Abstract
Background
There is evidence that cognitive remediation (CR) is moderately effective in improving cognitive and functional difficulties in people with schizophrenia. However, there is still a limited understanding of what influence different treatment responses.
Aim
To identify moderators influencing CR response in people with schizophrenia.
Methods
This systematic review follows PRISMA guidelines. Searches were conducted up to January 2019 on PubMed and PsychInfo to identify randomized controlled trials of CR reporting analyses of moderators of treatment response. All papers were assessed for methodological quality and information on sample size, intervention and control condition, moderators, outcomes, effect of moderator on outcomes and demographic characteristics from each study was extracted and critically summarised.
Results
Thirty-six studies were included, considering 2737 participants. Study participants consisted on average of people in their late-thirties, mostly men, with over 10 years of illness. The review identified moderators that could be grouped into five categories: demographics, biological, cognitive and functional, psychological, and illness-related characteristics. The assessment of methodological quality showed that many studies had a high risk of bias.
Conclusions
There was no high-quality replicated evidence which identifies reliable moderators of CR response. Many moderators were not replicated or presented in single, underpowered studies. Studies also investigated moderators independently despite their potential to overlap (e.g. age and education). Future research should concentrate on evaluating, with sound studies, the role moderators may play in affecting CR treatment response. This information can inform who will benefit most from the therapy and help to improve the benefits of CR.
Keywords: Cognitive remediation, Cognition, Moderator, Schizophrenia, Psychosis
1. Introduction
Cognitive impairment is a core feature of schizophrenia with a negative prognostic value for global functioning, social skills, poorer self-care, and independent living skills (Allott et al., 2011; Bowie et al., 2008; Bowie and Harvey, 2006; Green et al., 2000). In addition, cognitive deficits reduce the potential benefit of rehabilitation programs, even when high-quality rehabilitation is provided, contributing to higher rates of institutionalization (Bell and Bryson, 2001; McGurk and Meltzer, 2000; Wykes, 1994). It is for these reasons that cognitive training techniques were developed, in the hope that improving cognition would lead to lasting functional outcome improvements.
Cognitive remediation (CR) is “an intervention targeting cognitive deficit using scientific principles of learning with the ultimate goal of improving functional outcomes” (Cognitive Remediation Experts Workshop, 2012, p. 1). In the meta-analysis conducted by Wykes et al. (2011), CR was found to have a moderate but durable effect on global cognition and functional outcomes. In addition, functioning was improved most when CR was combined with other forms of rehabilitation.
Although CR is an effective approach, there is evidence that as many as one in four participants receiving this intervention will not improve (Murthy et al., 2012; Wykes et al., 2011). While many studies have focussed on the evaluation of CR efficacy, only a limited number have considered how individual characteristics, clinical presentation, and other factors may affect treatment response (Fiszdon et al., 2005; Medalia and Richardson, 2005; Twamley et al., 2011; Vita et al., 2013). Wykes and Spaulding (2011) suggested that these types of studies are important to improve the personalisation agenda of CR even if the results are negative. Systematic evidence on mediators and moderators may allow tailoring therapy according to patients' characteristics in order to maximise its potential benefits.
To date, there is no systematic review of the putative factors which may affect CR response, although some have been suggested in the literature. For instance, a number of studies have suggested that the individuals most likely to benefit from CR are younger (McGurk and Mueser, 2008; Wykes et al., 2009), with fewer symptoms (Wykes et al., 2011) and, more severe cognitive difficulties (Pillet et al., 2015; Wykes et al., 2011). However, these characteristics have been identified in single studies using underpowered samples. There is limited converging evidence, with some studies suggesting that higher or lower levels of a characteristic (e.g. functioning) may be important in influencing therapy outcomes (Farreny et al., 2016; Twamley et al., 2011). Further, studies have considered therapy moderators and mediators in relation to different therapy outcomes (e.g. different cognitive domains, functioning, motivation) contributing to the limited consensus in identifying reliable factors that can be used to tailor CR.
Despite the limited evidence, a number of authors (Demily and Franck, 2008; Levaux et al., 2009; Medalia et al., 2018; Silverstein and Wilkniss, 2004) have highlighted the importance of developing a more individualized treatment to improve therapy response. Franck et al. (2013) attempted to personalise CR by adapting training on modules participants received in relation to their initial cognitive assessment (e.g. receiving more training for the most compromised domain). These authors compared the personalised approach to general CR training but found no differences between the two methods suggesting that this personalisation method may not bring about benefits.
While personalisation is increasingly found important, there is no systematic evidence in the literature summarizing relevant findings that may be able to guide future studies. The current review aims to identify potential individual factors at baseline, moderators, that may predict treatment outcomes and that may be used to tailor CR and improve its benefits.
2. Methods
2.1. Research evidence identification
For this review, we followed the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) guidelines (Moher et al., 2009). The review protocol was registered on a public database (e.g. https://www.crd.york.ac.uk/prospero/) on the 27th of February 2018. Searches were conducted up to the 16th of January 2019 on PsycInfo and PubMed databases. We also searched potentially relevant websites including ResearchGate and Mendeley.
In order to identify any additional relevant papers, the reference lists of included studies, relevant and recent reviews (e.g. Wykes and Huddy, 2009; Wykes et al., 2011; Best and Bowie, 2017; Cella et al., 2017), and relevant articles in this field were also inspected.
2.2. Literature search
A broad search string strategy was adopted including the following terms: “exp. schizophrenia” OR “exp. psychosis” OR “exp. schizoaffective disorder” AND “cognitive enhancement” OR “cognitive rehabilitation” OR “cognitive remediation” OR “cognitive training”.
2.3. Inclusion criteria
Eligible studies:
-
•
Randomized controlled trials.
-
•
Assessed the relationship of one or more baseline moderators to CR treatment response. Moderators, according to Baron and Kenny (1986), are all those factors that identify for whom and under which circumstances treatments have different effects (e.g. age, cognitive profile).
-
•
Included participants over the age of 18 with a diagnosis of schizophrenia or schizoaffective disorder according to the Diagnostic and Statistical Manual of Mental Disorder (American Psychiatric Association, 2013), Research Diagnostic Criteria (Spitzer et al., 1978) or International Classification of Diseases (World Health Organization, 1992).
-
•
The sample considered had at least 75% of participants with a diagnosis of schizophrenia or schizoaffective disorders.
-
•
The study was in English language.
-
•
The CR interventions adopted use principles such as massed practice, errorless learning, and scaffolding to improve cognition and/or social cognition and/or functioning. All modes of administration (computer, pen and paper, individual, group, presence or absence of therapist) were considered.
2.4. Exclusion criteria
We excluded all study designs that were not randomized controlled trials (e.g. case studies and opinion papers) or were a combination of randomized and non-randomized controlled trials [e.g. the study conducted by Greenwood et al., 2011]. We also excluded studies where the focus of the intervention was psychoeducation about cognitive difficulties.
2.5. Study selection and data extraction
Two authors (BS and DT) independently conducted a screening of all titles and abstracts to identify eligible studies. Disagreements during the selection process were resolved by consultation with a third author (MC).
For all the included studies the following information was extracted:
-
•
sample size for the experimental and control condition;
-
•
demographic characteristics including age, gender, years of education, and duration of illness;
-
•
details of the intervention and control condition;
-
•
type of moderator considered;
-
•
study primary and secondary outcomes;
-
•
reported effect of the moderator on the outcome.
2.6. Quality assessment
All included studies were assessed for methodological rigor using the Clinical Trials Assessment Measure (CTAM) (Wykes et al., 2008). This is a 15-item measure of trial methodology specifically developed for psychological treatment studies. The maximum score is 100 and studies with a CTAM score < 65 are considered at higher risk of bias (Wykes et al., 2008). All studies were independently rated by two authors (BS and KN) and discrepancies resolved by consultation with a third author (MC). CTAM scores were checked with the study authors and adjusted according to their feedback if provided.
3. Results
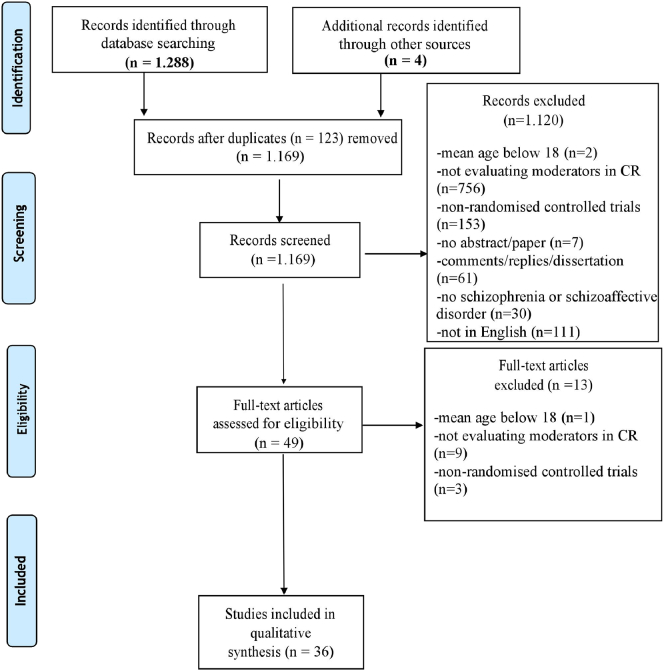
As shown in the PRISMA diagram (Fig. 1), the literature search identified thirty-six eligible studies, including 2737 participants. A summary of the studies characteristics is reported in Table 1.
Fig. 1.
Systematic search PRISMA diagram.
Table 1.
Characteristics of the included studies.
| Study | Study design | Original paper | Title | Moderator investigated | Participants |
Intervention |
Primary outcome measures | Secondary outcome measures | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean age (SD) | Male (%) | Sample size N (CR) | Mean years of education (SD) | Total included in analysis (dropouts; interventions) | Years of illness (mean) | Setting (inpatients, outpatients) | Treatment intervention | Control intervention | |||||||
| Corbera et al., 2017, USA | Secondary analysis of RCTs (Kurtz et al., 2007, 2015) | Kurtz et al., 2007 | Computer-assisted cognitive remediation in schizophrenia: what is the active ingredient? | Age, duration of illness | 32.96 (11.57) | 70.5% | 112 | 12.82 (2.40) | 112 | 9.34 | Outpatients | Cognitive remediation | Computer skills training | Working memory, functioning and symptoms | NR |
| Kurtz et al., 2015 | Social skills training and computer-assisted cognitive remediation in schizophrenia. | ||||||||||||||
| McGurk and Mueser, 2008, USA | Secondary analysis of two RCTs | McGurk et al., 2005 | Cognitive training and supported employment for persons with severe mental illness: one-year results from a randomized controlled trial | Age | NR | 55.26% | 76 (37) | NR | 76 | NR | NR | Cognitive training + vocational rehabilitations | Vocational rehabilitations | Cognitive functioning; symptoms | NR |
| (McGurk et al., 2005 and McGurk et al., 2015) | |||||||||||||||
| McGurk et al., 2015 | Cognitive enhancement treatment for people with mental illness who do not respond to supported employment: a randomized controlled trial | ||||||||||||||
| Wykes et al., 2009, UK | Secondary analysis of RCT (Wykes, Reeder, Landau et al., 2007) | Wykes, Reeder, Landau et al., 2007 | Cognitive remediation therapy in schizophrenia: a randomized controlled trial | Age | 36 (NR) | 73% | 85 (43) | Young = 11.85 | Memory: 75 PT; 68FU | NR | NR | Cognitive remediation (paper and pencil) + treatment as usual | Treatment as usual | Memory, cognitive flexibility and planning | Social functioning, symptoms, self-esteem |
| Older = 10.8 | Flexibility: 72 PT; 64 FU | ||||||||||||||
| Planning: 74 PT; 67 FU | |||||||||||||||
| Self-esteem: 75 PT; 67 FU | |||||||||||||||
| Symptoms: 79 PT; 69 FU | |||||||||||||||
| Social functioning: 77 PT; 74 FU | |||||||||||||||
| Franck et al., 2013, UK | RCT | / | / | Age; intellectual | 33.54 (6.9) | 73% | 138 (65) | NR | 92 | NR | Outpatients | Cognitive remediation therapy | RECOS program | BADS (Behavioural Assessment of Dysexecutive Syndrome) | Cognition and clinical measures |
| Bark et al., 2003, USA | Secondary analysis of RCT (Medalia et al., 2000) | Medalia et al., 2000 | Remediation of memory disorders in schizophrenia | Symptoms | 36.77 | 59.26% | 54 (36) | 10.99 | NR | NR | Inpatients | Cognitive remediation exercises + standard hospital care | Treatment as usual | Cognitive functioning; symptoms | NR |
| Wykes et al., 1999, UK | RCT | / | / | Medication; demographics (age, gender); and symptoms | 38.55 | 75.75% | 33 (17) | 12.35 | 33 | NR | Outpatients | Cognitive Remediation Therapy + standard rehabilitation treatment | Intensive occupational therapy | Working memory; cognitive flexibility and planning | Social functioning, symptoms, and self-esteem. |
| Wykes et al., 2007, UK | RCT | / | / | Medication | 36 (NR) | 73% | 85 (43) | NR | NR | NR | NR | Cognitive remediation therapy | Treatment as usual | Working memory; cognitive flexibility and planning | Social functioning, symptoms, self-esteem |
| Bosia et al., 2007, Italy | RCT | / | / | COMT allele | NR | 68% | 50 (27) | NR | 49 | NR | Outpatients | Function-specific computer-aided exercises + standard rehabilitation treatment | Standard rehabilitation treatment | Symptoms; functioning; cognitive flexibility; sustained attention | NR |
| Farreny et al., 2016, Spain | Secondary analysis of RCT, Farreny et al., 2012 | Farreny et al., 2012 | REPYFLEC cognitive remediation group training in schizophrenia Looking for an integrative approach | Demographics (sex, age, education); illness duration; medication; cognition; symptoms and functioning | 39.5 (8.5) | 65.5% | 62 (29) | NR | NR | 17.6 | Outpatients | REPYFLEC | Stimulating activities focused on leisure and socialisation | Neurocognition functioning symptoms | NR |
| Farreny et al., 2013, Spain | Secondary analysis of RCT, Farreny et al., 2012 | Farreny et al., 2012 | REPYFLEC cognitive remediation group training in schizophrenia looking for an integrative approach | Baseline negative symptoms and executive function | 40.6 (7.6) | 68% | 62 (29) | NR | NR | NR | Outpatients | REPYFLEC | Leisure activities | Neurocognition functioning symptoms | NR |
| Panizzutti et al., 2013, USA | Secondary analysis of 2 RCTs (Fisher et al., 2009, 2015) | Fisher et al., 2009 | Using neuroplasticity-based auditory training to improve verbal memory in schizophrenia | COMT allele | 33.6 (13.1) | 70.8% | 48 (48) | NR | NR | 12.9 | Outpatients | Posit science auditory training | Computer game | Global cognition | NR |
| Fisher et al., 2015 | Neuroplasticity-based auditory training via laptop computer improves cognition in young individuals with recent onset schizophrenia | ||||||||||||||
| Penades et al., 2016, Spain | Secondary analysis of RCT (Penadés et al., 2013) | Penadés et al., 2013 | Brain effects of cognitive remediation therapy in schizophrenia: a structural and functional neuroimaging study. | Demographic variables (age; education; duration of illness; number of hospitalisations) medication; baseline brain structure; baseline symptoms; baseline cognitive performance | 36.22 | 74% | 50 (17) | 13.34 | NR | 12.84 | Outpatients | Cognitive remediation therapy | Social skills training and healthy control group | Cognition | NR |
| Twamley et al., 2011, USA | Secondary analysis of RCT (Twamley et al., 2012) | Twamley et al., 2012 | Compensatory Cognitive Training for psychosis: effects in a randomized controlled trial | Demographic variables (age; gender; education; diagnosis; duration of illness); medication; symptoms; cognition; functioning; self-reported cognitive and functioning problems; intelligence | 47.3 (9.8) | 65% | 89 | 13.3 (1.8) | 89 | 12.7 | Outpatients | Compensatory Cognitive Training (CCT) + standard pharmacotherapy | Standard pharmacotherapy | Cognition; functioning, symptoms | NR |
| Bell et al., 2008, USA | RCT | / | / | Baseline community function | 40 | 54% | 77 (38) | NR | 72 | NR | Outpatients | Neurocognitive enhancement therapy + vocational program | Vocational program | Competitive employment rates and hours of competitive employment | NR |
| Bell et al., 2014, USA | Secondary analysis from RCT | Bell et al. 2008 | Neurocognitive enhancement therapy with vocational services: work outcomes at two-year follow-up. | Baseline community function | CR high community functioning = 40.35 (10.48) | CR high community functioning = 48% | 175 (99) | CR high community functioning = 12.26 (1.57) | 174 | NR | Outpatients | Neurocognitive enhancement therapy + vocational program | Vocational program | Competitive employment rates and hours of competitive employment | NR |
| CR low community functioning = 40.07 (8.96) | CR low community functioning = 55% | CR low community functioning = 12.20 (2.04) | |||||||||||||
| SE high community functioning = 42.51 (10.69) | SE high community functioning = 53% | SE high community functioning = 13.57 (2.68) | |||||||||||||
| SE low community functioning = 41.28 (10.28) | SE low community functioning = 72% | SE low community functioning = 12.57 (2.44) | |||||||||||||
| Burton and Twamley, 2015, USA | Secondary analysis of RCT (Twamley et al., 2012) | Twamley et al., 2012 | Compensatory Cognitive Training for psychosis: effects in a randomized controlled trial | Neurocognitive insight | 46.3 (9.7) | 65.2% | 69 | 12.9 (1.7) | 43 | 23.3 | Outpatients | Compensatory Cognitive Training + standard pharmacotherapy | Standard pharmacotherapy | Cognition and functioning | NR |
| Burton et al., 2015, USA | Secondary analysis of RCT (Twamley et al., 2012) | Twamley et al., 2012 | Compensatory Cognitive Training for psychosis: effects in a randomized controlled trial | COMT allele | 48 (8.6) | 65.9% | 41 (20) | 13.1 (1.7) | 41 | 23.8 | Outpatients | Compensatory Cognitive Training + standard pharmacotherapy | Standard pharmacotherapy | Cognition, functioning, symptoms | NR |
| Evensen et al., 2017, Norway | RCT | / | / | Global functioning, self-esteem | CBT = 33.2 (8.0) | CBT = 61.8% | 148 (64) | NR | 148 | CBT = 8.1 | NR | Vocational rehabilitation augmented + CR | Vocational rehabilitation augmented + CBT | Self-esteem; global functioning; depression; employment status | NR |
| CR = 32.4 (7.9) | CR = 79.4% | CR = 5.9 | |||||||||||||
| Fiszdon et al., 2006, USA | RCT | / | / | Intellectual (pre-morbid and morbid) | 42.82 (8.66) | 80% | 152 (72) | 13.38 (3.03) | 151 | NR | Outpatients | Neurocognitive enhancement therapy with work therapy | Work therapy | Cognitive functioning | NR |
| Davidson et al., 2016, USA | Secondary analysis of RCT (Fiszdon et al., 2016) | Fiszdon et al., 2016 | Cognitive remediation for individuals with psychosis: efficacy and mechanisms of treatment effects | Learning potential | CR = 47.3 (9.1) | CR = 78.4% | 75 (50) | CR = 12.5 (1.8) | 75 | NR | Outpatients | Cognitive remediation | Treatment as usual | Cognition | NR |
| TAU = 48.9 (9.9) | TAU = 62.5% | TAU = 12.1 (2.3) | |||||||||||||
| Keshavan et al., 2011, USA | Secondary analysis of RCT (Eack et al., 2009) | Eack et al., 2009 | Cognitive enhancement therapy for early-course schizophrenia: effects of a two-years randomized controlled trial. | Cortical reserve | 25.72 (5.94) | 64% | 58 | NR | 50 | 3.26 | NR | Cognitive enhancement therapy | Enriched supportive therapy | Cognition and social cognition | NR |
| Kurtz et al., 2009, USA | Secondary analysis of RCT (Kurts et al., 2007) | Kurts et al., 2007 | Computer-assisted cognitive remediation in schizophrenia: what is the active ingredient? | Cognition, symptoms | 32.4 (11.2) | 69% | 36 | 13.4 (1.9) | 36 | 8.7 | Outpatients | Cognitive remediation | Computer-skills training | Cognition, functioning, symptoms | NR |
| Kurtz et al., 2008, USA | RCT | / | / | Cognition, symptoms, functioning | 34.6 (10.0) | 72% | 46 | 13.4 (1.9) | 23 | 9.6 | Outpatients | Cognitive remediation | Computer-skills training | Functioning | NR |
| Rodewald et al., 2014, Switzerland | Secondary analysis of RCT (Rodewald et al. 2011) | Rodewald et al. 2011 | Planning and problem-solving training for patients with schizophrenia: a randomized controlled trial. | Cognition, symptoms, motivation | Problem-solving training = 28.0 (7.0) | Problem-solving training = 84% | 77 | Problem-solving training = 14.7 (2.9) | 75 | Problem-solving training = 5.0 | Inpatients | Training of planning and problem-solving ability (PLAN) | Basic cognitive training | Cognition | NR |
| Basic cognition training = 29.5 (7.4) | Basic cognition training = 77% | Basic cognition training = 15.6 (3.7) | Basic cognition training = 3.8 | ||||||||||||
| Subramaniam et al., 2017, USA | RCT | / | / | Brain Structure (White matter integrity) | HC = 41.41 (11.74) | HC = 60.71% | HC (N = 28) | HC = 15.15 (2.67) | HC (N = 28) | 24.52 | Outpatients | Targeted Cognitive training + Social Cognitive Training | Targeted Cognitive training | Cognition and symptoms, | NR |
| SZ = 45.59 (10.25) | SZ = 68.75% | SZ (N = 48) | SZ = 45.59 (10.25) | SZ (N = 30) | |||||||||||
| Fisher et al., 2015, USA | RCT | / | / | Motivation | Computerized auditory training = 21.70 (3.26) | Computerized auditory training = 72.09% | 121 (63) | Computerized auditory training = 12.88 (1.60) | 86 | NR | Outpatients | Computerized auditory training | Computer game | Cognition, symptoms, functioning and reward anticipation | NR |
| Computer game = 20.74 (3.37) | Computer game = 76.74% | Computer game = 12.86 (2.10) | |||||||||||||
| Vinogradov et al., 2009, USA | Secondary analysis of RCT (Twamley et al., 2012) | Twamley et al., 2012 | Compensatory Cognitive Training for Psychosis: Effects in a Randomized Controlled Trial | Medication (Serum anticholinergic activity) | 43.86 (10.29) | 71% | 49 (25) | 13.08 (2.20) | 49 | NR | Outpatients | Neuroplasticity-Based Computerized Auditory Training | Computer game | Cognition and symptoms | NR |
| Dickinson et al., 2010, USA | Secondary analysis of RCT (Fiszdon et al., 2016) | Fiszdon et al., 2016 | Cognitive remediation for individuals with psychosis: efficacy and mechanisms of treatment effects | Age | 38.10% | 63 (35) | CR = 12.2 (1.8) | 63 | NR | NR | Computer-assisted cognitive remediation | Computer game | Cognition and functioning | Self-described cognitive performance and symptoms | |
| CR = 46.9 (6.6) | Control = 12.8 (1.3) | ||||||||||||||
| Control = 48.5 (8.8) | |||||||||||||||
| Fiszdon et al., 2004, USA | RCT | / | / | Symptoms | NET + WT = 41.9 (9.9) | NET + WT = 76% | 94 (45) | NET + WT = 13.3 (2.1) | 94 | NR | Outpatients | Cognitive Remediation Therapy + work therapy | Work Therapy | Memory | NR |
| WT = 43.2 (8.0) | WT = 80% | WT = 13.5 (2.2) | |||||||||||||
| Control = 33.21 (6.89) | Control = 9.66 (2.28) | Control = 10.68 | |||||||||||||
| Lewandowski et al., 2011, USA | Secondary analysis from 2 RCT | Hogarty et al., 2006 | Durability and mechanism of effects of cognitive enhancement therapy. | Diagnosis | 25.9 (6.3) | 69% | 58 (31) | NR | 58 | 3.2 | Outpatients | Cognitive enhancement therapy | Enriched supportive therapy | Cognition, social cognition, symptoms and social adjustment | NR |
| Eack et al., 2009 | Cognitive enhancement therapy for early- course schizophrenia: effects of a two-year randomized controlled trial. | ||||||||||||||
| McGurk et al., 2009, USA | RCT | / | / | Cognition, demographic variables (substance abuse and medication comorbidity) | VR + CR = 45.5 (9.58) | VR + CR = 61% | 34 | VR + CR = 12.22 (2.73) | 34 | NR | Outpatients | Vocational Services Program + Cognitive Remediation Program | Vocational Services Program | Cognition, symptoms, comorbidity and employment | NR |
| VR = 42.44 (8.52) | VR = 56% | VR = 11.75 (1.81) | |||||||||||||
| Sanchez et al., 2014, Spain | RCT | / | / | Medication, symptoms | REHACOP = 33.60 (9.4) | REHACOP = 75% | 92 (38) | REHACOP = 9.23 (2.7) | 84 | NR | Inpatients | Neuropsychological rehabilitation (REHACOP) + TAU | Group activities including drawing, reading the daily news, and constructing objects using different materials | Cognition, symptoms and functioning | NR |
| Control = 36.92 (10.5) | Control = 77.1% | Control = 10.24 (2.8) | |||||||||||||
| Bellucci et al., 2003, Australia | RCT | / | / | Self-esteem | 42.0 | 47.1% | 32 | 12.6 | NR | NR | NR | Computer-assisted cognitive rehabilitation (CACR) | Wait-list | Cognition, symptoms and self-esteem | NR |
| Thomas et al., 2018, USA | RCT | / | / | Age, symptoms, medication, illness duration | 35.14 (12.57) | 47.5% | 46 (24) | 11.83 (2.08) | 46 | 15.68 | Outpatients | Computerized targeted cognitive training + TAU | TAU | Cognition, auditory perception, and symptoms | NR |
| Gomar et al., 2015, Spain | RCT | / | / | Age, medication | TAU = 45.40 (9.77) Control active = 46.13 (10.11) CRT = 46.68 (9.97) |
68.5% | 130 (43) | TAU = 10.33 (2.65) Control active = 9.53 (3.08) CRT = 9.30 (2.86) |
130 | TAU = 23.38 (8.63) Control active = 22.58 (9.10) CRT = 24.30 (8.52) |
Inpatients | Computerized CRT | TAU Computerized typing program and computerized games |
Cognition (executive function and memory) | Other cognitive tests and functioning |
| Ramsay et al., 2018, USA | Secondary analysis of RCT (Fisher et al. 2015) | Fisher et al. 2015 | Neuroplasticity-based auditory training via laptop computer improves cognition in young individuals with recent onset schizophrenia | Brain structure, baseline cognition and symptoms | 22.27 (4.13) | 65.9% | 44 (22) | 12.64 (2.54) | 44 | 1.70 | Outpatients | Targeted cognitive training | Computer games | Symptoms and cognition | NR |
3.1. Sample characteristics
Participants had a mean age of 37.7 years (SD 7.3; range 21.2–48.1), and the majority were men (mean = 66.6%; SD 9.4; range 38.1% - 80.5%), with 13.2 years of education (SD 3.8; range 9.7–30.4). Participants had an average illness duration of 12.6 years (SD 7.8; range 1.7–24.5).
3.2. Study characteristics
The mean sample size was 76 [(SD 36.9); range 32–175; CR group mean = 41 (SD 18.9); Control group mean = 41.4 (SD 22)]. Most studies were carried out in the United States (N = 23); five studies took place in Spain, four in the United Kingdom and the remaining four in Italy, Australia, Norway, and Switzerland.
3.3. Therapy characteristics
Nineteen studies provided CR alone, five combined CR with another active condition (e.g. vocational rehabilitation, social cognitive training) and twelve combined CR with treatment as usual.
3.4. Control condition
Twenty-one studies had an active control condition (e.g. computer game, leisure activities), twelve had treatment as usual or waiting list, two had two control conditions (one active and one passive) and another one had an active control condition and a control group including healthy people.
3.5. Trial quality
The Clinical Trial Assessment Measure scores for each study are summarised in Table 2. The mean score was 66.1 (SD 11.7; range 44–90) out of a maximum of 100. Only 21 (53%) studies scored above the cut-off of 65, indicating a low risk of bias (Wykes et al., 2008). Problems were sample size (33% were too small) with only three studies having adequately calculated power (7.3%), group allocation was not masked (35%), lack of independent randomization (60%), and lack of treatment fidelity assessment (83%).
Table 2.
Clinical Trial Assessment Measure scores.
| Study | Study design | Original paper | Clinical Trial Assessment Measure scores |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Sample (maximum 10) | Allocation procedure (maximum 16) | Assessment (maximum 32) | Comparison (maximum 16) | Analysis (maximum 15) | Treatment description (maximum 11) | Total score (maximum 100) | |||
| Corbera et al., 2017, USA | Secondary analysis of RCTs (Kurtz et al., 2007, 2015) | Kurtz et al., 2007 | 2 | 10 | 29 | 10 | 9 | 6 | 66 |
| Kurtz et al., 2015 | 7 | 10 | 29 | 10 | 11 | 3 | 70 | ||
| McGurk and Mueser, 2008, USA | Secondary analysis of two RCTs (McGurk et al., 2005 and McGurk et al., 2015) | McGurk et al., 2005 | 2 | 16 | 26 | 6 | 15 | 6 | 71 |
| McGurk et al., 2015 | 7 | 16 | 29 | 16 | 11 | 11 | 90 | ||
| Wykes et al., 2009 UK | Secondary analysis of RCT (Wykes, Reeder, Landau et al., 2007) | Wykes, Reeder, Landau et al., 2007 | 10 | 16 | 29 | 6 | 15 | 11 | 87 |
| Franck et al., 2013, UK | RCT | / | 7 | 10 | 26 | 10 | 5 | 3 | 61 |
| Bark et al., 2003, USA | Secondary analysis of RCT (Medalia et al., 2000) | Medalia et al., 2000 | 2 | 10 | 6 | 16 | 9 | 6 | 49 |
| Wykes et al., 1999, UK | RCT | / | 5 | 16 | 16 | 6 | 15 | 11 | 69 |
| Wykes et al., 2007, UK | RCT | / | 10 | 16 | 29 | 6 | 15 | 11 | 87 |
| Bosia et al., 2007, Italy | RCT | / | 2 | 10 | 26 | 16 | 5 | 3 | 62 |
| Farreny et al., 2016, Spain | Secondary analysis of RCT, Farreny et al., 2012 | Farreny et al., 2012 | 2 | 16 | 26 | 10 | 11 | 6 | 71 |
| Farreny et al., 2013, Spain | Secondary analysis of RCT, Farreny et al., 2012 | Farreny et al., 2012 | 2 | 16 | 26 | 10 | 11 | 6 | 71 |
| Panizzutti et al., 2013, USA | Secondary analysis of 2 RCTs (Fisher et al., 2009, 2015) | Fisher et al., 2009 | 7 | 13 | 26 | 10 | 9 | 6 | 71 |
| Fisher er al., 2015 | 7 | 10 | 26 | 10 | 15 | 11 | 79 | ||
| Penades et al., 2016, Spain | Secondary analysis of RCT (Penadés et al., 2013) | Penadés et al., 2013 | 2 | 16 | 6 | 10 | 11 | 6 | 51 |
| Twamley et al., 2011, USA | Secondary analysis of RCT (Twamley et al., 2012) | Twamley et al., 2012 | 7 | 13 | 26 | 6 | 15 | 6 | 73 |
| Bell et al., 2008, USA | RCT | / | 7 | 16 | 6 | 10 | 15 | 6 | 60 |
| Bell et al., 2014, USA | Secondary analysis from RCT | Bell et al., 2008 | 7 | 16 | 6 | 10 | 15 | 6 | 60 |
| Burton and Twamley, 2015, USA | Secondary analysis of RCT (Twamley et al., 2012) | Twamley et al., 2012 | 7 | 13 | 26 | 6 | 15 | 6 | 73 |
| Burton et al., 2015, USA | Secondary analysis of RCT (Twamley et al., 2012) | Twamley et al., 2012 | 7 | 13 | 26 | 6 | 15 | 6 | 73 |
| Davidson et al., 2016, USA | Secondary analysis of RCT (Fiszdon et al., 2016) | Fiszdon et al., 2016 | 2 | 16 | 6 | 6 | 11 | 6 | 47 |
| Evensen et al., 2017, Norway | RCT | / | 7 | 10 | 16 | 10 | 5 | 0 | 48 |
| Fiszdon et al., 2006, USA | RCT | / | 7 | 10 | 3 | 16 | 5 | 3 | 44 |
| Keshavan et al., 2011, USA | Secondary analysis of RCT (Eack et al., 2009) | Eack et al., 2009 | 7 | 16 | 6 | 10 | 11 | 6 | 56 |
| Kurtz et al., 2009, USA | Secondary analysis of RCT (Kurts et al., 2007) | Kurts et al., 2007 | 2 | 10 | 29 | 10 | 9 | 6 | 66 |
| Kurtz et al., 2008, USA | RCT | / | 7 | 10 | 26 | 10 | 5 | 6 | 64 |
| Rodewald et al., 2014, Switzerland | Secondary analysis of RCT (Rodewald et al. 2011) | Rodewald et al. 2011 | 7 | 10 | 26 | 10 | 5 | 6 | 64 |
| Subramaniam et al., 2017, USA | RCT | / | 7 | 10 | 16 | 10 | 5 | 3 | 51 |
| Fisher et al., 2015, USA | RCT | / | 7 | 10 | 26 | 10 | 15 | 6 | 74 |
| Vinogradov et al., 2009, USA | Secondary analysis of RCT (Twamley et al., 2012) | Twamley et al., 2012 | 7 | 13 | 26 | 6 | 15 | 6 | 73 |
| Dickinson et al., 2010, USA | Secondary analysis of RCT (Fiszdon et al., 2016) | Fiszdon et al., 2016 | 7 | 16 | 29 | 10 | 9 | 11 | 82 |
| Fiszdon et al., 2004, USA | RCT | / | 7 | 16 | 6 | 10 | 15 | 6 | 60 |
| Lewandowski et al., 2011, USA | Secondary analysis from two RCTs (Hogarty et al., 2006 and Eack et al., 2009) | Hogarty et al., 2006 | 7 | 10 | 16 | 10 | 9 | 6 | 58 |
| Eack et al., 2009 | 7 | 16 | 6 | 10 | 11 | 6 | 56 | ||
| McGurk et al., 2009, USA | RCT | / | 2 | 13 | 26 | 10 | 11 | 3 | 65 |
| Sanchez et al., 2014, Spain | RCT | / | 7 | 13 | 26 | 10 | 5 | 6 | 67 |
| Bellucci et al., 2003, Australia | RCT | / | 2 | 10 | 26 | 6 | 15 | 6 | 65 |
| Thomas et al., 2018, USA | RCT | / | 2 | 13 | 6 | 6 | 15 | 6 | 48 |
| Gomar et al., 2015, Spain | RCT | / | 7 | 16 | 26 | 16 | 11 | 6 | 82 |
| Ramsay et al., 2018, USA | Secondary analysis from one RCT (Fisher et al. 2015) | Fisher et al., 2015 | 7 | 10 | 26 | 10 | 15 | 11 | 79 |
3.6. Moderators affecting treatment response
Twenty studies evaluated at least one moderator; seven assessed two, four evaluated three and, five studies investigated more than three moderators. Taken together, they identified moderators falling into five broad categories: demographic; biological; cognitive and functional; psychological and illness-related aspects. Results for each category are summarised in Table 3.
Table 3.
Summary of identified moderators.
| Type of features | Factors | How many papers | Papers | Association with CR outcomes YES/NO | Outcomes |
|---|---|---|---|---|---|
| Demographics | Gender | 3 |
Farreny et al., 2016 Twamley et al., 2011 Wykes et al., 1999 |
NO | / |
| Education | 3 |
Farreny et al., 2016 Penades et al., 2016 Twamley et al., 2011 |
NO | / | |
| Age | 3 |
Corbera et al., 2017 McGurk and Mueser, 2008 Wykes et al., 2009 |
YES | Younger improve more than older in cognition | |
| 1 | Wykes et al., 2009 | YES | Younger improve more than older in negative symptoms and functioning | ||
| 1 | Twamley et al., 2011 | YES | Older improve more than younger in memory | ||
| 1 | Wykes et al., 2009 | YES | Older improve more than younger in self-esteem | ||
| 1 | Dickinson et al., 2010 | YES | Older improve more than younger in functioning | ||
| 1 | Thomas et al., 2018 | YES | Older improve more than younger in verbal learning | ||
| 4 |
Farreny et al., 2016 Franck et al., 2013 Penades et al., 2016 Wykes et al., 1999 Dickinson et al., 2010 Gomar et al., 2015 |
NO | / | ||
| Biological | Brain structure | 1 | Keshavan et al., 2011 | YES | Higher cortical reserve positively moderated social cognition |
| 1 | Penades et al., 2016 | YES | Greater cortical thickness in the temporal and frontal lobes, linked with greater improvement in verbal memory and non-verbal memory | ||
| 1 | Subramaniam et al., 2017 | YES | Greater integrity of white matter in the right front-occipital fasciculus predicted improvements in attention/vigilance Greater integrity of right corticospinal tract and bilateral medial lemnisci predicted improvements in executive functioning |
||
| 1 | Ramsay et al., 2018 | NO | / | ||
| Genetic variable | 1 | Bosia et al., 2007 | YES | People with Met on active treatment had better outcomes in cognitive flexibility and functioning | |
| 1 | Panizzutti et al., 2013 | YES | Association between COMT gene and response in global cognition | ||
| 1 | Burton et al., 2015 | NO | / | ||
| Cognition and functioning | IQ | 1 | Fiszdon et al., 2006 | YES | Lower IQ associated with cognitive gains |
| 1 | Franck et al., 2013 | YES | Higher IQ associated with lower cognitive gains | ||
| 1 | Twamley et al., 2011 | NO | / | ||
| Learning potential | 1 | Davidson et al., 2016 | YES | Learning potential predicted improvement in verbal and visual memory | |
| Baseline cognition | 2 |
Kurtz et al., 2009 Kurtz et al., 2008 |
YES | Higher baseline cognition larger improvement in functioning | |
| 1 | Farreny et al., 2016 | YES | Higher baseline cognition larger improvement in negative symptoms | ||
| 1 | Penades et al., 2016 | YES | Higher baseline cognition larger improvement in cognition | ||
| 2 |
Rodewald et al., 2014 Twamley et al., 2011 |
YES | Lower baseline cognition larger improvement in cognition | ||
| 1 | Twamley et al., 2011 | YES | Lower baseline cognition larger improvement in functioning | ||
| 3 |
Farreny et al., 2013 McGurk et al., 2009 Ramsay et al., 2018 |
NO | / | ||
| Cognitive insight | 1 | Twamley et al., 2011 | YES | Greater self-reported cognitive problems at baseline associated with larger improvements in cognition | |
| 1 | Burton and Twamley, 2015 | NO | / | ||
| Baseline functioning | 2 |
Farreny et al., 2016 Kurtz et al., 2008 |
YES | Higher baseline functioning associated with a larger improvement in functioning | |
| 1 | Evensen et al., 2017 | YES | Higher baseline functioning associated with higher rates of competitive employment | ||
| 1 | Twamley et al., 2011 | YES | Lower function at baseline associated with larger gains on functioning |
||
| 2 |
Bell et al., 2008 Bell et al., 2014 |
YES | People with poor community function receiving NET + VOC achieved better competitive employment rates and worked more hours than people only in the VOC No different outcomes between the conditions in people with higher community function |
||
| Psychological | Motivation | 1 | Fisher et al., 2015 | YES | Higher baseline motivational system functioning larger improvements in global cognition and verbal memory |
| 1 | Rodewald et al., 2014 | NO | / | ||
| Self-esteem | 1 | Evensen et al., 2017 | YES | Higher baseline self-esteem associated with higher competitive employment and lower unemployment | |
| 1 | Bellucci et al., 2003 | NO | / | ||
| Illness-related | Symptoms | 2 |
Farreny et al., 2013 Twamley et al., 2011 |
YES | Higher negative and positive symptoms at baseline associated with greater improvement in functioning |
| 1 | Twamley et al., 2011 | YES | Higher negative and positive symptoms at baseline associated with greater improvement in cognition | ||
| 1 | Farreny et al., 2016 | YES | Higher disorganized PANSS scale associated with greater improvement in cognition | ||
| 1 | Farreny et al., 2016 | YES | Lower scores for the PANSS excited scale, positive and negative symptoms associated with higher functioning improvements and negative symptoms reduction | ||
| 1 | Ramsay et al., 2018 | YES | Lower baseline symptoms associated with improvements in cognition and left thalamic volume | ||
| 9 |
Bark et al., 2003 Fiszdon et al., 2004 Kurtz et al., 2009 Kurtz et al., 2008 Penades et al., 2016 Rodewald et al., 2014 Sanchez et al., 2014 Wykes et al., 1999 Thomas et al., 2018 |
NO | / | ||
| Medication | 2 |
Twamley et al., 2011 Rodewald et al., 2014 |
YES | People on a lower antipsychotic dose were more likely to complete the therapy and improve | |
| 1 | Thomas et al., 2018 | YES | Higher antipsychotic loads associated with better improvement in verbal learning | ||
| 1 | Vinogradov et al., 2009 | YES | Serum anticholinergic activity associated with lower therapy gains | ||
| 1 | Wykes et al., 1999 | YES | People on atypical antipsychotic had larger effects on cognition compared to those on typical antipsychotics | ||
| 1 | Wykes et al., 2007 | YES | People who received clozapine or typical medication had larger response compared to those on atypical medications | ||
| 3 |
Penades et al., 2016 Farreny et al., 2016 Sanchez et al., 2014 Gomar et al., 2015 |
NO | / | ||
| Diagnosis | 1 | Twamley et al., 2011 | YES | People with schizoaffective disorder had greater improvement in subjective quality of life compared to those with schizophrenia | |
| 1 | Lewandowski et al., 2011 | NO | / | ||
| Comorbid disorders | 1 | McGurk et al., 2009 | YES | Comorbid substance abuse was associated with worse employment outcomes | |
| 1 | McGurk et al., 2009 | NO | Physical comorbid condition (e.g. metabolic deficits) was not associated with employment outcomes | ||
| Duration of illness | 1 | Corbera et al., 2017 | YES | People with shorter illness duration had better outcomes | |
| 4 |
Farreny et al., 2016 Penades et al., 2016 Twamley et al., 2011 Thomas et al., 2018 |
NO | / | ||
| Hospitalisation | 1 | Penades et al., 2016 | NO | / |
3.7. Demographic characteristics
A number of papers reported that gender (Farreny et al., 2016; Twamley et al., 2011; Wykes et al., 1999), education (Farreny et al., 2016; Penades et al., 2016; Twamley et al., 2011) and age (Farreny et al., 2016; Franck et al., 2013; Gomar et al., 2015; Penades et al., 2016; Wykes et al., 1999) were not significant moderators of the effect of CR on therapy outcomes. However, of the studies finding age as a moderator of therapy response, three reported that younger participants benefited more than older in several cognitive domains (Corbera et al., 2017; McGurk et al., 2007; Wykes et al., 2009), negative symptoms and functioning (Wykes et al., 2009). In contrast, four studies found that older participants showed larger improvements in cognition (Thomas et al., 2018; Twamley et al., 2011), self-esteem (Wykes et al., 2009) and, functioning (Dickinson et al., 2010) compared to younger. However, in the study conducted by Dickinson et al. (2010), age was not found as a moderator of the effect of CR on cognition and symptoms.
The generalisability of the demographic factors considered is subject to limitations. There is limited variability in terms of gender [males were the 75.8% (Wykes et al., 1999), 65.5% (Farreny et al., 2016), 68.6% (Twamley et al., 2011)]. Education was measured using different methods [years of education (Penades et al., 2016; Twamley et al., 2011), level of education (Farreny et al., 2016)]. These aspects are likely to affect the quality of the findings and limit the possibility of drawing reliable conclusions. Similarly, in the studies exploring participants' age, each study compared participants from a different age range [under 45 years old and age 45 years old or over, mean age is not reported (McGurk and Mueser, 2008); 17–65 years old, mean 36 (Wykes et al., 2009); younger than 25-older than 40, mean 33 (Corbera et al., 2017); 21–69 years old, mean 45 (Twamley et al., 2011); over age 44 vs. under age 45, mean 35.1 (Thomas et al., 2018); 18–60 years of age, mean 39.5 (Farreny et al., 2016); 18–45 years old, mean 33.5 (Franck et al., 2013); age <55 years, mean 36 (Penades et al., 2016); 19–64 years old, mean 38.6 (Wykes et al., 1999); 21–60 years old, mean 47.7 (Dickinson et al., 2010); 20–65 years old, mean 46 (Gomar et al., 2015)], making it difficult to compare different results. Another limitation is that these studies have a very narrow range to carry out an analysis, for example, in the study conducted by Dickinson et al. (2010) while the age range was 21–60 years old, the majority of participants (within one standard deviation above or below mean) were between 40.3 and 53.5 years limiting how these results will apply to those at the extremes of the distribution. In addition, seven studies analysed age as a continuous variable (Dickinson et al., 2010; Farreny et al., 2016; Franck et al., 2013; Penades et al., 2016; Thomas et al., 2018; Twamley et al., 2011; Wykes et al., 1999) while three studies (Corbera et al., 2017; McGurk and Mueser, 2008; Wykes et al., 2009) considered it as a categorical variable.
3.8. Biological features
The studies included highlighted several potential biological moderators including brain structure and genetic variability. Cortical reserve was identified as a moderator although studies used different measures of this concept. Grey matter volume (Keshavan et al., 2011), cortical thickness (Penades et al., 2016), integrity of the right front-occipital fasciculus, right corticospinal tract and, bilateral medial lemnisci (Subramaniam et al., 2017) were all found to moderate CR outcomes including social cognition, verbal and non-verbal memory, attention/vigilance and executive function. However, Ramsay et al. (2018) reported that baseline thalamic volume did not moderate improvements in cognition and subcortical volume after CR.
Our searches found two studies investigating genotype as a putative moderator of treatment response. These found differential improvement across variants of the COMT gene in favour of global cognition (Panizzutti et al., 2013), cognitive flexibility and functioning (Bosia et al., 2007). By contrast, Burton et al. (2015) suggested no significant effect of the COMT genotype on CR response.
Overall the total samples of these brain and genetic studies was small. No study assessed the possibility that the association between brain structure and COMT genotype and CR response could have been confounded by the effect of antipsychotic medications, despite the noted influence of drugs on brain structure and dopaminergic system (Bosia et al., 2014).
3.9. Cognition and functioning
Our search identified different cognitive and functional aspects as possible moderators. These include cognitive difficulties insight, baseline cognition, IQ, learning potential and baseline functioning.
Twamley et al. (2011) found that higher self-reported cognitive problems at baseline was associated with larger improvements in cognition after CR. Conversely, Burton and Twamley (2015) found no difference between people with good or poor cognitive difficulties awareness.
Nine studies evaluated baseline cognition with six finding significant effects and three no effect on CR outcomes (Farreny et al., 2013; McGurk et al., 2009; Ramsay et al., 2018). However, those that found significant effects reported an association with different outcomes. In four studies higher baseline cognition was associated with larger improvement in functioning (Kurtz et al., 2009; Kurtz et al., 2008), negative symptoms (Farreny et al., 2016) and cognition (Penades et al., 2016) after CR. Conversely, two studies reported that lower initial cognition was associated with larger cognitive improvements (Rodewald et al., 2014; Twamley et al., 2011) and functioning (Twamley et al., 2011) after CR.
Of the three studies investigating IQ, one found lower IQ was related to smaller gains (Fiszdon et al., 2006), one that higher premorbid IQ was related to fewer gains (Franck et al., 2013) and one reported no difference (Twamley et al., 2011).
Our search identified only one study evaluating learning potential which predicted improvement in verbal and visual memory (Davidson et al., 2016).
Of the six studies investigating baseline functioning, three noted that better functioning was associated with a larger improvement in functioning (Farreny et al., 2016; Kurtz et al., 2008) higher competitive employment and lower unemployment (Evensen et al., 2017). In contrast, Twamley et al. (2011) found that people with lower function showed larger gains; with this finding confirmed by Bell et al. (2008). In a more recent study by Bell et al. (2014), people with poor community function receiving CR plus supported employment program had better competitive employment rates and worked more hours than people who only received a supported employment program alone. However, for participants with higher community function at entry to the study CR conferred no extra benefit (Bell et al., 2014).
The main limitation of this set of studies was the relatively small sample sizes which meant that although they found a significant, the effect size reliability is low. Outcomes were measured with different tests, making the comparison complicated (e.g. in baseline cognition studies Kurtz et al. (2008) measured verbal learning and memory with the California Verbal Learning Test, whereas Twamley et al. (2011) used Hopkins Verbal Learning Test; in functioning, Farreny et al. (2016) used Life Skills Profile, Kurtz et al. (2008) the University of California San Diego Performance-based Skills Assessment and, Twamley et al. (2011) Quality of Life Interview; in IQ research, Fiszdon et al. (2006) used the Information subtest of the Wechsler Adult Intelligence Scale, Franck et al. (2013) French National Adult Reading Test).
3.10. Psychological features
Our search identified two psychological factors investigated as possible moderators: motivation, and self-esteem. For motivation, Fisher et al. (2015) reported that an individual's baseline motivation (assessed by anticipatory and consummatory of pleasure) was associated with improvements in global cognition and verbal memory after therapy. But, Rodewald et al. (2014), found that motivation (considered both as negative symptoms and intrinsic motivation) had no effect on improvement in problem-solving ability.
Two studies evaluated self-esteem with one showing that higher self-esteem at baseline was associated with better competitive employment and lower unemployment (Evensen et al., 2017) and the other found no influence on cognitive gains (Bellucci et al., 2003).
It is, however, important to highlight that an accurate comparison between motivation studies is difficult because each study considered a different facet of motivation and measuring motivation is complex. The studies conducted by Bellucci et al. (2003) and Evensen et al. (2017) also have a modest sample size and an active control group (vocational rehabilitation services) that might have influenced the results.
3.11. Illness-related features
We identified six illness-related factors as possible moderators: symptoms, medication, diagnosis, comorbid disorders, duration of illness and number of hospitalisations. In terms of symptoms, some studies found that higher baseline symptoms severity was associated to larger improvements in functioning (Farreny et al., 2013; Twamley et al., 2011) and cognition (Farreny et al., 2016; Twamley et al., 2011). But others reported that lower baseline symptoms severity was related to better functioning (Farreny et al., 2016), negative symptoms (Farreny et al., 2016), cognition and subcortical volume preservation (Ramsay et al., 2018) after therapy. Another nine studies (Bark et al., 2003; Fiszdon et al., 2004; Kurtz et al., 2009; Kurtz et al., 2008; Penades et al., 2016; Rodewald et al., 2014; Sanchez et al., 2014; Thomas et al., 2018; Wykes et al., 1999), found no association between baseline symptoms profile and CR outcomes.
Again, these studies had limitations: used different PANSS factor models and participants in different studies had different levels of symptoms. For example, Twamley et al. (2011) used the PANSS three-factor structure from Kay et al. (1987) but considered only the Positive (mean 16.0) and Negative dimensions (mean 15.6). Ramsay et al. (2018) used the same factor structure but considered Positive (mean 12.65), Negative (mean 17.18) and General symptoms (mean 33.32) scores. Farreny et al. (2013) used both PANSS three- and five-factor (Wallwork et al., 2012), analysing only Negative symptoms (mean 2.7). Farreny et al. (2016), instead, considered a 5-factor structure by Wallwork et al. (2012); Positive (mean 6.8), Negative (mean 16), Disorganized (mean 8.4) Depressed (mean 6.8) and Excited (mean 5.8).
There were also inconsistencies in how medication influenced therapy outcomes with two studies reporting that those on a lower dose of antipsychotic medication were more likely to complete the therapy (Twamley et al., 2011) and show improvement on problem-solving (Rodewald et al., 2014). One study, however, showed the opposite with higher medication levels being associated with improvements in verbal learning (Thomas et al., 2018). Gomar et al. (2015) did not find that antipsychotic dose moderated CR outcomes. Vinogradov et al. (2009) found that serum anticholinergic activity, an index of individual's anticholinergic burden, contributed by the cumulative effect of drugs and their metabolites, was associated with poorer CR response. A study by Wykes et al. (1999) showed that people who received atypical antipsychotic medications showed larger effects on cognition after CR compared to those who had been prescribed typical antipsychotics, but this difference was not maintained at follow-up. In a further study, Wykes et al. (2007) reported that people who received either clozapine or typical antipsychotic achieved better results after therapy in comparison with those who received other atypical medications. Finally, three studies showed that medication levels before therapy did not predict CR response for cognition, functioning or symptoms improvements (Farreny et al., 2016; Penades et al., 2016; Sanchez et al., 2014). It is, however, important to highlight that a comparison between these studies is difficult because each study used different medications (e.g. first- and second-generation of antipsychotics).
Diagnosis and additional comorbid disorders are other illness-related aspects identified as possible moderators. We found only one study (Twamley et al., 2011) suggesting that participants with schizoaffective disorder reported greater CR-associated improvement, in subjective quality of life, compared with those with a diagnosis of schizophrenia. However, Lewandowski et al. (2011) did not find the diagnosis as a moderator. McGurk et al. (2009), comorbid substance abuse was related to worse employment outcomes, after CR plus vocational rehabilitation and vocational rehabilitation alone, while the presence of a physical comorbid condition (e.g. metabolic deficits) was not associated with work outcomes.
The effects of illness duration on CR outcomes were mixed: with superior CR benefits reported for individuals with shorter illnesses length reported by Corbera et al. (2017) but no associations found in four other studies (Farreny et al., 2016; Penades et al., 2016; Thomas et al., 2018; Twamley et al., 2011). Penades et al. (2016) reported that the number of hospitalisations (mean 1.76) had no effects on CR outcomes. However, there is large variability in participants' illness duration across these studies making, again, comparisons difficult with average illness length ranging from 9.3 to 20.5 years. There were also differences in the way these studies analysed illness duration with the only study that found an effect considered it as categorical, unlike all other studies that considered illness duration as continuous and found negative results.
4. Discussion
The aim of this study was to review the literature to identify moderators of CR treatment response which can be used to understand why different participants achieve different outcome after CR.
This review identified 18 moderators considered to have an effect on CR; however, we found no high-quality replicated evidence for any of these. The majority of the studies reviewed lacked adequate power to conduct moderation analysis and half of the studies had poor methodological quality are considered at high risk of bias. The variability in the CR approaches and control groups considered might have also played a role in the lack of findings convergence. Studies also measured the same outcomes in different ways, particularly cognition but also functioning, with measures spanning from capacity to role functioning. Further, the studies included in this review considered a large number of moderators for a large number of outcomes. This created a vast amount of research questions which may make the current set of results at risk of reporting false positives. In addition, different individual potential predictors were investigated independently despite the possibility for a combined effect on CR (e.g. learning potential, education, and age).
To move the personalisation agenda of CR forward evidence on moderators needs to be stronger, replicated and based on appropriately powered research. In the section below, we have highlighted some research implications for the field to consider.
4.1. Research implications
While it is well known that positive findings are more likely to be published (Mlinarić et al., 2017), it is recognised that negative findings play an important role in shaping knowledge advancement. The majority of the studies we reviewed reported positive results. This may be because positive results are more often reported and mentioned in papers. However, it is likely that negative results were found as often but not reported contributing to a “skewed view” of the moderators' landscape. Future research should consider more routine reporting of negative findings.
As the results of this review show, there is no strong evidence for any of the moderators identified. While this is likely to be due to the lack of rigorous studies, it also shows that the field has, so far, focussed on exploratory studies to identify potential moderators. While this is a necessary first step, what the field needs now is replication and evidence consolidation. This will require large datasets and clear hypothesis-driven studies to test specific moderators and estimate more precisely their effect size on outcomes of interest.
It is also important to consider the mechanisms by which a moderator may act on therapy. Like other psychological therapies, CR relies on factors implicated in learning such as age, IQ, learning potential, motivation, self-esteem, and working alliance. These are hypothesis-based moderators and can be investigated based on a coherent theoretical framework. For example, there is evidence that people with schizophrenia have low self-esteem and that this has a negative impact on engagement and may have a detrimental effect on outcomes (Cella and Wykes, 2017; Huddy et al., 2012). Self-esteem also affects the perception that people with schizophrenia have about their cognitive difficulties (Cella et al., 2014). Moderators linked to hypothesised mechanisms of action may be more likely to show consistent trends and be used to understand mechanisms of CR effectively.
Research showed that people with schizophrenia have unique type and severity profiles of cognitive impairment (Silverstein, 2000). As CR targets cognitive difficulties, it is unclear whether different profiles of cognitive impairment would require different therapies regimes. Using an analogy from medication prescribing, one may hypothesise that more severe impairment may require higher therapy intensity (e.g. dose) or frequency. However, as psychological therapy, CR may respond to a different type of personalisation not necessarily to do with therapy dose and frequency but with ingredient types or dose. It may be that adapting or calibrating training to a particular profile of cognitive impairment may help to improve treatment response. A recent attempt at personalisation in this sense has not proven to be successful (Franck et al., 2013) but personalisation in this study was done only on one cognitive domain (e.g. executive function). It may be that training programs need to consider personalisation on multiple cognitive domains.
As research on personalisation progresses, it is also important to consider what outcome is the personalisation aiming to improve. A recent study compared different CR training methods targeting executive and perceptual processes (Best et al., 2019). Personalisation for perceptual processes programs may be very different to executive programs and research in these two areas may reflect different priorities. One, more research-based and more interested in the underlying mechanism of CR, while the other more clinical and focussed on improving outcomes for people with schizophrenia.
4.2. Limitations
The studies included have several limitations that can be grouped in main areas:
-
(i)
Generalisability: While the results in this study are based on a sample's characteristics which reflect people with schizophrenia presenting to clinical services, the generalisability of these findings may be subject to limitations. For instance, the majority of the included studies consider samples with a high proportion of male participants and with a restricted range of age (21.2–48.1 years old). While these are likely to be the most common demographics associated with participants taking part in CR studies, it may be difficult to generalise the findings to female and younger or older people. In addition, we included only English-language publications and the majority of the studies considered took place in United States. These aspects may limit the generalisability of our results to other countries and cultures.
-
(ii)
Methodological quality: The majority of the studies considered lacked independent randomization and/or treatment fidelity assessment. This is a potential source of bias as it may mean that assessor blinding was not rigorously implemented and that participants may have received treatment of variable quality within the same study. Caution should be used in drawing firm conclusions from these studies.”
-
(iii)
Measure heterogeneity: Studies measured the same outcomes using different methods tools, making the comparison and an overall conclusion about the effect of moderators difficult. Future research would benefit for using standardized assessments and well-normed neurocognitive, functional, and symptoms batteries.
-
(iv)
Ratio for study selection: This review only considered studies that mentioned the assessment of moderators in the abstract. This search strategy might therefore have missed relevant papers where the moderators were assessed but not reported. These moderation analyses were likely to be negative. In addition, it was difficult to ascertain if any moderators were hypothesis-driven or opportunistic as most studies did not have pre-registered analysis plans.
-
(v)
Heterogeneity of CR therapy and type of control: The results heterogeneity found in this review may be due to differences in the CR intervention used. These include differences in intervention length, mode of administration (paper and pencil, computer, individual, group), focus of training (single versus multi-domain as well as drill-and-practice versus drill plus strategy training) and whether the intervention is administered as a stand-alone or part of a broader rehabilitation program.
There is also heterogeneity in the control groups with some studies having active control groups (e.g. computer games), others a passive control condition (e.g. treatment as usual), and some studies both. For instance, Farreny et al. (2016) used a CR strategy-based training focus on executive function and metacognition, in a group format, with a duration of 16 weeks and consisting of 32 sessions and did not found age as a moderator of CR benefits. On the other hand, Wykes and Huddy (2009), used CR plus treatment-as-usual, 3 days per week until 40 sessions were completed, in an individual format, and with treatment-as-usual as control group and found age as a moderator of treatment response.
In the future, it might be useful to conduct studies using large datasets produced by aggregating data from existing trial to reduce the effect of different therapy programs and control groups. This is what the National Institute for Mental Health is aiming to do by developing the Database of Cognitive Training and Remediation Studies (DoCTRS) (for example of DoCTRS database use Cella et al., 2017). These data would allow to test mechanisms and moderators of CR with an adequate statistical power and limit the influence of individual studies procedures and control groups on CR outcomes.
5. Conclusion
Even though there is evidence of substantial individual differences in response to CR (Murthy et al., 2012; Wykes et al., 2011), we still have a limited understanding of what causes variability in CR response. This review highlighted five categories of moderators that might influence CR response. We did not find strong evidence in support of any of them. Many significant effects were in opposite directions and most studies were small. The importance of this work is in summarizing the evidence so far accumulated in the field and suggesting moderators to be investigated in future studies. A recommendation is for appropriately powered and hypothesis driven moderation studies. While this may be difficult to achieve in one study, merging data from existing trials may provide the solution. Achieving clear evidence on the role of moderators in CR and using this information for understanding who will benefit more from the therapy relies largely on future studies adhering to good quality methodology and more shared efforts to identify key factors to investigate.
Declaration of competing interest
The authors did not declare any conflicts of interest.
Acknowledgments
This research was supported by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care South London at King's College Hospital NHS Foundation Trust (NIHR CLAHRC-2013-10022). The authors would also like to acknowledge the support of the National Institute for Health Research (NIHR) Biomedical Research Centre in Mental Health at the South London and Maudsley NHS Foundation Trust and the Institute of Psychiatry, Psychology and Neuroscience at King’s College London. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
References
- Allott K., Liu P., Proffitt T.M., Killackey E. Cognition at illness onset as a predictor of later functional outcome in early psychosis: systematic review and methodological critique. Schizophr. Res. 2011;125(2–3):221–235. doi: 10.1016/j.schres.2010.11.001. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . American Psychiatric Pub; 2013. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®) [Google Scholar]
- Bark N., Revheim N., Huq F., Khalderov V., Ganz Z.W., Medalia A. The impact of cognitive remediation on psychiatric symptoms of schizophrenia. Schizophr. Res. 2003;63(3):229–235. doi: 10.1016/s0920-9964(02)00374-2. [DOI] [PubMed] [Google Scholar]
- Baron R.M., Kenny D.A. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J. Pers. Soc. Psychol. 1986;51(6):1173. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bell M.D., Bryson G. Work rehabilitation in schizophrenia: does cognitive impairment limit improvement? Schizophr. Bull. 2001;27(2):269–279. doi: 10.1093/oxfordjournals.schbul.a006873. [DOI] [PubMed] [Google Scholar]
- Bell M.D., Zito W., Greig T., Wexler B.E. Neurocognitive enhancement therapy with vocational services: work outcomes at two-year follow-up. Schizophr. Res. 2008;105(1–3):18–29. doi: 10.1016/j.schres.2008.06.026. [DOI] [PubMed] [Google Scholar]
- Bell M.D., Choi K.-H., Dyer C., Wexler B.E. Benefits of cognitive remediation and supported employment for schizophrenia patients with poor community functioning. Psychiatr. Serv. 2014;65(4):469–475. doi: 10.1176/appi.ps.201200505. [DOI] [PubMed] [Google Scholar]
- Bellucci D.M., Glaberman K., Haslam N. Computer-assisted cognitive rehabilitation reduces negative symptoms in the severely mentally ill. Schizophr. Res. 2003;59(2–3):225–232. doi: 10.1016/s0920-9964(01)00402-9. [DOI] [PubMed] [Google Scholar]
- Best M.W., Bowie C.R. A review of cognitive remediation approaches for schizophrenia: from top-down to bottom-up, brain training to psychotherapy. Expert. Rev. Neurother. 2017;17(7):713–723. doi: 10.1080/14737175.2017.1331128. [DOI] [PubMed] [Google Scholar]
- Best M.W., Milanovic M., Iftene F., Bowie C.R. A randomized controlled trial of executive functioning training compared with perceptual training for schizophrenia Spectrum disorders: effects on neurophysiology, neurocognition, and functioning. Am. J. Psychiatr. 2019;176(4):297–306. doi: 10.1176/appi.ajp.2018.18070849. [DOI] [PubMed] [Google Scholar]
- Bosia M., Bechi M., Marino E., Anselmetti S., Poletti S., Cocchi F., Cavallaro R. Influence of catechol-O-methyltransferase Val158Met polymorphism on neuropsychological and functional outcomes of classical rehabilitation and cognitive remediation in schizophrenia. Neurosci. Lett. 2007;417(3):271–274. doi: 10.1016/j.neulet.2007.02.076. [DOI] [PubMed] [Google Scholar]
- Bosia M., Zanoletti A., Spangaro M., Buonocore M., Bechi M., Cocchi F., Cavallaro R. Factors affecting cognitive remediation response in schizophrenia: the role of COMT gene and antipsychotic treatment. Psychiatry Res. 2014;217(1–2):9–14. doi: 10.1016/j.psychres.2014.02.015. [DOI] [PubMed] [Google Scholar]
- Bowie C.R., Leung W.W., Reichenberg A., McClure M.M., Patterson T.L., Heaton R.K., Harvey P.D. Predicting schizophrenia patients' real-world behavior with specific neuropsychological and functional capacity measures. Biol. Psychiatry. 2008;63(5):505–511. doi: 10.1016/j.biopsych.2007.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burton C.Z., Twamley E.W. Neurocognitive insight, treatment utilization, and cognitive training outcomes in schizophrenia. Schizophr. Res. 2015;161(2–3):399–402. doi: 10.1016/j.schres.2014.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burton C.Z., Vella L., Kelsoe J.R., Bilder R.M., Twamley E.W. Catechol-O-methyltransferase genotype and response to Compensatory Cognitive Training in outpatients with schizophrenia. Psychiatr. Genet. 2015;25(3):131–134. doi: 10.1097/YPG.0000000000000085. [DOI] [PubMed] [Google Scholar]
- Cella M., Wykes T. The nuts and bolts of cognitive remediation: exploring how different training components relate to cognitive and functional gains. Schizophr. Res. 2017;203:12–16. doi: 10.1016/j.schres.2017.09.012. [DOI] [PubMed] [Google Scholar]
- Cella M., Swan S., Medin E., Reeder C., Wykes T. Metacognitive awareness of cognitive problems in schizophrenia: exploring the role of symptoms and self-esteem. Psychol. Med. 2014;44(3):469–476. doi: 10.1017/S0033291713001189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cella M., Preti A., Edwards C., Dow T., Wykes T. Cognitive remediation for negative symptoms of schizophrenia: a network meta-analysis. Clin. Psychol. Rev. 2017;52:43–51. doi: 10.1016/j.cpr.2016.11.009. [DOI] [PubMed] [Google Scholar]
- Corbera S., Wexler B.E., Poltorak A., Thime W.R., Kurtz M.M. Cognitive remediation for adults with schizophrenia: does age matter? Psychiatry Res. 2017;247:21–27. doi: 10.1016/j.psychres.2016.10.084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson C.A., Johannesen J.K., Fiszdon J.M. Role of learning potential in cognitive remediation: construct and predictive validity. Schizophr. Res. 2016;171(1–3):117–124. doi: 10.1016/j.schres.2016.01.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demily C., Franck N. Cognitive remediation: a promising tool for the treatment of schizophrenia. Expert. Rev. Neurother. 2008;8(7):1029–1036. doi: 10.1586/14737175.8.7.1029. [DOI] [PubMed] [Google Scholar]
- Dickinson D., Tenhula W., Morris S., Brown C., Peer J., Spencer K., Bellack A.S. A randomized, controlled trial of computer-assisted cognitive remediation for schizophrenia. Am. J. Psychiatry. 2010;167(2):170–180. doi: 10.1176/appi.ajp.2009.09020264. [DOI] [PubMed] [Google Scholar]
- Evensen S., Ueland T., Lystad J.U., Bull H., Klungsoyr O., Martinsen E.W., Falkum E. Employment outcome and predictors of competitive employment at 2-year follow-up of a vocational rehabilitation programme for individuals with schizophrenia in a high-income welfare society. Nord. J. Psychiatry. 2017;71(3):180–187. doi: 10.1080/08039488.2016.1247195. [DOI] [PubMed] [Google Scholar]
- Farreny A., Aguado J., Ochoa S., Haro J.M., Usall J. The role of negative symptoms in the context of cognitive remediation for schizophrenia. Schizophr. Res. 2013;150(1):58–63. doi: 10.1016/j.schres.2013.08.008. [DOI] [PubMed] [Google Scholar]
- Farreny A., Aguado J., Corbera S., Ochoa S., Huerta-Ramos E., Usall J. Baseline predictors for success following strategy-based cognitive remediation group training in schizophrenia. J. Nerv. Ment. Dis. 2016;204(8):585–589. doi: 10.1097/NMD.0000000000000509. [DOI] [PubMed] [Google Scholar]
- Fisher M., Loewy R., Carter C., Lee A., Ragland D., Niendam T., Vinogradov S. Neuroplasticity-based auditory training via laptop computer improves cognition in young individuals with recent onset schizophrenia. Schizophr. Bull. 2015;41(1):250–258. doi: 10.1093/schbul/sbt232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiszdon J., Bryson G., Wexler B., Bell M. Durability of cognitive remediation training in schizophrenia: performance on two memory tasks at 6-month and 12-month follow-up. Psychiatry Res. 2004;125(1):1–7. doi: 10.1016/j.psychres.2003.10.004. [DOI] [PubMed] [Google Scholar]
- Fiszdon J.M., Cardenas A.S., Bryson G.J., Bell M.D. Predictors of remediation success on a trained memory task. J. Nerv. Ment. Dis. 2005;193(9):602–608. doi: 10.1097/01.nmd.0000177790.23311.ba. [DOI] [PubMed] [Google Scholar]
- Fiszdon J., Choi J., Bryson G., Bell M. Impact of intellectual status on response to cognitive task training in patients with schizophrenia. Schizophr. Res. 2006;87(1–3):261–269. doi: 10.1016/j.schres.2006.04.011. [DOI] [PubMed] [Google Scholar]
- Franck N., Duboc C., Sundby C., Amado I., Wykes T., Demily C., Vianin P. Specific vs general cognitive remediation for executive functioning in schizophrenia: a multicenter randomized trial. Schizophr. Res. 2013;147(1):68–74. doi: 10.1016/j.schres.2013.03.009. [DOI] [PubMed] [Google Scholar]
- Gomar J.J., Valls E., Radua J., Mareca C., Tristany J., del Olmo F., McKenna P.J. A multisite, randomized controlled clinical trial of computerized cognitive remediation therapy for schizophrenia. Schizophr. Bull. 2015;41(6):1387–1396. doi: 10.1093/schbul/sbv059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green M.F., Kern R.S., Braff D.L., Mintz J. Neurocognitive deficits and functional outcome in schizophrenia: are we measuring the “right stuff”? Schizophr. Bull. 2000;26(1):119–136. doi: 10.1093/oxfordjournals.schbul.a033430. [DOI] [PubMed] [Google Scholar]
- Greenwood K., Hung C.-F., Tropeano M., McGuffin P., Wykes T. No association between the catechol-O-methyltransferase (COMT) val158met polymorphism and cognitive improvement following cognitive remediation therapy (CRT) in schizophrenia. Neurosci. Lett. 2011;496(2):65–69. doi: 10.1016/j.neulet.2011.03.075. [DOI] [PubMed] [Google Scholar]
- Bowie, & Harvey, P. D. (2006). Cognitive deficits and functional outcome in schizophrenia. Neuropsychiatr. Dis. Treat., 2(4), 531. [DOI] [PMC free article] [PubMed]
- Huddy V., Reeder C., Kontis D., Wykes T., Stahl D. The effect of working alliance on adherence and outcome in cognitive remediation therapy. J. Nerv. Ment. Dis. 2012;200(7):614–619. doi: 10.1097/NMD.0b013e31825bfc31. [DOI] [PubMed] [Google Scholar]
- Kay S.R., Fiszbein A., Opler L.A. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr. Bull. 1987;13(2):261–276. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- Keshavan M.S., Eack S.M., Wojtalik J.A., Prasad K.M., Francis A.N., Bhojraj T.S., Hogarty S.S. A broad cortical reserve accelerates response to cognitive enhancement therapy in early course schizophrenia. Schizophr. Res. 2011;130(1–3):123–129. doi: 10.1016/j.schres.2011.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurtz M., Wexler B., Fujimoto M., Shagan D., Seltzer J. Symptoms versus neurocognition as predictors of change in life skills in schizophrenia after outpatient rehabilitation. Schizophr. Res. 2008;102(1–3):303–311. doi: 10.1016/j.schres.2008.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurtz M., Seltzer J., Fujimoto M., Shagan D., Wexler B. Predictors of change in life skills in schizophrenia after cognitive remediation. Schizophr. Res. 2009;107(2–3):267–274. doi: 10.1016/j.schres.2008.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levaux M.-N., Vezzaro J., Larøi F., Offerlin-Meyer I., Danion J., Van der Linden M. Cognitive rehabilitation of the updating sub-component of working memory in schizophrenia: a case study. Neuropsychol. Rehabil. 2009;19(2):244–273. doi: 10.1080/09602010802091829. [DOI] [PubMed] [Google Scholar]
- Lewandowski K.E., Eack S.M., Hogarty S.S., Greenwald D.P., Keshavan M.S. Is cognitive enhancement therapy equally effective for patients with schizophrenia and schizoaffective disorder? Schizophr. Res. 2011;125(2–3):291–294. doi: 10.1016/j.schres.2010.11.017. [DOI] [PubMed] [Google Scholar]
- McGurk S.R., Meltzer H.Y. The role of cognition in vocational functioning in schizophrenia. Schizophr. Res. 2000;45(3):175–184. doi: 10.1016/s0920-9964(99)00198-x. [DOI] [PubMed] [Google Scholar]
- McGurk, Mueser K. Response to cognitive rehabilitation in older versus younger persons with severe mental illness. Am. J. Psychiatr. Rehabil. 2008;11(1):90–105. [Google Scholar]
- McGurk S.R., Twamley E.W., Sitzer D.I., McHugo G.J., Mueser K.T. A meta-analysis of cognitive remediation in schizophrenia. Am. J. Psychiatry. 2007;164(12):1791–1802. doi: 10.1176/appi.ajp.2007.07060906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGurk S., Mueser K., DeRosa T., Wolfe R. Work, recovery, and comorbidity in schizophrenia: a randomized controlled trial of cognitive remediation. Schizophr. Bull. 2009;35(2):319–335. doi: 10.1093/schbul/sbn182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medalia, Richardson What predicts a good response to cognitive remediation interventions? Schizophr. Bull. 2005;31(4):942–953. doi: 10.1093/schbul/sbi045. [DOI] [PubMed] [Google Scholar]
- Medalia A., Saperstein A.M., Hansen M.C., Lee S. Personalised treatment for cognitive dysfunction in individuals with schizophrenia spectrum disorders. Neuropsychol. Rehabil. 2018;28(4):602–613. doi: 10.1080/09602011.2016.1189341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mlinarić A., Horvat M., Šupak Smolčić V. Dealing with the positive publication bias: why you should really publish your negative results. Biochem. Med. 2017;27(3):1–6. doi: 10.11613/BM.2017.030201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann. Intern. Med. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- Murthy N., Mahncke H., Wexler B., Maruff P., Inamdar A., Zucchetto M., Alexander R. Computerized cognitive remediation training for schizophrenia: an open label, multi-site, multinational methodology study. Schizophr. Res. 2012;139(1–3):87–91. doi: 10.1016/j.schres.2012.01.042. [DOI] [PubMed] [Google Scholar]
- Panizzutti R., Hamilton S.P., Vinogradov S. Genetic correlate of cognitive training response in schizophrenia. Neuropharmacology. 2013;64:264–267. doi: 10.1016/j.neuropharm.2012.07.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penades R., Pujol N., Catalan R., Masana G., Garcia-Rizo C., Bargallo N., Junque C. Cortical thickness in regions of frontal and temporal lobes is associated with responsiveness to cognitive remediation therapy in schizophrenia. Schizophr. Res. 2016;171(1–3):110–116. doi: 10.1016/j.schres.2016.01.006. [DOI] [PubMed] [Google Scholar]
- Pillet B., Morvan Y., Todd A., Franck N., Duboc C., Grosz A., Krebs M.-O. Cognitive remediation therapy (CRT) benefits more to patients with schizophrenia with low initial memory performances. Disabil. Rehabil. 2015;37(10):846–853. doi: 10.3109/09638288.2014.946153. [DOI] [PubMed] [Google Scholar]
- Ramsay I.S., Fryer S., Boos A., Roach B.J., Fisher M., Loewy R., Mathalon D.H. Response to targeted cognitive training correlates with change in thalamic volume in a randomized trial for early schizophrenia. Neuropsychopharmacology. 2018;43(3):590–597. doi: 10.1038/npp.2017.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodewald K., Holt D.V., Rentrop M., Roesch-Ely D., Liebrenz M., Funke J., Kaiser S. Predictors for improvement of problem-solving during cognitive remediation for patients with schizophrenia. J. Int. Neuropsychol. Soc. 2014;20(4):455–460. doi: 10.1017/S1355617714000162. [DOI] [PubMed] [Google Scholar]
- Sanchez P., Pena J., Bengoetxea E., Ojeda N., Elizagarate E., Ezcurra J., Gutierrez M. Improvements in negative symptoms and functional outcome after a new generation cognitive remediation program: a randomized controlled trial. Schizophr. Bull. 2014;40(3):707–715. doi: 10.1093/schbul/sbt057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverstein S.M. Psychiatric rehabilitation of schizophrenia: unresolved issues, current trends, and future directions. Appl. Prev. Psychol. 2000;9(4):227–247. [Google Scholar]
- Silverstein S.M., Wilkniss S.M. At issue: the future of cognitive rehabilitation of schizophrenia. Schizophr. Bull. 2004;30(4):679–692. doi: 10.1093/oxfordjournals.schbul.a007122. [DOI] [PubMed] [Google Scholar]
- Spitzer R.L., Endicott J., Robins E. Research diagnostic criteria: rationale and reliability. Arch. Gen. Psychiatry. 1978;35(6):773–782. doi: 10.1001/archpsyc.1978.01770300115013. [DOI] [PubMed] [Google Scholar]
- Subramaniam K., Gill J., Fisher M., Mukherjee P., Nagarajan S., Vinogradov S. White matter microstructure predicts cognitive training-induced improvements in attention and executive functioning in schizophrenia. Schizophr. Res. 2017 doi: 10.1016/j.schres.2017.06.062. No Pagination Specified. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas M.L., Bismark A.W., Joshi Y.B., Tarasenko M., Treichler E.B., Hochberger W.C., Light G.A. Targeted cognitive training improves auditory and verbal outcomes among treatment refractory schizophrenia patients mandated to residential care. Schizophr. Res. 2018;202:378–384. doi: 10.1016/j.schres.2018.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twamley, Burton, Vella Compensatory cognitive training for psychosis: who benefits? Who stays in treatment? Schizophr. Bull. 2011;37(Suppl. 2):S55–S62. doi: 10.1093/schbul/sbr059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vinogradov S., Fisher M., Warm H., Holland C., Kirshner M.A., Pollock B.G. The cognitive cost of anticholinergic burden: decreased response to cognitive training in schizophrenia. Am. J. Psychiatry. 2009;166(9):1055–1062. doi: 10.1176/appi.ajp.2009.09010017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vita A., Deste G., De Peri L., Barlati S., Poli R., Cesana B.M., Sacchetti E. Predictors of cognitive and functional improvement and normalization after cognitive remediation in patients with schizophrenia. Schizophr. Res. 2013;150(1):51–57. doi: 10.1016/j.schres.2013.08.011. [DOI] [PubMed] [Google Scholar]
- Wallwork R., Fortgang R., Hashimoto R., Weinberger D., Dickinson D. Searching for a consensus five-factor model of the Positive and Negative Syndrome Scale for schizophrenia. Schizophr. Res. 2012;137(1–3):246–250. doi: 10.1016/j.schres.2012.01.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . vol. 1. World Health Organization; 1992. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. [Google Scholar]
- Wykes T. Predicting symptomatic and behavioural outcomes of community care. Br. J. Psychiatry. 1994;165(4):486–492. doi: 10.1192/bjp.165.4.486. [DOI] [PubMed] [Google Scholar]
- Wykes T., Huddy V. Cognitive remediation for schizophrenia: it is even more complicated. Curr. Opin. Psychiatry. 2009;22(2):161–167. doi: 10.1097/YCO.0b013e328322fbf4. [DOI] [PubMed] [Google Scholar]
- Wykes T., Spaulding W.D. Thinking about the future cognitive remediation therapy—what works and could we do better? Schizophr. Bull. 2011;37(suppl_2):S80–S90. doi: 10.1093/schbul/sbr064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wykes T., Reeder C., Corner J., Williams C., Everitt B. The effects of neurocognitive remediation on executive processing in patients with schizophrenia. Schizophr. Bull. 1999;25(2):291–307. doi: 10.1093/oxfordjournals.schbul.a033379. [DOI] [PubMed] [Google Scholar]
- Wykes T., Reeder C., Landau S., Everitt B., Knapp M., Patel A., Romeo R. Cognitive remediation therapy in schizophrenia: randomised controlled trial. Br. J. Psychiatry. 2007;190:421–427. doi: 10.1192/bjp.bp.106.026575. [DOI] [PubMed] [Google Scholar]
- Wykes T., Steel C., Everitt B., Tarrier N. Cognitive behavior therapy for schizophrenia: effect sizes, clinical models, and methodological rigor. Schizophr. Bull. 2008;34(3):523–537. doi: 10.1093/schbul/sbm114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wykes T., Reeder C., Landau S., Matthiasson P., Haworth E., Hutchinson C. Does age matter? Effects of cognitive rehabilitation across the age span. Schizophr. Res. 2009;113(2–3):252–258. doi: 10.1016/j.schres.2009.05.025. [DOI] [PubMed] [Google Scholar]
- Wykes T., Huddy V., Cellard C., McGurk S., Czobor P. A meta-analysis of cognitive remediation for schizophrenia: methodology and effect sizes. Am. J. Psychiatr. 2011;168(5):472–485. doi: 10.1176/appi.ajp.2010.10060855. [DOI] [PubMed] [Google Scholar]