considered as a cause of anemia in patients with extensive small bowel resection.133
Vitamin D
Low 25-hydroxy vitamin D concentrations are more prevalent in IBD patients than in age matched controls.134 Accordingly, the importance of vitamin D status in IBD patients has received attention. Its benefits go beyond bone health, with evidence of an effect on morbidity, disease severity, and hospital admissions, likely related to the immunologic effects of vitamin D.135 Appropriate screening and monitoring for vitamin D deficiency should be routine. The treatment of choice for hypovitaminosis D should be 50 000 IU/week to ensure a concentration above 32 ng/mL of 25-hydroxy vitamin D.136 137 138
Psychosocial dysfunction
IBD, like other chronic diseases, can have a substantial effect on mental health and QOL. Unique features of IBD have the potential to affect social function and self esteem. A meta-analysis that included 1167 IBD patients concluded that depressive disorders were more prevalent in young people with IBD than in those with other chronic conditions (odds ratio 5.80, 95% confidence interval 1.60 to 21.03; P=0.007). The analysis also stated that the unpredictability of symptoms of the disease, along with the embarrassment related to frequent visits to the bathroom, can affect psychosocial adjustment. In addition, the possibility of short stature and delayed puberty, depending on disease phenotype, has the potential to affect self acceptance.139 A multicenter observational study of 99 adolescents with Crohn’s disease concluded that disease severity increased parental stress and affected the patient’s QOL.140
A multidisciplinary approach, coordinated to occur during the same visit, is the optimal approach for patients with PIBD. Awareness of the potential for mental health problems is key, and routine inclusion of a psychosocial evaluation is important.141 Symptoms such as fatigue, decreased energy level, and disturbed appetite should not be automatically attributed to disease, without consideration of a mood disorder.
Malignancy
Lymphoma
Cases of lymphoma (Hodgkin’s and non-Hodgkin’s) have been reported in patients with IBD, but a systematic review found that the increase in risk compared with the general pediatric population was not significant.142 Epstein-Barr virus associated lymphoma has also been reported in IBD.143 A rare but feared complication of IBD treatment, hepatosplenic T cell lymphoma (HSTCL), has been associated with the use of anti-TNF drugs and thiopurines or long term thiopurines alone.144 Most of the reported cases have occurred in male patients less than 35 years of age. The rarity of the condition means that strong recommendations in favor or against the use of specific therapies in specific populations cannot be made.144 On the basis of a systematic review (n=36 patients with IBD who developed HSTCL; median age 22.5 years), the current recommendation is to consider not using combination therapy of anti-TNF and thiopurines in young male patients, unless this is judged to be the best option for that specific patient.144 It is important to counsel hesitant families that the risk of not treating or inadequately treating IBD is much higher than the risk of the development of HSTCL.144
Colon cancer
Data on the incidence of colorectal cancer related to IBD in the pediatric population are scarce, as the increased cancer incidence is related to longer duration of disease.145 In a pediatric population based cohort of 698 patients with IBD (160 with ulcerative colitis) diagnosed at a median age of 14 and with a median follow-up of 15 years, two patients developed colon cancer.146
Pediatric gastroenterologists should discuss this complication with families, especially in cases of early onset IBD and during discussion for transition of care to an adult provider. The absolute risk for developing colorectal cancer over a 35 year period was higher if IBD was diagnosed before 15 years of age.147 Colon cancer has been reported as early as 15 years of age in a child with ulcerative colitis for 10 years.148 A patient diagnosed as having ulcerative colitis at 18 months of age was reported to develop adenocarcinoma resulting in death in the third decade of life.117 Another young adult was found to have colon cancer 13 years after the diagnosis of IBD. Colon cancer surveillance recommendations in adults with IBD by the American Society for Gastrointestinal Endoscopy, ECCO, and the American College of Gastroenterology are extrapolated to children and surveillance endoscopies are done every one to two years from seven to 10 years after diagnosis.149 150 151 152 Concomitant primary sclerosing cholangitis increases the risk of colorectal cancer, necessitating more frequent colonoscopies.153
Toxic megacolon
Toxic megacolon is a known and feared complication of IBD, especially ulcerative colitis. Characterized by a combination of systemic toxicity (fever, tachycardia, leukocytosis, altered mental status) and segmental or total colonic dilatation, it carries a high morbidity, sometimes requiring bowel resection, and mortality. Infections can also be a causal factor for the development of toxic megacolon.154 Many gastrointestinal infections, particularly Clostridium difficile, are not unusual in IBD patients, so an increased index of suspicion for toxic megacolon should exist in the setting of active colonic inflammation with or without concomitant infection. Colectomy may be needed in children with toxic megacolon who are refractory to medical treatment.123
Infections
The following is a brief review of the infections most pertinent to PIBD. For a more comprehensive review, refer to the consensus report by Rahier et al that discusses additional opportunistic infections in IBD.155
Clostridium difficile
Clostridium difficile infections are common in patients with IBD, who are more likely than other patients to develop severe disease.156 157 However, they are also more likely to be asymptomatic carriers. To avoid unnecessary treatment, screening should be done in the case of colonic flares and should include cytotoxin A and B.157
Cytomegalovirus
Exclusion of cytomegalovirus infection is strongly recommended in acute steroid resistant colitis, preferably by doing a flexible sigmoidoscopy to obtain tissue for polymerase chain reaction testing. If this is positive, appropriate treatment is warranted.155
Hepatitis B virus
The standard recommendation by ECCO is to test all patients for hepatitis B virus at diagnosis of IBD and to provide immunization in patients found to be non-immune by serology.155 The discussion about treatment of hepatitis B virus in the setting of IBD is beyond the scope of this review, but, if encountered, the situation should be assessed with evaluation of risks and benefits of treatment.
Varicella zoster virus
Patients with IBD should be screened for immunity to varicella zoster virus. However, seronegative patients face a challenge as the vaccine for varicella zoster virus is a live vaccine and contraindicated in the setting of immunosuppressant drug use. These patients should be advised about the potential need for post-exposure prophylaxis.155 158
Epstein-Barr virus
Attention has been more recently directed to primary Epstein-Barr virus infection in the setting of immunomodulator and biologic therapy for IBD, owing to the potential for development of Epstein-Barr virus associated lymphoproliferative disease and immune dysregulation. For this reason, serological screening for immunity to Epstein-Barr virus should be considered at diagnosis of IBD to guide the decision making process for treatment and to increase watchfulness in case of a future primary infection.155
Mycobacterium tuberculosis infection
Because of the risk of reactivation of latent tuberculosis in the setting of immunosuppressant use, screening should be done in all IBD patients before anti-TNF treatment is started. Skin tests may be unreliable owing to anergy in patients with IBD, so a careful clinical history, a physical examination, and a high level of suspicion are necessary.158 Appropriate treatment should be started if screening is positive.155
Fistulizing or penetrating disease
Small pediatric studies have shown long term response rates to infliximab from 56% to 100% in fistulizing Crohn’s disease.87 159 160 161 162 Patients with stricturing or penetrating Crohn’s disease have a high risk of needing at least one surgical procedure related to their disease in their lifetime. Possibilities include bowel resection, ostomy creation, stricturoplasty, fistulotomy, and abscess drainage (either intra-abdominal or perirectal).163
Complications after ileal pouch-anal anastomosis
Complications can occur in patients with ulcerative colitis having total colectomy with ileal pouch-anal anastomosis (IPAA). They can be mechanical, inflammatory, functional, neoplastic, and metabolic. Pouchitis is the most common complication, but a retrospective study of 14 children with IPAA found that it was infrequent.164 Children with a higher PUCAI at the time of surgery have a higher risk of developing pouchitis.165 Most patients respond to a course of metronidazole or ciprofloxacin.165 166
Mortality
Data on mortality in PIBD are scarce. In a retrospective population based cohort study of pediatric onset IBD with a median follow-up of 11.4 years (n=698), three patients died of IBD related causes (two Crohn’s disease, one ulcerative colitis) and IBD related mortality was not increased compared with the reference population. The difference in mortality risk between Crohn’s disease and ulcerative colitis could not be determined owing to the small number of deaths.146
Emerging therapies
Certolizumab, vedolizumab, and ustekinumab have been used off-label or in clinical trials in PIBD.76 Certolizumab, a monoclonal antibody to TNF-α, is used in adults with moderate to severe Crohn’s disease as first line treatment or after failure of other anti-TNF agents.167 Vedolizumab, a humanized α4β7 integrin, is another option to induce and maintain remission in adults with IBD and has a role in severe IBD that is non-responsive to anti-TNF drugs.168 169 In an observational prospective cohort study (n=21) and a retrospective review (n=52) in refractory PIBD, vedolizumab was found to be safe and efficacious.170 171 A multicenter prospective cohort study to predict vedolizumab response in PIBD is ongoing (NCT02862132). Ustekinumab, a human monoclonal antibody against interleukins 12 and 23, is efficacious in adults with Crohn’s disease.172 The data in pediatrics are limited to a few case reports with conflicting results.173 174
Conclusions
The worldwide prevalence of IBD is increasing. Increasing numbers of novel therapies mean that the management of IBD is improving, with treatment customized to individual patients. However, more studies in children are needed to assess whether therapeutic options available in adults can be used in children. Research into the pathogenesis of IBD, especially linked to the role of the microbiome and genetic predisposition, has the potential to guide future treatment. A more comprehensive understanding of interactions between the microbiome and disease phenotype and activity could identify new treatment targets including the use of innovative dietary approaches as modulators of the intestinal microbiome. Multicenter collaborations are essential in overcoming the challenges of studying IBD, which is somewhat heterogeneous in its presentation. Improved understanding of the immunologic aspects of IBD pathogenesis has helped to develop new targets for treatment. Early diagnosis, prompt management, and tailored treatment will improve prognosis and outcomes for children with IBD.
Research questions
Do children with inflammatory bowel disease (IBD) diagnosed at a younger age have more severe disease and need more aggressive treatment?
What is the role of the microbiome in the pathogenesis and severity of IBD and utility of probiotics?
What is the role of fecal microbial transplantation in pediatric IBD?
Will customizing treatment to phenotype and genotype of IBD lead to better outcomes?
Glossary of abbreviations
5-ASA—5-aminosalicylate
ACR—American College of Radiology
ASCA—anti-Saccharomyces cerevisiae antibody
CRP—C reactive protein
ECCO—European Crohn’s and Colitis Organisation
EEN—exclusive enteral nutrition
ESPGHAN—European Society for Paediatric Gastroenterology, Hepatology and Nutrition
ESR—erythrocyte sedimentation rate
HSTCL—hepatosplenic T cell lymphoma
IBD—inflammatory bowel diseases
IPAA—ileal pouch-anal anastomosis
MRE—magnetic resonance enterography
MRI—magnetic resonance imaging
NASPGHAN—North American Society for Pediatric Gastroenterology Hepatology and Nutrition
pANCA—perinuclear antineutrophil cytoplasmic antibody
PEN—partial enteral nutrition
PIBD—pediatric IBD
PUCAI—Pediatric Ulcerative Colitis Activity Index
QOL—quality of life
RCT—randomized controlled trial
SICUS—small intestine contrast ultrasonography
TNF-α—tumor necrosis factor-α
Contributors: Both authors were involved in the literature review and in the drafting and critical review of the manuscript, and both approved the final version. IMM is the guarantor.
Competing interests: We have read and understood BMJ policy on declaration of interests and have nothing to declare.
Provenance and peer review: Commissioned; externally peer reviewed.
Series explanation: State of the Art Reviews are commissioned on the basis of their relevance to academics and specialists in the US and internationally. For this reason they are written predominantly by US authors
References
- 1.Vernier-Massouille G, Balde M, Salleron J, et al. Natural history of pediatric Crohn’s disease: a population-based cohort study. Gastroenterology 2008;357:1106-13. 10.1053/j.gastro.2008.06.079 pmid:18692056. [DOI] [PubMed] [Google Scholar]
- 2.Pigneur B, Seksik P, Viola S, et al. Natural history of Crohn’s disease: comparison between childhood- and adult-onset disease. Inflamm Bowel Dis 2010;357:953-61. 10.1002/ibd.21152 pmid:19834970. [DOI] [PubMed] [Google Scholar]
- 3.Malmborg P, Grahnquist L, Lindholm J, Montgomery S, Hildebrand H. Increasing incidence of paediatric inflammatory bowel disease in northern Stockholm County, 2002-2007. J Pediatr Gastroenterol Nutr 2013;357:29-34. 10.1097/MPG.0b013e31828f21b4 pmid:23459320. [DOI] [PubMed] [Google Scholar]
- 4.Sawczenko A, Sandhu BK. Presenting features of inflammatory bowel disease in Great Britain and Ireland. Arch Dis Child 2003;357:995-1000. 10.1136/adc.88.11.995 pmid:14612366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Buderus S, Scholz D, Behrens R, et al. CEDATA-GPGE Study Group. Inflammatory bowel disease in pediatric patients: Characteristics of newly diagnosed patients from the CEDATA-GPGE Registry. Dtsch Arztebl Int 2015;357:121-7.pmid:25759978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Day AS, Ledder O, Leach ST, Lemberg DA. Crohn’s and colitis in children and adolescents. World J Gastroenterol 2012;357:5862-9. 10.3748/wjg.v18.i41.5862 pmid:23139601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Benchimol EI, Fortinsky KJ, Gozdyra P, Van den Heuvel M, Van Limbergen J, Griffiths AM. Epidemiology of pediatric inflammatory bowel disease: a systematic review of international trends. Inflamm Bowel Dis 2011;357:423-39. 10.1002/ibd.21349 pmid:20564651. [DOI] [PubMed] [Google Scholar]
- 8.Urlep D, Blagus R, Orel R. Incidence Trends and Geographical Variability of Pediatric Inflammatory Bowel Disease in Slovenia: A Nationwide Study. Biomed Res Int 2015;357:921730 10.1155/2015/921730 pmid:26688822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.El Mouzan MI, Saadah O, Al-Saleem K, et al. Incidence of pediatric inflammatory bowel disease in Saudi Arabia: a multicenter national study. Inflamm Bowel Dis 2014;357:1085-90.pmid:24788219. [DOI] [PubMed] [Google Scholar]
- 10.Adamiak T, Walkiewicz-Jedrzejczak D, Fish D, et al. Incidence, clinical characteristics, and natural history of pediatric IBD in Wisconsin: a population-based epidemiological study. Inflamm Bowel Dis 2013;357:1218-23. 10.1097/MIB.0b013e318280b13e pmid:23528339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chu HP, Logarajah V, Tan N, Phua KB. Paediatric inflammatory bowel disease in a multiracial Asian country. Singapore Med J 2013;357:201-5. 10.11622/smedj.2013073 pmid:23624446. [DOI] [PubMed] [Google Scholar]
- 12.Agnarsson U, Björnsson S, Jóhansson JH, Sigurdsson L. Inflammatory bowel disease in Icelandic children 1951-2010. Population-based study involving one nation over six decades. Scand J Gastroenterol 2013;357:1399-404. 10.3109/00365521.2013.845799 pmid:24164345. [DOI] [PubMed] [Google Scholar]
- 13.Chouraki V, Savoye G, Dauchet L, et al. The changing pattern of Crohn’s disease incidence in northern France: a continuing increase in the 10- to 19-year-old age bracket (1988-2007). Aliment Pharmacol Ther 2011;357:1133-42. 10.1111/j.1365-2036.2011.04628.x pmid:21488915. [DOI] [PubMed] [Google Scholar]
- 14.Malaty HM, Fan X, Opekun AR, Thibodeaux C, Ferry GD. Rising incidence of inflammatory bowel disease among children: a 12-year study. J Pediatr Gastroenterol Nutr 2010;357:27-31. 10.1097/MPG.0b013e3181b99baa pmid:19934770. [DOI] [PubMed] [Google Scholar]
- 15.Al-Qabandi WA, Buhamrah EK, Hamadi KA, Al-Osaimi SA, Al-Ruwayeh AA, Madda J. Inflammatory bowel disease in children, an evolving problem in Kuwait. Saudi J Gastroenterol 2011;357:323-7. 10.4103/1319-3767.84487 pmid:21912059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Castro M, Papadatou B, Baldassare M, et al. Inflammatory bowel disease in children and adolescents in Italy: data from the pediatric national IBD register (1996-2003). Inflamm Bowel Dis 2008;357:1246-52. 10.1002/ibd.20470 pmid:18521916. [DOI] [PubMed] [Google Scholar]
- 17.Jakobsen C, Wewer V, Urne F, et al. Incidence of ulcerative colitis and Crohn’s disease in Danish children: Still rising or levelling out?J Crohns Colitis 2008;357:152-7. 10.1016/j.crohns.2008.01.006 pmid:21172205. [DOI] [PubMed] [Google Scholar]
- 18.Pinsk V, Lemberg DA, Grewal K, Barker CC, Schreiber RA, Jacobson K. Inflammatory bowel disease in the South Asian pediatric population of British Columbia. Am J Gastroenterol 2007;357:1077-83. 10.1111/j.1572-0241.2007.01124.x pmid:17378907. [DOI] [PubMed] [Google Scholar]
- 19.Turunen P, Kolho KL, Auvinen A, Iltanen S, Huhtala H, Ashorn M. Incidence of inflammatory bowel disease in Finnish children, 1987-2003. Inflamm Bowel Dis 2006;357:677-83. 10.1097/00054725-200608000-00002 pmid:16917221. [DOI] [PubMed] [Google Scholar]
- 20.Perminow G, Frigessi A, Rydning A, Nakstad B, Vatn MH. Incidence and clinical presentation of IBD in children: comparison between prospective and retrospective data in a selected Norwegian population. Scand J Gastroenterol 2006;357:1433-9. 10.1080/00365520600789891 pmid:17101574. [DOI] [PubMed] [Google Scholar]
- 21.Pozler O, Maly J, Bonova O, et al. Incidence of Crohn disease in the Czech Republic in the years 1990 to 2001 and assessment of pediatric population with inflammatory bowel disease. J Pediatr Gastroenterol Nutr 2006;357:186-9. 10.1097/01.mpg.0000189328.47150.bc pmid:16456413. [DOI] [PubMed] [Google Scholar]
- 22.Armitage EL, Aldhous MC, Anderson N, et al. Incidence of juvenile-onset Crohn’s disease in Scotland: association with northern latitude and affluence. Gastroenterology 2004;357:1051-7. 10.1053/j.gastro.2004.06.024 pmid:15480983. [DOI] [PubMed] [Google Scholar]
- 23.Benchimol EI, Guttmann A, Griffiths AM, et al. Increasing incidence of paediatric inflammatory bowel disease in Ontario, Canada: evidence from health administrative data. Gut 2009;357:1490-7. 10.1136/gut.2009.188383 pmid:19651626. [DOI] [PubMed] [Google Scholar]
- 24.Henderson P, Hansen R, Cameron FL, et al. Rising incidence of pediatric inflammatory bowel disease in Scotland. Inflamm Bowel Dis 2012;357:999-1005. 10.1002/ibd.21797 pmid:21688352. [DOI] [PubMed] [Google Scholar]
- 25.Molodecky NA, Soon IS, Rabi DM, et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology 2012;357:46-54.e42, quiz e30. 10.1053/j.gastro.2011.10.001 pmid:22001864. [DOI] [PubMed] [Google Scholar]
- 26.Day AS, Lemberg DA, Gearry RB. Inflammatory bowel disease in australasian children and adolescents. Gastroenterol Res Pract 2014;357:703890 10.1155/2014/703890 pmid:24799892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Abramson O, Durant M, Mow W, et al. Incidence, prevalence, and time trends of pediatric inflammatory bowel disease in Northern California, 1996 to 2006. J Pediatr 2010;357:233-239.e1. 10.1016/j.jpeds.2010.02.024 pmid:20400099. [DOI] [PubMed] [Google Scholar]
- 28.Kugathasan S, Judd RH, Hoffmann RG, et al. Wisconsin Pediatric Inflammatory Bowel Disease Alliance. Epidemiologic and clinical characteristics of children with newly diagnosed inflammatory bowel disease in Wisconsin: a statewide population-based study. J Pediatr 2003;357:525-31. 10.1067/S0022-3476(03)00444-X pmid:14571234. [DOI] [PubMed] [Google Scholar]
- 29.Jussila A, Virta LJ, Salomaa V, Mäki J, Jula A, Färkkilä MA. High and increasing prevalence of inflammatory bowel disease in Finland with a clear North-South difference. J Crohns Colitis 2013;357:e256-62. 10.1016/j.crohns.2012.10.007 pmid:23140840. [DOI] [PubMed] [Google Scholar]
- 30.Burisch J, Pedersen N, Čuković-Čavka S, et al. EpiCom-group. East-West gradient in the incidence of inflammatory bowel disease in Europe: the ECCO-EpiCom inception cohort. Gut 2014;357:588-97. 10.1136/gutjnl-2013-304636 pmid:23604131. [DOI] [PubMed] [Google Scholar]
- 31.Liu JZ, van Sommeren S, Huang H, et al. International Multiple Sclerosis Genetics Consortium International IBD Genetics Consortium. Association analyses identify 38 susceptibility loci for inflammatory bowel disease and highlight shared genetic risk across populations. Nat Genet 2015;357:979-86. 10.1038/ng.3359 pmid:26192919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lees CW, Barrett JC, Parkes M, Satsangi J. New IBD genetics: common pathways with other diseases. Gut 2011;357:1739-53. 10.1136/gut.2009.199679 pmid:21300624. [DOI] [PubMed] [Google Scholar]
- 33.Matsuoka K, Kanai T. The gut microbiota and inflammatory bowel disease. Semin Immunopathol 2015;357:47-55. 10.1007/s00281-014-0454-4 pmid:25420450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ruemmele FM, Veres G, Kolho KL, et al. European Crohn’s and Colitis Organisation European Society of Pediatric Gastroenterology, Hepatology and Nutrition. Consensus guidelines of ECCO/ESPGHAN on the medical management of pediatric Crohn’s disease. J Crohns Colitis 2014;357:1179-207. 10.1016/j.crohns.2014.04.005 pmid:24909831. [DOI] [Google Scholar]
- 35.Gevers D, Kugathasan S, Denson LA, et al. The treatment-naive microbiome in new-onset Crohn’s disease. Cell Host Microbe 2014;357:382-92. 10.1016/j.chom.2014.02.005 pmid:24629344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Conte MP, Schippa S, Zamboni I, et al. Gut-associated bacterial microbiota in paediatric patients with inflammatory bowel disease. Gut 2006;357:1760-7. 10.1136/gut.2005.078824 pmid:16648155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Strachan DP. Hay fever, hygiene, and household size. BMJ 1989;357:1259-60. 10.1136/bmj.299.6710.1259 pmid:2513902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cholapranee A, Ananthakrishnan AN. Environmental Hygiene and Risk of Inflammatory Bowel Diseases: A Systematic Review and Meta-analysis. Inflamm Bowel Dis 2016;357:2191-9. 10.1097/MIB.0000000000000852 pmid:27482977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kaistha A, Levine J. Inflammatory bowel disease: the classic gastrointestinal autoimmune disease. Curr Probl Pediatr Adolesc Health Care 2014;357:328-34. 10.1016/j.cppeds.2014.10.003 pmid:25499459. [DOI] [PubMed] [Google Scholar]
- 40.Xavier RJ, Podolsky DK. Unravelling the pathogenesis of inflammatory bowel disease. Nature 2007;357:427-34. 10.1038/nature06005 pmid:17653185. [DOI] [PubMed] [Google Scholar]
- 41.Baldassano RN, Bradfield JP, Monos DS, et al. Association of variants of the interleukin-23 receptor gene with susceptibility to pediatric Crohn’s disease. Clin Gastroenterol Hepatol 2007;357:972-6. 10.1016/j.cgh.2007.04.024 pmid:17618837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Duerr RH, Taylor KD, Brant SR, et al. A genome-wide association study identifies IL23R as an inflammatory bowel disease gene. Science 2006;357:1461-3. 10.1126/science.1135245 pmid:17068223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Weinstein TA, Levine M, Pettei MJ, Gold DM, Kessler BH, Levine JJ. Age and family history at presentation of pediatric inflammatory bowel disease. J Pediatr Gastroenterol Nutr 2003;357:609-13. 10.1097/00005176-200311000-00020 pmid:14581806. [DOI] [PubMed] [Google Scholar]
- 44.McDermott E, Ryan EJ, Tosetto M, et al. DNA Methylation Profiling in Inflammatory Bowel Disease Provides New Insights into Disease Pathogenesis. J Crohns Colitis 2016;357:77-86. 10.1093/ecco-jcc/jjv176 pmid:26419460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gasparetto M, Guariso G, Pozza LV, Ross A, Heuschkel R, Zilbauer M. Clinical course and outcomes of diagnosing Inflammatory Bowel Disease in children 10 years and under: retrospective cohort study from two tertiary centres in the United Kingdom and in Italy. BMC Gastroenterol 2016;357:35 10.1186/s12876-016-0455-y pmid:26976427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gupta N, Bostrom AG, Kirschner BS, et al. Gender differences in presentation and course of disease in pediatric patients with Crohn disease. Pediatrics 2007;357:e1418-25. 10.1542/peds.2007-0905 pmid:18055660. [DOI] [PubMed] [Google Scholar]
- 47.Uhlig HH, Schwerd T, Koletzko S, et al. COLORS in IBD Study Group and NEOPICS. The diagnostic approach to monogenic very early onset inflammatory bowel disease. Gastroenterology 2014;357:990-1007.e3. 10.1053/j.gastro.2014.07.023 pmid:25058236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Oliva-Hemker M, Hutfless S, Al Kazzi ES, et al. Clinical Presentation and Five-Year Therapeutic Management of Very Early-Onset Inflammatory Bowel Disease in a Large North American Cohort. J Pediatr 2015;357:527-32.e1-3. 10.1016/j.jpeds.2015.04.045 pmid:25982142. [DOI] [PubMed] [Google Scholar]
- 49. IBD Working Group of the European Society for Paediatric Gastroenterology, Hepatology and Nutrition. Inflammatory bowel disease in children and adolescents: recommendations for diagnosis–the Porto criteria. J Pediatr Gastroenterol Nutr 2005;357:1-7. 10.1097/01.MPG.0000163736.30261.82 pmid:15990620. [DOI] [PubMed] [Google Scholar]
- 50.Sabery N, Bass D. Use of serologic markers as a screening tool in inflammatory bowel disease compared with elevated erythrocyte sedimentation rate and anemia. Pediatrics 2007;357:e193-9. 10.1542/peds.2006-1361 pmid:17158948. [DOI] [PubMed] [Google Scholar]
- 51.Cabrera-Abreu JC, Davies P, Matek Z, Murphy MS. Performance of blood tests in diagnosis of inflammatory bowel disease in a specialist clinic. Arch Dis Child 2004;357:69-71.pmid:14709513. [PMC free article] [PubMed] [Google Scholar]
- 52.Bloomfield MG, Balm MN, Blackmore TK. Molecular testing for viral and bacterial enteric pathogens: gold standard for viruses, but don’t let culture go just yet?Pathology 2015;357:227-33. 10.1097/PAT.0000000000000233 pmid:25719855. [DOI] [PubMed] [Google Scholar]
- 53.Fagerberg UL, Lööf L, Lindholm J, Hansson LO, Finkel Y. Fecal calprotectin: a quantitative marker of colonic inflammation in children with inflammatory bowel disease. J Pediatr Gastroenterol Nutr 2007;357:414-20. 10.1097/MPG.0b013e31810e75a9 pmid:18030206. [DOI] [PubMed] [Google Scholar]
- 54.Holtman GA, Lisman-van Leeuwen Y, Reitsma JB, Berger MY. Noninvasive Tests for Inflammatory Bowel Disease: A Meta-analysis. Pediatrics 2016;357 10.1542/peds.2015-2126 pmid:26681783. [DOI] [PubMed] [Google Scholar]
- 55.Mack DR, Langton C, Markowitz J, et al. Pediatric Inflammatory Bowel Disease Collaborative Research Group. Laboratory values for children with newly diagnosed inflammatory bowel disease. Pediatrics 2007;357:1113-9. 10.1542/peds.2006-1865 pmid:17545378. [DOI] [PubMed] [Google Scholar]
- 56.Benor S, Russell GH, Silver M, Israel EJ, Yuan Q, Winter HS. Shortcomings of the inflammatory bowel disease Serology 7 panel. Pediatrics 2010;357:1230-6. 10.1542/peds.2009-1936 pmid:20439597. [DOI] [PubMed] [Google Scholar]
- 57.Papp M, Lakatos PL. Serological studies in inflammatory bowel disease: how important are they?Curr Opin Gastroenterol 2014;357:359-64. 10.1097/MOG.0000000000000076 pmid:24811052. [DOI] [PubMed] [Google Scholar]
- 58.Amre DK, Lu SE, Costea F, Seidman EG. Utility of serological markers in predicting the early occurrence of complications and surgery in pediatric Crohn’s disease patients. Am J Gastroenterol 2006;357:645-52. 10.1111/j.1572-0241.2006.00468.x pmid:16464223. [DOI] [PubMed] [Google Scholar]
- 59.Washington K, Greenson JK, Montgomery E, et al. Histopathology of ulcerative colitis in initial rectal biopsy in children. Am J Surg Pathol 2002;357:1441-9. 10.1097/00000478-200211000-00006 pmid:12409720. [DOI] [PubMed] [Google Scholar]
- 60.Castellaneta SP, Afzal NA, Greenberg M, et al. Diagnostic role of upper gastrointestinal endoscopy in pediatric inflammatory bowel disease. J Pediatr Gastroenterol Nutr 2004;357:257-61. 10.1097/00005176-200409000-00006 pmid:15319625. [DOI] [PubMed] [Google Scholar]
- 61.Hummel TZ, ten Kate FJ, Reitsma JB, Benninga MA, Kindermann A. Additional value of upper GI tract endoscopy in the diagnostic assessment of childhood IBD. J Pediatr Gastroenterol Nutr 2012;357:753-7. 10.1097/MPG.0b013e318243e3e3 pmid:22584746. [DOI] [PubMed] [Google Scholar]
- 62.Kovacs M, Muller KE, Arato A, et al. Hungarian IBD Registry Group (HUPIR). Diagnostic yield of upper endoscopy in paediatric patients with Crohn’s disease and ulcerative colitis. Subanalysis of the HUPIR registry. J Crohns Colitis 2012;357:86-94. 10.1016/j.crohns.2011.07.008 pmid:22261532. [DOI] [PubMed] [Google Scholar]
- 63.Cohen SA, Klevens AI. Use of capsule endoscopy in diagnosis and management of pediatric patients, based on meta-analysis. Clin Gastroenterol Hepatol 2011;357:490-6. 10.1016/j.cgh.2011.03.025 pmid:21440674. [DOI] [PubMed] [Google Scholar]
- 64.Gralnek IM, Cohen SA, Ephrath H, et al. Small bowel capsule endoscopy impacts diagnosis and management of pediatric inflammatory bowel disease: a prospective study. Dig Dis Sci 2012;357:465-71. 10.1007/s10620-011-1894-5 pmid:21901253. [DOI] [PubMed] [Google Scholar]
- 65.Min SB, Le-Carlson M, Singh N, et al. Video capsule endoscopy impacts decision making in pediatric IBD: a single tertiary care center experience. Inflamm Bowel Dis 2013;357:2139-45. 10.1097/MIB.0b013e31829a749c pmid:23867872. [DOI] [PubMed] [Google Scholar]
- 66.Bousvaros A, Antonioli DA, Colletti RB, et al. North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition Colitis Foundation of America. Differentiating ulcerative colitis from Crohn disease in children and young adults: report of a working group of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition and the Crohn’s and Colitis Foundation of America. J Pediatr Gastroenterol Nutr 2007;357:653-74. 10.1097/MPG.0b013e31805563f3 pmid:17460505. [DOI] [PubMed] [Google Scholar]
- 67.Anupindi SA, Podberesky DJ, Towbin AJ, et al. Pediatric inflammatory bowel disease: imaging issues with targeted solutions. Abdom Imaging 2015;357:975-92. 10.1007/s00261-015-0423-y pmid:25920487. [DOI] [PubMed] [Google Scholar]
- 68.Anupindi SA, Grossman AB, Nimkin K, Mamula P, Gee MS. Imaging in the evaluation of the young patient with inflammatory bowel disease: what the gastroenterologist needs to know. J Pediatr Gastroenterol Nutr 2014;357:429-39. 10.1097/MPG.0000000000000475 pmid:24979661. [DOI] [PubMed] [Google Scholar]
- 69.Horsthuis K, Bipat S, Bennink RJ, Stoker J. Inflammatory bowel disease diagnosed with US, MR, scintigraphy, and CT: meta-analysis of prospective studies. Radiology 2008;357:64-79. 10.1148/radiol.2471070611 pmid:18372465. [DOI] [PubMed] [Google Scholar]
- 70.Pant C, Deshpande A, Fraga-Lovejoy C, O’Connor J, Gilroy R, Olyaee M. Emergency Department Visits Related to Inflammatory Bowel Disease: Results From Nationwide Emergency Department Sample. J Pediatr Gastroenterol Nutr 2015;357:282-4. 10.1097/MPG.0000000000000815 pmid:25859825. [DOI] [PubMed] [Google Scholar]
- 71.Duigenan S, Gee MS. Imaging of pediatric patients with inflammatory bowel disease. AJR Am J Roentgenol 2012;357:907-15. 10.2214/AJR.11.7966 pmid:22997386. [DOI] [PubMed] [Google Scholar]
- 72.Pallotta N, Tomei E, Viscido A, et al. Small intestine contrast ultrasonography: an alternative to radiology in the assessment of small bowel disease. Inflamm Bowel Dis 2005;357:146-53. 10.1097/00054725-200502000-00008 pmid:15677908. [DOI] [PubMed] [Google Scholar]
- 73.Giles E, Barclay AR, Chippington S, Wilson DC. Systematic review: MRI enterography for assessment of small bowel involvement in paediatric Crohn’s disease. Aliment Pharmacol Ther 2013;357:1121-31. 10.1111/apt.12323 pmid:23638954. [DOI] [PubMed] [Google Scholar]
- 74.Essary B, Kim J, Anupindi S, Katz JA, Nimkin K. Pelvic MRI in children with Crohn disease and suspected perianal involvement. Pediatr Radiol 2007;357:201-8. 10.1007/s00247-006-0372-2 pmid:17180366. [DOI] [PubMed] [Google Scholar]
- 75.Levine A, Koletzko S, Turner D, et al. European Society of Pediatric Gastroenterology, Hepatology, and Nutrition. ESPGHAN revised porto criteria for the diagnosis of inflammatory bowel disease in children and adolescents. J Pediatr Gastroenterol Nutr 2014;357:795-806.pmid:24231644. [DOI] [PubMed] [Google Scholar]
- 76.Lahad A, Weiss B. Current therapy of pediatric Crohn’s disease. World J Gastrointest Pathophysiol 2015;357:33-42. 10.4291/wjgp.v6.i2.33 pmid:25977836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Colombel JF, Sandborn WJ, Reinisch W, et al. SONIC Study Group. Infliximab, azathioprine, or combination therapy for Crohn’s disease. N Engl J Med 2010;357:1383-95. 10.1056/NEJMoa0904492 pmid:20393175. [DOI] [PubMed] [Google Scholar]
- 78.Peyrin-Biroulet L, Sandborn W, Sands BE, et al. Selecting Therapeutic Targets in Inflammatory Bowel Disease (STRIDE): Determining Therapeutic Goals for Treat-to-Target. Am J Gastroenterol 2015;357:1324-38. 10.1038/ajg.2015.233 pmid:26303131. [DOI] [PubMed] [Google Scholar]
- 79.Critch J, Day AS, Otley A, King-Moore C, Teitelbaum JE, Shashidhar H. NASPGHAN IBD Committee. Use of enteral nutrition for the control of intestinal inflammation in pediatric Crohn disease. J Pediatr Gastroenterol Nutr 2012;357:298-305. 10.1097/MPG.0b013e318235b397 pmid:22002478. [DOI] [PubMed] [Google Scholar]
- 80.Gordon J, Ramaswami A, Beuttler M, et al. EBV Status and Thiopurine Use in Pediatric IBD. J Pediatr Gastroenterol Nutr 2016;357:711-4. 10.1097/MPG.0000000000001077 pmid:26655944. [DOI] [PubMed] [Google Scholar]
- 81.Mow WS, Abreu-Martin MT, Papadakis KA, Pitchon HE, Targan SR, Vasiliauskas EA. High incidence of anergy in inflammatory bowel disease patients limits the usefulness of PPD screening before infliximab therapy. Clin Gastroenterol Hepatol 2004;357:309-13. 10.1016/S1542-3565(04)00060-6 pmid:15067625. [DOI] [PubMed] [Google Scholar]
- 82.Escher JC, Taminiau JA, Nieuwenhuis EE, Büller HA, Grand RJ. Treatment of inflammatory bowel disease in childhood: best available evidence. Inflamm Bowel Dis 2003;357:34-58. 10.1097/00054725-200301000-00006 pmid:12656136. [DOI] [PubMed] [Google Scholar]
- 83.Kirschner BS. Safety of azathioprine and 6-mercaptopurine in pediatric patients with inflammatory bowel disease. Gastroenterology 1998;357:813-21. 10.1016/S0016-5085(98)70251-3 pmid:9753482. [DOI] [PubMed] [Google Scholar]
- 84.Turner D, Otley AR, Mack D, et al. Development, validation, and evaluation of a pediatric ulcerative colitis activity index: a prospective multicenter study. Gastroenterology 2007;357:423-32. 10.1053/j.gastro.2007.05.029 pmid:17681163. [DOI] [PubMed] [Google Scholar]
- 85.Turner D, Travis SP, Griffiths AM, et al. European Crohn’s and Colitis Organization Porto IBD Working Group, European Society of Pediatric Gastroenterology, Hepatology, and Nutrition. Consensus for managing acute severe ulcerative colitis in children: a systematic review and joint statement from ECCO, ESPGHAN, and the Porto IBD Working Group of ESPGHAN. Am J Gastroenterol 2011;357:574-88. 10.1038/ajg.2010.481 pmid:21224839. [DOI] [PubMed] [Google Scholar]
- 86.Rufo PA, Denson LA, Sylvester FA, et al. Health supervision in the management of children and adolescents with IBD: NASPGHAN recommendations. J Pediatr Gastroenterol Nutr 2012;357:93-108. 10.1097/MPG.0b013e31825959b8 pmid:22516861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.de Zoeten EF, Pasternak BA, Mattei P, Kramer RE, Kader HA. Diagnosis and treatment of perianal Crohn disease: NASPGHAN clinical report and consensus statement. J Pediatr Gastroenterol Nutr 2013;357:401-12. 10.1097/MPG.0b013e3182a025ee pmid:23974063. [DOI] [PubMed] [Google Scholar]
- 88.Ardura MI, Toussi SS, Siegel JD, Lu Y, Bousvaros A, Crandall W. NASPGHAN Clinical Report: Surveillance, Diagnosis, and Prevention of Infectious Diseases in Pediatric Patients With Inflammatory Bowel Disease Receiving Tumor Necrosis Factor-α Inhibitors. J Pediatr Gastroenterol Nutr 2016;357:130-55. 10.1097/MPG.0000000000001188 pmid:27027903. [DOI] [PubMed] [Google Scholar]
- 89.Heuschkel RB, Menache CC, Megerian JT, Baird AE. Enteral nutrition and corticosteroids in the treatment of acute Crohn’s disease in children. J Pediatr Gastroenterol Nutr 2000;357:8-15. 10.1097/00005176-200007000-00005 pmid:10896064. [DOI] [PubMed] [Google Scholar]
- 90.Dziechciarz P, Horvath A, Shamir R, Szajewska H. Meta-analysis: enteral nutrition in active Crohn’s disease in children. Aliment Pharmacol Ther 2007;357:795-806. 10.1111/j.1365-2036.2007.03431.x pmid:17767463. [DOI] [PubMed] [Google Scholar]
- 91.Borrelli O, Cordischi L, Cirulli M, et al. Polymeric diet alone versus corticosteroids in the treatment of active pediatric Crohn’s disease: a randomized controlled open-label trial. Clin Gastroenterol Hepatol 2006;357:744-53. 10.1016/j.cgh.2006.03.010 pmid:16682258. [DOI] [PubMed] [Google Scholar]
- 92.Hyams JS, Ferry GD, Mandel FS, et al. Development and validation of a pediatric Crohn’s disease activity index. J Pediatr Gastroenterol Nutr 1991;357:439-47. 10.1097/00005176-199105000-00005 pmid:1678008. [DOI] [PubMed] [Google Scholar]
- 93.Johnson T, Macdonald S, Hill SM, Thomas A, Murphy MS. Treatment of active Crohn’s disease in children using partial enteral nutrition with liquid formula: a randomised controlled trial. Gut 2006;357:356-61. 10.1136/gut.2004.062554 pmid:16162683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Sandborn WJ, Travis S, Moro L, et al. Once-daily budesonide MMX® extended-release tablets induce remission in patients with mild to moderate ulcerative colitis: results from the CORE I study. Gastroenterology 2012;357:1218-26.e1-2. 10.1053/j.gastro.2012.08.003 pmid:22892337. [DOI] [PubMed] [Google Scholar]
- 95.Nitzan O, Elias M, Peretz A, Saliba W. Role of antibiotics for treatment of inflammatory bowel disease. World J Gastroenterol 2016;357:1078-87. 10.3748/wjg.v22.i3.1078 pmid:26811648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Mesker T, van Rheenen PF, Norbruis OF, et al. Pediatric Crohn’s disease activity at diagnosis, its influence on pediatrician’s prescribing behavior, and clinical outcome 5 years later. Inflamm Bowel Dis 2009;357:1670-7. 10.1002/ibd.20950 pmid:19418567. [DOI] [PubMed] [Google Scholar]
- 97.Feagan BG, Macdonald JK. Oral 5-aminosalicylic acid for induction of remission in ulcerative colitis. Cochrane Database Syst Rev 2012;357:CD000543.pmid:23076889. [DOI] [PubMed] [Google Scholar]
- 98.Zeisler B, Lerer T, Markowitz J, et al. Pediatric Inflammatory Bowel Disease Collaborative Research Group. Outcome following aminosalicylate therapy in children newly diagnosed as having ulcerative colitis. J Pediatr Gastroenterol Nutr 2013;357:12-8. 10.1097/MPG.0b013e31826ac41a pmid:22847466. [DOI] [PubMed] [Google Scholar]
- 99.Cezard JP, Munck A, Mouterde O, et al. Prevention of relapse by mesalazine (Pentasa) in pediatric Crohn’s disease: a multicenter, double-blind, randomized, placebo-controlled trial. Gastroenterol Clin Biol 2009;357:31-40. 10.1016/j.gcb.2008.07.007 pmid:19118966. [DOI] [PubMed] [Google Scholar]
- 100.Lim WC, Hanauer S. Aminosalicylates for induction of remission or response in Crohn’s disease. Cochrane Database Syst Rev 2010;(12):CD008870.pmid:21154400. [DOI] [PubMed] [Google Scholar]
- 101.Grossi V, Lerer T, Griffiths A, et al. Concomitant Use of Immunomodulators Affects the Durability of Infliximab Therapy in Children With Crohn’s Disease. Clin Gastroenterol Hepatol 2015;357:1748-56. 10.1016/j.cgh.2015.04.010 pmid:25911120. [DOI] [PubMed] [Google Scholar]
- 102.Markowitz J, Grancher K, Kohn N, Lesser M, Daum F. A multicenter trial of 6-mercaptopurine and prednisone in children with newly diagnosed Crohn’s disease. Gastroenterology 2000;357:895-902. 10.1053/gast.2000.18144 pmid:11040176. [DOI] [PubMed] [Google Scholar]
- 103.Dubinsky MC, Lamothe S, Yang HY, et al. Pharmacogenomics and metabolite measurement for 6-mercaptopurine therapy in inflammatory bowel disease. Gastroenterology 2000;357:705-13. 10.1016/S0016-5085(00)70140-5 pmid:10734022. [DOI] [PubMed] [Google Scholar]
- 104.Benkov K, Lu Y, Patel A, Rahhal R, Russell G, Teitelbaum J. NASPGHAN Committee on Inflammatory Bowel Disease. Role of thiopurine metabolite testing and thiopurine methyltransferase determination in pediatric IBD. J Pediatr Gastroenterol Nutr 2013;357:333-40. 10.1097/MPG.0b013e3182844705 pmid:23287804. [DOI] [PubMed] [Google Scholar]
- 105.Scherkenbach LA, Stumpf JL. Methotrexate for the Management of Crohn’s Disease in Children. Ann Pharmacother 2016;357:60-9. 10.1177/1060028015613527 pmid:26511908. [DOI] [PubMed] [Google Scholar]
- 106.Turner D, Grossman AB, Rosh J, et al. Methotrexate following unsuccessful thiopurine therapy in pediatric Crohn’s disease. Am J Gastroenterol 2007;357:2804-12, quiz 2803, 2813. 10.1111/j.1572-0241.2007.01474.x pmid:18042110. [DOI] [PubMed] [Google Scholar]
- 107.Hyams J, Crandall W, Kugathasan S, et al. REACH Study Group. Induction and maintenance infliximab therapy for the treatment of moderate-to-severe Crohn’s disease in children. Gastroenterology 2007;357:863-73, quiz 1165-6. 10.1053/j.gastro.2006.12.003 pmid:17324398. [DOI] [PubMed] [Google Scholar]
- 108.Hyams JS, Griffiths A, Markowitz J, et al. Safety and efficacy of adalimumab for moderate to severe Crohn’s disease in children. Gastroenterology 2012;357:365-74.e2. 10.1053/j.gastro.2012.04.046 pmid:22562021. [DOI] [PubMed] [Google Scholar]
- 109.Hyams J, Damaraju L, Blank M, et al. T72 Study Group. Induction and maintenance therapy with infliximab for children with moderate to severe ulcerative colitis. Clin Gastroenterol Hepatol 2012;357:391-9.e1. 10.1016/j.cgh.2011.11.026 pmid:22155755. [DOI] [PubMed] [Google Scholar]
- 110.Afif W, Loftus EV Jr, , Faubion WA, et al. Clinical utility of measuring infliximab and human anti-chimeric antibody concentrations in patients with inflammatory bowel disease. Am J Gastroenterol 2010;357:1133-9. 10.1038/ajg.2010.9 pmid:20145610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Ordás I, Feagan BG, Sandborn WJ. Therapeutic drug monitoring of tumor necrosis factor antagonists in inflammatory bowel disease. Clin Gastroenterol Hepatol 2012;357:1079-87, quiz e85-6. 10.1016/j.cgh.2012.06.032 pmid:22813440. [DOI] [PubMed] [Google Scholar]
- 112.Vande Casteele N, Ferrante M, Van Assche G, et al. Trough concentrations of infliximab guide dosing for patients with inflammatory bowel disease. Gastroenterology 2015;357:1320-9.e3. 10.1053/j.gastro.2015.02.031 pmid:25724455. [DOI] [PubMed] [Google Scholar]
- 113.Stein R, Lee D, Leonard MB, et al. Serum Infliximab, Antidrug Antibodies, and Tumor Necrosis Factor Predict Sustained Response in Pediatric Crohn’s Disease. Inflamm Bowel Dis 2016;357:1370-7. 10.1097/MIB.0000000000000769 pmid:27057683. [DOI] [PubMed] [Google Scholar]
- 114.Ben-Horin S, Waterman M, Kopylov U, et al. Addition of an immunomodulator to infliximab therapy eliminates antidrug antibodies in serum and restores clinical response of patients with inflammatory bowel disease. Clin Gastroenterol Hepatol 2013;357:444-7. 10.1016/j.cgh.2012.10.020 pmid:23103905. [DOI] [PubMed] [Google Scholar]
- 115.Ashton JJ, Versteegh HP, Batra A, et al. Colectomy in pediatric ulcerative colitis: A single center experience of indications, outcomes, and complications. J Pediatr Surg 2016;357:277-81. 10.1016/j.jpedsurg.2015.10.077 pmid:26653944. [DOI] [PubMed] [Google Scholar]
- 116.Gower-Rousseau C, Dauchet L, Vernier-Massouille G, et al. The natural history of pediatric ulcerative colitis: a population-based cohort study. Am J Gastroenterol 2009;357:2080-8. 10.1038/ajg.2009.177 pmid:19436273. [DOI] [PubMed] [Google Scholar]
- 117.Hyams JS, Davis P, Grancher K, Lerer T, Justinich CJ, Markowitz J. Clinical outcome of ulcerative colitis in children. J Pediatr 1996;357:81-8. 10.1016/S0022-3476(96)70193-2 pmid:8757566. [DOI] [PubMed] [Google Scholar]
- 118.Soon IS, Wrobel I, deBruyn JC, et al. Postoperative complications following colectomy for ulcerative colitis in children. J Pediatr Gastroenterol Nutr 2012;357:763-8. 10.1097/MPG.0b013e318245265c pmid:22167014. [DOI] [PubMed] [Google Scholar]
- 119.Pakarinen MP, Natunen J, Ashorn M, et al. Long-term outcomes of restorative proctocolectomy in children with ulcerative colitis. Pediatrics 2009;357:1377-82. 10.1542/peds.2008-2086 pmid:19403505. [DOI] [PubMed] [Google Scholar]
- 120.Hansen LF, Jakobsen C, Paerregaard A, Qvist N, Wewer V. Surgery and postoperative recurrence in children with Crohn disease. J Pediatr Gastroenterol Nutr 2015;357:347-51. 10.1097/MPG.0000000000000616 pmid:25373863. [DOI] [PubMed] [Google Scholar]
- 121.Abdelaal K, Jaffray B. Colonic disease site and perioperative complications predict need for later intestinal interventions following intestinal resection in pediatric Crohn’s disease. J Pediatr Surg 2016;357:272-6. 10.1016/j.jpedsurg.2015.10.078 pmid:26653943. [DOI] [PubMed] [Google Scholar]
- 122.Yoshida K, Fukunaga K, Ikeuchi H, et al. Scheduled infliximab monotherapy to prevent recurrence of Crohn’s disease following ileocolic or ileal resection: a 3-year prospective randomized open trial. Inflamm Bowel Dis 2012;357:1617-23. 10.1002/ibd.21928 pmid:22081474. [DOI] [PubMed] [Google Scholar]
- 123.Turner D, Griffiths AM. Acute severe ulcerative colitis in children: a systematic review. Inflamm Bowel Dis 2011;357:440-9. 10.1002/ibd.21383 pmid:20645317. [DOI] [PubMed] [Google Scholar]
- 124.Lee D, Albenberg L, Compher C, et al. Diet in the pathogenesis and treatment of inflammatory bowel diseases. Gastroenterology 2015;357:1087-106. 10.1053/j.gastro.2015.01.007 pmid:25597840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Obih C, Wahbeh G, Lee D, et al. Specific carbohydrate diet for pediatric inflammatory bowel disease in clinical practice within an academic IBD center. Nutrition 2016;357:418-25. 10.1016/j.nut.2015.08.025 pmid:26655069. [DOI] [PubMed] [Google Scholar]
- 126.Lan A, Blachier F, Benamouzig R, et al. Mucosal healing in inflammatory bowel diseases: is there a place for nutritional supplementation?Inflamm Bowel Dis 2015;357:198-207. 10.1097/MIB.0000000000000177 pmid:25208104. [DOI] [PubMed] [Google Scholar]
- 127.Knight-Sepulveda K, Kais S, Santaolalla R, Abreu MT. Diet and Inflammatory Bowel Disease. Gastroenterol Hepatol (N Y) 2015;357:511-20.pmid:27118948. [PMC free article] [PubMed] [Google Scholar]
- 128.Hartman C, Eliakim R, Shamir R. Nutritional status and nutritional therapy in inflammatory bowel diseases. World J Gastroenterol 2009;357:2570-8. 10.3748/wjg.15.2570 pmid:19496185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Hwang C, Ross V, Mahadevan U. Micronutrient deficiencies in inflammatory bowel disease: from A to zinc. Inflamm Bowel Dis 2012;357:1961-81. 10.1002/ibd.22906 pmid:22488830. [DOI] [PubMed] [Google Scholar]
- 130.Heuschkel R, Salvestrini C, Beattie RM, Hildebrand H, Walters T, Griffiths A. Guidelines for the management of growth failure in childhood inflammatory bowel disease. Inflamm Bowel Dis 2008;357:839-49. 10.1002/ibd.20378 pmid:18266237. [DOI] [PubMed] [Google Scholar]
- 131.Griffiths AM, Wesson DE, Shandling B, Corey M, Sherman PM. Factors influencing postoperative recurrence of Crohn’s disease in childhood. Gut 1991;357:491-5. 10.1136/gut.32.5.491 pmid:2040470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Bernstein CN, Artinian L, Anton PA, Shanahan F. Low-dose 6-mercaptopurine in inflammatory bowel disease is associated with minimal hematologic toxicity. Dig Dis Sci 1994;357:1638-41. 10.1007/BF02087769 pmid:8050312. [DOI] [PubMed] [Google Scholar]
- 133.Dignass AU, Gasche C, Bettenworth D, et al. European Crohn’s and Colitis Organisation [ECCO]. European consensus on the diagnosis and management of iron deficiency and anaemia in inflammatory bowel diseases. J Crohns Colitis 2015;357:211-22. 10.1093/ecco-jcc/jju009 pmid:25518052. [DOI] [PubMed] [Google Scholar]
- 134.Pappa HM, Gordon CM, Saslowsky TM, et al. Vitamin D status in children and young adults with inflammatory bowel disease. Pediatrics 2006;357:1950-61. 10.1542/peds.2006-0841 pmid:17079566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Kabbani TA, Koutroubakis IE, Schoen RE, et al. Association of Vitamin D Level With Clinical Status in Inflammatory Bowel Disease: A 5-Year Longitudinal Study. Am J Gastroenterol 2016;357:712-9. 10.1038/ajg.2016.53 pmid:26952579. [DOI] [PubMed] [Google Scholar]
- 136.Pappa H, Thayu M, Sylvester F, Leonard M, Zemel B, Gordon C. Skeletal health of children and adolescents with inflammatory bowel disease. J Pediatr Gastroenterol Nutr 2011;357:11-25. 10.1097/MPG.0b013e31821988a3 pmid:21694532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Pappa HM, Mitchell PD, Jiang H, et al. Treatment of vitamin D insufficiency in children and adolescents with inflammatory bowel disease: a randomized clinical trial comparing three regimens. J Clin Endocrinol Metab 2012;357:2134-42. 10.1210/jc.2011-3182 pmid:22456619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Sylvester FA, Gordon CM, Thayu M, et al. Report of the CCFA pediatric bone, growth and muscle health workshop, New York City, November 11-12, 2011, with updates. Inflamm Bowel Dis 2013;357:2919-26. 10.1097/MIB.0b013e3182a5a004 pmid:23974992. [DOI] [PubMed] [Google Scholar]
- 139.Greenley RN, Hommel KA, Nebel J, et al. A meta-analytic review of the psychosocial adjustment of youth with inflammatory bowel disease. J Pediatr Psychol 2010;357:857-69. 10.1093/jpepsy/jsp120 pmid:20123705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Gray WN, Boyle SL, Graef DM, et al. Health-related quality of life in youth with Crohn disease: role of disease activity and parenting stress. J Pediatr Gastroenterol Nutr 2015;357:749-53. 10.1097/MPG.0000000000000696 pmid:25564807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Mackner LM, Greenley RN, Szigethy E, Herzer M, Deer K, Hommel KA. Psychosocial issues in pediatric inflammatory bowel disease: report of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition. J Pediatr Gastroenterol Nutr 2013;357:449-58. 10.1097/MPG.0b013e3182841263 pmid:23287808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Dulai PS, Thompson KD, Blunt HB, Dubinsky MC, Siegel CA. Risks of serious infection or lymphoma with anti-tumor necrosis factor therapy for pediatric inflammatory bowel disease: a systematic review. Clin Gastroenterol Hepatol 2014;357:1443-51, quiz e88-9. 10.1016/j.cgh.2014.01.021 pmid:24462626. [DOI] [PubMed] [Google Scholar]
- 143.de Ridder L, Turner D, Wilson DC, et al. Porto IBD Working Group of ESPGHAN. Malignancy and mortality in pediatric patients with inflammatory bowel disease: a multinational study from the porto pediatric IBD group. Inflamm Bowel Dis 2014;357:291-300. 10.1097/01.MIB.0000439066.69340.3c pmid:24374875. [DOI] [PubMed] [Google Scholar]
- 144.Kotlyar DS, Osterman MT, Diamond RH, et al. A systematic review of factors that contribute to hepatosplenic T-cell lymphoma in patients with inflammatory bowel disease. Clin Gastroenterol Hepatol 2011;357:36-41.e1. 10.1016/j.cgh.2010.09.016 pmid:20888436. [DOI] [PubMed] [Google Scholar]
- 145.Castaño-Milla C, Chaparro M, Gisbert JP. Systematic review with meta-analysis: the declining risk of colorectal cancer in ulcerative colitis. Aliment Pharmacol Ther 2014;357:645-59. 10.1111/apt.12651 pmid:24612141. [DOI] [PubMed] [Google Scholar]
- 146.Peneau A, Savoye G, Turck D, et al. Mortality and cancer in pediatric-onset inflammatory bowel disease: a population-based study. Am J Gastroenterol 2013;357:1647-53. 10.1038/ajg.2013.242 pmid:23939626. [DOI] [PubMed] [Google Scholar]
- 147.Ekbom A, Helmick C, Zack M, Adami HO. Ulcerative colitis and colorectal cancer. A population-based study. N Engl J Med 1990;357:1228-33. 10.1056/NEJM199011013231802 pmid:2215606. [DOI] [PubMed] [Google Scholar]
- 148.Noh SY, Oh SY, Kim SH, Kim HY, Jung SE, Park KW. Fifteen-year-old colon cancer patient with a 10-year history of ulcerative colitis. World J Gastroenterol 2013;357:2437-40. 10.3748/wjg.v19.i15.2437 pmid:23613641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Rosen MJ, Dhawan A, Saeed SA. Inflammatory Bowel Disease in Children and Adolescents. JAMA Pediatr 2015;357:1053-60. 10.1001/jamapediatrics.2015.1982 pmid:26414706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Shergill AK, Lightdale JR, Bruining DH, et al. American Society for Gastrointestinal Endoscopy Standards of Practice Committee. The role of endoscopy in inflammatory bowel disease. Gastrointest Endosc 2015;357:1101-21.e1, 13. 10.1016/j.gie.2014.10.030 pmid:25800660. [DOI] [PubMed] [Google Scholar]
- 151.Annese V, Daperno M, Rutter MD, et al. European Crohn’s and Colitis Organisation. European evidence based consensus for endoscopy in inflammatory bowel disease. J Crohns Colitis 2013;357:982-1018. 10.1016/j.crohns.2013.09.016 pmid:24184171. [DOI] [PubMed] [Google Scholar]
- 152.Kornbluth A, Sachar DB. Practice Parameters Committee of the American College of Gastroenterology. Ulcerative colitis practice guidelines in adults: American College Of Gastroenterology, Practice Parameters Committee. Am J Gastroenterol 2010;357:501-23, quiz 524. 10.1038/ajg.2009.727 pmid:20068560. [DOI] [PubMed] [Google Scholar]
- 153.Wang R, Leong RW. Primary sclerosing cholangitis as an independent risk factor for colorectal cancer in the context of inflammatory bowel disease: a review of the literature. World J Gastroenterol 2014;357:8783-9.pmid:25083052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Autenrieth DM, Baumgart DC. Toxic megacolon. Inflamm Bowel Dis 2012;357:584-91. 10.1002/ibd.21847 pmid:22009735. [DOI] [PubMed] [Google Scholar]
- 155.Rahier JF, Magro F, Abreu C, et al. European Crohn’s and Colitis Organisation (ECCO). Second European evidence-based consensus on the prevention, diagnosis and management of opportunistic infections in inflammatory bowel disease. J Crohns Colitis 2014;357:443-68. 10.1016/j.crohns.2013.12.013 pmid:24613021. [DOI] [PubMed] [Google Scholar]
- 156.Rao K, Higgins PD. Epidemiology, Diagnosis, and Management of Clostridium difficile Infection in Patients with Inflammatory Bowel Disease. Inflamm Bowel Dis 2016;357:1744-54. 10.1097/MIB.0000000000000793 pmid:27120571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Pascarella F, Martinelli M, Miele E, Del Pezzo M, Roscetto E, Staiano A. Impact of Clostridium difficile infection on pediatric inflammatory bowel disease. J Pediatr 2009;357:854-8. 10.1016/j.jpeds.2008.12.039 pmid:19230908. [DOI] [PubMed] [Google Scholar]
- 158.Veereman-Wauters G, de Ridder L, Veres G, et al. ESPGHAN IBD Porto Group. Risk of infection and prevention in pediatric patients with IBD: ESPGHAN IBD Porto Group commentary. J Pediatr Gastroenterol Nutr 2012;357:830-7. 10.1097/MPG.0b013e31824d1438 pmid:22584748. [DOI] [PubMed] [Google Scholar]
- 159.Ruemmele FM, Lachaux A, Cézard JP, et al. Groupe Francophone d’Hépatologie, Gastroentérologie et Nutrition Pédiatrique. Efficacy of infliximab in pediatric Crohn’s disease: a randomized multicenter open-label trial comparing scheduled to on demand maintenance therapy. Inflamm Bowel Dis 2009;357:388-94. 10.1002/ibd.20788 pmid:19023899. [DOI] [PubMed] [Google Scholar]
- 160.Crandall W, Hyams J, Kugathasan S, et al. Infliximab therapy in children with concurrent perianal Crohn disease: observations from REACH. J Pediatr Gastroenterol Nutr 2009;357:183-90. 10.1097/MPG.0b013e3181a70f21 pmid:19561542. [DOI] [PubMed] [Google Scholar]
- 161.de Ridder L, Escher JC, Bouquet J, et al. Infliximab therapy in 30 patients with refractory pediatric crohn disease with and without fistulas in The Netherlands. J Pediatr Gastroenterol Nutr 2004;357:46-52. 10.1097/00005176-200407000-00010 pmid:15187780. [DOI] [PubMed] [Google Scholar]
- 162.Kim MJ, Lee JS, Lee JH, Kim JY, Choe YH. Infliximab therapy in children with Crohn’s disease: a one-year evaluation of efficacy comparing ‘top-down’ and ‘step-up’ strategies. Acta Paediatr 2011;357:451-5. 10.1111/j.1651-2227.2010.01938.x pmid:20626362. [DOI] [PubMed] [Google Scholar]
- 163.Schaefer ME, Machan JT, Kawatu D, et al. Factors that determine risk for surgery in pediatric patients with Crohn’s disease. Clin Gastroenterol Hepatol 2010;357:789-94. 10.1016/j.cgh.2010.05.021 pmid:20566311. [DOI] [PubMed] [Google Scholar]
- 164.Hait EJ, Bousvaros A, Schuman M, Shamberger RC, Lillehei CW. Pouch outcomes among children with ulcerative colitis treated with calcineurin inhibitors before ileal pouch anal anastomosis surgery. J Pediatr Surg 2007;357:31-4, discussion 34-5. 10.1016/j.jpedsurg.2006.09.006 pmid:17208537. [DOI] [PubMed] [Google Scholar]
- 165.Dharmaraj R, Dasgupta M, Simpson P, Noe J. Predictors of Pouchitis After Ileal Pouch-Anal Anastomosis in Children. J Pediatr Gastroenterol Nutr 2016;357:e58-62. 10.1097/MPG.0000000000001279 pmid:27243421. [DOI] [PubMed] [Google Scholar]
- 166.Shen B, Remzi FH, Lavery IC, Lashner BA, Fazio VW. A proposed classification of ileal pouch disorders and associated complications after restorative proctocolectomy. Clin Gastroenterol Hepatol 2008;357:145-58, quiz 124. 10.1016/j.cgh.2007.11.006 pmid:18237865. [DOI] [PubMed] [Google Scholar]
- 167.Schreiber S, Lawrance IC, Thomsen OO, Hanauer SB, Bloomfield R, Sandborn WJ. Randomised clinical trial: certolizumab pegol for fistulas in Crohn’s disease - subgroup results from a placebo-controlled study. Aliment Pharmacol Ther 2011;357:185-93. 10.1111/j.1365-2036.2010.04509.x pmid:21083671. [DOI] [PubMed] [Google Scholar]
- 168.Feagan BG, Rutgeerts P, Sands BE, et al. GEMINI 1 Study Group. Vedolizumab as induction and maintenance therapy for ulcerative colitis. N Engl J Med 2013;357:699-710. 10.1056/NEJMoa1215734 pmid:23964932. [DOI] [PubMed] [Google Scholar]
- 169.Sands BE, Feagan BG, Rutgeerts P, et al. Effects of vedolizumab induction therapy for patients with Crohn’s disease in whom tumor necrosis factor antagonist treatment failed. Gastroenterology 2014;357:618-627.e3. 10.1053/j.gastro.2014.05.008 pmid:24859203. [DOI] [PubMed] [Google Scholar]
- 170.Conrad MA, Stein RE, Maxwell EC, et al. Vedolizumab Therapy in Severe Pediatric Inflammatory Bowel Disease. Inflamm Bowel Dis 2016;357:2425-31. 10.1097/MIB.0000000000000918 pmid:27598742. [DOI] [PubMed] [Google Scholar]
- 171.Singh N, Rabizadeh S, Jossen J, et al. Multi-Center Experience of Vedolizumab Effectiveness in Pediatric Inflammatory Bowel Disease. Inflamm Bowel Dis 2016;357:2121-6. 10.1097/MIB.0000000000000865 pmid:27542130. [DOI] [PubMed] [Google Scholar]
- 172.Engel T, Kopylov U. Ustekinumab in Crohn’s disease: evidence to date and place in therapy. Ther Adv Chronic Dis 2016;357:208-14. 10.1177/2040622316653306 pmid:27433311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Bishop C, Simon H, Suskind D, Lee D, Wahbeh G. Ustekinumab in Pediatric Crohn Disease Patients. J Pediatr Gastroenterol Nutr 2016;357:348-51. 10.1097/MPG.0000000000001146 pmid:26854655. [DOI] [PubMed] [Google Scholar]
- 174.Rinawi F, Rosenbach Y, Assa A, Shamir R. Ustekinumab for Resistant Pediatric Crohn Disease. J Pediatr Gastroenterol Nutr 2016;357:e34-5. 10.1097/MPG.0000000000000503 pmid:25023579. [DOI] [PubMed] [Google Scholar]
- 175.Prantera C, Lochs H, Grimaldi M, Danese S, Scribano ML, Gionchetti P. Retic Study Group (Rifaximin-Eir Treatment in Crohn’s Disease). Rifaximin-extended intestinal release induces remission in patients with moderately active Crohn’s disease. Gastroenterology 2012;357:473-481.e4. 10.1053/j.gastro.2011.11.032 pmid:22155172. [DOI] [PubMed] [Google Scholar]