Abstract
Colorectal cancer (CRC) is the third most common cancer and has a high metastasis and reoccurrence rate. Long noncoding RNAs (lncRNAs) play an important role in CRC growth and metastasis. Recent studies revealed that lncRNAs participate in CRC progression by coordinating with microRNAs (miRNAs) and protein-coding mRNAs. LncRNAs function as competitive endogenous RNAs (ceRNAs) by competitively occupying the shared binding sequences of miRNAs, thus sequestering the miRNAs and changing the expression of their downstream target genes. Such ceRNA networks formed by lncRNA/miRNA/mRNA interactions have been found in a broad spectrum of biological processes in CRC, including liver metastasis, epithelial to mesenchymal transition (EMT), inflammation formation, and chemo-/radioresistance. In this review, we summarize typical paradigms of lncRNA-associated ceRNA networks, which are involved in the underlying molecular mechanisms of CRC initiation and progression. We comprehensively discuss the competitive crosstalk among RNA transcripts and the novel targets for CRC prognosis and therapy.
Keywords: colorectal cancer, lncRNA, miRNA, ceRNA
1. Introduction
Colorectal cancer (CRC) is the third most commonly diagnosed and fatal malignancy, with nearly 1.8 million new cases and almost 861,000 deaths in 2018 around the world [1]. In the past decade, the diagnosis and treatment of CRC have been greatly improved. However, distant metastasis, especially liver metastasis, and the cell stemness properties of cancer cells lead to the poor prognosis and high fatality rate in CRC patients [2]. Recent studies on the biology of noncoding RNAs in CRC and new gene therapy strategies for delivering therapeutic RNA, such as noncoding RNA or small interfering RNA (siRNA), have drawn intense interest in the investigation of long noncoding RNAs (lncRNAs) in the molecular mechanisms of CRC [3,4,5,6,7,8]. Besides the characterized lncRNAs or microRNAs (miRNAs) in important CRC-related signaling pathways, such as Wnt/β-catenin, studies in recent years have identified a novel competitive RNA network including lncRNA, miRNA, and mRNA, which mediates CRC cell proliferation, invasion, tumor growth, and metastasis. Moreover, competitive endogenous RNA (ceRNA) crosstalk has strong relevance to the acquisition of chemo-/radioresistance in CRC. Hence, deeper exploration and understanding of ceRNA mechanisms in CRC development are needed.
2. LncRNA in CRC
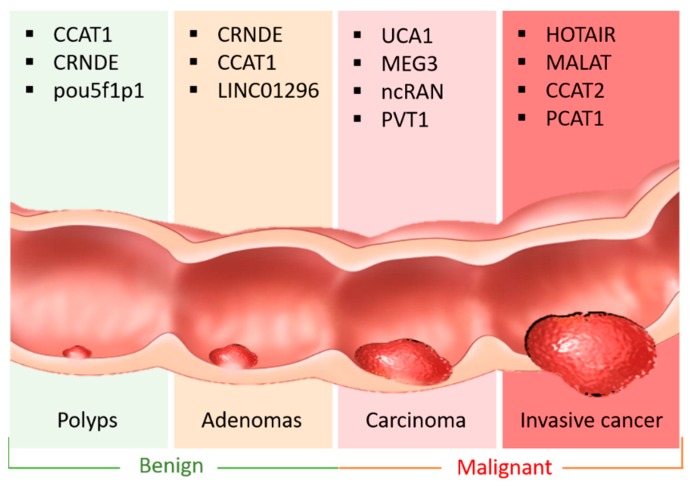
LncRNAs, defined as transcripts longer than 200 nucleotides, are not translated into proteins [9]. LncRNAs, aberrantly expressed in various types of cancer cells, play a vital role in several common hallmarks of cancer [10]. In general, lncRNAs exert regulatory functions at different levels of gene expression, including chromatin modification, transcription, and post-transcription. As for chromatin modification, lncRNAs interact with chromatin remodeling complexes to induce heterochromatin formation in specific genomic loci, resulting in reduced gene expression. Moreover, lncRNAs modulate transcription by interacting with RNA-binding proteins and co-activators of transcriptional factors, or by regulating the major promoters of their target genes. Mechanically, lncRNAs exert their regulatory effects through communication with DNA, mRNAs, ncRNAs, and proteins, serving as different functional molecules, such as signals, decoys, scaffolds, and guides in various cancer-related cellular processes [11,12]. Previous studies reported that lncRNAs work mainly as signaling molecules in many important CRC-related pathways, or as scaffold guides to decoy CRC-specific protein partners, as well as a cis- and trans- regulator element for gene expression. For example, the oncogenic lncRNAs mapped to chromosome 8q.24, such as CACS11, CCAT family, and PVT1, promote CRC progression by interacting with proteins to stimulate myc or other Wnt target gene expression at the posttranslational level [13]. Furthermore, lncRNAs (Figure 1) are frequently involved in different stages of CRC from precancerous polyps to distant metastasis, which could be considered potent diagnostic biomarkers [14,15]. In recent years, increasing studies have demonstrated the existence of lncRNA-mediated competitive RNA crosstalk in CRC progression (Table 1).
Figure 1.
Representative lncRNAs in the different stages of CRC. There are four major stages of CRC development: precancerous polys, Adenomas, Carcinoma and invasive cancer. Representative lncRNAs involved in the certain stages could be regarded as early-stage diagnostic biomarkers to evaluate CRC progression or therapeutic targets to suppress CRC metastasis.
Table 1.
LncRNA/miRNA/mRNA ceRNA network in CRC.
| LncRNA | Chromosome Location | Competitor mRNA | Shared miRNA | ceRNA Network | ceRNA Role | Related CRC Hallmark | Ref. |
|---|---|---|---|---|---|---|---|
| BCAR4 | 16p13.13 | STAT3 | miR-665 | BCAR4/miR-655/STAT3 | Oncogenic | Proliferation, migration | [152] |
| CACS15 | 6p22.3 | LGR5 | miR-4310 | CACS15/miR-4310/LGR5 | Oncogenic | Proliferation, invasion, TNM stage, metastasis | [153] |
| CASC19 | 8q24.21 | CEMIP | miR-140-5p | CASC19/miR-140-5p/CEMIP | Oncogenic | Proliferation, invasion, migration, apoptosis, EMT | [33] |
| CASC2 | 10q26.11 | PIAS3 | miR-18a | CASC2/miR-18a/PIAS3/STAT3 | Tumor suppressive | Proliferation, tumor growth, G0/G1-S phase transition | [154] |
| CCAT2 | 8q24.21 | miR-145 | CCAT2/miR-145/miR-21 | Oncogenic | CSC proliferation and differentiation | [155] | |
| CYTOR | 2p11.2 | MACC1 | miR-3679-5p | CYTOR/miR-3679-5p/MACC1 | Oncogenic | TNM stage, perineural and venous invasions | [156] |
| ENSG00000-231881 | 6 | VEGFC | miR-133b | ENSG00000231881/miR-133b/VEGFC | Oncogenic | Metastasis | [157] |
| FER1L4 | 20q11.22 | miR-106a-5p | FER1L4/miR-106a-5p | Tumor suppressive | Proliferation, cell cycle | [158] | |
| FOXD2-AS1 | 1p33 | CDC42 | miR-185-5p | FOXD2-AS1/miR-185-5p/CDC42 | Oncogenic | Proliferation, migration, invasion | [159] |
| FOXD3-AS1 | 1p31.3 | SIRT1 | miR-135a-5p | FOXD3-AS1/miR-135a-5p/SIRT1 | Oncogenic | Proliferation, migration, invasion, cell cycle, apoptosis | [160] |
| GACAT3 | 2p24.3 | SP1, STAT3 | miR-149 | GACAT3/miR-149/SP1/STAT3 | Oncogenic | Proliferation, invasion, migration | [161] |
| GAS5 | 1q25.1 | PTEN | miR-222-3p | GAS5/miR-222-3p/PTEN | Tumor suppressive | Proliferation, migration, apoptosis | [162] |
| H19 | 11p15.5 | Vimentin, ZEB1, ZEB2 | miR-138, miR-200a |
H19/miR-138/Vimentin, H19/miR-200a/ZEB1, H19/miR-200a/ZEB2 | Oncogenic | EMT progression | [58] |
| HAND2-AS1 | 4q34.1 | KLF14 | miR-1275 | HAND2-AS1/miR-1275/KLF14 | Tumor suppressive | Proliferation, invasion | [163] |
| HOTAIR | 12q13.13 | miR-34a | HOTAIR/miR-34a | Oncogenic | Metastasis | [164] | |
| HULC | 6p24.3 | RTKN | miR-613 | HULC/miR-613/RTKN | Oncogenic | Proliferation, metastasis | [165] |
| LINC00460 | 13q33.2 | LIMK2 | miR-939-5p | LINC00460/LIMK2/miR-939-5p | Oncogenic | Metastasis | [166] |
| LINC00668 | 18p11.31 | USP47 | miR-188–5p | LINC000668/miR-188-5p/USP47 | Oncogenic | Proliferation, metastasis | [167] |
| LINC00858 | 10q23.1 | YWHAZ | miR-22-3p | LINC00858/miR-22-3p/YWHAZ | Oncogenic | Proliferation, migration, invasion | [168] |
| LINC01234 | 12q24.13 | SHMT2 | miR-642a-5p | LINC01234/miR-642a-5p/SHMT2 | Oncogenic | Proliferation | [169] |
| LINC01296 | 14q11.2 | PDCD4 | miR-21a | LINC01296/miR-21a/PDCD4 | Oncogenic | Proliferation | [170] |
| LINC02418 | 12q24.33 | MELK | miR-1273g-3p | LINC02418/miR-1273g-3p/MELK | Oncogenic | Proliferation, apoptosis | [171] |
| MALAT1 | 11q13.1 | p53 | miR-663a | MALAT1/miR-663a/p53 | Oncogenic | Proliferation, migration, invasion, apoptosis | [100] |
| MBNL1-AS1 | 3q25.1 | MYL9 | miR-412-3p | MBNL-AS1/miR-412-3p/MYL9 | Tumor suppressive | Proliferation, invasion | [172] |
| MIAT | 22q12.1 | Derlin-1 | miR-132 | MIAT/miR-132/Derlin-1 | Oncogenic | Tumor growth, metastasis | [173] |
| MIR17HG | 13q31.3 | Wnt, β-catenin |
miR-17, miR-18a | MIR17HG-miR-17/18a-Wnt/ β-catenin |
Oncogenic | Lymph node metastasis, TNM stage | [174] |
| MNX1-AS1 | 7q36.3 | SEC61A1 | miR-218-5p | MNX1-AS1/miR-218-5p/ SEC61A1 |
Oncogenic | progression of colon adenocarcinoma | [175] |
| NEAT1 | 11q13.1 | CDK6 | miR-495-3p | NEAT1/miR-495-3p/CDK6 | Oncogenic | Proliferation, migration, invasion | [43] |
| OECC | 8q24 | NF-κB, p38MAPK | miR-143-3p | OECC/miR-143-3p/NF-κB/ p38 MAPK |
Oncogenic | Proliferation, apoptosis, migration | [176] |
| PART-1 | 5q12.1 | DNMT3A | miR-143 | PART-1/miR-143/DNMT3A | Oncogenic | Proliferation, metastasis | [177] |
| PVT1 | 8q24.21 | RUNX2 | miR-30d-5p | PVT1/miR-30d-5p/RUNX2 | Oncogenic | Proliferation, metastasis | [26] |
| PVT1 | 8q24.21 | RUNX2 | miR-455 | PVT1/miR-455/RUNX2 | Oncogenic | Proliferation, migration, invasion, apoptosis | [31] |
| PVT1-214 | 8q24.21 | Lin28 | miR-128 | PVT1-214/miR-128/Lin28/let-7 | Oncogenic | Proliferation, invasion | [32] |
| ROR | 18q21.31 | miR-145 | ROR/miR-145 | Oncogenic | Proliferation, migration, invasion | [178] | |
| SNHG15 | 7p13 | SIRT1 | miR-141 | SNHG15/miR-141/SIRT1 | Oncogenic | Proliferation, apoptosis | [179] |
| SNHG16 | 17q25.1 | AKT | miR-302a-3p | SNHG16/miR-302a-3p/AKT | Oncogenic | Proliferation | [180] |
| TP73-AS1 | 1p36.32 | PTEN | miR-103 | TP73-AS1/miR-103/PTEN | Tumor suppressive | Proliferation | [181] |
| TP73-AS1 | 1p36.32 | TGF-a | miR-194 | TP73-AS1/miR-194/TGF-a | Oncogenic | Proliferation, migration, invasion | [182] |
| TUG1 | 22q12.2 | KIAA1199 | miR-600 | TUG1/miR-600/KIAA1199 | Oncogenic | Metastasis, EMT | [183] |
| TUSC7 | 3q13.31 | CDK6 | miR-211-3p | TUSC7/miR-211-3p/CDK6 | Tumor suppressive | Proliferation | [184] |
| UCA1 | 19p13.12 | HOXB3 | miR-28-5p | UCA1/miR-28-5p/HOXB3 | Oncogenic | Proliferation, migration | [39] |
| UCC | 7p15.2 | KRAS | miR-143 | UCC/miR-143/KRAS | Oncogenic | Cell growth, invasion | [185] |
| ucoo2kmd.1 | 17q11.2 | CD44 | miR-211-3p | ucoo2lmd.1/miR-211-3p/CD44 | Oncogenic | Proliferation | [186] |
| ZDHHC8P1 | 22q11.23 | miR-34a | ZDHHC8P1/miRNA-34a | Oncogenic | Proliferation, metastasis | [187] | |
| ZFAS1 | 20q13.13 | miR-7-5p | ZFAS1/miR-7-5p | Oncogenic | Proliferation, migration, invasion, apoptosis | [188] | |
| ZFAS1 | 20q13.13 | CDK1/ cyclinB1, p53 |
miR-590-3p | ZFAS1/miR-590-3p | Oncogenic | Apoptosis, p53 dependent cell cycle control | [189] |
| ZNFX1-AS1 | 20q13.13 | EZH2 | miR-144 | ZNFX1-AS1/miR-144/EZH2 | Oncogenic | Proliferation, migration, invasion, metastasis | [190] |
CRC: colorectal cancer, EMT: epithelial mesenchymal transition, CSC: cancer stem cell, TMN stage: classification of malignant tumors, T (tumor), N (lymph nodes), M (metastasis).
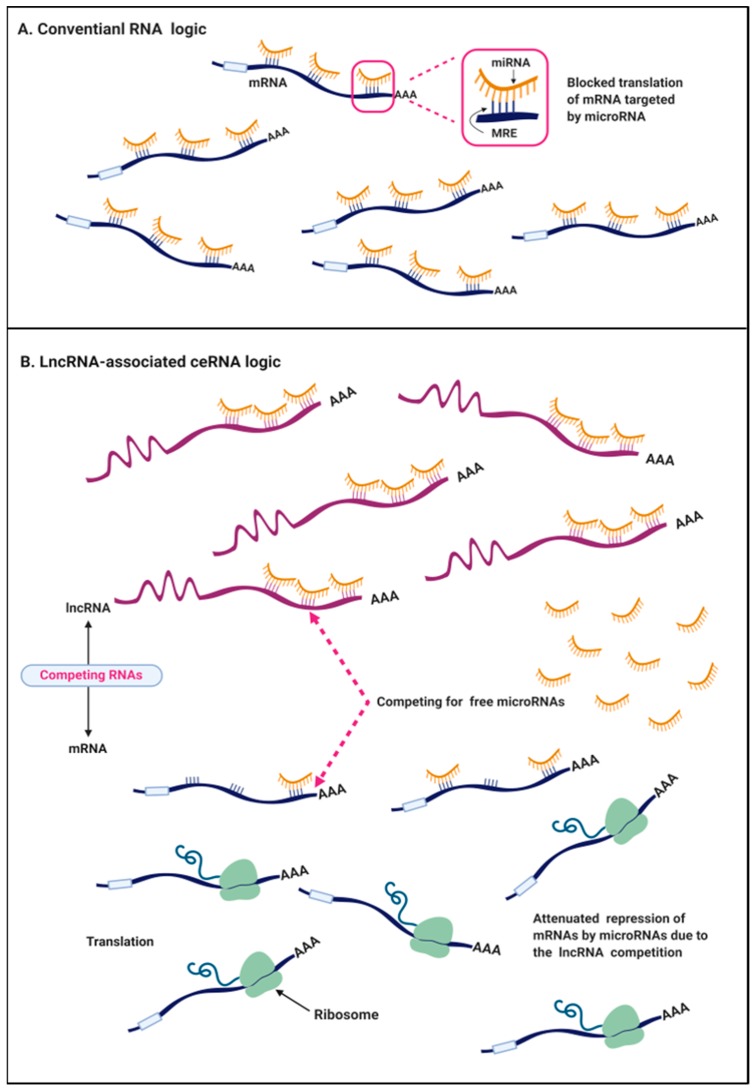
3. The ceRNA Hypothesis in Cancers
The conventional view in the RNA field is that microRNAs (miRNAs), the short endogenous RNA ~23 nt in length, pair to the miRNA recognition elements (MREs) in the protein-coding mRNAs by partial complementarity (Figure 2A) [16]. MREs are often located in 5′ untranslated regions (5′UTRs), coding sequences (CDS), and especially in 3′ untranslated regions (3′UTRs) of various types of RNA transcripts, such as ncRNA and mRNA. Once mature miRNAs guide the miRNA-programmed RNA-induced silencing complex (miR-RISC) to MREs, the mRNA destabilization or posttranslational repression will be actively triggered, leading to the inhibition of gene expression [17]. Most miRNAs pair imperfectly with their cognate mRNAs. A target prediction algorithm has showed that the pairing of miRNA nucleotides 2-8mer to the 3′UTR of the target mRNA is often important [16]. Each miRNA is able to target numerous MREs and repress up to hundreds of transcripts. The best estimate, considering all the 2-8mer perfect and imperfect 3′UTR matches, is that over 60% of human protein-coding genes are potential targets of miRNA, highlighting the involvement of miRNA‒mRNA interaction in diseases including cancer [18,19]. However, surprisingly, many cases of miRNA-mediated regulation are modest, which repress targeted protein expression by less than 2-fold, and usually yield no consequence at a physiological level [20,21]. This discrepancy hints that a large member of RNA communication has been missing, which likely contributes to the repressive effect of miRNA.
Figure 2.
The competitive endogenous RNA (ceRNA) mechanism. (A) In the conventional crosstalk of RNA transcripts, in the cytoplasm, miRNAs exert the suppressive function on protein-coding mRNAs by base pairing with partial complementarity via the miRNA recognition element (MREs) mapped to the 3′UTR of mRNAs. (B) Under the ceRNA mechanism in cancer cells, aberrantly expressed long noncoding RNAs (lncRNAs) with MREs competitively sequestrate miRNAs and reduce the interaction between miRNA and mRNA, and thus attenuate the repression on the downstream mRNAs.
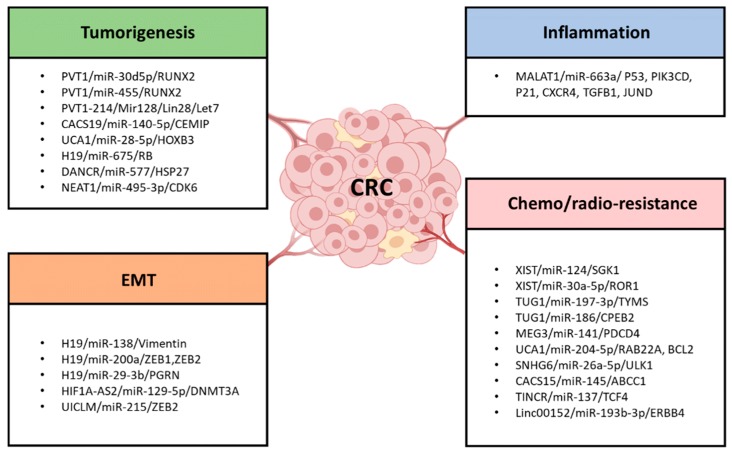
Since miRNA repressors began to be found in plants, animals, and artificial constructs, in 2009, Seitz proposed that a large proportion of RNA transcripts with MREs act as competitive inhibitors of miRNA, so-called “miRNA sponge,” which modulate miRNA expression and function by competing for miRNA binding sites with endogenous mRNAs [20]. Experimental observations supported his theory that the noncoding 3′UTR fragment inhibited miR-199a-3p expression and its activity by acting as a sponge of miRNA [22]. Notably, the competitive endogenous RNA (ceRNA) hypothesis was proposed by Selmena et al. in 2011 [19]. They speculated that ncRNAs, particularly lncRNAs, compete for the miRNA binding sites through partial complementarity, and they named these ncRNAs ceRNAs. This interplay leads to a decrease in the miRNA level and impairment of miRNA activity. The novel ceRNA logic has been validated in Herpesvirus saimiri noncoding RNA, which manipulates host-cell gene expression by degrading mature miR-27 in a binding-dependent manner [23]. Additionally, the effectiveness of the ceRNA pathway is primarily based on the relative levels of ceRNA transcripts. Changes at the ceRNA level are critical to potentiate or attenuate the functions of miRNA on target genes because of the intensified competition. In cancer cells and tissues, miRNAs might be more susceptible to degradation due to the interaction with the aberrantly expressed ncRNAs, especially lncRNAs, thereby regulating important cancer-related genes’ expression. Soon after the novel ceRNA notion was proposed, increasing bioinformatics data have identified that most cancer-related lncRNAs and protein-coding genes in the human genome densely contain MREs, which validates the existence of lncRNA‒miRNA‒mRNA logic in cancers (Figure 2B). Wang et al. first identified the lncRNA-associated ceRNA mechanism in liver cancer, where lncRNA HULC, as a sponge of miR-372, inhibited its activities and consequently reduced the repression of PRKACB [24]. Further experimental evidence indicated that the lncRNA-mediated ceRNA network plays a key role in the carcinogenesis of various cancers, including colorectal cancer, breast cancer, and ovarian cancer. Here, we specially discuss the recent identified lncRNA/ceRNA mechanisms in several hallmarks of colorectal cancer (Figure 3).
Figure 3.
The lncRNA-associated ceRNA networks affect the four common hallmarks of colorectal cancer. Representative lncRNA‒miRNA‒mRNA networks are listed, which highlighted the involvement of lncRNA-ceRNA networks in four major hallmarks of CRC: tumorigenesis, EMT formation, inflammatory process and chemo-/radioresistance.
4. LncRNAs as ceRNA in CRC Tumorigenesis and Progression
Recent studies showed that lncRNA-related ceRNA crosstalk is closely related to the CRC initiation and progression. In this section, we discuss some ceRNA networks and their role in CRC cell proliferation, invasion, and metastasis. Also, we highlight the ceRNA regulatory networks consisting of a lncRNA/miRNA/mRNA axis.
4.1. PVT1/miR-30d-5p/RUNX2
LncRNA PVT1 is located at chromosome 8q.24.21, a region containing many CRC-associated lncRNAs, such as those involved in the Wnt signaling pathway [25]. PVT1 is highly upregulated in CRC cells and tissues. In CRC patients, upregulated PVT1 positively correlates with cell proliferation, invasion, tumor stages, and lymph node metastasis [15]. Previous studies reported that PVT1 promotes CRC development through its regulatory effect on c-myc protein [25]. The latest study conducted by Yu et al. revealed that PVT1 functions as a ceRNA in CRC via the PVT1/miR-30d-5p/RUNX2 axis [26]. Overexpressed PVT1 binds to miR-30d-5p directly, and such competitive binding decreases the abundance of miR-30d-5p and relieves its repression of the downstream target, RUNX2. RUNX2, a novel oncogene correlated with tumor growth and metastasis, can be regulated by several noncoding RNAs by an unclear mechanism [27,28,29,30]. This study presented a positive correlation of PVT1 and RUX2 in CRC tumor tissues in that PVT1 increased RUX2 expression. Likewise, supplementary studies showed that the RUX2 level was reduced in PVT1-knockdown CRC cell lines, but was induced in miR-30d-5p-knockdown CRC cells, suggesting that PVT1 promoted CRC tumorigenesis partly via this PVT1/miR-30d-5p/RUX2 ceRNA network.
4.2. PVT1/miR-455/RUNX2
Chai et al. reported that PVT1 served as a ceRNA of RUNX2 in CRC via the PVT1-miR-455-RUNX2 axis [31]. In CRC cells, PVT1 sponged miR-455 and negatively regulated miR-455 expression, which functions as a tumor suppressor in human cancers. The proliferation of CRC cells is markedly inhibited by PVT1 knockdown, along with increased miR-455, which could be rescued by the miR-455 inhibitor, suggesting that PVT1-induced CRC progression is partly caused by the inhibition of miR-455. Software predicted the potential binding sequences in miR-455 and 3′UTR of PVT1 and RUNX2. Subsequent experiments verified the competitive binding event and indicated that PVT1 promoted CRC development by sponging and inhibiting miR-455 to elevate RUNX2 expression.
4.3. PVT1-214/Mir128/Lin28/Let7
PVT1-214, one of the PVT1 transcripts, is upregulated in human CRC tissues. Recent research demonstrated that, in CRC cells, upregulated PVT1-214 stabilized the expression of Lin28 by harboring miR-128, which eventually repressed the Let7 family, the downstream target of Lin28. This study clearly showed that PVT1-214, as an oncogenic driver of CRC, promoted CRC tumorigenesis via the PVT1-214/miR-128/Lin28/Let7 axis [32].
Taken together, these findings indicated that lncRNA PVT1 acts as ceRNAs of several miRNAs. The identified ceRNA network frame plays a remarkable role in CRC initiation and progression. Moreover, PVT1 as well as the members of the PVT1-associated crosstalk could be potential targets to inhibit cell proliferation and the invasion of CRC.
4.4. CACS19/miR-140-5p/CEMIP
Wang et al. discovered a novel ceRNA interaction of CACS19/miR-140-5p/CEMIP in CRC progression [33]. LncRNA CACS19 is also located on chromosome 8q24.21, which is rich in CRC-related oncogenic lncRNAs. Their study revealed that CACS19 reversed the tumor-suppressive effect of miR-140-5p by competing for the MREs with CEMIP mRNA, miR-140-5p’s direct target, which led to an upregulation of CEMIP mRNA. CEMIP promotes tumor cell survival through the breakdown of glycogen [34]. This investigation uncovered a novel CACS19-related ceRNA mechanism whereby CACS19 enhanced CEMIP by physically harboring miR-140-5p and abolishing its availability, thus contributing to CRC cell proliferation and tumor growth. As a result, all the members of this novel CACS9/miR-140-5p/CEMIP axis could serve as potential therapeutic targets for CRC.
4.5. UCA1/miR-28-5p/HOXB3
As an oncogenic lncRNA, UCA1 is upregulated and exerts a tumor-promoting effect in CRC [35,36,37,38]. Cui et al. reported that UCA1 expression is upregulated in CRC and is positively associated with tumor growth and advanced stages [39]. The data showed that the silencing of UCA1 inhibited CRC proliferation and invasion, not only by suppressing MMP-2/9, but also by a novel lncRNA/miRNA interaction. It was proven that UCA1 acted as a ceRNA of the tumor suppressor miR-28-5p via 3′UTR binding and thereby impeded the repression of HOXB3, which promoted cancer cell proliferation and invasion. This study also indicated that both UCT1 knockdown and miR-28-5P overexpression could be strategies for CRC suppression.
4.6. Other lncRNA/miRNA/mRNA Axis
Additionally, numerous CRC-associated lncRNA/miRNA/mRNA axis have been reported in recent studies; they are involved in CRC cell proliferation, migration, invasion, tumor growth, and metastasis. Most of the previously identified lncRNAs, located on different chromosomes, exert a regulatory effect as ceRNAs of miRNAs in CRC. For instance, LncRNA H19 promotes CRC development and malignancy transformation, partly through the H19/miR-675/RB axis [40]. LncRNA DANCR exerts its oncogenic function on CRC tumor growth and liver metastasis through the DANCR/miR-577/HSP27 axis [41]. LncRNA ZNF148 induces cell proliferation in CRC via the ZNF148/miR-101,144,336,356/TOP2A axis [42]. LncRNA NEAT1 is proven to be positively associated with CRC tumor differentiation, metastasis, and TNM stages through the NEAT1/miR-495-3p/CDK6 axis [27,43]. These competitive interactions reveal the hidden lncRNA-mediated mechanisms underlying CRC initiation and progression.
5. LncRNAs as ceRNA in the EMT and Cell Stemness Formation in CRC
In cancer, epithelial to mesenchymal transition (EMT), marked by the loss of E-cadherin, enables the epithelial cells of a primary tumor to lose cell polarity and break the cellular adhesion constraints, which allows carcinoma cells to gain migratory and invasive properties and be mesenchymal-like towards aggressive malignancy [44,45,46]. As a pathological mechanism, EMT has been reported to initiate CRC metastasis from the primary tumor to distant sites, especially to liver and lymph nodes. Moreover, previous studies have indicated a strong association between the chemoresistance and acquisition of EMT in various cancers [29]. Clinical evidence clearly suggests that the altered expression of EMT-related markers (e.g., the reduced cell adhesion molecules E-cadherin and increased mesenchymal marker, Vimentin [47,48,49]) is not only involved in CRC metastasis, but also in chemotherapy resistance [50,51,52,53,54,55]. Emerging evidence indicates that lncRNAs could be considered as novel EMT markers in various cancers. Mechanically, several lncRNAs promote EMT formation via traditional mechanisms. For instant, lncRNA MALAT1 showed a positive correlation with the expression level of EMT-transcriptional factor, ZEB1, ZEB2, and SNAI2 [56]. HOTAIR mediated EMT formation, together with PRC2 and LSD1 proteins, reprogramming the chromatin profile of the epithelial cells to that of mesenchymal cells [57]. Furthermore, recent studies based on the ceRNA mechanism provide a new understanding of lncRNA-associated EMT formation CRC.
5.1. H19
LncRNA H19, located on chromosome 11 in humans, contributes to EMT formation by regulating relevant signaling pathways or molecules in colorectal cancer, lung cancer, breast cancer, and pancreatic cancer [58,59,60,61]. Transforming growth factor-β1 (TGF-β1) is a conventional inducer to establish an EMT model in various epithelial cells, and potentiated H19 expression has been found in TGF-β1-induced EMT model in CRC cells [58,62]. Furthermore, cells expressing H19 displayed mesenchymal-like properties. Recently, H19 has been reported to promote EMT in CRC via a novel ceRNA mechanism, suggesting that upregulated H19 is a biomarker of CRC metastasis and, more importantly, could be a promising therapeutic target for CRC treatment.
5.1.1. H19/miR-138/Vimentin and H19/miR-200a/ZEB1, ZEB2
Liang et al. reported that, in colon cancer cells, upregulated H19 competitively harbors miRNA-138 and miRNA-200a, which hampers the complementary bindings between miRNAs and the mRNAs of Vimentin, ZEB1, and ZEB2. miR-138 and miR-200 are known to suppress EMT in cancer cells by suppressing the translation of EMT regulators, such as Vimentin and ZEB1/2 [63,64,65]. Long et al. detected that the ectopic expression of miR-138 results in a suppression of CRC metastasis by inhibiting the EMT inducer TWIST2 in CRC cells and tissues [66]. Similarly, in breast cancer, miR-138 inhibited EMT by increasing E-cadherin and reducing Vimentin, which is a filament protein highly expressed in mesenchymal cells [67]. Additionally, miR-200a, belonging to the miR-200 family, inhibits colon cancer EMT by targeting and repressing ZEB1/2 [68]. In summary, this study found that H19 promoted EMT formation in CRC through H19/miR-138/Vimentin and H19/miR-200a/ZEB1/2 ceRNA networks [58], by which: 1) H19 acted as a ceRNA to compete for free miR-138 and miR-200a, which sequestered these two miRNA species and freed the 3′UTR of targeted mRNAs; 2) due to the competitive binding events, H19 abolished the suppressive effect on Vimentin and ZEB1/2. Similarly, the investigation of Yang et al. found that H19 promoted the migration and invasion of CRC cells, as well as CRC tumor growth and liver metastasis, by competitively sponging miR-138 to derepress the oncoprotein HMGA1 [69,70].
5.1.2. H19/miR-29-3b/PGRN
Intriguingly, another study conducted by Ding et al. confirmed that H19 promoted EMT in CRC via the ceRNA mechanism [71]. Clinical pathological studies of CRC patients indicated that overexpressed H19 and downregulated miR-29-3b were both observed in the tissue samples of CRC patients with poor differentiation, advanced stages, and distant metastasis. Consistently, H19 attenuated E-cadherin and increased Vimentin and Snail in CRC cells. MiR-29-3b acts as a tumor suppressor, which increased E-cadherin and constrained Vimentin and Snail. More importantly, miR-29-3b suppressed Wnt/β-catenin signaling and c-Myc, Cyclin D1 by inhibiting PGRN (a growth factor involved in tumorigenesis and would healing) [72]. On the other hand, PGRN exhibited the regulatory effect on EMT of epithelial ovarian cancer cells [73]. Based on software prediction and in vitro evidence, it is found that 1) H19 was positively correlated with the pathogenesis of EMT of CRC; 2) H19 competitively sponged miR-29-3b; and 3) H19 negatively regulated miR-29-3b abundance and abolished its suppressive effect on PGRN and Wnt signaling in CRC cells. Overall, H19 promoted EMT in colorectal cancer via a novel ceRNA network of H19/miR-29-3b/PGRN/Wnt signaling axis.
5.2. HIF1A-AS2/miR-129-5p/DNMT3A
LncRNA HIF1A-AS2, which is an antisense transcript of HIF1A, plays a key role in the tumorigenesis of various cancers, such as glioblastoma and bladder cancer [74,75,76]. A recent study by Lin et al. reported that HIF1A-AS2 induced the EMT formation of colorectal cancer through the miR-129-5p/DNMT3A ceRNA pathway [77]. Clinical evidence showed a strong correlation between the highly-expressed HIF1A-AS2 and advanced stage in CRC patients. HIF1A-AS2 promoted cell invasion and EMT of CRC cells by inhibiting E-cadherin. It was observed that HIF1A-AS2 enhanced DNMT3A by competitively binding with miR-129-5p and diminishing its suppressive effect on the translation of DNMT3A mRNA. DNMT3A is a member of the DNA methyltransferases (DNMTs) family [78]. The dysregulation of the DNMTs family, including DNMT1, DNMT3A, and DNMT3B, has been reported to be responsible for malignant transformation in colon, lung, liver, and breast cancer [79,80,81,82]. HIF1A-AS2 augmented DNMT3A by acting as a ceRNA of miR-129-5p, leading to EMT formation and CRC progression. This study not only identified the oncogenic function of HIF1A-AS2 in CRC, but also provided new therapeutic targets based on the HIF1A-AS2/miR-129-5p/DNMT3A ceRNA network.
5.3. UICLM/miR-215/ZEB2
Chen and colleagues first characterized the role of lncRNA UICLM-mediated ceRNA network in CRC liver metastasis. UICLM promoted EMT formation and cell stemness through the UICLM/miR-215/ZEB2 network [83]. Clinicopathological evidence showed that UICLM is highly overexpressed in CRC patients with liver metastasis, suggesting that UICLM is required for the CRC cell EMT process and stemness formation. In vitro evidence further demonstrated that UICLM enhanced ZEB2, the activator of EMT and liver metastasis, by competitively harboring miR-215, thus antagonizing its inhibitory effect on the translation of ZEB2. This finding provided the missing link between lncRNA and CRC liver metastasis, as well as a novel paradigm for the ceRNA mechanisms underlying CRC metastasis. Taken together, UICLM is a promising therapeutic target since the knockdown of UICLM not only negatively regulates ZEB2, but also markedly inhibits stemness-related genes such as SOX2, Notch1, and cancer stem cell (CSC)-associated surface antigens, such as CD44 and CD24.
6. LncRNA as ceRNA in the Inflammation Formation in CRC
Chronic inflammation plays a causal role in CRC development. An increased risk of developing CRC has been observed in patients with inflammatory bowel disease (IBD) [84]. IBD are chronic inflammatory conditions of the gastrointestinal (GI) tract and mainly include Crohn’s disease (CD) and ulcerative colitis (UC) [85]. CD has been acknowledged as transmural intestinal inflammation, which could impact any part of the GI tract, while UC is a superficial inflammation that typically involves the large bowel [86]. CRC developed from IBD is known as colitis-associated colorectal cancer (CAC). LncRNAs are uniquely expressed in certain IBD conditions and play critical roles in the inflammation process in both CD and UC [87]. For instance, lncRNA DQ786243 is the first reported lncRNA that participates in the pathogenesis of CD and CRC; ANRIL (also called CDKN2B-AS1) is dysregulated in an IBD pathology context and may regulate inflammatory responses by acting as a component of the nuclear factor-κB (NF-κB) pathway; the UC-associated lncRNA BC012900 represents its potential as a diagnostic biomarker in IBD progression since BC012900 is particularly differentially expressed in UC samples [88,89,90]. Notably, several lncRNAs are involved in the autophagy process in CRC development [91,92]. Autophagy is a cellular hemostatic process, whereby the cell eliminates intracellular components and removes harmful pathogens from the cytoplasm. Autophagy is critical to inflammation and the tumor microenvironment of CRC since it impacts the hemostasis and survival of inflammatory cells, including macrophages, neutrophils, T lymphocytes, and B lymphocytes [93]. LncRNA KCNQ1OT1 and lincRNA POU3F3 knockdown induced autophagy in CRC cell lines [94,95]. In particular, some lncRNAs regulate autophagy in the tumorigenesis of CRC and CAC by behaving as ceRNA of inflammation/autophagy-related miRNAs.
The study conducted by Zheng et al. found that lncRNA HAGLROS regulated the autophagy and apoptosis of HCT116 cells by acting as ceRNA of autophagy-related miRNA, miR-100 and inhibiting its availability [96]. miR-100 targeted the 3′UTR of autophagy-related 5 (ATG5) and consequently inhibited its expression, thus resulting in the suppression of cell autophagy. Also, miR-100 promoted cell autophagy in osteosarcoma and hepatocellular carcinoma (HCC) [97,98]. Knockdown of HAGLROS efficiently inhibited autophagy and induced apoptosis via the ceRNA network linking autophagy-related miRNA and proteins. In addition, Liu et al. reported that lncRNA UCA1 contributed to the autophagy of CRC cells by harboring miR-185-5p to activate the WNT1-inducible signaling pathway protein 2 (WISP2)/β-catenin pathway [99].
Tian et al. revealed that inflammation-related lncRNA MALAT1 and miR-663a constitute a ceRNA network in CRC cells through sequence-dependent binding [100]. They illustrated that MALAT1 reduced miR-663a expression via a ceRNA mechanism, to prevent the degradation of most of miR-663a’s targets (P53, PIK3CD, P21, CXCR4, TGFB1, and JUND) in CRC cells and tissues. Notably, MALAT1 has been identified as an inflammatory regulator in human systematic lupus erythematosus, and miR-663a is involved in the pathology in chronic inflammation, whereby it induced pro-inflammatory cytokines to promote inflammation in joints [101,102]. MALAT1 and miR-663a may be involved in CRC development and inflammation formation.
7. LncRNA as ceRNA in Chemoresistance/Radioresistance of CRC
Chemo-/radioresistance causes cancer recurrence and failed clinical outcome [103]. However, the molecular mechanisms of chemo-/radioresistance remain poorly understood, which prevents the success of cancer treatment. Since studies have indicated that the ceRNA mechanism has strong relevance to cancer initiation and progression, it is increasingly speculated that the lncRNA-mediated ceRNA network plays a key role in the acquirement of chemo-/radioresistance in cancers. The latest research has identified that the lncRNA/miRNA/mRNA pathway regulated doxorubicin-based, 5-fluoroural-based, and oxaliplatin-based chemotherapies for CRC. For example, MALAT1 conferred oxaliplatin resistance to CRC via the miR-218/EZH2 axis by promoting EMT formation, suggesting that lncRNA, as well as members of the lncRNA-related ceRNA crosstalk, could be therapeutic targets for CRC [104].
7.1. XIST
Doxorubicin (DOX) is a commonly used chemotherapeutic agent for CRC treatment. However, the occurrence of chemoresistance limits its application in clinic. A previous study has suggested that the acquisition of DOX resistance is related to the EMT formation in CRC cells [105]. After knockdown of TGFβ signaling in CRC cells, the EMT process was reversed and the sensitivity to DOX was significantly increased. Apart from EMT, recent studies revealed that lncRNA XIST participated in the mechanism of DOX resistance acquisition in colorectal cancer. The study conducted by Zhu et al. found that XIST induced DOX resistance by sponging miR-124 to upregulate SGK1 expression [106]. It has been reported that SGK1 could confer chemo- and radioresistance in various malignancies [107]. Amato et al. reported that activated SGK1 induced the DOX resistance in renal carcinoma cells [108]. Considering the involvement of the XIST-mediated ceRNA mechanism in DOX-resistant CRC cells, knockdown/silencing of XIST might be a potential strategy to overcome chemoresistance in human CRC cells. Additionally, Zhang et al. confirmed that XIST promoted CRC progression under the influence of chemo drugs via a novel ceRNA-dependent mechanism. The upregulated XIST competitively interacted with miR-30a-5p at the 3′UTR and, thus, alleviated the repression effect on its downstream target, the mRNA of ROR1 [109]. Previous studies reported that ROR1 functions as a regulator of EMT-related genes and highly expressed ROR1 exhibited a positive correlation to the malignancy attributes of CRC patients [110,111]. Furthermore, they discovered that atractylenolide II, a natural product extracted from the dried rhizome of Atractylodes macrocephala, successfully enhanced the sensitivity of CRC cells to several first-line chemo drugs, such as 5-fluorouracil (5-FU), doxorubicin (DOX), and cisplatin, by disturbing the XIST/miR-30-5p/ROR1 ceRNA network [112]. Mechanically, Atractylenolide II suppressed the cell proliferation capacity by decreasing XIST and ROR1 expression, thus efficiently reversing the XIST-induced chemoresistance of CRC cells. In summary, these findings indicated the crucial role of XIST-mediated ceRNA crosstalk in the chemoresistance of CRC. More importantly, they identified the XIST ceRNA axis as a promising target to overcome chemoresistance in CRC.
7.2. TUG1
5-fluorouracil (5-FU) is a primary chemotherapy drug for various cancers, particularly for colorectal cancer. 5-FU inhibits the nucleotide synthetic enzyme thymidylate synthase (TYMS) and incorporates its metabolites into DNA and RNA, which leads to the inhibition of the DNA synthesis and the disruption of RNA processing and post-transcriptional modification in cancer cells [113]. However, chemoresistance limits the response rates of 5-FU-based chemotherapy for advanced CRC treatment. A recent study suggested that lncRNA TUG1 modulated 5-FU resistance in CRC cells via the TUG1/miR-197-3p/TYMS signaling [114]. Researchers found that TUG1 promoted the cell viability and proliferation of 5-FU-resistant CRC cells by a novel ceRNA mechanism. TUG1 upregulated TYMS by competitively sequestering miR-197-3p. TYMS is a direct target of miR-197-3p. This interaction decreased the miR-197-3p expression and relieved its suppression effect on TYMS. Moreover, this study reported that TUG1 is positively correlated to 5-FU resistance as well as CRC recurrence. TUG1 could be considered not only as a potential silencing target to overcome 5-FU resistance in CRC cells, but also as a biomarker to assess the clinical response to 5-FU in CRC patients. The TUG1-mediated ceRNA mechanism also plays a key role in methotrexate (MTX) resistance in colorectal cancer. MTX has been used for cancer treatment since 1956 [115]. It works as an inhibitor of the dihydrofolate reductase (DHFR) enzyme to block the biosynthesis of DNA [116]. However, MTX resistance limits its clinical outcomes in CRC therapy. Li et al. first discovered that TUG1 is highly upregulated in MTX-resistant CRC tumors [117]. Based on software predictions, TUG1 and mRNA of CPEB2 are both potential targets of miR-186. Further studies showed that overexpressed TUG1 elevated CPEB2 by competitively hijacking miR-186. This study found that CPEB2 could confer MTX resistance to CRC cells. The role of CPEB2 in CRC remains unknown. Overall, TUG1 exhibited a positive correlation to chemoresistance in CRC cells and tissue specimens via ceRNA networks, and therefore represented a therapeutic target to overcome drug resistance for CRC treatment.
7.3. MEG3
Oxaliplatin (OXA) is a first-line platinum drug with proven suppression activity upon colon tumors [118]. OXA resistance caused failure in CRC treatment via an unclear mechanism. Li et al. reported that MEG3 enhanced the susceptibility of CRC to oxaliplatin by promoting cell cytotoxicity [119]. Importantly, Wang et al. identified that overexpressed MEG3 ameliorated CRC sensitivity to oxaliplatin via the ceRNA mechanism [120]. MEG3 functions as ceRNA of miR-141, which results in the inhibition of miR-141 and thus the de-repression of downstream target, PDCD4. Notably, PDCD4 sensitized cancer cells to cisplatin, paclitaxel, and docetaxel by acting as a tumor suppressor to induce apoptosis [121,122,123]. This study proves that the overexpression of MEG3 could be a potential strategy to improve therapeutic outcomes for CRC.
7.4. UCA1
Clinicopathological evidence obtained from CRC patients highlighted that the expression of UCA1 was correlated with lymph node metastasis, tumor stage, and poor prognosis [124]. A previous study demonstrated that UCA1 increased cisplatin resistance in bladder cancer cells [125]. Recently, Bian et al. observed that UCA1 induced 5-FU resistance in CRC cells via a ceRNA logic, whereby UCA1 inhibited miR-204-5p expression and its activity through competitively enriching miR-204-5p at its 3′UTR binding sequences, leading to the release of the mRNA of RAB22A and BCL2 [38]. Therefore, as the inducers of cell apoptosis, RAB22A and BCL2 protein level and activities were activated in 5-FU resistant cells. A subsequent study confirmed that knockdown of RAB22A increased chemo responsiveness in CRC cells [126]. This investigation illustrated that UCA1 induced 5-FU resistance via the miR-204-5p/BCL2, RAB22A ceRNA axis.
7.5. Linc00152
Emerging evidence revealed that Linc00152 promoted tumorigenesis via ceRNA pathways in various cancers. For example, Linc00152 increased cell proliferation by sponging miR-193b-3p in osteosarcoma, and promoted leukemogenesis by targeting the miR-193a/CDK9 axis [127,128]. A recent study evaluated the pivotal role of linc00152 in the ceRNA mechanism, by which it conferred chemoresistance in colorectal cancer. Yue et al. demonstrated that linc00512 reduced the sensitivity of CRC cells to oxaliplatin via the miR-193a-3p/ERBB4/AKT pathway to regulate the expression of miR-193a-3p and ERBB4 [129]. In CRC, miR-193a-3p showed tumor suppressor properties by arresting the cell cycle and inducing apoptosis; in contrast, ERBB4 enhanced the survival rate of CRC cells with activated P13K, EGFR pathway, and inflammation factors [130,131]. Thus, linc00512 induces resistance in oxaliplatin-treated CRC cells due to its induction effect on ERBB4 by competitively harboring and titrating miR-193a-3p. Another study confirmed that linc00512 was involved in chemoresistance by more than one ceRNA logic [132]. Linc00512 promoted 5-FU resistance in CRC via miR-139-5p/NOTCH1 axis by driving growth and metastasis. Mechanically, overexpressed linc00512 inhibited tumor suppressor miR-139-5p to relieve its repression on NOCH1, which was positively related to the poor survival rate of CRC. Taken together, these studies revealed that the linc00512-mediated ceRNA network is closely correlated with the occurrence of chemoresistance in CRC.
7.6. SNHG6
Recent studies elucidated that LncRNA SNHG6 (also known as ncRAN) contributed to 5-FU resistance in CRC by promoting CRC cell autophagy [133]. Autophagy is a cellular self-digestion process that contributes to tumor development and resistance to chemotherapy drugs [134,135,136,137,138]. SNHG6 induced autophagy with enhanced autophagosome formation, thus leading to the acquisition of 5-FU resistance in CRC cells. ULK1 is an important initiator of autophagy. It was observed that SNHG6 interacted with ULK1 and motivated its autophagy-induced function by sequestrating miR-26a-5p, which is an autophagy suppressor. This study illustrated that lncRNAs could regulate autophagy and autophagy-related chemoresistance through the ceRNA network in CRC cells.
7.7. CACS15
Gao et al. investigated the molecular mechanism of the oncogenic lncRNA CACS15 in oxaliplatin-resistant CRC cells [139]. They discovered that CASC15 was upregulated in OXA-resistant CRC cells, while, CASC15-silenced OXA-resistance CRC cells regained sensitivity to OXA. Mechanistically, CACS15 promoted oxaliplatin resistance to CRC cells by elevating ABCC1 via the CACS15/miR-145 axis. In this case, downregulation of CASC15 could be a therapeutic strategy to facilitate the response of CRC patients to oxaliplatin.
7.8. TINCR
Besides chemotherapy, radiation is a widely used CRC treatment. However, the high occurrence of radioresistance results in failed radiotherapy in CRC patients [140]. Kang et al. demonstrated that knockdown of TINCR inhibited radioresistance via the miR-137/TCF4 ceRNA axis [141]. They speculated that the stemness of CRC cells was associated with the radioresistance since cancer stem cells possess tumor-initiating capacity [142]. Intriguingly, TINCR and TCF4 both induced stemness in radioresistant CRC cells. Though the mechanism is still unknown, this study provided potential biomarkers for assessing the outcomes of radioresistance for CRC therapy.
Collectively, mounting evidence indicated the involvement of lncRNA-mediated ceRNA interplay in chemo-/radioresistance in colorectal cancer. These findings provided potential predictors for the acquisition of chemo-/radioresistance and shed light on the clinical implication of lncRNA-associated ceRNA mechanisms in overcoming cancer chemoresistance. So far, there are still a large number of resistance-related lncRNAs in CRC that have not been studied. For example, lncRNA CCAT1 enhanced the 5-FU resistance in CRC cells by an unidentified mechanism. Therefore, further investigations of lncRNAs in CRC chemoresistance are needed to ensure better clinical outcomes.
8. Databases for the Prediction of lncRNA-Associated ceRNA Interactions
Bioinformatics and software algorithms are potent tools for the prediction and validation of RNA interactions based on the ceRNA hypothesis. Below we list some freely available databases for the exploration of lncRNA-associated ceRNA networks.
starBase v2.0 (http://starbase.sysu.edu.cn/) is a database used for the systematic identification of miRNA‒ncRNA (including lncRNAs, pseudogenes, circRNAs) and miRNA‒mRNA interaction networks from 108 CLIP-Seq (HITS-CLIP, PAR-CLIP, iCLIP, CLASH) datasets. More importantly, starBase v2.0 is the first database containing miRNA‒pseudogene and miRNA‒circular RNA interactions based on Ago and RBP binding sites, which contributes to the construction of miRNA‒lncRNA ceRNA regulatory networks [143].
DIANA-LncBase (www.microrna.gr/LncBase) is a comprehensive annotation first established for the transcriptome-wide prediction of lncRNA and miRNA functional interactions based on MREs in human and mouse lncRNAs. It also details information for each miRNA‒lncRNA pair, such as representation of the binding sites, MREs conservation, and prediction scores, as well as lncRNA tissue expression [144].
spongeScan (http://spongescan.rc.ufl.edu) is the first web algorithm used for the identification of putative MREs in lncRNAs and the assessment of their likely behavior as ceRNAs. This novel application is based on sequence complementarity and sequence information is available for any organism [145].
lnCeDB database (http://gyanxet-beta.com/lncedb/) was developed to browse for lncRNA‒mRNA pairs sharing common miRNA, and to estimate the probability of each pair being ceRNAs in 22 human tissues [146].
LncNetP is a large-scale RNA-seq database developed for the systematic identification and prioritization of disease/cancer-associated lncRNAs based on the ceRNA hypothesis [147].
Other databases: The SomamiR database (http://compbio.uthsc.edu/SomamiR) was designed for detecting potential alterations of miRNA‒ceRNA interactions in cancer somatic mutations, including miRNA‒lncRNA interplay [148]. miRsponge was developed from the data on 500 miRNA sponge interactions and 463 ceRNA relationships from 11 species based on published articles [149]. PceRBase (http://bis.zju.edu.cn/pcernadb/index.jsp) is a plant ceRNA database containing potential ceRNA pairs from 26 plant species [150]. Linc2GO is the first lincRNA functional annotation database based on the ceRNA hypothesis, and is freely available (http://www.bioinfo.tsinghua.edu.cn/~liuke/Linc2GO/index.htm) [151].
9. Conclusions and Future Outlook
While only ~1.5% of the human genome encodes protein-coding genes, the rest of the genome contains noncoding sequences. Most of these non-protein-coding DNA sequences are transcribed into RNA; among those are thousands of miRNAs and tens of thousands of lnRNAs. As discussed in this review, many lnRNAs compete with specific mRNAs in their binding to miRNAs. These lnRNA‒miRNA‒mRNA competitive endogenous RNA networks form a complex and highly regulated mechanism to control gene expression and cellular functions. Since the lncRNA members of the ceRNA networks are frequently involved in the advanced stages of CRC (for example, CACS15, CYTOR, HOTAIR, MALAT1, TUG1, NEAT1 and MIR17HG) these lncRNAs may serve as potent prognostic biomarkers. More importantly, knockdown/overexpression of these abovementioned members within CRC-associated ceRNA networks significantly suppressed CRC progression, suggesting their potential role as therapeutic targets. Despite intensive research on the molecular mechanisms behind colorectal cancer in recent decades, this cancer remains one of the most lethal malignancies due to the frequent occurrence of EMT, metastasis, and chemo-/radioresistance. Research on the novel lncRNA-associated ceRNA network may open up new avenues in CRC therapy and overcoming drug resistance. Our understanding of these ceRNA networks is still in the early stages. The precise mechanisms of their involvement in cancer progression are still largely unknown. More advanced genome-wide algorithms are needed for ceRNA prediction in order to identify new prognostic biomarkers. New strategies need to be developed (such as new delivery methods to deploy siRNA or CRISPR) to target these ceRNA networks for cancer therapy.
Abbreviations
| ABCC1 | ATP Binding Cassette Subfamily C Member 1 |
| AKT | AKT Serine/Threonine Kinase 1 |
| BCAR4 | Breast Cancer Anti-Estrogen Resistance 4 |
| BCL2 | B-Cell CLL/Lymphoma 2 |
| CACS15 | Cancer Susceptibility 15 |
| CASC19 | Cancer Susceptibility 19 |
| CASC2 | Cancer Susceptibility 2 |
| CCAT1 | Colon Cancer Associated Transcript 1 |
| CCAT2 | Colon Cancer Associated Transcript 2 |
| CDC42 | Cell Division Cycle 42 |
| CDK1 | Cyclin-Dependent Kinase 1 |
| CDK6 | Cyclin-Dependent Kinase 6 |
| CDK9 | Cyclin-Dependent Kinase 9 |
| CEMIP | Cell Migration Inducing Hyaluronidase 1 |
| CPEB2 | Cytoplasmic Polyadenylation Element Binding Protein 2 |
| CRNDE | colorectal neoplasia differentially expressed |
| CXCR4 | C-X-C Motif Chemokine Receptor 4 |
| CYTOR | Long Intergenic Non-Protein Coding RNA 152 |
| DANCR | Differentiation antagonizing non-protein noding RNA |
| DNMT3A | DNA Methyltransferase 3 Alpha |
| ERBB2 | Erb-B2 Receptor Tyrosine Kinase 4 |
| EZH2 | Enhancer of Zeste 2 Polycomb Repressive Complex 2 |
| FOXD2-AS1 | FOXD2 Antisense RNA 1 |
| FOXD3-AS1 | FOXD3 Antisense RNA 1 |
| GACAT3 | Gastric Cancer Associated Transcript 3 |
| HAND2-AS1 | HAND2 Antisense RNA 1 |
| HAGLROS | HAGLR opposite strand lncRNA |
| HIF1A-AS2 | HIF1A Antisense RNA 2 |
| HOTAIR | HOX Transcript Antisense RNA |
| HSP27 | Heat Shock Protein 27 |
| HULC | Hepatocellular Carcinoma Associated Transcript 1 |
| KCNQ1OT1 | KCNQ1 opposite strand/antisense transcript 1 |
| KIAA1199 | Cell Migration Inducing Hyaluronidase 1 |
| KLF14 | Kruppel-Like Factor 14 |
| KRAS | K-Ras |
| LGR5 | Leucine Rich Repeat Containing G Protein-Coupled Receptor 5 |
| LIMK2 | LIM Domain Kinase 2 |
| LINC00460 | Long Intergenic Non-Protein Coding RNA 460 |
| LINC00668 | Long Intergenic Non-Protein Coding RNA 668 |
| LINC00858 | Long Intergenic Non-Protein Coding RNA 858 |
| LINC01234 | Long Intergenic Non-Protein Coding RNA 1234 |
| LINC01296 | Long Intergenic Non-Protein Coding RNA 1296 |
| LINC02418 | Long Intergenic Non-Protein Coding RNA 2418 |
| LSD1 | Lysine Demethylase 1A |
| MACC1 | MET Transcriptional Regulator MACC1 |
| MALAT1 | Metastasis Associated Lung Adenocarcinoma Transcript 1 |
| MBNL1-AS1 | MBNL1 Antisense RNA 1 |
| MEG3 | Maternally Expressed 3 |
| MELK | Maternal Embryonic Leucine Zipper Kinase |
| MIAT | Myocardial Infarction Associated Transcript |
| MIR17HG | MIR17 Host Gene |
| MNX1-AS1 | MNX1 Antisense RNA 1 |
| MYL9 | Myosin Light Chain 9 |
| NEAT1 | Nuclear Paraspeckle Assembly Transcript 1 |
| OECC | Overexpressed in Colorectal Cancer lncRNA |
| PART-1 | Prostate Androgen-Regulated Transcript 1 |
| PCAT1 | prostate cancer associated transcript 1 |
| PDCD4 | Programmed Cell Death 4 |
| PDCD4 | Programmed Cell Death 4 |
| PGRN | Progranulin |
| PIAS3 | Protein Inhibitor Of Activated STAT 3 |
| PIK3CD | Phosphatidylinositol-4,5-Bisphosphate 3-Kinase Catalytic Subunit Delta |
| POU3F3 | POU class 3 homeobox 3 |
| POU5F1P1 | POU class 5 homeobox 1B |
| PRC2 | Polycomb Repressive Complex 2 |
| PTEN | Phosphatase And Tensin Homolog |
| PTEN | Phosphatase And Tensin Homolog |
| PVT1 | Plasmacytoma Variant Translocation 1 |
| RAB22A | Ras-Related Protein Rab-22A |
| ROR | Long Intergenic Non-Protein Coding RNA, Regulator Of Reprogramming |
| ROR1 | Receptor Tyrosine Kinase Like Orphan Receptor 1 |
| RTKN | Rhotekin |
| RUNX2 | Runt-Related Transcription Factor 2 |
| SEC61A1 | SEC61 Translocon Alpha 1 Subunit |
| SHMT2 | Serine Hydroxymethyltransferase 2 |
| SIRT1 | Sirtuin 1 |
| SNHG15 | Small Nucleolar RNA Host Gene 15 |
| SNHG16 | Small Nucleolar RNA Host Gene 16 |
| SNRHG6 | Small Nucleolar RNA Host Gene 6 |
| SP1 | Sp1 Transcription Factor |
| STAT3 | Signal Transducer And Activator Of Transcription 3 |
| TCF4 | Transcription Factor 4 |
| TGF-a | Transforming Growth Factor Alpha |
| TGFB1 | Transforming Growth Factor Beta 1 |
| TINCR | Tissue Differentiation-Inducing Non-Protein Coding RNA |
| TOP2A | Topoisomerase (DNA) II Alpha |
| TP73-AS1 | lncRNA P73 antisense RNA 1T |
| TUG1 | Taurine Up-Regulated 1 |
| TUSC7 | Tumor Suppressor Candidate 7 |
| TYMS | Thymidylate Synthetase |
| UCA1 | Urothelial Cancer Associated 1 |
| UCC | A novel lincRNA termed upregulated in CRC |
| ULK1 | Unc-51 Like Autophagy Activating Kinase 1 |
| USP47 | Ubiquitin Specific Peptidase 47 |
| VEGFC | Vascular Endothelial Growth Factor C |
| XIST | X Inactive Specific Transcript |
| YWHAZ | Tyrosine 3-Monooxygenase/Tryptophan 5-Monooxygenase Activation Protein Zeta |
| ZDHHC8P1 | Zinc Finger DHHC-Type Containing 8 Pseudogene 1 |
| ZEB1 | Zinc Finger E-Box Binding Homeobox 1 |
| ZEB2 | Zinc Finger E-Box Binding Homeobox 2 |
| ZFAS1 | ZNFX1 Antisense RNA 1 |
| ZNF148 | Zinc Finger Protein 148 |
| ZNFX1-AS1 | ZNFX1 Antisense RNA 1 |
Funding
This research was supported by NIH grant CA186100.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Macrae F.A. Colorectal Cancer: Epidemiology, Risk Factors, and Protective Factors. [(accessed on 25 October 2019)]; Available online: https://www.uptodate.com/contents/colorectal-cancer-epidemiology-risk-factors-and-protective-factors.
- 2.Fearnhead N.S., Wilding J.L., Bodmer W.F. Genetics of colorectal cancer: Hereditary aspects and overview of colorectal tumorigenesis. Br. Med. Bull. 2002;64:27–43. doi: 10.1093/bmb/64.1.27. [DOI] [PubMed] [Google Scholar]
- 3.Dong Y., Yu T., Ding L., Laurini E., Huang Y., Zhang M., Weng Y., Lin S., Chen P., Marson D., et al. A Dual Targeting Dendrimer-Mediated siRNA Delivery System for Effective Gene Silencing in Cancer Therapy. J. Am. Chem. Soc. 2018;140:16264–16274. doi: 10.1021/jacs.8b10021. [DOI] [PubMed] [Google Scholar]
- 4.Kim H.J., Kim A., Miyata K., Kataoka K. Recent progress in development of siRNA delivery vehicles for cancer therapy. Adv. Drug Deliv. Rev. 2016;104:61–77. doi: 10.1016/j.addr.2016.06.011. [DOI] [PubMed] [Google Scholar]
- 5.Katsushima K., Natsume A., Ohka F., Shinjo K., Hatanaka A., Ichimura N., Sato S., Takahashi S., Kimura H., Totoki Y., et al. Targeting the Notch-regulated non-coding RNA TUG1 for glioma treatment. Nat. Commun. 2016;7:13616. doi: 10.1038/ncomms13616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li X., Xie Z., Xie C., Lu W., Gao C., Ren H., Ying M., Wei X., Gao J., Su B., et al. D-SP5 Peptide-Modified Highly Branched Polyethylenimine for Gene Therapy of Gastric Adenocarcinoma. Bioconj. Chem. 2015;26:1494–1503. doi: 10.1021/acs.bioconjchem.5b00137. [DOI] [PubMed] [Google Scholar]
- 7.Wang J., Lei Y., Xie C., Lu W., Wagner E., Xie Z., Gao J., Zhang X., Yan Z., Liu M. Retro-inverso CendR peptide-mediated polyethyleneimine for intracranial glioblastoma-targeting gene therapy. Bioconj. Chem. 2014;25:414–423. doi: 10.1021/bc400552t. [DOI] [PubMed] [Google Scholar]
- 8.Wang J., Lei Y., Xie C., Lu W., Yan Z., Gao J., Xie Z., Zhang X., Liu M. Targeted gene delivery to glioblastoma using a C-end rule RGERPPR peptide-functionalised polyethylenimine complex. Int. J. Pharm. 2013;458:48–56. doi: 10.1016/j.ijpharm.2013.10.017. [DOI] [PubMed] [Google Scholar]
- 9.Chan J.J., Tay Y. Noncoding RNA: RNA Regulatory Networks in Cancer. Int. J. Mol. Sci. 2018;19:1310. doi: 10.3390/ijms19051310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hanahan D., Weinberg R.A. The hallmarks of cancer. Cell. 2000;100:57–70. doi: 10.1016/S0092-8674(00)81683-9. [DOI] [PubMed] [Google Scholar]
- 11.Orom U.A., Derrien T., Beringer M., Gumireddy K., Gardini A., Bussotti G., Lai F., Zytnicki M., Notredame C., Huang Q., et al. Long noncoding RNAs with enhancer-like function in human cells. Cell. 2010;143:46–58. doi: 10.1016/j.cell.2010.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang K.C., Chang H.Y. Molecular mechanisms of long noncoding RNAs. Mol. Cell. 2011;43:904–914. doi: 10.1016/j.molcel.2011.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shen P., Pichler M., Chen M., Calin G.A., Ling H. To Wnt or Lose: The Missing Non-Coding Linc in Colorectal Cancer. Int. J. Mol. Sci. 2017;18:2003. doi: 10.3390/ijms18092003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ye L.C., Zhu X., Qiu J.J., Xu J., Wei Y. Involvement of long non-coding RNA in colorectal cancer: From benchtop to bedside (Review) Oncol. Lett. 2015;9:1039–1045. doi: 10.3892/ol.2015.2846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Saus E., Brunet-Vega A., Iraola-Guzman S., Pegueroles C., Gabaldon T., Pericay C. Long Non-Coding RNAs As Potential Novel Prognostic Biomarkers in Colorectal Cancer. Front. Genet. 2016;7:54. doi: 10.3389/fgene.2016.00054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bartel D.P. MicroRNAs: Target recognition and regulatory functions. Cell. 2009;136:215–233. doi: 10.1016/j.cell.2009.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thomas M., Lieberman J., Lal A. Desperately seeking microRNA targets. Nat. Struct. Mol. Biol. 2010;17:1169–1174. doi: 10.1038/nsmb.1921. [DOI] [PubMed] [Google Scholar]
- 18.Friedman R.C., Farh K.K., Burge C.B., Bartel D.P. Most mammalian mRNAs are conserved targets of microRNAs. Genome Res. 2009;19:92–105. doi: 10.1101/gr.082701.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Salmena L., Poliseno L., Tay Y., Kats L., Pandolfi P.P. A ceRNA hypothesis: The Rosetta Stone of a hidden RNA language? Cell. 2011;146:353–358. doi: 10.1016/j.cell.2011.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Seitz H. Redefining microRNA targets. Curr. Biol. 2009;19:870–873. doi: 10.1016/j.cub.2009.03.059. [DOI] [PubMed] [Google Scholar]
- 21.Selbach M., Schwanhausser B., Thierfelder N., Fang Z., Khanin R., Rajewsky N. Widespread changes in protein synthesis induced by microRNAs. Nature. 2008;455:58–63. doi: 10.1038/nature07228. [DOI] [PubMed] [Google Scholar]
- 22.Lee D.Y., Jeyapalan Z., Fang L., Yang J., Zhang Y., Yee A.Y., Li M., Du W.W., Shatseva T., Yang B.B. Expression of versican 3’-untranslated region modulates endogenous microRNA functions. PLoS ONE. 2010;5:e13599. doi: 10.1371/journal.pone.0013599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cazalla D., Yario T., Steitz J.A. Down-regulation of a host microRNA by a Herpesvirus saimiri noncoding RNA. Science. 2010;328:1563–1566. doi: 10.1126/science.1187197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang J., Liu X., Wu H., Ni P., Gu Z., Qiao Y., Chen N., Sun F., Fan Q. CREB up-regulates long non-coding RNA, HULC expression through interaction with microRNA-372 in liver cancer. Nucl. Acids Res. 2010;38:5366–5383. doi: 10.1093/nar/gkq285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tseng Y.Y., Moriarity B.S., Gong W., Akiyama R., Tiwari A., Kawakami H., Ronning P., Reuland B., Guenther K., Beadnell T.C., et al. PVT1 dependence in cancer with MYC copy-number increase. Nature. 2014;512:82–86. doi: 10.1038/nature13311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yu X., Zhao J., He Y. Long non-coding RNA PVT1 functions as an oncogene in human colon cancer through miR-30d-5p/RUNX2 axis. J. B.U.ON Off. J. Balk. Union Oncol. 2018;23:48–54. [PubMed] [Google Scholar]
- 27.Gokulnath M., Partridge N.C., Selvamurugan N. Runx2, a target gene for activating transcription factor-3 in human breast cancer cells. Tumour Biol. J. Int. Soc. Oncodev. Biol. Med. 2015;36:1923–1931. doi: 10.1007/s13277-014-2796-x. [DOI] [PubMed] [Google Scholar]
- 28.Tandon M., Chen Z., Pratap J. Runx2 activates PI3K/Akt signaling via mTORC2 regulation in invasive breast cancer cells. Breast Cancer Res. 2014;16:R16. doi: 10.1186/bcr3611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Qin L., Zhang Y., Lin J., Shentu Y., Xie X. MicroRNA-455 regulates migration and invasion of human hepatocellular carcinoma by targeting Runx2. Oncol. Rep. 2016;36:3325–3332. doi: 10.3892/or.2016.5139. [DOI] [PubMed] [Google Scholar]
- 30.Wen C., Liu X., Ma H., Zhang W., Li H. miR3383p suppresses tumor growth of ovarian epithelial carcinoma by targeting Runx2. Int. J. Oncol. 2015;46:2277–2285. doi: 10.3892/ijo.2015.2929. [DOI] [PubMed] [Google Scholar]
- 31.Chai J., Guo D., Ma W., Han D., Dong W., Guo H., Zhang Y. A feedback loop consisting of RUNX2/LncRNA-PVT1/miR-455 is involved in the progression of colorectal cancer. Am. J. Cancer Res. 2018;8:538–550. [PMC free article] [PubMed] [Google Scholar]
- 32.He F., Song Z., Chen H., Chen Z., Yang P., Li W., Yang Z., Zhang T., Wang F., Wei J., et al. Long noncoding RNA PVT1-214 promotes proliferation and invasion of colorectal cancer by stabilizing Lin28 and interacting with miR-128. Oncogene. 2019;38:164–179. doi: 10.1038/s41388-018-0432-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang X.D., Lu J., Lin Y.S., Gao C., Qi F. Functional role of long non-coding RNA CASC19/miR-140-5p/CEMIP axis in colorectal cancer progression in vitro. World J. Gastroenterol. 2019;25:1697–1714. doi: 10.3748/wjg.v25.i14.1697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Banach A., Jiang Y.P., Roth E., Kuscu C., Cao J., Lin R.Z. CEMIP upregulates BiP to promote breast cancer cell survival in hypoxia. Oncotarget. 2019;10:4307–4320. doi: 10.18632/oncotarget.27036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yang X., Liu W., Xu X., Zhu J., Wu Y., Zhao K., He S., Li M., Wu Y., Zhang S., et al. Downregulation of long noncoding RNA UCA1 enhances the radiosensitivity and inhibits migration via suppression of epithelialmesenchymal transition in colorectal cancer cells. Oncol. Rep. 2018;40:1554–1564. doi: 10.3892/or.2018.6573. [DOI] [PubMed] [Google Scholar]
- 36.Han Y., Yang Y.N., Yuan H.H., Zhang T.T., Sui H., Wei X.L., Liu L., Huang P., Zhang W.J., Bai Y.X. UCA1, a long non-coding RNA up-regulated in colorectal cancer influences cell proliferation, apoptosis and cell cycle distribution. Pathology. 2014;46:396–401. doi: 10.1097/PAT.0000000000000125. [DOI] [PubMed] [Google Scholar]
- 37.Neve B., Jonckheere N., Vincent A., Van Seuningen I. Epigenetic Regulation by lncRNAs: An Overview Focused on UCA1 in Colorectal Cancer. Cancers. 2018;10:440. doi: 10.3390/cancers10110440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bian Z., Jin L., Zhang J., Yin Y., Quan C., Hu Y., Feng Y., Liu H., Fei B., Mao Y., et al. LncRNA-UCA1 enhances cell proliferation and 5-fluorouracil resistance in colorectal cancer by inhibiting miR-204-5p. Sci. Rep. 2016;6:23892. doi: 10.1038/srep23892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cui M., Chen M., Shen Z., Wang R., Fang X., Song B. LncRNA-UCA1 modulates progression of colon cancer through regulating the miR-28-5p/HOXB3 axis. J. Cell. Biochem. 2019 doi: 10.1002/jcb.27630. [DOI] [PubMed] [Google Scholar]
- 40.Li X., Wang H., Yao B., Xu W., Chen J., Zhou X. lncRNA H19/miR-675 axis regulates cardiomyocyte apoptosis by targeting VDAC1 in diabetic cardiomyopathy. Sci. Rep. 2016;6:36340. doi: 10.1038/srep36340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wang Y., Lu Z., Wang N., Feng J., Zhang J., Luan L., Zhao W., Zeng X. Long noncoding RNA DANCR promotes colorectal cancer proliferation and metastasis via miR-577 sponging. Exp. Mol. Med. 2018;50:57. doi: 10.1038/s12276-018-0082-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gao X.H., Li J., Liu Y., Liu Q.Z., Hao L.Q., Liu L.J., Zhang W. ZNF148 modulates TOP2A expression and cell proliferation via ceRNA regulatory mechanism in colorectal cancer. Medicine. 2017;96:e5845. doi: 10.1097/MD.0000000000005845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.He Z., Dang J., Song A., Cui X., Ma Z., Zhang Z. NEAT1 promotes colon cancer progression through sponging miR-495-3p and activating CDK6 in vitro and in vivo. J. Cell. Physiol. 2019;234:19582–19591. doi: 10.1002/jcp.28557. [DOI] [PubMed] [Google Scholar]
- 44.Ishiwata T. Cancer stem cells and epithelial-mesenchymal transition: Novel therapeutic targets for cancer. Pathol. Int. 2016;66:601–608. doi: 10.1111/pin.12447. [DOI] [PubMed] [Google Scholar]
- 45.Bates R.C., Pursell B.M., Mercurio A.M. Epithelial-mesenchymal transition and colorectal cancer: Gaining insights into tumor progression using LIM 1863 cells. Cells Tissues Organs. 2007;185:29–39. doi: 10.1159/000101300. [DOI] [PubMed] [Google Scholar]
- 46.Bates R.C. Colorectal cancer progression: Integrin alphavbeta6 and the epithelial-mesenchymal transition (EMT) Cell Cycle (Georget. Tex.) 2005;4:1350–1352. doi: 10.4161/cc.4.10.2053. [DOI] [PubMed] [Google Scholar]
- 47.Yap A.S. The morphogenetic role of cadherin cell adhesion molecules in human cancer: A thematic review. Cancer Investig. 1998;16:252–261. doi: 10.3109/07357909809039774. [DOI] [PubMed] [Google Scholar]
- 48.Thoreson M.A., Reynolds A.B. Altered expression of the catenin p120 in human cancer: Implications for tumor progression. Differ. Res. Biol. Divers. 2002;70:583–589. doi: 10.1046/j.1432-0436.2002.700911.x. [DOI] [PubMed] [Google Scholar]
- 49.Mendez M.G., Kojima S., Goldman R.D. Vimentin induces changes in cell shape, motility, and adhesion during the epithelial to mesenchymal transition. FASEB J. Off. Publ. Fed. Am. Soc. Exp. Biol. 2010;24:1838–1851. doi: 10.1096/fj.09-151639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Skarkova V., Kralova V., Vitovcova B., Rudolf E. Selected Aspects of Chemoresistance Mechanisms in Colorectal Carcinoma-A Focus on Epithelial-to-Mesenchymal Transition, Autophagy, and Apoptosis. Cells. 2019;8:234. doi: 10.3390/cells8030234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ikeguchi M., Taniguchi T., Makino M., Kaibara N. Reduced E-cadherin expression and enlargement of cancer nuclei strongly correlate with hematogenic metastasis in colorectal adenocarcinoma. Scand. J. Gastroenterol. 2000;35:839–846. doi: 10.1080/003655200750023219. [DOI] [PubMed] [Google Scholar]
- 52.Lugli A., Zlobec I., Minoo P., Baker K., Tornillo L., Terracciano L., Jass J.R. Prognostic significance of the wnt signalling pathway molecules APC, beta-catenin and E-cadherin in colorectal cancer: A tissue microarray-based analysis. Histopathology. 2007;50:453–464. doi: 10.1111/j.1365-2559.2007.02620.x. [DOI] [PubMed] [Google Scholar]
- 53.Roca F., Mauro L.V., Morandi A., Bonadeo F., Vaccaro C., Quintana G.O., Specterman S., de Kier Joffe E.B., Pallotta M.G., Puricelli L.I., et al. Prognostic value of E-cadherin, beta-catenin, MMPs (7 and 9), and TIMPs (1 and 2) in patients with colorectal carcinoma. J. Surg. Oncol. 2006;93:151–160. doi: 10.1002/jso.20413. [DOI] [PubMed] [Google Scholar]
- 54.Ye Z., Zhou M., Tian B., Wu B., Li J. Expression of lncRNA-CCAT1, E-cadherin and N-cadherin in colorectal cancer and its clinical significance. Int. J. Clin. Exp. Med. 2015;8:3707–3715. [PMC free article] [PubMed] [Google Scholar]
- 55.Shan Z.Z., Yan X.B., Yan L.L., Tian Y., Meng Q.C., Qiu W.W., Zhang Z., Jin Z.M. Overexpression of Tbx3 is correlated with Epithelial-Mesenchymal Transition phenotype and predicts poor prognosis of colorectal cancer. Am. J. Cancer Res. 2015;5:344–353. [PMC free article] [PubMed] [Google Scholar]
- 56.Ying L., Chen Q., Wang Y., Zhou Z., Huang Y., Qiu F. Upregulated MALAT-1 contributes to bladder cancer cell migration by inducing epithelial-to-mesenchymal transition. Mol. BioSyst. 2012;8:2289–2294. doi: 10.1039/c2mb25070e. [DOI] [PubMed] [Google Scholar]
- 57.Bhan A., Mandal S.S. LncRNA HOTAIR: A master regulator of chromatin dynamics and cancer. Biochim. Biophys. Acta. 2015;1856:151–164. doi: 10.1016/j.bbcan.2015.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Liang W.C., Fu W.M., Wong C.W., Wang Y., Wang W.M., Hu G.X., Zhang L., Xiao L.J., Wan D.C., Zhang J.F., et al. The lncRNA H19 promotes epithelial to mesenchymal transition by functioning as miRNA sponges in colorectal cancer. Oncotarget. 2015;6:22513–22525. doi: 10.18632/oncotarget.4154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhang Q., Li X., Li X., Li X., Chen Z. LncRNA H19 promotes epithelial-mesenchymal transition (EMT) by targeting miR-484 in human lung cancer cells. J. Cell. Biochem. 2018;119:4447–4457. doi: 10.1002/jcb.26537. [DOI] [PubMed] [Google Scholar]
- 60.Zhou W., Ye X.L., Xu J., Cao M.G., Fang Z.Y., Li L.Y., Guan G.H., Liu Q., Qian Y.H., Xie D. The lncRNA H19 mediates breast cancer cell plasticity during EMT and MET plasticity by differentially sponging miR-200b/c and let-7b. Sci. Signal. 2017;10 doi: 10.1126/scisignal.aak9557. [DOI] [PubMed] [Google Scholar]
- 61.Ma C., Nong K., Zhu H., Wang W., Huang X., Yuan Z., Ai K. H19 promotes pancreatic cancer metastasis by derepressing let-7’s suppression on its target HMGA2-mediated EMT. Tumour Biol. J. Int. Soc. Oncodev. Biol. Med. 2014;35:9163–9169. doi: 10.1007/s13277-014-2185-5. [DOI] [PubMed] [Google Scholar]
- 62.Xu J., Lamouille S., Derynck R. TGF-beta-induced epithelial to mesenchymal transition. Cell Res. 2009;19:156–172. doi: 10.1038/cr.2009.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Park S.M., Gaur A.B., Lengyel E., Peter M.E. The miR-200 family determines the epithelial phenotype of cancer cells by targeting the E-cadherin repressors ZEB1 and ZEB2. Genes Dev. 2008;22:894–907. doi: 10.1101/gad.1640608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gregory P.A., Bert A.G., Paterson E.L., Barry S.C., Tsykin A., Farshid G., Vadas M.A., Khew-Goodall Y., Goodall G.J. The miR-200 family and miR-205 regulate epithelial to mesenchymal transition by targeting ZEB1 and SIP1. Nat. Cell Biol. 2008;10:593–601. doi: 10.1038/ncb1722. [DOI] [PubMed] [Google Scholar]
- 65.Liu X., Wang C., Chen Z., Jin Y., Wang Y., Kolokythas A., Dai Y., Zhou X. MicroRNA-138 suppresses epithelial-mesenchymal transition in squamous cell carcinoma cell lines. Biochem. J. 2011;440:23–31. doi: 10.1042/BJ20111006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Long L., Huang G., Zhu H., Guo Y., Liu Y., Huo J. Down-regulation of miR-138 promotes colorectal cancer metastasis via directly targeting TWIST2. J. Transl. Med. 2013;11:275. doi: 10.1186/1479-5876-11-275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zhang J., Liu D., Feng Z., Mao J., Zhang C., Lu Y., Li J., Zhang Q., Li Q., Li L. MicroRNA-138 modulates metastasis and EMT in breast cancer cells by targeting vimentin. Biomed. Pharmacother. 2016;77:135–141. doi: 10.1016/j.biopha.2015.12.018. [DOI] [PubMed] [Google Scholar]
- 68.Jin D., Fang Y., Li Z., Chen Z., Xiang J. Epithelial-mesenchymal transitionassociated microRNAs in colorectal cancer and drug-targeted therapies (Review) Oncol. Rep. 2015;33:515–525. doi: 10.3892/or.2014.3638. [DOI] [PubMed] [Google Scholar]
- 69.Yang Q., Wang X., Tang C., Chen X., He J. H19 promotes the migration and invasion of colon cancer by sponging miR-138 to upregulate the expression of HMGA1. Int. J. Oncol. 2017;50:1801–1809. doi: 10.3892/ijo.2017.3941. [DOI] [PubMed] [Google Scholar]
- 70.Fu F., Wang T., Wu Z., Feng Y., Wang W., Zhou S., Ma X., Wang S. HMGA1 exacerbates tumor growth through regulating the cell cycle and accelerates migration/invasion via targeting miR-221/222 in cervical cancer. Cell Death Dis. 2018;9:594. doi: 10.1038/s41419-018-0683-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ding D., Li C., Zhao T., Li D., Yang L., Zhang B. LncRNA H19/miR-29b-3p/PGRN Axis Promoted Epithelial-Mesenchymal Transition of Colorectal Cancer Cells by Acting on Wnt Signaling. Mol. Cells. 2018;41:423–435. doi: 10.14348/molcells.2018.2258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Chen L., Li Q., Wang J., Jin S., Zheng H., Lin J., He F., Zhang H., Ma S., Mei J., et al. MiR-29b-3p promotes chondrocyte apoptosis and facilitates the occurrence and development of osteoarthritis by targeting PGRN. J. Cell. Mol. Med. 2017;21:3347–3359. doi: 10.1111/jcmm.13237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Dong T., Yang D., Li R., Zhang L., Zhao H., Shen Y., Zhang X., Kong B., Wang L. PGRN promotes migration and invasion of epithelial ovarian cancer cells through an epithelial mesenchymal transition program and the activation of cancer associated fibroblasts. Exp. Mol. Pathol. 2016;100:17–25. doi: 10.1016/j.yexmp.2015.11.021. [DOI] [PubMed] [Google Scholar]
- 74.Chen M., Zhuang C., Liu Y., Li J., Dai F., Xia M., Zhan Y., Lin J., Chen Z., He A., et al. Tetracycline-inducible shRNA targeting antisense long non-coding RNA HIF1A-AS2 represses the malignant phenotypes of bladder cancer. Cancer Lett. 2016;376:155–164. doi: 10.1016/j.canlet.2016.03.037. [DOI] [PubMed] [Google Scholar]
- 75.Li L., Wang M., Mei Z., Cao W., Yang Y., Wang Y., Wen A. lncRNAs HIF1A-AS2 facilitates the up-regulation of HIF-1alpha by sponging to miR-153-3p, whereby promoting angiogenesis in HUVECs in hypoxia. Biomed. Pharmacother. 2017;96:165–172. doi: 10.1016/j.biopha.2017.09.113. [DOI] [PubMed] [Google Scholar]
- 76.Mineo M., Ricklefs F., Rooj A.K., Lyons S.M., Ivanov P., Ansari K.I., Nakano I., Chiocca E.A., Godlewski J., Bronisz A. The Long Non-coding RNA HIF1A-AS2 Facilitates the Maintenance of Mesenchymal Glioblastoma Stem-like Cells in Hypoxic Niches. Cell Rep. 2016;15:2500–2509. doi: 10.1016/j.celrep.2016.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Lin J., Shi Z., Yu Z., He Z. LncRNA HIF1A-AS2 positively affects the progression and EMT formation of colorectal cancer through regulating miR-129-5p and DNMT3A. Biomed. Pharmacother. 2018;98:433–439. doi: 10.1016/j.biopha.2017.12.058. [DOI] [PubMed] [Google Scholar]
- 78.Zhang W., Xu J. DNA methyltransferases and their roles in tumorigenesis. Biomark. Res. 2017;5:1. doi: 10.1186/s40364-017-0081-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ibrahim A.E., Arends M.J., Silva A.L., Wyllie A.H., Greger L., Ito Y., Vowler S.L., Huang T.H., Tavare S., Murrell A., et al. Sequential DNA methylation changes are associated with DNMT3B overexpression in colorectal neoplastic progression. Gut. 2011;60:499–508. doi: 10.1136/gut.2010.223602. [DOI] [PubMed] [Google Scholar]
- 80.Gao Q., Steine E.J., Barrasa M.I., Hockemeyer D., Pawlak M., Fu D., Reddy S., Bell G.W., Jaenisch R. Deletion of the de novo DNA methyltransferase Dnmt3a promotes lung tumor progression. Proc. Natl. Acad. Sci. USA. 2011;108:18061–18066. doi: 10.1073/pnas.1114946108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Zhao Z., Wu Q., Cheng J., Qiu X., Zhang J., Fan H. Depletion of DNMT3A suppressed cell proliferation and restored PTEN in hepatocellular carcinoma cell. J. Biomed. Biotechnol. 2010;2010:737535. doi: 10.1155/2010/737535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Pathania R., Ramachandran S., Elangovan S., Padia R., Yang P., Cinghu S., Veeranan-Karmegam R., Arjunan P., Gnana-Prakasam J.P., Sadanand F., et al. DNMT1 is essential for mammary and cancer stem cell maintenance and tumorigenesis. Nat. Commun. 2015;6:6910. doi: 10.1038/ncomms7910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Chen D.L., Lu Y.X., Zhang J.X., Wei X.L., Wang F., Zeng Z.L., Pan Z.Z., Yuan Y.F., Wang F.H., Pelicano H., et al. Long non-coding RNA UICLM promotes colorectal cancer liver metastasis by acting as a ceRNA for microRNA-215 to regulate ZEB2 expression. Theranostics. 2017;7:4836–4849. doi: 10.7150/thno.20942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bernstein C.N., Blanchard J.F., Kliewer E., Wajda A. Cancer risk in patients with inflammatory bowel disease: A population-based study. Cancer. 2001;91:854–862. doi: 10.1002/1097-0142(20010215)91:4<854::AID-CNCR1073>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 85.Zacharopoulou E., Gazouli M., Tzouvala M., Vezakis A., Karamanolis G. The contribution of long non-coding RNAs in Inflammatory Bowel Diseases. Dig. Liver Dis. 2017;49:1067–1072. doi: 10.1016/j.dld.2017.08.003. [DOI] [PubMed] [Google Scholar]
- 86.Wu Y., Yao J., Xie J., Liu Z., Zhou Y., Pan H., Han W. The role of autophagy in colitis-associated colorectal cancer. Sign. Transduct. Targ. Ther. 2018;3:31. doi: 10.1038/s41392-018-0031-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Yarani R., Mirza A.H., Kaur S., Pociot F. The emerging role of lncRNAs in inflammatory bowel disease. Exp. Mol. Med. 2018;50:161. doi: 10.1038/s12276-018-0188-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Qiao Y.Q., Huang M.L., Xu A.T., Zhao D., Ran Z.H., Shen J. LncRNA DQ786243 affects Treg related CREB and Foxp3 expression in Crohn’s disease. J. Biomed. Sci. 2013;20:87. doi: 10.1186/1423-0127-20-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Zhou X., Han X., Wittfeldt A., Sun J., Liu C., Wang X., Gan L.M., Cao H., Liang Z. Long non-coding RNA ANRIL regulates inflammatory responses as a novel component of NF-kappaB pathway. RNA Biol. 2016;13:98–108. doi: 10.1080/15476286.2015.1122164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Wu F., Huang Y., Dong F., Kwon J.H. Ulcerative Colitis-Associated Long Noncoding RNA, BC012900, Regulates Intestinal Epithelial Cell Apoptosis. Inflamm. Bowel Dis. 2016;22:782–795. doi: 10.1097/MIB.0000000000000691. [DOI] [PubMed] [Google Scholar]
- 91.Yang L., Wang H., Shen Q., Feng L., Jin H. Long non-coding RNAs involved in autophagy regulation. Cell Death Dis. 2017;8:e3073. doi: 10.1038/cddis.2017.464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Bermudez M., Aguilar-Medina M., Lizarraga-Verdugo E., Avendano-Felix M., Silva-Benitez E., Lopez-Camarillo C., Ramos-Payan R. LncRNAs as Regulators of Autophagy and Drug Resistance in Colorectal Cancer. Front. Oncol. 2019;9:1008. doi: 10.3389/fonc.2019.01008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Qian M., Fang X., Wang X. Autophagy and inflammation. Clin. Transl. Med. 2017;6:24. doi: 10.1186/s40169-017-0154-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Li Y., Li C., Li D., Yang L., Jin J., Zhang B. lncRNA KCNQ1OT1 enhances the chemoresistance of oxaliplatin in colon cancer by targeting the miR-34a/ATG4B pathway. OncoTarg. Ther. 2019;12:2649–2660. doi: 10.2147/OTT.S188054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Shan T.D., Xu J.H., Yu T., Li J.Y., Zhao L.N., Ouyang H., Luo S., Lu X.J., Huang C.Z., Lan Q.S., et al. Knockdown of linc-POU3F3 suppresses the proliferation, apoptosis, and migration resistance of colorectal cancer. Oncotarget. 2016;7:961–975. doi: 10.18632/oncotarget.5830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Zheng Y., Tan K., Huang H. Long noncoding RNA HAGLROS regulates apoptosis and autophagy in colorectal cancer cells via sponging miR-100 to target ATG5 expression. J. Cell. Biochem. 2019;120:3922–3933. doi: 10.1002/jcb.27676. [DOI] [PubMed] [Google Scholar]
- 97.Yu Z., Li N., Jiang K., Zhang N., Yao L.L. MiR-100 up-regulation enhanced cell autophagy and apoptosis induced by cisplatin in osteosarcoma by targeting mTOR. Eur. Rev. Med. Pharmacol. Sci. 2018;22:5867–5873. doi: 10.26355/eurrev_201809_15913. [DOI] [PubMed] [Google Scholar]
- 98.Ge Y.Y., Shi Q., Zheng Z.Y., Gong J., Zeng C., Yang J., Zhuang S.M. MicroRNA-100 promotes the autophagy of hepatocellular carcinoma cells by inhibiting the expression of mTOR and IGF-1R. Oncotarget. 2014;5:6218–6228. doi: 10.18632/oncotarget.2189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Liu C., Ji L., Song X. Long non coding RNA UCA1 contributes to the autophagy and survival of colorectal cancer cells via sponging miR-185-5p to up-regulate the WISP2/β-catenin pathway. RSC Adv. 2019;9:14160–14166. doi: 10.1039/C8RA10468A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Tian W., Du Y., Ma Y., Gu L., Zhou J., Deng D. MALAT1-miR663a negative feedback loop in colon cancer cell functions through direct miRNA-lncRNA binding. Cell Death Dis. 2018;9:857. doi: 10.1038/s41419-018-0925-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Yang H., Liang N., Wang M., Fei Y., Sun J., Li Z., Xu Y., Guo C., Cao Z., Li S., et al. Long noncoding RNA MALAT-1 is a novel inflammatory regulator in human systemic lupus erythematosus. Oncotarget. 2017;8:77400–77406. doi: 10.18632/oncotarget.20490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Michaille J.J., Piurowski V., Rigot B., Kelani H., Fortman E.C., Tili E. MiR-663, a MicroRNA Linked with Inflammation and Cancer That Is under the Influence of Resveratrol. Medicines. 2018;5:74. doi: 10.3390/medicines5030074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Zheng H.C. The molecular mechanisms of chemoresistance in cancers. Oncotarget. 2017;8:59950–59964. doi: 10.18632/oncotarget.19048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Li P., Zhang X., Wang H., Wang L., Liu T., Du L., Yang Y., Wang C. MALAT1 Is Associated with Poor Response to Oxaliplatin-Based Chemotherapy in Colorectal Cancer Patients and Promotes Chemoresistance through EZH2. Mol. Cancer Ther. 2017;16:739–751. doi: 10.1158/1535-7163.MCT-16-0591. [DOI] [PubMed] [Google Scholar]
- 105.Li J., Liu H., Yu J., Yu H. Chemoresistance to doxorubicin induces epithelial-mesenchymal transition via upregulation of transforming growth factor beta signaling in HCT116 colon cancer cells. Mol. Med. Rep. 2015;12:192–198. doi: 10.3892/mmr.2015.3356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Zhu J., Zhang R., Yang D., Li J., Yan X., Jin K., Li W., Liu X., Zhao J., Shang W., et al. Knockdown of Long Non-Coding RNA XIST Inhibited Doxorubicin Resistance in Colorectal Cancer by Upregulation of miR-124 and Downregulation of SGK1. Cell. Physiol. Biochem. Int. J. Exp. Cell. Physiol. Biochem. Pharmacol. 2018;51:113–128. doi: 10.1159/000495168. [DOI] [PubMed] [Google Scholar]
- 107.Talarico C., Dattilo V., D’Antona L., Menniti M., Bianco C., Ortuso F., Alcaro S., Schenone S., Perrotti N., Amato R. SGK1, the New Player in the Game of Resistance: Chemo-Radio Molecular Target and Strategy for Inhibition. Cell. Physiol. Biochem. Int. J. Exp. Cell. Physiol. Biochem. Pharmacol. 2016;39:1863–1876. doi: 10.1159/000447885. [DOI] [PubMed] [Google Scholar]
- 108.Amato R., Menniti M., Agosti V., Boito R., Costa N., Bond H.M., Barbieri V., Tagliaferri P., Venuta S., Perrotti N. IL-2 signals through Sgk1 and inhibits proliferation and apoptosis in kidney cancer cells. J. Mol. Med. 2007;85:707–721. doi: 10.1007/s00109-007-0205-2. [DOI] [PubMed] [Google Scholar]
- 109.Zhang R., Wang Z., Yu Q., Shen J., He W., Zhou D., Yu Q., Fan J., Gao S., Duan L. Atractylenolide II reverses the influence of lncRNA XIST/miR-30a-5p/ROR1 axis on chemo-resistance of colorectal cancer cells. J. Cell. Mol. Med. 2019;23:3151–3165. doi: 10.1111/jcmm.14148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Cui B., Zhang S., Chen L., Yu J., Widhopf G.F., 2nd, Fecteau J.F., Rassenti L.Z., Kipps T.J. Targeting ROR1 inhibits epithelial-mesenchymal transition and metastasis. Cancer Res. 2013;73:3649–3660. doi: 10.1158/0008-5472.CAN-12-3832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Zhou J.K., Zheng Y.Z., Liu X.S., Gou Q., Ma R., Guo C.L., Croce C.M., Liu L., Peng Y. ROR1 expression as a biomarker for predicting prognosis in patients with colorectal cancer. Oncotarget. 2017;8:32864–32872. doi: 10.18632/oncotarget.15860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Shi Y.Y., Guan S.H., Tang R.N., Tao S.J., Guo D.A. Simultaneous determination of atractylenolide II and atractylenolide III by liquid chromatography-tandem mass spectrometry in rat plasma and its application in a pharmacokinetic study after oral administration of Atractylodes Macrocephala Rhizoma extract. Biomed. Chromatogr. BMC. 2012;26:1386–1392. doi: 10.1002/bmc.2709. [DOI] [PubMed] [Google Scholar]
- 113.Longley D.B., Harkin D.P., Johnston P.G. 5-fluorouracil: Mechanisms of action and clinical strategies. Nat. Rev. Cancer. 2003;3:330–338. doi: 10.1038/nrc1074. [DOI] [PubMed] [Google Scholar]
- 114.Wang M., Hu H., Wang Y., Huang Q., Huang R., Chen Y., Ma T., Qiao T., Zhang Q., Wu H., et al. Long non-coding RNA TUG1 mediates 5-fluorouracil resistance by acting as a ceRNA of miR-197-3p in colorectal cancer. J. Cancer. 2019;10:4603–4613. doi: 10.7150/jca.32065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Hertz R., Li M.C., Spencer D.B. Effect of methotrexate therapy upon choriocarcinoma and chorioadenoma. Proc. Soc. Exp. Biol. Med. 1956;93:361–366. doi: 10.3181/00379727-93-22757. [DOI] [PubMed] [Google Scholar]
- 116.Bertino J.R., Goker E., Gorlick R., Li W.W., Banerjee D. Resistance Mechanisms to Methotrexate in Tumors. Oncologist. 1996;1:223–226. doi: 10.1002/stem.140005. [DOI] [PubMed] [Google Scholar]
- 117.Li C., Gao Y., Li Y., Ding D. TUG1 mediates methotrexate resistance in colorectal cancer via miR-186/CPEB2 axis. Biochem. Biophys. Res. Commun. 2017;491:552–557. doi: 10.1016/j.bbrc.2017.03.042. [DOI] [PubMed] [Google Scholar]
- 118.Martinez-Balibrea E., Martinez-Cardus A., Gines A., Ruiz de Porras V., Moutinho C., Layos L., Manzano J.L., Buges C., Bystrup S., Esteller M., et al. Tumor-Related Molecular Mechanisms of Oxaliplatin Resistance. Mol. Cancer ther. 2015;14:1767–1776. doi: 10.1158/1535-7163.MCT-14-0636. [DOI] [PubMed] [Google Scholar]
- 119.Li L., Shang J., Zhang Y., Liu S., Peng Y., Zhou Z., Pan H., Wang X., Chen L., Zhao Q. MEG3 is a prognostic factor for CRC and promotes chemosensitivity by enhancing oxaliplatin-induced cell apoptosis. Oncol. Rep. 2017;38:1383–1392. doi: 10.3892/or.2017.5828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Wang H., Li H., Zhang L., Yang D. Overexpression of MEG3 sensitizes colorectal cancer cells to oxaliplatin through regulation of miR-141/PDCD4 axis. Biomed. Pharmacother. 2018;106:1607–1615. doi: 10.1016/j.biopha.2018.07.131. [DOI] [PubMed] [Google Scholar]
- 121.Afonja O., Juste D., Das S., Matsuhashi S., Samuels H.H. Induction of PDCD4 tumor suppressor gene expression by RAR agonists, antiestrogen and HER-2/neu antagonist in breast cancer cells. Evidence for a role in apoptosis. Oncogene. 2004;23:8135–8145. doi: 10.1038/sj.onc.1207983. [DOI] [PubMed] [Google Scholar]
- 122.Shi G.H., Ye D.W., Yao X.D., Zhang S.L., Dai B., Zhang H.L., Shen Y.J., Zhu Y., Zhu Y.P., Xiao W.J., et al. Involvement of microRNA-21 in mediating chemo-resistance to docetaxel in androgen-independent prostate cancer PC3 cells. Acta Pharmacol. Sin. 2010;31:867–873. doi: 10.1038/aps.2010.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Shiota M., Izumi H., Tanimoto A., Takahashi M., Miyamoto N., Kashiwagi E., Kidani A., Hirano G., Masubuchi D., Fukunaka Y., et al. Programmed cell death protein 4 down-regulates Y-box binding protein-1 expression via a direct interaction with Twist1 to suppress cancer cell growth. Cancer Res. 2009;69:3148–3156. doi: 10.1158/0008-5472.CAN-08-2334. [DOI] [PubMed] [Google Scholar]
- 124.Ni B., Yu X., Guo X., Fan X., Yang Z., Wu P., Yuan Z., Deng Y., Wang J., Chen D., et al. Increased urothelial cancer associated 1 is associated with tumor proliferation and metastasis and predicts poor prognosis in colorectal cancer. Int. J. Oncol. 2015;47:1329–1338. doi: 10.3892/ijo.2015.3109. [DOI] [PubMed] [Google Scholar]
- 125.Fan Y., Shen B., Tan M., Mu X., Qin Y., Zhang F., Liu Y. Long non-coding RNA UCA1 increases chemoresistance of bladder cancer cells by regulating Wnt signaling. FEBS J. 2014;281:1750–1758. doi: 10.1111/febs.12737. [DOI] [PubMed] [Google Scholar]
- 126.Yin Y., Zhang B., Wang W., Fei B., Quan C., Zhang J., Song M., Bian Z., Wang Q., Ni S., et al. miR-204-5p inhibits proliferation and invasion and enhances chemotherapeutic sensitivity of colorectal cancer cells by downregulating RAB22A. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2014;20:6187–6199. doi: 10.1158/1078-0432.CCR-14-1030. [DOI] [PubMed] [Google Scholar]
- 127.Liu P., He W., Lu Y., Wang Y. Long non-coding RNA LINC00152 promotes tumorigenesis via sponging miR-193b-3p in osteosarcoma. Oncol. Lett. 2019;18:3630–3636. doi: 10.3892/ol.2019.10700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Zhang X., Tao W. Long Noncoding RNA LINC00152 Facilitates the Leukemogenesis of Acute Myeloid Leukemia by Promoting CDK9 Through miR-193a. DNA Cell Biol. 2019;38:236–242. doi: 10.1089/dna.2018.4482. [DOI] [PubMed] [Google Scholar]
- 129.Yue B., Cai D., Liu C., Fang C., Yan D. Linc00152 Functions as a Competing Endogenous RNA to Confer Oxaliplatin Resistance and Holds Prognostic Values in Colon Cancer. Mol. Ther. J. Am. Soc. Gene Ther. 2016;24:2064–2077. doi: 10.1038/mt.2016.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Mamoori A., Wahab R., Islam F., Lee K., Vider J., Lu C.T., Gopalan V., Lam A.K. Clinical and biological significance of miR-193a-3p targeted KRAS in colorectal cancer pathogenesis. Hum. Pathol. 2018;71:145–156. doi: 10.1016/j.humpath.2017.10.024. [DOI] [PubMed] [Google Scholar]
- 131.Williams C.S., Bernard J.K., Demory Beckler M., Almohazey D., Washington M.K., Smith J.J., Frey M.R. ERBB4 is over-expressed in human colon cancer and enhances cellular transformation. Carcinogenesis. 2015;36:710–718. doi: 10.1093/carcin/bgv049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Bian Z., Zhang J., Li M., Feng Y., Yao S., Song M., Qi X., Fei B., Yin Y., Hua D., et al. Long non-coding RNA LINC00152 promotes cell proliferation, metastasis, and confers 5-FU resistance in colorectal cancer by inhibiting miR-139-5p. Oncogenesis. 2017;6:395. doi: 10.1038/s41389-017-0008-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Wang X., Lan Z., He J., Lai Q., Yao X., Li Q., Liu Y., Lai H., Gu C., Yan Q., et al. LncRNA SNHG6 promotes chemoresistance through ULK1-induced autophagy by sponging miR-26a-5p in colorectal cancer cells. Cancer Cell Int. 2019;19:234. doi: 10.1186/s12935-019-0951-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Antonioli M., Di Rienzo M., Piacentini M., Fimia G.M. Emerging Mechanisms in Initiating and Terminating Autophagy. Trends Biochem. Sci. 2017;42:28–41. doi: 10.1016/j.tibs.2016.09.008. [DOI] [PubMed] [Google Scholar]
- 135.Levy J.M.M., Towers C.G., Thorburn A. Targeting autophagy in cancer. Nat. Rev. Cancer. 2017;17:528–542. doi: 10.1038/nrc.2017.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Hurley J.H., Young L.N. Mechanisms of Autophagy Initiation. Annu. Rev. Biochem. 2017;86:225–244. doi: 10.1146/annurev-biochem-061516-044820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Yu T., Guo F., Yu Y., Sun T., Ma D., Han J., Qian Y., Kryczek I., Sun D., Nagarsheth N., et al. Fusobacterium nucleatum Promotes Chemoresistance to Colorectal Cancer by Modulating Autophagy. Cell. 2017;170:548–563.e516. doi: 10.1016/j.cell.2017.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Wang M., Han D., Yuan Z., Hu H., Zhao Z., Yang R., Jin Y., Zou C., Chen Y., Wang G., et al. Long non-coding RNA H19 confers 5-Fu resistance in colorectal cancer by promoting SIRT1-mediated autophagy. Cell Death Dis. 2018;9:1149. doi: 10.1038/s41419-018-1187-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Gao R., Fang C., Xu J., Tan H., Li P., Ma L. LncRNA CACS15 contributes to oxaliplatin resistance in colorectal cancer by positively regulating ABCC1 through sponging miR-145. Arch. Biochem. Biophys. 2019;663:183–191. doi: 10.1016/j.abb.2019.01.005. [DOI] [PubMed] [Google Scholar]
- 140.Ji D., Zhan T., Li M., Yao Y., Jia J., Yi H., Qiao M., Xia J., Zhang Z., Ding H., et al. Enhancement of Sensitivity to Chemo/Radiation Therapy by Using miR-15b against DCLK1 in Colorectal Cancer. Stem Cell Rep. 2018;11:1506–1522. doi: 10.1016/j.stemcr.2018.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Kang Z., Jifu E., Guo K., Ma X., Zhang Y., Yu E. Knockdown of long non-coding RNA TINCR decreases radioresistance in colorectal cancer cells. Pathol. Res. Pract. 2019:152622. doi: 10.1016/j.prp.2019.152622. [DOI] [PubMed] [Google Scholar]
- 142.Ben-Porath I., Thomson M.W., Carey V.J., Ge R., Bell G.W., Regev A., Weinberg R.A. An embryonic stem cell-like gene expression signature in poorly differentiated aggressive human tumors. Nat. Genet. 2008;40:499–507. doi: 10.1038/ng.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Li J.H., Liu S., Zhou H., Qu L.H., Yang J.H. starBase v2.0: Decoding miRNA-ceRNA, miRNA-ncRNA and protein-RNA interaction networks from large-scale CLIP-Seq data. Nucl. Acids Res. 2014;42:D92–D97. doi: 10.1093/nar/gkt1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Paraskevopoulou M.D., Georgakilas G., Kostoulas N., Reczko M., Maragkakis M., Dalamagas T.M., Hatzigeorgiou A.G. DIANA-LncBase: Experimentally verified and computationally predicted microRNA targets on long non-coding RNAs. Nucl. Acids Res. 2013;41:D239–D245. doi: 10.1093/nar/gks1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Furio-Tari P., Tarazona S., Gabaldon T., Enright A.J., Conesa A. spongeScan: A web for detecting microRNA binding elements in lncRNA sequences. Nucl. Acids Res. 2016;44:W176–W180. doi: 10.1093/nar/gkw443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Das S., Ghosal S., Sen R., Chakrabarti J. lnCeDB: Database of human long noncoding RNA acting as competing endogenous RNA. PLoS ONE. 2014;9:e98965. doi: 10.1371/journal.pone.0098965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Xu C., Ping Y., Zhao H., Ning S., Xia P., Wang W., Wan L., Li J., Zhang L., Yu L., et al. LncNetP, a systematical lncRNA prioritization approach based on ceRNA and disease phenotype association assumptions. Oncotarget. 2017;8:114603–114612. doi: 10.18632/oncotarget.23059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Bhattacharya A., Cui Y. SomamiR 2.0: A database of cancer somatic mutations altering microRNA-ceRNA interactions. Nucl. Acids Res. 2016;44:D1005–D1010. doi: 10.1093/nar/gkv1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Wang P., Zhi H., Zhang Y., Liu Y., Zhang J., Gao Y., Guo M., Ning S., Li X. miRSponge: A manually curated database for experimentally supported miRNA sponges and ceRNAs. Database J. Biol. Databases Curation. 2015;2015 doi: 10.1093/database/bav098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Yuan C., Meng X., Li X., Illing N., Ingle R.A., Wang J., Chen M. PceRBase: A database of plant competing endogenous RNA. Nucl. Acids Res. 2017;45:D1009–D1014. doi: 10.1093/nar/gkw916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Liu K., Yan Z., Li Y., Sun Z. Linc2GO: A human LincRNA function annotation resource based on ceRNA hypothesis. Bioinformatics. 2013;29:2221–2222. doi: 10.1093/bioinformatics/btt361. [DOI] [PubMed] [Google Scholar]
- 152.Ouyang S., Zhou X., Chen Z., Wang M., Zheng X., Xie M. LncRNA BCAR4, targeting to miR-665/STAT3 signaling, maintains cancer stem cells stemness and promotes tumorigenicity in colorectal cancer. Cancer Cell Int. 2019;19:72. doi: 10.1186/s12935-019-0784-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Jing N., Huang T., Guo H., Yang J., Li M., Chen Z., Zhang Y. LncRNA CASC15 promotes colon cancer cell proliferation and metastasis by regulating the miR4310/LGR5/Wnt/betacatenin signaling pathway. Mol. Med. Rep. 2018;18:2269–2276. doi: 10.3892/mmr.2018.9191. [DOI] [PubMed] [Google Scholar]
- 154.Huang G., Wu X., Li S., Xu X., Zhu H., Chen X. The long noncoding RNA CASC2 functions as a competing endogenous RNA by sponging miR-18a in colorectal cancer. Sci. Rep. 2016;6:26524. doi: 10.1038/srep26524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Yu Y., Nangia-Makker P., Farhana L., Majumdar A.P.N. A novel mechanism of lncRNA and miRNA interaction: CCAT2 regulates miR-145 expression by suppressing its maturation process in colon cancer cells. Mol. Cancer. 2017;16:155. doi: 10.1186/s12943-017-0725-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Li M., Wang Q., Xue F., Wu Y. lncRNA-CYTOR Works as an Oncogene Through the CYTOR/miR-3679-5p/MACC1 Axis in Colorectal Cancer. DNA Cell Biol. 2019;38:572–582. doi: 10.1089/dna.2018.4548. [DOI] [PubMed] [Google Scholar]
- 157.Zhou J., Zou Y., Hu G., Lin C., Guo Y., Gao K., Wu M. Facilitating colorectal cancer cell metastasis by targeted binding of long non-coding RNA ENSG00000231881 with miR-133b via VEGFC signaling pathway. Biochem. Biophys. Res. Commun. 2019;509:1–7. doi: 10.1016/j.bbrc.2018.08.004. [DOI] [PubMed] [Google Scholar]
- 158.Yue B., Sun B., Liu C., Zhao S., Zhang D., Yu F., Yan D. Long non-coding RNA Fer-1-like protein 4 suppresses oncogenesis and exhibits prognostic value by associating with miR-106a-5p in colon cancer. Cancer Sci. 2015;106:1323–1332. doi: 10.1111/cas.12759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Zhu Y., Qiao L., Zhou Y., Ma N., Wang C., Zhou J. Long non-coding RNA FOXD2-AS1 contributes to colorectal cancer proliferation through its interaction with microRNA-185-5p. Cancer Sci. 2018;109:2235–2242. doi: 10.1111/cas.13632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Wu Q., Shi M., Meng W., Wang Y., Hui P., Ma J. Long noncoding RNA FOXD3-AS1 promotes colon adenocarcinoma progression and functions as a competing endogenous RNA to regulate SIRT1 by sponging miR-135a-5p. J. Cell. Physiol. 2019;234:21889–21902. doi: 10.1002/jcp.28752. [DOI] [PubMed] [Google Scholar]
- 161.Zhou W., Wang L., Miao Y., Xing R. Novel long noncoding RNA GACAT3 promotes colorectal cancer cell proliferation, invasion, and migration through miR-149. OncoTarg. Ther. 2018;11:1543–1552. doi: 10.2147/OTT.S144103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Liu L., Wang H.J., Meng T., Lei C., Yang X.H., Wang Q.S., Jin B., Zhu J.F. lncRNA GAS5 Inhibits Cell Migration and Invasion and Promotes Autophagy by Targeting miR-222-3p via the GAS5/PTEN-Signaling Pathway in CRC. Mol. Ther. Nucl. Acids. 2019;17:644–656. doi: 10.1016/j.omtn.2019.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 163.Zhou J., Lin J., Zhang H., Zhu F., Xie R. LncRNA HAND2-AS1 sponging miR-1275 suppresses colorectal cancer progression by upregulating KLF14. Biochem. Biophys. Res. Commun. 2018;503:1848–1853. doi: 10.1016/j.bbrc.2018.07.125. [DOI] [PubMed] [Google Scholar]
- 164.Peng C.L., Zhao X.J., Wei C.C., Wu J.W. LncRNA HOTAIR promotes colon cancer development by down-regulating miRNA-34a. Eur. Rev. Med. Pharmacol. Sci. 2019;23:5752–5761. doi: 10.26355/eurrev_201907_18312. [DOI] [PubMed] [Google Scholar]
- 165.Dong Y., Wei M.-H., Lu J.-G., Bi C.-Y. Long non-coding RNA HULC interacts with miR-613 to regulate colon cancer growth and metastasis through targeting RTKN. Biomed. Pharmacother. 2019;109:2035–2042. doi: 10.1016/j.biopha.2018.08.017. [DOI] [PubMed] [Google Scholar]
- 166.Zhang Y., Liu X., Li Q., Zhang Y. lncRNA LINC00460 promoted colorectal cancer cells metastasis via miR-939-5p sponging. Cancer Manag. Res. 2019;11:1779–1789. doi: 10.2147/CMAR.S192452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Yan S., Yue Y., Wang J., Li W., Sun M., Gu C., Zeng L. LINC00668 promotes tumorigenesis and progression through sponging miR-188–5p and regulating USP47 in colorectal cancer. Eur. J. Pharmacol. 2019;858:172464. doi: 10.1016/j.ejphar.2019.172464. [DOI] [PubMed] [Google Scholar]
- 168.Sha Q.K., Chen L., Xi J.Z., Song H. Long non-coding RNA LINC00858 promotes cells proliferation, migration and invasion by acting as a ceRNA of miR-22-3p in colorectal cancer. Artif. Cells Nanomed. Biotechnol. 2019;47:1057–1066. doi: 10.1080/21691401.2018.1544143. [DOI] [PubMed] [Google Scholar]
- 169.Lin C., Zhang Y., Chen Y., Bai Y., Zhang Y. Long noncoding RNA LINC01234 promotes serine hydroxymethyltransferase 2 expression and proliferation by competitively binding miR-642a-5p in colon cancer. Cell Death Dis. 2019;10:137. doi: 10.1038/s41419-019-1352-4. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 170.Wang K., Zhang M., Wang C., Ning X. Long Noncoding RNA LINC01296 Harbors miR-21a to Regulate Colon Carcinoma Proliferation and Invasion. Oncol. Res. 2019;27:541–549. doi: 10.3727/096504018X15234931503876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Zhao Y., Du T., Du L., Li P., Li J., Duan W., Wang Y., Wang C. Long noncoding RNA LINC02418 regulates MELK expression by acting as a ceRNA and may serve as a diagnostic marker for colorectal cancer. Cell Death Dis. 2019;10:568. doi: 10.1038/s41419-019-1804-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Zhu K., Wang Y., Liu L., Li S., Yu W. Long non-coding RNA MBNL1-AS1 regulates proliferation, migration, and invasion of cancer stem cells in colon cancer by interacting with MYL9 via sponging microRNA-412-3p. Clin. Res. Hepatol. Gastroenterol. 2019 doi: 10.1016/j.clinre.2019.05.001. [DOI] [PubMed] [Google Scholar]
- 173.Liu Z., Wang H., Cai H., Hong Y., Li Y., Su D., Fan Z. Long non-coding RNA MIAT promotes growth and metastasis of colorectal cancer cells through regulation of miR-132/Derlin-1 pathway. Cancer Cell Int. 2018;18:59. doi: 10.1186/s12935-017-0477-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Yuan G., Liu B., Han W., Zhao D. LncRNA-MIR17HG mediated upregulation of miR-17 and miR-18a promotes colon cancer progression via activating Wnt/β-catenin signaling. Transl. Cancer Res. 2019;8:1097–1108. doi: 10.21037/tcr.2019.06.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Ye Y., Gu B., Wang Y., Shen S., Huang W. E2F1-mediated MNX1-AS1-miR-218-5p-SEC61A1 feedback loop contributes to the progression of colon adenocarcinoma. J. Cell. Biochem. 2019;120:6145–6153. doi: 10.1002/jcb.27902. [DOI] [PubMed] [Google Scholar]
- 176.Huang F., Wen C., Zhuansun Y., Huang L., Chen W., Yang X., Liu H. A novel long noncoding RNA OECC promotes colorectal cancer development and is negatively regulated by miR-143-3p. Biochem. Biophys. Res. Commun. 2018;503:2949–2955. doi: 10.1016/j.bbrc.2018.08.075. [DOI] [PubMed] [Google Scholar]
- 177.Hu Y., Ma Z., He Y., Liu W., Su Y., Tang Z. PART-1 functions as a competitive endogenous RNA for promoting tumor progression by sponging miR-143 in colorectal cancer. Biochem. Biophys. Res. Commun. 2017;490:317–323. doi: 10.1016/j.bbrc.2017.06.042. [DOI] [PubMed] [Google Scholar]
- 178.Zhou P., Sun L., Liu D., Liu C., Sun L. Long Non-Coding RNA lincRNA-ROR Promotes the Progression of Colon Cancer and Holds Prognostic Value by Associating with miR-145. Pathol. Oncol. Res. POR. 2016;22:733–740. doi: 10.1007/s12253-016-0061-x. [DOI] [PubMed] [Google Scholar]
- 179.Sun X., Bai Y., Yang C., Hu S., Hou Z., Wang G. Long noncoding RNA SNHG15 enhances the development of colorectal carcinoma via functioning as a ceRNA through miR-141/SIRT1/Wnt/beta-catenin axis. Artif. Cells Nanomed. Biotechnol. 2019;47:2536–2544. doi: 10.1080/21691401.2019.1621328. [DOI] [PubMed] [Google Scholar]
- 180.Ke D., Wang Q., Ke S., Zou L., Wang Q. Long-Non Coding RNA SNHG16 Supports Colon Cancer Cell Growth by Modulating miR-302a-3p/AKT Axis. Pathol. Oncol. Res. POR. 2019 doi: 10.1007/s12253-019-00743-9. [DOI] [PubMed] [Google Scholar]
- 181.Jia Z., Peng J., Yang Z., Chen J., Liu L., Luo D., He P. Long non-coding RNA TP73AS1 promotes colorectal cancer proliferation by acting as a ceRNA for miR103 to regulate PTEN expression. Gene. 2019;685:222–229. doi: 10.1016/j.gene.2018.11.072. [DOI] [PubMed] [Google Scholar]
- 182.Cai Y., Yan P., Zhang G., Yang W., Wang H., Cheng X. Long non-coding RNA TP73-AS1 sponges miR-194 to promote colorectal cancer cell proliferation, migration and invasion via up-regulating TGFalpha. Cancer Biomark. Sect. Dis. Mark. 2018;23:145–156. doi: 10.3233/CBM-181503. [DOI] [PubMed] [Google Scholar]
- 183.Sun J., Hu J., Wang G., Yang Z., Zhao C., Zhang X., Wang J. LncRNA TUG1 promoted KIAA1199 expression via miR-600 to accelerate cell metastasis and epithelial-mesenchymal transition in colorectal cancer. J. Exp. Clin. Cancer Res. CR. 2018;37:106. doi: 10.1186/s13046-018-0771-x. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 184.Xu J., Zhang R., Zhao J. The Novel Long Noncoding RNA TUSC7 Inhibits Proliferation by Sponging MiR-211 in Colorectal Cancer. Cell. Physiol. Biochem. Int. J. Exp. Cell. Physiol. Biochem. Pharmacol. 2017;41:635–644. doi: 10.1159/000457938. [DOI] [PubMed] [Google Scholar]
- 185.Huang F.T., Chen W.Y., Gu Z.Q., Zhuang Y.Y., Li C.Q., Wang L.Y., Peng J.F., Zhu Z., Luo X., Li Y.H., et al. The novel long intergenic noncoding RNA UCC promotes colorectal cancer progression by sponging miR-143. Cell Death Dis. 2017;8:e2778. doi: 10.1038/cddis.2017.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Wu X., He X., Li S., Xu X., Chen X., Zhu H. Long Non-Coding RNA ucoo2kmd.1 Regulates CD44-Dependent Cell Growth by Competing for miR-211-3p in Colorectal Cancer. PLoS ONE. 2016;11:e0151287. doi: 10.1371/journal.pone.0151287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Li C., Liu T., Zhang Y., Li Q., Jin L.K. LncRNA-ZDHHC8P1 promotes the progression and metastasis of colorectal cancer by targeting miR-34a. Eur. Rev. Med. Pharmacol. Sci. 2019;23:1476–1486. doi: 10.26355/eurrev_201902_17105. [DOI] [PubMed] [Google Scholar]
- 188.Mo D., Liu W., Li Y., Cui W. Long Non-coding RNA Zinc Finger Antisense 1 (ZFAS1) Regulates Proliferation, Migration, Invasion, and Apoptosis by Targeting MiR-7-5p in Colorectal Cancer. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2019;25:5150–5158. doi: 10.12659/MSM.916619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Thorenoor N., Faltejskova-Vychytilova P., Hombach S., Mlcochova J., Kretz M., Svoboda M., Slaby O. Long non-coding RNA ZFAS1 interacts with CDK1 and is involved in p53-dependent cell cycle control and apoptosis in colorectal cancer. Oncotarget. 2016;7:622–637. doi: 10.18632/oncotarget.5807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Shi L., Hong X., Ba L., He X., Xiong Y., Ding Q., Yang S., Peng G. Long non-coding RNA ZNFX1-AS1 promotes the tumor progression and metastasis of colorectal cancer by acting as a competing endogenous RNA of miR-144 to regulate EZH2 expression. Cell Death Dis. 2019;10:150. doi: 10.1038/s41419-019-1332-8. [DOI] [PMC free article] [PubMed] [Google Scholar]