Abstract
Schizophrenia (SZ) is a multifactorial mental disorder, which has been associated with a number of environmental factors, such as hypoxia. Considering that numerous neural mechanisms depends on energetic supply (ATP synthesis), the maintenance of mitochondrial metabolism is essential to keep cellular balance and survival. Therefore, in the present work, we evaluated functional parameters related to mitochondrial function, namely calcium levels, mitochondrial membrane potential, redox homeostasis, high-energy compounds levels and oxygen consumption, in astrocytes from control (Wistar) and Spontaneously Hypertensive Rats (SHR) animals exposed both to chemical and gaseous hypoxia. We show that astrocytes after hypoxia presented depolarized mitochondria, disturbances in Ca2+ handling, destabilization in redox system and alterations in ATP, ADP, Pyruvate and Lactate levels, in addition to modification in NAD+/NADH ratio, and Nfe2l2 and Nrf1 expression. Interestingly, intrauterine hypoxia also induced augmentation in mitochondrial biogenesis and content. Altogether, our data suggest that hypoxia can induce mitochondrial deregulation and a decrease in energy metabolism in the most prevalent cell type in the brain, astrocytes. Since SHR are also considered an animal model of SZ, our results can likewise be related to their phenotypic alterations and, therefore, our work also allow an increase in the knowledge of this burdensome disorder.
Subject terms: Cellular neuroscience, Schizophrenia, Energy metabolism
Introduction
Schizophrenia (SZ) is a multifactorial mental disorder that is related to several hypotheses, including the neurodevelopment theory1,2. According to this concept, modifications in the brain machinery, caused by combined environmental factors at critical times, such as pregnancy2,3, could lead to changes in brain anatomy and dynamics and, consequently, in its function1. One of the main environmental factors related to SZ in clinical practice is hypoxia4–6. In 2002, Tyrone and colleagues reported abnormalities in brains from SZ patients that were exposed to intrauterine hypoxia from obstetric complications6. Moreover, it is known that intrauterine hypoxia seems to contribute to a reduction in the gray matter and an enlargement in the lateral ventricular zone3,6. Interestingly, studies have also shown that hypertension during pregnancy was well documented in records of women that become mothers of schizophrenic patients7–9. In agreement, a study designed by Mayoral and collaborators using rodents showed that exposure to chronic hypoxia may lead to loss of tissue volume, decreased myelination and increased ventricles10. Surprisingly, many of these abnormalities are also observed schizophrenic patients brains11–13.
Although hypoxia contributes to the occurrence of SZ4,9,14, it is necessary to investigate the role of mitochondria under this condition, in order to understand how brain cells could adapt and provide energy even with low oxygen voltages. Since mitochondria rely on O2 consumption for ATP production15, one might speculate that hypoxic conditions could, in turn, negatively affect all ATP-dependent processes contributing to SZ development16. Indeed, mitochondria dysfunction seems to play a crucial role in the SZ’s neurobiology, since it was already demonstrated changes in cytochrome C release, mitochondrial translocases expression and lipid peroxidation17–20 in addition to changes in genes associated to mitochondrial maintenance, volume, density, dynamics and metabolism19,21–32. Therefore, in the present work, we evaluated in astrocytes from Spontaneously Hypertensive Rats (SHR animals) (model of intrauterine hypoxia) and astrocytes exposed to chemical and gaseous hypoxia functional parameters related to mitochondrial function, namely calcium handling, mitochondrial membrane potential, redox homeostasis, oxygen consumption and ATP, ADP, Pyruvate, Lactate and NAD+/NADH levels, in addition to gene expression and protein levels related to mitochondrial metabolism. Astrocytes are a very important cell type because they not only give support for neurons, but also play an important role in neurodevelopment33–35 since they are involved in neuronal formation and development, orientation and migration of developing axons34,36.
Overall, our data reveal that astrocytes submitted to hypoxia have alterations in Ca2+ handling, mitochondrial Ca2+ uptake and mitochondrial membrane potential, besides an augmentation of redox homeostasis. Concomitantly, intrauterine and chemical hypoxia induce changes in ATP, ADP, Pyruvate and Lactate levels and NAD+/NADH ratio, despite an intensification of mitochondrial biogenesis and mitochondrial content.
Results
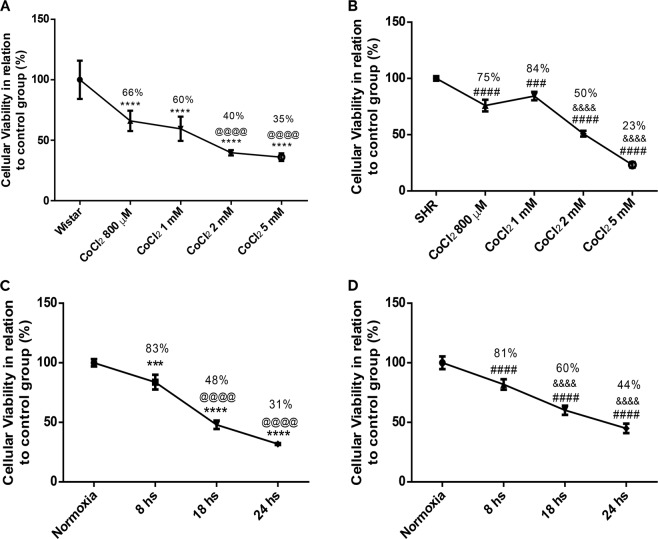
Reduction of astrocytes viability after chemical and gaseous hypoxias
To verify the effects of hypoxia on cellular viability submitted to various stimuli, we performed MTT assay. As shown in Fig. 1A, there is a dose-dependent reduction on the viability of Wistar astrocytes after CoCl2 treatments (800 µM, 1 mM, 2 mM and 5 mM, 24 hours) in relation to untreated/control group. The same effect was demonstrated in astrocytes from SHR animals (Fig. 1B). In Fig. 1C,D, we can observe that there is a time-dependent reduction of astrocytes survival from either Wistar or SHR animals after exposure to gaseous hypoxia (for 8, 18 and 24 hours).
Figure 1.
Cellular viability reduction in Wistar (A,C) and SHR (B,D) astrocytes after exposure to chemical and gaseous hypoxia. Cells were exposed to CoCl2 (800 µM, 1 mM, 2 mM and 5 mM for 24 hrs) and gaseous hypoxia (8, 18 and 24 hrs) and it was performed MTT test. Data is represented by mean ± SD, and it was normalized as percentage of control group (N = 4, in duplicates). Statistical analysis was performed using One-Way ANOVA followed by post-hoc Duncan. It was considered significant p < 0.05; ***p < 0.0001 and ****p < 0.00001, in relation to Wistar (both without treatment and normoxia group); @@@@p < 0.00001, in relation to Wistar cells exposed to both CoCl2 800 µM and 8 hrs of hypoxia; ###p < 0.0001 and ####p < 0.00001, in relation to SHR (both without treatment and normoxia group); &&&&p < 0.00001, in relation to SHR cells exposed to CoCl2 800 µM and 1 mM, and 8 hrs of hypoxia.
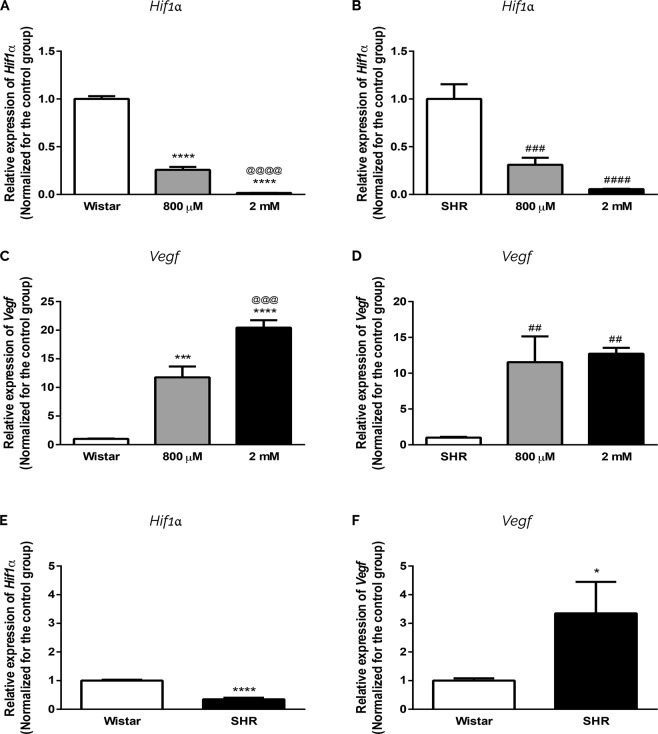
Induction of Hif1α pathway in astrocytes submitted to chemical and intrauterine hypoxias
To get evidences regarding the induction of hypoxia pathway, we investigated Hif1α and Vegf expression35,37–39. We demonstrated that CoCl2 leads to a significant diminishment in Hif1α expression in both Wistar and SHR astrocytes (Fig. 2A,B). However, CoCl2 treatment induces a significant augmentation in the expression of Vegf in Wistar astrocytes in a dose-dependent manner; the same happens in SHR group (Fig. 2C,D).
Figure 2.
Induction of Hif1α pathway in astrocytes submitted to intrauterine and chemical hypoxia. Astrocytes from both groups (Wistar: A,C; SHR: B,D) were exposed to 800 µM and 2 mM of CoCl2 for 24 hrs. Expression of Hif1α (A,C,E) and Vegf (B,D,F) is in relation to βActin. Data in graphs is the mean ± SD and the results were normalized as percentage of control group (N = 3, in duplicates). Statistical analysis was performed using One-Way ANOVA with post-hoc Duncan and Student’s t Test. It was considered significant, p < 0.05; *p < 0.01, ***p < 0.0001 and **** < 0.00001, in relation to Wistar group; @@@p < 0.0001 and @@@@p < 0.00001, in relation to Wistar 800 µM group; ##p < 0.001, ###p < 0.0001 and ####p < 0.0001, in relation to SHR group.
Comparing the expression of Hif1α between untreated Wistar and SHR astrocytes, we also observe a significant decrease in Hif1α expression in cells exposed to intrauterine hypoxia (Fig. 2E). Concomitantly, and as expected, there is a significant increase in Vegf expression in SHR astrocytes (Fig. 2F).
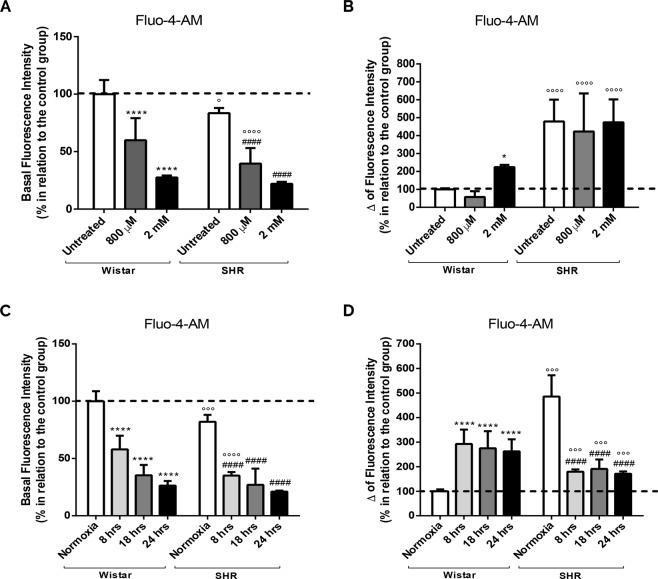
Intrauterine, chemical and gaseous hypoxias induce changes in Ca2+ handling and mitochondrial Ca2+ uptake
Because mitochondrial function and ATP synthesis relies on oxidative phosphorylation capacity40, and modification in the transport of electron and the proton motive force can affect the transport of ions, such as Ca2+ 41, we evaluated the Ca2+ homeostasis (Fig. 3). We can notice that astrocytes from SHR present lower cytosolic Ca2+ level in comparison to Wistar’s (untreated groups) (Fig. 3A). Curiously, there is a significant reduction in cytosolic Ca2+ level, in relation to untreated cells, after CoCl2 exposure in both groups as well (Fig. 3A). In the presence of FCCP, the results show a 5-fold increase in cytosolic Ca2+ level in untreated SHR astrocytes (Fig. 3B), suggesting that mitochondria from SHR can uptake more Ca2+. Chemical hypoxia also induced a significant release of Ca2+ to cytosol in Wistar astrocytes, but only when CoCl2 was added at 2 mM (intense hypoxia) (Fig. 3B). On the contrary, SHR astrocytes exposed to chemical hypoxia (800 µM and 2 mM) does not increase Ca2+ uptake by mitochondria (Fig. 3B).
Figure 3.
Reduction of cytosolic Ca2+ after chemical, gaseous and intrauterine hypoxia and increased calcium uptake by SHR mitochondria. Astrocytes from both groups (Wistar and SHR) were exposed to CoCl2 (800 µM and 2 mM, for 24 hrs) and gaseous hypoxia (for 8, 18 and 24 hrs). The histograms represent the basal level of cytosolic Ca2+ after incubation with Fluo-4-AM (10 µM, 1 hr) (A,C) and after stimulation with FCCP (5 µM) (Δ of fluorescence intensity) (B,D). Data is represented by mean ± SD, and the results were normalized as percentage of control group (N = 4, in duplicates). Statistical analysis was performed using Two-Way ANOVA followed by post-hoc Duncan. It was considered significant p < 0.05; *p < 0.01 and ****p < 0.00001, in relation to untreated and normoxia Wistar group; ####p < 0.00001, in relation to untreated and normoxia SHR group; °p < 0.01, °°°p < 0.0001 and °°°°p < 0.00001, in relation to the respective Wistar group.
In order to compare the effect of CoCl2 treatment with the absence of oxygen, we decided to induce gaseous hypoxia. Corroborating our previous data, there is a reduction in the cytosolic Ca2+ in untreated SHR astrocytes when compared to Wistar’s (Fig. 3C). Interestingly, gaseous hypoxia also induces a decrease in cytosolic Ca2+ in both Wistar and SHR groups (Fig. 3C). Still, when astrocytes are challenged with FCCP, we get not only an increase in the fluorescent signal in untreated SHR astrocytes when compared to Wistar astrocytes, but also an augmentation in both groups after gaseous hypoxia (Fig. 3D). Surprisingly, SHR astrocytes release less Ca2+ to cytosol than Wistar astrocytes. These records suggest that gaseous hypoxia does not induce Ca2+ uptake by SHR mitochondria.
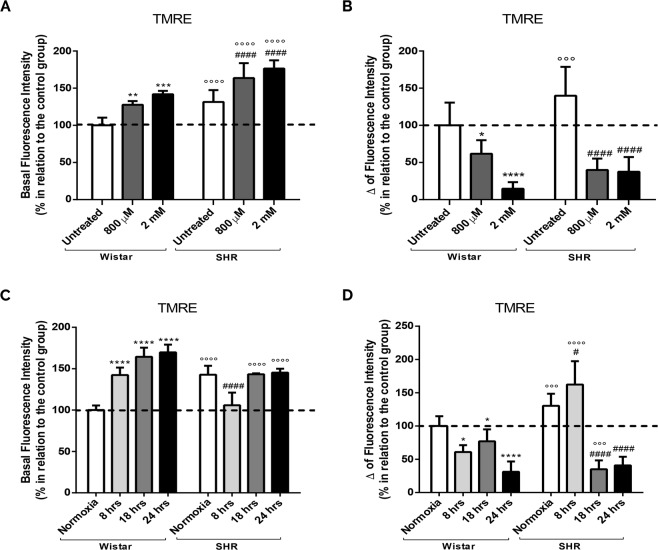
Mitochondria depolarization after intrauterine, chemical and gaseous hypoxias
To verify if hypoxia and mitochondrial Ca2+ uptake was influencing mitochondrial membrane potential, cells were loaded with TMRE. SHR astrocytes show a significant increase in cytosolic TMRE in comparison to untreated Wistar astrocytes (Fig. 4A). Similarly, CoCl2 also induce a significant increase in cytosolic TMRE (Fig. 4A), meaning that less TMRE are being uptake by mitochondria after intrauterine and chemical hypoxia.
Figure 4.
Mitochondrial membrane potential depolarization after chemical, gaseous and intrauterine hypoxia. Astrocytes from both groups (Wistar and SHR) were exposed to CoCl2 (800 µM and 2 mM, for 24 hrs) and gaseous hypoxia (for 8, 18 and 24 hrs). The histograms represent the basal level of TMRE fluorescence (500 nM, 1 hr) (A,C) and after stimulation with FCCP (5 µM) (Δ fluorescence intensity) (B,D). Data is represented by mean ± SD, and the results were normalized as percentage of control group (N = 4, in duplicates). Statistical analysis was performed using Two-Way ANOVA followed by post-hoc Duncan. It was considered significant p < 0.05; *p < 0.01, ***p < 0.0001 and ****p < 0.00001, in relation to untreated and normoxia Wistar group; ####p < 0.00001, in relation to untreated and normoxia SHR group; °°°p < 0.0001 and °°°°p < 0.00001, in relation to the respective Wistar group.
Thus, in order to check this hypothesis, all cells were challenged with FCCP. Figure 4B shows that there is an increase in TMRE cytosolic fluorescence in SHR astrocytes in relation to untreated Wistar, indicating a greater capacity of SHR mitochondria to TMRE retain. Curiously, after CoCl2 treatment, astrocytes from both Wistar and SHR animals show a lower fluorescent signal (Fig. 4B), suggesting a massive mitochondrial depolarization.
After SHR and Wistar astrocytes were exposed to 0% of O2, we also observe an increase in cytosolic TMRE signal in Wistar astrocytes in relation to normoxia, but there is a reduction on the TMRE fluorescence in SHR astrocytes after 8 hours and no differences is found after 18 hours and 24 hours (Fig. 4C). After FCCP challenge, we can observer that there is less TMRE being sequestered by Wistar astrocytes mitochondria; the same result is seen in SHR astrocytes after 18 and 24 hours (Fig. 4D). Curiously, after 8 hours of lower O2, FCCP induces a higher release of mitochondrial TMRE to cytosol, suggesting that mild gaseous hypoxia, on the other hand, can lead to a greater uptake of calcium by mitochondria.
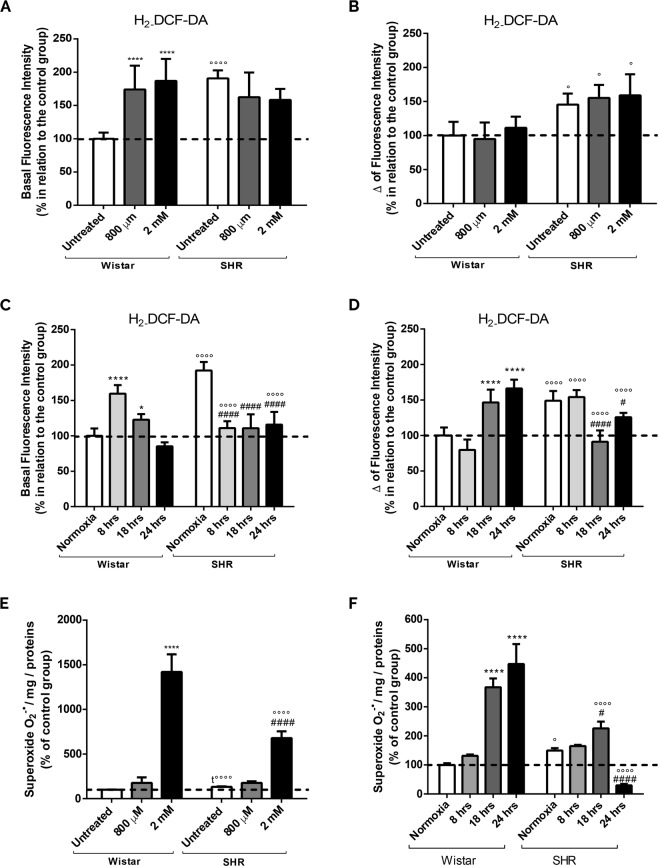
Increased ROS production in astrocytes exposed to intrauterine, chemical and gaseous hypoxias
We further decided to investigate whether redox homeostasis was also disturbed in our cellular systems. There is a significant increase in ROS (indicated by CM-H2DCFDA fluorescence) in untreated SHR astrocytes in relation to Wistar cells (Fig. 5A), indicating that intrauterine hypoxia is able to induce a significant increment in ROS production. However, CoCl2 treatment just leads to a significant ROS augmentation in Wistar astrocytes (Fig. 5A). Our data may be related to the fact that astrocytes from SHR animals already present an increase in ROS.
Figure 5.
Augmentation of oxidative stress after chemical, gaseous and intrauterine hypoxia. Astrocytes from both groups (Wistar and SHR) were exposed to CoCl2 (800 µM and 2 mM, for 24 hrs) and gaseous hypoxia (8, 18 and 24 hrs). Representative histograms of basal H2DCF-DA (20 µM for 30 min) fluorescence (A,C), and after stimulation with FCCP (5 µM) (Δ fluorescence intensity) (B,D). (E,F) Representative histograms of the kinetic slope of the O2°− levels after chemical (E) and gaseous (F) hypoxia in cells loaded with Mitosox (5 µM, 10 min). Data is represented by mean ± SD, and the results were normalized as percentage of control group (N = 4, in duplicates). Statistical analysis was performed using Two-Way ANOVA followed by post-hoc Duncan or Student’s t Test. It was considered significant p < 0.05; *p < 0.01 and ****p < 0.00001 in relation to untreated and normoxia Wistar group; #p < 0.01 and ####p < 0.00001, in relation to untreated and normoxia SHR group; °p < 0.01, °°°°p < 0.00001 and t°°°°p < 0.00001, in relation to the respective Wistar group.
To check an additional increase in ROS, we performed the experiments in the presence of FCCP (Fig. 5B). We get no difference in Wistar or SHR group between treatments, but there is a significant increment in SHR astrocytes fluorescence signal only when compared to the respectively Wistar treated group. This result indicates that intrauterine and chemical hypoxias promote an increase in ROS production that is not affected by further hypoxic stimuli.
Concerning to gaseous hypoxia, as shown in Fig. 5C, there is a significant ROS production in astrocytes from SHR strain when compared to Wistar group (normoxia) (Fig. 5A); data resemble those with CoCl2 treatment. We also detect that Wistar astrocytes exposed to gaseous hypoxia (8 and 18 hours) have an increase in the basal fluorescence in comparison to normoxia group. On the other hand, astrocytes from SHR animals present a significant reduction in ROS production when exposed to gaseous hypoxia in comparison to normoxia condition. In the presence of FCCP, we observe an increase in DCF signal in Wistar astrocytes after 18 and 24 hours of hypoxia (Fig. 5D). Moreover, in the SHR group, the opposite effect is detected, meaning that FCCP does not induce any increase in ROS after hypoxia.
In order to identify superoxide (O2°−) formation, cells were loaded with Mitosox. Figure 5E shows a significant intensification in the fluorescent slope in SHR astrocytes when compared to Wistar cells (untreated). Additionally, there is a significant increase in O2°− levels in Wistar and SHR astrocytes after intense chemical hypoxia compared to its respectively untreated group (Fig. 5E). In agreement, an intense gaseous hypoxia (18 hours) also induces a significant enhancement of O2°− in astrocytes from Wistar and SHR animals (Fig. 5F). Strangely, after 24 hours of 0% of O2, we have a decrease in the fluorescence signal in SHR astrocytes when compared to SHR.
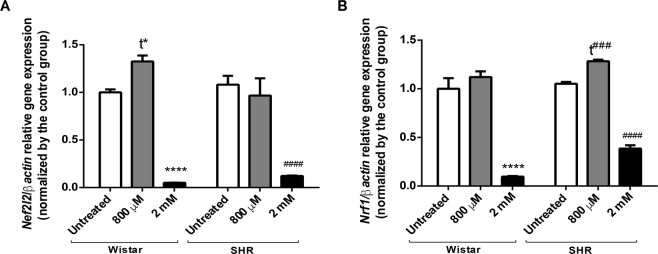
Decreased antioxidant defense and reduced expression of key metabolic gene regulators upon intense chemical hypoxia
Because redox homeostasis is deregulated after hypoxia, we further investigated Nfe2l2 expression (Fig. 6A). Curiously, there is no significant change in its expression in SHR astrocytes when compared to astrocytes from Wistar rats. However, there is a significant decline in Nfe2l2 expression after intense chemical hypoxia in both groups. Interestingly, we verify an augmentation of Nfe2l2 expression when Wistar astrocytes are exposed to 800 µM of CoCl2, suggesting an increase in antioxidant defense after moderate hypoxia. This outcome strongly suggests that a severe chemical hypoxia could induce higher levels of ROS, which in turn leads to a significant decrease in Nef2l2 expression42–44.
Figure 6.
Changes in Nfe2l2 and Nrf-1 expression after chemical hypoxia. Relative expression of Nfe2l2 (A) and Nrf-1 (B) in astrocytes from both Wistar and SHR animals treated with CoCl2 (800 µM and 2 mM) for 24 hrs. Data is represented by mean ± SD. Results were normalized as percentage of control group (N = 3, in duplicates). Statistical analysis was performed using Two-Way ANOVA followed by post-hoc Duncan or Student’s t Test. It was considered significant p < 0.05; ****p < 0.00001 and t* = p < 0.01, in relation to untreated Wistar group; ####p < 0.00001, t### = p < 0.0001, in relation to untreated SHR group.
Concerning to Nrf-145 expression, there is no differences between Wistar and SHR untreated groups. As occurred with Nfe2l2 expression, Nrf-1 expression diminishes after intense hypoxia (Fig. 6B). On the contrary, there is a significant increase in Nrf-1 expression after mild hypoxia in SHR cells, which may be related to a possible adaptation to moderate hypoxia, where ROS levels are increased and could be able to stimulate Nrf1 expression.
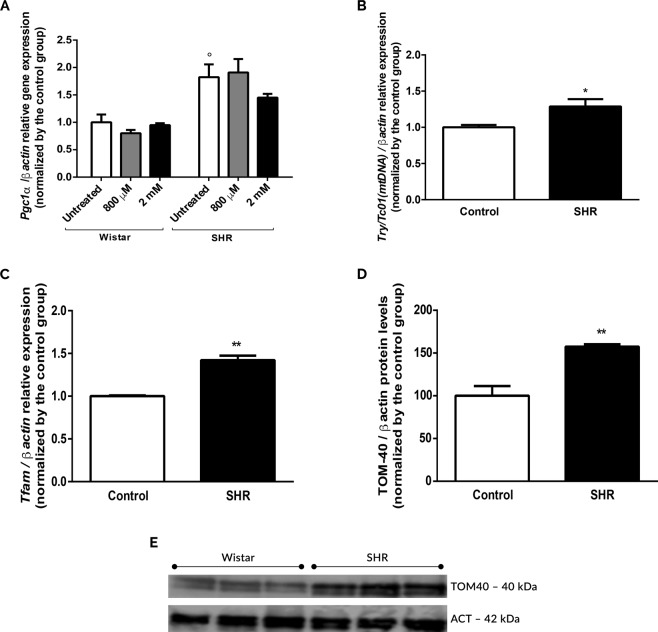
Enhancement of mitochondrial biogenesis and content in SHR astrocytes
In order to evaluate changes in mitochondrial content, we assessed Pgc1-α, Mtco1 and Tfam expression and TOM-40 levels46–52. As shown in Fig. 7A, there is a significant increase in Pgc1-α expression in astrocytes from SHR animals in relation to Wistar’s cells. Curiously, CoCl2 does not induce any significant changes (Fig. 7A). Corroborating this data, we demonstrated that SHR astrocytes show a significant increase in Mtco153–56 (Fig. 7B) and Tfam57–61 expressions in SHR astrocytes (Fig. 7C). Concomitantly, we detect a significant increment in TOM-40 levels in SHR astrocytes (Fig. 7D,E). All these data reinforce that, indeed, an increased mitochondrial biogenesis as well as mitochondrial content in SHR astrocytes could be related to changes in mitochondrial metabolism.
Figure 7.
Increased mitochondrial biogenesis and mitochondria copy number in SHR astrocytes. Relative expression of Pgc-1α (A), Mtco1 (mtDNA) (B) and Tfam (C), and TOM-40 levels (D,E) in astrocytes from Wistar and SHR animals in the presence and absence of CoCl2 treatment (800 µM and 2 mM, for 24 hrs). Data in graphs are the mean ± SD and the results were normalized as percentage of control group (N = 4, in duplicates). (E) is a cropped image; the uncropped blot is included in Supplementary Information. Statistical analysis was performed using Two-Way ANOVA followed by post-hoc Duncan or Student’s t Test. It was considered significant, p < 0.05; °p < 0.01, *p < 0.01 and **p < 0.001 in relation to Wistar group.
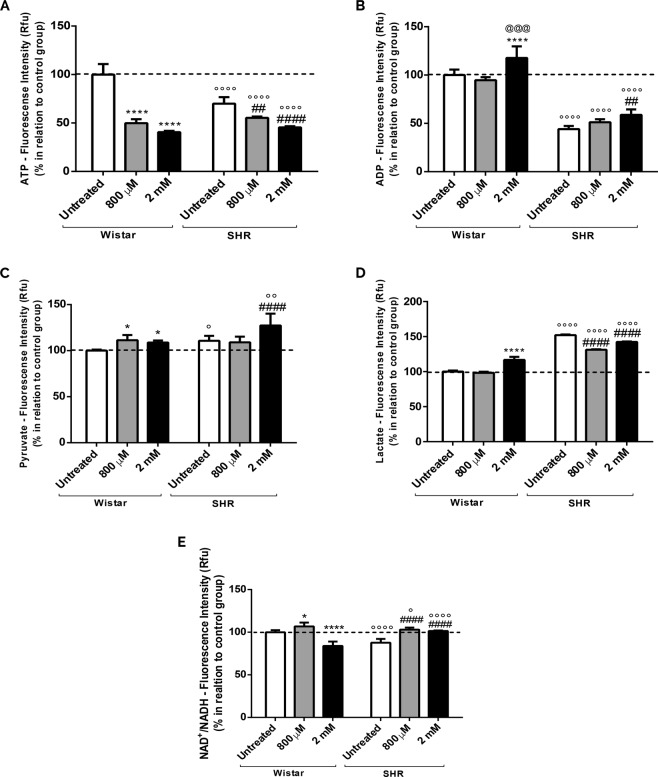
Intrauterine and chemical hypoxias lead to a decreased energy metabolism
Since we demonstrated that astrocytes submitted to hypoxia present changes in calcium handling, mitochondria membrane potential and redox homeostasis, in addition to oxygen consumption (See Supplementary Fig. 2SS) and lipid peroxidation (See Supplementary Fig. 1SS), we investigated whether the increase in mitochondrial biogenesis and content could represent a compensation to keep cellular energy metabolism. As presented in Fig. 8A, there is a decrease in the ATP production in SHR astrocytes when compared to the untreated Wistar group (Fig. 8A). On top of that, when cells are exposed to chemical hypoxia, ATP levels are drastically reduced (Fig. 8A). Regarding to ADP levels, we note a reduction in SHR astrocytes in relation to the untreated Wistar group. On the other hand, after intense chemical hypoxia, there is a significant augmentation in ADP (Fig. 8B).
Figure 8.
Alterations in high-energy compounds (ATP, ADP, Pyruvate, Lactate, NAD+ and NADH) after intrauterine and chemical hypoxia. Astrocytes were treated with CoCl2 (800 µM and 2 mM) for 24 hrs. (A) Measurement of ATP; (B) ADP levels; (C) Pyruvate analysis; (D) Evaluation of Lactate; (E) NAD+/NADH ratio. Data in graphs are the mean ± SD and the results were normalized as percentage of control group (N = 3, in duplicates). Statistical analysis was performed using Two-Way ANOVA followed by post-hoc Duncan and it was considered significant p < 0.05; ****p < 0.00001 and *p < 0.01, in relation to untreated Wistar group; @@@p < 0.001, in relation to Wistar 800 µM group; ####p < 0.00001 and ##p < 0.001, in relation to untreated SHR group; °p < 0.01 and °°°°p < 0.00001, in relation to the respective Wistar group.
In order to verify if changes in ATP and ADP are accompanied by changes in intermediate metabolic products, Pyruvate and Lactate levels were measured. Figure 8C show an increase in Pyruvate on SHR astrocytes (untreated) in relation to Wistar cells. Curiously, chemical hypoxia induces a significant enrichment in Pyruvate in both Wistar and SHR astrocytes (Fig. 8C), indicating that either SHR astrocytes can have an increase in glycolytic pathway, or Pyruvate is being less converted into acetyl-CoA.
As an increase in Pyruvate may be favoring Lactate production, and hypoxia can induce an increase in lactate dehydrogenase A activity35,62,63, we also analyzed Lactate levels. We observe that there is a significant increase in Lactate production in SHR astrocytes when compared to Wistar untreated cells (Fig. 8D). Interestingly, only high-intensity chemical hypoxia was able to promote an augmentation in Lactate production in Wistar astrocytes.
To evaluate whether hypoxia is influencing the aerobic pathways through changes in high-energy compounds, we evaluated the levels of NAD+ and NADH. There is a significant reduction in the ratio NAD+/NADH in SHR cells in comparison to Wistar’s; the same result is obtained in Wistar astrocytes exposed to intense chemical hypoxia. On the other hand, moderate hypoxia on Wistar astrocytes, as well as moderate and intense hypoxia on SHR astrocytes, lead to a significant increment in the NAD+/NADH (Fig. 8E).
The compilation of all these data show that there is an energetic disturbance in SHR, despite increased biogenesis, and a worsening of the situation is noticed after exposure to intense hypoxia. Interestingly, the same occurs after induction of chemical hypoxia in Wistar astrocytes.
Discussion
Along this manuscript, we showed that hypoxia (intrauterine, chemical and gaseous) could induce mitochondrial deregulation and consequently diminishment in energy metabolism in primary astrocytes. Curiously, astrocytes submitted to intrauterine hypoxia only, seem to activate compensatory mechanisms, namely mitochondrial biogenesis. Since SHR are described in literature as a SZ model, we further speculate that our data can be likewise related to phenotypic alterations and neuropathological features observed in these animals.
In our systems, we firstly investigated if CoCl2 treatment would be capable of hypoxia induction; thus we evaluated Hif1α expression35,64–69. Surprisingly, we observed a significant reduction in Hif1α (Fig. 2), that could be related to the presence of atmospheric oxygen leading to Hif1α degradation70,71. Indeed, reports mention that this degradation is fast70 and only Hif1α would not be sufficient to indicate hypoxia activation. Therefore, we evaluated the vascular endothelial growth factor (Vegf), which is the most abundant secondary element after the accumulation and activation of Hif1α37–39. We observed a significant increase in Vegf expression after intrauterine and chemical hypoxias, demonstrating that SHR and CoCl2 stimulation are capable of hypoxia activation.
To understand the processes in which hypoxia could be able to cause abnormalities in mitochondrial function, we used several methods to evaluate mitochondrial metabolism, including the evaluation of Ca2+ homeostasis (Fig. 3). Concerning to that, our data show that SHR astrocytes, in comparison to Wistar’s, presented less Ca2+ in the cytosol, but more Ca2+ were release from mitochondria after FCCP. Interestingly, it was described that periods of intrauterine hypoxia have the ability to modify Ca2+ levels causing ion accumulation in the cytosol and bringing damage to the developing fetus72. Concomitantly, chemical and gaseous hypoxias also induced an increase in mitochondrial Ca2+ uptake (Fig. 3). Such process would act as a protective factor avoiding accumulation of Ca2+ in the cytosol and the activation of cell death72,73. Consequently, the intrauterine (SHR), chemical and gaseous hypoxias could be inducing an increase in mitochondrial Ca2+ uptake as a protective mechanism. This data was not yet observed, and it is being reported herein for the first time.
Since an increase in mitochondrial Ca2+ can also be detrimental, since leads to a deregulation of mitochondrial membrane potential58 favouring the exit of cytochrome C74–77, we further evaluated mitochondrial membrane potential (∆Ψm) in our cellular models. We observed that all kind of hypoxias tested herein induced changes in mitochondrial polarization (Fig. 4). Therefore, the higher retention of Ca2+ in the mitochondrial matrix can be due its membrane potential74–76. Curiously, we detected, after FCCP, an increase in TMRE cytosolic fluorescence in SHR cells in relation to untreated Wistar astrocytes, even though these cells present more TMRE in the cytosol (Fig. 4). This result seems contradictory, although it can imply that SHR astrocytes have more mitochondria. Consequently, the increased release of TMRE after FCCP addition could be a reflection of mitochondria augmentation40,41,47,48. Specifically after CoCl2, there is a significant decrease in TMRE fluorescent signal after FCCP, indicating that organelles are depolarized; similar results were obtained after cells were exposed to 0% of O2 (Fig. 4). Conversely, this result was not obtained in SHR astrocytes after 8 hours of hypoxia. This event may suggest that short periods of gaseous hypoxia could favour polarization of mitochondria instead. Turcotte et al. using cells resistant to hypoxia demonstrated that this cell type suffers less from changes caused by hypoxia and tends to ensure ∆Ψm modifications78. Thus, one can suggest that SHR astrocytes could be more tolerant to gaseous hypoxia because they have already experienced an intrauterine lack of O2 as a preconditioning status.
To a better understanding of mitochondrial function after hypoxia, we also evaluated oxidative stress in astrocytes. As we can observe in Fig. 5, intrauterine hypoxia and CoCl2 treatment on Wistar astrocytes induced a significant increment in the DCF signal; chemical hypoxia did not interfere in SHR ROS production. In fact, some studies have proposed that SHR strain is inclined to have genetically based modifications in the redox system, which seems to be correlated with long periods of intrauterine hypoxia79. Curiously, gaseous hypoxia in SHR astrocytes decreased DCF signal. In this case, it is hypothesized that a severe hypoxia could modify the redox homeostasis leading the cell to a metabolically collapse, decreasing the DCF signal80–82. Alternatively, it can induce an increase in antioxidant capacity, which would decrease ROS. In fact, it was previously described that there is augmentation in antioxidant enzymes (catalase, GSH and SOD) in varied cell types exposed to hypoxia83–85.
Because DCF is capable of providing data about general ROS synthesis, we sequentially evaluated Mitosox fluorescence (in order to check O2°− levels) (Fig. 5). Equally, astrocytes from SHR presented a significant intensification in O2°− production. In addition, we detected an increase in O2°− in Wistar and SHR astrocytes exposed to intense chemical hypoxia. However, after gaseous hypoxia, we only observed an increase in Mitosox fluorescence in Wistar cells after 18 and 24 hours, and after 18 hours in SHR groups. The drastic reduction of Mitosox after 24 hours of gaseous hypoxia, can be due to modifications in redox metabolism after long periods of hypoxia (intrauterine)81,82 or, alternatively, to a mitochondrial destabilization and even metabolic collapse, that could in part, explain the less superoxide synthesis82,83.
To check if intrauterine hypoxia could also lead to an increase in lipid peroxidation, which would be expected since we demonstrated an enrichment in DCF and Mitosox signals, we evaluated malondialdehyde (MDA) and 4-hydroxynonenal (HNE) levels (supplementary material)86–89 (See Supplementary Fig. 1SS). We revealed that SHR astrocytes presented a significant increment in MDA and 4-HNE levels in comparison to control cells. Hence, SHR astrocytes could be, in fact, particularly susceptible to changes in mitochondrial function and metabolism because they are continuously exposed to modification of redox status79,81.
Taking redox homeostasis data altogether, we latter checked changes in Nef2l2 and Nrf1 expression, genes directly implicated in cellular detoxifying systems42–45,90 and in the regulation and transcription of several nuclear-encoded electron transport chain proteins45, respectively. Interestingly, no changes were detected between Wistar and SHR groups regarding Nef2l2 and Nrf1 (Fig. 6). Though, there was an increase in Nef2l2 expression in Wistar cells treated with 800 µM CoCl2 (moderate hypoxia), but not in SHR. Interestingly, it was already demonstrated that short periods of hypoxia could favour the antioxidant response64,81. Looking to the groups exposed to intense hypoxia, we detected a drastic reduction in both Nef2l2 and Nrf1 expression in Wistar and SHR astrocytes (Fig. 6). Remarkably, increased levels of ROS have been related to the fall in Nfe2l2 levels in some cell types, such as epithelial and cardiac42–44 in the sense that during intense oxidative stress, there is a failure in the translocation of the gene to its binding site in the cell nucleus, reducing the transcription of secondary factors of the antioxidant cascade44.
Recalling mitochondrial deregulation, we postulated that perhaps intrauterine hypoxia could increase mitochondrial content and biogenesis in astrocytes to compensate changes in calcium handling, mitochondrial potential and redox homeostasis. Corroborating our hypothesis, we showed that SHR astrocytes presented a significant increase in Pgc1-α expression, the central regulator of mitochondrial biogenesis46,47 (Fig. 7), indicating that SHR strain would be predisposed to mitochondrial biogenesis. Concordantly, there was a significant increase in mitochondrial encoded complex IV subunit cytochrome c oxidase I (Mtco1)53,56,91 expression, a candidate gene downstream of Pgc-1α, and in Tfam expression, a transcription factor that activates transcription of mtDNA61 and is involved with mitochondrial formation and replication57–61. Corroborating our findings, we also showed a significant increase in TOM-40 level, a mitochondrial translocase of the outer membrane used for estimate the amount of mitochondrial in different cell types91–93 (Fig. 7). Interestingly, it was already demonstrated alterations in mtDNA copy number in SZ too94–96 as an association between mtDNA mutation and cognitive deficits in SZ’s subjects97. Since the hypoxia-effect on mitochondrial biogenesis was never described previously in SHR astrocytes, our data is the first that suggest that SHR cells could compensate mitochondrial dysfunction induced by intrauterine hypoxia by increasing mitochondrial content.
Due to all these findings, we also evaluated oxygen consumption in our cellular models (See Supplementary Fig. 2SS). The analysis revealed that there was no change in O2 consumption between untreated Wistar and SHR astrocytes. This result indicates that SHR astrocytes need more mitochondria to keep the same rate of oxygen consumption. Nonetheless, we saw a decrease in respiration in Wistar cells exposed to moderate chemical hypoxia and an increase in the O2 consumption in the astrocytes from both groups exposed to intense chemical hypoxia. Thereupon, we suggest that the elevated respiration rate, along with higher O2°− concentration, can be, in fact, related to uncoupled mitochondria. Consequently, the organelle would consume more O2 pursuing to keep cellular energy metabolism98,99.
Afterwards, we evaluated the metabolites responsible for the regulation of cell’s energy pathways, named ATP, ADP, Pyruvate, Lactate, NAD+ and NADH levels. As shown in Fig. 8, there was a reduction in ATP levels in SHR cells in relation to controls. Interestingly, chemical hypoxia induces a further decrease in ATP in both Wistar and SHR astrocytes. It is worthy to mention that in the context of SZ, changes in mitochondrial energetic metabolism, including a decrease in ATP, was already described100–103. When we observed ADP, we also detected a decrease in SHR cells in relation to Wistar’s. Despite of that, intense chemical hypoxia led to higher ADP in both groups. This outcome can suggest that these cells can be consuming the available ATP to modify energetic pathways, such as the blockage of Pyruvate Dehydrogenase activity64. Besides, it is known that hypoxia induces inactivation of pyruvate dehydrogenase and a further reduction in the acetyl-coa supply, decreasing the activity of tricarboxylic acid cycle (TCA) and oxidative phosphorylation35,62,64. It was also demonstrated that hypoxia increases the activity of enzymes from glycolytic pathway in attempt to keep energetic requirement35,62. Consequently, Pyruvate levels would increase. Indeed, we saw a significant increase in Pyruvate in astrocytes exposed either to intrauterine or chemical hypoxia. Thus, the reduction of ATP and the increase in ADP can be related to the increase of Pyruvate induced by hypoxia35,62,63.
Moreover, it was already demonstrated that hypoxia induces an increase in the activity of Lactate Dehydrogenase A62 favouring Lactate synthesis. Concerning to that, our data shows a significant increase in Lactate levels in untreated SHR cells in relation to Wistar astrocytes (Fig. 8). Specifically, in Wistar group, only intense hypoxia was able to cause this effect. Interestingly, a cohort study with SZ’s persons presented a correlation between negative symptoms, increase in lactate levels and function of mitochondrial complex III104. Moreover, it was recently described that there is an increase in lactate levels in SZ’s subjects’ brain, in DISC1 (disrupted in schizophrenia 1) mouse model, as well as in inducible pluripotent stem cells (iPSCs) from a schizophrenia individuals105. As well, our results demonstrate that SHR astrocytes submitted to CoCl2 treatment present a decrease in Lactate in relation to untreated SHR cells, indicating that Lactate could be reappointed to other intracellular signalling pathways. It is known that under intense hypoxia a great amount of Lactate is extruded or deviated to glutamate synthesis106–108. In this case, hypoxia can promote the activation of monocarboxylate transporter 4 (MCT4), which transports the Lactate out of the cell106. Furthermore, it can be suggested that higher levels of Lactate could provide more substrates for the conversion of glutamine to glutamate and could increase glutamate oxidation and its conversion into alpha-ketoglutarate; both processes are recognized as the essential functions to astrocytes106–108.
We further demonstrated that after intrauterine and intense chemical hypoxia in Wistar cells there was a significant decrease in the NAD+/NADH ratio, result that can be due to an increased reconversion of Lactate into Pyruvate (Fig. 8). Additionally, knowing that mitochondria under hypoxia is dysfunctional, the lower formation of NAD+ and a consequent increase in NADH can be due to the incapability of its reconversion109,110. On the contrary, SHR astrocytes submitted to intense chemical hypoxia, presented an augmentation of NAD+/NADH ratio. In fact, the decrease in NADH could be an attempt of Pyruvate formation, from Lactate, to achieve a higher production of ATP108. Moreover, this can reflect an increased activity of the respiratory chain that, in turn, consume more NADH (decreasing its levels) and produce more NAD+ 109,110. Because there is no ATP production under this situation, even after mitochondrial biogenesis, it is possible that the organelles are uncoupled.
Altogether, this work brings new insights into how hypoxia is connected to mitochondrial deregulation, and how intrauterine hypoxia could be related to neuronal dysfunction, since SHR is an animal model of SZ. Consequently, we do hope that our results can contribute to new findings regarding psychiatry disorders target therapy.
Material and Methods
Animal models
For the present study, our group used Wistar (control group) and SHR (Spontaneous Hypertensive Rats) pups. Colonies of both lines were maintained at the housing facility of Santa Casa de São Paulo School of Medical Sciences; the first breeding pairs were acquired from University of São Paulo (USP) (Veterinary Medicine Faculty), São Paulo, Brazil.
All adult animals were housed in number of five in plastic cages measuring 33 × 40 × 17 cm. They were kept in rooms with ventilation and temperature control system (20 to 23 °C) in light-dark cycle of 12/12 hours; light phase starts at 6:30 am. The mating method for both strains was “harem”; it means that for each male, two females were added in the cage. Water and food were provided ad libitum.
All the experimental procedures, including euthanasia and decapitation, were performed according to the ethical principles for the use of laboratory animals described by the Brazilian Society for Laboratory Animal Science (SBCAL), National Council for Control of Animal Experimentation (CONCEA), Arouca Law (approved in 2008) and the Ethics Committee on Animal Use of Santa Casa de São Paulo School of Medical Sciences (CEUA Santa Casa). Our experimental protocols were carried out in accordance with the guidelines and they were approved by the number 003/15 by our Institutional Committee (President of CEUA Santa Casa, Dra. Fernanda Vasquez Daud).
Spontaneously hypertensive rat (SHR)
SHR is a genetically hypertensive animal characterized by an increase in the arterial tension111 and, as a result, SHR females impose an intrauterine hypoxia situation to their embryos112,113. Curiously, several phenotypic hallmarks observed in newborn rats are also shown in humans when they are exposed to intrauterine hypoxic conditions due to their hypertensive mothers, named growth retardation, neurodevelopmental impairment and cognitive deficits112,113. Concomitantly, SHR females present an abnormal expression of placental proteins and deregulation of the renin-angiotensin-aldosterone system, as described in hypertensive women114,115. Thus, it is agreed that SHR rats are often used to mimic gestational hypertension112,116.
Due to modifications in neural circuit, as well as behavioral phenotypes present in these rats, SHR started to be used to investigate psychiatric disorders such as SZ117. Indeed, SHRs present hyper locomotion (correlated with SZ positive symptoms), social interaction deficit (associated to SZ negative symptoms) and decreased contextual fear conditioning, which denotes cognitive symptoms and diminished emotional processing. In addition, SHR show increased rearing behaviour (associated with positive symptoms in human beings) and decreased performance in prepulse inhibition of startle (PPI) (a pre-attentional information processing test corresponding to positive/cognitive symptoms in humans)115–124. PPI model has been used to study sensorimotor deficits related to SZ124,125. Specifically, regarding the augmentation in rearing phenotype in social context, it is also considered an antisocial behaviour, indicating that the animal prefers to explore the environment to have to interact with an unfamiliar rodent114,115. Therefore, it can be interpreted as a negative symptom as well.
It is worth mentioning that all phenotypes presented by SHR were pharmacologically validated for SZ, since they were reversed with antipsychotics used in the clinic for patients, but not with psych stimulant drugs, mood stabilizers or anxiety modulators114,123. These findings show not only that SHR present a hypofunctional prefrontal cortex and a hyperfunctional nucleus accumbens, but also reinforce the intersections between contextual fear conditioning deficit and emotional processing abnormalities in SZ, strengthening the use of SHR as an animal model of this disorder.
Recently, an article to validate behavioral variables observed in the SHR strain that could act as a general index of schizophrenic behavior was published126. Interestingly, all the behavioural assessments were re-evaluated and tested for schizophrenia-like trait (SLT) indices (such as locomotor activity, social interaction, PPI and Fear Conditioning test). It was found that these behavioural parameters revealed a SLT as a continuum, a result according to the nature of SZ in humans126. A matter of great importance is the fact that a deficit in emotional memory of SHR114,117,118 is reverted by antipsychotics114. Interestingly, these drugs are also used in SZ therapy, suggesting that the SHR strain could be used as a model for SZ-associated emotional memory deficits117. On the contrary, and in agreement with SHR as a SZ-model, SHR animals treated with amphetamine present an exacerbation of overall symptoms linked to SZ114. Thus, experimental evidences reinforce the behavioral profile of SHR associated with SZ. Neurochemical evidences also suggest that SHR present SZ-related features127. Actually, they present amygdala activation and prefrontal cortex deficits126,128–131, in addition to an increase in the release of dopamine induced by amphetamine into striatum130. Similarly, there is a decrease in the expression of dopaminergic receptors of type D4 (belonging to the family of D2 receptors) in the cortex of SZ carriers and SHR rats131, and an increase in dopamine transporters (DAT) in striatum of SHR131–134 (more information on Supplementary Material).
Primary culture of astrocytes
In order to perform primary culture of astrocytes, we used cortexes from 3–4 days-old pups135,136. Animals were sacrificed and their brains were removed and transferred to a petri dish containing Dulbecco’s Modified Eagle Medium (DMEM). The cortex was dissected and dispersed mechanically with scissors and, subsequently, we used three-gauge needles (24G × ¾″, 26G × ½″ and 30G × ½″) for complete tissue dissociation. After this procedure, cell suspension was centrifuged at 435 g for 5 minutes (centrifuge 5810R − Eppendorf) and the supernatant was discarded. The final pellet was resuspended in 2 mL of DMEM supplemented medium (10% of fetal bovine serum and 1% of antimycotic/antibiotic) and the cells were distributed in T75 cm² flasks. The culture was maintained at 5% CO2 and 37 °C, and the medium was changed every four days. To each T75 cm² culture flask, it was used cortexes from three brain hemispheres. Thus, three animals (six hemispheres of cortex) were enough to two T75 cm² flasks. Each N sample was considered per litter, and not for each newborn. We did not consider sex or weight of the newborn animals.
Cellular model of chemical hypoxia (CoCl2)
To mimic cellular hypoxia, primary astrocytes were treated with cobalt chloride (CoCl2). CoCl2 is known as a chemical inducer of hypoxia since it blocks the degradation of the transcription factor Hypoxia Inducible Factor 1 alpha (Hif1α) leading, consequently, to the increased activation of the hypoxia cascade. In normoxia situation (normal concentrations of O2), there is the hydroxylation of HIF1α by prolyl-hydroxylases (PHDs), which in turns, leads to its degradation through the ubiquitin proteasome system (UPS)35,64,65.
In our experiments, CoCl2 was dissolved in water and latter, following its physicochemical standards, it was aliquoted at 50 mM stock solution. We used along this study 800 µM, 1 mM, 2 mM and 5 mM of CoCl2 for 24 hours (hrs). In order to mimic a moderate and intense hypoxia, we used 800 µM and 2 mM of CoCl2, respectively.
Cellular model of gaseous hypoxia (Hypoxia Chamber – 0% O2)
To ascertain the action of the hypoxia cascade on mitochondrial metabolism without the use of a chemical inducer, we also used the hypoxia chamber as a strategy (Hypoxia chamber Stemcell Technologies; Cat. No. 27310). Knowing that astrocytes are resistant to hypoxia137,138 and that 4%, 3% or even 1% of O2 over short periods, such as 8, 10 and 12 hours, did not alter cellular viability137–139, the primary culture from our lab was submitted to a regimen of 0% of O2 for 8, 18 and 24 hours. To establish the 0% of O2, we used a protocol based on the internal volume of the chamber (cm3), in which O2 are displaced by N2 in a volume of 30 L/min for 4 minutes140. In our experiments, to resemble moderate and intense gaseous hypoxia, we exposed the cells to 0% of O2 for 8 h, or 18 and 24 hours, respectively.
Viability assay - chemical and gaseous hypoxias
Cell viability was assessed by the [3- (4,5-dimethylthiazol-2yl)-2,5-diphenyl tetrazolyum] bromide assay (MTT). Cells were plated in a 96-well plates (3 × 104 cells per well) in duplicate, and after 24 hours of CoCl2 treatment or upon exposure to the hypoxia chamber at the proposed times, cells were washed with PBS 1× (PBS, mM: 0,14 NaCl, 2,7 KCl, 1,5 K2HPO4 e 8,1 Na2HPO4), and incubated with the MTT reagent at the final concentration of 12 mM at 37 °C for 4 hours (Vybrant ™ MTT Cell Proliferation Assay Kit, Molecular Probes). Following the manufacturer’s protocol, the 96-well plate was then allocated into a plate reader (spectrophotometer) to read the absorbance at 540 mm at 37 °C. All assays were performed with control cells as well (without any treatment and in normoxia). Cellular viability was normalized as percentage of control group (mean ± SD).
Mitochondrial metabolism analysis – functional parameters
In order to evaluate Ca2+ levels and mitochondrial membrane potential (ΔΨm), control and SHR astrocytes were re-plated in 96-well plates (6 × 104 cells per well) for 24 hours as described previously135,136,141,142. After this period, the cells were treated with the proposed concentrations of CoCl2 (800 µM or 2 mM) for 24 hours or exposed to hypoxia chamber (8, 18 or 24 hours). Specifically, to evaluate cytosolic Ca2+ level, cells were loaded with Fluo-4-AM (10 µM) plus Pluronic F-127™ (20%) (1 hour, 37 °C) (485 nm excitation; 525 nm emission). Mitochondrial membrane potential was accessed after incubating the cells with Tetramethylrhodamine ethyl ester (TMRE, 500 nM) (1 hour, 37 °C) (540 nm excitation; 590 nm emission). Both dyes were incubated in microscopy medium (mM: 120 NaCl, 3,5 KCl, 0,4 KH2P O4, 5 NaHCO3, 1,2 NaSO4, 20 HEPES, 15 Glucose e pH 7.4), supplemented with 1 mM of calcium chloride (CaCl2).
For the experiments related to redox homeostasis, cells were also re-plated in 96-well plates (6 × 104 cells per well), but they were loaded in microscopy medium or Krebs medium (mM: 132 NaCl, 4 KCl, 1 CaCl2, 1.2 NaH2PO4, 1.4 MgCl2, 6 Glucose, 10 HEPES) supplemented with 1 mM of CaCl2 accordingly to the fluorescent probe. To evaluate general ROS measurements, cells were incubated in microscopy medium with Fluorescein Diclohidro Carboxylated Reagent (CM-H2DCF-DA) (20 µM; 30 min, 37 °C) (495 nm excitation; 520 nm emission)135,136,141–143; to assess superoxide (O2°−) levels, cells were loaded with Mitosox in Krebs medium (5 µM, 10 minutes at 37 °C) (510 nm excitation; 580 nm emission)144. The CM-H2DCF-DA shows much better retention in live cells tan DCFH2-DA and it is used to detect the generation of reactive oxygen intermediates. CM-H2DCFDA passively diffuses into cells, where the acetate groups are cleaved by intracellular esterases becoming DCFH, which is retained inside the cell. Afterwards, it is rapidly oxidized to the highly green fluorescent compound 2,7-dichlorofluorescein (DCF)141–143. On the other hand, Mitosox is a cationic derivative of dihydroethidum designed for highly selective detection of superoxide in the mitochondria of live cells. The cationic triphenylphosphonium substituent of MitoSOX Red indicator is responsible for the electrophoretically driven uptake of the probe in actively respiring mitochondria144. Once in the mitochondrial matrix, the radical is oxidized by superoxide and the radical become fluorescent.
The Fluo-4-AM, TMRE and DCF fluorescence were acquired on a spectrofluorimeter (Spectramaxi3™) for a period of 5 minutes, to get basal signal, and for another 5 minutes after the addition of fluorocarbonyl cyanide phenylhydrazone (FCCP) (5 μM), a mitochondrial protonophore used as an internal experimental control to obtain maximum fluorescence and the delta value (Δ). The baseline fluorescence was calculated from the mean of the last 10 reading points before FCCP, while the delta (Δ) was calculated by the difference between the maximum fluorescence after FCCP and the basal fluorescence intensity135,136,141–143. All these experiments were performed in duplicate and data were expressed as percentage of control cells (mean ± SD).
Regarding Mitosox, a kinetic reading was performed for 1 hour and 30 minutes on the spectrofluorimeter. The results were obtained as RFU (relative fluorescence units) per minute, and data was expressed by the slope of the curve144. After reading, the medium was removed, cells were washed with PBS 1x and then they were incubated with 0.2% TRITON (for 30 minutes on ice). This process is required for protein extraction in order to normalize the slope per mg of protein144. Proteins were quantified by the Bradford method using the Bradford Quick Start reagent (BioRad) and data were expressed as percentage of control cells (mean ± SD).
Mitochondrial function and hypoxia cascade activation – Gene expression
The expression of transcription factors related to mitochondrial metabolism was evaluated by real-time PCR (qPCR)145,146. For each reaction, performed by Universal SYBR®Green Supermix, it was used 200 ng of cDNA and sequence-specific primers (300 nM); the analysis of mitochondrial content was also evaluated through qPCR. The template was performed with an initial cycle of 30 secs at 95 °C, followed by 46 cycles of 15 secs at 95 °C plus 30 secs at 61 °C. After amplification, melting temperature of the PCR products were determined by performing melting curves, with 0.5 °C increments every 5 secs, from 65 °C to 95 °C. Primers sequences were as follow: I) Peroxisome proliferator-activated receptor gamma coativator 1-alpha (α) (Pgc1-α) (Forward 5′-3′: CTCGACACGGAGAGTTAAAGG, Reverse 5′-3′: TAAACTGAGCTACCCTTGGG); II) Mitochondrial Transcription Factor A (Tfam) (Forward 5′-3′: CAGAGTTGTCATTGGGATTGG, Reverse 5′-3′: CATTCAGTGGGCAGAAGTCC); III) Nuclear Respiratory Factor 1 (Nrf-1) (Forward 5′-3′: GCTAAGGCTGCTGGGAAGTA, Reverse 5′-3′: TCAGTTGCTGTGGCGAGTTA); IV) Nuclear Factor (erythroid-derived 2) Like 2 (Nfe2l2) (Forward 5′-3′: CTGCTGCCATTAGTCAGTCG, Reverse 5′-3′: GTGCCTTCAGTGTGCTTCTG); V) Mitochondrial-encoded Complex IV Subunit Cytochrome c Oxidase Subunit 1 (Mtco1) (Forward 5′-3′: TGGCTTCGTCCACTGATTCC, Reverse 5′-3′: CGAGGTATCCCCGCTAATCC); VI) β-actin, that was used as housekeeping gene (Forward 5′-3′: AGGGAAATCGTGCGGTGAC, Reverse 5′-3′: CGCTCATTGCCGATAGTG).
At the end of each cycle, SYBR®Green fluorescence was recorded to enable determination of Cq. After amplification, melting temperature of the PCR products were determined. For qPCR analysis, the BioRad CFX Manager software was used. Normalization was carried out in relation to β-actin expression and data were expressed as percentage of control cells (mean ± SD).
Mitochondrial content investigation – protein levels
To evaluate protein level related to mitochondrial content, total fraction from astrocytes culture were obtained as described previously141,144–147. In brief, extracts were prepared in ice-cold RIPA buffer (mM: 150 NaCl, 50 Tris HCl – pH 7.4, 5 EGTA; still containing 1% TRITON, 0.5% DOC, 0.1% SDS) (pH 7.5) supplemented with MS-SAFE protease and phosphatase inhibitor (Sigma-Aldrich) accordingly to manufacturer’s protocol. The final supernatant was collected and stored at −80 °C for later use. Samples were prepared using 50 μg of protein. Proteins were transferred to PVDF membrane (0.2 µM) and were incubated overnight, at 4 °C, with primary antibodies directed against: I) TOM-40 (Santa Cruz – SC-11414; 1:1000), protein coupled to mitochondrial outer membrane and II) ACTIN (Sigma – A2103; 1:5000). The secondary antibodies were Horseradish Peroxidase (HRP) pAb goat anti-mouse IgG, HRP pAb goat anti-rabbit IgG and IgG rabbit anti-goat-conjugated peroxidase. Immunoreactive bands were visualized with ECL substrate (GE - Healthcare) in ImageQuanty LAS 500 (GE-Healthcare). The Quantity One software (Biorad) was used to analyze the optical density of all bands. All data were expressed as percentage of control cells (mean ± SD) after normalization by ACTIN.
Measurement of adenine nucleotides and metabolic compounds
To comprehend the relationship between mitochondrial dysfunctions and hypoxia, we further evaluated the levels of bio products related to energy metabolism, named ATP, ADP, Pyruvate, Lactate, NAD+ and NADH141,145–147. All of them were measured using commercially available kits (Abcam, ab83355, ab83359, ab65342, ab65330 and ab65348).
For the analysis, astrocytes (from Wistar and SHR pups) were plated at the concentration of 1 × 106 cells/well (6-well-plate) and exposed with the proposed concentrations of CoCl2 (800 µM and 2 mM). After treatment, the procedure was started following information from the proposed kits (ab83355, ab83359, ab65342, ab65330 and ab65348). For all analysis, ATP, ADP, Pyruvate, Lactate, NAD+ and NADH levels were normalized for the number of cells (1 × 106/N) and expressed as percentage of control cells (mean ± SD).
Analysis of results and statistical analysis
Results are expressed as mean ± SD of the number of independent experiments indicated in figure legends. The graphs were assembled using the GraphPad Prism 6 program (GraphPad Prism Version 6.0), and the statistical analysis was performed with One- or Two-Way ANOVA followed by post-hoc test Duncan. Student’s t Test was performed when necessary. It was considered statistically different p < 0.05.
Supplementary information
Acknowledgements
This work was supported by São Paulo Research Foundation (FAPESP) (ref. 2015/02041-1) and Fundação de Amparo à Pesquisa of Santa Casa de São Paulo School of Medical Science (FCMSCSP) (2015-2016). LFSS was supported by Master FAPESP fellowship (2015/25595-2). MDB was supported by Master CAPES fellowship and FAPESP fellowship (2016/12039-7). We thank Prof. Dr. Ivarne Tersariol and Prof. Dr. Marimélia Porcionato, both from UNIFESP, for let us use the hypoxia chamber. We also thank the staff of the animal facilities for excellent animal care, the technicians from our Department and Bruno Coelho for figure formatting.
Author contributions
L.F.S.S. performed all experiments regarding mitochondrial function (functional experiments and qPCR); he also did the analysis and the statistics and wrote this manuscript. MDB contributed performing astrocytes cultures along the study. J.M.C.Y. is an undergrad student and she performed the western blot. TRR designed the study, wrote the protocols, revised the manuscript and wrote the final version of it. All authors approved the final version of manuscript.
Data availability
All data generated or analysed during this study are included in this published article (and its Supplementary Information files).
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
is available for this paper at 10.1038/s41598-019-53605-4.
References
- 1.Clouston, T. S. The neuroses of development: being the Morison lectures for 1890. viii, 138 p. (1891).
- 2.Owen MJ, O’Donovan MC. Schizophrenia and the neurodevelopmental continuum:evidence from genomics. World Psychiatry. 2017;16(3):227–235. doi: 10.1002/wps.20440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cannon M, Jones PB, Murray RM. Obstetric complications and schizophrenia: Historical and meta-analytic review. Am. J. Psychiatry. 2002;159(7):1080–92. doi: 10.1176/appi.ajp.159.7.1080. [DOI] [PubMed] [Google Scholar]
- 4.Jenkins TA. Perinatal complications and schizophrenia: Involvement of the immune system. Front. Neurosci. 2013;7:110. doi: 10.3389/fnins.2013.00110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schmidt-Kastner R, van Os J, W.M. Steinbusch H, Schmitz C. Gene regulation by hypoxia and the neurodevelopmental origin of schizophrenia. Schizophr. Res. 2006;84(2–3):253–71. doi: 10.1016/j.schres.2006.02.022. [DOI] [PubMed] [Google Scholar]
- 6.Cannon Tyrone D., van Erp Theo G. M., Rosso Isabelle M., Huttunen Matti, Lönnqvist Jouko, Pirkola Tiia, Salonen Oili, Valanne Leena, Poutanen Veli-Pekka, Standertskjöld-Nordenstam Carl-Gustav. Fetal Hypoxia and Structural Brain Abnormalities in Schizophrenic Patients, Their Siblings, and Controls. Archives of General Psychiatry. 2002;59(1):35. doi: 10.1001/archpsyc.59.1.35. [DOI] [PubMed] [Google Scholar]
- 7.Van Erp TGM, et al. Contributions of genetic risk and fetal hypoxia to hippocampal volume in patients with schizophrenia or schizoaffective disorder, their unaffected siblings, and healthy unrelated volunteers. Am. J. Psychiatry. 2002;159(9):1514–1520. doi: 10.1176/appi.ajp.159.9.1514. [DOI] [PubMed] [Google Scholar]
- 8.Demjaha A, MacCabe JH, Murray RM. How genes and environmental factors determine the different neurodevelopmental trajectories of schizophrenia and bipolar disorder. Schizophr. Bull. 2012;38(2):209–214. doi: 10.1093/schbul/sbr100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Howell KR, Pillai A. Effects of prenatal hypoxia on schizophrenia-related phenotypes in heterozygous reeler mice: A gene × environment interaction study. Eur. Neuropsychopharmacol. 2014;24(8):1324–1336. doi: 10.1016/j.euroneuro.2014.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mayoral SR, Omar G, Penn AA. Sex differences in a hypoxia model of preterm brain damage. Pediatr. Res. 2009;66(3):248–253. doi: 10.1203/PDR.0b013e3181b1bc34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Asami Takeshi, Bouix Sylvain, Whitford Thomas J., Shenton Martha E., Salisbury Dean F., McCarley Robert W. Longitudinal loss of gray matter volume in patients with first-episode schizophrenia: DARTEL automated analysis and ROI validation. NeuroImage. 2012;59(2):986–996. doi: 10.1016/j.neuroimage.2011.08.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Andreasen NC, Liu D, Ziebell S, Vora A, Ho BC. Relapse duration, treatment intensity, and brain tissue loss in schizophrenia: A prospective longitudinal MRI study. Am. J. Psychiatry. 2013;170(6):609–615. doi: 10.1176/appi.ajp.2013.12050674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dietsche B, Kircher T, Falkenberg I. Structural brain changes in schizophrenia at different stages of the illness: A selective review of longitudinal magnetic resonance imaging studies. Aust. N. Z. J. Psychiatry. 2017;51(5):500–508. doi: 10.1177/0004867417699473. [DOI] [PubMed] [Google Scholar]
- 14.Schmitt A, Malchow B, Hasan A, Falkai P. The impact of environmental factors in severe psychiatric disorders. Front. Neurosci. 2014;8:19. doi: 10.3389/fnins.2014.00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rosenstock, T. & Rego, A. Modified mitochondrial dynamics, turnover and function in neurodegeneration: a focus on Huntington’s. Resear. Signp., 149–194 (2012).
- 16.Sanderson TH, Raghunayakula S, Kumar R. Neuronal hypoxia disrupts mitochondrial fusion. Neuroscience. 2015;301:71–78. doi: 10.1016/j.neuroscience.2015.05.078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sullivan Courtney R., O’Donovan Sinead M., McCullumsmith Robert E., Ramsey Amy. Defects in Bioenergetic Coupling in Schizophrenia. Biological Psychiatry. 2018;83(9):739–750. doi: 10.1016/j.biopsych.2017.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schulmann A, et al. Novel Complex Interactions between Mitochondrial and Nuclear DNA in Schizophrenia and Bipolar Disorder. Mol. Neuropsychiatry. 2019;5:13–27. doi: 10.1159/000495658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Prabakaran S, et al. Mitochondrial dysfunction in schizophrenia: Evidence for compromised brain metabolism and oxidative stress. Mol. Psychiatry. 2004;9(7):684–97,643. doi: 10.1038/sj.mp.4001511. [DOI] [PubMed] [Google Scholar]
- 20.Faizi M, Salimi A, Rasoulzadeh M, Naserzadeh P, Pourahmad J. Schizophrenia induces oxidative stress and cytochrome c release in isolated rat brain mitochondria: A possible pathway for induction of apoptosis and neurodegeneration. Iran. J. Pharm. Res. 2014;13(suppl):93–100. doi: 10.22037/ijpr.2014.1463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Park C, Park SK. Molecular links between mitochondrial dysfunctions and schizophrenia. Mol. Cells. 2012;33(2):105–110. doi: 10.1007/s10059-012-2284-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Konradi C, Sillivan SE, Clay HB. Mitochondria, oligodendrocytes and inflammation in bipolar disorder: Evidence from transcriptome studies points to intriguing parallels with multiple sclerosis. Neurobiol. Dis. 2012;45(1):35–47. doi: 10.1016/j.nbd.2011.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cuperfain AB, Zhang ZL, Kennedy JL, Gonçalves VF. The Complex Interaction of Mitochondrial Genetics and Mitochondrial Pathways in Psychiatric Disease. Mol. Neuropsychiatry. 2018;4(1):52–69. doi: 10.1159/000488031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ben-Shachar D, Karry R. Neuroanatomical pattern of mithochondrial complex I pathology varies between schizoprenia, bipolar disorder and major depression. PLoS One. 2008;3(11):e3676. doi: 10.1371/journal.pone.0003676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kolomeets NS, Uranova N. Ultrastructural abnormalities of astrocytes in the hippocampus in schizophrenia and duration of illness: A postortem morphometric study. World J. Biol. Psychiatry. 2010;11(2):282–92. doi: 10.3109/15622970902806124. [DOI] [PubMed] [Google Scholar]
- 26.Uranova NA, Aganova EA. Ultrastructure of the synapses of the anterior limbic cortex in schizophrenia. Zh. Nevropatol. Psikhiatr. Im. S. S. Korsakova. 1989;89(7):56–59. [PubMed] [Google Scholar]
- 27.Kolomeets NS, Uranova NA. Synaptic contacts in schizophrenia: Studies using immunocytochemical identification of dopaminergic neurons. Neurosci. Behav. Physiol. 1999;97(12):39–43. doi: 10.1007/BF02465329.. [DOI] [PubMed] [Google Scholar]
- 28.Scaglia F. The role of mitochondrial dysfunction in psychiatric disease. Dev. Disbil. Res. Rev. 2010;16(2):136–143. doi: 10.1002/ddrr.115. [DOI] [PubMed] [Google Scholar]
- 29.Clay HB, Sillivan S, Konradi C. Mitochondrial dysfunction and pathology in bipolar disorder and schizophrenia. Int. j. Dev. Neurosci. 2011;29(3):311–324. doi: 10.1016/j.ijdevneu.2010.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Neumann M, et al. Ubiquitinated TDP-43 in frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Science. 2006;314(5796):130–133. doi: 10.1126/science.1134108. [DOI] [PubMed] [Google Scholar]
- 31.Shi P, Wei Y, Zhang J, Gal J, Zhu H. Mitochondrial dysfunction is a converging point of multiple pathological pathways in amyotrophic lateral sclerosis. J. Alzheimers Dis. 2010;20(suppl):S311–24. doi: 10.3233/JAD-2010-100366. [DOI] [PubMed] [Google Scholar]
- 32.Atkin TA, Brandon NJ, Kittler JT. Disrupted in schizophrenia 1 forms pathological aggresomes that disrupt its function in intracellular transport. Hum. Mol. Genet. 2012;21(9):2017–2028. doi: 10.1093/hmg/dds018. [DOI] [PubMed] [Google Scholar]
- 33.Ben Haim L, Rowitch DH. Functional diversity of astrocytes in neural circuit regulation. Nat. Rev. Neurosci. 2016;18(1):31–41. doi: 10.1038/nrn.2016.159. [DOI] [PubMed] [Google Scholar]
- 34.Brown AM, Ransom BR. Astrocyte glycogen and brain energy metabolism. Glia. 2007;55(120):1263–1271. doi: 10.1002/glia.20557. [DOI] [PubMed] [Google Scholar]
- 35.Fuhrmann DC, Brüne B. Mitochondrial composition and function under the control of hypoxia. Redox Biol. 2017;12:208–205. doi: 10.1016/j.redox.2017.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Barres BA. The Mystery and Magic of Glia: A Perspective on Their Roles in Health and Disease. Neuron. 2008;60(3):430–440. doi: 10.1016/j.neuron.2008.10.013. [DOI] [PubMed] [Google Scholar]
- 37.Ramakrishnan S, Anand V, Roy S. Vascular endothelial growth factor signaling in hypoxia and inflammation. J. Neuroimmune Pharmacol. 2014;9(2):142–160. doi: 10.1007/s11481-014-9531-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kurihara T, Westenskow PD, Friedlander M. Hypoxia-inducible factor (HIF)/vascular endothelial growth factor (VEGF) signaling in the retina. Adv. Exp. Med. Biol. 2014;801:275–281. doi: 10.1007/978-1-4614-3209-8_35. [DOI] [PubMed] [Google Scholar]
- 39.Pagès G, Pouysségur J. Transcriptional regulation of the Vascular Endothelial Growth Factor gene–a concert of activating factors. Cardiovasc. Res. 2005;65:564–573. doi: 10.1016/j.cardiores.2004.09.032. [DOI] [PubMed] [Google Scholar]
- 40.Gnaiger E. Mitochondrial Pathways and Respiratory Control An Introduction to OXPHOS Analysis. Mitochondr. Phsysiol. Network. 2014;19:12. [Google Scholar]
- 41.Crompton M, Barksby E, Johnson N, Capano M. Mitochondrial intermembrane junctional complexes and their involvement in cell death. Biochimie. 2002;84:143–152. doi: 10.1016/s0300-9084(02)01368-8. [DOI] [PubMed] [Google Scholar]
- 42.Wang RY, et al. Nrf2 protects against diabetic dysfunction of endothelial progenitor cells via regulating cell senescence. Int. J. Mol. Med. 2018;42(3):1327–1340. doi: 10.3892/ijmm.2018.3727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Liu T, Knowlton AA. Repetitive ROS injury leads to inactivation of NRF2-induced antioxidant defense and mitochondrial dysfunction in ischemic heart failure. FASEB J. 2016;30(suppl):958.5–958.5. [Google Scholar]
- 44.Morales Pantoja IE, Hu CL, Perrone-Bizzozero NI, Zheng J, Bizzozero OA. Nrf2-dysregulation correlates with reduced synthesis and low glutathione levels in experimental autoimmune encephalomyelitis. J. Neurochem. 2016;139(4):640–650. doi: 10.1111/jnc.13837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chang WT, Chen HI, Chiou RJ, Chen CY, Huang AM. A novel function of transcription factor α-Pal/NRF-1: Increasing neurite outgrowth. Biochem. Biophys. Res. Commun. 2005;334(1):199–206. doi: 10.1016/j.bbrc.2005.06.079. [DOI] [PubMed] [Google Scholar]
- 46.Weydt P, et al. Thermoregulatory and metabolic defects in Huntington’s disease transgenic mice implicate PGC-1α in Huntington’s disease neurodegeneration. Cell Metab. 2006;4:349–362. doi: 10.1016/j.cmet.2006.10.004. [DOI] [PubMed] [Google Scholar]
- 47.Choi J, Chandrasekaran K, Inoue T, Muragundla A, Russell JW. PGC-1α regulation of mitochondrial degeneration in experimental diabetic neuropathy. Neurobiol. Dis. 2014;64:118–130. doi: 10.1016/j.nbd.2014.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rapaport D, Neupert W. Biogenesis of Tom40, core component of the TOM complex of mitochondria. J. Cell Biol. 1999;146:321–331. doi: 10.1083/jcb.146.2.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Weydt P, et al. The gene coding for PGC-1α modifies age at onset in Huntington’s Disease. Mol. Neurodegener. 2009;8(4):3. doi: 10.1186/1750-1326-4-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bayer H, et al. ALS-causing mutations differentially affect PGC-1α expression and function in the brain vs. peripheral tissues. Neurobiol. Dis. 2017;97:36–45. doi: 10.1016/j.nbd.2016.11.001. [DOI] [PubMed] [Google Scholar]
- 51.Weydt, P., Soyal, S. M., Landwehrmeyer, G. B. & Patsch, W. A single nucleotide polymorphism in the coding region of PGC-1α is a male-specific modifier of Huntington disease age-at-onset in a large European cohort. BMC Neurol. 2:14:1, 10.1186/1471-2377-14-1 (2014). [DOI] [PMC free article] [PubMed]
- 52.Handschin C. The biology of PGC-1α and its therapeutic potential. Trends Pharmacol. Sci. 2009;30(6):322–9. doi: 10.1016/j.tips.2009.03.006. [DOI] [PubMed] [Google Scholar]
- 53.Facucho-Oliveira JM, Alderson J, Spikings EC, Egginton S, St. John JC. Mitochondrial DNA replication during differentiation of murine embryonic stem cells. J. Cell Sci. 2007;120(22):4025–34. doi: 10.1242/jcs.016972. [DOI] [PubMed] [Google Scholar]
- 54.Novin MG, et al. Comparison of mitochondrial-related transcriptional levels of TFAM, NRF1 and MT-C01 genes in single human oocytes at various stages of the oocyte maturation. Iran. Biomed. J. 2015;19(10):23–8. doi: 10.6091/ibj.1400.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ghaffari Novin M, et al. The Relationship between Transcript Expression Levels of Nuclear Encoded (TFAM, NRF1) and Mitochondrial Encoded (MT-CO1) Genes in Single Human Oocytes during Oocyte Maturation. Balk. J. Med. Genet. 2015;18(1):39–46. doi: 10.1515/bjmg-2015-0004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Venegas V, Halberg MC. Measurement of mitochondrial DNA copy number. Methods Mol. Biol. 2012;837:327–35. doi: 10.1007/978-1-61779-504-6_22. [DOI] [PubMed] [Google Scholar]
- 57.Taherzadeh-Fard E, et al. PGC-1alpha downstream transcription factors NRF-1 and TFAM are genetic modifiers of Huntington disease. Mol. Neurodegener. 2011;6:32. doi: 10.1186/1750-1326-6-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ngo, H. B., Lovely, G. A., Phillips, R. & Chan, D. C. Distinct structural features of TFAM drive mitochondrial DNA packaging versus transcriptional activation. Nat. Commun. 5, 10.1038/ncomms4077 (2014). [DOI] [PMC free article] [PubMed]
- 59.Lezza AMS. Mitochondrial transcription factor A (TFAM): One actor for different roles. Front. Biol. 2012;7:30–39. doi: 10.1007/s11515-011-1175-x. [DOI] [Google Scholar]
- 60.Reyes A, Mezzina M, Gadaleta G. Human mitochondrial transcription factor A (mtTFA): Gene structure and characterization of related pseudogenes. Gene. 2002;291:223–232. doi: 10.1016/s0378-1119(02)00600-5. [DOI] [PubMed] [Google Scholar]
- 61.Larsson NG, et al. Mitochondrial transcription factor A is necessary for mtDNA maintenance and embryogenesis in mice. Nat. Genet. 1998;18:231–236. doi: 10.1038/ng0398-231. [DOI] [PubMed] [Google Scholar]
- 62.Kim J, Tchernyshyov I, Semenza GL, Dang CV. HIF-1-mediated expression of pyruvate dehydrogenase kinase: A metabolic switch required for cellular adaptation to hypoxia. Cell Metab. 2006;3:177–185. doi: 10.1016/j.cmet.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 63.Semenza GL, et al. Hypoxia response elements in the aldolase A, enolase 1, and lactate dehydrogenase a gene promoters contain essential binding sites for hypoxia-inducible factor 1. J. Biol. Chem. 1996;271:32529–32537. doi: 10.1074/jbc.271.51.32529. [DOI] [PubMed] [Google Scholar]
- 64.Solaini G, Baracca A, Lenaz G, Sgarbi G. Hypoxia and mitochondrial oxidative metabolism. Biochim Biophys Acta. 2010;1797:1171–7. doi: 10.1016/j.bbabio.2010.02.011. [DOI] [PubMed] [Google Scholar]
- 65.Semenza GL, Roth PH, Fang HM, Wang GL. Transcriptional regulation of genes encoding glycolytic enzymes by hypoxia-inducible factor 1. J. Biol. Chem. 1994;269:23757–63. [PubMed] [Google Scholar]
- 66.Koos BJ. Adenosine A 2a receptors and O 2 sensing in development. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2011;301(3):601–22. doi: 10.1152/ajpregu.00664.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Pugh CW. Modulation of the hypoxic response. Adv. Exp. Med. Biol. 2016;903:259–271. doi: 10.1007/978-1-4899-7678-9_18. [DOI] [PubMed] [Google Scholar]
- 68.Kaufman DM, Crowder CM. Mitochondrial proteostatic collapse leads to hypoxic injury. Curr. Biol. 2015;25(16):2171–6. doi: 10.1016/j.cub.2015.06.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hamanaka RB, Weinberg SE, Reczek CR, Chandel NS. The Mitochondrial Respiratory Chain Is Required for Organismal Adaptation to Hypoxia. Cell Rep. 2016;15:451–459. doi: 10.1016/j.celrep.2016.03.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Iommarini L, Porcelli AM, Gasparre G, Kurelac I. Non-Canonical Mechanisms Regulating Hypoxia-Inducible Factor 1 Alpha in Cancer. Front. Oncol. 2017;27(7):286. doi: 10.3389/fonc.2017.00286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Marxsen JH, et al. Hypoxia-inducible factor-1 (HIF-1) promotes its degradation by induction of HIF-α-prolyl-4-hydroxylases. Biochem. J. 2004;1(381(3)):761–767. doi: 10.1042/BJ20040620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Giussani DA. The fetal brain sparing response to hypoxia: Physiological mechanisms. J. Physiol. 2016;594:1215–1230. doi: 10.1113/JP271099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Santo-Domingo J, Demaurex N. Calcium uptake mechanisms of mitochondria. Biochim. Biophys. Acta Bioenerg. 2010;1797:907–912. doi: 10.1016/j.bbabio.2010.01.005. [DOI] [PubMed] [Google Scholar]
- 74.Orrenius S, Zhivotovsky B, Nicotera P. Calcium: Regulation of cell death: the calcium–apoptosis link. Nat. Rev. Mol. Cell Biol. 2003;4:552–565. doi: 10.1038/nrm1150. [DOI] [PubMed] [Google Scholar]
- 75.Lemasters JJ, Theruvath TP, Zhong Z, Nieminen A-L. Mitochondrial calcium and the permeability transition in cell death. Biochim. Biophys. Acta - Bioenerg. 2009;1787:1395–1401. doi: 10.1016/j.bbabio.2009.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Smaili S, et al. Calcium and cell death signaling in neurodegeneration and aging. An. Acad. Bras. Ciênc. 2009;81:467–475. doi: 10.1590/S0001-37652009000300011. [DOI] [PubMed] [Google Scholar]
- 77.Andreyev A, Tamrakar P, Rosenthal RE, Fiskum G. Calcium uptake and cytochrome c release from normal and ischemic brain mitochondria. Neurochem. Int. 2018;117:15–22. doi: 10.1016/j.neuint.2017.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Turcotte ML, Parliament M, Franko A, Allalunis-Turner J. Variation in mitochondrial function in hypoxia-sensitive and hypoxia-tolerant human glioma cells. Br. J. Cancer. 2002;86:619–24. doi: 10.1038/sj.bjc.6600087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ritz M-F, Grond-Ginsbach C, Engelter S, Lyrer P. Gene Expression Suggests Spontaneously Hypertensive Rats May Have Altered Metabolism and Reduced Hypoxic Tolerance. Curr. Neurovasc. Res. 2012;9:10–19. doi: 10.2174/156720212799297074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Zhou Y-F, Zheng X-W, Zhang G-H, Zong Z-H, Qi G-X. The effect of hypoxia-inducible factor 1-alpha on hypoxia-induced apoptosis in primary neonatal rat ventricular myocytes. Cardiovasc. J. Afr. 2010;21(1):37–41. doi: 10.1007/s12630-014-0302-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Gonchar OA, Mankovska IN. Moderate intermittent hypoxia/hyperoxia: Implication for correction of mitochondrial dysfunction. Cent. Eur. J. Biol. 2012;7:801–809. doi: 10.2478/s11535-012-0072-x. [DOI] [Google Scholar]
- 82.Merino JJ, Roncero C, Oset-Gasque MJ, Naddaf A, González MP. Antioxidant and protective mechanisms against hypoxia and hypoglycaemia in cortical neurons in Vitro. Int. J. Mol. Sci. 2014;15:2475–2493. doi: 10.3390/ijms15022475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Geihs MA, et al. Effects of hypoxia and reoxygenation on the antioxidant defense system of the locomotor muscle of the crab Neohelice granulata (Decapoda, Varunidae) J. Comp. Physiol. B Biochem. Syst. Environ. Physiol. 2016;186:569–579. doi: 10.1007/s00360-016-0976-2. [DOI] [PubMed] [Google Scholar]
- 84.Semenza GL. Defining the role of hypoxia-inducible factor 1 in cancer biology and therapeutics. Oncogene. 2010;29:625–634. doi: 10.1038/onc.2009.441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Tafani M, et al. The Interplay of Reactive Oxygen Species, Hypoxia, Inflammation, and Sirtuins in Cancer Initiation and Progression. Oxid. Med. Cell. Longev. 2016;2016:3907147. doi: 10.1155/2016/3907147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ayala A, Muñoz MF, Argüelles S. Lipid peroxidation: Production, metabolism, and signaling mechanisms of malondialdehyde and 4-hydroxy-2-nonenal. Oxid. Med. Cell. Longev. 2014;2014:360438. doi: 10.1155/2014/360438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Perluigi M, Coccia R, Butterfield DA. 4-Hydroxy-2-Nonenal, a Reactive Product of Lipid Peroxidation, and Neurodegenerative Diseases: A Toxic Combination Illuminated by Redox Proteomics Studies. Antioxid. Redox Signal. 2012;17(11):1590–1609. doi: 10.1089/ars.2011.4406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Behn C, Araneda OF, Llanos AJ, Celedón G, González G. Hypoxia-related lipid peroxidation: Evidences, implications and approaches. Respir. Physiol. Neurobiol. 2007;158(2-3):143–50. doi: 10.1016/j.resp.2007.06.001. [DOI] [PubMed] [Google Scholar]
- 89.Rauchová H, Vokurková M, Koudelová J. Hypoxia-induced lipid peroxidation in the brain during postnatal ontogenesis. Physiol. Res. 2012;61((Suppl.1):S89–S101. doi: 10.33549/physiolres.932374. [DOI] [PubMed] [Google Scholar]
- 90.Nakaso K, et al. PI3K is a key molecule in the Nrf2-mediated regulation of antioxidative proteins by hemin in human neuroblastoma cells. FEBS Lett. 2003;546:181–184. doi: 10.1016/s0014-5793(03)00517-9. [DOI] [PubMed] [Google Scholar]
- 91.Rooney JP, et al. PCR based determination of mitochondrial DNA copy number in multiple species. Methods Mol. Biol. 2015;1241:23–38. doi: 10.1007/978-1-4939-1875-1_3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Kuzmenko, A. et al. Single molecule tracking fluorescence microscopy in mitochondria reveals highly dynamic but confined movement of Tom40. Sci. Rep. 1, 10.1038/srep00195 (2011). [DOI] [PMC free article] [PubMed]
- 93.Meisinger C, et al. The mitochondrial morphology protein Mdm10 functions in assembly of the preprotein translocase of the outer membrane. Dev. Cell. 2004;7:61–71. doi: 10.1016/j.devcel.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 94.Verge B, et al. Mitochondrial DNA (mtDNA) and schizophrenia. Eur. Psychiatry. 2011;26(1):45–46. doi: 10.1016/j.eurpsy.2010.08.008. [DOI] [PubMed] [Google Scholar]
- 95.Verge B, et al. New evidence for the involvement of mitochondrial inheritance in schizophrenia: Results from a cross-sectional study evaluating the risk of illness in relatives of schizophrenia patients. J. Clin. Psychiatry. 2012;73(5):684–690. doi: 10.4088/JCP.10m06718. [DOI] [PubMed] [Google Scholar]
- 96.Mamdani F, Rollins B, Morgan L, Sequeira PA, Vawter MP. The somatic common deletion in mitochondrial DNA is decreased in schizophrenia. Schizophr. Res. 2014;159(2-3):370–375. doi: 10.1016/j.schres.2014.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.García-de la Cruz DD, et al. Association between mitochondrial DNA and cognitive impairment in schizophrenia: study protocol for a Mexican population. Neuropsychiatr. Dis. Treat. 2019;28(15):1717–1722. doi: 10.2147/ndt.s208587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Dorofeyeva N, Goshovska Y, Sagach V. Mitochondrial Membrane Potential and Oxygen Consumption in Spontaneously Hypertensive Rats. Int. J. Physiol. Pathophysiol. 2012;3:61–68. doi: 10.1615/IntJPhysPathophys.v3.i1.70. [DOI] [Google Scholar]
- 99.Calderón-Cortés E, et al. Changes in mitochondrial functionality and calcium uptake in hypertensive rats as a function of age. Mitochondrion. 2008;8:262–272. doi: 10.1016/j.mito.2008.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Martins-de-Souza D, et al. Proteomic analysis of dorsolateral prefrontal cortex indicates the involvement of cytoskeleton, oligodendrocyte, energy metabolism and new potential markers in schizophrenia. J. Psychiatr. Res. 2009;43(11):978–86. doi: 10.1016/j.jpsychires.2008.11.006. [DOI] [PubMed] [Google Scholar]
- 101.Nascimento JM, Martins-De-Souza D. The proteome of schizophrenia. Npj Schiz. 2015;1:14003. doi: 10.1038/npjschz.2014.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Ngounou Wetie AG, et al. Mass spectrometry for the detection of potential psychiatric biomarkers. J. Mol. Psychiatry. 2013;1:8. doi: 10.1186/2049-9256-1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Zuccoli GS, Saia-Cereda VM, Nascimento JM, Martins-de-Souza D. The energy metabolism dysfunction in psychiatric disorders postmortem brains: Focus on proteomic evidence. Front. Neurosci. 2017;11:493. doi: 10.3389/fnins.2017.00493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Wu A, et al. Validating mitochondrial electron transport chain content in individuals at clinical high risk for psychosis. Sci. Rep. 2019;9:12695. doi: 10.1038/s41598-019-49180-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Sullivan CR, et al. Measurement of lactate levels in postmortem brain, iPSCs, and animal models of schizophrenia. Sci. Rep. 2019;9(27):5087. doi: 10.1038/s41598-019-41572-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Logica T, et al. Metabolic changes following perinatal Asphyxia: Role of astrocytes and their interaction with neurons. Front. Aging Neurosci. 2016;8:116. doi: 10.3389/fnagi.2016.00116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Dienel GA. Fluxes of Lactate Into, From, and Among Gap Junction-Coupled Astroglia and Their Interaction With Noradrenaline. Front. Neurosci. 2017;9(8):261. doi: 10.1016/B978-0-12-805088-0.00007-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Schönenberger M, Kovacs W. Hypoxia signaling pathways: modulators of oxygen-related organelles. Front. Cell Dev. Biol. 2015;3:42. doi: 10.3389/fcell.2015.00042.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Prolla TA, Denu JM. NAD+ deficiency in age-related mitochondrial dysfunction. Cell Metab. 2014;19(2):178–80. doi: 10.1016/j.cmet.2014.01.005. [DOI] [PubMed] [Google Scholar]
- 110.Stein LR, Imai SI. The dynamic regulation of NAD metabolism in mitochondria. Trends Endocrinol. Metab. 2012;23(9):420–8. doi: 10.1016/j.tem.2012.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Okamoto K, Aoki K. Development of a Strain of Spontaneously Hypertensive Rats. Jpn. Circ. J. 1963;27:282–293. doi: 10.1253/jcj.27.282. [DOI] [PubMed] [Google Scholar]
- 112.Bassan H, et al. The pregnant spontaneously hypertensive rat as a model of asymmetric intrauterine growth retardation and neurodevelopmental delay. Hypertens. Pregnancy. 2005;24:201–211. doi: 10.1080/10641950500281142. [DOI] [PubMed] [Google Scholar]
- 113.Peraçoli JC, Rudge MV, Sartori MS, da Silva Franco RJ. Effects of hypertension on maternal adaptations to pregnancy: experimental study on spontaneously hypertensive rats. Sao Paulo Med. J. 2001;119:54–58. doi: 10.1590/S1516-31802001000200003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Calzavara MB, et al. Effects of antipsychotics and amphetamine on social behaviors in spontaneously hypertensive rats. Behav. Brain Res. 2011;225:15–22. doi: 10.1016/j.bbr.2011.06.026. [DOI] [PubMed] [Google Scholar]
- 115.Mattace Raso G, et al. Evaluation of Placental Protein Modifications in Normotensive and Spontaneously Hypertensive Rats. Placenta. 2008;29:429–435. doi: 10.1016/j.placenta.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 116.Pinto YM, Paul M, Ganten D. Lessons from rat models of hypertension: From Goldblatt to genetic engineering. Cardio. Res. 1998;39:77–88. doi: 10.1016/s0008-6363(98)00077-7. [DOI] [PubMed] [Google Scholar]
- 117.Calzavara MB, et al. Neuroleptic drugs revert the contextual fear conditioning deficit presented by spontaneously hypertensive rats: A potential animal model of emotional context processing in Schizophrenia? Schizophr. Bull. 2009;35:748–759. doi: 10.1093/schbul/sbn006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Ledoux JE, Sakaguchi A, Reis DJ. Strain differences in fear between spontaneously hypertensive and normotensive rats. Brain Res. 1983;277:137–143. doi: 10.1016/0006-8993(83)90915-0. [DOI] [PubMed] [Google Scholar]
- 119.Palmer AA, et al. Prepulse startle deficit in the brown norway rat: A potential genetic model. Behav. Neurosci. 2000;114:374–388. doi: 10.1037//0735-7044.114.2.374. [DOI] [PubMed] [Google Scholar]
- 120.Ferguson SA, Cada AM. A longitudinal study of short- and long-term activity levels in male and female spontaneously hypertensive, Wistar-Kyoto, and Sprague-Dawley rats. Behav. Neurosci. 2003;117:271–282. doi: 10.1037/0735-7044.117.2.271. [DOI] [PubMed] [Google Scholar]
- 121.Kinkead B, Selz KA, Owens MJ, Mandell AJ. Algorithmically designed peptides ameliorate behavioral defects in animal model of ADHD by an allosteric mechanism. J. Neurosci. Methods. 2006;151:68–81. doi: 10.1016/j.jneumeth.2005.07.015. [DOI] [PubMed] [Google Scholar]
- 122.Vendruscolo Leandro, Terenina-Rigaldie Elena, Raba Frantz, Ramos André, Takahashi Reinaldo, Mormède Pierre. Behavioral and Brain Functions. 2006;2(1):21. doi: 10.1186/1744-9081-2-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Levin R, et al. Spontaneously Hypertensive Rats (SHR) present deficits in prepulse inhibition of startle specifically reverted by clozapine. Prog. Neuro-Psychopharmacology Biol. Psychiatry. 2011;35:1748–1752. doi: 10.1016/j.pnpbp.2011.06.003. [DOI] [PubMed] [Google Scholar]
- 124.Geyer MA, Krebs-Thomson K, Braff DL, Swerdlow NR. Pharmacological studies of prepulse inhibition models of sensorimotor gating deficits in schizophrenia: A decade in review. Psychopharmacology. 2001;156:117–154. doi: 10.1007/s002130100811. [DOI] [PubMed] [Google Scholar]
- 125.Hsieh MH, Swerdlow NR, Braff DL. Effects of background and prepulse characteristics on prepulse inhibition and facilitation: Implications for neuropsychiatric research. Biol. Psychiatry. 2006;59:555–559. doi: 10.1016/j.biopsych.2005.07.032. [DOI] [PubMed] [Google Scholar]
- 126.Peres FF, et al. A schizophrenia-like behavioral trait in the SHR model: Applying confirmatory factor analysis as a new statistical tool. Prog. Neuro-Psychopharmacology Biol. Psychiatry. 2018;85:16–22. doi: 10.1016/j.pnpbp.2018.03.021. [DOI] [PubMed] [Google Scholar]
- 127.Watanabe Y, et al. Brain dopamine transporter in spontaneously hypertensive rats. J. Nucl. Med. 1997;38:470–474. [PubMed] [Google Scholar]
- 128.Galeno TM, Van Hoesen GW, Brody MJ. Central amygdaloid nucleus lesion attenuates exaggerated hemodynamic responses to noise stress in the spontaneously hypertensive rat. Brain Res. 1984;291:249–259. doi: 10.1016/0006-8993(84)91257-5. [DOI] [PubMed] [Google Scholar]
- 129.Kunkler PE, Hwang BH. Lower GABAA receptor binding in the amygdala and hypothalamus of spontaneously hypertensive rats. Brain Res. Bull. 1995;36:57–61. doi: 10.1016/0361-9230(94)00164-v. [DOI] [PubMed] [Google Scholar]
- 130.Papa M, Sellitti S, Sadile AG. Remodeling of neural networks in the anterior forebrain of an animal model of hyperactivity and attention deficits as monitored by molecular imaging probes. Neuro. Biobehav. Res. 2000;24:149–156. doi: 10.1016/S0149-7634(99)00052-4. [DOI] [PubMed] [Google Scholar]
- 131.Viggiano D, Vallone D, Sadile A. Dysfunctions in dopamine systems and ADHD: Evidence from animals and modeling. Neural Plast. 2004;11:97–114. doi: 10.1155/NP.2004.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Li Q, et al. The usefulness of the spontaneously hypertensive rat to model attention-deficit/hyperactivity disorder (ADHD) may be explained by the differential expression of dopamine-related genes in the brain. Neurochem. Int. 2007;50:848–857. doi: 10.1016/j.neuint.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 133.Russell V, De Villiers A, Sagvolden T, Lamm M, Taljaard J. Differences between electrically-, ritalin- and D-amphetamine-stimulated release of [3H]dopamine from brain slices suggest impaired vesicular storage of dopamine in an animal model of Attention-Deficit Hyperactivity Disorder. Behav. Brain Res. 1998;94:163–171. doi: 10.1016/s0166-4328(97)00177-0. [DOI] [PubMed] [Google Scholar]
- 134.Meador-Woodruff JH, Clinton SM, Beneyto M, McCullumsmith RE. Molecular Abnormalities of the Glutamate Synapse in the Thalamus in Schizophrenia. Ann. N. Y. Acad. Sci. 2003;1003:75–93. doi: 10.1196/annals.1300.005. [DOI] [PubMed] [Google Scholar]
- 135.Rosenstock TR, Carvalho ACP, Jurkiewicz A, Frussa-Filho R, Smaili SS. Mitochondrial calcium, oxidative stress and apoptosis in a neurodegenerative disease model induced by 3-nitropropionic acid. J. Neurochem. 2004;88:1220–1228. doi: 10.1046/j.1471-4159.2003.02250.x. [DOI] [PubMed] [Google Scholar]
- 136.Carvalho ACP, et al. Bax affects intracellular Ca2+ stores and induces Ca2+ wave propagation. Cell Death Differ. 2004;11:1265–1276. doi: 10.1038/sj.cdd.4401508. [DOI] [PubMed] [Google Scholar]
- 137.Badawi Y, Ramamoorthy P, Shi G. Hypoxia-Inducible Factor 1 Protects Hypoxic Astrocytes against Glutamate Toxicity. ASN Neuro. 2012;4(4):231–41. doi: 10.1042/AN20120006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Willcox JM, Summerlee AJS. Relaxin protects astrocytes from hypoxia in vitro. PLoS One. 2014;9(3):e90864. doi: 10.1371/journal.pone.0090864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Kelleher Ja, Chan PH, Chan TY, Gregory Ga. Modification of hypoxia-induced injury in cultured rat astrocytes by high levels of glucose. Stroke. 1993;24:855–63. doi: 10.1161/01.str.24.6.855. [DOI] [PubMed] [Google Scholar]
- 140.Su Ruijun Jeanna, Neises Amanda, Zhang Xiao-Bing. Methods in Molecular Biology. New York, NY: Springer New York; 2014. Generation of iPS Cells from Human Peripheral Blood Mononuclear Cells Using Episomal Vectors; pp. 57–69. [DOI] [PubMed] [Google Scholar]
- 141.Naia L, et al. Activation of IGF-1 and Insulin Signaling Pathways Ameliorate Mitochondrial Function and Energy Metabolism in Huntington’s Disease Human Lymphoblasts. Mol. Neurobiol. 2014;51(1):331–48. doi: 10.1007/s12035-014-8735-4. [DOI] [PubMed] [Google Scholar]
- 142.Rosenstock TR, et al. Glutamate-induced alterations in Ca2+ signaling are modulated by mitochondrial Ca2+ handling capacity in brain slices of R6/1 transgenic mice. Eur. J. Neurosci. 2010;32:60–70. doi: 10.1111/j.14609568.2010.07268.x. [DOI] [PubMed] [Google Scholar]
- 143.Ribeiro M, et al. Glutathione redox cycle dysregulation in Huntington’s disease knock-in striatal cells. Free Radic. Biol. Med. 2012;53:1857–67. doi: 10.1016/j.freeradbiomed.2012.09.004. [DOI] [PubMed] [Google Scholar]
- 144.Ribeiro M, Rosenstock TR, Oliveira AM, Oliveira CR, Rego AC. Insulin and IGF-1 improve mitochondrial function in a PI-3K/Akt-dependent manner and reduce mitochondrial generation of reactive oxygen species in Huntington’s disease knock-in striatal cells. Free Radic. Biol. Med. 2014;74:129–44. doi: 10.1016/j.freeradbiomed.2014.06.023. [DOI] [PubMed] [Google Scholar]
- 145.Naia L, et al. Histone deacetylase inhibitors protect against pyruvate dehydrogenase dysfunction in huntington’s disease. J. Neurosci. 2017;8(37(10)):2276–2794. doi: 10.1523/JNEUROSCI.2006-14.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Naia L, et al. Comparative Mitochondrial-Based Protective Effects of Resveratrol and Nicotinamide in Huntington’s Disease Models. Mol. Neurobiol. 2017;54(7):5385–8399. doi: 10.1007/s12035-016-0048-3. [DOI] [PubMed] [Google Scholar]
- 147.Naia L, et al. Insulin and IGF-1 regularize energy metabolites in neural cells expressing full-length mutant huntingtin. Neuropeptides. 2016;58:73–81. doi: 10.1016/j.npep.2016.01.009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analysed during this study are included in this published article (and its Supplementary Information files).