Abstract
Objective
Commercial motor vehicle (CMV) drivers face many challenges to their health, including poor diet, disease, and crash risk. This study quantifies relationships between the percentage of calories from fat (PCF) and markers of poor health, many of which are associated with increased crash risk.
Methods
Cross-sectional data from 790 CMV drivers were analyzed. Percentages of calories from fat (PCF) were estimated using the National Cancer Institute Percentage Energy from Fat Screener. Adjusted odds ratios (OR) were calculated.
Results
The highest category of PCF (>38.2%) were statistically significantly more likely to not exercise (OR=2.08), have sleep apnea (OR=2.31), snore (OR=1.90), smoke (OR=2.28) and use alcohol (OR=1.87) after adjustments.
Conclusion
Meaningful relationships between PCF and poor health indicators exist. These indicators may provide an intervention to improve the health and safety of CMV drivers.
Keywords: Truck Drivers, Commercial Drivers, Calories, Percent calories from fat, Transportation health, Cross-sectional study
INTRODUCTION
The 5.7 million commercial truck drivers in the United States workforce play a vital role in today’s economy (1). Nearly 71% of all freight transportation involves trucks (2), but truck drivers remain an understudied and underserved population who experience significant health-related risks (3). Truck drivers have high rates of obesity, cardiovascular disease, hypertension, diabetes mellitus, and sleep apnea (4). Previous studies have observed that drivers with these chronic medical conditions are disproportionately more likely to be involved in a number of truck crashes, including preventable crashes (5). The poor working conditions experienced by truck drivers often facilitate unhealthy lifestyles that include inadequate physical activity, poor sleep hygiene, and improper diets, especially high calorie and high-fat diets (6-12). While potentially causal relationships between poor diet and poor health have been observed in the general population, there has not been an evaluation between dietary measures and disease outcome among this at-risk and medically underserved population.
While ketogenic diets have been affirmed effective in weight reduction and obesity, high ‘dietary fat,’ particularly saturated and trans fat, is considered synonymous with risk of obesity and heart disease (13, 14). Strong and consistent associations from a wide body of evidence accrued from observational studies, clinical trials and metabolic studies conducted in diverse human populations have noted that diet and nutritional factors are risk factors for major cardiovascular diseases (CVD) (15). The effect of various dietary fats on plasma lipids (e.g., total cholesterol, lipoprotein fractions, and triglycerides) has constituted a key link in the causal pathway that connects diet to CVD (16). Although dietary recommendations have adapted in response to these findings, total caloric intake has not measurably declined, and the prevalence of diet-related conditions such as obesity and Type 2 diabetes mellitus has grown dramatically (14, 17).
The goal of this study is to assess relationships between the percent of calories from fat and poor health measures (e.g., high BMI, high A1C, high cholesterol, self-reported alcohol use) among truck drivers in a large cross-sectional study. These health measures are indicative of adverse health outcomes previously observed to be prevalent among truck drivers, including CVD, diabetes, and sleep apnea. By examining these associations, this study may facilitate future avenues for intervention in this unusually susceptible population.
METHODS
The study was approved by the Institutional Review Boards of the University of Utah (IRB #22252) and the University of Wisconsin-Milwaukee (IRB #07.02.297). As this is a substudy of a larger cross-sectional study that has been detailed in a prior publication [18], only methods relevant to this particular substudy are described hereafter. This cross-sectional study involved the recruitment of truck drivers at trucking employers, truck stops and truck between 2008 and 2011. Informed consent was obtained prior to enrollment.
Drivers were enrolled at truck shows or truck stops in Iowa, Illinois, Kentucky, Nevada, Texas, Utah, and Wisconsin. Eligible drivers (N=797) were commercial truck drivers in possession of a current United States Commercial Driver’s License (CDL), at least one year of driving experience, and the ability to read in English (English language proficiency is generally a job requirement for truck drivers, and therefore the study questionnaire was not translated). A minority (n=7) were recruited online.
Drivers completed a computerized questionnaire (864 questions) with a research assistant on site. Most drivers successfully completed the questionnaire without assistance. The questionnaire included demographic information, reportable motor vehicle crashes, past medical history, family medical history, physical activities, hobbies, psychosocial factors, and diet. Diet was determined by the use of questions from the National Cancer Institute’s screening tool to estimate the percentage of dietary calories from fat (PCF). This tool has been reported in other studies (19, 20). The questionnaire assessed the frequency of eating a range of foods including protein, fruit, and grains, with a focus on high-fat foods (e.g., fried foods, butter, salad dressing, and cheese). Drivers were asked a series of questions about the frequency of consuming high fat foods, which was then compiled into an estimate of the percentage of total calories which come from fat. The dietary data for each participant were used in a calculation to estimate the percent of calories from fat for each individual.
The questionnaires also recorded self-reported data on health measures, including regular exercise, snoring, regular tobacco use, and regular alcohol use. Reported snoring was used as both a marker for poor sleep quality and possible undiagnosed sleep apnea. Additionally, participants were asked to report any prior diagnoses of sleep apnea, diabetes mellitus, and high cholesterol. Together these were selected as markers of overall poor health.
Additional health-related factors were obtained by a medical professional and were included as variables for this study. These variables included measured height, weight, neck/waist/hip circumferences, blood pressure, and heart rate. Body Mass Index (BMI) was used both as a continuous variable and as a categorical variable categorized into the following five levels (kg/m2): underweight (BMI<18.5), normal weight (18.5 ≤ BMI<25), overweight (25 ≤ BMI<30), obese (30 ≤ BMI<35), and morbidly obese (35 ≤ BMI).
Laboratory-obtained factors included total cholesterol, low-density lipoprotein, high-density lipoprotein, triglycerides, non-fasting glucose, and hemoglobin A1C. Certified testers obtained non-fasting blood measurements via sterile finger-stick. Hemoglobin A1c was measured using a Cholestech® GDX machine (Alere, Inc., Waltham, MA). Total cholesterol, HDL cholesterol, triglycerides, LDL cholesterol, and blood glucose was measured using a Cholestech® LDX machine (Alere, Inc., Waltham, MA). Participants were provided with their results and those with abnormal results were additionally directed to seek medical advice.
Statistical Analyses
Statistical analyses were performed using SAS 9.4 software (SAS Institute Inc., Cary, NC). Statistical significance was determined at α=0.05. Descriptive statistics were calculated to assess normality and distribution prior to categorization and assessing potential relationships. The PCF measure was analyzed two ways: first continually in a linear assessment and secondly categorized into six (6) equally sized groups for assessment of the potential for non-linear relationships. The decision to divide the PCF measures into six (6) equal groups was made a priori in order to maximize statistical power while preserving ability to show non-linear responses. Univariate logistic regression was used to assess the relationships, if any, between PCF and poor health measures. Some factors, such as gender, age, and BMI, were included in the adjusted model to control for confounding even though there was not a statistically significant relationship between the factor and the health measure. Unadjusted and adjusted odds ratios (ORs) with corresponding confidence intervals (CIs) were used to assess the effects of PCF.
RESULTS
There were 797 CMV drivers enrolled in this study, of which 790 had complete data, including objective factors, and were thus included in these analyses.
Descriptive statistics are reported in Table 1. Most study drivers were male (680, 86.1%) and obese (489, 61.9%) with a mean BMI of 32.9 kg/m2. PCF ranged from 24.6% to 51.1%, with 80% of the drivers between 30.1% and 40.0% (interquartile range 31.7% to 36.8%).
TABLE 1.
DESCRIPTIVE STATISTICS
| 1. | Demographic Variables | Mean (SD) or n (%) | |
| Age (years) | 47.2 (10.5) | ||
| Male | 680 (86.1%) | ||
| 2. | Laboratory Variables | ||
| Non-Fasting Glucose | 121.7 (54.8) mg/dL | ||
| Hemoglobin A1C | 5.0 (1.2)% | ||
| Low Density Lipoprotein | 112.7 (33.9) mg/dL | ||
| High Density Lipoprotein | 36.6 (14.1) mg/dL | ||
| High Cholesterol | 208 (26.3%) mg/dL | ||
| Total Cholesterol | 191.5 (41.2) mg/dL | ||
| 3. | Measured Variables | ||
| Neck Circumference | 107.3 (41.7) cm | ||
| Hip Circumference | 114.5 (13.9) cm | ||
| Waist Circumference | 113.2 (17.3) cm | ||
| Systolic Blood Pressure | 131.9 (17.4) mmHg | ||
| Diastolic Blood Pressure | 84.3 (10.7) mmHg | ||
| Body Mass Index (kg/m2) | 32.9 (7.5) kg/m2 | ||
| 4. | Self-Reporting Variables | ||
| Regular Exercise ± | 454 (57.5%) | ||
| Sleep Apnea* | 113 (14.3%) | ||
| Snoring* | 400 (50.6%) | ||
| Tobacco Use§ | 392 (49.6%) | ||
| Alcohol Use | 464 (58.7%) | ||
| Diabetes Mellitus* | 84 (10.6%) | ||
| 5. | Dietary Variables | ||
| Percent Calories from Fat (%) | 34.6 (4.2) | ||
| 24.6%-30.8% | 131 (16.6%) | ||
| 30.8%-32.5% | 132 (16.7%) | ||
| 32.5%-34.0% | 132 (16.7%) | ||
| 34.0%-35.8% | 132 (16.7%) | ||
| 35.8%-38.2% | 132 (16.7%) | ||
| 38.2%-51.1% | 131 (16.6%) |
Self-reported data.
If respondent ever smoked.
If respondent exercise regularly.
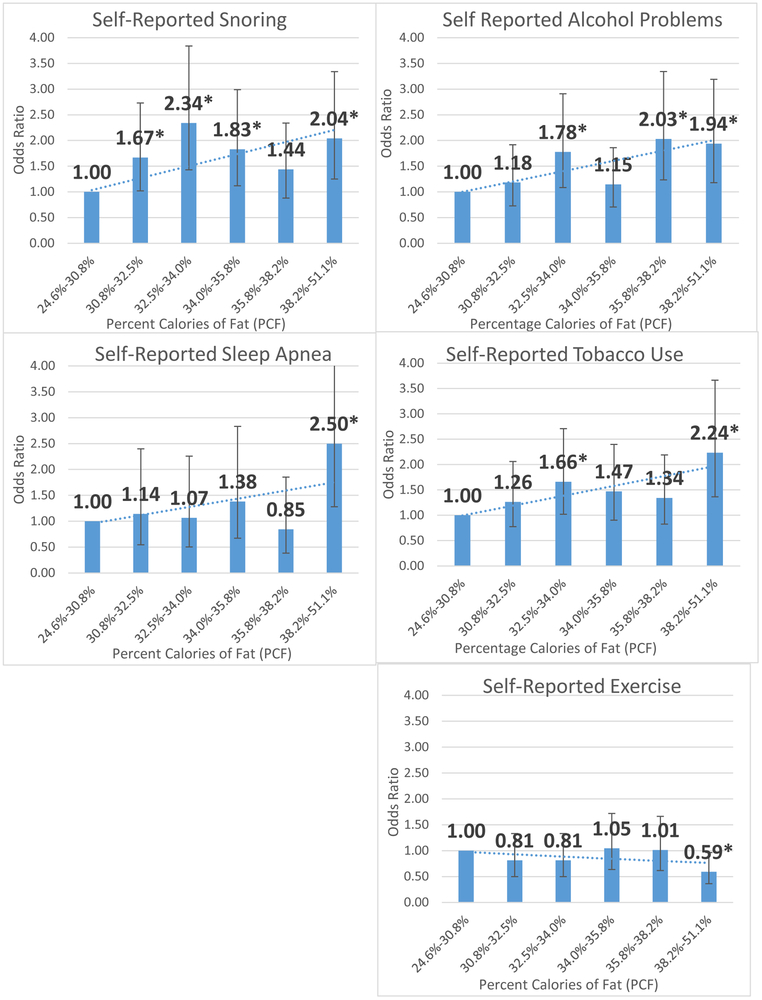
Unadjusted analyses values are shown in Table 2 with drivers in the highest category (38.2%-51.1%) of PCF having approximately about twice the likelihood for all the reported health measures. Adjusted ORs and 95% CI for both categorical and linear relationships between PCF and poor health measures are provided in Figure 1. Adjustment was made for age, gender, and BMI, with analyses finding many statistically significant associations between poor health measures and PCF. Statistically significant linear relationships were found between PCF as a continuous measure and a lack of regular physical activity (p=0.011), diagnosis of sleep apnea (p=0.019), tobacco use (p=0.003), and alcohol use (p=0.020). Non-significant relationships were found between PCF as a continuous measure and snoring (p=0.070), PCF and diagnosis of diabetes mellitus (p=0.155), and PCF and diagnosis of high cholesterol (p=0.700). Analysis of the categorized PCF found similar results; however, there are non-linear relationships between PCF and some poor health measures that are more apparent. These categorical relationships can be seen in Figure 1. Some of the relationships were only statistically significant for the very highest category of PCF (e.g., no regular exercise OR=2.08 and sleep apnea OR=2.31). Others relationships peaked at the lower middle category and the highest category of PCF, but were not statistically significant for the upper middle categories.
Table 2.
Unadjusted Odds Ratios For Poor Health Measures Statistically Associated With Percent Calories From Fat.
| Percent Calories from Fat |
No Regular Physical Activity |
Sleep Apnea | Reported Snoring | Tobacco Use | Alcohol Use |
|---|---|---|---|---|---|
| 24.6%-30.8% | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| 30.8%-32.5% | 1.23 (0.75, 2.01) | 1.14 (0.55, 2.40) | 1.67* (1.02, 2.73) | 1.26 (0.78, 2.06) | 1.18 (0.73, 1.92) |
| 32.5%-34.0% | 1.23 (0.75, 2.01) | 1.07 (0.50, 2.26) | 2.34* (1.43, 3.84) | 1.66* (1.02, 2.71) | 1.78* (1.09, 2.91) |
| 34.0%-35.8% | 0.96 (0.58, 1.57) | 1.38 (0.67, 2.83) | 1.83* (1.12, 2.99) | 1.47 (0.90, 2.40) | 1.15 (0.71, 1.86) |
| 35.8%-38.2% | 0.99 (0.60, 1.62) | 0.85 (0.39, 1.85) | 1.44 (0.88, 2.34) | 1.34 (0.83, 2.19) | 2.03* (1.23, 3.34) |
| 38.2%-51.1% | 1.69* (1.04, 2.76) | 2.50* (1.28, 4.88) | 2.04* (1.25, 3.34) | 2.24* (1.36, 3.67) | 1.94* (1.18, 3.19) |
| Linear Relationship per 10% calories from fat | 1.57 (1.11, 2.22) | 1.76 (1.10-2.82) | 1.37 (0.97-1.93) | 1.68 (1.19-2.37) | 1.52 (1.07-2.16) |
Figure 1:
Odds Ratios And 95% Confidence Intervals For The Relationship Between Percent Calories From Fat And Health Indicators, After Adjusting For Age, Gender And Body Mass Index.
* Indicates Statistical Significance
Following the adjustment of values, the overall trend and relationships remained the same. However, some changes to point estimates were found. There are four significant unadjusted ORs but three significant adjusted ORs in reported snoring. Drivers in the highest category (38.2%-51.1%) of PCF had approximately a two-fold increase in likelihood of also having no regular physical activity (OR=2.08), sleep apnea (OR=2.31), reported snoring (OR=1.90), tobacco use (OR=2.28) and alcohol use (OR=1.87). The category of 32.5%-34.0% PCF also had a significantly higher odds of reporting snoring (OR=2.21), using tobacco (OR=1.70), and using alcohol (OR=1.71). The category of 35.8%-38.2% of PCF had a significantly higher odds of using alcohol (OR=1.90) and the category of 34.0-35.8% of PCF had higher odds of reporting snoring (OR=1.65).
DISCUSSION
This study found significant associations between PCF and lack of regular physical activity, self-reported snoring/sleep apnea, tobacco use, and alcohol use. These relationships are approximately 50% stronger per each 10% increase in fat calories, with the most pronounced associations found in those truck drivers whose diets contained the highest PCF (38.2%-51%). This finding aligns with prior research that notes that unhealthy dietary behaviors often occur in association with other unhealthy behaviors (e.g., smoking, physical inactivity) (21, 22).
The PCF among these CMV drivers is relatively high, with nearly half of study participants reporting PCF greater than 34%. This is meaningfully higher than the mean PCF reported by the general population, which has been estimated at 33.6% among men (23), and suggests PCF may be an indicator of other co-morbid conditions experienced by truck drivers. Dietary recommendations list the ideal PCF at 20–35%, while guidelines from the American Heart Association suggest a PCF of 25–35% (24). This study’s general findings are comparable with others reporting that CMV drivers have considerably worse overall health than other populations (4, 12, 25).
While this study does not implicate a specific cause for the general poor health of drivers, it does find meaningful and statistically significant relationships between PCF and other poor health habits. While there is no causal relationship definable from this study’s data, a plausible theory may be that all of these factors are related to overall driver health behaviors. The strong association of tobacco with heart disease, stroke, and other CVDs may be in part due to the association with a higher fat diet (26). Interestingly, as compared to nonsmokers, smokers have elevated levels of low-density lipoproteins (LDL) and verylow-density lipoproteins (VLDL) and reduced levels of high-density lipoproteins (HDL), which can also be tied to diet (27). Sleep apnea, another common condition among truck drivers, is linked to male sex, higher body mass index (BMI), and increasing age, all of which are characteristics found among many truck drivers (28) and puts drivers at an increased risk of a crash (18).
These results suggest targeted interventions addressing PCF are likely to result in considerable improvements in CMV drivers’ overall health and crash risks. Prior research has indicated that persons who habitually adopt one healthy dietary practice are more likely to adopt other healthy dietary habits as well as practice regular physical activity and abstinence from smoking (29). Physical activity may reduce the risk of CVD by preventing obesity, hypertension, dyslipidemia, and glucose intolerance (30). There is some evidence that physically active adults tend to smoke less, consume healthier diets, and maintain a more favorable body constitution (31).
Strengths of this study include the large sample size of CMV drivers enrolled from a wide variety of geographic locations, with data largely mirroring other national data (32), suggesting these data are representative and generalizable nationally. The assessment of PCF using a validated screener and the ability to control for potential confounders are also strengths. Weaknesses include the inability to assess temporality due to the cross-sectional study design and the potential for systemic error associated with PCF, as these questionnaire-based data naturally have some subjective weaknesses. Longitudinal studies are needed, e.g., to assess if a driver who reduces his/her PCF will experience improvements in health and reduced crashes, or rather if high fat consumption is instead a surrogate marker for risk-taking behavior among CMV drivers for which fat reduction has no impact on crashes.
CONCLUSION
Commercial drivers have significant associations between PCF and lack of regular physical activity, sleep apnea, tobacco use, and alcohol use. These relationships are about 50% higher per 10% increase in fat calories. These data identify drivers at increased risk for these poor health measures. Interventions targeting reductions in fat calories seem likely to improve driver health, although longitudinal studies are required to prove this hypothesis.
ACKNOWLEDGEMENTS:
The authors wish to acknowledge the contributions of numerous individuals, many of whom perform volunteer, or only partially compensated work on this project. Additional sources of funding include the Universities and other, non-commercial resources.
This research was supported, in part, by grants from the Centers for Disease Control and Prevention (NIOSH), 1R01OH009155-01, and 3TC42OH0NI08414. Also supported by the ERC.
Footnotes
Work performed at the University of Utah and the University of Wisconsin—Milwaukee
Conflict of Interest: None
ETHICS REVIEW AND APPROVAL: Signed informed consent was obtained from each driver or from their legal guardian and the study protocol was reviewed and approved by the University of Utah Institutional Review Board (IRB #: 22252) and the University of Wisconsin–Milwaukee Institutional Review Board (IRB#: 07.02.297)
REFERENCES
- 1.FMCSA. Commercial Motor Vehicle Facts—March 2013. Washington, DC: U.S. Department of Transportation, Federal Motor Carrier Safety Administration; 2013. [Google Scholar]
- 2.ATA. Reports, Trends, and Statistics. American Trucking Associations; 2019. [Google Scholar]
- 3.Solomon AJ, Doucette JT, Garland E, McGinn T. Healthcare and the long haul: Long distance truck drivers—a medically underserved population. American journal of industrial medicine. 2004;46:463–471. [DOI] [PubMed] [Google Scholar]
- 4.Thiese M, Effiong A, Ott U, et al. A clinical trial on weight loss among truck drivers. 2015;6:551-104–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thiese MS, Hanowski RJ, Kales SN, et al. Multiple conditions increase preventable crash risks among truck drivers in a cohort study. Journal of occupational environmental medicine. 2017;59:205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Angeles R, McDonough B, Howard M, et al. Primary health care needs for a priority population: A survey of professional truck drivers. Work (Reading, Mass. 2013. [DOI] [PubMed] [Google Scholar]
- 7.Apostolopoulos Y, Sonmez S, Shattell MM, Gonzales C, Fehrenbacher C. Health survey of U.S. long-haul truck drivers: work environment, physical health, and healthcare access. Work (Reading, Mass. 2013;46:113–123. [DOI] [PubMed] [Google Scholar]
- 8.Austin M Clinic keeping truckers tuned up. Truck stop offers health on the road. Colo Nurse. 2006;106:19. [PubMed] [Google Scholar]
- 9.Passey DG, Robbins R, Hegmann KT, et al. Long haul truck drivers’ views on the barriers and facilitators to healthy eating and physical activity: A qualitative study. International Journal of Workplace Health Management. 2014;7:121–135. [Google Scholar]
- 10.Ronna BB, Thiese MS, Ott U, et al. The association between cardiovascular disease risk factors and motor vehicle crashes among professional truck drivers. Journal of occupational and environmental medicine/American College of Occupational and Environmental Medicine. 2016;58:828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thiese MS, Hanowski RJ, Kales SN, et al. Multiple conditions increase preventable crash risks among truck drivers in a cohort study. Journal of occupational and environmental medicine. 2017;59:205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thiese MS, Hanowski RJ, Moffitt G, et al. A retrospective analysis of cardiometabolic health in a large cohort of truck drivers compared to the American working population. American journal of industrial medicine. 2018;61:103–110. [DOI] [PubMed] [Google Scholar]
- 13.Forouhi NG, Krauss RM, Taubes G, Willett W. Dietary fat and cardiometabolic health: evidence, controversies, and consensus for guidance. BMJ. 2018;361:k2139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dashti HM, Mathew TC, Khadada M, et al. Beneficial effects of ketogenic diet in obese diabetic subjects. J Molecular cellular biochemistry. 2007;302:249–256. [DOI] [PubMed] [Google Scholar]
- 15.Reddy KS, Katan MBJPhn. Diet, nutrition and the prevention of hypertension and cardiovascular diseases. 2004;7:167–186. [DOI] [PubMed] [Google Scholar]
- 16.Assmann G, Schulte HJTAjoc. Relation of high-density lipoprotein cholesterol and triglycerides to incidence of atherosclerotic coronary artery disease (the PROCAM experience). 1992;70:733–737. [DOI] [PubMed] [Google Scholar]
- 17.Hu FB, Manson JE, Willett WCJJotACoN. Types of dietary fat and risk of coronary heart disease: a critical review. 2001;20:5–19. [DOI] [PubMed] [Google Scholar]
- 18.Thiese MS, Ott U, Robbins R, et al. Factors Associated With Truck Crashes in a Large Cross Section of Commercial Motor Vehicle Drivers. Journal of Occupational and Environmental Medicine. 2015;57:1098–1106. [DOI] [PubMed] [Google Scholar]
- 19.Thompson FE, Midthune D, Subar AF, Kipnis V, Kahle LL, Schatzkin A. Development and evaluation of a short instrument to estimate usual dietary intake of percentage energy from fat. Journal of the American Dietetic Association. 2007;107:760–767. [DOI] [PubMed] [Google Scholar]
- 20.Thompson FE, Midthune D, Williams GC, et al. Evaluation of a short dietary assessment instrument for percentage energy from fat in an intervention study. The Journal of nutrition. 2008;138:193S–199S. [DOI] [PubMed] [Google Scholar]
- 21.Yach D, Leeder SR, Bell J, Kistnasamy B. Global Chronic Diseases. Science. 2005;307:317–317. [DOI] [PubMed] [Google Scholar]
- 22.Jezewska-Zychowicz M, Gębski J, Guzek D, et al. The Associations between Dietary Patterns and Sedentary Behaviors in Polish Adults (LifeStyle Study). Nutrients. 2018;10:1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.CDC. Diet/Nutrition: Dietary intake for adults aged 20 and over. 2017.
- 24.Mozaffarian D, Ludwig DS. The 2015 US dietary guidelines: lifting the ban on total dietary fat. Jama. 2015;313:2421–2422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sieber WK, Robinson CF, Birdsey J, et al. Obesity and other risk factors: the national survey of US long‐haul truck driver health and injury. 2014;57:615–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cundiff DKJMMgm. Diet and tobacco use: analysis of data from the diabetic control and complications trial, a randomized study. 2002;4:2–2. [PubMed] [Google Scholar]
- 27.Gossett LK, Johnson HM, Piper ME, Fiore MC, Baker TB, Stein JH. Smoking intensity and lipoprotein abnormalities in active smokers. J Clin Lipidol. 2009;3:372–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bauters F, Rietzschel ER, Hertegonne KB, Chirinos JAJCar. The link between obstructive sleep apnea and cardiovascular disease. 2016;18:1. [DOI] [PubMed] [Google Scholar]
- 29.Kesaniemi YA, Danforth E, Jensen MD, et al. Dose-response issues concerning physical activity and health: an evidence-based symposium. 2001;33:S351–S358. [DOI] [PubMed] [Google Scholar]
- 30.Kubota Y, Evenson KR, MacLehose RF, et al. Physical activity and lifetime risk of cardiovascular disease and cancer. 2017;49:1599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pate RR, Heath GW, Dowda M, Trost SGJAjoph. Associations between physical activity and other health behaviors in a representative sample of US adolescents. 1996;86:1577–1581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sieber WK, Robinson CF, Birdsey J, et al. Obesity and other risk factors: the national survey of U.S. long-haul truck driver health and injury. American journal of industrial medicine. 2014;57:615–626. [DOI] [PMC free article] [PubMed] [Google Scholar]