Abstract
Objective
To develop a brief screening instrument to assess risk of suicide in pediatric emergency department (ED) patients.
Design
A prospective, cross-sectional instrument development study which evaluated 17 candidate screening questions assessing suicide risk in young patients. The Suicidal Ideation Questionnaire (SIQ) served as criterion standard.
Setting
Three urban, pediatric EDs associated with tertiary care teaching hospitals.
Patients/Participants
A convenience sample of 524 patients aged 10–21 years who presented with either medical/surgical or psychiatric chief complaints to the ED between September 2008–December 2010.
Main Exposure
Participants answered 17 candidate questions followed by the SIQ.
Main Outcome Measures
Sensitivity, specificity, predictive values, likelihood ratios, and area under the receiver operating characteristic curves of the best-fitting combinations of screening questions for detecting elevated risk of suicide.
Results
524 patients were screened (344 medical/surgical and 180 psychiatric). Fourteen (4%) of the medical/surgical patients and 84 (47%) of the psychiatric patients were at elevated suicide risk on the SIQ. Of the 17 candidate questions, the best-fitting model was comprised of 4 questions assessing: current thoughts of being better off dead, current wish to die, current suicidal ideation, and past suicide attempt. This model had a sensitivity of 96.9% (95% CI, 91.3%–99.4%), specificity of 87.6% (95% CI, 84.0%–90.5%), and a negative predictive value (NPV) of 99.7% (95% CI, 98.2%–99.9%) for medical/surgical patients; 96.9% (95% CI, 89.3%–99.6%) for psychiatric patients.
Conclusions
A four-question screening instrument, the Ask Suicide-Screening Questions (ASQ), with high sensitivity and NPV, can identify risk of suicide in patients presenting to pediatric EDs.
Keywords: suicide screening, emergency department, pediatric patients, children, adolescent, young adults, risk of suicide, suicidal ideation, suicidal behavior
INTRODUCTION
Youth suicide is an international public health problem. In 2007, suicide was the third leading cause of death among youth ages 10 to 24 years, accounting for 4,320 deaths in the United States.1 Non-fatal suicide attempts are more prevalent, affecting as many as 5–8% of children and adolescents annually,2–5 resulting in significant morbidity and increased utilization of emergency departments (EDs) and hospitals.
Early identification and treatment of patients at elevated risk of suicide is a key suicide prevention strategy,6 yet high-risk patients are often not recognized by healthcare providers.7 In fact, the majority of individuals who die by suicide have visited a healthcare provider in the year before their death, most within the prior three months.7–8 Whereas medical visits afford clinicians an opportunity to identify and refer patients at risk for suicide,9 individuals often present solely with somatic complaints and infrequently discuss suicidal thoughts and plans unless asked directly.10
In 2010, the Joint Commission (JC) issued a “Sentinel Event Alert,” suggesting suicide screening for all patients visiting healthcare settings.11 Additionally, the American Academy of Pediatrics (AAP) called for rapid, easy to administer suicide screening tools to guide healthcare clinicians in the assessment of suicide risk among young people in medical settings.12
The ED is a promising venue for identifying young people at risk of suicide.13 ED clinicians are often the sole connection with the healthcare system for millions of youth and their families; they are uniquely positioned to screen for suicide risk in patients and assist in the process of making clinically appropriate referrals for mental health treatment.14–16 Nevertheless, the majority of patients presenting to the ED are not currently assessed for risk of suicide.17 Time constraints, inadequate training and the lack of proper screening instruments are reported as reasons why ED clinicians do not routinely screen for suicide risk.18
ED clinicians require tools that do not assume extensive psychiatric training to administer.19 Instruments to guide these clinicians, such as the 4-item Risk of Suicide Questionnaire (RSQ), were developed and validated on pediatric ED psychiatric populations.20–22 However, brief instruments to assess risk of suicide in patients that present to EDs for medical or surgical reasons do not yet exist.
The primary aim of this study was to develop a brief valid screening instrument that could assess risk of suicide in pediatric and young adult patients evaluated in EDs for medical/surgical reasons. In order not to burden ED workflow, we sought to include the smallest number of questions in our instrument that could identify youth with suicidal thoughts, yet maintained high sensitivity, specificity, and NPV. Psychiatric patients were included in the sample to determine if one screening instrument could be valid for all pediatric patients evaluated in the ED, regardless of their chief complaint.
METHODS
Study Settings and Sample
Between September 2008 and December 2010, we prospectively enrolled convenience samples of patients aged 10–21 years who presented with either medical/surgical or psychiatric complaints to one of three large pediatric EDs associated with major urban teaching hospitals.
Exclusion criteria included (1) developmental disability, cognitive impairment, or communication disorder such that the patient was not able to comprehend questions or communicate their answers; (2) triage level 1(for the medical/surgical patients only)23 suggesting that the patient was not physiologically stable enough to be approached; (3) parent/legal guardian unavailable for patients < 18 years; and (4) parents/guardians and/or patients were non-English speaking. No exclusions were based on gender, race, or ethnicity.
Patients with psychiatric complaints were included to achieve our secondary aim of creating a screening instrument for all patients in a pediatric ED, and to ensure that enough subjects with the outcome of interest (at risk of suicide) were included in the total sample. Given that patients with psychiatric complaints accounted for less than 5% of total annual ED visits across sites, we adopted a strategy of approaching every eligible psychiatric patient and every other patient with a medical/surgical complaint for recruitment into the study.
The Institutional Review Boards at the participating institutions and the National Institute of Mental Health approved this study. For participants <18 years of age, written informed consent was obtained from the parent/guardian, and written informed assent was obtained from the patient. All participants ≥18 years of age provided written informed consent.
Instruments
17 Candidate Suicide Screening Questions
Seventeen candidate screening questions were assembled based on risk factors for suicide in adolescents, including previous suicide attempt history, suicidal ideation, depression, hopelessness, substance abuse, and social isolation. The 17 candidate questions were identified from several sources, including published literature on adolescent suicide risk, interviews with adolescent suicide experts and senior pediatric mental health clinicians, items from the Centers for Disease Control and Prevention Youth Risk Behavior Survey,2 and from the existing RSQ.20 The 17 candidate questions for the new measure were reviewed and revised by a panel of mental health clinicians, health services researchers, and survey methodologists for use among young patients presenting to an ED. The adapted questions were then pilot-tested by several pediatric ED clinicians and mental health specialists in a sample of adolescent psychiatric inpatients and healthy youths, for appropriateness, comprehensibility and ease of administration. All items were phrased in the form of a question with possible responses of “yes,” “no,” or “no response.” Nine of the items were considered “trigger” items because positive endorsement represented potential significant emotional distress; if a subject responded positively, further psychiatric assessment would be “triggered” automatically, regardless of other answers. These questions asked about severe depression, suicidal ideation and suicidal behavior.
Suicidal Ideation Questionnaire
The Suicidal Ideation Questionnaire (SIQ),24 a self-reported measure of the severity of suicidal ideation in adolescents, was used as the criterion standard to validate the 17 candidate questions. Two versions of the SIQ are available, depending on the participant’s age. For this study, the 30-item SIQ was administered to participants > 15 years of age; the 15-item SIQ-JR was administered to participants ≤ 14 years of age. In both versions of the SIQ, individuals are asked to rate the frequency with which a thought occurs on a 7-point scale ranging from “almost every day” to “never.” A cutoff score is used to judge the severity level of suicidal ideation warranting additional psychiatric evaluation. A total score of 41 or above was considered clinically significant (31 or above for the SIQ-JR). In addition, the SIQ has 8 items (6 on the SIQ-Jr) deemed “critical items” because they directly assess serious self-destructive behavior. If a person responds positively to 3 or more of those items (2 or more on the SIQ-Jr), they are also considered to have clinically significant suicidal ideation.24 The SIQ has demonstrated a high reliability (r = 0.97 [SIQ], r = 0.94 [SIQ-JR]), validity and predictive ability.24–25
Procedure
After the initial triage assessment and room assignment, participants were administered the 17 candidate questions followed by the SIQ by trained bachelor or masters level research assistants. A survey containing questions about socio-demographic information, history of medical and psychiatric illness, prior healthcare utilization, and a screening evaluation was also administered. Interviews were conducted without the parent/guardian in the room, but participants were told that if the research assistants had any concerns about their safety, their parents would be notified and pertinent information would be shared with the ED clinical staff.
As a safety measure, any patient who responded positively to any 1 of 9 “trigger” screening questions on the 17 item questionnaire (e.g., any level of current suicidal ideation, past suicidal behavior, or severe depression) or scored positive on the SIQ, or responded positively to any of the 8 SIQ critical items, required a further psychiatric assessment, which was conducted as per standard of care for suicidal risk in each ED.
Statistical Analysis
We calculated the frequencies of positive responses to all 17 candidate and SIQ items as well as the frequencies of all demographic, clinical, and healthcare utilization characteristics for our sample. To measure validity of the candidate questions, we examined the agreement between individual candidate questions and risk of suicide as assessed by the SIQ, with the chance corrected kappa statistic.26 We then constructed logistic regression models to examine the ability of different combinations of the candidate questions to predict risk of suicide as assessed by the SIQ; only candidate questions with kappa ≥0.40 were considered in these models.
Models were estimated using the logistic procedure of SAS Version 9.2.27 Because a prior suicide attempt is the most potent predictor of future suicidal behavior,28 we made an a priori decision to retain question 16 (“Have you ever tried to kill yourself?”) in all regression models. Initially, we used a backward stepwise procedure to arrive at a reasonably parsimonious model that retained a high level of sensitivity. Next, we evaluated all possible combinations of the candidate questions remaining after the stepwise procedure. A positive response to any one of the candidate questions constituted a positive screen for risk of suicide. The predictive ability of each model was assessed using the c statistic, which represents the area under the receiver operating characteristic curve.29–30
We calculated the sensitivity (the probability of a positive result when given to youth who are at risk for suicide), the specificity (the probability of a negative result when given to youth who are not at risk for suicide), the positive predictive value (PPV; the probability that a child who screened positive actually is at risk for suicide), and the negative predictive value (NPV; the probability that a child who screened negative actually is not at risk for suicide). Likelihood ratios (LRs) were calculated to summarize the diagnostic accuracy of the best-fitting combination of screening questions. Ninety-five percent confidence intervals (CIs) for the sensitivity, specificity, PPV, and NPV were calculated using exact binomial methods.31 Because of the clinical significance and relative importance of not misclassifying suicidal youths as false-negatives, we also identified the proportion of youth at risk of suicide (as determined by the SIQ), who would have been undetected by each combination of the 17 candidate questions. We arrived at the final model by choosing the candidate items that maximized sensitivity, specificity, and NPV such that the minimum number of suicide positive patients would be misclassified and ED clinicians would not be overburdened managing false-positive patients.
The sample size calculation was based on sensitivity (98%)/specificity (37%) results reported in the previous study by Horowitz et al.,13 and on the expectation that two-thirds of our participants would present to the ED with medical/surgical concerns (by design, medical/surgical patients were oversampled). α and β were set at 0.05 (two-tailed) and 0.10 (90% power), respectively. Using McNemar’s test of equality of paired proportions, we calculated a minimum sample size of 388 participants, which we rounded up to 450 (~150 participants per site).
RESULTS
A total of 1,170 (783 medical/surgical, 364 psychiatric, 23 undetermined) patients were approached during the study period across the three sites; 803 (69%) patients were eligible for participation; 529 (66%) consented to participate, of whom 524 (344 medical/surgical and 180 psychiatric) completed the screening protocol (Figure 1). There were no significant differences in age, race/ethnicity, gender, or presenting complaint (medical/surgical or psychiatric) between those who did and did not participate in this study. Characteristics of study participants are shown in Table 1. The mean age (standard deviation) at enrollment was 15.2 (±2.6) years. The majority of the sample was female (57.0%), white (50.4%), and privately insured (53.2%).
Figure 1. Participant Flow.
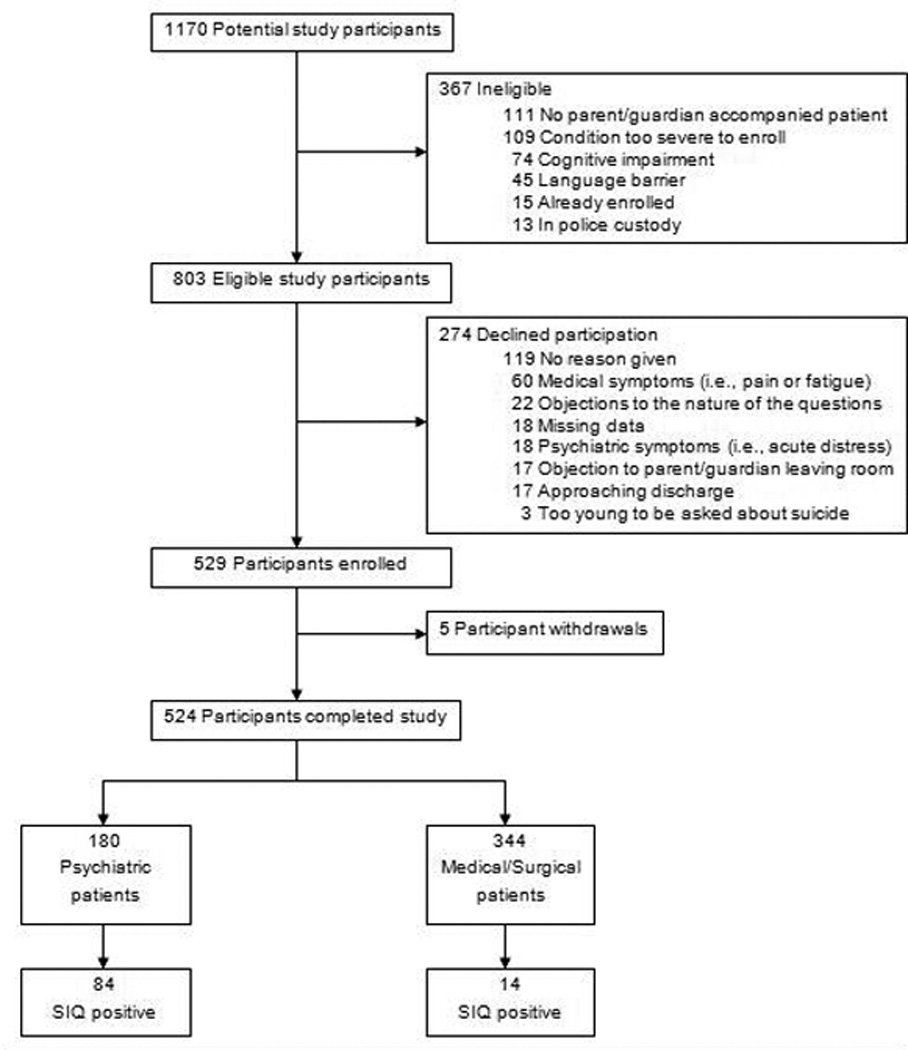
*A positive score on the Suicidal Ideation Questionnaire (SIQ) is defined as scoring above a cut-off of 31 on the SIQ-Jr or 41on the SIQ and/or a positive SIQ Critical Item response.
Table 1.
Characteristics of the 524 Study Patientsa
| Total (N=524) |
Psychiatric (N=180) |
Medical/Surgical (N=344) |
|
|---|---|---|---|
| Age in years | |||
| Mean (SD) | 15.2 (2.6) | 14.4 (2.3) | 15.6 (2.6) |
| Gender | |||
| Male | 226 (43.1) | 75 (41.7) | 151 (43.9) |
| Female | 298 (56.9) | 105 (58.3) | 193 (56.1) |
| Race/ethnicity | |||
| White | 264 (50.4) | 102 (56.7) | 162 (47.1) |
| Black | 155 (29.6) | 52 (28.9) | 103 (29.9) |
| Hispanic/Latino | 47 (9.0) | 11 (6.1) | 36 (10.5) |
| Asian | 12 (2.3) | 3 (1.7) | 9 (2.6) |
| Other/unknown | 46 (8.8) | 12 (6.7) | 34 (9.9) |
| Insurance | |||
| Private | 279 (53.2) | 100 (55.6) | 179 (52.0) |
| Public | 196 (37.4) | 64 (35.6) | 132 (38.4) |
| Public & Private | 16 (3.1) | 7 (3.9) | 9 (2.6) |
| None | 33 (6.3) | 9 (5.0) | 24 (7.0) |
| Site | |||
| CNMC | 156 (29.8) | 50 (27.8) | 106 (30.8) |
| CHB | 199 (38.0) | 82 (45.6) | 117 (34.0) |
| NCH | 169 (32.2) | 48 (26.7) | 121 (35.2) |
Abbreviations: SD indicates standard deviation; CNMC, Children’s National Medical Center; CHB, Children’s Hospital Boston; NCH, Nationwide Children’s Hospital.
Data are presented as number (percentage) unless otherwise specified.
Ninety-eight of 524 (N=84 psychiatric, N=14 medical/surgical) participants (18.7%) were at elevated risk for suicide based on the criterion standard SIQ. The chance-corrected agreement between individual candidate questions and suicidal risk as determined by the SIQ ranged from kappa of 0.78 (95% CI, 0.72–0.85) to −0.06 (95% CI, −0.09–0.02) (Table 2). Logistic regression analyses revealed that there was little improvement in the model properties obtained beyond the inclusion of 4 candidate questions. The top 6 combinations of candidate questions are provided (Table 3). These models represent the best-fitting combinations of screening questions that maximized sensitivity, specificity and NPV.
Table 2.
Chance-corrected agreement between 17 candidate screening items and the SIQ for the assessment of risk for suicide in entire cohort of patients with medical/surgical and psychiatric complaints (N=524)
| Item | Question | % Yes |
LR | Kappa (95% CI) |
c- statistic |
|---|---|---|---|---|---|
| 1 | Has something very stressful happened to you in the past few weeks? |
48.1 | 50.3 | 0.24 (0.17–0.31) | 0.69 |
| 2 | In the past few weeks, have you felt so nervous or worried in a way that felt unbearable, like you couldn’t stand it anymore? |
29.8 | 106.4 | 0.45 (0.36–0.53) | 0.77 |
| 3 | In the past few weeks, have you been bullied or picked on so much that you felt like you couldn’t stand it anymore? |
11.5 | 10.2 | 0.14 (0.04–0.24) | 0.56 |
| 4 | Do you or anyone in your life think you have a problem with drugs or alcohol? |
10.3 | 28.1 | 0.24 (0.14–0.35) | 0.60 |
| 5 | Have you ever felt hopeless, like things would never get better? |
51.7 | 89.5 | 0.29 (0.23–0.36) | 0.75 |
| 6 | Do you feel like you might as well give up because you can’t make things better for yourself? |
24.0 | 182.8 | 0.62 (0.54–0.70) | 0.85 |
| 7 | In the past few weeks, have you been sad or depressed most of the time? |
40.0 | 151.3 | 0.45 (0.38–0.53) | 0.82 |
| 8 |
In the past few weeks, have you felt so sad or depressed in a way that felt unbearable, like you couldn’t stand it anymore? |
24.3 | 170.1 | 0.60 (0.52–0.68) | 0.83 |
| 9 |
In the past few weeks, have you felt that you or your family would be better off if you were dead? |
16.4 | 239.9 | 0.75 (0.67–0.82) | 0.86 |
| 10 |
In the past few weeks, have you though that your life was so bad that you didn’t want to live anymore? |
18.6 | 224.2 | 0.72 (0.64–0.80) | 0.86 |
| 11 |
In the past few weeks, have you wished you were dead? |
19.7 | 273.4 | 0.78 (0.72–0.85) | 0.90 |
| 12 | Are you here because you tried to hurt yourself? | 13.9 | 102.5 | 0.50 (0.39–0.59) | 0.72 |
| 13 | Have you ever tried to hurt yourself in the past? | 24.5 | 97.5 | 0.46 (0.36–0.55) | 0.75 |
| 14 |
Have you ever seriously considered killing yourself? |
19.3 | 181.0 | 0.65 (0.56–0.73) | 0.83 |
| 15 |
In the past week, have you been having thoughts about killing yourself? |
15.8 | 207.4 | 0.70 (0.62–0.78) | 0.83 |
| 16 | Have you ever tried to kill yourself? | 13.9 | 97.0 | 0.48 (0.38–0.58) | 0.72 |
| 17* | Do you have close friends or family that you can go to when you have a serious problem? |
93.1 | 19.6 | −0.06 (−0.09–0.02) | 0.57 |
Abbreviations: LR, likelihood ratio;
A negative kappa, while uncommon, suggests that this item agrees with the SIQ less than would be expected by chance. Bolded items are “trigger” items for a psychiatric consultation.
Table 3.
Predictive Abilities for the Best-Fitting Combinations of Screening Items
| Model | Screen Items | Sensitivity | Specificity | c- statistic |
PPV | NPV | Patients misclassified | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Psychiatric | Medical/ Surgical |
Psychiatric | Medical/ Surgical |
Psychiatric | Medical/ Surgical |
|||||
| 6 | 9,10,11,14,15,16 | 98.0 (92.8–99.7) |
83.6 (79.7–87.0) |
0.91 | 68.0 (59.0–76.2) |
29.5 (16.8–45.2) |
98.3 (90.8–100.0) |
99.7 (98.2–100.0) |
1 | 1 |
| 5 | 9,10,11,15,16 | 98.0 (92.8–99.7) |
85.9 (82.2–89.1) |
0.92 | 69.7 (60.6–77.8) |
35.1 (20.2–19.7) |
98.4 (91.2–100.0) |
99.7 (98.2–100.0) |
1 | 1 |
| 4 | 9,11,15,16 | 96.9 (91.3–99.4) |
87.6 (84.0–90.5) |
0.92 | 71.3 (62.1–79.3) |
39.4 (22.9–57.9) |
96.9 (89.3–99.6) |
99.7 (98.2–100.0) |
2 | 1 |
| 3 | 9,11,16 | 93.9 (87.1–97.7) |
89.2 (85.9–92.0) |
0.91 | 74.5 (65.1–82.5) |
40.6 (23.7–59.4) |
93.2 (84.9–97.8) |
99.7 (98.2–100.0) |
5 | 1 |
| 2 | 11,16 | 89.9 (82.0–95.0) |
90.6 (87.4–93.2) |
0.90 | 76.2 (66.7–84.1) |
40.7 (22.4–61.2) |
91.1 (82.6–96.4) |
99.1 (97.3–99.8) |
7 | 3 |
| 1 | 16 | 49.0 (38.7–59.3) |
94.1 (91.5–96.2) |
0.72 | 73.7 (60.3–84.5) |
37.5 (15.2–64.6) |
65.9 (56.8–74.2) |
97.6 (95.2–98.9) |
42 | 8 |
All values shown are % (95% confidence interval) except for c-statistic which is equivalent to the area under the curve.
While the 6- and 5-question models had a higher sensitivity, model 4 showed a comparable NPV and a 3-point improvement in PPV from the 5-question model, resulting in fewer false- positives. Additionally, model 4 correctly classified all but one SIQ-positive patient with medical/surgical complaints. Therefore, we chose model 4 as the final Ask Suicide-Screening Questions (ASQ) instrument (eTable 1). The selection of the best-fitting models was based on both clinical and statistical significance.
The performance of the ASQ in detecting elevated suicidal risk (Table 4), consists of responses to the combination of candidate question 9 (current thoughts of being better off dead), question 11 (current wish to die), question 15 (current suicidal ideation), and question 16 (past suicide attempt). The sensitivity and specificity of having one or more positive responses on the ASQ in identifying either patients with medical/surgical or psychiatric complaints at elevated suicidal risk were 96.9% (95%CI, 91.3%–99.4%) and 87.6% (95%CI, 84.0%–90.5%), respectively. Of the 311 patients with medical/surgical complaints who screened negative on the ASQ, only 1 (0.3%) screened positive on the SIQ (NPV, 99.7%; 95% CI, 98.2%–99.9%). The positive LR for patients with medical/surgical complaints was 15.2 (95% CI, 7.2–27.0), indicating that a positive screen on the ASQ was 15.2 times more likely to be seen in someone actually at suicidal risk than in someone not at risk. The negative LR was 0.08 (95% CI, 0.002–0.37), meaning that a negative 4-item ASQ was 0.08 times as likely to be seen in someone at suicidal risk than in someone not at risk. The corresponding NPV and LRs (positive and negative) in patients with psychiatric complaints were 96.9% (95%CI, 89.3%–99.6%), 2.8 (95% CI, 2.1–4.0), and 0.04 (95% CI, 0.004–0.15), respectively.
Table 4.
Performance of the 4-Item ASQ in Detecting Elevated Suicide Risk in Youths Presenting to the ED
| Elevated Suicide Risk | ||||||
|---|---|---|---|---|---|---|
| Total ED Sample (N=524) |
Presented to ED with Primary Psychiatric Concern (n=180) |
Presented to ED with Primary Medical Concern (n=344) |
||||
| ASQ Result | Present | Absent | Present | Absent | Present | Absent |
| Positive, No. (%) | 95 (64.2) | 53 (35.8) | 82 (71.3) | 33 (28.7) | 13 (39.4) | 20 (60.6) |
| Negative, No. (%) | 3 (0.8) | 373 (99.2) | 2 (3.1) | 63 (96.9) | 1 (0.3) | 310 (99.7) |
| Value (95% CI) | ||||||
| Sensitivity | 96.9 (91.3–99.4) | 97.6 (91.7–99.7) | 92.9 (66.1–99.8) | |||
| Specificity | 87.6 (84.0–90.5) | 65.6 (55.2–75.0) | 93.9 (90.8–96.3) | |||
| Positive predictive value | …a | 71.3 (62.1–79.4) | 39.4 (22.9–57.9) | |||
| Negative predictive value | …a | 96.9 (89.3–99.6) | 99.7 (98.2–99.9) | |||
| LR+ | 7.8 (5.7–10.5) | 2.8 (2.1–4.0) | 15.2 (7.2–27.0) | |||
| LR− | 0.04 (0.01–0.10) | 0.04 (0.004–0.15) | 0.08 (0.002–0.37) | |||
| c-statistic | 0.92 | 0.83 | 0.93 | |||
Abbreviations: ASQ, Ask Suicide-Screening Questions; ED, emergency department; CI, confidence interval; LR+, likelihood ratio positive; LR−, likelihood ratio negative
Values are not given for the total sample because the prevalence of suicide risk differs in psychiatric and medical patients.
We examined the performance of the 4-item ASQ in subgroups defined by age, gender, and race (eTable 2). There were no statistical differences in the sensitivity, specificity, PPV, and NPV of the ASQ results in males and females and in younger and older participants. However, the sensitivity of the ASQ was significantly lower in African American participants compared with White participants and participants of other races (P=0.02).
Comment
The ED is a viable medical setting for implementing routine suicide screening among youth. With the longer SIQ as the criterion standard, our four-question screening instrument, the ASQ, accurately assesses risk of suicide in young ED patients with medical/surgical or psychiatric chief complaints.
The ASQ appears to have good content validity. The four questions together assess major facets of established suicide risk factors, including three questions that target current suicidal ideation in a manner in which youth with medical concerns in particular, can relate: current thoughts of being better off dead, current wish to die, and current suicidal ideation; a fourth question inquires about the most critical risk factor for future suicidal behavior, a past history of suicide attempt. Positive responses to one or more of these four questions identified 97% of the youth at risk of suicide, as assessed by the SIQ, a much longer criterion standard instrument typically administered by mental health clinicians. In addition, the high specificity demonstrated by the 4 questions, the ability to correctly identify young patients who are currently not at elevated risk for suicide (87.6%), is of paramount importance in not overburdening a busy ED setting with limited mental health resources. Given the consequences of failing to detect an increased risk of suicide, the high NPV (99.7%), or the probability that the young person who screened negative is not at elevated risk for suicide, is also an important attribute of an instrument utilized by ED clinicians.
Overall, 19% (98 of the 524) of the ED patients screened positive for risk of suicide; the majority of whom were patients with psychiatric complaints. Elevated risk of suicide was detected in 4.1% (14 of the 344) of the ED patients with medical/surgical complaints. Had it not been for the screening, risk of suicide in these 14 patients would have perhaps been undetected, as their chief complaints were medical in nature, (e.g. ankle injury, abdominal pain, headaches). This is a relatively small number of patients in terms of overburdening a busy ED; yet, a notable number of youth that could be identified with a screening instrument that takes less than 2 minutes to administer. These data are consistent with King et al. (2009), who examined suicide screening in non-psychiatric patients in the ED with a much longer battery of assessments, and concluded that risk identification may be a critical step in reducing the youth suicide rate.31
Limitations
These findings are subject to the following limitations. Participating EDs were all in urban, tertiary care teaching hospitals and may not generalize to other ED settings. We used convenience sampling, which could have introduced bias into our findings, and did not administer the ASQ to a validation cohort. There may also have been a fatigue effect by asking the participants repeatedly about suicidal thoughts; however, this did not arise as a concern in study evaluation interviews. In addition, although the criterion standard SIQ has sound psychometric properties, including good validity and reliability, it primarily identifies youth at risk for clinically significant suicidal ideation, and may not necessarily be predictive of suicidal behavior. Ideally, our protocol would have included a longitudinal follow-up component to determine if patients that screened positive for risk of suicide were more likely than others to attempt suicide after ED discharge.
Future Directions
Future studies measuring the impact of suicide screening in pediatric EDs on such critical outcomes as linkage with mental health services and future suicidal behavior are warranted. Potential racial differences in sensitivity of suicide screening instruments should also be examined. In addition, evaluating the acceptance of such screening instruments by clinicians and the costs associated with implementing universal suicide screening in EDs would inform implementation strategies.
Conclusions
Youth presenting to pediatric EDs can be rapidly assessed for risk of suicide with a brief 4-question screening instrument, the ASQ, which demonstrates high sensitivity, specificity and negative predictive value. The ASQ may be an appropriate tool for implementation in this venue as part of the JC11 and the AAP12 recommendations.
Acknowledgments
The authors thank David Jobes (Catholic University of America); Abigail Bosk, Deborah Snyder, Rebecca Prengler, Amy Goldstein, Erica Ludi, Sarah Western (National Institutes of Mental Health); Janet Heekin (National Institutes of Health); Arielle Sheftall, Sandra M. McBee-Strayer, Rachel Jones, Kristen Mendoza (Nationwide Children’s Hospital); Eliza Hutchinson (Children’s Hospital Boston); Angelica Kloos, Khristine Heflin, Amanda Lewis, Marc Dalton (Children’s National Medical Center); the emergency department social workers, nurses and physicians at Children’s National Medical Center, Nationwide Children’s Hospital and Children’s Hospital Boston; as well as the patients and their families for their participation.
Funding /Support
The research in this article was supported by the Intramural Research Program of the National Institutes of Health and the National Institute of Mental Health. Dr. Bridge was supported by institutional research funds from the Research Institute at Nationwide Children’s Hospital and NIMH grant K01 MH-69948. Dr. Wharff and Ms. Ginnis were supported by institutional research funds from the Program for Patient Safety and Quality at Children’s Hospital Boston.
Dr. Bridge reports that he has received honoraria from Best Practice Project Management for participation in a suicidality consensus conference that was supported by independent education or other unrestricted grant support from the following companies: AstraZeneca, Dainippon Sumitomo, Eli Lilly, Forest Research Institute, Janssen, Division of Ortho-McNeil-Janssen Pharmaceuticals, Inc, administered by Ortho-McNeil-Janssen Scientific Affairs, LLC, Roche Pharmaceuticals, Sanofi-Aventis, Schering-Plough, Sepracor, and United BioSource.
Footnotes
Financial Disclosures
The other authors report no conflicts of interest.
The opinions expressed in the article are the views of the authors and do not reflect the views of the Department of Health and Human Services or the United States government.
Author Contributions
Drs. Horowitz, Bridge and Klima had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Horowitz, Bridge, Ballard, Rosenstein, Pao
Acquisition of data: Horowitz, Bridge, Teach, Ballard, Wharff, Ginnis, Cannon, Joshi
Analysis and interpretation of data: Horowitz, Bridge, Teach, Ballard, Klima, Rosenstein, Wharff, Ginnis, Cannon, Joshi, Pao
Drafting of the manuscript: Horowitz, Bridge, Teach, Klima, Cannon, Pao
Critical revision of the manuscript for important intellectual content: Horowitz, Bridge, Teach, Ballard, Rosenstein, Wharff, Ginnis, Joshi, Pao
Statistical analysis: Bridge, Klima
Obtained funding: Bridge, Wharff, Ginnis, Pao
Administrative, technical, or material support: Horowitz, Bridge, Teach, Ballard, Joshi, Rosenstein, Pao
Study supervision: Horowitz, Bridge, Teach, Pao
REFERENCES
- 1.Centers for Disease Control and Prevention. National Center for Injury Prevention and Control, Centers for Disease Control and Prevention (producer); 2008. [2011 Dec 6]. Web-based Injury Statistics Query and Reporting System (WISQARS) [Online] Available from: URL: www.cdc.gov/ncipc/wisqars. [Google Scholar]
- 2.Eaton DK, Kann L, Kinchen S, et al. Youth risk behavior surveillance - United States, 2009. MMWR: Surveillance Summaries. 2010;59(5):1–142. [PubMed] [Google Scholar]
- 3.Pfeffer CR, Lipkins R, Plutchik R, Mizruchi M. Normal children at risk for suicidal behavior: a two year follow-up study. J Am Acad Child Adolesc Psychiatry. 1988;27:34–41. doi: 10.1097/00004583-198801000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Tishler CL, Reiss NS, Rhodes AR. Suicidal behavior in children younger than twelve: a diagnostic challenge for emergency department personnel. Acad Emerg Med. 2007;14(9):810–818. doi: 10.1197/j.aem.2007.05.014. [DOI] [PubMed] [Google Scholar]
- 5.McIntire MS, Angle CR, Schlicht ML. Suicide and self poisoning pediatrics. Advances in Pediatrics. 1977;24:291–309. [PubMed] [Google Scholar]
- 6.US Public Health Service. National Strategy for Suicide Prevention: Goals and Objectives for Action. Rockville, Md: US Department of Health and Human Services; 2001. [PubMed] [Google Scholar]
- 7.Luoma JB, Martin CE, Pearson JL. Contact with mental health and primary care providers before suicide: a review of the evidence. Am J Psychiatry. 2002 Jun;159(6):909–916. doi: 10.1176/appi.ajp.159.6.909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gairin I, House A, Owens D. Attendance at the accident and emergency department in the year before suicide: retrospective study. Br J Psychiatry. 2003;183:28–33. doi: 10.1192/bjp.183.1.28. [DOI] [PubMed] [Google Scholar]
- 9.Wintersteen MB. Standardized screening for suicidal adolescents in primary care. Pediatrics. 2010;125(5):938–944. doi: 10.1542/peds.2009-2458. [DOI] [PubMed] [Google Scholar]
- 10.Pan YJ, Lee MB, Chiang HC, Liao SC. The recognition of diagnosable psychiatric disorders in suicide cases' last medical contacts. Gen Hosp Psychiatry. 2009;31:181–184. doi: 10.1016/j.genhosppsych.2008.12.010. [DOI] [PubMed] [Google Scholar]
- 11.The Joint Commission. A follow-up report on preventing suicide: focus on medical/surgical units and the emergency department. Sentinel Event Alert. 2010:1–4. [PubMed] [Google Scholar]
- 12.Dolan MA, Fein JA The Committee on Pediatric Emergency Medicine. Pediatric and adolescent mental health emergencies in the emergency medical services system. Pediatrics. 2011 May;127(5):e1356–e1366. doi: 10.1542/peds.2011-0522. [DOI] [PubMed] [Google Scholar]
- 13.Horowitz L, Ballard E, Teach SJ, et al. Feasibility of screening patients with non-psychiatric complaints for suicide risk in a pediatric emergency department: a good time to talk? Pediatr Emerg Care. 2010;26(11):787–792. doi: 10.1097/PEC.0b013e3181fa8568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McKay MP, Vaca FE, Field C, et al. Public health in the emergency department: overcoming barriers to implementation and dissemination. Acad Emerg Med. 2009;16(11):1132–1137. doi: 10.1111/j.1553-2712.2009.00547.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grupp-Phelan J, Wade TJ, Pickup T, et al. Mental health problems in children and caregivers in the emergency department setting. J Dev Behav Pediatr. 2007 Feb;28(1):16–21. doi: 10.1097/dbp.0b013e31802d0bb2. [DOI] [PubMed] [Google Scholar]
- 16.Olfson M, Marcus SC, Bridge JA. Emergency treatment of deliberate self-harm. Arch Gen Psychiatry. 2011 Sep 5; doi: 10.1001/archgenpsychiatry.2011.108. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 17.Larkin GL, Beautrais AL, Spirito A, et al. Mental health and emergency medicine: A research agenda. Academic Emergency Medicine. 2009;16(11):1110–1119. doi: 10.1111/j.1553-2712.2009.00545.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Habis A, Tall L, Smith J, Guenther E. Pediatric emergency medicine physicians' current practices and beliefs regarding mental health screening. Pediatr Emerg Care. 2007;23(6):387–393. doi: 10.1097/01.pec.0000278401.37697.79. [DOI] [PubMed] [Google Scholar]
- 19.Horowitz LM, Ballard ED, Pao M. Suicide screening in schools, primary care and emergency departments. Current Opinion in Pediatrics. 2009;21:620–627. doi: 10.1097/MOP.0b013e3283307a89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Horowitz LM, Wang PS, Koocher GP, et al. Detecting suicide risk in a pediatric emergency department: development of a brief screening tool. Pediatrics. 2001 May;107(5):1133–1137. doi: 10.1542/peds.107.5.1133. [DOI] [PubMed] [Google Scholar]
- 21.Folse VN, Hahn RL. Suicide risk screening in an emergency department: engaging staff nurses in continued testing of a brief instrument. Clin Nurs Res. 2009;18(3):253–271. doi: 10.1177/1054773809335296. [DOI] [PubMed] [Google Scholar]
- 22.Garcia R. Evaluation of suicide risk in children: psychometric properties of the Spanish version of the Risk of Suicide Questionnaire (RSQ) Actas Esp Psiquiatr. 2005;33(5):292–297. [PubMed] [Google Scholar]
- 23.Wuerz RC, Travers D, Gilboy N, et al. Implementation and refinement of the emergency severity index. Acad Emerg Med. 2001;8(2):170–176. doi: 10.1111/j.1553-2712.2001.tb01283.x. [DOI] [PubMed] [Google Scholar]
- 24.Reynolds W. Suicidal Ideation Questionnaire. Odessa, FL: Psychological Assessment Resources; 1987. [Google Scholar]
- 25.Keane E, Dick R, Bechtold D, Manson S. Predictive and concurrent validity of the Suicidal Ideation Questionnaire among American Indian adolescents. J Abnormal Child Psychology. 1996;35:1183–1192. doi: 10.1007/BF01664737. [DOI] [PubMed] [Google Scholar]
- 26.Fleiss J. Statistical Methods for Rates and Proportions. New York, NY: John Wiley; 1981. [Google Scholar]
- 27.SAS Institute Inc. SAS/STAT® 9.2 User’s Guide. Cary, NC: SAS Institute Inc; 2008. [Google Scholar]
- 28.Gould MS, Greenberg T, Velting DM, Shaffer D. Youth suicide risk and preventive interventions: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 2003;42:386–405. doi: 10.1097/01.CHI.0000046821.95464.CF. [DOI] [PubMed] [Google Scholar]
- 29.Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982;143(1):29–36. doi: 10.1148/radiology.143.1.7063747. [DOI] [PubMed] [Google Scholar]
- 30.Hanley JA, McNeil BJ. A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology. 1983;148(3):839–843. doi: 10.1148/radiology.148.3.6878708. [DOI] [PubMed] [Google Scholar]
- 31.Bergstralh E. Division of Biostatistics, Mayo Clinic. Locally written SAS macros. 2008 Available at: http://www.mayo.edu/hsr/sasmac.html. [Google Scholar]
- 32.King CA, O’Mara RM, Hayward CN, et al. Adolescent suicide risk screening in the emergency department. Academic Emergency Medicine. 2009;16:1234–1241. doi: 10.1111/j.1553-2712.2009.00500.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


