Abstract
From birth, children living in disadvantaged socioeconomic circumstances (SECs) suffer from worse health than their more advantaged peers. The pathways through which SECs influence children’s health are complex and inter-related, but in general are driven by differences in the distribution of power and resources that determine the economic, material and psychosocial conditions in which children grow up. A better understanding of why children from more disadvantaged backgrounds have worse health and how interventions work, for whom and in what contexts, will help to reduce these unfair differences. Macro-level change is also required, including the reduction of child poverty through improved social security systems and employment opportunities, and continued investment in high-quality and accessible services (eg, childcare, key workers, children’s centres and healthy school environments). Child health professionals can play a crucial role by being mindful of the social determinants of health in their daily practice, and through advocating for more equitable and child-focussed resource allocation.
Keywords: child health, health inequalities, life course, policy, social determinants of health
Background and purpose
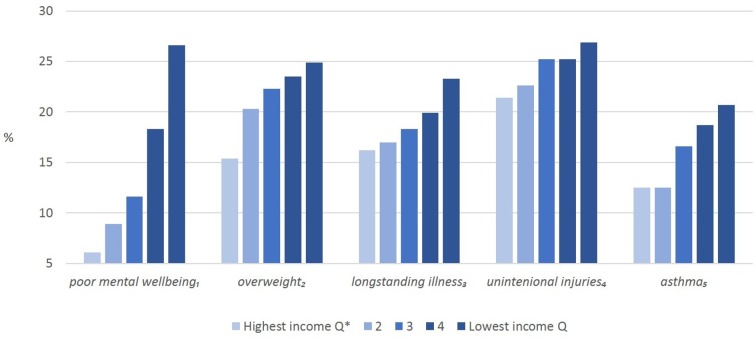
Today, in the UK and across the globe, socioeconomic inequalities are observed in almost all aspects of child physical and mental health,1–3 whereby children living in more socioeconomically disadvantaged circumstances experience worse health than their more advantaged peers. Figure 1 illustrates the degree of inequality seen among children living in the UK, for several important mental and physical health outcomes. These socioeconomic inequalities in health (or health inequalities (HIs)) are preventable and unfair, particularly in the case of children who have little control over their health and the factors which influence it. Socioeconomic HIs emerge early in life, influencing birth weight and risk of prematurity4 and persist throughout childhood, into adolescence,1 adulthood5 and from one generation to the next.5 As shown in figure 1, these health differences are not limited to the most socioeconomically disadvantaged: for every unit increase in socioeconomic disadvantage (regardless of how it is represented), average health worsens. The societal costs of HIs, which have their origins in childhood, carry huge costs to healthcare systems (eg, >£5 billion to the UK National Health Service each year) and society more widely (~£60 billion per annum from welfare payments and lost productivity).6 While the association between socioeconomic circumstances and children’s health is clear, the pathways linking them are complex. The purpose of this review is to consider how inequalities in child health emerge and provide child health professionals with a better understanding of what might be done to alleviate these differences. We begin with a brief description of the social determinants of child health, before turning to the ways in which HIs develop, drawing on a range of key theories. We highlight the ways in which policies might support or exacerbate HIs and finish by discussing future challenges, including for health professionals.
Figure 1.
Child health inequalities, UK Millennium Cohort Study (http://doi.org/10.5255/UKDA-SN-6411-7) (age 7 years, 2008). 1Borderline—abnormal total difficulties score, using the parent-reported Strengths and Difficulties Questionnaire. 2Including obese, applying International Obesity Task Force cut-offs to measured body mass index. 3Parent report of conditions that have troubled or are likely to trouble the child for a period of time. 4Medical opinion sought for one or more unintentional injuries occuring since the last survey (∼5 years). 5Parent report of the child having ever had asthma. *Quintiles, based on OECD equivalised household income.
The term health inequity is sometimes used to refer to HIs which are unfair and avoidable, thus differentiating them from health differences due to natural variation between individuals or those expected because of biological processes (eg, lower mortality rates among children compared with adults due to ageing processes).7 Here, we use the term health inequalities synonymously with health inequities, because it has been and continues to be the most commonly used term in the UK and among Archives readers. We emphasise that, in the context of socioeconomic inequalities in health (which as noted above are unfair and potentially avoidable), inequality carries the same meaning as inequity.7 Socioeconomic HIs in adults are usually captured according to socioeconomic position (SEP). Here, we prefer to use the term socioeconomic circumstances (SECs), because children do not have their own SEP but experience a multitude of SECs that come from their parents or caregivers (eg, educational qualifications, occupational status), the household unit (eg, housing tenure, household income) and the neighbourhood in which they live (eg, area deprivation).5 See online supplementary material for an expanded discussion on measuring HIs. Finally, although we focus on HIs in high-income countries (and predominantly the UK), addressing child HIs is a public health priority globally (https://www.un.org/sustainabledevelopment/sustainable-development-goals/).
archdischild-2018-314808supp001.docx (19.2KB, docx)
Social determinants of child health
Crucial to our understanding of population health and HIs are the social determinants of health (SDH)—the ‘conditions in which we are born, grow up, work and live'.6 The SDH for children are visually represented in the now widely recognised ‘rainbow’, adapted in figure 2 from Bronfenbrenner’s Ecological Systems Theory of Child Development8 and Social Model of Health by Dahlgren and Whitehead.9 At the centre of the model lies the child and their largely fixed characteristics (such as age, sex and ethnicity), and surrounding this are concentric layers of influence that are potentially modifiable—the SDH. The innermost layer includes the determinants that are most proximal to individual health, such as health behaviours and lifestyle factors. For children, this layer also includes the nature of interactions between carer and child (ie, parenting), which directly influence health behaviours in early childhood. Parenting is separate from the characteristics of the carers themselves, which, as depicted in the next layer, include parents’ own health and behaviours. Next are household resources (such as housing quality, income), and then community and social networks. Beyond this are more structural influences of health: the living and working conditions which influence children’s health directly (eg, childcare, schools, health services) and indirectly via their parents (eg, workplace policies around flexible hours and parental leave). And, in the outer layer, macro-level political, cultural, commercial and economic conditions. All of the SDH are inter-related, both within and between the layers, as depicted by the arrows (figure 2).
Figure 2.
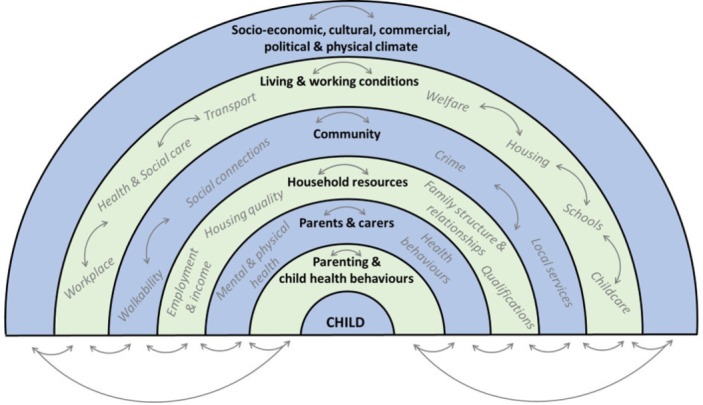
Social determinants of child health. Adapted from Bronfenbrenner8 and Dahlgren and Whitehead.9
The SDH should not be conflated with the social determinants of HIs (after all, history provides many examples of improvements to health determinants which have led to population health improvement but no change or a widening in HIs).10 It is the unequal distribution of the SDH that leads to HIs. The SDH framework has made major contributions to the discourse around HIs, through highlighting the profound influence that the structural SDHs (in the outer layers) have on the socioeconomic circumstances in which people live (ie, the creation of social inequality itself). It has also been used to frame thinking around why health differences exist between socioeconomic groups, including the fact that the SDH are socially distributed and that their influence on health may not be equal across socioeconomic groups (ie, that the consequences of exposure to health risks may be greater for some than others). A more detailed consideration of pathways through which SECs affect health is crucial for identifying the ways in which HIs can be reduced and prevented. The main pathways and the processes through which they unfold are unpacked in the following sections.
Pathways to child health inequalities
A number of theories have arisen around the pathways through which SECs influence health,11–13 developed chiefly with adult health in mind, with the most commonly cited differentiating between material, psychosocial, behavioural and structural factors. The relative importance of these pathways has been widely debated, although it is now generally accepted that no single one dominates.12 We now summarise these pathways, paying attention to their relevance for children’s health in particular.
Material
This pathway focusses on material living conditions and the fact that those from more advantaged social positions have greater access to the resources that support health, such as a warm safe home and nutritional foods.12 14 Despite high levels of average wealth in the UK and other high-income countries, levels of child poverty are high and many families still struggle to afford basic material items, such as food, warm clothing and footwear,15 thus contributing to HIs. For young children, the physical home environment is particularly influential for health. Less socioeconomically advantaged families have lower control over the physical aspects of their home environment—they are more likely to live in homes of insufficient size and quality and are less likely to have direct garden access.12 Material hardship and poor housing quality have been found to mediate the association between SECs and child health, including respiratory problems in childhood.16
Psychosocial
Situated within the psychosocial pathway are two complementary pathways through which SECs influence health. The first refers to the feelings of inferiority, subordination or lack of control that may be produced by social inequality, in turn influencing physical and mental well-being via neuroendocrine pathways. Empirical research has predominantly focused on status and control within the workplace and its influence with cardiovascular health and mortality, with a growing literature on control in the living environment.13 For infants and young children, the influence of this pathway must almost entirely manifest through the feelings and subsequent behaviours of their caregivers, since they have little awareness of social structures and limited influence over their health and health behaviours. As children transition into adolescence they start to develop a sense of social position and gain independence from the family, psychosocial influences on health may become increasingly important. For example, perceptions of social status17 or of family wealth relative to peers,18 has been related to physical and socioemotional well-being, after accounting for other aspects of SECs such as household income.
The second psychosocial pathway refers to the stressors associated with living in social disadvantage and their influence on health and health behaviours. For example, parents’ experiencing increases in financial strain are less likely to quit smoking and more likely to experience relapse.19 Experiences of poverty can have a negative impact on maternal mental health, which in turn influences child health.20 Social support systems can help parents in navigating and overcoming barriers related to social adversity, for example, higher frequency of social contact and receipt of practical or emotional support are associated with higher rates of immunisation.21 However, the meaning of social support and how it ameliorates stress and adversity may have a complex relationship with SECs.22 The emergence of psychosocial stressors and the consequences for parent and child health most likely interact with other SDH, such as flexibility of employment and the availability and quality of housing and childcare.
Behavioural
This pathway suggests that adult HIs arise from inequalities in health behaviours including smoking, alcohol consumption, diet and physical activity. Unhealthy behaviours tend to be more prevalent in less advantaged groups and these undoubtedly influence health. However, empirical research indicates that the behavioural pathway may be less important than others and certainly not sufficient to entirely account for the gap in health observed between the rich and poor. Furthermore, this pathway has been criticised for its simplistic focus, since health behaviours are structurally determined and heavily influenced by psychosocial and material pathways and the wider SDH.23 During pregnancy, infancy and early childhood, children have little control over what they eat or how active they are. Thus, this pathway includes parental and carers’ health-related behaviours (including smoking in pregnancy, infant feeding, immunisations), which are socially distributed and have direct consequences for child health. Some aspects of parenting, such as parenting activities, might also be included in this pathway. For example, inequalities in childhood overweight have been in part attributed to mealtime interactions and rules around screen time.24 As children age they start to develop their own health-seeking and risk-taking behaviours, and these are influenced by SECs and the health behaviours of those around them (including siblings and peers). The criticism of the behavioural pathway’s individualistic focus is even more pertinent to children’s health: parents and carers want to provide the healthiest environment possible for their child, but their capacity to do this may be influenced by the material and psychosocial pathways described above and the structural determinants of health. For example, with rising maternal employment, children are spending increasing periods of time in non-parental care and the type and quality of childcare settings are associated with child health and health behaviours.25 26
Structural
The structural SDH, depicted in the outer layers of figure 2, are the socioeconomic, political, cultural and commercial structures that influence the control, distribution and accessibility of power, resources and services across the population. Health visiting and paediatric services, children’s centres and childcare, schools, social housing, neighbourhood deprivation, the welfare system and food marketing are examples of structural factors that influence child health both directly and via material, psychosocial and behavioural pathways. Seemingly more adult-centric forces (such as working environments) also influence children, by affecting the material and psychological well-being of parents and their parenting capacity (eg, flexible working hours and generous parental leave policies can support infant feeding and parental mental health). Structural theorists believe these structural determinants, particularly those in the very outer layer of the rainbow, to be the root causes of HIs. This is because (in addition to their powerful influence on health) they create social inequality, through market forces on employment rates or the redistribution of income via the tax and benefits system. Fundamental causes theory posits that the influence of SECs on health is so powerful that even if one pathway is intervened on or blocked, SECs will exert their influence via another.27 Thus, also leading to the conclusion that the most effective way to eradicate HIs is to address the structural forces behind the unequal distribution of resources.
Life course approach
The life course approach unifies the SDH and the pathways to HIs outlined above and provides a lens through which we might consider how these factors may vary, operate and interact across an individual’s life and from one generation to the next.28 One component of this is how a child’s family SECs, health and own emerging SEP co-evolve and influence one another over the life course. Health Selection Theory refers to the effects that ill health (in childhood or adulthood) can have on adult SEP, through influencing educational attainment and employment. This reverse association is thought to at least partly explain the higher prevalence of ill health among adults living in less advantaged circumstances.29 However, health selection is implausible in explaining socioeconomic HIs in early life. While parents with children with long-term health conditions may find it harder to maintain well-paid employment30 (thus affecting family SECs), this relationship is not strong enough to explain the large inequalities observed in all aspects of children’s health and well-being31 (including conditions less likely to affect current family SECs, such as childhood overweight). Instead health selection theory serves to demonstrate how HIs, which have their origins in childhood, can perpetuate or widen over the lifecourse.
The life course approach also acknowledges that there are periods within the life course in which exposure to risk factors may be particularly detrimental or beneficial for health and development (eg, environmental lead exposure in infancy and childhood results in serious neurodevelopmental deficits in adulthood; or secure attachment between caregiver and infant supports child development and academic attainment). It also highlights that the relative influences of the SDHs may shift with age (eg, the mother, main caregiver and home are particularly influential during pregnancy and infancy, while childcare, school and neighbourhoods become increasingly important in mid-childhood and beyond). Importantly, the life course perspective provides a framework to consider how exposure to risk factors can accumulate over time (eg, persistent poverty has a deleterious effect on adolescent health14) and how exposure to one risk factor may lead to a chain reaction of additional risk28 (eg, financial insecurity can cause strain on relationships, leading to separation and in turn greater financial strain14).
Two decades ago, the idea that SEP is inherited through genes had been debunked.32 The plausibility of genetic contributions to HIs were still considered possible, if (for example) there was a common set of genes which influenced individual attributes such as intelligence and personality as well as health and health behaviours. The evidence base at the time was minimal and many feared that genetic arguments would distract policy-makers from action on the SDH.33 Since then, the burgeoning field of epigenetics has demonstrated how the interaction between genes and environmental influences may exacerbate rather than explain HIs: environmental exposures (such as stress due to socioeconomic disadvantage) can influence gene expression, in turn altering health.34 Emerging evidence (although predominantly from animal studies) indicates that such alterations can be passed on from one generation to the next, independent of the SECs of those future generations.34 More evidence is required, and it is possible that the overall contribution to HIs will be small. But if proven, this theory would reinforce the argument that the benefits of reducing socioeconomic adversity in today’s children will be seen for generations to come.
Child HIs: mechanisms and policy entry-points
The conceptual model by Diderichsen et al for ‘elucidating the pathways from social context to health outcomes and for introducing policy interventions'35 encompasses the full range of processes through which HIs may arise, perpetuate and be altered, and thus provides a synthesis of the concepts discussed above. The prime driver, or root cause of HIs, is social stratification, shown as mechanism I of figure 3: the process by which structures in society influence SECs for children. The second (II) refers to the greater burden of health risk factors (including material, psychosocial and behavioural) among less advantaged groups (differential exposure). The third (III) highlights how the adverse health impacts of any given risk factor may be greater in less advantaged groups, due to their greater likelihood of also being exposed to other important risk factors that interact (differential vulnerability). For example, the mental health impacts of job loss or unemployment may be greater among lone parent than couple families, because they are more likely to also to experience poverty, health damaging environments and weaker social support systems.36 Fourth (IV), SECs affect the social consequences of childhood illness (differential consequences), thus perpetuating social inequality and HIs across the life course though the process of further social stratification (V). For instance, the adverse impacts of poor health in childhood on academic achievement (and in turn employment status and adult SEP)5 might be greater for those from less advantaged backgrounds.
Figure 3.
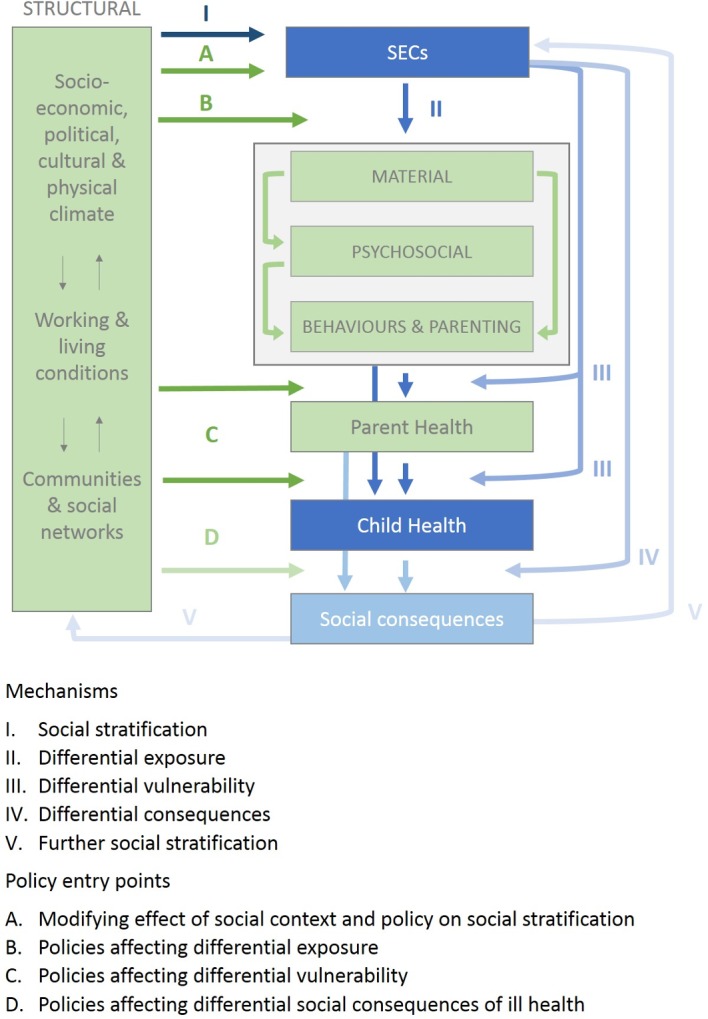
Conceptual model demonstrating the pathways to child health inequalities. Adapted from Diderichsen et al.35 SECs, socioeconomic circumstances.
Importantly, figure 3 also outlines the ‘policy entry points’ through which HIs might be reduced (labelled A–D). This is achieved through intervening on mechanisms I–V, starting with the creation of social inequalities (via entry point A). Policies which influence the process of social stratification relate to the labour market, educational system, welfare and poverty reduction. Sweden provides an inspirational example of entry point A, being among the most equitable countries globally in terms of income distribution and child poverty. Policies to reduce exposures (entry point B) include classic public health interventions such as improvements to housing, working conditions and health services. These may be applied universally, but should disproportionately benefit those from less advantaged backgrounds who are exposed to the worst conditions. Also of relevance to child health and development are early years’ learning services. Although the UK has made important progress in its childcare policies over the past two decades, it still falls behind other countries like Denmark, which has one of the most comprehensive early years’ learning systems in terms of quality, funding and access across all socioeconomic groups. Differential vulnerability (entry point C) might be addressed through schemes such as Sure Start, which was initially introduced in disadvantaged areas of the UK to address the amplified health impacts experienced by families who experience multiple risk factors. The potential of such services to alter inequalities is heavily dependent on how they are rolled out and the context in which they are enacted. Although Sure Start improved outcomes for its recipients, impact on HIs was limited because it failed to reach those most likely to benefit.3 The success of the family nurse partnership in the USA has so far not been replicated in the UK, where high-quality health visiting is already universally available.37 Finally, strategies to reduce differential social consequences (entry point D) might include flexible working policies and social security systems, to protect parents against negative social consequences (eg, loss of earnings) of being ill or having a child with higher healthcare needs. The Scandinavian countries again lead the way, with flexible and generous parental leave policies and high levels of spending on social protection.
Future challenges and possible actions
In general, the drivers of child HIs are the unequal distribution of the power, resources and opportunities to enjoy nurturing environments that give children the best start in life.38 There is no silver bullet for the elimination of child HIs, because they are created, maintained and exacerbated through multiple, related pathways. Macro-level changes are essential, with comprehensive poverty-reduction strategies likely to be some of the most successful.14 However, strategies which take a synergistic approach, across multiple layers of the SDH, hold the greatest potential.23 It has long been pointed out that simply intervening on the SDH will not solve HIs10; we must also consider the processes that lead to the unequal distribution of the SDH. To support this a better evidence base is required, including a more detailed understanding of why children from less advantaged backgrounds have worse health and, from an intervention perspective, how policies and interventions work, for whom and under what circumstances. Intervention studies largely focus on behavioural determinants, which hold the least potential for population health improvement and reduction of HIs, with a dearth of research examining macro-level influences. Few experimental or quasi-experimental studies seek to examine whether the effects of interventions or policy changes vary by SECs. This leads to the Inverse Evidence Law, whereby there is least research on the interventions most likely to have the largest population health impact.39 Ongoing developments in data availability (eg, through multisectoral data linkage) and methods (such as the evaluation of natural experiments and complex interventions) offer enormous potential for building the evidence base going forward. Proportionate universalism, which entails providing a combination of universal services and targeted programmes which change in nature and intensity according to need, has become a favoured recommendation for inequality reduction across the entire social gradient.6 Challenges to implementation exist, however, including ascertaining ways to better identify and engage with families most in need of additional support, while avoiding stigmatisation and balancing limited resources.40 Qualitative research has a crucial role to play in this, as well as in furthering our understanding of how SECs affect people’s day-to-day lives and how together, as families and communities, they strive to reduce the impacts of socioeconomic adversity on their health and well-being.5
In a context of widening inequalities, immediate action is also required. The importance of the early years for population health, HIs and society as a whole is undeniable and actions to tackle inequalities must start before conception and continue throughout childhood.6 This should include the reduction of child poverty and continued investment in high quality and accessible early years' learning and childcare, parenting programmes, key workers and children’s centres38 (while ensuring that the least advantaged benefit most). Although child health professionals may feel disempowered to influence the SDHs and forced to focus on immediate clinical problems, there are a number of important actions that they might take3 41:
Take an equity focus in practice and training: be mindful and make others aware of the unequal distribution of health. Consider the material, psychosocial or behavioural barriers that patients may be experiencing and possible solutions (eg, referrals to welfare benefit advice, food banks, parenting programmes, children’s centres, psychological support).
Generate evidence: put inequalities at the heart of the design, implementation and evaluation of interventions and services, considering representativeness of participants and the possibility of differential uptake and effectiveness. Create examples of best practice. Seize opportunities to harness the increasing powers of service data to further our understanding of child HIs.
Advocate: for more equitable and child-focussed resource allocation and distribution, both within National Health Service policies and among other government sectors.
Acknowledgments
The authors would like to thank colleagues from the MRC/CSO Social and Public Health Sciences Unit, the University of Liverpool and the UCL Great Ormond Street Hospital Institute of Child Health. The authors would also like to thank the many researchers who have contributed to the learning and evidence base around child health and inequalities.
Footnotes
Contributors: AP and DT-R produced the original draft and MW and RD provided critical revisions. All authors have seen and approved the final version.
Funding: AP is funded by a Wellcome Trust University Award (205412/Z/16/Z). AP and RD both received support from the Medical Research Council (MC_UU_12017/13) and the Scottish Government Chief Scientist Office (SPHSU13). DT-R is funded by an MRC Clinician Scientist Fellowship (MR/P008577/1). No special funding for MW.
Competing interests: None declared.
Provenance and peer review: Commissioned; externally peer reviewed.
Patient consent for publication: Not required.
References
- 1. Rougeaux E, Hope S, Law C, et al. . Have health inequalities changed during childhood in the New Labour generation? Findings from the UK Millennium Cohort Study. BMJ Open 2017;7:e012868 10.1136/bmjopen-2016-012868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Viner RM, Hargreaves D, Cheung C. State of Child Health Report. London: Royal College of Paediatrics and Child Health, 2017. [Google Scholar]
- 3. Law C, Parkin C, Lewis H. Policies to tackle inequalities in child health: why haven’t they worked (better)? Arch Dis Child 2012;97:301–3. 10.1136/archdischild-2011-300827 [DOI] [PubMed] [Google Scholar]
- 4. Weightman AL, Morgan HE, Shepherd MA, et al. . Social inequality and infant health in the UK: systematic review and meta-analyses. BMJ Open 20122:e000964 10.1136/bmjopen-2012-000964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Graham H, Power C. Childhood disadvantage and adult health: a lifecourse framework. London: Health Development Agency, 2004. [DOI] [PubMed] [Google Scholar]
- 6. Marmot M, Allen J, Goldblatt P, et al. . Fair society, healthy lives. The Marmot review. London: The Marmot Review, 2010. [Google Scholar]
- 7. Whitehead M, Dahlgren G. Concepts and principles for tackling social inequities in health: Levelling up part 1 Studies on social and economic determinants of population health, No 2. Copenhagen: World Health Organization Regional Office for Europe, 2006. [Google Scholar]
- 8. Bronfenbrenner U. The ecology of human development: Experiments by nature and design. Cambridge, MA: Harvard University Press, 1979. [Google Scholar]
- 9. Dahlgren G, Whitehead M. Tackling inequalities in health: what can we learn from what has been tried? Working paper prepared for the King’s Fund International Seminar on Tackling Inequalities in Health. Ditchley Park, Oxfordshire: London, King’s Fund, 1993. Accessible in: Dahlgren G, and Whitehead M European strategies for tackling social inequities in health Levelling up Part 2 Copenhagen: World Health Organisation Regional Office for Europe 2007. [Google Scholar]
- 10. Graham H. Social determinants and their unequal distribution: clarifying policy understandings. Milbank Q 2004;82:101–24. 10.1111/j.0887-378X.2004.00303.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Macintyre S. The black report and beyond: What are the issues?. Soc Sci Med 1997;44:723–45. 10.1016/S0277-9536(96)00183-9 [DOI] [PubMed] [Google Scholar]
- 12. Benzeval M, Bond L, Campbell M, et al. . How does money influence health? York: Jospeh Rowntree Foundation, 2014. [Google Scholar]
- 13. Whitehead M, Pennington A, Orton L, et al. . How could differences in ‘control over destiny’ lead to socio-economic inequalities in health? A synthesis of theories and pathways in the living environment. Health Place 2016;39:51–61. 10.1016/j.healthplace.2016.02.002 [DOI] [PubMed] [Google Scholar]
- 14. Cooper K, Stewart K. Does Money Affect Children’s Outcomes?: A Systematic Review. York: Joseph Rowntree Foundation, 2013. [Google Scholar]
- 15. Wickham S, Anwar E, Barr B, et al. . Poverty and child health in the UK: using evidence for action. Arch Dis Child 2016;101:759–66. 10.1136/archdischild-2014-306746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Spencer N. Maternal education, lone parenthood, material hardship, maternal smoking, and longstanding respiratory problems in childhood: testing a hierarchical conceptual framework. J Epidemiol Community Health 2005;59:842–6. 10.1136/jech.2005.036301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Sweeting H, Hunt K. Adolescent socio-economic and school-based social status, health and well-being. Soc Sci Med 2014;121:39–47. 10.1016/j.socscimed.2014.09.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bannink R, Pearce A, Hope S. Family income and young adolescents' perceived social position: associations with self-esteem and life satisfaction in the UK Millennium Cohort Study. Arch Dis Child 2016;101:917–21. 10.1136/archdischild-2015-309651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. McKenna CS, Law C, Pearce A. Financial Strain, Parental Smoking, and the Great Recession: An Analysis of the UK Millennium Cohort Study. Nicotine Tob Res 2017;19:1521–5. 10.1093/ntr/ntw269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wickham S, Whitehead M, Taylor-Robinson D, et al. . The effect of a transition into poverty on child and maternal mental health: a longitudinal analysis of the UK Millennium Cohort Study. Lancet Public Health 2017;2:e141–e148. 10.1016/S2468-2667(17)30011-7 [DOI] [PubMed] [Google Scholar]
- 21. Pearce A, Marshall H, Bedford H, et al. . Barriers to childhood immunisation: Findings from the Longitudinal Study of Australian Children. Vaccine 2015;33:3377–83. 10.1016/j.vaccine.2015.04.089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Parkes A, Sweeting H, Wight D. Parenting stress and parent support among mothers with high and low education. J Fam Psychol 2015;29:907–18. 10.1037/fam0000129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Dahlgren G, Whitehead M. European Strategies for tackling social inequalities in health: Levelling up part 2. Studies on social and economic determinants of population health, No 3. Copenhagen: World Health Organisation Regional Office for Europe, 2007. [Google Scholar]
- 24. Parkes A, Sweeting H, Young R, et al. . Does parenting help to explain socioeconomic inequalities in children’s body mass index trajectories? Longitudinal analysis using the Growing Up in Scotland study. J Epidemiol Community Health 2016;70:868–73. 10.1136/jech-2015-206616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Chambers SA, Rowa-Dewar N, Radley A, et al. . A systematic review of grandparents' influence on grandchildren’s cancer risk factors. PLoS One 2017;12:e0185420 10.1371/journal.pone.0185420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Melhuish E, Ereky-Stevens K, Petrogiannis K, et al. . A review of research on the effects of Early Childhood Education and Care (ECEC) upon child development: CARE project; Curriculum Quality Analysis and Impact Review of European Early Childhood Education and Care, 2015. [Google Scholar]
- 27. Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav 1995;35:80–94. 10.2307/2626958 [DOI] [PubMed] [Google Scholar]
- 28. Kuh D, Ben-Shlomo Y, Lynch J, et al. . Life course epidemiology. J Epidemiol Community Health 2003;57:778–83. 10.1136/jech.57.10.778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. O’Donnell O, Van Doorslaer E, Van Ourti T. Health and inequality Volume 2A In: Atkinson A, Bourguignon F, eds Handbook of Income Distribution. Oxford: Elsevier, 2015:1419–533. [Google Scholar]
- 30. Hope S, Pearce A, Whitehead M, et al. . Effects of child long-term illness on maternal employment: longitudinal findings from the UK Millennium Cohort Study. European Journal of Public Health 2017;27:48–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Spencer N, Strazdins L. Socioeconomic disadvantage and onset of childhood chronic disabling conditions: a cohort study. Arch Dis Child 2015;100:317–22. 10.1136/archdischild-2013-305634 [DOI] [PubMed] [Google Scholar]
- 32. Holtzman NA. Genetics and social class. J Epidemiol Community Health 2002;56:529–35. 10.1136/jech.56.7.529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Mackenbach JP. Genetics and health inequalities: hypotheses and controversies. J Epidemiol Community Health 2005;59:268–73. 10.1136/jech.2004.026807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Scorza P, Duarte CS, Hipwell AE, et al. . Research Review: Intergenerational transmission of disadvantage: epigenetics and parents' childhoods as the first exposure. J Child Psychol Psychiatry 2018;67 10.1111/jcpp.12877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Diderichsen F, Evans T, Whitehead M. The social basis of disparities in health : Evans T, Whitehead M, Diderichsen F, Challenging inequities in health: from ethics to action. New York: Oxford University Press, 2001:12–23. [Google Scholar]
- 36. Whitehead M, Burström B, Diderichsen F. Social policies and the pathways to inequalities in health: a comparative analysis of lone mothers in Britain and Sweden. Soc Sci Med 2000;50:255–70. 10.1016/S0277-9536(99)00280-4 [DOI] [PubMed] [Google Scholar]
- 37. Robling M, Bekkers M-J, Bell K, et al. . Effectiveness of a nurse-led intensive home-visitation programme for first-time teenage mothers (Building Blocks): a pragmatic randomised controlled trial. The Lancet 2016;387:146–55. 10.1016/S0140-6736(15)00392-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Whitehead M, Bambra C, Barr B, et al. . Due North: Report of the Inquiry on Health Equity for the North. Liverpool: University of Liverpool and the Centre for Economic Strategies, 2014. [Google Scholar]
- 39. Petticrew M, Whitehead M, Macintyre SJ, et al. . Evidence for public health policy on inequalities: 1: the reality according to policymakers. J Epidemiol Community Health 2004;58:811–6. 10.1136/jech.2003.015289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Lynch JW, Law C, Brinkman S, et al. . Inequalities in child healthy development: some challenges for effective implementation. Soc Sci Med 2010;71:1244–8. 10.1016/j.socscimed.2010.07.008 [DOI] [PubMed] [Google Scholar]
- 41. Spencer N. The social determinants of child health. Paediatr Child Health 2018;28:138–43. 10.1016/j.paed.2018.01.001 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
archdischild-2018-314808supp001.docx (19.2KB, docx)