Abstract
Introduction
The aim of this analysis was to investigate whether the standardized uptake value (SUV) normalized by lean body mass (SUL) is a more appropriate quantitative parameter compared to the commonly used SUV normalized by patient’s weight in 68Ga-PSMA11 PET/CT.
Material and methods
68Ga-PSMA11 PET/CT scans of 121 patients with prostate cancer from two institutions were evaluated. Liver SUV was measured within a 3-cm volume-of-interest (VOI) in the right hepatic lobe and corrected for lean body mass using the Janmahasatian formula. SUV and SUL repeatability between baseline and follow-up scans of the same patients were assessed.
Results
SUV was significantly positively correlated with body weight (r = 0.35, p = 0.02). In contrast, SUL was not correlated with body weight (r = 0.23, p = 0.07). No significant differences were found between baseline and follow-up scan (p = 0.52).
Conclusion
The Janmahasatian formula annuls the positive correlations between SUV and body weight, suggesting that SUL is preferable to SUV for quantitative analyses of 68Ga-PSMA11 PET/CT scans.
Keywords: SUL, PSMA PET, SUV
Introduction
In the last decade, positron emission tomography/computer tomography (PET/CT) has gradually emerged as the standard-of-care imaging modality in the diagnosis and treatment response monitoring of different oncological malignancies [1, 2]. Moreover, standardized uptake value (SUV), which is the commonly used quantitative parameter in PET/CT showed a high predictive value for treatment outcome [3, 4]. However, quantitative SUV is still hampered by a number of physiological, technical and physical factors widely discussed in the literature [5].
In 18F-FDG PET/CT, SUV normalized by patient’s weight is known to be highly dependent on body weight [6]. Since 18F-FDG does not significantly accumulate in adipose tissue in the fasting state, the use of SUV can falsely lead to high values in patients with high body mass. Subsequently, SUL (lean body mass (LBM)–corrected SUV) has been proposed as a more appropriate quantitative method, with Janmahasatian formulation for LBM showing most accurate results [7].
The liver is typically used as reference organ in PET imaging, with a 3-cm spherical volume of interest (VOI) computed to measure the liver background activity [8]. In 18F-FDG PET/CT, liver SUL showed only a fair repeatability between two time points in the same patient [9].
In the past 5 years, prostate-specific membrane antigen (PSMA), a transmembrane protein highly expressed in prostate cancer, has become a promising target for PET in prostate cancer imaging [10]. 68Ga-PSMA11 PET/CT has shown enhanced accuracy compared to conventional imaging modalities in lesion detection [11], with SUV being largely used as a quantitative PET-derived parameter [12, 13]. However, the effect of body weight on SUV in 68Ga-PSMA11 PET/CT has not been yet investigated. Since 68Ga-PSMA11 does not typically accumulate in adipose tissue [14], we hypothesized that liver SUV is dependent from body weight.
The aim of the present study was to investigate whether SUL is a more appropriate quantitative method compared to the commonly used SUV normalized by body weight in 68Ga-PSMA11 PET/CT imaging.
Material and methods
Patients
Patients from two institutions, Technical University Munich (COH1) and University of California Los Angeles (COH2), who underwent 68Ga-PSMA11 PET/CT prior to 177Lu-PSMA radioligand therapy were included. Patients in whom it was not feasible to draw a 3-cm VOI in healthy liver tissue were excluded.
For COH1, 91 subsequent patients who received between October 2014 and March 2018 were considered for this analysis. For COH2, 43 subsequent patients were prospectively enrolled in a phase 2 trial (NCT03515577). All patients signed a written consent for evaluation of their data and the institutional review board of the Technical University Munich (permit 5665/13) and University of California Los Angeles (permit 17-000330) approved this analysis.
Image acquisition
Images were obtained in accordance with the international guideline [15] in conjunction with a diagnostic following application of 68Ga-PSMA-11 that was synthesized as described previously [16]. The 68Ga-PSMA-ligand complex solution was applied to patients via an intravenous bolus with a mean of 146.0 ± 45.4 and 192.3 ± 19.7 MBq for COH1 and COH2, respectively. PET acquisition was started at a mean time of 66.5 ± 12.8 and 56.4 ± 9.7 min after tracer injection for COH1 and COH2. The PET was reconstructed by ordered subset expectation maximization (OSEM)-based algorithms. Data from the CT scan were used for attenuation correction.
Image analyses
Images were reviewed using qPSMA, an in-house developed software [17]. Body weights were recorded from the patients’ records.
SUV and SUL
For liver SUV computation, the VOI was semi-automatically placed using an algorithm [18] that has shown excellent intra- and inter-reader agreement. SUL was calculated according to the Janmahasatian formula as follows:
Repeatability
To assess repeatability and the potential influence of tumor sink effect two 68Ga-PSMA11 PET/CT scans from a subset of patients at two different dates were included in the analysis. SUV and SUL of both scans were compared.
Statistical analysis
Values were reported as mean ± SD. Pearson correlations were performed to evaluate the relationship between SUV, SUL, and body weights. Paired t-test was used when the values were considered as paired. p value < 0.05 was considered statistically significant. Analyses were performed using SPSS Statistics v22.0 (IBM Corp., USA).
Results
Patient cohort
In total, 121 patients were included in the final analyses. Eighty patients of COH1 were eligible; as in 11 patients, the 3-cm VOI in the liver was not feasible due to severe breathing artifacts. Forty-one patients of COH2 could be included as two patients underwent 18F-DCFPyL PET/CT prior to 177LuPSMA treatment. Notably, significantly higher activity doses were injected for COH2 (mean ± SD,118 ± 25 vs. 192 ± 19 MBq, p < 0.001). Mean ± SD of body weight were 80.3 ± 11.4, 82.5 ± 17.5 and 81.0 ± 13.7 kg for COH1, COH2, and all patients, respectively. Patient characteristics are presented in Table 1.
Table 1.
Patients characteristics
| All patients (n = 121) | |
|---|---|
| Age (years) | 73 ± 7.3 |
| Body weight (kg) | 81.0 ± 13.7 |
| Time since diagnosis of prostate cancer (years) | 7 ± 11 |
| Gleason score at diagnosisa | |
| < 8 | 38 (36%) |
| ≥ 8 | 69 (64%) |
| PSA at the time of PET/CT imaging (ng/ml) | 114 ± 671 |
| Prior lines of systemic treatment | |
| 2 | 8 (7%) |
| ≥ 3 | 113 (93%) |
| ≥ 4 | 78 (64%) |
| ≥ 5 | 44 (36%) |
| ≥6 | 25 (21%) |
| Sites of disease on PSMA-PET | |
| Bone | 112 (93%) |
| Lymph nodes | 97 (80%) |
| Visceralb | 43 (36%) |
| Bone + lymph nodes | 88 (73%) |
| Bone + lymph nodes + visceral | 34 (28%) |
Data are median ± standard deviation or n (%)
PSA, prostate-specific antigen; PSMA, prostate-specific membrane antigen
aData missing for 14 patients
bVisceral includes liver, lungs, and adrenal glands
SUV, SUL, and comparisons
Mean ± SD of liver SUV were 4.30 ± 1.55, 4.58 ± 1.57, and 4.36 ± 1.56 for COH1, COH2, and all patients, respectively. Mean ± SD of liver SUL were 3.23 ± 1.16, 3.41 ± 1.03, and 3.29 ± 1.12 for COH1, COH2, and all patients, respectively. Both cohorts did not show any significant differences for body weights (p = 0.46), SUVs (p = 0.27), or SULs (p = 0.37).
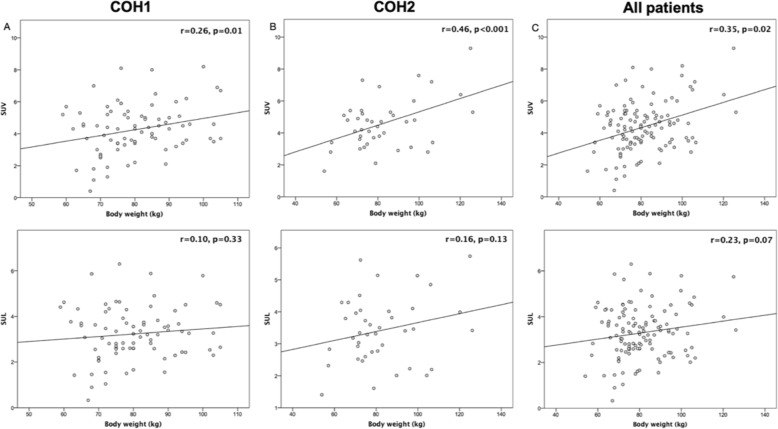
SUV showed a significant, but weak correlation with body weight (r = 0.26, p = 0.01), (r = 0.46, p < 0.001), and (r = 0.35, p = 0.02) for COH1, COH2, and all patients, respectively. In contrast, SUL was not significantly correlated with body weight (r = 0.10, p = 0.33), (r = 0.16, p = 0.13), and (r = 0.23, p = 0.07) for COH1, COH2, and all patients, respectively. Scatter plots of correlations for both SUV and SUL with body weight are displayed in Fig. 1.
Fig. 1.
Scatter plots of both SUV and SUL correlations with body weight for a COH1, b COH2, and c all patients
Repeatability
Sixty patients from COH1 received a follow-up 68Ga-PSMA11 PET/CT during 177Lu-PSMA radioligand therapy at a mean ± SD of 3.7 ± 0.6 months after the baseline scan. Mean ± SD-injected dose for baseline and follow-up scan was 118 ± 25 and 105 ± 23 MBq, respectively.
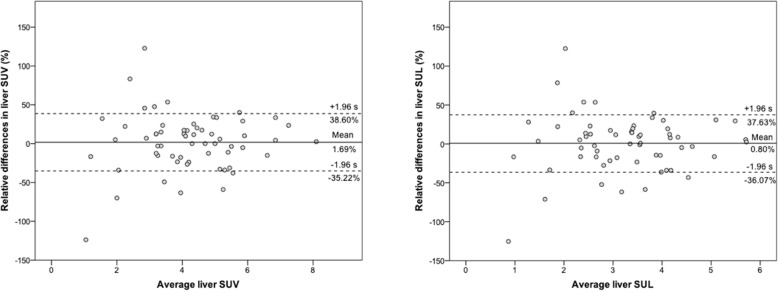
Mean liver SUV did not change significantly (p = 0.52) between the baseline (4.26 ± 1.64) and follow-up scan (4.16 ± 1.60). Mean (95%CI) relative difference was 1.69 (−7.84;11.22)% with ICC of 0.821 (0.701–0.893). Mean liver SUL did not change significantly (p = 0.72) between the baseline (3.25 ± 1.22) and follow-up scans (3.21 ± 1.22). Mean (95% CI) relative difference was 0.80 (−8.70; 10.32)%, with ICC of 0.818 (0.696–0.892). Figure 2 displays the Bland-Altman plots for SUV and SUL.
Fig. 2.
Bland-Altman plots of baseline and follow-up 68Ga-PSMA11 PET/CTs agreement for both liver SUV and SUL
Discussion
To the best of our knowledge, this is the first report evaluating the potential of using SUL as compared to the commonly used SUV as quantitative parameter in 68Ga-PSMA11 PET/CT. Our data indicate that a weak but significant positive correlation is present between liver SUV and body weight. Contrarily, SUL as alternative parameter seems to be unaffected from body weight. Since 68Ga-PSMA11 does not typically accumulate in adipose tissue the use of SUL can be recommended to avoid any influence from patient habitus.
PET-derived parameters, such as SUVmean or SUVmax, are increasingly used for therapy response monitoring or patient outcome prediction. Therefore, highly accurate computed parameters should be addressed given their potential decisive role for the clinical image–based decisions. The present study attempted to reproduce a clinical setting where quantitative 68Ga-PSMA11 PET/CT scans are used in the framework of 177Lu-PSMA radioligand therapy.
We investigated the relation of body weight with SUV and SUL in a patient cohort including subcohorts of both European and North-American patients. Consistently among the subgroups, our findings indicate that liver SUL calculated based on Janmahasatian formula annuls the body weight dependence of liver SUV. Noteworthy, even though a significant correlation was found between body weight and SUV, its strength is rather weak (r = 0.35, p = 0.02). However, since SUL (r = 0.23, p = 0.07) annuls and lowers the strength of the positive correlations to BW, the use of SUL should be preferred over SUV. In FDG PET/CT, liver SUV showed a moderate correlation for women (r = 0.58, p < 0.001) and men (r = 0.54, p < 0.001) with body weight, which was annulled and reduced by the Janmahasatian formula, respectively [7].
In addition, we have to stress that the high interpatient repeatability of both liver SUV and SUL between two time points (ICC = 0.821 and 0.818) demonstrates an acceptable mean difference of 1.69% and 0.80%. Despite potential changes of liver 68Ga-PSMA11 uptake during 177Lu-PSMA therapy upon shifts of biodistribution depending on tumor sink effect, the use of liver as the reference organ to threshold malignancy comparing subsequent timepoints is feasible [19]. Notably, it has been shown that only high differences in tumor burden have significant implications on liver 68Ga-PSMA11-uptake, with low vs. high tumor load exhibiting a liver SUVmean of 4.34 vs. 3.27, p < 0.001 [13].
Androgen deprivation therapy (ADT) has shown to increase the PSMA-ligand uptake in the first weeks after treatment initiation in metastatic sensitive prostate-cancer [20]. Moreover, continuous long-term ADT significantly decreased lesion uptake in 68Ga-PSMA11 PET imaging [21]. However, these findings might not be valid for patients with metastatic castration-resistant prostate cancer, since most of their tumor lesions are not responding properly to first-line ADT. No significant differences were noted between liver SUV in patients receiving ADT versus not receiving [22]. Same analysis further evaluated the 68Ga-PSMA11 uptake of other tissues such blood pool (SUVmean 1.08) or muscle (SUVmean 0.50). Nevertheless, the liver showed the most feasible values (SUVmean 4.73) to be used for PSMA PET quantification. The mean liver SUV obtained in the present analysis (4.36) is in concordance with those obtained by Jansen et al (4.73) and Gaertner et al. (4.25) [13].
Interestingly, in an analysis including 64 patients who received 18F-DCFPyL PET/CT no correlations were found between both liver SUV and SUL with body weight [23]. Comparing the results, for 18F-DCFPyL were obtained higher liver SUV and SUL values: 5.1 ± 0.7 vs. 4.4 ± 1.5 and 3.8 ± 0.5 vs. 3.3 ± 1.1 respectively. Similar to FDG, PSMA-ligands do not typically accumulate in adipose tissue, therefore a positive correlation between SUV and BW annulated by SUL was expected to be found for both radiopharmaceuticals.
For PSMA-targeted radioligand therapies, 68GaPSMA11 PET imaging is typically used at baseline for patient selection, as well as during treatment for radiographic response assessment. However, the clinical utility of 68GaPSMA11 PET in metastatic castration-resistant prostate cancer goes beyond the radioligand therapy, being increasingly used for evaluation of treatment response in patients receiving, e.g., taxanes [24]. Since the traditional SUV has shown a significant correlation with body weight, its clinical value in 68Ga-PSMA11 PET quantification remains questionable. Thus, our findings may have clinical implications especially in treatment response assessment. However, further studies comparing the prognostic value of both SUV and SUL for imaging response evaluation are warranted.
Notable limitations of the current analysis are the retrospective nature of the study and the inclusion of a selected patient cohort scheduled for 177Lu-PSMA radioligand therapy. However, as our patients have shown both high and low tumor load the potential influence of different tumor burden is already acknowledged. Finally, our analysis is focused on the liver as most important normal organ in PSMA-ligand PET imaging severing as reference tissue. We have not investigated the influence of body weight on other normal tissues.
Conclusion
Our results indicate that the Janmahasatian formula annuls the positive correlations between absolute SUV and body weight, suggesting that SUL is preferable to SUV for quantitative analyses in 68Ga-PSMA11 PET. Future studies, are necessary to determine the clinical significance of the differences between SUV and SUL for different clinical applications, such as thresholds for delineation of tumor volumes or monitoring tumor response to therapy.
Acknowledgements
The authors thank the technicians Alexandra Bartel, Coletta Kruschke, Amanda Reinhardt, Brigitte Mackert, Alida Wachendorf, and Gitti Dzewas for their excellent work on PET/CT.
Abbreviations
- ADT
Androgen deprivation therapy
- BW
Body weight
- LBM
Lean body mass
- PET
Positron emission tomography
- PET/CT
Positron emission tomography/computer tomography imaging
- PSMA
Prostate-specific membrane antigen
- SUL
Standardized uptake value normalized to lean body mass
- SUV
Standard uptake value
- VOI
Volume of interest
Authors’ contributions
AG and ME participated in the design of the study, data analysis, and drafted the manuscript. AG, JC, CF, IR, HW, and AR performed the data analysis and statistics. ME, JCZ, and WW revised the manuscript. All authors read and approved the final manuscript.
Funding
M.E. received funding from the SFB 824 (DFG Sonderforschungsbereich 824, Project B11) from the Deutsche Forschungsgemeinschaft, Bonn, Germany. Siemens Medical Solutions (Erlangen, Germany) provided the continuous bed motion option for the Biograph mCT as part of an academic collaboration.
Availability of data and materials
Please contact the corresponding author for data requests.
Ethics approval and consent to participate
All patients signed a written consent for evaluation of their data and the institutional review board of the Technical University Munich (permit 5665/13) and University of California Los Angeles (permit 17-000330) approved this analysis.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Cheson BD. PET/CT in lymphoma: current overview and future directions. Semin Nucl Med. 2018;48:76–81. doi: 10.1053/j.semnuclmed.2017.09.007. [DOI] [PubMed] [Google Scholar]
- 2.Subramaniam SM, Joyce CM, Prashanti L, Gregory R, Gustavo M, Rathan M. The role of PET/CT in the management of cervical cancer. AJR Am J Roentgenol. 2013;201(2):W192–W205. doi: 10.2214/AJR.12.9830. [DOI] [PubMed] [Google Scholar]
- 3.van Rossum PS, Fried DV, Zhang L, Hofstetter WL, Ho L, Meijer GJ, et al. The value of (18)F-FDG PET before and after induction chemotherapy for the early prediction of a poor pathologic response to subsequent preoperative chemoradiotherapy in oesophageal adenocarcinoma. Eur J Nucl Med Mol Imaging. 2017;44:71–80. doi: 10.1007/s00259-016-3478-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mikhaeel NG, Smith D, Dunn JT, Phillips M, Moller H, Fields PA, et al. Combination of baseline metabolic tumour volume and early response on PET/CT improves progression-free survival prediction in DLBCL. Eur J Nucl Med Mol Imaging. 2016;43:1209–1219. doi: 10.1007/s00259-016-3315-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zaidi H. Quantitative analysis in nuclear medicine imaging | Habib Zaidi | Springer. New York: Springer; 2006. [Google Scholar]
- 6.Zasadny KR, Wahl RL. Standardized uptake values of normal tissues at PET with 2-[fluorine-18]-fluoro-2-deoxy-D-glucose: variations with body weight and a method for correction. Radiology. 1993;189:847–850. doi: 10.1148/radiology.189.3.8234714. [DOI] [PubMed] [Google Scholar]
- 7.Tahari AK, Chien D, Azadi JR, Wahl RL. Optimum lean body formulation for correction of standardized uptake value in PET imaging. J Nucl Med. 2014;55:1481–1484. doi: 10.2967/jnumed.113.136986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wahl RL, Jacene H, Kasamon Y, Lodge MA. From RECIST to PERCIST: evolving considerations for PET response criteria in solid tumors. Journal of nuclear medicine: official publication. Soc Nucl Med. 2009;50(Suppl 1):122s–150s. doi: 10.2967/jnumed.108.057307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tahari AK, Paidpally V, Chirindel A, Wahl RL, Subramaniam RM. Two-time-point FDG PET/CT: liver SULmean repeatability. AJR Am J Roentgenol. 2015;204:402–407. doi: 10.2214/ajr.14.12719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eiber M, Fendler WP, Rowe SP, Calais J, Hofman MS, Maurer T, et al. Prostate-specific membrane antigen ligands for imaging and therapy. J Nucl Med. 2017;58:67s–76s. doi: 10.2967/jnumed.116.186767. [DOI] [PubMed] [Google Scholar]
- 11.Eiber M, Maurer T, Souvatzoglou M, Beer AJ, Ruffani A, Haller B, et al. Evaluation of Hybrid (6)(8)Ga-PSMA Ligand PET/CT in 248 patients with biochemical recurrence after radical prostatectomy. J Nucl Med. 2015;56:668–674. doi: 10.2967/jnumed.115.154153. [DOI] [PubMed] [Google Scholar]
- 12.Schmidkonz Christian, Cordes Michael, Schmidt Daniela, Bäuerle Tobias, Goetz Theresa Ida, Beck Michael, Prante Olaf, Cavallaro Alexander, Uder Michael, Wullich Bernd, Goebell Peter, Kuwert Torsten, Ritt Philipp. 68Ga-PSMA-11 PET/CT-derived metabolic parameters for determination of whole-body tumor burden and treatment response in prostate cancer. European Journal of Nuclear Medicine and Molecular Imaging. 2018;45(11):1862–1872. doi: 10.1007/s00259-018-4042-z. [DOI] [PubMed] [Google Scholar]
- 13.Gaertner FC, Halabi K, Ahmadzadehfar H, Kurpig S, Eppard E, Kotsikopoulos C, et al. Uptake of PSMA-ligands in normal tissues is dependent on tumor load in patients with prostate cancer. Oncotarget. 2017;8:55094–55103. doi: 10.18632/oncotarget.19049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Demirci E, Sahin OE, Ocak M, Akovali B, Nematyazar J, Kabasakal L. Normal distribution pattern and physiological variants of 68Ga-PSMA-11 PET/CT imaging. Nucl Med Commun. 2016;37:1169–1179. doi: 10.1097/mnm.0000000000000566. [DOI] [PubMed] [Google Scholar]
- 15.Fendler WP, Eiber M, Beheshti M, Bomanji J, Ceci F, Cho S, et al. (68)Ga-PSMA PET/CT: Joint EANM and SNMMI procedure guideline for prostate cancer imaging: version 1.0. Eur J Nucl Med Mol Imaging. 2017;44:1014–1024. doi: 10.1007/s00259-017-3670-z. [DOI] [PubMed] [Google Scholar]
- 16.Eder M, Neels O, Muller M, Bauder-Wust U, Remde Y, Schafer M, et al. Novel preclinical and radiopharmaceutical aspects of [68Ga]Ga-PSMA-HBED-CC: a new PET tracer for imaging of prostate cancer. Pharmaceuticals. 2014;7:779–796. doi: 10.3390/ph7070779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gafita Andrei, Bieth Marie, Krönke Markus, Tetteh Giles, Navarro Fernando, Wang Hui, Günther Elisabeth, Menze Bjoern, Weber Wolfgang A., Eiber Matthias. qPSMA: Semiautomatic Software for Whole-Body Tumor Burden Assessment in Prostate Cancer Using 68Ga-PSMA11 PET/CT. Journal of Nuclear Medicine. 2019;60(9):1277–1283. doi: 10.2967/jnumed.118.224055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hirata K, Kobayashi K, Wong KP, Manabe O, Surmak A, Tamaki N, et al. A semi-automated technique determining the liver standardized uptake value reference for tumor delineation in FDG PET-CT. PLoS One. 2014;9:e105682. doi: 10.1371/journal.pone.0105682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Eiber M, Herrmann K, Calais J, Hadaschik B, Giesel FL, Hartenbach M, et al. Prostate cancer molecular imaging standardized evaluation (PROMISE): proposed miTNM classification for the interpretation of PSMA-Ligand PET/CT. J Nucl Med. 2018;59:469–478. doi: 10.2967/jnumed.117.198119. [DOI] [PubMed] [Google Scholar]
- 20.Hope TA, Truillet C, Ehman EC, Afshar-Oromieh A, Aggarwal R, Ryan CJ, et al. 68Ga-PSMA-11 PET imaging of response to androgen receptor inhibition: first human experience. J Nucl Med. 2017;58:81–84. doi: 10.2967/jnumed.116.181800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Afshar-Oromieh A, Debus N, Uhrig M, Hope TA, Evans MJ, Holland-Letz T, et al. Impact of long-term androgen deprivation therapy on PSMA ligand PET/CT in patients with castration-sensitive prostate cancer. European journal of nuclear medicine and molecular imaging. 2018;45:2045–2054. doi: 10.1007/s00259-018-4079-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jansen Bernard H.E., Kramer Gem M., Cysouw Matthijs C.F., Yaqub Maqsood M., de Keizer Bart, Lavalaye Jules, Booij Jan, Vargas Hebert Alberto, Morris Michael J., Vis André N., van Moorselaar Reindert J.A., Hoekstra Otto S., Boellaard Ronald, Oprea-Lager Daniela E. Healthy Tissue Uptake of 68Ga-Prostate-Specific Membrane Antigen, 18F-DCFPyL, 18F-Fluoromethylcholine, and 18F-Dihydrotestosterone. Journal of Nuclear Medicine. 2019;60(8):1111–1117. doi: 10.2967/jnumed.118.222505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li X, Rowe SP, Leal JP, Gorin MA, Allaf ME, Ross AE, et al. Semiquantitative parameters in PSMA-targeted PET imaging with (18)F-DCFPyL: variability in normal-organ uptake. J Nucl Med. 2017;58:942–946. doi: 10.2967/jnumed.116.179739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Seitz AK, Rauscher I, Haller B, Kronke M, Luther S, Heck MM, et al. Preliminary results on response assessment using (68)Ga-HBED-CC-PSMA PET/CT in patients with metastatic prostate cancer undergoing docetaxel chemotherapy. Eur J Nucl Med Mol Imaging. 2018;45:602–612. doi: 10.1007/s00259-017-3887-x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Please contact the corresponding author for data requests.