Abstract
Recovery high schools (RHS) provide a recovery-supportive academic environment for adolescents in recovery from an SUD and are located across the United States. However, only a small proportion of the 160,000 youth in recovery each year in the US enroll in RHSs posttreatment, indicating that many youth do not access this relapse prevention resource despite its effectiveness. Thus, this study uses the adolescent-adapted recovery capital model (RCAM), to understand individual- and community-level predictors of attendance and identify disparities leading to barriers to accessing RHSs.
Data were collected as part of a multisite observational study of adolescents in recovery (N = 294). Logistic regressions and classification trees explored which different recovery capital factors predicted the odds of attending a RHS for at least 28-days during a 12-month period (n = 171) versus a non-RHS (e.g., traditional school: n = 123).
The RCAM model is a useful theoretical framework for examining predictors of RHS attendance and both analysis methods identified multiple unique predictors of RHS attendance. The strongest predictors of RHS attendance were individual-level factors including problem solving skills, 12-Step frequency, and financial resources. The classification trees highlighted additional interactions that should be explored in future empirical research.
Keywords: Adolescent, Recovery Capital, Recovery High Schools, Substance Use Disorders
In 2014, approximately 78,000 adolescents enrolled in publicly-funded substance abuse treatment in the United States (SAMHSA, 2016). Many adolescents who leave treatment return to the same community where they were previously using substances, and these “recovery hostile” environments increase the risk of return to use (Brown et al., 2001; Cerdá, Wall, Keyes, Galea, & Hasin, 2012; Ramo, Prince, Roesch, & Brown, 2012; White et al., 2004). Indeed, given the availability of substances in environments adolescents frequent (Centers for Disease Control and Prevention, 2012; Substance Abuse and Mental Health Services Administration [SAMHSA], 2013) and the influence of social pressures on return to use (Ramo et al., 2012), continuing care services should focus on settings of potential risk and address gaps in community supports by promoting environments that foster sobriety among youth (Gonzales et al., 2012; White, 2009). To address this need, recovery high schools (RHSs) were created to ensure academic advancement and recovery maintenance among adolescents in recovery (Finch & Frieden, 2014): Federal offices have recently identified RHSs as viable youth recovery supports (National Institutes of Drug Abuse, 2014; Office of National Drug Control Policy, 2014) and preliminary research indicates benefits for youth attending these schools (Finch, Tanner-Smith, Hennessy, & Moberg, 2018; Kochanek, 2008; Moberg & Thaler, 1995).
RHS Model and Recovery Capital
Recovery capital is an ecological model that attends to individuals, their social networks, and their communities and encompasses all resources that an individual has to use towards SUD recovery (Granfield & Cloud, 1999; White & Cloud, 2008). This model has recently been adapted from adult-focused recovery capital models to fit the adolescent experience (Hennessy, Cristello, & Kelly, 2018). It is comprised of four primary domains: (1) financial recovery capital (FRC): material resources such as caregiver income, health insurance, and access to treatment; (2) human recovery capital (HRC): personal characteristics that one can use to achieve personal goals; (3) social recovery capital (SRC): resources that enable an adolescent to effectively bond with family, peers, and community institutions and the resources available to an individual through these relationships; (4) community recovery capital (CRC): including community-level, culturally-appropriate resources related to addiction and recovery and cultural capital such as individual values and behavioral patterns generated from cultural group membership(s) that support sobriety. Thus, from an ecological perspective, RHSs are one form of CRC and an especially important one given the amount of time adolescents are expected to spend in an academic environment.
The primary goal in an RHS is academic advancement within a recovery-supportive culture (Karakos, 2014; Moberg & Finch, 2007). RHSs provide recovery-focused services (e.g., daily group check-ins and individual counseling) as a tangible form of CRC for students, which can help to generate new or build upon existing recovery capital. For example, school attendance, engagement, and academic achievement encourages personal growth and replaces substance use activity, peers, and environments with alternative positive activities and sober peers. Thus, RHSs could foster HRC, by teaching adolescents academic and other skills for postsecondary education or later employment, and foster SRC, by surrounding an adolescent with supportive peers.
Research suggests that individuals with some recovery capital have a better chance of developing more recovery capital (Best et al., 2012; 2011; Granfield & Cloud, 2001; Neale & Stevenson, 2014). In the case of RHSs, adolescents with a certain degree of financial stability may attend a treatment center that is knowledgeable about community resources, whereas adolescents with less financial stability might not have access to such resources. Alternatively, adolescents with supportive, connected parents or friends in recovery may be more likely to hear about an RHS, or through peer affiliation, adolescents might be more motivated to attend a school focused on sobriety, such as an RHS. Yet, despite the support an RHS offers, far fewer adolescents in the United States attend an RHS relative to the number of adolescents admitted to treatment centers (Association of Recovery Schools, 2016; SAMHSA, 2016). Yet, research has not yet addressed predictors of attending an RHS among similar samples of youth in recovery, and despite the extensive body of research on adult recovery capital, few studies have applied the model to adolescents (Hennessy, 2017).
Study aims.
This exploratory study sought to identity key factors predicting RHS attendance. Previous research with this sample indicated that adolescents who attended RHSs versus other schools were more likely to remain abstinent from substances and remained in school longer (Finch et al., 2018), suggesting that these schools build recovery capital and assist in recovery. Conceptualized this way, RCAM suggests that adolescents attending an RHS, which is indicative of CRC, would have higher levels of other recovery capital resources, compared to adolescents who do not attend an RHS; factors from all four recovery capital domains were used to predict RHS attendance among this sample. Additionally, factors likely interact to influence the likelihood of attendance. Because of this complexity and the lack of RCAM research, this study employs exploratory methods to identity factors predictive of RHS attendance.
Methods
This project used data collected through a multi-site, longitudinal, observational study on the effectiveness of RHSs, which received University of Minnesota Institutional Review Board approval. In this study, adolescents and their caregiver(s) in three states in the United States were recruited at the end of adolescents’ substance use treatment or at the initiation of school attendance posttreatment, and interviewed at baseline, 3-, 6- and 12-month follow-ups. Trained interviewers collected study data using a structured interview schedule with youth and caregivers. Prior to interviews, study staff met with a potential adolescent participant and his/her caregiver to review the consent/assent forms. Adolescents younger than 18 years were given assent forms and their respective caregiver signed consent for themselves and their adolescent to participate.
Data.
The interview schedule (60–90 minutes) was compiled from validated measures. For the current study, a subset of variables collected from youth during baseline were selected and categorized by recovery capital domain: FRC (family income, health insurance, homelessness history, and family social position score [Haug & Sussman, 1970]); HRC (substance use expectancies, school attitudes, life satisfaction, school problems, stress, and physical health, a five-factor measure of problem solving (PS) orientation and skills, and mental health diagnoses); SRC (social and spiritual social support, substance approving peer attitudes, social competence, neighborhood social connections, and youth-parent relationships); CRC (perceived availability of drugs, youth knowledge of RHS, receipt of AOD/SUD counseling outside school, and 12-Step meeting attendance). Control variables included demographic information and substance use history and diagnoses. See Supplemental Material for scale details and Botzet and colleagues (Botzet et al., 2014) for development of the interview schedule.
Analysis.
This study compares two primary statistical methods: (1) logistic regression and (2) classification trees (McArdle, 2014). In this study we compare the two methods because unlike traditional regression methods where interactions must be specified a priori, exploratory methods such as classification trees can identify important novel interactions between variables (McArdle, 2014; Morgan, 2005; Sonquist et al., 1974). That is, a classification tree sequentially tests available predictors and categorizes participants into subgroups using covariate(s) that best predict the outcome of interest. The resulting subgroups are indications of interactions between included variables; i.e., what characteristics, in combination, predict a particular outcome. Classification trees are also not limited by variable collinearity or missing data.
In all analyses, baseline data from the 294 adolescents retained at three months (91% retention rate) reflecting the four recovery capital domains were used to predict whether an adolescent enrolled at an RHS (1 = yes; n = 171; 0 = no; n = 123) for at least 28-days1 during the 12-month follow-up period.
Logistic regression.
This study first conducted separate confirmatory logistic regressions in Stata SE (14.2; StataCorp, 2015), one for each unique recovery capital domain (either FRC, HRC, SRC or CRC); variables specific to that domain were included as covariates in separate analyses to predict RHS attendance (See Table 1). Control variables (k = 11; e.g., age, race, sex, SUD service history and baseline substance use) were included in each analysis as these were expected to interact with recovery capital (Becker et al., 2012; Sterling et al., 2009; Stevens et al., 2004; Wellman et al., 2014). Due to the number of potentially important key covariates and the sample size, we used a step-wise approach where significant predictors (p <.05) in each recovery capital domain from these four regressions were included in one final regression predicting RHS attendance from overall recovery capital (ORC = FRC + HRC + SRC + CRC).
Table 1.
Recovery Capital Variables – Baseline Measurements by Group
| RHS | RHS | nonR | nonR | Total | Total | ||
|---|---|---|---|---|---|---|---|
| M / n | SD/(%) | M / n | SD/(%) | M / n | SD/(%) | n | |
| Variables in each model (k = 11) | |||||||
| Age (range 13–19) | 16.51 | 1.05 | 16.06 | 1.09 | 16.32 | 1.09 | 294 |
| Age first treated for AOD | 15.29 | 1.23 | 15.50 | 1.21 | 15.38 | 1.23 | 293 |
| Race/ethnicity – Whitea | 147 | (86) | 95 | (77) | 242 | (82) | 294 |
| Race/ethnicity - Blacka | 14 | (8.19) | 13 | (10.57) | 27 | (9.18) | 294 |
| Race/ethnicity – Hispanica | 17 | (9.94) | 17 | (13.82) | 34 | (11.56) | 294 |
| Race/ethnicity – Asiana | 5 | (2.93) | 8 | (6.50) | 13 | (4.42) | 294 |
| Race/ethnicity - Native Americana | 6 | (3.51) | 6 | (4.88) | 12 | (4.08) | 294 |
| Race/ethnicity – Othera | 3 | (1.75) | 3 | (2.44) | 6 | (2.04) | 294 |
| Sex (male = 1) | 88 | (51.46) | 74 | (60.16) | 162 | (55.10) | 294 |
| Days of alcohol use, past 90 days | 19.76 | 25.77 | 15.40 | 22.68 | 17.94 | 24.58 | 294 |
| Days of marijuana use, past 90 days | 54 | 35.43 | 55.71 | 33.28 | 54.71 | 34.50 | 294 |
| Days of other drug use, past 90 days | 32.69 | 36.24 | 16.94 | 26.29 | 26.10 | 33.32 | 294 |
| SUD diagnosis - alcohol | 118 | (69) | 72 | (58.54) | 190 | (64.63) | 294 |
| SUD diagnosis - other drugs | 163 | (95.32) | 115 | (93.50) | 278 | (94.56) | 294 |
| MH service receipt (# times) | 5.92 | 18.58 | 3.53 | 3.83 | 4.94 | 14.51 | 288 |
| AOD treatment (# times) | 4.33 | 23.15 | 1.67 | 1.04 | 3.20 | 17.61 | 290 |
| Human Capital (k = 19) | |||||||
| SU expectancies - psychological benefits | 22.18 | 3.80 | 21.45 | 3.35 | 21.87 | 3.63 | 292 |
| SU expectancies - social benefits | 22.43 | 3.73 | 20.75 | 3.89 | 21.72 | 3.88 | 291 |
| Negative attitudes towards school | 0.57 | 0.26 | 0.56 | 0.26 | 0.57 | 0.26 | 291 |
| General (life) satisfaction | 3.64 | 0.63 | 3.41 | 0.66 | 3.54 | 0.65 | 294 |
| Physical health | 3.58 | 1.70 | 3.15 | 1.65 | 3.40 | 1.69 | 294 |
| School attendance, last 12 months (days) | 159.39 | 46.53 | 146.18 | 50.36 | 153.86 | 48.53 | 294 |
| Cumulative GPA (entire year) | 2.49 | 0.85 | 2.40 | 0.88 | 2.45 | 0.86 | 249 |
| Stress | 3.54 | 1.78 | 2.80 | 1.65 | 3.23 | 1.76 | 294 |
| School problems | 12.87 | 3.19 | 13.02 | 3.10 | 12.93 | 3.15 | 275 |
| Crime and violence screener, lifetime | 2.50 | 1.53 | 2.65 | 1.50 | 2.56 | 1.51 | 294 |
| Avoidance PS style (F1) | 0.08 | 0.87 | −0.11 | 0.89 | 0.00 | 0.88 | 273 |
| Rational PS style (F2) | 0.07 | 0.75 | −0.10 | 0.93 | 0.00 | 0.83 | 273 |
| Impulsivity/carelessness PS style (F3)b | −0.23 | 0.83 | 0.32 | 0.74 | 0.00 | 0.84 | 273 |
| Negative problem orientation (F4) | 0.02 | 0.78 | −0.03 | 0.81 | 0.00 | 0.79 | 273 |
| Positive problem orientation (F5) | −0.06 | 0.77 | 0.09 | 0.75 | 0.00 | 0.77 | 273 |
| DSM-IV diagnosis: major depression | 141 | (82) | 79 | (64) | 220 | (75) | 294 |
| DSM-IV diagnosis: manic episode | 29 | (17) | 22 | (18) | 51 | (17) | 294 |
| DSM-IV diagnosis: PTSD | 59 | (35) | 24 | (20) | 83 | (28) | 294 |
| MH screens: eating disorder | 54 | (32) | 33 | (27) | 87 | (30) | 294 |
| Financial Capital (k = 4) | |||||||
| Family income level (range 1 −7) | 5.61 | 1.27 | 4.97 | 1.44 | 5.34 | 1.38 | 273 |
| Parental social position score (range 4–77) | 33.68 | 13.77 | 38.50 | 16.09 | 35.75 | 14.98 | 275 |
| Ever homeless | 43 | (25.44) | 24 | (19.67) | 67 | (23.02) | 291 |
| Any health insurance | 149 | (97.39) | 100 | (91.74) | 249 | (95.04) | 262 |
| Social capital (k = 8) | |||||||
| General social support index | 8.17 | 1.14 | 8.09 | 1.27 | 8.14 | 1.19 | 294 |
| Social competence index | 3.11 | 0.36 | 3.06 | 0.33 | 3.09 | 0.35 | 292 |
| Neighborhood social connections index | 2.99 | 0.77 | 2.91 | 0.73 | 2.96 | 0.75 | 290 |
| Spiritual social support index | 1.17 | 2.04 | 1.82 | 2.25 | 1.44 | 2.15 | 294 |
| Youth-parent relationship | 60.96 | 22.01 | 56.22 | 21.38 | 58.96 | 21.83 | 291 |
| Substance approving peer attitudes | 3.10 | 0.58 | 2.99 | 0.41 | 3.05 | 0.52 | 290 |
| Immediate family AOD history | 112 | (65) | 88 | (72) | 200 | (68) | 294 |
| Sibling AOD history | 45 | (26) | 34 | (28) | 79 | (27) | 294 |
| Parent AOD history | 103 | (60) | 80 | (65) | 183 | (62) | 294 |
| Immediate family MH history | 104 | (61) | 83 | (67) | 187 | (64) | 294 |
| Sibling MH history | 39 | (23) | 36 | (29) | 75 | (26) | 294 |
| Parent MH history | 97 | (57) | 77 | (63) | 174 | (59) | 294 |
| Community Capital (k =5) | |||||||
| Perceived availability of drugs | 4.35 | 0.58 | 4.09 | 0.70 | 4.24 | 0.65 | 294 |
| Parent knowledge of RHS prior to TX | 59 | (37.82) | 41 | (36.61) | 100 | (37.31) | 268 |
| Youth knowledge of RHS prior to TX | 52 | (32.70) | 50 | (43.86) | 102 | (37.36) | 273 |
| AOD/MH counseling outside school | 128 | (75.29) | 95 | (77.24) | 223 | (76.11) | 293 |
| AA/NA/12-Step meeting attendance | 3.79 | 1.56 | 2.88 | 1.56 | 3.41 | 1.62 | 293 |
Note. AOD = alcohol and other drug. MH = Mental Health. RHS = Recovery High School. Non-RHS = non Recovery High School. SU = Substance use. TX = treatment.
Ethnic/racial demographic categories are presented for each collected category; however, given the proportion of White youth compared to youth of other race/ethnicities in the sample, only a binary variable indicating White/Non-White was used in the analysis.
Given space limitations, in the text, this variable has been truncated to “impulsivity”.
Classification trees.
Following the logistic regressions, classification trees were generated in the RStudio statistical environment (0.99.486) utilizing the Recursive PARTitioning (rpart) package (Therneau, Atkinson, & Ripley, 2015); as with the logistic regressions, one tree for each unique recovery capital domain (either FRC, HRC, SRC or CRC) were used to predict RHS attendance. 10-fold cross validation was used where the sample is randomly divided into 10 equal subsamples and for each iteration a tree is grown from nine of the subsamples and the 10th is used as a pseudo-test sample so that the sum of squared errors for the tree can be calculated (Hastie, Tibshairani, & Friedman, 2008). This process is repeated 10 times, allowing each sub-sample to serve as a pseudo-test and training sample. Trees were allowed to grow with no stopping rules. The complexity parameter (Therneau et al., 2015) generated from this process was used to prune each tree, i.e., remove spurious variables to create a more parsimonious model. In the final model of ORC, only those variables that appeared in the pruned tree for each recovery capital domain were included in the analysis.
Results
The sample was primarily male (55%) and White (82%) and around 16 years of age (SD = 1.09; range 13–19). On average, participants had first received treatment for AOD use around the age of 15 years (SD = 1.23; range 12–18): at baseline, 65% were diagnosed with an alcohol use disorder and 95% were diagnosed with a drug use disorder. See Table 1 for further participant details. Detailed results from the ORC logistic regression and classification tree analyses are presented below (appendices provide results from each unique domain).
Logistic Regression
Based on the logistic regression analyses for each unique recovery capital domain, 10 variables were included in the model of ORC. This model explained approximately 32% of the variance in 28-days of RHS attendance (χ2 = 98.93, p < 0.0001). The odds of attending an RHS were significantly higher for older youth (OR = 1.95, 95% CI [1.21, 3.17]), and for youth with more “other” drug use (OR = 1.02, 95% CI [1.01, 1.03]), health insurance (OR = 10.30, 95% CI [1.58, 67.04]), higher stress (OR = 1.34, 95% CI [1.09, 1.65]), and youth with greater 12-Step meeting attendance frequency (OR = 1.31, 95% CI [1.03, 1.65]). The odds of attending an RHS were significantly lower for youth with an older age of first AOD treatment (OR = 0.61, 95% CI [0.40, 0.94]), with higher impulsivity PS style scores (OR = 0.41, 95% CI [0.26, 0.64]), higher spiritual social support (OR = 0.82, 95% CI [0.70, 0.96]), and those who had knowledge of RHSs prior to treatment (OR = 0.31, 95% CI [0.15, 0.65]).
Classification Tree
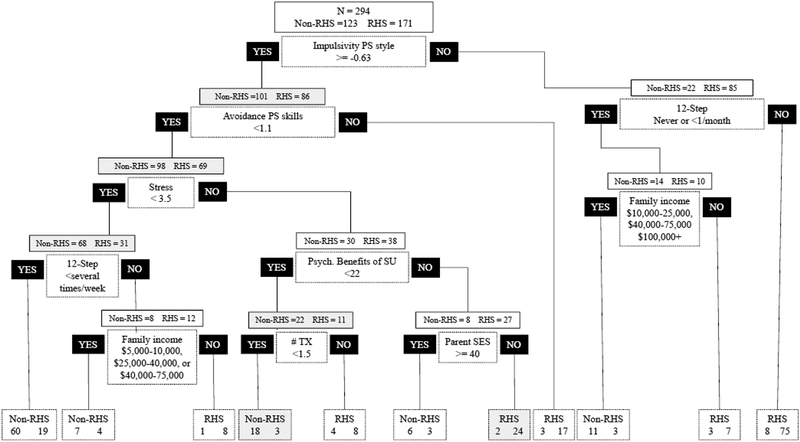
Based on the pruned trees from each unique recovery capital domain, 15 variables were included in the initial classification tree of ORC. The pruned classification tree contained 10 pairs of branches and 11 terminal nodes (see Figure 1). This model correctly identified approximately 81% (n = 139) of RHS attendees and 84% (n = 103) of non-RHS attendees (pseudo-R2 = 57%). Similar to the logistic regressions, the classification tree identified self-reported stress, impulsivity PS style scores, and frequency of self-help group attendance as predictive of 28-day RHS attendance. The tree also indicated other additional variables as predictive of school attendance.
Figure 1.
Overall Recovery Capital Classification Tree Predicting RHS Attendance.
Note. PS = problem solving. SES = socioeconomic status. SU = substance use. TX = Treatment.
Impulsivity PS style scores (higher scores indicate impulsivity) split the sample (107 to the right side of the tree and 187 to the left side). Focusing on the right side of the tree, students with lower impulsivity PS style scores were more likely to be non-RHS students if they attended 12-Step programs never/less than once a month and were in one of three annual income brackets (i.e., $10,000–25,000, $40,000–75,000 or $100,000+). Among similar youth who also attended 12-Step programs infrequently, they were more likely to be RHS students if they were in other income brackets (i.e., $10,000 or less, $25,000–40,000, or $75,000–100,000). Students with lower impulsivity PS style scores were more likely to be RHS students if they attended 12-Step programs once a month or more. The 187 students with higher impulsivity PS style scores (left side of the tree) were more likely to be RHS students if they also had higher avoidance PS scores. If, however, they had lower avoidance PS scores and attended 12-step programs less than several times a week, they were more likely to be non-RHS students. Alternatively, youth with higher scores on impulsivity PS style, lower avoidance PS scores, lower self-reported stress, and more frequent 12-Step group attendance were more likely to be non-RHS students if their parents were in a middle income bracket and RHS students if they were in the very bottom or top of the income range. Furthermore, youth with higher impulsivity PS style, lower avoidance PS scores, and higher self-reported stress, were more likely to be RHS students if they also scored higher on the psychological benefits of substance use scale and had a combined parental SPS score of 40 or less. Alternatively, youth with higher impulsivity PS style, lower avoidance PS scores, and higher self-reported stress, were more likely to be non-RHS students if they also reported higher psychological benefits of substance use and had a family SPS of 40 or more. History of previous treatment receipt was also important: youth with higher impulsivity PS style, lower avoidance PS scores, higher self-reported stress, and lower perceived psychological benefits of substance use were more likely to be non-RHS students if they had fewer than 1.5 treatment instances, and more likely to be RHS students if they had 1.5 or more treatment instances.
In sum, although RHS students were more likely to be more frequent 12-Step attendees and more likely to receive multiple AOD treatment episodes, they had fewer HRC resources; youth were more likely to have lower PS capabilities (higher impulsivity PS style, increased tendency to avoid problems) and greater stress. They were also more likely to report higher perceived psychological benefits of substance use. FRC also indicated a complex picture: RHS youth might be at the bottom and the top of the income spectrum.
Discussion
RHS students, like other youth in recovery, have a mix of strengths and vulnerabilities (Table 2 and Figure 1). The logistic regression and classification tree methods somewhat agreed in their identification of variables important in predicting RHS attendance, and indicated that the key predictors were PS orientation and stress (HRC) and 12-Step meeting attendance (CRC). Both models also identified different aspects of FRC as predictive of RHS attendance (Tree: parental SPS and income; Regression: health insurance), suggesting that some FRC is necessary for RHS access. Indeed, the regression indicated that adolescents were 10 times as likely to attend RHSs if they had health insurance, highlighting the importance of adequate treatment access. Youth in the lowest income spectrum are also eligible for financial aid, fee waivers, and other assistance to attend treatment and to enroll in RHSs; thus, given the parental income patterns, youth in both low and high (but not middle) income brackets may have the fewest FRC barriers to RHS attendance. The classification trees also identified psychological benefits of substance use and avoidance PS style and receipt of AOD treatment as predictive of RHS attendance, while days of other drug use and age were predictive of school choice in the logistic regressions. Differences indicate that the trees may have identified some novel predictors, which only appear when incorporated as interaction terms.
Table 2.
Results from Logistic Regression predicting RHS Attendance from Baseline Recovery Capital Variables
| Overall Recovery Capital (k = 10; N = 226) |
|||
|---|---|---|---|
| OR | 95% CI | ||
| Age | 1.95** | 1.21 | 3.17 |
| Age first treated for AOD | 0.61* | 0.40 | 0.94 |
| Other drug use | 1.02** | 1.01 | 1.03 |
| Parental income | 1.19 | 0.92 | 1.53 |
| Any health insurance | 10.30* | 1.58 | 67.04 |
| Stress | 1.34** | 1.09 | 1.65 |
| Impulsivity/carelessness PS style (F3) | 0.41*** | 0.26 | 0.64 |
| Spiritual social support | 0.82* | 0.70 | 0.96 |
| Youth knowledge of RHS | 0.31** | 0.15 | 0.65 |
| 12-step meeting attendance frequency | 1.31* | 1.03 | 1.65 |
| constant | 0.00* | 0.00 | 0.27 |
| R2 | 32.10 | ||
| Chi2 | 98.93*** | ||
Note. k = number of variables included in model. N = sample size for the model. PS = Problem solving.
p<.05;
p<.01;
p<.001
A culture of recovery is fostered through accessible recovery supports (White, 2009) and RHSs appear to fit this need for some youth, especially those with specific risk factors. Impulsivity PS styles, a measure of negative PS cognition, was a key initial factor for predicting RHS attendance. Students were more likely to be in an RHS than a non-RHS if they had a combination of lower impulsivity style PS style factor scores and frequently attended 12-Step meetings. Lack of coping skills such as PS are predictive of substance use especially among youth who heavily use substances (Jaffee & D’Zurilla, 2009; Waldron & Kaminer, 2004; Wills et al., 2001). As a result, continuing care supports, such as RHSs and 12-step programs, emphasize life skills to help youth manage the challenges of being an adolescent in recovery; thus, youth lacking these skills may choose to attend supports that advertise these components.
Limitations.
We had a small sample for this study, yet, similar to other studies of this size, we addressed this limitation through 10-fold cross validation and pruning, which permit a more parsimonious model and accounts for relative error. Classification tree analysis parses the sample into small groups for particular combinations of variables; thus, the smallest groups should be interpreted with caution because the findings might not hold for different samples. Surveys were administered in a structured interview so some responses could be biased by social desirability. The timeline of recruitment is a limitation; some youth recruited at school entry may have experienced gains in recovery capital domains compared to youth recruited immediately from treatment. Similarly, RHS programs encourage youth to attend outside supports so it is difficult to ascertain whether 12-Step meeting attendance among youth who also attended RHSs resulted from a culture which encourages this support or self-selection.
Implications.
This study used an exploratory method and logistic regressions to explore the RCAM and identity novel interactions for examination in future research. Important individual factors that would affect decisions in the social environment were identified, thus, their interaction with predictors identified via exploratory methods are worth future examination. Future research must consider the multiple interacting factors that affect adolescent recovery processes and the RCAM appears a useful tool for continued research on this issue.
Supplementary Material
Acknowledgements:
The analysis for this manuscript was funded in part by the Institute for Social Research and the James Morgan Fund for New Directions in the Analysis of Complex Interactions. Funding for the research study was made possible by Grant Number R01DA029785-01A1 from the National Institute on Drug Abuse (NIDA). Its contents are solely the responsibility of the author and do not necessarily represent the official views of NIDA or the NIH.
Footnotes
Results from this study were included as part of the first authors’ dissertation and were originally presented at the following conferences: (1) Oral presentation at the Modern Modeling Methods Conference, Storrs, CT in 2018; (2) Poster presentation at the Collaborative Perspectives on Addiction Conference, Tampa, FL in 2018. However, the original analysis of the data utilized a smaller analytic sample as data collection/cleaning had not yet been completed at the time of these events.
28-days of attendance was utilized in this study to be consistent with the operationalization of RHS attendance in the study examining substance use outcomes of RHS versus other-school enrolled use (Finch et al., 2018).
Contributor Information
Emily A. Hennessy, Vanderbilt University
Andrew J. Finch, Vanderbilt University
References
- Association of Recovery Schools. (2016). State of recovery high schools, 2016 biennial report. Denton, TX: Association of Recovery High Schools. [Google Scholar]
- Becker SJ, Stein GL, Curry JF, & Hersh J (2012). Ethnic differences among substance-abusing adolescents in a treatment dissemination project. Journal of Substance Abuse Treatment, 42(3), 328–36. doi: 10.1016/j.jsat.2011.08.007 [DOI] [PubMed] [Google Scholar]
- Best D, Gow J, Taylor A, Knox A, & White W (2011). Recovery from heroin or alcohol dependence: A qualitative account of the recovery experience in Glasgow. Journal of Drug Issues, 41(3), 359–378. [Google Scholar]
- Best D, Gow J, Knox T, Taylor A, Groshkova T, & White W (2012). Mapping the recovery stories of drinkers and drug users in Glasgow: Quality of life and its associations with measures of recovery capital. Drug and Alcohol Review, 31(3), 334–41. doi: 10.1111/j.1465-3362.2011.00321.x [DOI] [PubMed] [Google Scholar]
- Botzet AM, McIlvaine PW, Winters KC, Fahnhorst T, & Dittel C (2014). Data collection strategies and measurement tools for assessing academic and therapeutic outcomes in recovery schools. Peabody Journal of Education, 89(2), 197–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown SA, D’Amico EJ, McCarthy DM, & Tapert SF (2001). Four-year outcomes from adolescent alcohol and drug treatment. Journal of Studies on Alcohol, 62(3), 381–388. [DOI] [PubMed] [Google Scholar]
- Cerdá M, Wall M, Keyes KM, Galea S, & Hasin D (2012). Medical marijuana laws in 50 states: Investigating the relationship between state legalization of medical marijuana and marijuana use, abuse and dependence. Drug and Alcohol Dependence, 120(1), 22–27. doi: 10.1016/j.drugalcdep.2011.06.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. [Youth Risk Behavior Surveillance- United States, 2011]. MMWR 2012; 61(4): 24 Available from: http://www.cdc.gov/mmwr/pdf/ss/ss6104.pdf [PubMed] [Google Scholar]
- DeCato LA, Donohue B, Azrin NA, & Teichner GA (2001). Satisfaction of conduct disordered and substance abusing youth with their parents. Behavior Modification, 25(1),44–52. [DOI] [PubMed] [Google Scholar]
- Dennis ML (2010). Global Appraisal of Individual Needs (GAIN): A Standardized Biopsychosocial Assessment Tool. Bloomington, IL: Chestnut Health Systems. [Google Scholar]
- D’Zurilla TJ, & Nezu AM (1990). Development and preliminary evaluation of the Social Problem-Solving Inventory. Psychological Assessment: A Journal of Consulting and Clinical Psychology, 2, 156–163. [Google Scholar]
- D’Zurilla T, Nezu A, & Maydeu-Olivares A. (2002) Social Problem-Solving Inventory-Revised (SPSI-R): Manual. North Tonawanda, NY: Multi-Health Systems. [Google Scholar]
- Finch AJ, & Frieden G (2014). The ecological and developmental role of recovery high schools. Peabody Journal of Education, 89(2), 271–287. doi: 10.1080/0161956X.2014.897106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finch AJ, Tanner-Smith E, Hennessy E, & Moberg DP (2018). Recovery high schools: Effect of schools supporting recovery from substance use disorders. The American Journal of Drug and Alcohol Abuse, 44(2), 175–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzales R, Anglin MD, Beattie R, Ong CA, & Glik DC (2012). Understanding recovery barriers: Youth perceptions about substance use relapse. American Journal of Health Behavior, 36(5), 602–14. doi: 10.5993/AJHB.36.5.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granfield R, & Cloud W (1999). Coming clean: Overcoming addiction without treatment. New York: New York University Press. [Google Scholar]
- Granfield R, & Cloud W (2001). Social context and “natural recovery”: The role of social capital in the resolution of drug-associated problems. Substance Use & Misuse, 36(11), 1543–1570. [DOI] [PubMed] [Google Scholar]
- Haug MR, & Sussman MB (1970). Reply to Hollingshead. Social Forces, 49, 568. [Google Scholar]
- Haug MR, & Sussman MB (1971). The indiscriminate state of social class measurement. Social Forces, 49(4), 549–563. [Google Scholar]
- Hennessy EA (2017). Recovery capital: a systematic review of the literature. Addiction Research & Theory, 25(5), 349–360. [Google Scholar]
- Hennessy EA, Cristello JV, & Kelly JF (2018). RCAM: a proposed model of recovery capital for adolescents. Addiction Research & Theory, 1–8. [Google Scholar]
- Jaffee WB, & D’Zurilla TJ (2009). Personality, problem solving, and adolescent substance use. Behavior therapy, 40(1), 93–101. [DOI] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, & Schulenberg JE (2011). Monitoring the Future national results on adolescent drug use: Overview of key findings, 2010. Ann Arbor: Institute for Social Research, The University of Michigan. [Google Scholar]
- Karakos HL (2014). Positive peer support or negative peer influence? The role of peers among adolescents in recovery high schools. Peabody Journal of Education, 89(2), 214–228. doi: 10.1080/0161956X.2014.897094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kochanek TT (2008). Recovery high schools in Massachusetts: A promising, comprehensive model for adolescent substance abuse and dependence. Reno, NV: The Stacie Mathewson Foundation; Retrieved from http://massrecoveryhs.org/documents/RecoveryHighSchooloverview.pdf [Google Scholar]
- Leffert N, Benson PL, Scales PC, Sharma AR, Drake DR, & Blyth DA (1998). Developmental assets: Measurement and Prediction of risk behaviors among adolescents. Applied Developmental Science, 2, 209–230 [Google Scholar]
- McArdle JJ (2014). Exploratory data mining using decision trees in the behavioral sciences In McArdle JJ & Ritschard G (Eds.), Quantitative Methodology Series: Contemporary issues in exploratory mining in the behavioral sciences (pp. 1–47). New York, NY: Routledge. [Google Scholar]
- Moberg DP, & Finch AJ (2007). Recovery high schools: A descriptive study of school programs and students. Journal of Groups in Addiction & Recovery, 2, 128–161. doi: 10.1080/15560350802081314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moberg DP, & Thaler SL (1995). An evaluation of Recovery High School: An alternative high school for adolescents in recovery from chemical dependence. Madison, WI: University of Wisconsin-Madison Medical School Department of Preventive Medicine Center for Health Policy and Program Evaluation. [Google Scholar]
- Morgan JN (2005). History and potential of binary segmentation for exploratory data analysis. Journal of Data Science, 3(2), 123–136. [Google Scholar]
- National Institute on Drug Abuse (NIDA). (2014, January). Principles of adolescent substance use disorder treatment: A research-based guide. Retrieved from http://www.drugabuse.gov/sites/default/files/podata_1_17_14.pdf
- Neale J, & Stevenson C (2014). Social and recovery capital amongst homeless hostel residents who use drugs and alcohol. International Journal of Drug Policy, in press. 10.1016/j.drugpo.2014.09012 [DOI] [PubMed] [Google Scholar]
- Office of National Drug Control Policy (ONDCP). (2014). National drug control strategy. Washington, D.C.: Office of National Drug Control Policy; Retrieved from http://www.whitehouse.gov/sites/default/files/ondcp/policy-and-research/ndcs_2014.pdf [DOI] [PubMed] [Google Scholar]
- Ramo DE, Prince MA, Roesch SC, & Brown SA (2012). Variation in substance use relapse episodes among adolescents: A longitudinal investigation. Journal of Substance Abuse Treatment, 43(1), 44–52. doi: 10.1016/j.jsat.2011.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds CR, & Kamphaus RW (1992). Behavior Assessment System for Children: Manual. Circle Pines, MN: American Guidance. [Google Scholar]
- Sheehan DV, Janavs R, Baker R, Harnett-Sheehan K, Knapp E, & Sheehan M (1999). Mini International Neuropsychiatric Interview. Tampa: University of South Florida Press. [Google Scholar]
- Sobell LC, & Sobell MB, (1992). Timeline Followback: A technique for assessing self-reported alcohol consumption In Litten RZ & Allen J (Eds.), Measuring alcohol consumption: Psychosocial and biological methods (pp. 41–72). New Jersey: Humana Press. [Google Scholar]
- Sonquist JA, Baker EL, & Morgan JN (1974). Searching for structure. Michigan: The University of Michigan. [Google Scholar]
- StataCorp (2015). Stata Statistical Software: Release 14. College Station, TX: StataCorp LP. [Google Scholar]
- Sterling S, Chi F, Campbell C, & Weisner C (2009). Three-year chemical dependency and mental health treatment outcomes among adolescents: The role of continuing care. Alcoholism, Clinical and Experimental Research, 33(8), 1417–29. doi: 10.1111/j.1530-0277.2009.00972.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens SJ, Estrada B, Murphy BS, McKnight KM, & Tims F (2004). Gender difference in substance use, mental health, and criminal justice involvement of adolescents at treatment entry and at three, six, 12 and 30 month follow-up. Journal of Psychoactive Drugs, 36(1), 13–25. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2013). Results from the 2012 National Survey on Drug Use and Health: Summary of National Findings, NSDUH Series H-46, HHS Publication No. (SMA) 13-4795. Rockville, MD: Substance Abuse and Mental Health Services Administration. [Google Scholar]
- Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality (2016). Treatment Episode Data Set (TEDS): 2004–2014. National Admissions to Substance Abuse Treatment Services. BHSIS Series S-84, HHS Publication No. (SMA) 16-4986. Rockville, MD: Substance Abuse and Mental Health Services Administration. [Google Scholar]
- Therneau T, Atkinson B, & Ripley B (2015). Recursive partitioning and regression trees [Version 4.1.−10] (Software). Available from: https://cran.r-project.org/web/packages/rpart/
- Therneau TM, Atkinson EJ, & Mayo Foundation (2015). An introduction to recursive partitioning using the RPART routines. Available from https://cran.r-project.org/web/packages/rpart/vignettes/longintro.pdf
- Waldron HB, & Kaminer Y (2004). On the learning curve: The emerging evidence supporting cognitive--behavioral therapies for adolescent substance abuse. Addiction, 99(s2), 93–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wellman RJ, Contreras GA, Dugas EN, O’Loughlin EK, & O’Loughlin JL (2014). Determinants of sustained binge drinking in young adults. Alcoholism, Clinical and Experimental Research, 38(5), 1409–15. doi: 10.1111/acer.12365 [DOI] [PubMed] [Google Scholar]
- White WL (2009). The mobilization of community resources to support long-term addiction recovery. Journal of Substance Abuse Treatment, 36(2), 146–58. doi: 10.1016/j.jsat.2008.10.006 [DOI] [PubMed] [Google Scholar]
- White W, & Cloud W (2008). Recovery capital: A primer for addictions professionals. Counselor, 9(5), 22–27. [Google Scholar]
- White AM, Jordan JD, Schroeder KM, Acheson SK, Georgi BD, Sauls G, … Swartzwelder HS (2004). Predictors of relapse during treatment and treatment completion among marijuana-dependent adolescents in an intensive outpatient substance abuse program. Substance Abuse, 25(1), 53–9. doi: 10.1300/J465v25n01_08 [DOI] [PubMed] [Google Scholar]
- Wills TA, Sandy JM, Yaeger AM, Cleary SD, & Shinar O (2001). Coping dimensions, life stress, and adolescent substance use: A latent growth analysis. Journal of Abnormal Psychology, 110(2), 309. [DOI] [PubMed] [Google Scholar]
- Winters K & Henly G (1993). Adolescent Diagnostic Interview (ADI) Manual. Los Angeles, CA: Western Psychological Services. [Google Scholar]
- Winters KC & Henly GA (1989). Personal Experience Inventory (PEI) Test and Manual. Los Angeles: Western Psychological Services. [Google Scholar]
- Winters KC, Stinchfield R, Latimer WW, & Lee S (2007). Long-term outcome of substance-dependent youth following 12-step treatment. Journal of Substance Abuse Treatment, 33(1), 61–9. doi: 10.1016/j.jsat.2006.12.003 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.