Abstract
Pemafibrate is the first clinically-available selective peroxisome proliferator-activated receptor α modulator (SPPARMα) that has been shown to effectively improve hypertriglyceridemia and low high-density lipoprotein cholesterol (HDL-C) levels. Global gene expression analysis reveals that the activation of PPARα by pemafibrate induces fatty acid (FA) uptake, binding, and mitochondrial or peroxisomal oxidation as well as ketogenesis in mouse liver. Pemafibrate most profoundly induces HMGCS2 and PDK4, which regulate the rate-limiting step of ketogenesis and glucose oxidation, respectively, compared to other fatty acid metabolic genes in human hepatocytes. This suggests that PPARα plays a crucial role in nutrient flux in the human liver. Additionally, pemafibrate induces clinically favorable genes, such as ABCA1, FGF21, and VLDLR. Furthermore, pemafibrate shows anti-inflammatory effects in vascular endothelial cells. Pemafibrate is predicted to exhibit beneficial effects in patients with atherogenic dyslipidemia and diabetic microvascular complications.
Keywords: pemafibrate, SPPARMα, ketogenesis, fatty acid β-oxidation, ASCVD, EndMT
1. Introduction
Although low density lipoprotein cholesterol (LDL-C)-lowering therapy by statins has been proven to reduce the events of atherosclerotic cardiovascular disease (ASCVD) [1,2], there still remains a high residual cardiovascular risk from elevated triglycerides (TG) and low HDL cholesterol (HDL-C) levels [3,4,5,6]. Synthetic PPARα ligands and fibrates have been shown to effectively reduce plasma TG levels by 25–50% and increase HDL-C levels by 5–20% [7,8,9,10]. Therefore, theoretically, fibrates are suitable drugs to use as an add-on statin treatment to improve hypertriglyceridemia and atherogenic dyslipidemia. However, there is a lack of adequate evidence to support statin-fibrate combination therapy for the prevention of definitive mortality rate. In addition, the use of fibrates in patients with hepatic and renal insufficiency has been limited due to adverse drug reactions (ADRs) such as plasma transaminase and creatinine elevation, as well as reduced estimated glomerular filtration rates (eGFRs) [11,12,13,14]. Under these circumstances, pemafibrate was developed as a selective peroxisome proliferator-activated receptor α modulator (SPPARMα) that enhances the beneficial effects and reduces the adverse effects of fibrates. To date, 50 papers have been published on this subject and few papers reported the effect of pemafibrate on target gene expression. Through the limited reports, we describe the pemafibrate-regulated genes and potential clinical implications.
2. Pemafibrate as a Novel SPPARMα
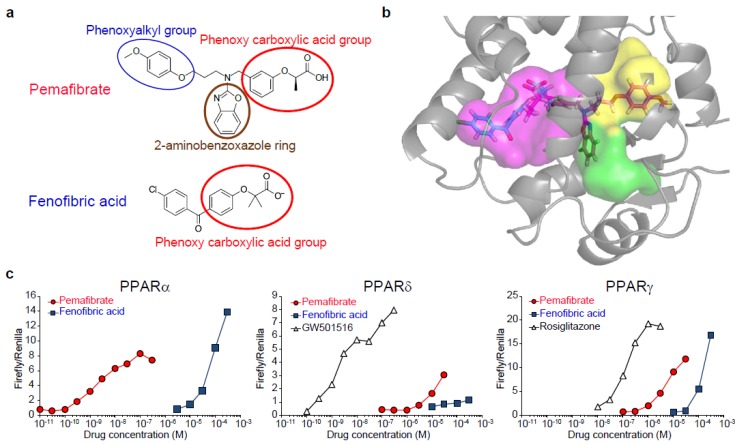
Pemafibrate (K-877, Parmodia®) was developed as a novel SPPARMα that enhances PPARα activity and selectivity by introducing a 2-aminobenzoxazolic ring and phenoxyalkyl chain into fibric acid (Figure 1a) [15,16,17]. These side-chains confer a Y-shape structure and fill the entire ligand-binding pocket of PPARα [18] (Figure 1b), thereby allosterically changing the PPARα conformation to enhance complex formation with coactivators such as peroxisome proliferative activated receptor gamma coactivator 1α (PGC1α) and exhibiting full agonistic activity. Actually, pemafibrate has greater PPARα activation potency than fenofibrate, along with a lower EC50 value (1.5 nM) and a higher degree of subtype selectivity (>2000-fold) (Figure 1c) [19]. In preclinical studies, pemafibrate exhibited a greater TG-lowering effect than fenofibrate in normolipidemic and hypertriglyceridemic rodent models [15,20,21]. In addition, in human apoA-I transgenic mice, pemafibrate treatment resulted in a greater increase in levels of plasma h-apoAI, a major component of HDL, than occurred with fenofibrate treatment [15,22]. Furthermore, pemafibrate has been shown to reduce atherosclerotic lesion areas in Ldlr-null mice [17] and western diet-fed APOE2 KI mice [22]. Although fibrates have been specifically shown to induce peroxisome proliferation and related hepatomegaly and hepatocellular carcinoma in rodents [23,24,25], pemafibrate causes less weight gain of the liver than fenofibrate [15]. Under the fed condition, the liver accumulated the highest concentration of pemafibrate and reached 105 nM after four weeks of treatment with a 0.0006% (w/w) pemafibrate-containing diet, which is an equivalent or higher dose than needed to demonstrate pharmacological action [22,26,27]. As indicated in Figure 1c, pemafibrate was unable to activate PPARγ or PPARδ at this concentration. In addition, the therapeutic dose of pemafibrate is 0.2–0.4 mg/day, which is equivalent to the dose of 0.004–0.008 mg/kg/day (based on a 50 kg human); therefore, it is unlikely that pemafibrate shows the other PPARs subtype-mediated pharmacological effect in clinical use.
Figure 1.
Structure and PPARα selectivity of pemafibrate. (a) Structure of pemafibrate and fenofibrate. (b) Binding mode of the ligand with human PPARα. Pemafibrate in magenta and fenofibrate in blue. The binding pocket is divided into three pharmacophore regions according to the interactions with the ligands. While fenofibric acid occupies the magenta cavity, 2-aminobenozoxazole ring and phenoxyalkyl group of Y-shaped pemafibrate occupies the green cavity and yellow cavity, respectively. Therefore, pemafibrate fills all the areas of the ligand-binding pocket. Reprinted from Yamamoto Y, et al. with permission from Elsevier [18]. (c) Transactivation profile of pemafibrate. Transactivation curves for human PPARα, PPARδ, and PPARγ are shown. Reproduced Raza-Iqbal S., et al. with permission from authors [19].
Pemafibrate was approved in Japan 2017 for the treatment of dyslipidemia [28,29,30,31,32,33,34,35,36,37,38]. A phase II study showed that 0.05–0.4 mg/day pemafibrate significantly reduced plasma TG levels (−30.9% to −42.7%) and increased HDL-C levels (11.9% to 21.0%) [29]. Although the difference was not statistically significant, the improvement of these parameters was more significant with pemafibrate than fenofibrate. The incidence of adverse events (AEs) in the pemafibrate treatment group was comparable to those in the placebo and 100 mg/day fenofibrate groups. However, the incidence of ADRs in the pemafibrate treatment group was lower than those in the placebo and 100 mg/day fenofibrate groups [29,31]. In addition, when compared to placebo and fenofibrate treatment, pemafibrate significantly increased the level of plasma FGF21, which is an endocrine factor regulating glucose uptake, metabolism, and energy expenditure [39]. Therefore, pemafibrate could replace fibrates as the first clinically-available SPPARMα to improve atherogenic dyslipidemia and prevent macro- and microvascular risks.
3. Pemafibrate Regulates the Availability of FA and Glucose Oxidation
Species differences have been well documented for PPARα-regulated genes, such as those involved in peroxisome biogenesis and peroxisomal FA β-oxidation [40,41,42]. In addition, whether PPARα mediates gene expression regulation by pemafibrate and whether human exposure to pemafibrate regulates the same target genes as those found in mice are still a matter of debate. To predict the mode of action and untoward effects of pemafibrate in humans, we carried out microarray analyses and compared the data of pemafibrate-treated primary human hepatocytes and mouse livers [19].
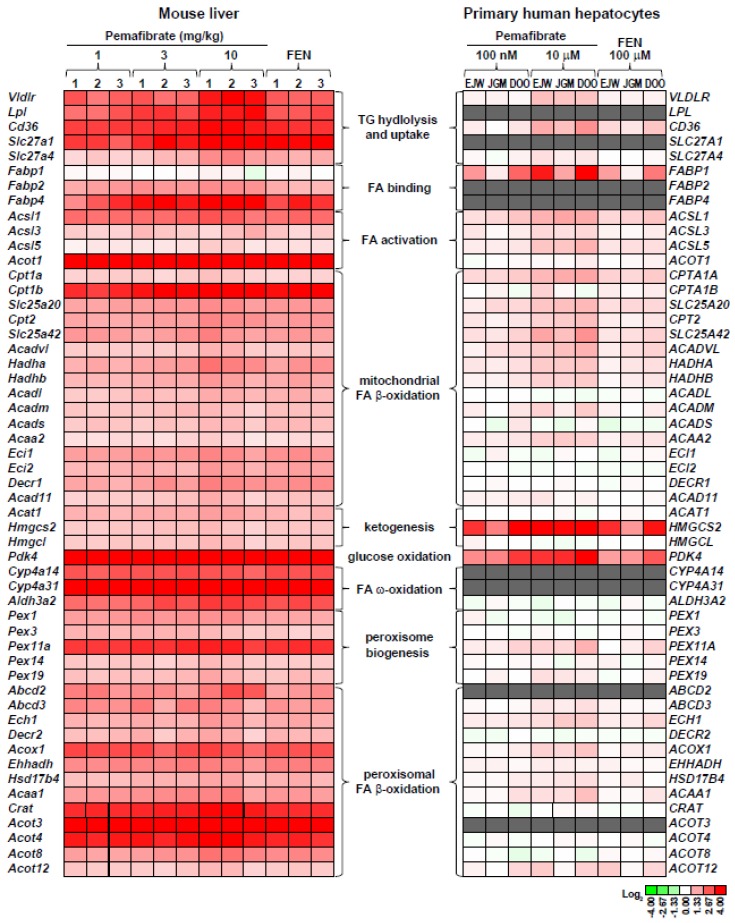
Global gene expression profiling clearly demonstrated that pemafibrate regulates the entire FA catabolism in mouse liver. Pemafibrate significantly induces Vldlr, TG hydrolysis (Lpl), FA cellular uptake (Cd36/Fat, Slc27a1, and Slc27a4), FA binding (Fabp2 and Fabp4), FA activation (Acsl1, Acsl3, Acsl5, and Acot1), FA ω-oxidation (Cyp4a14, Cyp4a31, and Aldh3a2), and peroxisomal (Abcd2, Abcbd3, Ech1, Decr2, Acox1, Ehhadh, Hsd17b4, Acaa1, Crat, Acot3, Acot4, and Acot8) and mitochondrial (Cpt1, Cpt2, Slc25a20, Acadvl, Acadl, Acads, Acadm, Acad11, Ehhadh, Hadha, Hadhb, and Decr1) FA β-oxidation, and ketogenesis (Acat1, Hmgcs2, and Hmgcl). In addition, pemafibrate induces peroxisome biogenesis genes (Pex1, Pex3, Pex11a, Pex14, and Pex19). The upregulation of these genes was not observed in the pemafibrate-treated Ppara-null mouse liver [19]. In accordance with our results, Takei et al. also reported that the effect of pemafibrate was abolished in Ppara-null mice [21]. Thus, these observations indicate that PPARα is crucial for the regulation of FA catabolic genes in mouse liver following pemafibrate treatment.
Similarly, pemafibrate induced VLDLR, FABP1, and mitochondrial FA β-oxidation gene (ACSL1, ACSL5, CPT1A, CPT2, SLC25A20, ACADVL, HADHA, HADHB, and ACAA2) expression in human hepatocytes, as seen in the livers of pemafibrate-treated mice. However, the induction of these genes was much lower in the human hepatocytes (Figure 2). Additionally, pemafibrate did not induce almost all FA ω-oxidation, peroxisomal FA β-oxidation, and peroxisome biogenesis genes expressions. The first step of FA ω-oxidation is ω-hydroxylation, which is catalyzed by the CYP4A family. Generated products are further metabolized to dicarboxylic acid by cytosolic aldehyde dehydrogenase, which is encoded by ALDH3A2, and they are efficiently metabolized by peroxisomal FA β-oxidation [43,44]. Numerous reports clearly indicated that the CYP4A family of enzymes are regulated by PPARα in rodent livers and are shown to parallel the induction of peroxisomal fatty acid β-oxidation enzymes and peroxisome proliferation [45]. In contrast, respect to the induction of CYP4A subtype is controversial in humans. Some studies showed that fibrates induce CYP4A11 mRNA expression in primary human hepatocytes and PPARα overexpressed HepG2 cells [46,47]. However, 100 μM of fenofibric acid, a concentration which is equal with our previous study, has been reported to fail induction of CYP4A11 expression in HepG2 cells [41]. Although it is difficult to declare the possibility to induce FA ω-oxidation enzyme in humans at present, peroxisome proliferation and related liver toxicities would not occur following a clinical dose of pemafibrate treatment.
Figure 2.
Effect of pemafibrate on fatty acid metabolism-related gene expression. Heat map illustrating the genes regulated by pemafibrate treatment in mouse liver and primary hepatocytes. Gray boxes represent the absence call or no probe of the genes from microarray data.
Interestingly, pemafibrate most profoundly induced PDK4 and HMGCS2 gene expression in the primary human hepatocytes. Robust induction of PDK4 indicated inactivation of pyruvate dehydrogenase (PDH) and glucose oxidation [48,49,50]. In contrast, HMGCS2 expression has been reported to control not only ketogenesis but also mitochondrial fatty acid oxidation in HepG2 cells [51]. In addition, this report also showed that the expression of FGF21 (another target of pemafibrate) is upregulated by HMGCS2 activity or acetoacetate, which is the oxidized form of the ketone bodies. Furthermore, the ketone body, β-hydroxybutyrate, as an inhibitor of class I histone deacetylases (HDAC), and β-hydroxybutyrate-integrated histone H3 lysine 9 (H3K9bhb) are associated with the upregulation of genes involved in the starvation-responsive pathways, including the PPAR signaling pathway [52]. Thus, PPARα activation by pemafibrate cooperatively regulates nutrient availability through the induction of the key target genes, namely PDK4 and HMGCS2, which suppress the availability of carbohydrate oxidation and enhance acyl-CoA flux. This thereby facilitates mitochondrial long-chain fatty acid β-oxidation and ketogenesis in human hepatocytes. As a result, pemafibrate reduces the availability of acetyl-CoA for de novo lipogenesis and VLDL secretion.
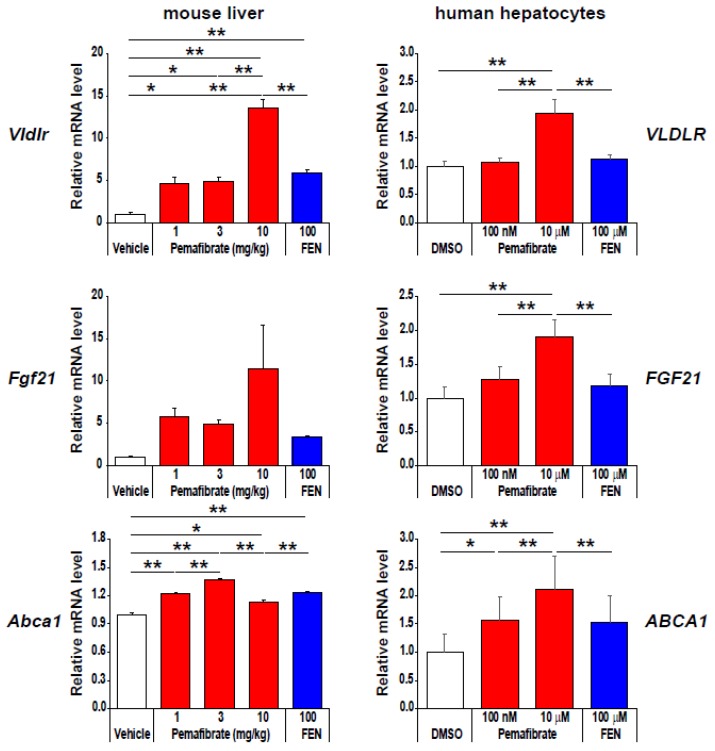
4. Pharmacologically Favorable Target Genes of Pemafibrate as a SPPARMα
As shown in Figure 3, compared to fenofibrate, pemafibrate effectively induces the expression of pharmacologically favorable genes, such as very-low-density lipoprotein receptor (VLDLR), ATP binding cassette subfamily A member 1 (ABCA1), and fibroblast growth factor 21 (FGF21), by maximizing PPARα activation [19]. VLDLR is a member of the LDL-receptor family and is expressed in many tissues, including skeletal muscles, heart, and adipose tissues, whereas its expression is very low in the liver, under normal conditions [53,54]. VLDLR binds TG-rich lipoproteins such as chylomicron and VLDL and mediates the uptake of TG-rich lipoproteins by peripheral tissues through LPL-dependent lipolysis or receptor-mediated endocytosis. Importantly, Gao et al. [55] reported that fenofibrate induces liver Vldlr expression in a PPARα-dependent manner and that the TG-lowering effect of fenofibrate was abolished in Vldlr-null mice. In addition, although LPL is typically not expressed in the adult liver [56], pemafibrate PPARα dependently induced the expression of Lpl in the mouse liver. Thus, pemafibrate enhances TG-rich lipoprotein hydrolysis and uptake by coordinated regulation of Vldlr, Lpl, and Cd36 expression. ABCA1, a member of the superfamily of ATP-binding cassette (ABC) transporters, regulates the formation and function of HDL by facilitating the efflux of cholesterol and phosphatidylcholine to lipid-poor apoAI [57,58]. In fact, pemafibrate significantly induced ABCA1 and ABCG1 in human primary macrophages and enhanced HDL stimulated cholesterol efflux [22]. ABCA1 not only plays an important role in the initial step of reverse cholesterol transport (RCT) but is also involved in the anti-inflammatory action to suppress the expression of pro-inflammatory factors [59,60]. Therefore, pemafibrate-mediated increased ABCA1 expression could contribute to HDL-C elevation as well as anti-inflammatory and anti-atherosclerotic activities. FGF21 is a member of the fibroblast growth factor family [39,61], and its administration has been shown to reduce fasting plasma glucose, TG, insulin, and glucagon levels in diabetic rhesus monkeys [62]. FGF21 is a direct target of PPARα [63,64], and pemafibrate increases fasting and postprandial FGF21 levels along with improving dyslipidemia in humans [65]. Interestingly, CREBH [66] and HMGCS2 [51], the liver target genes of pemafibrate, have been reported to regulate FGF21 gene expression. Moreover, similar upregulation of Abca1, Crebh, and Fgf21 was observed in pemafibrate-treated Ldlr knockout mice liver [26]. Thus, pemafibrate enhances the combination of PPARα, CREBH, and HMGCS2 for the regulation of FGF21 expression.
Figure 3.
Pemafibrate effectively induces VLDLR, FGF21, and ABCA1 mRNA expression in primary human hepatocytes. Data represent ± s.e.m. * P < 0.05; ** P < 0.01. Reproduced Raza-Iqbal S., et al. with permission from authors [19].
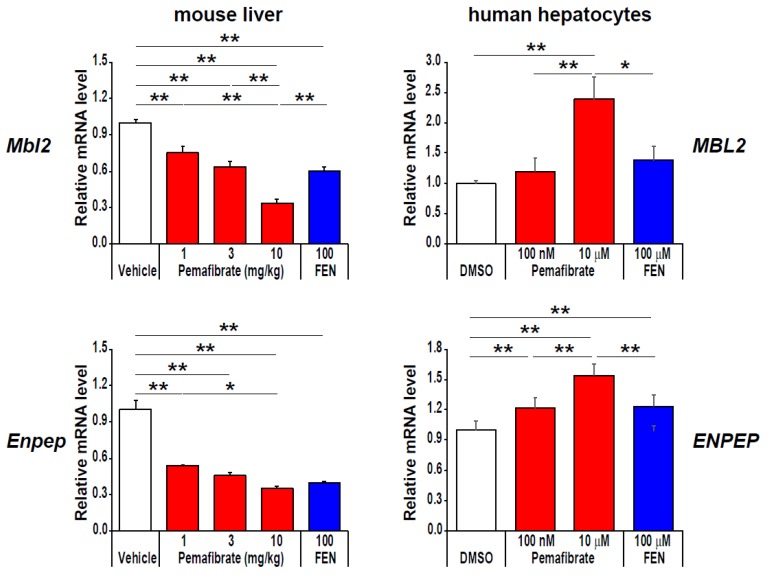
Beyond regulation of nutrient oxidation, pemafibrate induces mannose-binding lectin 2 (MBL2) and glutamyl aminopeptidase (ENPEP) only in human hepatocytes (Figure 4). MBL is a soluble pattern recognition molecule involved in the humoral innate immune system [67,68]. In consecutive non-diabetic men, the serum MBL concentration was reduced in obese individuals accompanied by low insulin sensitivity and increased levels of inflammatory markers [69]. ENPEP encodes aminopeptidase A (APA), a member of the M1 endopeptidase family, involved in the catabolic pathway of the renin-angiotensin-aldosterone system that converts angiotensin II to angiotensin III [70,71,72]. In an animal study, the loss of function of ENPEP led to hypertension, and recombinant APA reduced the systolic blood pressure (SBP) [73]. Moreover, a rare nonsense variant in ENPEP is reported to be associated with increased SBP [74]. Therefore, these additional pemafibrate targets are likely to reduce cardiovascular disease risks.
Figure 4.
Pemafibrate effectively induces MBL2 and ENPEP mRNA expression in primary human hepatocytes. Data represent ± s.e.m. * P < 0.05; ** P < 0.01. Reproduced Raza-Iqbal S., et al. with permission from authors [19].
Dysfunction and injury of vascular endothelial cells play a critical role in the pathogenesis of ASCVD and chronic kidney disease (CKD) [75,76,77]. ASCVD and CKD share common risk factors including hypertension, hyperglycemia, obesity, and dyslipidemia and are associated with endothelial activation and dysfunction. In particular, high glucose-induced reactive oxygen species (ROS) have been shown to be involved in vascular dysfunction via a diacylglycerol (DAG)-protein kinase C (PKC)-dependent activation of nicotinamide adenine dinucleotide phosphate NAD(P)H oxidase pathway. Pemafibrate has been reported to reduce Fn1, Tgfb1, Nox4, and Ncf1 expression, and reduce DAG level, PKC activity, and oxidative stress marker (urinary 8-OHdG excretion) level in kidneys of diabetic db/db mice [78]. Pemafibrate also reduces serum starvation induced monocyte chemoattractant protein-1(MCP-1), regulated on activation, normal T cell expressed and secreted (RANTES), interleukin 6 (IL6), and interferon gamma (IFNγ) expression and secretion in human coronary endothelial cells (HCECs) [79]. Besides its role in inflammation and ROS production, we found that pemafibrate suppresses high glucose-induced endothelial-mesenchymal transition (EndMT) in human umbilical vein endothelial cells (HUVECs). EndMT has emerged as an important process in the pathobiology of valve calcification, myocardial fibrosis, macrovascular complications, and microvascular complications such as diabetic nephropathy and retinopathy [80,81,82]. Experimental evidence demonstrated that TGFβ and Wnt/β-catenin signaling play a role in EndMT and may further contribute to tissue fibrosis [83,84,85]. Interestingly, pemafibrate reduces high glucose-induced TGFB2, COL1A2, CX3CL1, VCAM1 and DKK1 expression in HUVECs (Tanaka et al. personal communication). Likewise, fenofibrate has been reported to inhibit TGFβ-induced endothelin-1 (ET-1) expression in human microvascular endothelial cells [86]. ET-1 is a major vasoactive peptide that has been implicated in organ fibrosis through stimulation of EndMT [87,88]. In addition, fenofibrate has been reported to reduce progression of albuminuria and improve diabetic retinopathy [89,90,91]. Therefore, pemafibrate would be expected to prevent endothelial activation and dysfunction, thereby revealing protective effects against diabetic retinopathy, nephropathy, neuropathy, and ASCVD.
5. Possible Mechanism for the Gene Expression Regulation Induced by Pemafibrate?
Finally, we will discuss a potential mechanism for transcriptional regulation of hepatic target genes via PPARα activation by pemafibrate. As described in the text, PPARα activation by pemafibrate not only activates transcription of hepatic lipid metabolism genes, but also represses transcription of pro-inflammatory and EndMT-related genes. From the numerous observations, several models have been proposed for gene transcriptional regulation induced by PPARα [92,93,94]. In particular, PPARα functions as obligate heterodimers with retinoid X receptor (RXR). Ligand activated PPARα-RXR heterodimer mainly binds to DR1 elements termed PPAR response elements (PPREs) and recruits numerous coactivators, including CBP/p300 and SRC/p160 family, which contain histone acetyl transferase (HAT) activity, mediators, and the transcriptional preinitiation complex (PIC) [95,96,97,98]. This mechanism explains the main PPARα-dependent transactivation because DNA binding domain (DBD) mutant of PPARα (PPARαDISS), which maintains heterodimerization and coactivator interaction ability, lost PPRE binding and transactivation of PPRE-driven reporter genes [99]. On the other hand, transcriptional repression by PPARα is mainly mediated through protein-protein interactions. Ligand-activated PPARα has been reported to directly interact with pro-inflammatory transcription factor p65 and c-Jun, thereby suppressing their target genes such as IL6 and TNFα [100,101,102]. Interestingly, transcriptional repression ability is retained in PPARαDISS, indicating PPARα-dependent transrepression of the pro-inflammatory signaling pathway is PPRE-independent [99]. In addition, ligand-activated PPARα binds to coactivator of GRIP1/TIF2, thereby interfering with the C/EBPβ-induced fibrinogen-β gene transcription [103]. Furthermore, several nuclear receptors such as HNF4s, COUP-TFs, and RXR homodimer bind DR1 PPREs and may modulate PPARα-regulated gene expression [104,105,106,107]. Therefore, pemafibrate-induced gene expression appears as a combination of these multiple mechanisms.
6. Conclusions
PPARα regulates many hepatic metabolic genes along with lipid and glucose metabolism during prolonged starvation at the transcription levels and produces ketone bodies to provide metabolic fuel for the extrahepatic tissues. Despite accumulating evidence of the residual cardiovascular risks resulting from elevated TGs and lower HDL-C levels, low potent synthetic PPARα agonists (fibrates) have not shown enough evidence to reduce the definitive mortality rate when combined with statin treatment, despite an improvement in dyslipidemia. To overcome this issue, pemafibrate, a more potent and subtype-selective SPPARMα, was developed. By maximizing PPARα activation, pemafibrate effectively enhances TG hydrolysis, FA uptake, FA β-oxidation, and ketogenesis and thereby stimulates plasma TG hydrolysis and reduces VLDL secretion. In addition, pemafibrate enhances ABCA1-mediated HDL neogenesis and prevents the transfer of HDL-cholesteryl esters into TG-rich lipoproteins through the TG-lowering effect of pemafibrate. Through these mechanisms, pemafibrate effectively improves hypertriglyceridemia and low HDL-C levels. Importantly, PPARα activation by pemafibrate induces not only the generation of FAs via TG hydrolysis but also the generation of ketone bodies via FA β-oxidation and ketogenesis. In turn, the FAs could further activate PPARα, and the ketone bodies could promote the transcriptional activity of PPARα. Therefore, pemafibrate is expected to exert strong pharmacological effects and novel therapeutic action through a positive feedback loop and cooperative target gene regulation (Figure 5). In fact, pemafibrate induces clinically favorable key target genes (VLDLR, FGF21, ABCA1, MBL2, and ENPEP) and thereby has the therapeutic potential to address the residual cardiovascular risk. In addition, pemafibrate would expect to show vascular endothelial cell protective effects and prevent diabetic microvascular complications. Currently, a major outcome study, PROMINENT (Pemafibrate to Reduce cardiovascular OutcoMes by reducing triglycerides IN diabetic patiENTs), is underway to investigate whether pemafibrate reduces cardiovascular events in type 2 diabetic patients with atherogenic dyslipidemia [108]. This study will evaluate the role of pemafibrate in the management of residual cardiovascular risk as an add-on therapy to statins.
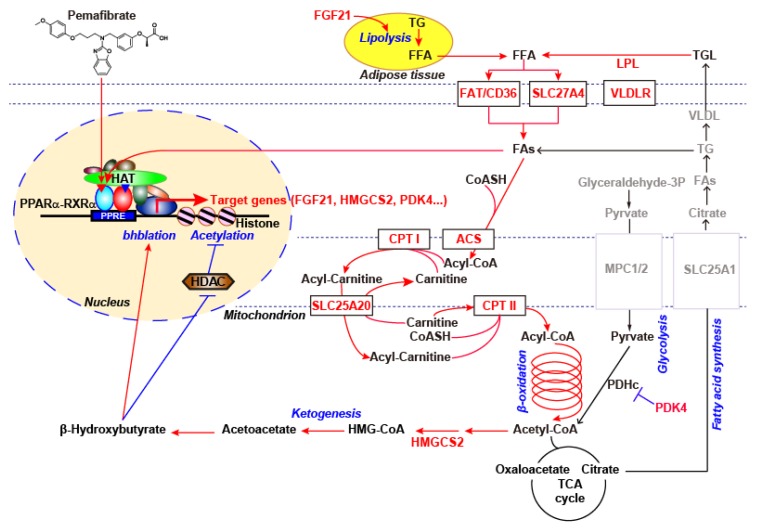
Figure 5.
Overviewing pemafibrate regulated fatty acid metabolism genes in human hepatocytes. Red font and arrows indicate the upregulated genes and pathways in the expression microarray of pemafibrate-treated human hepatocytes, respectively, which are based on our microarray data and the published literature.
Acknowledgments
We thank all the members of our laboratory for their continuous support of this project.
Abbreviations
| ABCA1 | ATP binding cassette subfamily A member 1 |
| Abcd2 | ATP binding cassette subfamily D member 2 |
| ABCG1 | ATP binding cassette subfamily G member 1 |
| Acaa1 | acetyl-CoA acyltransferase 1 |
| Acadl | acyl-Coenzyme A dehydrogenase long-chain |
| Acadm | acyl-Coenzyme A dehydrogenase medium-chain |
| Acads | acyl-Coenzyme A dehydrogenase short chain |
| Acadvl | acyl-Coenzyme A dehydrogenase very long-chain |
| Acad11 | acyl-Coenzyme A dehydrogenase family member 11 |
| Acat1 | acetyl-CoA acetyltransferase 1 |
| Acot3 | acyl-CoA thioesterase 3 |
| Acox1 | acyl-Coenzyme A oxidase 1 |
| Acsl1 | acyl-CoA synthetase long-chain family member 1 |
| Acsf3 | acyl-CoA synthetase family member 3 |
| ADR | adverse drug reaction |
| Aldh3a2 | aldehyde dehydrogenase 3 family member A2 |
| APA | aminopeptidase A |
| ASCVD | atherosclerotic cardiovascular disease |
| CBP/p300 | cAMP-response element binding protein (CREB) binding protein |
| C/EBPβ | CCAAT enhancer binding protein β |
| CKD | chronic kidney disease |
| COL1A2 | collagen type I alpha 2 chain |
| COUP-TFs | chicken ovalbumin upstream promotor-transcription factors |
| Cpt1 | carnitine palmitoyltransferase I |
| Crat | carnitine acetyltransferase |
| CREBH | cAMP-responsive element-binding protein 3 like 3 |
| CX3CL1 | C-X3-C motif chemokine ligand 1 |
| Cyp4a10 | cytochrome P450, family 4, subfamily a, polypeptide 10 |
| DAG | diacylglycerol |
| DBD | DNA binding domain |
| Decr1 | 2,4-dienoyl-CoA reductase 1 |
| DKK1 | dickkopf WNT signaling pathway inhibitor 1 |
| DR1 | direct repeat 1 |
| Ech1 | enoyl-CoA hydratase 1 |
| eGFR | estimated glomerular filtration rate |
| Ehhadh | enoyl-Coenzyme A, hydratase/3-hydroxyacyl Coenzyme A dehydrogenase |
| EndMT | endothelial-mesenchymal transition |
| ENPEP | glutamyl aminopeptidase |
| ET-1 | endothelin-1 |
| FA | fatty acid |
| FAT | fatty acid translocase |
| Fabp2 | fatty acid-binding protein 2 |
| FGF21 | fibroblast growth factor 21 |
| Fn1 | fibronectin 1 |
| GRIP1/TIF2 | glucocorticoid receptor interacting protein1/transcriptional intermediary factor 2 |
| Hadha | hydroxyacyl-CoA dehydrogenase trifunctional multienzyme complex subunit alpha |
| Hadhb | hydroxyacyl-CoA dehydrogenase trifunctional multienzyme complex subunit beta |
| HAT | histone acetyl transferase |
| HCECs | human coronary endothelial cells |
| HDAC | histone deacetylases |
| HDL-C | high-density lipoprotein cholesterol |
| Hmgcl | 3-hydroxy-3-methylglutaryl-CoA lyase |
| HMGCS2 | 3-hydroxy-3-methylglutaryl-CoA synthase 2 |
| HNF4s | hepatocyte nuclear factor 4s |
| Hsd17b4 | hydroxysteroid 17-beta dehydrogenase 4 |
| HUVECs | human umbilical vein endothelial cells |
| H3K9bhb | β-hydroxybutyrated histone H3 lysine 9 |
| IFNγ | interferon gamma |
| IL6 | interleukin 6 |
| LDL | low-density lipoprotein |
| LDLR | low-density lipoprotein receptor |
| Lpl | lipoprotein lipase |
| MBL2 | mannose-binding lectin 2 |
| MCP-1 | monocyte chemoattractant protein-1 |
| NAD(P)H | nicotinamide adenine dinucleotide phosphate |
| Ncf1 | neutrophil cytosolic factor 1 |
| Nox4 | NADPH oxidase 4 |
| 8-OHdG | 8-hydroxy-2’- deoxyguanosine |
| PDK4 | pyruvate dehydrogenase kinase 4 |
| Pex1 | peroxisome biogenesis factor 1 |
| PDH | pyruvate dehydrogenase |
| PGC1α | peroxisome proliferative activated receptor gamma coactivator 1α |
| PIC | preinitiation complex |
| PKC | protein kinase C |
| PPARα | peroxisome proliferator-activated receptor α |
| PPREs | PPAR response elements |
| RANTES | regulated on activation, normal T cell expressed and secreted |
| ROS | reactive oxygen species |
| RXR | retinoid X receptor |
| SBP | systolic blood pressure |
| Slc27a1 | solute carrier family 27 member 1 |
| Slc25a20 | solute carrier family 25 member 20 |
| SPPARMα | selective peroxisome proliferator-activated receptor α modulator |
| SRC/p160 | steroid receptor coactivator |
| TG | triglyceride |
| Tgfb1 | transforming growth factor beta 1 |
| TNFα | tumor necrosis factor α |
| VCAM1 | vascular cell adhesion molecule 1 |
| VLDLR | very-low-density lipoprotein receptor |
Author Contributions
J.S. and T.K. contributed to the conceptualization of the review. Y.S., S.R.-I., K.M., and T.T. contributed to the execution of the study and the writing of the manuscript. M.A., T.O., and Y.M. contributed to the critical review of the manuscript.
Funding
This work was supported by a grant for the Translational Systems Biology and Medicine Initiative from Ministry of Education, Culture, Sports, Science and Technology of Japan.
Conflicts of Interest
The authors declare no conflict of interest. T.K. is an advisory board member of Kowa Co. and a recipient of a collaborative research fund from Kowa Co. Kowa Company, Ltd. had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results. Y.S. and K.M. are employees of Kowa Company, Ltd.
References
- 1.Cholesterol Treatment Trialists’ Collaboration Efficacy and safety of statin therapy in older people: A meta-analysis of individual participant data from 28 randomised controlled trials. Lancet. 2019;393:407–415. doi: 10.1016/S0140-6736(18)31942-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cholesterol Treatment Trialists’ (CTT) Collaboration. Fulcher J., O’Connell R., Voysey M., Emberson J., Blackwell L., Mihaylova B., Simes J., Collins R., Kirby A., et al. Efficacy and safety of LDL-lowering therapy among men and women: Meta-analysis of individual data from 174,000 participants in 27 randomised trials. Lancet. 2015;385:1397–1405. doi: 10.1016/S0140-6736(14)61368-4. [DOI] [PubMed] [Google Scholar]
- 3.Fruchart J.C., Sacks F., Hermans M.P., Assmann G., Brown W.V., Ceska R., Chapman M.J., Dodson P.M., Fioretto P., Ginsberg H.N., et al. The Residual Risk Reduction Initiative: A call to action to reduce residual vascular risk in patients with dyslipidemia. Am. J. Cardiol. 2008;102:1K–34K. doi: 10.1016/j.amjcard.2008.10.002. [DOI] [PubMed] [Google Scholar]
- 4.Alagona P., Jr. Beyond LDL cholesterol: The role of elevated triglycerides and low HDL cholesterol in residual CVD risk remaining after statin therapy. Am. J. Manag. Care. 2009;15:S65–S73. [PubMed] [Google Scholar]
- 5.Reiner Z. Managing the residual cardiovascular disease risk associated with HDL-cholesterol and triglycerides in statin-treated patients: A clinical update. Nutr. Metab. Cardiovasc. Dis. 2013;23:799–807. doi: 10.1016/j.numecd.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 6.Hermans M.P., Valensi P. Elevated triglycerides and low high-density lipoprotein cholesterol level as marker of very high risk in type 2 diabetes. Curr. Opin. Endocrinol. Diabetes Obes. 2018;25:118–129. doi: 10.1097/MED.0000000000000398. [DOI] [PubMed] [Google Scholar]
- 7.Chapman M.J., Ginsberg H.N., Amarenco P., Andreotti F., Borén J., Catapano A.L., Descamps O.S., Fisher E., Kovanen P.T., Kuivenhoven J.A., et al. European Atherosclerosis Society Consensus Panel. Triglyceride-rich lipoproteins and high-density lipoprotein cholesterol in patients at high risk of cardiovascular disease: Evidence and guidance for management. Eur. Heart J. 2011;32:1345–1361. doi: 10.1093/eurheartj/ehr112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vrablík M., Češka R. Treatment of hypertriglyceridemia: A review of current options. Physiol. Res. 2015;64:S331–S340. doi: 10.33549/physiolres.933199. [DOI] [PubMed] [Google Scholar]
- 9.Katsiki N., Nikolic D., Montalto G., Banach M., Mikhailidis D.P., Rizzo M. The role of fibrate treatment in dyslipidemia: An overview. Curr. Pharm. Des. 2013;19:3124–3131. doi: 10.2174/1381612811319170020. [DOI] [PubMed] [Google Scholar]
- 10.McCullough P.A., Ahmed A.B., Zughaib M.T., Glanz E.D., Di Loreto M.J. Treatment of hypertriglyceridemia with fibric acid derivatives: Impact on lipid subfractions and translation into a reduction in cardiovascular events. Rev. Cardiovasc. Med. 2011;12:173–185. doi: 10.3909/ricm0619. [DOI] [PubMed] [Google Scholar]
- 11.Nakaya N., Goto Y. A retrospective meta-analysis of the efficacy and tolerability of fenofibrate 300 mg/d on high-density lipoprotein cholesterol levels in randomized, double-blind, comparative studies conducted in Japan. Curr. Res. Clin. Exp. 2003;64:634–644. doi: 10.1016/j.curtheres.2003.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davidson M.H., Armani A., McKenney J.M., Jacobson T.A. Safety considerations with fibrate therapy. Am. J. Cardiol. 2007;99:3C–18C. doi: 10.1016/j.amjcard.2006.11.016. [DOI] [PubMed] [Google Scholar]
- 13.Ahmad J., Odin J.A., Hayashi P.H., Chalasani N., Fontana R.J., Barnhart H., Cirulli E.T., Kleiner D.E., Hoofnagle J.H. Identification and Characterization of Fenofibrate-Induced Liver Injury. Dig. Dis. Sci. 2017;62:3596–3604. doi: 10.1007/s10620-017-4812-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abbas A., Saraf S., Ramachandran S., Raju J., Ramachandran S. Fibrates and estimated glomerular filtration rate: Observations from an outpatient clinic setting and clinical implications. Postgrad. Med. J. 2012;88:503–506. doi: 10.1136/postgradmedj-2011-130594. [DOI] [PubMed] [Google Scholar]
- 15.Yamazaki Y., Abe K., Toma T., Nishikawa M., Ozawa H., Okuda A., Araki T., Oda S., Inoue K., Shibuya K., et al. Design and synthesis of highly potent and selective human peroxisome proliferator-activated receptor α agonists. Bioorg. Med. Chem. Lett. 2007;17:4689–4693. doi: 10.1016/j.bmcl.2007.05.066. [DOI] [PubMed] [Google Scholar]
- 16.Fruchart J.C. Peroxisome proliferator-activated receptor-α (PPARα): At the crossroads of obesity, diabetes and cardiovascular disease. Atherosclerosis. 2009;205:1–8. doi: 10.1016/j.atherosclerosis.2009.03.008. [DOI] [PubMed] [Google Scholar]
- 17.Fruchart J.C. Selective peroxisome proliferator-activated receptor α modulators (SPPARMα): The next generation of peroxisome proliferator-activated receptor α-agonists. Cardiovasc. Diabetol. 2013;12:82. doi: 10.1186/1475-2840-12-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yamamoto Y., Takei K., Arulmozhiraja S., Sladek V., Matsuo N., Han S.I., Matsuzaka T., Sekiya M., Tokiwa T., Shoji M., et al. Molecular association model of PPARα and its new specific and efficient ligand, pemafibrate: Structural basis for SPPARMα. Biochem. Biophys. Res. Commun. 2018;499:239–245. doi: 10.1016/j.bbrc.2018.03.135. [DOI] [PubMed] [Google Scholar]
- 19.Raza-Iqbal S., Tanaka T., Anai M., Inagaki T., Matsumura Y., Ikeda K., Taguchi A., Gonzalez F.J., Sakai J., Kodama T. Transcriptome Analysis of K-877 (a Novel Selective PPARα Modulator (SPPARMα))-Regulated Genes in Primary Human Hepatocytes and the Mouse Liver. J. Atheroscler. Thromb. 2015;22:754–772. doi: 10.5551/jat.28720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fruchart J.C. Pemafibrate (K-877), a novel selective peroxisome proliferator-activated receptor α modulator for management of atherogenic dyslipidaemia. Cardiovasc. Diabetol. 2017;16:124. doi: 10.1186/s12933-017-0602-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Takei K., Han S.I., Murayama Y., Satoh A., Oikawa F., Ohno H., Osaki Y., Matsuzaka T., Sekiya M., Iwasaki H., et al. Selective peroxisome proliferator-activated receptor-α modulator K-877 efficiently activates the peroxisome proliferator-activated receptor-α pathway and improves lipid metabolism in mice. J. Diabetes Investig. 2017;8:446–452. doi: 10.1111/jdi.12621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hennuyer N., Duplan I., Paquet C., Vanhoutte J., Woitrain E., Touche V., Colin S., Vallez E., Lestavel S., Lefebvre P., et al. The novel selective PPARα modulator (SPPARMα) pemafibrate improves dyslipidemia, enhances reverse cholesterol transport and decreases inflammation and atherosclerosis. Atherosclerosis. 2016;249:200–208. doi: 10.1016/j.atherosclerosis.2016.03.003. [DOI] [PubMed] [Google Scholar]
- 23.Gibson G.G. Peroxisome proliferators: Paradigms and prospects. Toxicol. Lett. 1993;68:193–201. doi: 10.1016/0378-4274(93)90130-P. [DOI] [PubMed] [Google Scholar]
- 24.Misra P., Viswakarma N., Reddy J.K. Peroxisome proliferator-activated receptor-α signaling in hepatocarcinogenesis. Subcell. Biochem. 2013;69:77–99. doi: 10.1007/978-94-007-6889-5_5. [DOI] [PubMed] [Google Scholar]
- 25.Peters J.M., Shah Y.M., Gonzalez F.J. The role of peroxisome proliferator-activated receptors in carcinogenesis and chemoprevention. Nat. Rev. Cancer. 2012;12:181–195. doi: 10.1038/nrc3214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Takei K., Nakagawa Y., Wang Y., Han S.I., Satoh A., Sekiya M., Matsuzaka T., Shimano H. Effects of K-877, a novel selective PPARα modulator, on small intestine contribute to the amelioration of hyperlipidemia in low-density lipoprotein receptor knockout mice. J. Pharm. Sci. 2017;133:214–222. doi: 10.1016/j.jphs.2017.02.003. [DOI] [PubMed] [Google Scholar]
- 27.Sairyo M., Kobayashi T., Masuda D., Kanno K., Zhu Y., Okada T., Koseki M., Ohama T., Nishida M., Sakata Y., et al. A Novel Selective PPARα Modulator (SPPARMα), K-877 (Pemafibrate), Attenuates Postprandial Hypertriglyceridemia in Mice. J. Atheroscler. Thromb. 2018;25:142–152. doi: 10.5551/jat.39693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fruchart J.C., Santos R.D., Aguilar-Salinas C., Aikawa M., Al Rasadi K., Amarenco P., Barter P.J., Ceska R., Corsini A., Després J.P., et al. The selective peroxisome proliferator-activated receptor α modulator (SPPARMα) paradigm: Conceptual framework and therapeutic potential: A consensus statement from the International Atherosclerosis Society (IAS) and the Residual Risk Reduction Initiative (R3i) Foundation. Cardiovasc. Diabetol. 2019;18:71. doi: 10.1186/s12933-019-0864-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ishibashi S., Yamashita S., Arai H., Araki E., Yokote K., Suganami H., Fruchart J.C., Kodama T., K-877-04 Study Group Effects of K-877, a novel selective PPARα modulator (SPPARMα), in dyslipidaemic patients: A randomized, double blind, active- and placebo-controlled, phase 2 trial. Atherosclerosis. 2016;249:36–43. doi: 10.1016/j.atherosclerosis.2016.02.029. [DOI] [PubMed] [Google Scholar]
- 30.Arai H., Yamashita S., Yokote K., Araki E., Suganami H., Ishibashi S., K-877 Study Group Efficacy and safety of K-877, a novel selective peroxisome proliferator-activated receptor α modulator (SPPARMα), in combination with statin treatment: Two randomised, double-blind, placebo-controlled clinical trials in patients with dyslipidaemia. Atherosclerosis. 2017;261:144–152. doi: 10.1016/j.atherosclerosis.2017.03.032. [DOI] [PubMed] [Google Scholar]
- 31.Ishibashi S., Arai H., Yokote K., Araki E., Suganami H., Yamashita S., K-877 Study Group Efficacy and safety of pemafibrate (K-877), a selective peroxisome proliferator-activated receptor α modulator, in patients with dyslipidemia: Results from a 24-week, randomized, double blind, active-controlled, phase 3 trial. J. Clin. Lipidol. 2018;12:173–184. doi: 10.1016/j.jacl.2017.10.006. [DOI] [PubMed] [Google Scholar]
- 32.Araki E., Yamashita S., Arai H., Yokote K., Satoh J., Inoguchi T., Nakamura J., Maegawa H., Yoshioka N., Tanizawa Y., et al. Effects of Pemafibrate, a Novel Selective PPARα Modulator, on Lipid and Glucose Metabolism in Patients with Type 2 Diabetes and Hypertriglyceridemia: A Randomized, Double-Blind, Placebo-Controlled, Phase 3 Trial. Diabetes Care. 2018;41:538–546. doi: 10.2337/dc17-1589. [DOI] [PubMed] [Google Scholar]
- 33.Arai H., Yamashita S., Yokote K., Araki E., Suganami H., Ishibashi S., K-877 Study Group Efficacy and Safety of Pemafibrate Versus Fenofibrate in Patients with High Triglyceride and Low HDL Cholesterol Levels: A Multicenter, Placebo-Controlled, Double-Blind, Randomized Trial. J. Atheroscler. Thromb. 2018;25:521–538. doi: 10.5551/jat.44412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Matsuba I., Matsuba R., Ishibashi S., Yamashita S., Arai H., Yokote K., Suganami H., Araki E. Effects of a novel selective peroxisome proliferator-activated receptor-α modulator, pemafibrate, on hepatic and peripheral glucose uptake in patients with hypertriglyceridemia and insulin resistance. J. Diabetes Investig. 2018;9:1323–1332. doi: 10.1111/jdi.12845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yamashita S., Masuda D., Matsuzawa Y. Clinical Applications of a Novel Selective PPARα Modulator, Pemafibrate, in Dyslipidemia and Metabolic Diseases. J. Atheroscler. Thromb. 2019;26:389–402. doi: 10.5551/jat.48918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ida S., Kaneko R., Murata K. Efficacy and safety of pemafibrate administration in patients with dyslipidemia: A systematic review and meta-analysis. Cardiovasc. Diabetol. 2019;18:38. doi: 10.1186/s12933-019-0845-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Araki E., Yamashita S., Arai H., Yokote K., Satoh J., Inoguchi T., Nakamura J., Maegawa H., Yoshioka N., Tanizawa Y., et al. Efficacy and safety of pemafibrate in people with type 2 diabetes and elevated triglyceride levels: 52-week data from the PROVIDE study. Diabetes Obes. Metab. 2019;21:1737–1744. doi: 10.1111/dom.13686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yokote K., Yamashita S., Arai H., Araki E., Suganami H., Ishibashi S., K-Study Group Long-Term Efficacy and Safety of Pemafibrate, a Novel Selective Peroxisome Proliferator-Activated Receptor-α Modulator (SPPARMα), in Dyslipidemic Patients with Renal Impairment. Int. J. Mol. Sci. 2019;20:706. doi: 10.3390/ijms20030706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fisher F.M., Maratos-Flier E. Understanding the Physiology of FGF21. Annu. Rev. Physiol. 2016;78:223–241. doi: 10.1146/annurev-physiol-021115-105339. [DOI] [PubMed] [Google Scholar]
- 40.Holden P.R., Tugwood J.D. Peroxisome proliferator-activated receptor α: Role in rodent liver cancer and species differences. J. Mol. Endocrinol. 1999;22:1–8. doi: 10.1677/jme.0.0220001. [DOI] [PubMed] [Google Scholar]
- 41.Lawrence J.W., Li Y., Chen S., DeLuca J.G., Berger J.P., Umbenhauer D.R., Moller D.E., Zhou G. Differential gene regulation in human versus rodent hepatocytes by peroxisome proliferator-activated receptor (PPAR) α. PPARα fails to induce peroxisome proliferation-associated genes in human cells independently of the level of receptor expression. J. Biol. Chem. 2001;276:31521–31527. doi: 10.1074/jbc.M103306200. [DOI] [PubMed] [Google Scholar]
- 42.Hsu M.H., Savas U., Griffin K.J., Johnson E.F. Identification of peroxisome proliferator-responsive human genes by elevated expression of the peroxisome proliferator-activated receptor α in HepG2 cells. J. Biol. Chem. 2001;276:27950–27958. doi: 10.1074/jbc.M100258200. [DOI] [PubMed] [Google Scholar]
- 43.Adeva-Andany M.M., Carneiro-Freire N., Seco-Filgueira M., Fernández-Fernández C., Mouriño-Bayolo D. Mitochondrial β-oxidation of saturated fatty acids in humans. Mitochondrion. 2019;46:73–90. doi: 10.1016/j.mito.2018.02.009. [DOI] [PubMed] [Google Scholar]
- 44.Ferdinandusse S., Denis S., Van Roermund C.W., Wanders R.J., Dacremont G. Identification of the peroxisomal beta-oxidation enzymes involved in the degradation of long-chain dicarboxylic acids. J. Lipid Res. 2004;45:1104–1111. doi: 10.1194/jlr.M300512-JLR200. [DOI] [PubMed] [Google Scholar]
- 45.Yeldandi A.V., Rao M.S., Reddy J.K. Hydrogen peroxide generation in peroxisome proliferator-induced oncogenesis. Mutat. Res. 2000;448:159–177. doi: 10.1016/S0027-5107(99)00234-1. [DOI] [PubMed] [Google Scholar]
- 46.Raucy J.L., Lasker J., Ozaki K., Zoleta V. Regulation of CYP2E1 by ethanol and palmitic acid and CYP4A11 by clofibrate in primary cultures of human hepatocytes. Toxicol. Sci. 2004;79:233–241. doi: 10.1093/toxsci/kfh126. [DOI] [PubMed] [Google Scholar]
- 47.Savas U., Hsu M.H., Johnson E.F. Differential regulation of human CYP4A genes by peroxisome proliferators and dexamethasone. Arch. Biochem. Biophys. 2003;409:212–220. doi: 10.1016/S0003-9861(02)00499-X. [DOI] [PubMed] [Google Scholar]
- 48.Pettersen I.K.N., Tusubira D., Ashrafi H., Dyrstad S.E., Hansen L., Liu X.Z., Nilsson L.I.H., Løvsletten N.G., Berge K., Wergedahl H., et al. Upregulated PDK4 expression is a sensitive marker of increased fatty acid oxidation. Mitochondrion. 2019;49:97–110. doi: 10.1016/j.mito.2019.07.009. [DOI] [PubMed] [Google Scholar]
- 49.Attia R.R., Sharma P., Janssen R.C., Friedman J.E., Deng X., Lee J.S., Elam M.B., Cook G.A., Park E.A. Regulation of pyruvate dehydrogenase kinase 4 (PDK4) by CCAAT/enhancer-binding protein beta (C/EBPbeta) J. Biol. Chem. 2011;286:23799–23807. doi: 10.1074/jbc.M111.246389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Holness M.J., Bulmer K., Smith N.D., Sugden M.C. Investigation of potential mechanisms regulating protein expression of hepatic pyruvate dehydrogenase kinase isoforms 2 and 4 by fatty acids and thyroid hormone. Biochem. J. 2003;369:687–695. doi: 10.1042/bj20021509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Vilà-Brau A., De Sousa-Coelho A.L., Mayordomo C., Haro D., Marrero P.F. Human HMGCS2 regulates mitochondrial fatty acid oxidation and FGF21 expression in HepG2 cell line. J. Biol. Chem. 2011;286:20423–20430. doi: 10.1074/jbc.M111.235044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Xie Z., Zhang D., Chung D., Tang Z., Huang H., Dai L., Qi S., Li J., Colak G., Chen Y., et al. Metabolic Regulation of Gene Expression by Histone Lysine β-Hydroxybutyrylation. Mol. Cell. 2016;62:194–206. doi: 10.1016/j.molcel.2016.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Webb J.C., Patel D.D., Jones M.D., Knight B.L., Soutar A.K. Characterization and tissue-specific expression of the human ‘very low density lipoprotein (VLDL) receptor’ mRNA. Hum. Mol. Genet. 1994;3:531–537. doi: 10.1093/hmg/3.4.531. [DOI] [PubMed] [Google Scholar]
- 54.Tiebel O., Oka K., Robinson K., Sullivan M., Martinez J., Nakamuta M., Ishimura-Oka K., Chan L. Mouse very low-density lipoprotein receptor (VLDLR): Gene structure, tissue-specific expression and dietary and developmental regulation. Atherosclerosis. 1999;145:239–251. doi: 10.1016/S0021-9150(99)00068-4. [DOI] [PubMed] [Google Scholar]
- 55.Gao Y., Shen W., Lu B., Zhang Q., Hu Y., Chen Y. Upregulation of hepatic VLDLR via PPARα is required for the triglyceride-lowering effect of fenofibrate. J. Lipid Res. 2014;55:1622–1633. doi: 10.1194/jlr.M041988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Merkel M., Weinstock P.H., Chajek-Shaul T., Radner H., Yin B., Breslow J.L., Goldberg I.J. Lipoprotein lipase expression exclusively in liver. A mouse model for metabolism in the neonatal period and during cachexia. J. Clin. Investig. 1998;102:893–901. doi: 10.1172/JCI2912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wang S., Smith J.D. ABCA1 and nascent HDL biogenesis. Biofactors. 2014;40:547–554. doi: 10.1002/biof.1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Babashamsi M.M., Koukhaloo S.Z., Halalkhor S., Salimi A., Babashamsi M. ABCA1 and metabolic syndrome; a review of the ABCA1 role in HDL-VLDL production, insulin-glucose homeostasis, inflammation and obesity. Diabetes Metab. Syndr. 2019;13:1529–1534. doi: 10.1016/j.dsx.2019.03.004. [DOI] [PubMed] [Google Scholar]
- 59.Liu Y., Tang C. Regulation of ABCA1 functions by signaling pathways. Biochim. Biophys. Acta. 2012;1821:522–529. doi: 10.1016/j.bbalip.2011.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Brunham L.R., Singaraja R.R., Duong M., Timmins J.M., Fievet C., Bissada N., Kang M.H., Samra A., Fruchart J.C., McManus B., et al. Tissue-specific roles of ABCA1 influence susceptibility to atherosclerosis. Arterioscler. Thromb. Vasc. Biol. 2009;29:548–554. doi: 10.1161/ATVBAHA.108.182303. [DOI] [PubMed] [Google Scholar]
- 61.Kharitonenkov A., Shiyanova T.L., Koester A., Ford A.M., Micanovic R., Galbreath E.J., Sandusky G.E., Hammond L.J., Moyers J.S., Owens R.A., et al. FGF-21 as a novel metabolic regulator. J. Clin. Investig. 2005;115:1627–1635. doi: 10.1172/JCI23606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Véniant M.M., Komorowski R., Chen P., Stanislaus S., Winters K., Hager T., Zhou L., Wada R., Hecht R., Xu J. Long-acting FGF21 has enhanced efficacy in diet-induced obese mice and in obese rhesus monkeys. Endocrinology. 2012;153:4192–4203. doi: 10.1210/en.2012-1211. [DOI] [PubMed] [Google Scholar]
- 63.Inagaki T., Dutchak P., Zhao G., Ding X., Gautron L., Parameswara V., Li Y., Goetz R., Mohammadi M., Esser V., et al. Endocrine regulation of the fasting response by PPARα-mediated induction of fibroblast growth factor 21. Cell Metab. 2007;5:415–425. doi: 10.1016/j.cmet.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 64.Lundåsen T., Hunt M.C., Nilsson L.M., Sanyal S., Angelin B., Alexson S.E., Rudling M. PPARα is a key regulator of hepatic FGF21. Biochem. Biophys. Res. Commun. 2007;360:437–440. doi: 10.1016/j.bbrc.2007.06.068. [DOI] [PubMed] [Google Scholar]
- 65.Yamashita S., Arai H., Yokote K., Araki E., Suganami H., Ishibashi S., K-877 Study Group Effects of pemafibrate (K-877) on cholesterol efflux capacity and postprandial hyperlipidemia in patients with atherogenic dyslipidemia. J. Clin. Lipidol. 2018;12:1267–1279. doi: 10.1016/j.jacl.2018.06.010. [DOI] [PubMed] [Google Scholar]
- 66.Kim H., Mendez R., Zheng Z., Chang L., Cai J., Zhang R., Zhang K. Liver-enriched transcription factor CREBH interacts with peroxisome proliferator-activated receptor α to regulate metabolic hormone FGF21. Endocrinology. 2014;155:769–782. doi: 10.1210/en.2013-1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ip W.K., Takahashi K., Ezekowitz R.A., Stuart L.M. Mannose-binding lectin and innate immunity. Immunol. Rev. 2009;230:9–21. doi: 10.1111/j.1600-065X.2009.00789.x. [DOI] [PubMed] [Google Scholar]
- 68.Hansen T.K. Growth hormone and mannan-binding lectin: Emerging evidence for hormonal regulation of humoral innate immunity. Minerva. Endocrinologica. 2003;28:75–84. [PubMed] [Google Scholar]
- 69.Fernández-Real J.M., Straczkowski M., Vendrell J., Soriguer F., Pérez Del Pulgar S., Gallart L., López-Bermejo A., Kowalska I., Manco M., Cardona F., et al. Protection from inflammatory disease in insulin resistance: The role of mannan-binding lectin. Diabetologia. 2006;49:2402–2411. doi: 10.1007/s00125-006-0381-6. [DOI] [PubMed] [Google Scholar]
- 70.Holmes R.S., Spradling-Reeves K.D., Cox L.A. Mammalian Glutamyl Aminopeptidase Genes (ENPEP) and Proteins: Comparative Studies of a Major Contributor to Arterial Hypertension. J. Data Min. Genomics Proteom. 2017;8:2. doi: 10.4172/2153-0602.1000211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Mizutani S., Ishii M., Hattori A., Nomura S., Numaguchi Y., Tsujimoto M., Kobayshi H., Murohara T., Wright J.W. New insights into the importance of aminopeptidase A in hypertension. Heart Fail. Rev. 2008;13:273–284. doi: 10.1007/s10741-007-9065-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Tsujimoto M., Goto Y., Maruyama M., Hattori A. Biochemical and enzymatic properties of the M1 family of aminopeptidases involved in the regulation of blood pressure. Heart. Fail. Rev. 2008;13:285–291. doi: 10.1007/s10741-007-9064-8. [DOI] [PubMed] [Google Scholar]
- 73.Mitsui T., Nomura S., Okada M., Ohno Y., Kobayashi H., Nakashima Y., Murata Y., Takeuchi M., Kuno N., Nagasaka T., et al. Hypertension and angiotensin II hypersensitivity in aminopeptidase A-deficient mice. Mol. Med. 2003;9:57–62. doi: 10.1007/BF03402108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Surendran P., Drenos F., Young R., Warren H., Cook J.P., Manning A.K., Grarup N., Sim X., Barnes D.R., Witkowska K., et al. Trans-ancestry meta-analyses identify rare and common variants associated with blood pressure and hypertension. Nat. Genet. 2016;48:1151–1161. doi: 10.1038/ng.3654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Rajendran P., Rengarajan T., Thangavel J., Nishigaki Y., Sakthisekaran D., Sethi G., Nishigaki I. The vascular endothelium and human diseases. Int. J. Biol. Sci. 2013;9:1057–1069. doi: 10.7150/ijbs.7502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Cheng H., Harris R.C. Renal Endothelial Dysfunction in Diabetic Nephropathy. Cardiovasc. Hematol. Disord. Drug Targets. 2014;14:22–33. doi: 10.2174/1871529X14666140401110841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Gimbrone M.A., Jr., García-Cardeña G. Endothelial Cell Dysfunction and the Pathobiology of Atherosclerosis. Circ. Res. 2016;118:620–636. doi: 10.1161/CIRCRESAHA.115.306301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Maki T., Maeda Y., Sonoda N., Makimura H., Kimura S., Maeno S., Takayanagi R., Inoguchi T. Renoprotective effect of a novel selective PPARα modulator K-877 in db/db mice: A role of diacylglycerol-protein kinase C-NAD(P)H oxidase pathway. Metabolism. 2017;71:33–45. doi: 10.1016/j.metabol.2017.02.013. [DOI] [PubMed] [Google Scholar]
- 79.Kitajima K., Miura S., Mastuo Y., Uehara Y., Saku K. Newly developed PPAR-agonist (R)-K-13675 inhibits the secretion of inflammatory markers without affecting cell proliferation or tube formation. Atherosclerosis. 2009;203:75–81. doi: 10.1016/j.atherosclerosis.2008.05.055. [DOI] [PubMed] [Google Scholar]
- 80.Kovacic J.C., Dimmeler S., Harvey R.P., Finkel T., Aikawa E., Krenning G., Baker A.H. Endothelial to Mesenchymal Transition in Cardiovascular Disease: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2019;73:190–209. doi: 10.1016/j.jacc.2018.09.089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Cho J.G., Lee A., Chang W., Lee M.S., Kim J. Endothelial to Mesenchymal Transition Represents a Key Link in the Interaction between Inflammation and Endothelial Dysfunction. Front. Immunol. 2018;9:294. doi: 10.3389/fimmu.2018.00294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Thomas A.A., Biswas S., Feng B., Chen S., Gonder J., Chakrabarti S. lncRNA H19 prevents endothelial-mesenchymal transition in diabetic retinopathy. Diabetologia. 2019;62:517–530. doi: 10.1007/s00125-018-4797-6. [DOI] [PubMed] [Google Scholar]
- 83.Gong H., Lyu X., Wang Q., Hu M., Zhang X. Endothelial to mesenchymal transition in the cardiovascular system. Life Sci. 2017;184:95–102. doi: 10.1016/j.lfs.2017.07.014. [DOI] [PubMed] [Google Scholar]
- 84.Li Y., Lui K.O., Zhou B. Reassessing endothelial-to-mesenchymal transition in cardiovascular diseases. Nat. Rev. Cardiol. 2018;15:445–456. doi: 10.1038/s41569-018-0023-y. [DOI] [PubMed] [Google Scholar]
- 85.Cheng S.L., Shao J.S., Behrmann A., Krchma K., Towler D.A. Dkk1 and MSX2-Wnt7b signaling reciprocally regulate the endothelial-mesenchymal transition in aortic endothelial cells. Arter. Thromb. Vasc. Biol. 2013;33:1679–1689. doi: 10.1161/ATVBAHA.113.300647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Glineur C., Gross B., Neve B., Rommens C., Chew G.T., Martin-Nizard F., Rodríguez-Pascual F., Lamas S., Watts G.F., Staels B. Fenofibrate inhibits endothelin-1 expression by peroxisome proliferator-activated receptor α-dependent and independent mechanisms in human endothelial cells. Arter. Thromb. Vasc. Biol. 2013;33:621–628. doi: 10.1161/ATVBAHA.112.300665. [DOI] [PubMed] [Google Scholar]
- 87.Widyantoro B., Emoto N., Nakayama K., Anggrahini D.W., Adiarto S., Iwasa N., Yagi K., Miyagawa K., Rikitake Y., Suzuki T., et al. Endothelial cell-derived endothelin-1 promotes cardiac fibrosis in diabetic hearts through stimulation of endothelial-to-mesenchymal transition. Circulation. 2010;121:2407–2418. doi: 10.1161/CIRCULATIONAHA.110.938217. [DOI] [PubMed] [Google Scholar]
- 88.Cipriani P., Di Benedetto P., Ruscitti P., Capece D., Zazzeroni F., Liakouli V., Pantano I., Berardicurti O., Carubbi F., Pecetti G., et al. The Endothelial-mesenchymal Transition in Systemic Sclerosis Is Induced by Endothelin-1 and Transforming Growth Factor-β and May Be Blocked by Macitentan, a Dual Endothelin-1 Receptor Antagonist. J. Rheumatol. 2015;42:1808–1816. doi: 10.3899/jrheum.150088. [DOI] [PubMed] [Google Scholar]
- 89.Keech A., Simes R.J., Barter P., Best J., Scott R., Taskinen M.R., Forder P., Pillai A., Davis T., Glasziou P., et al. FIELD study investigators. Effects of long-term fenofibrate therapy on cardiovascular events in 9795 people with type 2 diabetes mellitus (the FIELD study): Randomised controlled trial. Lancet. 2005;366:1849–1861. doi: 10.1016/S0140-6736(05)67667-2. [DOI] [PubMed] [Google Scholar]
- 90.Keech A.C., Mitchell P., Summanen P.A., O’Day J., Davis T.M., Moffitt M.S., Taskinen M.R., Simes R.J., Tse D., Williamson E., et al. FIELD study investigators. Effect of fenofibrate on the need for laser treatment for diabetic retinopathy (FIELD study): A randomised controlled trial. Lancet. 2007;370:1687–1697. doi: 10.1016/S0140-6736(07)61607-9. [DOI] [PubMed] [Google Scholar]
- 91.Chew E.Y., Davis M.D., Danis R.P., Lovato J.F., Perdue L.H., Greven C., Genuth S., Goff D.C., Leiter L.A., Ismail-Beigi F., et al. Action to Control Cardiovascular Risk in Diabetes Eye Study Research Group. The effects of medical management on the progression of diabetic retinopathy in persons with type 2 diabetes: The Action to Control Cardiovascular Risk in Diabetes (ACCORD) Eye Study. Ophthalmology. 2014;121:2443–2451. doi: 10.1016/j.ophtha.2014.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Bougarne N., Weyers B., Desmet S.J., Deckers J., Ray D.W., Staels B., De Bosscher K. Molecular Actions of PPARα in Lipid Metabolism and Inflammation. Endocr. Rev. 2018;39:760–802. doi: 10.1210/er.2018-00064. [DOI] [PubMed] [Google Scholar]
- 93.Duncan J.G. Peroxisome proliferator activated receptor-α (PPARα) and PPAR gamma coactivator-1α (PGC-1α) regulation of cardiac metabolism in diabetes. Pediatr. Cardiol. 2011;32:323–328. doi: 10.1007/s00246-011-9889-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Pawlak M., Lefebvre P., Staels B. Molecular mechanism of PPARα action and its impact on lipid metabolism, inflammation and fibrosis in non-alcoholic fatty liver disease. J. Hepatol. 2015;62:720–733. doi: 10.1016/j.jhep.2014.10.039. [DOI] [PubMed] [Google Scholar]
- 95.Viswakarma N., Jia Y., Bai L., Gao Q., Lin B., Zhang X., Misra P., Rana A., Jain S., Gonzalez F.J., et al. The Med1 subunit of the mediator complex induces liver cell proliferation and is phosphorylated by AMP kinase. J. Biol. Chem. 2013;288:27898–27911. doi: 10.1074/jbc.M113.486696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Mukherjee R., Sun S., Santomenna L., Miao B., Walton H., Liao B., Locke K., Zhang J.H., Nguyen S.H., Zhang L.T., et al. Ligand and coactivator recruitment preferences of peroxisome proliferator activated receptor α. J. Steroid Biochem. Mol. Biol. 2002;81:217–225. doi: 10.1016/S0960-0760(02)00066-3. [DOI] [PubMed] [Google Scholar]
- 97.Surapureddi S., Yu S., Bu H., Hashimoto T., Yeldandi A.V., Kashireddy P., Cherkaoui-Malki M., Qi C., Zhu Y.J., Rao M.S., et al. Identification of a transcriptionally active peroxisome proliferator-activated receptor α-interacting cofactor complex in rat liver and characterization of PRIC285 as a coactivator. Proc. Natl. Acad. Sci. USA. 2002;99:11836–11841. doi: 10.1073/pnas.182426699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Jia Y., Qi C., Kashireddi P., Surapureddi S., Zhu Y.J., Rao M.S., Le Roith D., Chambon P., Gonzalez F.J., Reddy J.K. Transcription coactivator PBP, the peroxisome proliferator-activated receptor (PPAR)-binding protein, is required for PPARα-regulated gene expression in liver. J. Biol. Chem. 2004;279:24427–244234. doi: 10.1074/jbc.M402391200. [DOI] [PubMed] [Google Scholar]
- 99.Pawlak M., Baugé E., Bourguet W., De Bosscher K., Lalloyer F., Tailleux A., Lebherz C., Lefebvre P., Staels B. The transrepressive activity of peroxisome proliferator-activated receptor α is necessary and sufficient to prevent liver fibrosis in mice. Hepatology. 2014;60:1593–1606. doi: 10.1002/hep.27297. [DOI] [PubMed] [Google Scholar]
- 100.Delerive P., De Bosscher K., Besnard S., Vanden Berghe W., Peters J.M., Gonzalez F.J., Fruchart J.C., Tedgui A., Haegeman G., Staels B. Peroxisome proliferator-activated receptor α negatively regulates the vascular inflammatory gene response by negative cross-talk with transcription factors NF-κB and AP-1. J. Biol. Chem. 1999;274:32048–32054. doi: 10.1074/jbc.274.45.32048. [DOI] [PubMed] [Google Scholar]
- 101.Planavila A., Iglesias R., Giralt M., Villarroya F. Sirt1 acts in association with PPARα to protect the heart from hypertrophy, metabolic dysregulation, and inflammation. Cardiovasc. Res. 2011;90:276–284. doi: 10.1093/cvr/cvq376. [DOI] [PubMed] [Google Scholar]
- 102.Bougarne N., Paumelle R., Caron S., Hennuyer N., Mansouri R., Gervois P., Staels B., Haegeman G., De Bosscher K. PPARα blocks glucocorticoid receptor α-mediated transactivation but cooperates with the activated glucocorticoid receptor α for transrepression on NF-κB. Proc. Natl. Acad. Sci. USA. 2009;106:7397–7402. doi: 10.1073/pnas.0806742106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Gervois P., Vu-Dac N., Kleemann R., Kockx M., Dubois G., Laine B., Kosykh V., Fruchart J.C., Kooistra T., Staels B. Negative regulation of human fibrinogen gene expression by peroxisome proliferator-activated receptor α agonists via inhibition of CCAAT box/enhancer-binding protein β. J. Biol. Chem. 2001;276:33471–33477. doi: 10.1074/jbc.M102839200. [DOI] [PubMed] [Google Scholar]
- 104.Dongol B., Shah Y., Kim I., Gonzalez F.J., Hunt M.C. The acyl-CoA thioesterase I is regulated by PPARαand HNF4αvia a distal response element in the promoter. J. Lipid Res. 2007;48:1781–1791. doi: 10.1194/jlr.M700119-JLR200. [DOI] [PubMed] [Google Scholar]
- 105.Marrapodi M., Chiang J.Y. Peroxisome proliferator-activated receptor α (PPARα) and agonist inhibit cholesterol 7α-hydroxylase gene (CYP7A1) transcription. J. Lipid Res. 2000;41:514–520. [PubMed] [Google Scholar]
- 106.Spann N.J., Kang S., Li A.C., Chen A.Z., Newberry E.P., Davidson N.O., Hui S.T., Davis R.A. Coordinate transcriptional repression of liver fatty acid-binding protein and microsomal triglyceride transfer protein blocks hepatic very low density lipoprotein secretion without hepatosteatosis. J. Biol. Chem. 2006;281:33066–33077. doi: 10.1074/jbc.M607148200. [DOI] [PubMed] [Google Scholar]
- 107.IJpenberg A., Tan N.S., Gelman L., Kersten S., Seydoux J., Xu J., Metzger D., Canaple L., Chambon P., Wahli W., et al. In vivo activation of PPAR target genes by RXR homodimers. EMBO J. 2004;23:2083–2091. doi: 10.1038/sj.emboj.7600209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Pradhan A.D., Paynter N.P., Everett B.M., Glynn R.J., Amarenco P., Elam M., Ginsberg H., Hiatt W.R., Ishibashi S., Koenig W., et al. Rationale and design of the Pemafibrate to Reduce Cardiovascular Outcomes by Reducing Triglycerides in Patients with Diabetes (PROMINENT) study. Am. Heart J. 2018;206:80–93. doi: 10.1016/j.ahj.2018.09.011. [DOI] [PubMed] [Google Scholar]