Clinical practice guidelines advise clinicians on the management of patients based on evidence and evolving knowledge. Questions that are important to patients and clinicians are posed by an expert panel, and a full systematic review of the evidence is performed by methodologists who have neither financial nor intellectual conflicts of interest. The synthesized evidence is discussed by content experts whose potential conflicts of interest are managed, and then recommendations are formulated after considering the balance of benefits versus harms and burdens, quality of evidence, patient values and preferences, cost, and feasibility.
In 2018, the American Thoracic Society (ATS), European Respiratory Society (ERS), Japanese Respiratory Society (JRS), and Latin American Thoracic Society (ALAT) published a clinical practice guideline on the diagnosis of idiopathic pulmonary fibrosis (IPF), updating guidelines from 2011 (1, 2). The new guidelines 1) used systematic reviews to inform each recommendation in strict accordance with the Institute of Medicine Standards for Trustworthy Guidelines (3), 2) eliminated the radiological categories of “possible UIP pattern” and “inconsistent for UIP pattern” and the pathological categories of “possible UIP” and “nonclassifiable fibrosis,” and 3) refined the radiological and pathological patterns of “UIP” and defined “probable UIP” and “indeterminate for UIP.” The overriding goal of the guidelines was to help clinicians diagnose IPF more accurately, thereby facilitating appropriate treatment, as described in the 2015 guidelines for the treatment of IPF (4).
The radiological patterns of usual interstitial pneumonia (UIP) described in the ATS/ERS/JRS/ALAT guidelines are like those described in a statement from the Fleischner Society (5); however, the two documents make seemingly different recommendations about whether to perform surgical lung biopsy (SLB) in patients with the radiological probable UIP pattern by high-resolution computed tomography (HRCT) (6). Specifically, the ATS/ERS/JRS/ALAT guidelines make a conditional recommendation for SLB after multidisciplinary discussions (MDDs), whereas the Fleischner Society statement indicates that a confident diagnosis of IPF can be made without SLB in the right clinical context. This reflects differences in methodology and terminology rather than any substantive difference in principles and recommended practices.
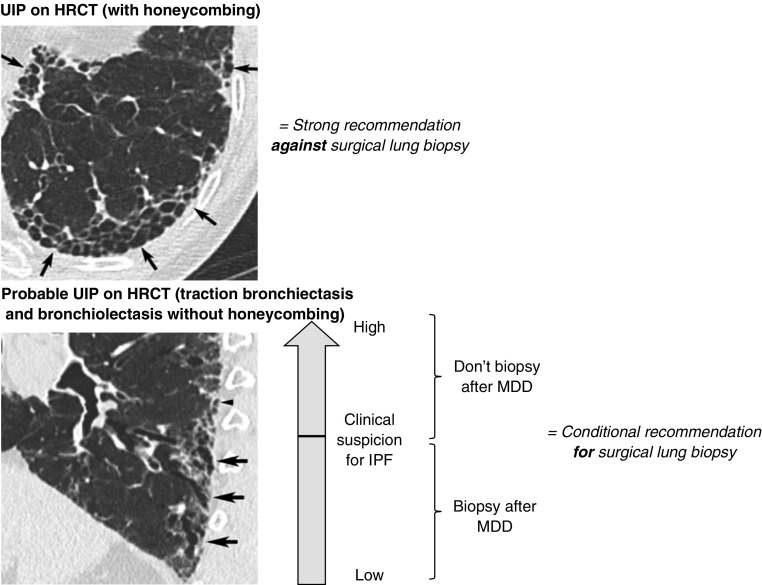
It is apparent that the recommendations in the ATS/ERS/JRS/ALAT guidelines are subject to misinterpretation as a mandate for SLB in patients with probable UIP. Avoiding this misinterpretation is precisely why the ATS/ERS/JRS/ALAT recommendation was assigned a strength of “conditional” (Table 1), a grading option that was not available to the authors of the Fleischner Society statement. A conditional recommendation conveys that the course of action is appropriate for most patients but may not be appropriate for a sizeable minority of patients. The guideline panel anticipated that among patients who meet HRCT criteria for probable UIP, there will be a spectrum of suspicion for IPF ranging from high to low depending on the clinical context. The conditional strength of the recommendation provides clinicians with equipoise to forgo SLB when the clinical context is strongly suggestive of IPF and to perform SLB when the clinical context is uncertain (Figure 1). This is aligned with the Fleischner Society statement that “surgical lung biopsy remains an important method for the diagnosis of IPF in a large subset of patients who cannot be diagnosed on the basis of clinical and imaging features alone.” In other words, the ATS/ERS/JRS/ALAT guidelines and the Fleischner Society statement recommend the same courses of action—patients with a probable UIP pattern on HRCT and a high clinical likelihood of IPF may forgo SLB, and patients with probable UIP for whom the clinical likelihood of IPF is uncertain may undergo SLB. The ATS/ERS/JRS/ALAT proposal suggests that MDDs among experts in interstitial lung diseases may play a pivotal role in navigating this key inflection point.
Table 1.
Strengths of Recommendations
| Strong Recommendation (“We recommend . . .”) | Conditional Recommendation (“We suggest . . .”) | |
|---|---|---|
| From the GRADE Working Group | ||
| For patients | The overwhelming majority of individuals in this situation would want the recommended course of action, and only a small minority would not. | The majority of individuals in this situation would want the suggested course of action, but a sizeable minority would not. |
| For clinicians | The overwhelming majority of individuals should receive the recommended course of action. Adherence to this recommendation according to the guideline could be used as a quality criterion or performance indicator. Formal decision aids are not likely to be needed to help individuals make decisions consistent with their values and preferences. | Different choices will be appropriate for different patients and you must help each patient arrive at a management decision consistent with her or his values and preferences. Decision aids may be useful to help individuals make decisions consistent with their values and preferences. Clinicians should expect to spend more time with patients when working toward a decision. |
| For policy makers | The recommendation can be adapted as policy in most situations, including for use as a performance indicator. | Policy making will require substantial debates and involvement of many stakeholders. Policies are also more likely to vary between regions. Performance indicators would have to focus on the fact that adequate deliberation about the management options has taken place. |
| From the ATS/ERS/JRS/ALAT Diagnosis of Idiopathic Pulmonary Fibrosis Guidelines panel discussion | ||
| It is the right course of action for >95% of patients. | It is the right course of action for >50% of patients but may not be right the right course for a sizeable minority. | |
| “Just do it.” | “Slow down, think about it, discuss it.” | |
| You would be willing to tell a colleague who did not follow the recommendation that he/she did the wrong thing. | You would not be willing to tell a colleague who did not follow the recommendation that he/she did the wrong thing; it is a matter of “style” or “equipoise.” | |
| The recommended course of action may be an appropriate performance measure. | The recommended course of action is not appropriate for a performance measure. |
Definition of abbreviations: ALAT = Latin American Thoracic Society; ATS = American Thoracic Society; ERS = European Respiratory Society; GRADE = Grading of Recommendations, Assessment, and Evaluation; JRS = Japanese Respiratory Society.
Figure 1.
Consideration of surgical lung biopsy to determine histological features in patients with high-resolution computed tomography (HRCT) patterns of usual interstitial pneumonia (UIP) and probable UIP. (Top) UIP magnified view of the left lower lobe (transverse computed tomography section) showing typical characteristics of honeycombing, consisting of clustered cystic airspaces with well-defined walls and variable diameters, seen in single or multiple layers (arrows). (Bottom) Probable UIP magnified sagittal view (reconstructed) of the right lower lobe illustrating the presence of a reticular pattern with subpleural, peripheral, and basal predominance of traction bronchiolectasis that appears as tubular (arrows) or cystic (arrowhead) structures. Images reprinted from Reference 2. IPF = idiopathic pulmonary fibrosis; MDD = multidisciplinary discussion.
The ATS/ERS/JRS/ALAT guideline panel formulated its recommendations by weighing the diagnostic characteristics of SLB (100% adequate samples, 90% diagnostic yield) versus the risks of SLB (1.7% surgical mortality) in patients with newly detected interstitial lung disease, along with patient preferences, cost, and feasibility. The panel voted 17 to 4 to suggest SLB (i.e., make a conditional recommendation for SLB), while acknowledging the very low quality of the evidence. The panel emphasized the need for an MDD to decide whether to proceed to SLB, as well as the conclusion that SLB should not be performed in patients at high risk for intra-, peri-, and/or postoperative complications, such as those with severe hypoxemia at rest and/or severe pulmonary hypertension with DlCO <25% after correction for the hematocrit (7). The panel also stated that SLB may be unnecessary in some familial cases.
The suggestion to perform SLB in patients with probable UIP was supported by a prospective study (8). In that study, IPF experts who were not on the ATS/ERS/JRS/ALAT guideline panel and had no knowledge of the guideline’s systematic reviews or recommendations answered the same questions as the ATS/ERS/JRS/ALAT panel using the modified Convergence of Opinion on Recommendations and Evidence (CORE) approach, an electronic consensus-building process (8). The recommendations developed using the modified CORE process were highly concordant with those developed by the guideline panel, including the suggestion for SLB.
In summary, it is apparent that the ATS/ERS/JRS/ALAT guideline’s recommendation for SLB in patients with probable UIP has been interpreted as a mandate for SLB. This was never the intent. We emphasize that the recommendation was assigned a strength of “conditional” for the primary purpose of avoiding this interpretation, and we reiterate that there is equipoise in deciding which patients with a probable UIP pattern on HRCT warrant an SLB. Specifically, patients with probable UIP for whom the clinical context is suggestive of IPF may forgo SLB, whereas patients with probable UIP for whom the clinical context is uncertain may undergo SLB. The clinician and patient need to discuss SLB within the individual clinical context, including potential desirable and undesirable consequences, and then make the decision to either pursue or forgo SLB.
Supplementary Material
Footnotes
Originally Published in Press as DOI: 10.1164/rccm.201907-1324ED on September 9, 2019
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Raghu G, Collard HR, Egan JJ, Martinez FJ, Behr J, Brown KK, et al. ATS/ERS/JRS/ALAT Committee on Idiopathic Pulmonary Fibrosis. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med. 2011;183:788–824. doi: 10.1164/rccm.2009-040GL. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Raghu G, Remy-Jardin M, Meyers JL, Richeldi L, Ryerson CJ, Lederer DJ, et al. Diagnosis of idiopathic pulmonary fibrosis: an official ATS/ERS/JRS/ALAT clinical practice guideline. Am J Respir Crit Care Med. 2018;198:e44–e68. doi: 10.1164/rccm.201807-1255ST. [DOI] [PubMed] [Google Scholar]
- 3.Graham R, Mancher M, Wolman DM, Greenfield S, Steinberg E, editors. Institute of Medicine (US) Committee on Standards for Developing Trustworthy Clinical Practice Guidelines. Clinical practice guidelines we can trust. Washington, DC: National Academies Press; 2011. [PubMed] [Google Scholar]
- 4.Raghu G, Rochwerg B, Zhang Y, Garcia CA, Azuma A, Behr J, et al. American Thoracic Society; European Respiratory society; Japanese Respiratory Society; Latin American Thoracic Association. An official ATS/ERS/JRS/ALAT clinical practice guideline: treatment of idiopathic pulmonary fibrosis: an update of the 2011 clinical practice guideline. Am J Respir Crit Care Med. 2015;192:e3–e19. doi: 10.1164/rccm.201506-1063ST. [Published erratum appears in Am J Respir Crit Care Med 192:644.] [DOI] [PubMed] [Google Scholar]
- 5.Lynch DA, Sverzellati N, Travis WD, Brown KK, Colby TV, Galvin JR, et al. Diagnostic criteria for idiopathic pulmonary fibrosis: a Fleischner Society white paper. Lancet Respir Med. 2018;6:138–153. doi: 10.1016/S2213-2600(17)30433-2. [DOI] [PubMed] [Google Scholar]
- 6.Richeldi L, Wilson KC, Raghu G. Diagnosing idiopathic pulmonary fibrosis in 2018: bridging recommendations made by experts serving different societies. Eur Respir J. 2018;52:1801485. doi: 10.1183/13993003.01485-2018. [DOI] [PubMed] [Google Scholar]
- 7.Hutchinson JP, Fogarty AW, McKeever TM, Hubbard RB. In-hospital mortality after surgical lung biopsy for interstitial lung disease in the United States: 2000 to 2011. Am J Respir Crit Care Med. 2016;193:1161–1167. doi: 10.1164/rccm.201508-1632OC. [DOI] [PubMed] [Google Scholar]
- 8.Wilson KC, Schoenberg NC, Raghu G Need for Adherence to Institute of Medicine Methodology. Idiopathic pulmonary fibrosis guideline recommendations. Ann Am Thorac Soc. 2019;16:681–686. doi: 10.1513/AnnalsATS.201812-871OC. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.