Highlights
-
•
EMA data were analyzed using network analysis (e.g., temporal networks).
-
•
Suicidal ideation at t was predicted by itself and perceived burdensomeness at t – 1.
-
•
Suicidal ideation at t − 1 predicted perceived burdensomeness, depression etc. at t.
-
•
At the same beep, suicidal ideation was related to all variables in the network.
-
•
Patients with higher average suicidal ideation had higher average hopelessness.
1. Introduction
Suicidal behavior may emerge as the result of an interaction between many different psychological, social, and biological variables (Hawton and Van Heeringen, 2000; O'Connor and Nock, 2014). Analysis from traditional epidemiological studies gave insight into the role of more static risk factors of suicidal behavior, such as sex and a history of depression (Brown et al., 2000; Wang et al., 2015), but neglected the dynamic nature of suicidal ideation and its psychological risk factors. For that reason, recent studies made use of a method called ecological momentary assessment (EMA), using repeated measurements of a combination of fluctuating state-like factors and short follow-up intervals of minutes or hours.
1.1. EMA studies in suicidology
Within the field of suicide research, real time monitoring via EMA has just recently been introduced. First EMA studies not only demonstrated high fluctuations of suicidal ideation (SI) over time, even from hour to hour (cf. preliminary data analysis by Hallensleben et al., 2017; Kleiman et al., 2017), but also large intrapersonal differences in fluctuations. These results show that a considerable amount of variance of SI is caused by within-person processes over time. Kleiman et al. (2017) reported similar results not only for SI, but also for psychological risk factors associated with SI, such as hopelessness, perceived burdensomeness, and thwarted belongingness. Importantly, the well-known psychological risk factors hopelessness, perceived burdensomeness, and thwarted belongingness co-occurred with SI, but did not predict SI at short-term follow up.
By the end of August 2017, data collection from the comprehensive AMBAS study (Ambulatory Assessment of Suicidality, Hallensleben et al., 2017; Forkmann et al., 2018) was completed. The aim of this EMA study was to investigate proximal risk factors for SI based on the assumptions of the Interpersonal Theory of Suicidal Behavior (IPTS; Joiner, 2007; Van Orden et al., 2010). According to the IPTS, high levels of perceived burdensomeness and thwarted belongingness can lead to SI. Multilevel analyses were used in order to test these assumptions (cf. Hallensleben et al., 2019). The analyses of the complete EMA data containing 74 inpatients with a depressive disorder and current/lifetime suicidal ideation revealed two major findings. First, perceived burdensomeness, thwarted belongingness, depressive feelings, and hopelessness co-occurred with SI within the same assessment, even when controlling for SI at t − 1. Second, hopelessness, perceived burdensomeness (but not thwarted belongingness), and SI at t − 1 prospectively predicted SI at t (Hallensleben et al., 2019).
Differences between cross-sectional and temporal analyses have also been reported by Kleiman and Nock (2018) and Ben-Zeev et al. (2012), which led Kleiman and Nock to distinguish between correlates, predictors, and predictors of change for SI (Kleiman and Nock, 2018).
1.2. A network perspective
In this paper, we want to extend the findings of Hallensleben et al., 2017, Hallensleben et al., 2019 by re-analyzing the EMA data from the AMBAS study using network analysis. Although the method of network analysis is not new, there has been an increasing interest in thinking of psychological disorders such as depression as a network of interacting symptoms (Bringmann et al., 2015; De Beurs et al., 2017; Epskamp et al., 2012; Epskamp et al., 2018; van Borkulo et al., 2015; Wigman et al., 2015).
According to the network perspective in psychopathology, mental health problems (in our case SI) develop as a result of interacting symptoms or risk factors (Borsboom, 2017). For example, if one has trouble sleeping, this may result in concentration problems, which may result in more rumination, which may result in higher levels of SI. When the dynamical relations between risk factors are sufficiently strong, they can be self-sustained via a negative feedback loop (Borsboom, 2017). By presenting all possible relationships between all variables in one clear graph, network analysis can guide researchers and clinicians towards more complex and dynamic thinking about mental disorders (Bringmann and Eronen, 2018). Indeed, inspecting network structures of SI as well as well-known risk factors over time should result in a more comprehensive understanding of how different risk factors relate to each other and to SI, whereas previous analyses only focused on the outcome of interest (cf. Hallensleben et al., 2019; see Fig. 1).
Fig. 1.
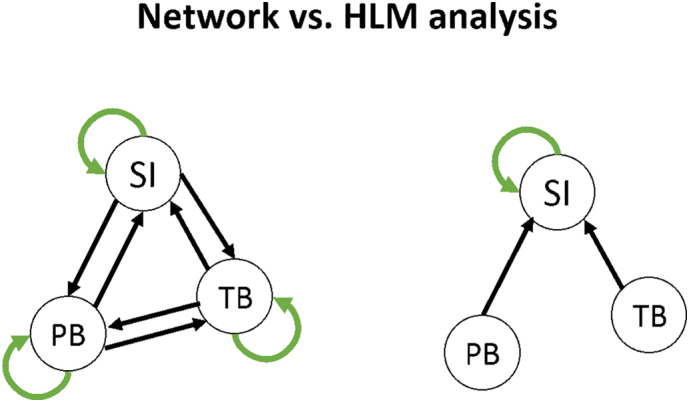
Differences between network and HLM analysis as used in Hallensleben et al. (2019).
Network analysis has recently made its way into suicide research (De Beurs, 2017; De Beurs et al., 2018; De Beurs et al., 2017). As suicidal behavior is not a mental disorder such as depression, the rationale of thinking about suicidal behavior within a network perspective requires a bit more explanation. One proposed hypothesis from the network perspective on suicidal behavior is that a suicide attempt is the result of the interaction between different risk factors, such as hopelessness, depression, impulsivity, and suicidal ideation (De Beurs, 2017). A suicide attempt is then argued to arise from the interaction between these different risk factors. In a recent study, suicidal ideation was represented as a node in the network, a single symptom, just like all other 20 risk factors, such as entrapment and perceived burdensomeness (De Beurs et al., 2019). The main research question was how all other variables interact with suicidal ideation, either directly or indirectly, and how these risk factors interact among each other. Network analysis offers a unique opportunity to visualize and quantify the relations between suicidal ideation and all other variables. Results showed that many more variables are directly related to suicidal ideation than current theories propose, even when controlling for all other symptoms in the network. Additionally, all risk factors within the network were connected with each other, none of them being isolated.
1.2.1. Estimating a temporal network with EMA data
Network analysis has mostly been applied to cross-sectional data (De Beurs et al., 2018, De Beurs et al., 2019), but can also be applied to EMA data. With time series data, one can estimate a temporal network, often via vector autoregression techniques (VAR). In VAR, a variable at a certain time point t is predicted by the same variable at the previous time point t − 1 (autoregressive effects) and all other variables at t − 1 (cross-lagged effects). These autoregressive and cross-lagged effects can be quantified and visualized in a temporal network (cf. Bringmann et al., 2013). By allowing VAR coefficients to differ across individuals via multilevel modeling, it is possible to model and visualize time dynamics at the group level (for more detailed information see in the Methods section). In the graphical representation of the network, variables are presented as nodes. A variable being associated with another variable over time is graphically represented by an edge with an arrowhead towards the other node. These networks are called temporal networks, as they can be indicative of potential causality given that one variable preceded the other in time. This time order is a necessary (but not sufficient) condition for causality. The relation over time could also be explained by variables that had not been measured. Therefore, temporal networks are mainly useful for hypothesis generating. As in our study the time between two assessments was between 30 and 120 min, the temporal network offers insights into relations between variables within this short period of time. In order to get insight into relations that occur much faster, during the same assessment, one can use another network, the contemporaneous network.
1.2.2. Contemporaneous network with EMA data
Epskamp et al. (2018) introduced an additional network one can estimate using EMA data, called a contemporaneous (or non-temporal) network. One can use the associations between the residuals of the temporal network (partial correlations) resulting from associations between variables that are not explained by the current chosen time interval, the chosen lag, or anything else that is not explicitly measured and modeled. These correlations are then used to estimate a partial correlation network structure. In this contemporaneous network, each variable is again represented as a node. However, the edges between two nodes are graphically not presented by arrowheads but by lines, representing cross-sectional associations within one measurement (and not temporally directed effects). The edges now represent the partial correlation obtained after controlling for both temporal effects and all other variables in the same window of measurement (Epskamp et al., 2017, Epskamp et al., 2018; Fisher et al., 2017).
1.2.3. Between-subjects network with EMA data
The temporal as well as the contemporaneous networks were within-persons networks. When data is collected from multiple subjects, it is also possible to estimate a between-persons network using EMA data. Between-subjects predictors are calculated using the covariance structure of stationary means (over time in case of EMA data). For instance, each person has his/her own means for SI and perceived burdensomeness over time. One can then obtain a correlation between the personal means of SI and perceived burdensomeness across persons over time. A positive correlation would imply that people with a high mean score for SI also tend to have a high mean score for perceived burdensomeness.
In sum, network analysis extends previously used multilevel analysis by controlling for autoregressive effects of all variables included in the network (not only autoregressive effects of SI), by revealing temporal and contemporaneous associations as well as between-subjects differences, and by offering a visual representation of the relations between all assessed variables.
In this study, we hypothesized, first, that we would replicate the findings of our previous multilevel analysis (cf. Hallensleben et al., 2019): SI at one measurement t would be related to perceived burdensomeness, thwarted belongingness, hopelessness, and depressiveness at the same measurement t (contemporaneous network), and predicted by perceived burdensomeness, hopelessness, and itself at t − 1 over time (temporal network). We further expected to replicate findings by Hallensleben et al. (2019) when controlling not only for autoregressive effects of SI but also for autoregressive effects of all other variables as well as for all cross-lagged effects. Moreover, we were interested in examining further cross-lagged associations between all variables in the network (beyond associations with SI). Finally, we assumed that participants with high levels of perceived burdensomeness, thwarted belongingness, hopelessness, and depressiveness on average would also show high levels of SI.
2. Material and methods
2.1. Sample and study procedure
Seventy-four psychiatric inpatients with a primary unipolar depressive disorder (major depression, dysthymia) and current or lifetime SI were included in the EMA study (see Table 1; cf. Forkmann et al., 2018). Patients were 37.6 years on average (SD = 14.3, ranging from 18 to 85 years). 71.6% were female. Patients were recruited in the psychiatric department of the University Hospital Leipzig and the HELIOS Park-Klinikum Leipzig between September 2015 and August 2017. Suicidality was assessed by using the Suicide Behaviors Questionnaire Revised (SBQ-R; Kleiman and Nock, 2018; Osman et al., 2001) as well as the Structured Clinical Interview for DSM-IV (SCID-I; Wittchen et al., 1997). Patients with a score ≥8 in the SBQ-R or reporting at least suicidal ideation in the SCID-I were included in the sample. Since mood, stress reactivity, and the experience and the impact of positive events is distinctive in patients with a Major Depression, we did not include patients with bipolar disorders, substance use disorders in the past year, current psychotic symptoms, and primary diagnosis of personality disorder in this study. Further exclusion criteria were insufficient knowledge of German language, and IQ < 85 in a language-based intelligence test (German “Mehrfachwahl-Wortschatz-Intelligenztest”, MWT-B; Lehrl, 2005). For an overview of the study procedure and a flow chart of study inclusion see Forkmann et al. (2018). Table 1 summarizes the clinical characteristics of the study sample (cf. Forkmann et al., 2018).
Table 1.
Clinical characteristics of the study sample (n = 74) and for males vs. females.
| Total sample |
Males (n = 21) |
Females (n = 53) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | M (SD) | n | % | M (SD) | n | % | M (SD) | |
| Diagnoses (SCID-I interview) | |||||||||
| Major depression | 69 | 93.2 | 18 | 85.7 | 51 | 96.6 | |||
| Severity of current episode: mild | 10 | 13.5 | 3 | 14.3 | 7 | 13.2 | |||
| Severity of current episode: moderate | 44 | 59.5 | 10 | 47.6 | 34 | 64.2 | |||
| Severity of current episode: severe | 15 | 20.2 | 5 | 23.8 | 10 | 18.9 | |||
| Number of depressive episodes (lifetime) | 3.9 (3.4) | 4.6 (4.9) | 3.6 (2.5) | ||||||
| Dysthymia | 5 | 6.8 | 3 | 14.3 | 2 | 3.8 | |||
| Comorbid anxiety disorderb | 16 | 21.6 | 2 | 9.5 | 14 | 26.4 | |||
| Comorbid obsessive-compulsive disorderb | 3 | 4.1 | 0 | 0 | 3 | 5.7 | |||
| Comorbid somatic symptom disorderb | 4 | 5.4 | 3 | 14.3 | 1 | 1.9 | |||
| Comorbid eating disorderb | 3 | 4.1 | 0 | 0 | 3 | 5.7 | |||
| Symptom severity (questionnaires) | |||||||||
| Suicidal ideation (BSS) | 9.3 (9.0) | 12.1 (11.1) | 8.2 (7.9) | ||||||
| Depressiveness (DESC)a | 25.9 (6.2) | 26.7 (6.3) | 25.6 (6.2) | ||||||
| Above DESC cut-off (≥11) | 74 | 100 | 21 | 100 | 53 | 100 | |||
Note. Data for the total sample have also been published in Forkmann et al. (2018).
Any diagnosis current or lifetime.
After an extensive baseline-assessment (Forkmann et al., 2018), participants underwent a 6-days-EMA-assessment with 10 signal-contingent assessments per day using an EMA software on Android smartphones (movisensXS©) resulting in a maximum of 60 assessments per participant. The EMA signals occurred randomly between 8:00 am and 8:00 pm with at least 30 minute in-between prompts. Participants could postpone a prompt for 5, 10, or 15 min if they were not able to answer the questions immediately (e.g., due to therapeutic sessions) and they had the possibility to reject a prompt. The dataset consisted of 4440 observations (60 assessments on level 1 ∗ 74 persons on level 2). Participants completed 89.7% of the EMA assessments on average (min = 75%, max = 100%), resulting in 4295 valid observations. Missing data was handled via listwise deletion. All data was directly transferred and could be monitored using a web-based platform enabling the research team to check regularly on compliance rates. For more detailed information about the study protocol, please see Forkmann et al. (2018). All participants provided written informed consent prior to participation. The study was approved by the ethics committee of the Medical Faculty of the University of Leipzig (No. 388-13-16122013).
2.2. Measures
During the EMA assessment, patients rated their momentary SI, perceived burdensomeness, thwarted belongingness, depressiveness, hopelessness, positive affect, and anxiety. The EMA items were either newly developed or selected from respective retrospective self-report inventories, assessing the construct of interest regarding item-total correlation, item content, and wording. In a second step, wording of all items was adapted to optimally relate to the actual moment. The whole EMA assessment comprised 28 items (for items see Forkmann et al., 2018). We used 16 for network analysis: SI (2 passive, 2 active), thwarted belongingness (2 items), perceived burdensomeness (2 items), depressiveness (2 items), hopelessness (2 items), anxiety (2 items), and positive affect (2 items). The rest of the EMA items, which we did not analyze, assessed mood (6 items), context (activity: 1 item, company: 4 items), and medication (1 item) since the last measurement. We decided to delete them from analysis for two reasons: 1) we focused on the impact of the interpersonal variables perceived burdensomeness and perceived burdensomeness and well-known risk factors, such as depression and hopelessness, 2) we thought that our data did not have the power to include even twelve more items.
2.3. Analysis
In order to estimate the different network structures over all participants, we applied multilevel vector autoregression (mlVAR) models on the data as implemented within the mlVAR package in R (Epskamp et al., 2017). Temporal dynamics within individuals are estimated by regressing scores of a symptom at time t on a previous (i.e. lagged) value of itself at t − 1 (AR: autoregression, Chatfield, 2016; Shumway and Stoffer, 2000). Vector autoregressive modelling (VAR) indicates that all variables at time t are regressed on a t − 1 version of themselves, resulting in a vector of lagged regression coefficients (fixed effects). The multilevel modelling allows the VAR coefficients to differ between individuals (random effects). Hence, a temporal network can be estimated, i.e. a network visualizing the temporal effects of symptoms (e.g. Bos et al., 2017; Bringmann et al., 2017; Snippe et al., 2017; Wigman et al., 2015). To visualize the temporal network in a two-dimensional graph, we used the Fruchterman-Reingold (FR) algorithm. This algorithm aims to place nodes that are not central (i.e. have little connection to other nodes) at the periphery of the network, whereas central, highly connected nodes are placed towards the centre. FR is the most frequently used placing algorithm within network analysis, although alternatives exist (Jones et al., 2018).
To obtain estimates of between-subject effects, the sample means of every subject can be included as predictors at the subject level (except for the mean of the dependent variable; Hamaker and Grasman, 2015; Hoffman and Stawski, 2009; Curran and Bauer, 2011). Finally, the contemporaneous network was estimated using the residuals of the multilevel model that was used to estimate the temporal and between-subjects effects. These residuals were used to estimate multilevel models that estimate the association between the residuals of one variable from the residuals of all other variables at the same time points.
For a more detailed discussion about estimation and differences between each of the three networks, we refer to Epskamp et al. (2018). All participants were included in the analysis. Variables were standardized before estimation and scaled within persons via mlVAR. As the last assessment of the day is rather not correlated with the first assessment of the next day, we added a row of missing values between consecutive days. All networks are graphed using the qgraph package in R (Epskamp et al., 2012). We further did not detrend the data because the Dickey-Fuller test indicated all variables to be stationary over time (all p < .01).
3. Results
Means and standard deviations for all EMA scales across all 60 assessments are presented in Table 2 (cf. Forkmann et al., 2018).
Table 2.
Descriptive statistics of the EMA scales for total sample and males vs. females averages over all 60 assessments.
| EMA-constructs | Range | Total sample |
Males |
Females |
|||
|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | ||
| SI | 4–20 | 7.7 | 3.6 | 8.0 | 3.4 | 7.6 | 3.7 |
| PB | 2–10 | 5.4 | 2.1 | 5.4 | 1.8 | 5.4 | 2.2 |
| TB | 2–10 | 5.1 | 1.9 | 5.0 | 1.9 | 5.2 | 2.0 |
| D | 2–10 | 5.9 | 1.8 | 5.5 | 1.8 | 6.0 | 1.8 |
| H | 2–10 | 5.5 | 2.2 | 5.5 | 2.4 | 5.5 | 2.2 |
| PA | 2–10 | 4.6 | 1.4 | 4.8 | 0.9 | 4.5 | 1.5 |
| A | 2–10 | 5.3 | 1.4 | 5.2 | 1.2 | 5.3 | 1.4 |
Note. Data for the total sample have also been published by Forkmann et al. (2018). No significant differences in means between males vs. females (all p > .05).
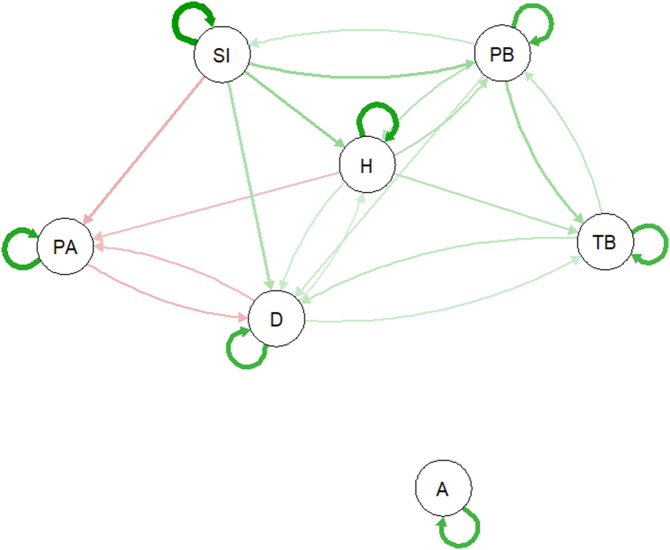
3.1. Temporal network
As illustrated in the temporal network (see Fig. 2), SI at time point t was solely predicted by perceived burdensomeness (fixed effects coefficient: 0.06, p < .05) and SI at t − 1 (fixed effects coefficient: 0.26, p < .001). While all variables predicted themselves in the consecutive measurement, SI predicted itself in the strongest manner, as depicted by the thickest directed connection and the largest coefficient in the temporal network (see Table A-1 in the Appendix for all coefficients). SI, however, predicted perceived burdensomeness (0.10, p < .001), hopelessness (0.11, p < .001), depressiveness (0.08, p = .001), and positive affect (−0.08, p < .001) over time. Relations between SI and thwarted belongingness were missing; neither did SI predict thwarted belongingness (0.03, p > .05), nor did thwarted belongingness predict SI (0.02, p > .05; for more detailed information see Table A-1 in the Appendix). Anxiety was only predicted by itself, but neither influenced nor was influenced by any other variables at t − 1.
Fig. 2.
Temporal network of the fixed effects with green lines representing positive associations and red lines negative associations; the thicker the line, the stronger the association; SI: suicidal ideation, PB: perceived burdensomeness, TB: thwarted belongingness, PA: positive affect, D: depressiveness, H: hopelessness, A: anxiety. Non-significant edges were omitted.
3.2. Contemporaneous network and between-subjects network
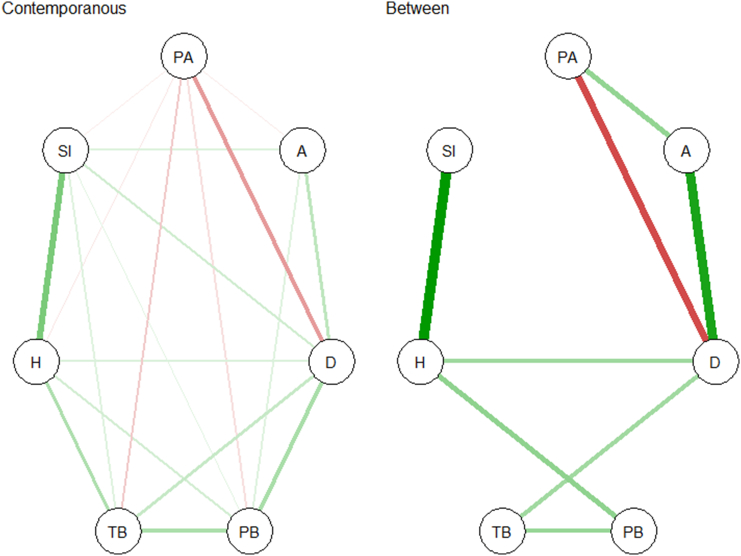
Fig. 3 presents the contemporaneous network (left). SI is most strongly associated with hopelessness. Furthermore, SI is associated with all other variables. As expected, positive affect had a strong negative correlation with depression (for more detailed information see Table A-2 in the Appendix).
Fig. 3.
Temporal, contemporaneous, and between-subjects network: green lines representing positive associations, red lines representing negative associations; the thicker the line, the stronger the association; SI: suicidal ideation, PB: perceived burdensomeness, TB: thwarted belongingness, PA: positive affect, D: depressiveness, H: hopelessness, A: anxiety. Non-significant edges were omitted.
With regard to the between-subjects network (Fig. 3, right), participants that on average scored high on hopelessness also scored high on average on SI. No other between-subjects relation between SI and any other variables was found. As expected, participants that scored high on depression also scored high on anxiety and hopelessness. They also scored low on positive affect and high on thwarted belongingness, whereas they did not score high on perceived burdensomeness (for more detailed information see Table A-3 in the Appendix).
4. Discussion
To the best of our knowledge, this is the first study in suicide research applying network analysis on EMA data to better understand the relation between SI and several psychological risk factors. A sample of 74 patients with a depressive disorder and current/lifetime SI reported their momentary level of SI, thwarted belongingness, perceived burdensomeness, and further risk factors (e.g. hopelessness and depressiveness) ten times a day over a period of six days. We computed and graphed three different networks: a temporal, a contemporaneous, and a between-subjects network.
The temporal network revealed, first, that SI at t was solely predicted by itself and the level of perceived burdensomeness at t − 1 and, second, that SI at t − 1 predicted almost all the other variables in the temporal network at t. This differs somewhat from the results of the multilevel analysis where, besides SI and perceived burdensomeness, hopelessness at t − 1 was also predictive of SI at t (Hallensleben et al., 2019). The differences in model outcomes might be explained by different ways of estimating residuals. In VAR, all variables are fitted on a lagged version of themselves and cross-lagged version of all other variables in the network, whereas in multilevel analysis only the dependent variable is explained as a function of a lagged version of itself and cross-lagged versions of all other variables in the regression equation. The findings are in line with an EMA study by Kleiman et al. (2017), reporting that SI mainly predicts itself, while other variables are less useful in order to predict SI over time. The contemporaneous and between-subjects networks, however, did confirm the strong relationship between SI and hopelessness. Within a much shorter time frame than 30 to 120 min (lag-1), hopelessness is strongly associated with SI. Additionally, patients with higher average SI scores also tended to have higher hopelessness scores. This is in line with both EMA studies on SI (Hallensleben et al., 2019; Kleiman et al., 2017) and more traditional epidemiological studies (e.g. Franklin et al., 2017). The contemporaneous network also revealed a direct relation between SI, perceived burdensomeness, and thwarted belongingness. These results have also been found by Kleiman and Nock (2018), concluding that well-known risk factors, such as hopelessness and perceived burdensomeness, are most useful to predict SI at the moment, but less useful to predict SI over time.
Our as well as previous findings by Kleiman and Nock (2018) and Kleiman et al. (2017) are not in line with the assumptions of the IPTS, stating that perceived burdensomeness and thwarted belongingness are the main predictors of SI over time (Joiner, 2007; Van Orden et al., 2010). It might be possible that the relationship between the IPTS variables and SI follow another time dynamic than captured within our analysis. According to the results from the contemporaneous network, both thwarted belongingness and perceived burdensomeness are related to SI at the same measurement suggesting faster unfolding relations. However, it might also be possible that thwarted belongingness effects suicidal ideation slower than after 120 min, for instance, after one full day, or even a week. In the existing theory, there is no explicit mentioning of a time frame in which associations between thwarted belongingness, perceived burdensomeness, and suicidal ideation unfold. At least with our design, momentary intrusive suicidal thoughts seem to make people feel hopeless and a burden for others 30 to 120 min afterwards, which in turn might make them feel isolated (in terms of higher thwarted belongingness) further 30 to 120 min later. What causes SI in the first run, besides SI itself and perceived burdensomeness, might either happen faster, for instance within the same assessment, as was the case for hopelessness, or in a time frame between approximately 5 (after one assessment) and 30 min (before the next assessment). Another reason might be that there are variables not assessed in the current study that might predict SI. If anything, these results indicate that the (temporal) relation between psychological risk factors and SI is more complex than theorized. Indeed, based on their EMA results, Kleiman and Nock (2018) suggested a distinction between different ways of how variables can influence SI. While some variables might be associated with SI at the same measurement, others seem to predict SI or the change in SI at the subsequent measurement (cf. Kleiman et al., 2017). Regarding the IPTS variables, only perceived burdensomeness had a direct temporal impact on SI. This is in line with other studies reporting perceived burdensomeness to be associated more directly with SI compared to thwarted belongingness (Hames et al., 2015; Ma et al., 2016).
As expected, positive affect was negatively related to all other variables. We found that SI at t resulted in less positive affect at t − 1, supporting the hypothesis of Kleiman et al. (2018) that the presence of SI leads to shifts in affect. However, there was no support for a negative feedback loop, as we did not find that less positive affect in return also influenced SI over time. One reason for this discrepancy with the study of Kleiman et al. (2018) might be the shorter period in our EMA study from one beep to the next (1.5 vs. 4 to 8 h). Moreover, even when a node has no impact on other variables in the temporal network, it still can have an impact on subsequent variables by being central in the contemporaneous network (Epskamp et al., 2018).
Anxiety and thwarted belongingness were the only variables in the temporal network that had no relation to SI, at least in our study's timeframe of 30 to 120 min. Literature on thwarted belongingness does indeed suggest that it influences SI via perceived burdensomeness (e.g., Rogers and Joiner, 2019). The role of anxiety in the development of SI is less clear, since results of prospective studies are mixed – some confirmed and some falsified the effect of anxiety disorders on SI (Abreu et al., 2018; Bolton et al., 2010; Oquendo et al., 2004). Future EMA studies should replicate our findings to better understand the potential association of self-reported momentary anxiety and SI.
A limitation of this study is the sample only consisting of patients with a Major Depression. Hence, we should be cautious when concluding for patients with any other diagnosis and suicidal ideation. On the other hand, our findings regarding the assumptions of the IPTS are in line with findings reported by other authors, for instance Kleiman et al. (2017), who examined inpatients, admitted for suicide risk. Moreover, the sample only consists of inpatients also slightly diminishing ecological validity. Future research should replicate our findings for outpatient samples with different diagnosis.
Furthermore, one may assume that inpatients in contrast to outpatients or persons not in therapy show less variability in variables, such as suicidal ideation, thwarted belongingness, perceived burdensomeness, etc., because the number and nature of interpersonal events might differ in an inpatient setting compared to being at home. However, we found considerable variance within person over time (at level 1, e.g., 48% of variance for TB, 38% of variance for PB), contradicting this assumption.
We further do not know whether we chose the appropriate EMA design with ten measurements a day every 30 to 120 min and between 8 am and 8 pm. Using this interval, we might have missed important events in the late evenings, early mornings, and during the nights. However, we wanted to warrant the participants' compliance by minimizing the effort and burden for participants (already being prompted ten times a day) and not interfering with the participants' natural sleep-wake rhythm. Moreover, we tried to avoid unnecessary missings. Statistically, this gap has been taken into account by not correlating the last assessment of one day with the first assessment of the consecutive day.
Another limitation is that important risk factors for SI, such as defeat and entrapment, were not included in the study. This kind of data is currently being collected in the CASPAR study and will probably result in more predictive power over time (Nuij et al., 2018). Although suicide research needs objective ways of measuring suicide risk (i.e., assessment not biased by opinion or interpretation) and should also include indirect measures of suicide-related variables as well as behavioral proxies (Chu et al., 2017; Glenn and Nock, 2014), we only used self-reports. Moreover, our design and sampling strategy (i.e. 10 beeps per day with at least 30 min within beeps) might not capture the natural course of SI and its risk factors (Ebner-Priemer and Trull, 2012; Verhagen et al., 2016). It is also likely that we were underpowered to detect more subtle dynamic relations. For example, one would expect positive affect to be related to all other variables over time, but this was not confirmed in our network. Future research is required using extended observations of several weeks and comparing different sampling strategies, leading to more insight in the individual dynamics of SI. Finally, the connections within the networks should only be interpreted as indications of potential causal relationships, and serve as hypothesis generating networks. True causal relationships can only be found after some type of intervention.
In perspective, networks based on EMA data might also be used in psychotherapy. Individual courses of SI and risk factors, such as perceived burdensomeness, thwarted belongingness, hopelessness, and depressiveness (and further variables of interest), could be measured at the beginning of the therapeutic process and be used for individual networks. This kind of information could then be discussed with the patient during therapeutic sessions in order to identify individual risk factors of suicidality (such as Kroeze et al., 2017). Interestingly, we observed intra-individual differences in networks revealing different associations and risk factors per person.
With regard to the IPTS, the networks show that the relationship between PB and TB is not as straight forward as assumed in the theory. However, our findings should be replicated before we can better understand the dynamic relation between perceived burdensomeness, thwarted belongingness, and SI. Moreover, since the IPTS is a relatively young theory, it remains unclear whether a satisfactory operationalization of the IPTS constructs has already been attained by the available instruments and items (i.e. the INQ; Hallensleben et al., 2016).
Taken together, the network analysis shows that the relation between known risk factors and SI over time is more complex than theorized or presented in epidemiological studies. As stated by Kleiman and Nock (2018), risk factors can be associated with, predictive of, or related to change in SI. Network analysis of EMA data extends our previously used multilevel analysis by offering a visualization of the relation between all variables and an insight into both the within and between-subjects effects.
Acknowledgments
Acknowledgments
This work was supported by research grants no. SP 1556/1-1, GL 818/1-1 and FO 784/1-1 from the German Research Foundation.
Role of the funding source
The supporters had no role in the design, analysis, interpretation, or publication of this study.
Declaration of competing interest
We have no conflicts of interest to declare.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.invent.2019.100292.
Appendix A. Supplementary data
Supplementary tables
References
- Abreu L., Oquendo M., Galfavy H., Burke A., Grunebaum M., Sher L.…Lafer B. Are comorbid anxiety disorders a risk factor for suicide attempts in patients with mood disorders? A two-year prospective study. European Psychiatry. 2018;47:19–24. doi: 10.1016/j.eurpsy.2017.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Zeev D., Young M.A., Depp C.A. Real-time predictors of suicidal ideation: mobile assessment of hospitalized depressed patients. Psychiatry Res. 2012;197(1):55–59. doi: 10.1016/j.psychres.2011.11.025. [DOI] [PubMed] [Google Scholar]
- Bolton J.M., Pagura J., Enns M.W., Grant B., Sareen J. A population-based longitudinal study of risk factors for suicide attempts in major depressive disorder. J. Psychiatr. Res. 2010;44(13):817–826. doi: 10.1016/j.jpsychires.2010.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsboom D. A network theory of mental disorders. World Psychiatry. 2017;16(1):5–13. doi: 10.1002/wps.20375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bos F.M., Snippe E., de Vos S., Hartmann J.A., Simons C.J., van der Krieke L.…Wichers M. Can We Jump from Cross-Sectional to Dynamic Interpretations of Networks Implications for the Network Perspective in Psychiatry. Psychotherapy and psychosomatics. 2017;86(3):175–177. doi: 10.1159/000453583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bringmann L.F., Eronen M.I. Don’t blame the model: reconsidering the network approach to psychopathology. Psychol. Rev. 2018;125(4):606. doi: 10.1037/rev0000108. [DOI] [PubMed] [Google Scholar]
- Bringmann L.F., Vissers N., Wichers M., Geschwind N., Kuppens P., Peeters F.…Tuerlinckx F. A network approach to psychopathology: new insights into clinical longitudinal data. PloS one. 2013;8(4) doi: 10.1371/journal.pone.0060188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bringmann L., Lemmens L., Huibers M., Borsboom D., Tuerlinckx F. Revealing the dynamic network structure of the Beck Depression Inventory-II. Psychol. Med. 2015;45(4):747–757. doi: 10.1017/S0033291714001809. [DOI] [PubMed] [Google Scholar]
- Bringmann L.F., Hamaker E.L., Vigo D.E., Aubert A., Borsboom D., Tuerlinckx F. Changing dynamics: time-varying autoregressive models using generalized additive modeling. Psychol. Methods. 2017;22(3):409. doi: 10.1037/met0000085. [DOI] [PubMed] [Google Scholar]
- Brown G.K., Beck A.T., Steer R.A., Grisham J.R. Risk factors for suicide in psychiatric outpatients: a 20-year prospective study. J. Consult. Clin. Psychol. 2000;68(3):371–377. [PubMed] [Google Scholar]
- Chatfield C. CRC press; 2016. The Analysis of Time Series: An Introduction. [Google Scholar]
- Chu C., Buchman-Schmitt J.M., Stanley I.H., Hom M.A., Tucker R.P., Hagan C.R.…Ringer F.B. The interpersonal theory of suicide: A systematic review and meta-analysis of a decade of cross-national research. Psychological bulletin. 2017;143(12):1313. doi: 10.1037/bul0000123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curran P.J., Bauer D.J. The disaggregation of within-person and between-person effects in longitudinal models of change. Annu. Rev. Psychol. 2011;62:583–619. doi: 10.1146/annurev.psych.093008.100356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Beurs D. Network analysis: a novel approach to understand suicidal behaviour. Int. J. Environ. Res. Public Health. 2017;14(3):219. [Google Scholar]
- De Beurs D.P., van Borkulo C.D., O’Connor R.C. Association between suicidal symptoms and repeat suicidal behaviour within a sample of hospital-treated suicide attempters. Br. J. Psychiatry Open. 2017;3(3):120–126. doi: 10.1192/bjpo.bp.116.004275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Beurs D., Vancayseele N., van Borkulo C., Portzky G., van Heeringen K. The association between motives, perceived problems and current thoughts of self-harm following an episode of self-harm. A network analysis. J. Affect. Disord. 2018;240:262–270. doi: 10.1016/j.jad.2018.07.047. [DOI] [PubMed] [Google Scholar]
- De Beurs D., Fried E., Wetherall K., Cleare S., O’Connor D.B., Ferguson E.…O’Connor R.C. Exploring the psychology of suicidal ideation: a theory driven network analysis. Behaviour research and therapy. 2019;120 doi: 10.1016/j.brat.2019.103419. [DOI] [PubMed] [Google Scholar]
- Ebner-Priemer U., Trull T. Handbook of Research Methods for Studying Daily Life. 2012. Investigating temporal instability in psychological variables: Understanding the real world as time dependent; pp. 423–439. [Google Scholar]
- Epskamp S., Cramer A.O., Waldorp L.J., Schmittmann V.D., Borsboom D. qgraph: network visualizations of relationships in psychometric data. J. Stat. Softw. 2012;48(4):1–18. [Google Scholar]
- Epskamp S., Deserno M.K., Bringmann L.F. mlVAR: multi-level vector autoregression. 2017. https://CRAN.R-project.org/package=mlVAR from.
- Epskamp S., van Borkulo C.D., van der Veen D.C., Servaas M.N., Isvoranu A.-M., Riese H., Cramer A.O. Personalized network modeling in psychopathology: the importance of contemporaneous and temporal connections. Clin. Psychol. Sci. 2018;6(3):416–427. doi: 10.1177/2167702617744325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher A.J., Reeves J.W., Lawyer G., Medaglia J.D., Rubel J.A. Exploring the idiographic dynamics of mood and anxiety via network analysis. J. Abnorm. Psychol. 2017;126(8):1044. doi: 10.1037/abn0000311. [DOI] [PubMed] [Google Scholar]
- Forkmann T., Boecker M., Wirtz M., Glaesmer H., Brähler E., Norra C., Gauggel S. Validation of the Rasch-based Depression Screening in a large scale German general population sample. Health Qual. Life Outcomes. 2010;8:105. doi: 10.1186/1477-7525-8-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forkmann T., Spangenberg L., Rath D., Hallensleben N., Hegerl U., Kersting A., Glaesmer H. Assessing suicidality in real time: a psychometric evaluation of self-report items for the assessment of suicidal ideation and its proximal risk factors using ecological momentary assessments. J. Abnorm. Psychol. 2018;127(8):758. doi: 10.1037/abn0000381. [DOI] [PubMed] [Google Scholar]
- Franklin J.C., Ribeiro J.D., Fox K.R., Bentley K.H., Kleiman E.M., Huang X.…Nock M.K. Risk factors for suicidal thoughts and behaviors: A meta-analysis of 50 years of research. Psychological bulletin. 2017;143(2):187. doi: 10.1037/bul0000084. [DOI] [PubMed] [Google Scholar]
- Glenn C.R., Nock M.K. Improving the short-term prediction of suicidal behavior. Am. J. Prev. Med. 2014;47(3):S176–S180. doi: 10.1016/j.amepre.2014.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallensleben N., Spangenberg L., Kapusta N., Forkmann T., Glaesmer H. The German version of the Interpersonal Needs Questionnaire (INQ)–dimensionality, psychometric properties and population-based norms. J. Affect. Disord. 2016;195:191–198. doi: 10.1016/j.jad.2016.01.045. [DOI] [PubMed] [Google Scholar]
- Hallensleben N., Spangenberg L., Forkmann T., Rath D., Hegerl U., Kersting A.…Glaesmer H. Investigating the Dynamics of Suicidal Ideation. Crisis. 2017;39:65–69. doi: 10.1027/0227-5910/a000464. [DOI] [PubMed] [Google Scholar]
- Hallensleben N., Glaesmer H., Forkmann T., Rath D., Strauss M., Kersting A., Spangenberg L. Predicting suicidal ideation by interpersonal variables, hopelessness and depression in real-time. An ecological momentary assessment study in psychiatric inpatients with depression. Eur. Psychiatry. 2019;56:43–50. doi: 10.1016/j.eurpsy.2018.11.003. [DOI] [PubMed] [Google Scholar]
- Hamaker E.L., Grasman R.P. To center or not to center? Investigating inertia with a multilevel autoregressive model. Front. Psychol. 2015;5:1492. doi: 10.3389/fpsyg.2014.01492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hames J.L., Chiurliza B., Podlogar M.C., Smith A.R., Selby E.A., Anestis M.D., Joiner T.E. Perceived burdensomeness and thwarted belongingness predict excessive reassurance seeking among clinical outpatients. J. Clin. Psychol. 2015;71(6):597–605. doi: 10.1002/jclp.22158. [DOI] [PubMed] [Google Scholar]
- Hawton K., Van Heeringen C. John Wiley & Sons; Chichester: 2000. The International Handbook on Suicide and Attempted Suicide. (755 p) [Google Scholar]
- Hoffman L., Stawski R.S. Persons as contexts: Evaluating between-person and within-person effects in longitudinal analysis. Res. Hum. Dev. 2009;6(2-3):97–120. [Google Scholar]
- Joiner T. Harvard University Press; 2007. Why People Die by Suicide. [Google Scholar]
- Jones P.J., Mair P., McNally R.J. Visualizing psychological networks: a tutorial in R. Front. Psychol. 2018;9 doi: 10.3389/fpsyg.2018.01742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleiman E.M., Nock M.K. Real-time assessment of suicidal thoughts and behaviors. Curr. Opin. Psychol. 2018;22:33–37. doi: 10.1016/j.copsyc.2017.07.026. [DOI] [PubMed] [Google Scholar]
- Kleiman E.M., Turner B.J., Fedor S., Beale E.E., Huffman J.C., Nock M.K. Examination of real-time fluctuations in suicidal ideation and its risk factors: results from two ecological momentary assessment studies. J. Abnorm. Psychol. 2017;126(6):726. doi: 10.1037/abn0000273. [DOI] [PubMed] [Google Scholar]
- Kleiman E.M., Coppersmith D.D., Millner A.J., Franz P.J., Fox K.R., Nock M.K. Are suicidal thoughts reinforcing? A preliminary real-time monitoring study on the potential affect regulation function of suicidal thinking. J. Affect. Disord. 2018;232:122–126. doi: 10.1016/j.jad.2018.02.033. [DOI] [PubMed] [Google Scholar]
- Kroeze R., van der Veen D.C., Servaas M.N., Bastiaansen J.A., Oude Voshaar R., Borsboom D., Riese H. Personalized feedback on symptom dynamics of psychopathology: a proof-of-principle study. J. Person-Oriented Res. 2017;3(1):1–11. doi: 10.17505/jpor.2017.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehrl S. Spitta-Verlag; Balingen: 2005. Manual zum MWT-B. Manual of the MWT-B. [Google Scholar]
- Ma J., Batterham P.J., Calear A.L., Han J. A systematic review of the predictions of the Interpersonal–Psychological Theory of Suicidal Behavior. Clin. Psychol. Rev. 2016;46:34–45. doi: 10.1016/j.cpr.2016.04.008. [DOI] [PubMed] [Google Scholar]
- Nuij C., van Ballegooijen W., Ruwaard J., de Beurs D., Mokkenstorm J., van Duijn E.…Riper H. 2018. Smartphone-based safety planning and self-monitoring for suicidal patients: rationale and study protocol of the CASPAR (Continuous Assessment for Suicide Prevention And Research) study. Internet Interventions. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor R.C., Nock M.K. The psychology of suicidal behaviour. Lancet Psychiatry. 2014;1(1):73–85. doi: 10.1016/S2215-0366(14)70222-6. [DOI] [PubMed] [Google Scholar]
- Oquendo M.A., Galfalvy H., Russo S., Ellis S.P., Grunebaum M.F., Burke A., Mann J.J. Prospective study of clinical predictors of suicidal acts after a major depressive episode in patients with major depressive disorder or bipolar disorder. Am. J. Psychiatr. 2004;161(8):1433–1441. doi: 10.1176/appi.ajp.161.8.1433. [DOI] [PubMed] [Google Scholar]
- Osman A., Bagge C.L., Gutierrez P.M., Konick L.C., Kopper B.A., Barrios F.X. The Suicidal Behaviors Questionnaire-Revised (SBQ-R): validation with clinical and nonclinical samples. Assessment. 2001;8(4):443–454. doi: 10.1177/107319110100800409. [DOI] [PubMed] [Google Scholar]
- Rogers M.L., Joiner T.E. Exploring the temporal dynamics of the interpersonal theory of suicide constructs: a dynamic systems modeling approach. J. Consult. Clin. Psychol. 2019;87(1):56. doi: 10.1037/ccp0000373. [DOI] [PubMed] [Google Scholar]
- Shumway R.H., Stoffer D.S. Time Series Analysis and Its Applications. Springer; 2000. Time series regression and ARIMA models; pp. 89–212. [Google Scholar]
- Snippe E., Viechtbauer W., Geschwind N., Klippel A., De Jonge P., Wichers M. The impact of treatments for depression on the dynamic network structure of mental states: two randomized controlled trials. Sci. Rep. 2017;7 doi: 10.1038/srep46523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Borkulo C., Boschloo L., Borsboom D., Penninx B.W., Waldorp L.J., Schoevers R.A. Association of symptom network structure with the course of depression. JAMA Psychiat. 2015;72(12):1219–1226. doi: 10.1001/jamapsychiatry.2015.2079. [DOI] [PubMed] [Google Scholar]
- Van Orden K.A., Witte T.K., Cukrowicz K.C., Braithwaite S.R., Selby E.A., Joiner T.E., Jr. The interpersonal theory of suicide. Psychol. Rev. 2010;117(2):575. doi: 10.1037/a0018697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verhagen S.J., Hasmi L., Drukker M., van Os J., Delespaul P.A. Use of the experience sampling method in the context of clinical trials. Evid. Based Ment. Health. 2016;19(3):86–89. doi: 10.1136/ebmental-2016-102418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Jiang N., Cheung E.F.C., Sun H., Chan R.C.K. Role of depression severity and impulsivity in the relationship between hopelessness and suicidal ideation in patients with major depressive disorder. J. Affect. Disord. 2015;183:83–89. doi: 10.1016/j.jad.2015.05.001. [DOI] [PubMed] [Google Scholar]
- Wigman J., Van Os J., Borsboom D., Wardenaar K., Epskamp S., Klippel A.…Wichers M. Exploring the underlying structure of mental disorders: cross-diagnostic differences and similarities from a network perspective using both a top-down and a bottom-up approach. Psychological medicine. 2015;45(11):2375–2387. doi: 10.1017/S0033291715000331. [DOI] [PubMed] [Google Scholar]
- Wittchen H.-U., Zaudig M., Fydrich T. 1997. Skid. Strukturiertes klinisches Interview für DSM-IV. Achse I und II. Handanweisung. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary tables