On the basis of >40 000 parent reports, we present normative data for young children’s developmental milestones and compare to CDC guidelines.
Abstract
Video Abstract
BACKGROUND AND OBJECTIVES:
Pediatric surveillance of young children depends on providers’ assessment of developmental milestones, yet normative data are sparse. Our objectives were to develop new norms for common milestones to aid in clinical interpretation of milestone attainment.
METHODS:
We analyzed responses to the developmental screening form of the Survey of Well-being of Young Children from 41 465 screens across 3 states. Associations between developmental status and a range of child characteristics were analyzed, and norms for individual questions were compared to guidelines regarding attainment of critical milestones from the Centers for Disease Control and Prevention (CDC).
RESULTS:
A contemporary resource of normative data for developmental milestone attainment was established. Lower developmental status was associated with child age in the presence of positive behavioral screening scores (P < .01), social determinants of health (P < .01), Medicaid (P < .01), male sex (P < .01), and child race (P < .01). Comparisons between Survey of Well-being of Young Children developmental questions and CDC guidelines reveal that a high percentage of children are reported to pass milestones by the age at which the CDC states that “most children pass” and that an even higher percentage of children are reported to pass milestones by the age at which the CDC states that parents should “act early.” An interactive data visualization tool that can assist clinicians in real-time developmental screening and surveillance interpretation is also provided.
CONCLUSIONS:
Detailed normative data on individual developmental milestones can help clinicians guide caregivers’ expectations for milestone attainment, thereby offering greater specificity to CDC guidelines.
What’s Known on This Subject:
Developmental milestones are commonly assessed to support pediatric surveillance and as part of developmental screening. However, normative data for individual milestones are sparse, and existing guidelines lack specificity.
What This Study Adds:
Early development varies across a range of child factors. A high proportion of children pass milestones by the ages at which Centers for Disease Control and Prevention guidelines indicate that parents should “act early.” Normative data can help clinicians set realistic expectations for milestone attainment.
Evaluating young children’s mastery of selected developmental milestones is a standard element of pediatric care.1–4 Organizations such as the Centers for Disease Control and Prevention (CDC) and Bright Futures, a health promotion initiative led by the American Academy of Pediatrics, publish guidelines that include lists of individual milestones and the ages at which most children are expected to pass. The CDC guidance goes a step further by suggesting when parents should “act early by talking to their physician” if particular milestones have not been reached.2
A range of evidence supports assessment of developmental milestones. For example, developmental milestones are commonly incorporated into pediatric screening questionnaires, which are widely recommended on the basis of evidence supporting their accuracy in detecting developmental delays.4 Evidence also supports the validity of individual milestones as markers of developmental status. Consistent with recent evidence that early childhood is a critical developmental period for long-term health and productivity,5–7 several large cohort studies conducted in the United Kingdom, Denmark, and Finland report small-to-medium correlations between the age at which children attain specific developmental milestones and a range of adult outcomes. For example, evidence suggests that parents’ reports of early language skills, such as forming sentences by 2 years, are associated with adult IQ.8,9 Parents’ reports of earlier standing, walking, and talking have each been associated with greater educational attainment in adulthood,10 and age of walking has been linked to sports participation.11 Although correlations are far too small to be diagnostic, research supports the overall validity of monitoring individual developmental milestones in early childhood.
Unfortunately, guidelines for the assessment of developmental milestones lack strong normative data. For example, both Bright Futures and the CDC report ages at which “most children pass” specific developmental milestones; however, they do not define their terminology (eg, Does “most” mean 50% or 99%?) and do not cite sources of normative data used to create their guidelines. Both omissions are likely accounted for by a gap in the published literature. Despite growing international interest in research on developmental status,12 as exemplified by World Health Organization initiatives to assess children’s developmental status across the globe,13,14 few US studies of the validity of screening instruments reveal normative data by question. Notable exceptions include the Denver Developmental Screening Questionnaire, Second Edition15 and the developmental screening component of the Survey of Well-being of Young Children (SWYC) (known elsewhere as the “SWYC Milestones”).16,17
Our goal for this article is to address this evidence gap. Based on analyses of >40 000 screens across 3 US states, our aims for this article are to (1) report new age-based norms for 45 developmental milestones, (2) analyze associations with child-level variables, and (3) compare results to CDC recommendations, thereby helping to operationalize definitions of when most children pass and when parents should act early.
Methods
Participants
Participants included parents of young children who completed a developmental screening questionnaire as part of routine pediatric care in the states of Rhode Island, Minnesota, and Massachusetts. In the Rhode Island sample, de-identified question-level data were drawn from the central server of the Child Health and Development Interactive System, an electronic system available for a licensing fee to clinicians that presents and scores screening questionnaires. Data were available from 13 076 patients who completed 22 438 independent screens at different ages at 33 pediatric practices that participated in a screening initiative between July 24, 2014, and December 31, 2016. For the Minnesota sample, de-identified question-level data were extracted from the electronic medical record system at Essentia Health, which conducted screening between March 1, 2015, and March 15, 2017. Data were available from 8985 patients who completed 17 667 screens.
The Massachusetts sample was drawn from studies used to standardize and evaluate the accuracy of the SWYC’s developmental screen. These studies included original validation samples17 as well as a new sample from an evaluation of the comparative accuracy of several developmental-behavioral screening instruments supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development. For all Massachusetts samples, parents were approached in pediatric waiting rooms by research assistants who described the study. Parents who consented were asked to complete a packet of questionnaires that included the SWYC. Data were available from 1459 patients and 1459 screens.
Measures
Analyses were focused on the SWYC Milestones, which includes a series of 54 questions about developmental milestones, 10 of which are administered at each age of the pediatric periodicity schedule up to 5 years of age.17 Initial research suggests that the validity of the SWYC’s developmental screen is comparable with that of other evidence-based screening instruments in English17 and in Spanish.18 Because developmental screens were available in our data set for children beginning at 9 months of age, we focused on the 45 SWYC questions appropriate for children in this age range. In addition, the SWYC includes behavioral screeners (the Baby Pediatric Symptom Checklist [BPSC]19 and the Preschool Pediatric Symptom Checklist [PPSC]20) as well as a series of questions about social determinants of health (SDoH), which include parent depression, hunger, child exposure to tobacco and substance abuse, and family discord.21
Analyses
To create new age-based norms for developmental milestones, we used item response theory (IRT) and Mplus software version 8.1 to estimate a graded response model, as described in the original article on the SWYC’s developmental screen.17 These analyses were conducted on the combined sample from Rhode Island, Minnesota, and Massachusetts, but children born prematurely (<37 weeks’ gestation) were excluded. Before combining samples, we conducted tests of differential item functioning (DIF)22,23 to determine if milestones functioned in an equivalent way across the Rhode Island, Minnesota, and Massachusetts samples. The IRT-based method we use to calculate developmental quotient (DQ) is flexible in that it uses all available information but does not require complete responses. Thus, participants were included even if not all milestone questions were completed. For the full sample (including those born prematurely), IRT-model parameters were then used to estimate DQ, which is defined as the estimate of child age based on all available developmental milestones (ie, developmental age) divided by chronological age. Additional details are provided in the Supplemental Information.
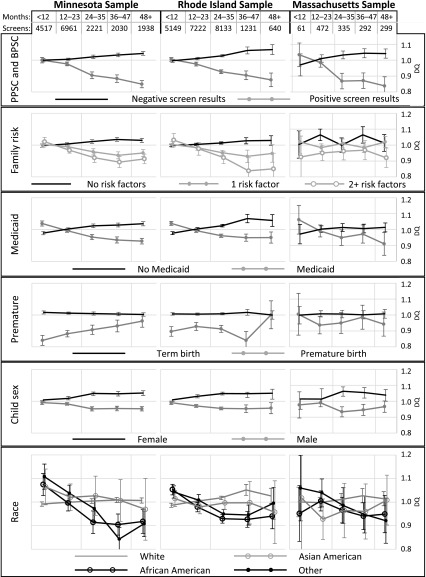
Next, regression analyses were used to test whether DQ was associated with available demographic variables (race and/or ethnicity and Medicaid status), with positive scores on the BPSC and PPSC, and with a positive sum score of SWYC family risk variables (hereafter, cumulative SDoH). Regression models included only complete cases, adjusted for repeated measures by child, and interaction terms for each independent variable and child age in years. DQ standardized by age and state as well as 95% confidence intervals are displayed in Figure 1.
FIGURE 1.
Moderators of developmental status by child age in months. DQ = age estimate on the basis of developmental milestones ÷ chronological age (adjusted for state). Although for clinical purposes, chronological age is typically adjusted for prematurity, for the purposes of this study, it was defined as the date of screening minus the date of birth. Therefore, DQ < 1 suggests milestone attainment below expectations for age; DQ = 1 suggests milestone attainment as expected for age; and DQ >1 indicates milestone attainment exceeding expectations for age.
Finally, specific questions from the SWYC’s developmental screen were compared with questions recommended by the CDC. For questions with constructs that overlapped with CDC milestones, we estimated the proportion of children expected to pass each SWYC developmental question at the ages at which the CDC states that most children achieve each task and the ages at which the CDC states that parents should act early by talking to their pediatrician if children do not pass.
Results
Available demographic variables are summarized in Table 1, which also includes national estimates from the 2010 US Census. Analyses to update age-based norms for questions on the SWYC’s developmental screen were conducted on samples from Rhode Island, Minnesota, and Massachusetts. Although DIF between states was detected, the magnitude of such differences was small, and estimates of DQ that were based on state-specific parameters were nearly identical to estimates that were based on full-sample parameters. Therefore, we concluded that although small differences in item parameters were present, DIF was clinically nonsignificant with respect to DQs and screening scores (see the Supplemental Information for further details). Therefore, summary parameters derived from the combined samples were used in additional analyses, and in all primary analyses, a common set of population parameters was used to estimate both norms and DQ.
TABLE 1.
Sample Characteristics
| Sample | 2010 US Census Estimate, % | |||
|---|---|---|---|---|
| Rhode Island, % | Minnesota, % | Massachusetts, % | ||
| Race and/or ethnicity | ||||
| White | 63.5 | 91.1 | 73.9 | 72.4 |
| African American | 8.5 | 3.4 | 13.2 | 12.6 |
| Asian American | 4.5 | 0.9 | 6.4 | 4.8 |
| Native Hawaiian or Pacific Islander | 0.1 | 0.3 | 0.1 | 0.2 |
| American Indian or Alaskan native | 0.6 | 1.8 | 0.0 | 0.9 |
| Unknown or other | 22.9 | 2.5 | 6.4 | 9.1 |
| Hispanic | 17.4 | 1.5 | 17.7 | 16.3 |
| Child sex: female | 49.0 | 48.0 | 47.6 | 48.9 |
| Medicaid status | 41.8 | 36.7 | 20.3 | 15.9 |
In the Massachusetts sample, child race and/or ethnicity was assessed by parent report. In the Minnesota sample, child race and/or ethnicity was derived from the electronic health record. In the Rhode Island sample, child race and/or ethnicity was not available, so parent race and/or ethnicity was assessed from birth records.
Regression analyses revealed that across states, linear trends of DQ by child age differed with respect to several variables (see Supplemental Table 4). Figure 1 depicts DQ for each year of child age (based on regression models detailed in Supplemental Table 5). Specifically, older age was associated with lower DQ in the presence of positive behavioral screening scores (P < .01 for MN, RI, and MA), cumulative SDoH (P < .01 for MN and RI), Medicaid (P < .01 for MN and RI), male sex (P < .01 for MN and RI), and African American or “other” race (P < .01 for MN and RI). However, results suggest that some variables are associated with higher developmental status for children younger than 12 months, namely Medicaid (P < .01 for MN and RI) and African American or “other” race (P < .05 for MN and RI). Premature birth revealed the opposite pattern, with lower DQ for children younger than 12 months (P < .01 for MN and RI; P < .05 in MA) and increasing trends thereafter (P < .01 in MN).
We identified 31 CDC milestones used to assess behaviors similar to those assessed by 26 of the 45 questions from the SWYC’s developmental screen included in this study. In Table 2, we report comparisons for the CDC act early recommendation, and in Table 3, we report CDC guidelines for most children. Both Tables 2 and 3 include norms for SWYC Milestones questions, calculated in 2 different ways: (1) by scoring the item as a pass if the parent reports that the child “somewhat” or “very much” exhibits the behavior described in the question and (2) by scoring the item as a pass only if the parent reports that the child “very much” exhibits the behavior described. Overall, a high percentage of children achieved these milestones by the age at which the CDC states that most children pass, and an even higher percentage of children achieved these milestones by the age at which the CDC states that parents should act early.
TABLE 2.
CDC Act Early Recommendations and SWYC Normative Data
| CDC Recommendation | Parents’ Report | |||
|---|---|---|---|---|
| Act Early if Child | By Age, mo | SWYC Milestones Question | Very Much, %a | Somewhat or Very Much, %a |
| Cognitive and communication milestones | ||||
| Does not play games involving back-and-forth play | 9 | Plays games such as “peek-a-boo” or “pat-a-cake” | 49 | 90 |
| Does not copy others | 12 | Copies sounds that you make | 65 | 97 |
| Does not say single words such as “mama” or “dada” | 12 | Calls you “mama” or “dada” or similar name | 66 | 91 |
| Does not have at least 6 words | 18 | Names at least 5 familiar objects such as a ball or milk | 82 | 97 |
| Does not use 2-word phrases (eg, “drink milk”) | 24 | Puts ≥2 words together such as “more water” or “go outside” | 93 | >99 |
| Speaks unclearly | 48 | Talks so other people can understand him or her most of the time | >99 | >99 |
| Cannot retell a favorite story | 48 | Tells you a story from a book or television | 98 | >99 |
| Cannot give first and last name | 60 | Says his or her first name when asked | >99 | >99 |
| Does not play a variety of games and activities | 60 | Follows simple rules when playing a board game or card game | 93 | >99 |
| Does not respond to own name | 9 | Looks when you call his or her name | 87 | >99 |
| Motor milestones | ||||
| Does not transfer toys from 1 hand to the other | 9 | Passes a toy from 1 hand to the other | 96 | >99 |
| Cannot walk | 18 | Walks across a room without help | >99 | >99 |
| Cannot jump in place | 48 | Jumps off the ground with 2 ft | >99 | >99 |
| Bangs 2 things together | 12 | Holds 2 objects and bangs them together | 98 | >99 |
| Walks alone | 18 | Walks across a room without help | >99 | >99 |
| May walk up steps and run | 18 | Runs | 85 | 97 |
| Begins to run | 24 | Runs | >99 | >99 |
| May walk up steps and run | 18 | Walks up the stairs with help | 82 | 96 |
| Walks up and down stairs holding on | 24 | Walks up the stairs with help | 98 | >99 |
| Kicks a ball | 24 | Kicks a ball | 89 | >99 |
| Makes or copies straight lines or circles | 24 | Draws lines | 58 | 92 |
| Climbs well | 36 | Climbs up a ladder at a playground | 96 | >99 |
| Copies a circle with pencil or crayon | 36 | Draws simple shapes such as a circle or a square | 48 | 94 |
Response options for SWYC Milestones included not yet, somewhat, and very much.
TABLE 3.
CDC Guidelines for Most Children and SWYC Normative Data
| CDC Recommendation | Parents’ Report | |||
|---|---|---|---|---|
| Most Children | By Age, mo | SWYC Milestones Question | Very Much, % | Somewhat or Very Much, % |
| Cognitive and communication milestones | ||||
| Babbles with expression and copies sounds he or she hears | 4 | Copies sounds that you make | 6 | 51 |
| Copies sounds and gestures of others | 9 | Copies sounds that you make | 44 | 93 |
| Responds to own name | 6 | Looks when you call his or her name | 63 | 97 |
| Plays “peek-a-boo” | 9 | Plays games like “peek-a-boo” or “pat-a-cake” | 49 | 90 |
| Plays games such as “peek-a-boo” and “pat-a-cake” | 12 | Plays games like “peek-a-boo” or “pat-a-cake” | 80 | 98 |
| Says “mama” and “dada” and exclamations such as “uh-oh!” | 12 | Calls you “mama” or “dada” or similar name | 66 | 91 |
| Follows simple directions such as “pick up the toy” | 12 | Follows directions such as “Come here” or “Give me the ball” | 41 | 94 |
| Follows simple instructions | 24 | Follows directions such as “Come here” or “Give me the ball” | >99 | >99 |
| Says several single words | 18 | Names at least 5 familiar objects- such as a ball or milk | 82 | 97 |
| Says sentences with 2–4 words | 24 | Puts ≥2 words together such as “more water” or “go outside” | 93 | >99 |
| Talks well enough for strangers to understand most of the time | 36 | Talks so other people can understand him or her most of the time | 90 | >99 |
| Starts to understand time | 48 | Uses words such as “yesterday” and “tomorrow” correctly | 79 | 98 |
| Tells stories | 48 | Tells you a story from a book or television | 98 | >99 |
| Plays board or card games | 48 | Follows simple rules when playing a board game or card game | 73 | 98 |
| Motor milestones | ||||
| May be able to roll over from tummy to back | 4 | Rolls over | 27 | 78 |
| Begins to pass things from 1 hand to the other | 6 | Passes a toy from 1 hand to the other | 75 | 97 |
| Can get into sitting position | 9 | Gets to a sitting position by himself or herself | 78 | 94 |
| Pulls to stand | 9 | Holds 2 objects and bangs them together | 59 | 84 |
| Bangs 2 things together | 12 | Holds 2 objects and bangs them together | 98 | >99 |
| Walks alone | 18 | Walks across a room without help | >99 | >99 |
| May walk up steps and run | 18 | Runs | 85 | 97 |
| Begins to run | 24 | Runs | >99 | >99 |
| May walk up steps and run | 18 | Walks up the stairs with help | 82 | 96 |
| Walks up and down the stairs holding onto the railing | 24 | Walks up the stairs with help | 98 | >99 |
| Kicks a ball | 24 | Kicks a ball | 89 | >99 |
| Makes or copies straight lines or circles | 24 | Draws lines | 58 | 92 |
| Climbs well | 36 | Climbs up a ladder at a playground | 96 | >99 |
| Copies a circle with pencil or crayon | 36 | Draws simple shapes such as a circle or a square | 48 | 94 |
Finally, age-based normative curves for all SWYC milestones are included in a Microsoft Excel file that accompanies this article (Supplemental Information; see Supplemental Fig 2). With this file, users can select an individual milestone question from the SWYC and inspect normative data presented as both item characteristic curves (which reflect the probability of each response at each age) and percentiles (consistent with the format adopted by the Denver Developmental Screening Questionnaire, Second Edition). In addition, users can inspect the degree to which expected values based on SWYC norms (eg, the expectation that 66% of parents will report that their child “calls you ‘mama’ or ‘dada’ or similar name” by 12 months) correspond to observed values at various ages in each sample (eg, the proportion of parents who actually report passing this milestone). Known as calibration, this correspondence is important for understanding the degree of variation that can be expected when milestones are used in practice with different populations. Overall, differences in the degree of calibration between milestones are notable, especially between those for younger and older children (see Supplemental Fig 3 for an example of an older milestone in which wider confidence intervals indicate more variability in milestone attainment). Note also that item characteristic curves are based on IRT parameters that correct for estimated developmental status; thus, some discrepancies between observed values are to be expected because developmental status varies across samples.
Discussion
We present normative data to facilitate interpretation of developmental milestones. Our sample is diverse and broadly representative, and tests of DIF suggest that questions regarding developmental milestones perform in a similar way across the 3 states included in our analyses. However, associations between developmental status and a range of child-level variables suggest that overall development is sensitive to the different constellations of social factors experienced by specific populations. Consistent with previous research, lower developmental status was associated with age among children with positive behavioral screen results,24–27 SDoH,28–30 and public health insurance.31 Similar patterns were identified for boys and for certain categories of race. Unexpectedly, results also suggest that some of these factors are associated with parent reports of better performance on developmental milestones before 12 months of age. A post hoc literature review revealed previous findings that associations between developmental delays and SDoH become apparent in the second year of life31,32 and that children from certain disadvantaged populations display advanced development during infancy.33–35 Previous researchers have hypothesized that specific cultural practices that are prevalent in these populations offer the most plausible explanation for the early attainment of certain developmental skills.36,37 For example, researchers have pointed to early motor stimulation common to some cultures as a cause of advanced gross motor development. This finding highlights the importance of a comprehensive approach to pediatric screening that does not solely rely on developmental questionnaires and that is also used to assess behavioral risk and SDoH starting at early ages.38
Regarding CDC milestones, parents in our 3 samples reported that a high percentage of children achieved developmental milestones by the age at which the CDC states that most children pass and that an even higher percentage of children achieved developmental milestones by the age at which the CDC states that parents should act early. Although only a subset of CDC milestones were assessed, it is notable that only 3 of the 13 motor milestones received an act early recommendation, all of which occurred at ages well after 90% of children pass. In contrast, 9 of 13 social, cognitive, and communication milestones received an act early recommendation, several of which occurred at ages well before 90% of children pass. These differences suggest that CDC guidelines are likely to be more sensitive to delays in the development of social, cognitive, and communication skills than to delays in motor development.
Results also highlight the degree to which responses to individual milestones are sensitive not only to parent beliefs about child development but also to how a passing response is defined. For example, including somewhat responses in our definition of a pass substantially increased the proportion of children who passed at any given age. In contrast, restricting passes to responses of very much (a more conservative threshold) decreased the proportion of children who passed. Although the CDC offers images and videos to help parents understand most milestones, it does not suggest a threshold for what constitutes a pass. In practice, thresholds are therefore likely to vary among providers, often with important consequences. Lower, more generous thresholds (eg, awarding a pass even if the child only somewhat exhibits the behavior) are likely to generate fewer false-positive results, but they are also likely to be less sensitive to actual developmental delays. In contrast, higher, more stringent thresholds (eg, only accepting very much as a pass) are likely to be more sensitive to developmental delays but will also generate more false-positive results.39
Likewise, how milestones are assessed likely influences results. Each CDC milestone is used to describe a particular behavior but does not include a specific question for parents. Although the CDC’s inclusion of images and videos suggests that observation is encouraged, no specific guidance is offered, for example, by asking parents to rate the degree to which their child can perform the skill depicted in the video.40 This lack of specificity may limit the impact of information disseminated by the CDC. The CDC’s campaign has been shown to increase parents’ reported knowledge of and engagement with child development,2,41,42 yet evidence suggests that parents are often unclear about how to act early,43 and effects on early detection have not been demonstrated. Greater specificity regarding how milestones should be assessed and what thresholds are appropriate to determine if a child passes (both of which depend on detailed normative data) may be an important ingredient (alongside broader consideration of when intervention is justified44) for improving the impact of CDC recommendations.
We note several limitations to our study. Both norms and our regression analyses of developmental status represent average population-level statistics from 3 US states. Implications for individual children requires clinical judgement, especially for populations that are substantially different with respect to SDoH from those described here. Whereas large sample sizes allow for estimates of mean values within narrow confidence intervals (defined by SEs), actual population variance (defined by SDs) is much larger. For example, whereas a statement like “healthy cheetahs are faster than humans” is valid at both the population and the individual level (all healthy cheetahs are faster than all humans), the same is not true for the association between child sex and development; that is, although the average age at which girls pass milestones appears to be younger than the average age for boys, this (of course) does not imply that all girls develop more rapidly than all boys. Furthermore, we urge caution in drawing causal inferences from our observational data, particularly regarding social factors (such as race and public insurance) that are multicausal and in which unmeasured confounders likely play a significant role.
Moreover, in our analyses, we do not directly evaluate the validity of CDC recommendations. Lacking a valid and measurable outcome, we are unable to estimate the sensitivity and specificity of CDC recommendations. Instead, our presentation of norms offers a more detailed perspective on the proportion of children who can be expected to pass specific milestones at different ages. Although these results do not provide explicit quantitative data on accuracy, they do provide important context for assessing developmental progress.
Finally, although the sample is large, results are limited to children who present for pediatric care in 3 US states and to the limited number of milestones that are assessed by using the SWYC’s developmental screen. Associations between developmental status and social factors suggest significant heterogeneity in child development, implying that population-level means are best conceptualized as guidelines rather than strict standards. We urge investigators who have access to large representative data sets that include other developmental assessment instruments (in particular, companies that own and market such assessment tools) to conduct analyses of DIF and to publish detailed normative data at the question level.
Conclusions
Given their important role in pediatric care for young children, we suggest that assessment of developmental milestones deserves greater attention. In particular, clinicians would benefit from guidelines that are accompanied by normative data to help interpret and act on surveillance of milestones, and developmental screening should include assessment of behavioral risk and SDoH to contextualize results. The data visualization tool developed from this analysis offers clinicians age-based normative data to facilitate interpretation of individual milestones, and the results of our regression analyses offer insights into how these norms are likely to differ across communities that vary on a range of relevant variables.
Acknowledgments
We acknowledge assistance in facilitating access to de-identified data from the Rhode Island Department of Health, the Child Health and Development Interactive System, and Essentia Health in Minnesota as well as support from all members of our research teams, most notably, Daryl Garfinkle. Finally, we thank the many pediatric providers whose commitment to ensuring children’s healthy development makes this research possible.
Glossary
- BPSC
Baby Pediatric Symptom Checklist
- CDC
Centers for Disease Control and Prevention
- DIF
differential item functioning
- DQ
developmental quotient
- IRT
item response theory
- PPSC
Preschool Pediatric Symptom Checklist
- SDoH
social determinants of health
- SWYC
Survey of Well-being of Young Children
Footnotes
Dr Sheldrick conceptualized the study, conducted data analyses, drafted the initial manuscript, and reviewed and revised the manuscript; Drs Schlichting and Ni conducted data analyses and also reviewed and revised the manuscript; Drs Berger, Clyne, Perrin, and Vivier critically reviewed the manuscript for important intellectual content and made substantive revisions; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
POTENTIAL CONFLICT OF INTEREST: Drs Sheldrick and Perrin are cocreators of the Survey of Well-being of Young Children, an instrument that was used to collect data for this study; the other authors have indicated they have no potential conflicts of interest to disclose.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R01 HD072778), the David and Lucille Packard Foundation, and the Hassenfeld Child Health Innovation Institute. Funded by the National Institutes of Health (NIH).
COMPANION PAPER: A companion to this paper can be found online at www.pediatrics.org/cgi/doi/10.1542/peds.2019-2936.
References
- 1.Hagan JF, Shaw JS, Duncan PM, eds. Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents, 4th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2017 [Google Scholar]
- 2.Daniel KL, Prue C, Taylor MK, Thomas J, Scales M. ‘Learn the signs. Act early’: a campaign to help every child reach his or her full potential. Public Health. 2009;123(suppl 1):e11–e16 [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. CDC’s developmental milestones. Available at: https://www.cdc.gov/ncbddd/actearly/milestones/index.html, Accessed August 24, 2018
- 4.Council on Children With Disabilities; Section on Developmental Behavioral Pediatrics; Bright Futures Steering Committee; Medical Home Initiatives for Children With Special Needs Project Advisory Committee . Identifying infants and young children with developmental disorders in the medical home: an algorithm for developmental surveillance and screening. Pediatrics. 2006;118(1):405–420 [DOI] [PubMed] [Google Scholar]
- 5.Campbell F, Conti G, Heckman JJ, et al. Early childhood investments substantially boost adult health. Science. 2014;343(6178):1478–1485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Heckman J, Pinto R, Savelyev P. Understanding the mechanisms through which an influential early childhood program boosted adult outcomes. Am Econ Rev. 2013;103(6):2052–2086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shonkoff JP, Garner AS; Committee on Psychosocial Aspects of Child and Family Health; Committee on Early Childhood, Adoption, and Dependent Care; Section on Developmental and Behavioral Pediatrics. The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129(1). Available at: www.pediatrics.org/cgi/content/full/129/1/e232 [DOI] [PubMed] [Google Scholar]
- 8.Flensborg-Madsen T, Mortensen EL. Associations of early developmental milestones with adult intelligence. Child Dev. 2018;89(2):638–648 [DOI] [PubMed] [Google Scholar]
- 9.Flensborg-Madsen T, Mortensen EL. Infant developmental milestones and adult intelligence: a 34-year follow-up. Early Hum Dev. 2015;91(7):393–400 [DOI] [PubMed] [Google Scholar]
- 10.Taanila A, Murray GK, Jokelainen J, Isohanni M, Rantakallio P. Infant developmental milestones: a 31-year follow-up. Dev Med Child Neurol. 2005;47(9):581–586 [PubMed] [Google Scholar]
- 11.Ridgway CL, Ong KK, Tammelin TH, et al. Infant motor development predicts sports participation at age 14 years: northern Finland birth cohort of 1966. PLoS One. 2009;4(8):e6837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ertem IO, Krishnamurthy V, Mulaudzi MC, et al. Similarities and differences in child development from birth to age 3 years by sex and across four countries: a cross-sectional, observational study. Lancet Glob Health. 2018;6(3):e279–e291 [DOI] [PubMed] [Google Scholar]
- 13.McCoy DC, Waldman M, Fink G; CREDI Field Team . Measuring early childhood development at a global scale: evidence from the Caregiver-Reported Early Development Instruments. Early Child Res Q. 2018;45:58–68 [Google Scholar]
- 14.McCoy DC, Sudfeld CR, Bellinger DC, et al. Development and validation of an early childhood development scale for use in low-resourced settings. Popul Health Metr. 2017;15(1):3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Frankenburg WK, Dodds J, Archer P, Shapiro H, Bresnick B. The Denver II: a major revision and restandardization of the Denver Developmental Screening Test. Pediatrics. 1992;89(1):91–97 [PubMed] [Google Scholar]
- 16.El-Behadli AF, Neger EN, Perrin EC, Sheldrick RC. Translations of developmental screening instruments: an evidence map of available research. J Dev Behav Pediatr. 2015;36(6):471–483 [DOI] [PubMed] [Google Scholar]
- 17.Sheldrick RC, Perrin EC. Evidence-based milestones for surveillance of cognitive, language, and motor development. Acad Pediatr. 2013;13(6):577–586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gerdes M, Garcia-Espana JF, Webb D, et al. Psychometric properties of two developmental screening instruments for Hispanic children in the Philadelphia region. Acad Pediatr. 2019;19(6):638–645 [DOI] [PubMed] [Google Scholar]
- 19.Sheldrick RC, Henson BS, Neger EN, et al. The baby pediatric symptom checklist: development and initial validation of a new social/emotional screening instrument for very young children. Acad Pediatr. 2013;13(1):72–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sheldrick RC, Henson BS, Merchant S, et al. The Preschool Pediatric Symptom Checklist (PPSC): development and initial validation of a new social/emotional screening instrument. Acad Pediatr. 2012;12(5):456–467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Perrin EC, Sheldrick RC, Visco Z, Mattern K The Survey of Well-Being of Young Children (SWYC) user’s manual. Available at: https://www.floatinghospital.org/The-Survey-of-Wellbeing-of-Young-Children/Manual-Training-Resources. Accessed October 21, 2019
- 22.Jones RN, Tommet D, Ramirez M, Jensen R, Teresi JA. Differential item functioning in Patient Reported Outcomes Measurement Information System (PROMIS) Physical Functioning short forms: analyses across ethnically diverse groups. Psychol Test Assess Model. 2016;58(2):371–402 [Google Scholar]
- 23.Edelen MO, Stucky BD, Chandra A. Quantifying ‘problematic’ DIF within an IRT framework: application to a cancer stigma index. Qual Life Res. 2015;24(1):95–103 [DOI] [PubMed] [Google Scholar]
- 24.Baker BL, McIntyre LL, Blacher J, et al. Pre-school children with and without developmental delay: behaviour problems and parenting stress over time. J Intellect Disabil Res. 2003;47(pt 4–5):217–230 [DOI] [PubMed] [Google Scholar]
- 25.Baker BL, Neece CL, Fenning RM, Crnic KA, Blacher J. Mental disorders in five-year-old children with or without developmental delay: focus on ADHD. J Clin Child Adolesc Psychol. 2010;39(4):492–505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Beitchman JH, Nair R, Clegg M, Ferguson B, Patel PG. Prevalence of psychiatric disorders in children with speech and language disorders. J Am Acad Child Psychiatry. 1986;25(4):528–535 [DOI] [PubMed] [Google Scholar]
- 27.Feldman MA, Hancock CL, Rielly N, Minnes P, Cairns C. Behavior problems in young children with or at risk for developmental delay. J Child Fam Stud. 2000;9(2):247–261 [Google Scholar]
- 28.Hooper SR, Burchinal MR, Roberts JE, Zeisel S, Neebe EC. Social and family risk factors for infant development at one year: an application of the cumulative risk model. J Appl Dev Psychol. 1998;19(1):85–96 [Google Scholar]
- 29.Sameroff AJ, Seifer R, Baldwin A, Baldwin C. Stability of intelligence from preschool to adolescence: the influence of social and family risk factors. Child Dev. 1993;64(1):80–97 [DOI] [PubMed] [Google Scholar]
- 30.Sameroff AJ, Seifer R, Barocas R, Zax M, Greenspan S. Intelligence quotient scores of 4-year-old children: social-environmental risk factors. Pediatrics. 1987;79(3):343–350 [PubMed] [Google Scholar]
- 31.Black MM, Hess CR, Berenson-Howard J. Toddlers from low-income families have below normal mental, motor, and behavior scores on the revised Bayley scales. J Appl Dev Psychol. 2001;21(6):655–666 [Google Scholar]
- 32.Hess CR, Papas MA, Black MM. Use of the Bayley Infant Neurodevelopmental Screener with an environmental risk group. J Pediatr Psychol. 2004;29(5):321–330 [DOI] [PubMed] [Google Scholar]
- 33.Kelly Y, Sacker A, Schoon I, Nazroo J. Ethnic differences in achievement of developmental milestones by 9 months of age: the Millennium Cohort Study. Dev Med Child Neurol. 2006;48(10):825–830 [DOI] [PubMed] [Google Scholar]
- 34.Findlay L, Kohen D, Miller A. Developmental milestones among Aboriginal children in Canada. Paediatr Child Health. 2014;19(5):241–246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lejarraga H, Pascucci MC, Krupitzky S, et al. Psychomotor development in Argentinean children aged 0-5 years. Paediatr Perinat Epidemiol. 2002;16(1):47–60 [DOI] [PubMed] [Google Scholar]
- 36.Golding J, Emmett P, Iles-Caven Y, Steer C, Lingam R. A review of environmental contributions to childhood motor skills. J Child Neurol. 2014;29(11):1531–1547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Venetsanou F, Kambas A. Environmental factors affecting preschoolers’ motor development. Early Child Educ J. 2010;37(4):319–327 [Google Scholar]
- 38.Committee on Psychosocial Aspects of Child and Family Health; Task Force on Mental Health . Policy statement–the future of pediatrics: mental health competencies for pediatric primary care. Pediatrics. 2009;124(1):410–421 [DOI] [PubMed] [Google Scholar]
- 39.Sheldrick RC, Benneyan JC, Kiss IG, et al. Thresholds and accuracy in screening tools for early detection of psychopathology. J Child Psychol Psychiatry. 2015;56(9):936–948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Marrus N, Glowinski AL, Jacob T, et al. Rapid video-referenced ratings of reciprocal social behavior in toddlers: a twin study. J Child Psychol Psychiatry. 2015;56(12):1338–1346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gadomski AM, Riley MR, Scribani M, Tallman N. Impact of “Learn the signs. Act early.” Materials on parental engagement and doctor interaction regarding child development. J Dev Behav Pediatr. 2018;39(9):693–700 [DOI] [PubMed] [Google Scholar]
- 42.Graybill E, Self-Brown S, Lai B, et al. Addressing disparities in parent education: examining the effects of learn the signs/act early parent education materials on parent outcomes. Early Child Educ J. 2016;44(1):31–38 [Google Scholar]
- 43.Raspa M, Levis DM, Kish-Doto J, et al. Examining parents’ experiences and information needs regarding early identification of developmental delays: qualitative research to inform a public health campaign. J Dev Behav Pediatr. 2015;36(8):575–585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sheldrick RC, Garfinkel D. Is a positive developmental-behavioral screening score sufficient to justify referral? A review of evidence and theory. Acad Pediatr. 2017;17(5):464–470 [DOI] [PMC free article] [PubMed] [Google Scholar]