This study found significant positive associations between neighborhood child poverty and PICU use when examining admissions to 1 large PICU.
Abstract
BACKGROUND:
Disparities in health service use have been described across a range of sociodemographic factors. Patterns of PICU use have not been thoroughly assessed.
METHODS:
This was a population-level, retrospective analysis of admissions to the Cincinnati Children’s Hospital Medical Center PICU between 2011 and 2016. Residential addresses of patients were geocoded and spatially joined to census tracts. Pediatric patients were eligible for inclusion if they resided within Hamilton County, Ohio. PICU admission and bed-day rates were calculated by using numerators of admissions and bed days, respectively, over a denominator of tract child population. Relationships between tract-level PICU use and child poverty were assessed by using Spearman’s ρ and analysis of variance. Analyses were event based; children admitted multiple times were counted as discrete admissions.
RESULTS:
There were 4071 included admissions involving 3129 unique children contributing a total of 12 297 PICU bed days. Child poverty was positively associated with PICU admission rates (r = 0.59; P < .001) and bed-day rates (r = 0.47; P < .001). When tracts were grouped into quintiles based on child poverty rates, the PICU bed-day rate ranged from 23.4 days per 1000 children in the lowest poverty quintile to 81.9 days in the highest poverty quintile (P < .001).
CONCLUSIONS:
The association between poverty and poor health outcomes includes pediatric intensive care use. This association exists for children who grow up in poverty and around poverty. Future efforts should characterize the interplay between patient- and neighborhood-level risk factors and explore neighborhood-level interventions to improve child health.
What’s Known on This Subject:
Poverty adversely affects health. The health impacts of socioeconomic status and poverty occur at the individual and community levels. Socioeconomic disparities in PICU use have not been as robustly assessed compared with other medical disciplines.
What This Study Adds:
Socioeconomic disparities extend to pediatric critical illness. Neighborhood poverty affects children’s need for intensive care. We argue that this association represents more than an aggregate of individual risk factors, and the interplay of individual and community demographics merits further investigation.
Poverty is linked to adverse health outcomes across multiple pediatric conditions.1–10 For the 13 million children currently growing up in poverty in the United States, the adverse exposures, heightened stress, and diminished access to health-promoting resources that accompany a lower socioeconomic status negatively affect health and development through their entire lifetimes.11–14 Socioeconomic disparities extend to pediatric critical illness. Although the relationships between poverty and critical illness have not been thoroughly explored, available evidence suggests that children from lower-income families and communities are more likely to be admitted to the PICU because of both acute and chronic illnesses,1,15 are more gravely ill at the time of admission,15,16 and are more likely to die before PICU or hospital discharge.17,18
We recently used the inpatient bed-day (IPBD) rate to calculate and evaluate the burden of acute childhood illnesses across neighborhoods in our region. We calculated the IPBD rate by dividing the number of days children from a specified neighborhood (defined as a census tract) spent in the hospital by the number of children living within that neighborhood. We found that census tracts with higher rates of child poverty had significantly higher IPBD rates across all causes and across a range of specific conditions managed by nearly every hospital-based pediatric subspecialty.19 In this investigation, we explored the burden of pediatric critical illness across neighborhoods in our region. To do this, we calculated the IPBD rate specific to the PICU setting, hypothesizing that there would be similarly strong associations between neighborhood-level child poverty and rates of PICU use.
Methods
Study Setting and Design
We identified all PICU admissions that occurred at Cincinnati Children’s Hospital Medical Center (CCHMC) between January 1, 2011, and December 31, 2016, using the electronic health record (EHR). CCHMC is a large quaternary pediatric care facility in Cincinnati, Ohio, that cares for >90% of children who require hospitalization from within Cincinnati and the surrounding Hamilton County.20 The general PICU is a 35-bed unit that admits children with general and subspecialty medical and surgical pediatric conditions. Critically ill cardiac patients are cared for in a separate cardiac ICU; newborns are cared for in a separate NICU. CCHMC is located in Hamilton County, Ohio, which includes 222 census tracts and ∼187 000 children. The overall poverty rate for the county is 16% with a child poverty rate of 24%. The county is 26% African American, 3% Latino, and 66% white.21
Residential addresses were extracted from the EHR for all children <18 years of age admitted to the PICU during the study period. Addresses were geocoded to census tracts by using custom, Health Insurance Portability and Accountability Act–compliant software on the basis of the 2015 Topologically Integrated Geographic Encoding and Referencing/Line address range files.22 We chose to include only in-county admissions given the predominance of CCHMC as the pediatric care provider in Hamilton County, which allowed us to capture and analyze virtually all of the county’s intensive care needs; including all PICU admissions at our quaternary referral center in this analysis would have confounded our results by failing to account for an unknown number of children receiving care at other centers. Therefore, children who resided outside Hamilton County, Ohio, were excluded. CCHMC also cares for a large number of international patients, many of whom relocate to temporary housing near the hospital for the duration of their hospital stay; for this reason, any patient who specified an international primary payer in the EHR was also excluded from the analysis even if they presently listed a local address. Analyses were event based, meaning children admitted multiple times were counted each time they contributed a discrete PICU admission. The study received approval from CCHMC’s institutional review board.
Measures
Our outcome measures were PICU admission and PICU bed-day rates, each measured at the level of the census tract. As described above, these measures were calculated by dividing the number of PICU admissions and bed days attributable to a specific census tract by the number of children living within the tract. Thus, we obtained a rate measured per 1000 children for each of Hamilton County’s 222 census tracts. These rate variables were measured both on a continuous scale and after tracts were aggregated into quintiles based on the degree of child poverty.
The child population, used as the denominator for our PICU admission and bed-day rate measures, was estimated by using the US Census Bureau’s 2011–2015 American Community Survey (ACS).23 We also used the child poverty measure from the ACS to characterize and aggregate Hamilton County census tracts. The child poverty rate is calculated in the ACS by dividing the number of children in a tract who live below the federal poverty level (defined in 2017 as an annual income of $25 094 for a family of 413) by the number of children in the tract whose poverty status is known. As in our previous work,19 children were divided into quintiles based on the child poverty rate of the census tract in which they resided. Quintiles were based on the number of children rather than number of census tracts (ie, ∼20% of the child population fell into each quintile). The quintiles were divided from the lowest to highest rates of child poverty as follows: 0% to 5% (Quintile 1), 5% to 10% (Quintile 2), 10% to 18% (Quintile 3), 18% to 31% (Quintile 4), and 31% to 87% (Quintile 5).
Statistical Analyses
We depicted relationships between each of our PICU use measures and neighborhood child poverty rates using scatter plots. To ease visual interpretation of plots, both outcome and child poverty rates were log10 transformed, and we calculated correlation coefficients between use measures and child poverty rates. We also assessed these relationships after categorization of tracts into quintiles using analysis of variance. Finally, we illustrated the geographic distributions of poverty and PICU use throughout the county with choropleth maps.
Results
During the study period, 4071 PICU admissions met criteria for study inclusion, representing 3129 unique children who spent a total of 12 297 days in a PICU bed. The median age at the time of PICU admission was 5.9 years, and female children accounted for 45.3% of the admissions. The sample was 48.4% African American, 44.1% white, and <0.5% Latino. Public insurance covered just less than two-thirds of the children admitted, and <0.5% of children were uninsured. Median PICU length of stay was 2.4 days across all admissions. Two of Hamilton County’s 222 census tracts did not experience any PICU admissions during the study period. We elected to exclude these tracts from the analysis because they also had a low total child population.
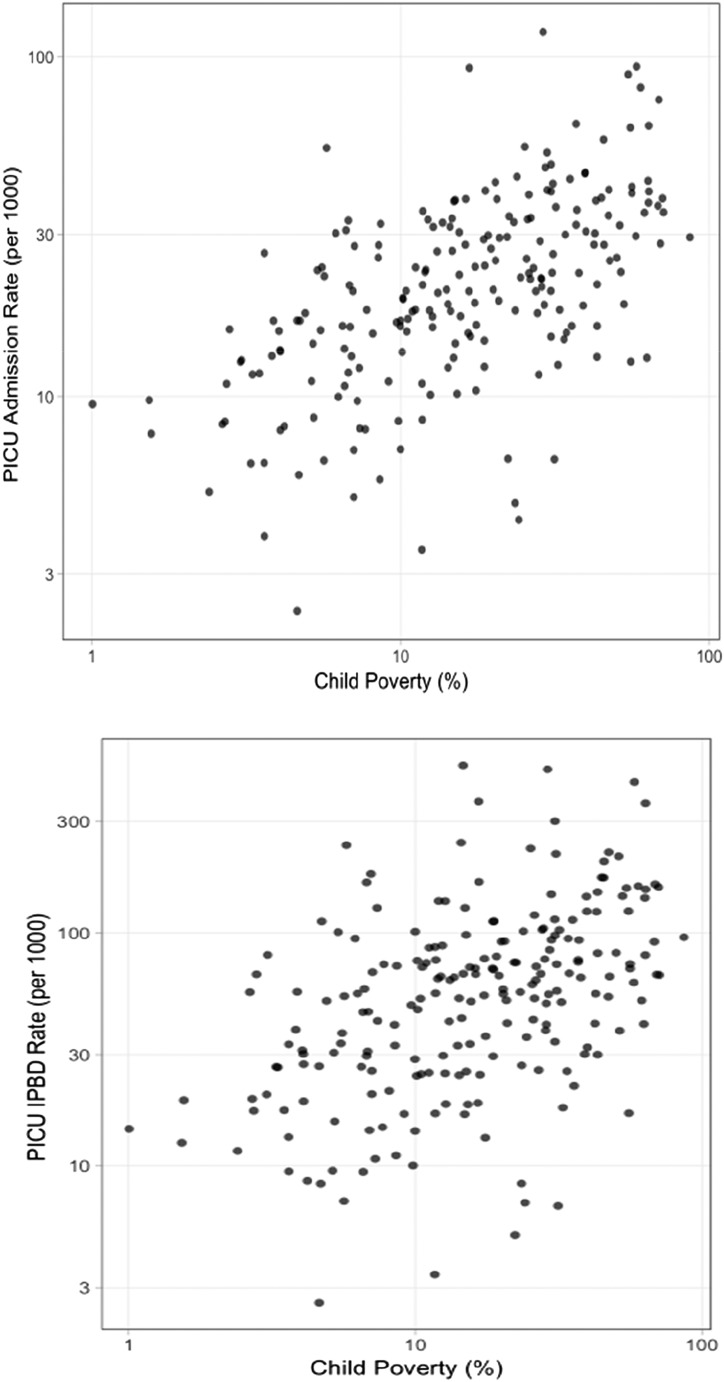
Figure 1 depicts the scatter plots for our log10-transformed outcome rates and child poverty rates. Figure 1A illustrates the census tract-level PICU admission rate on the y-axis and the child poverty rate on the x-axis. When these data were subject to correlation analysis, we found a significant positive relationship, as indicated by a Spearman correlation coefficient of 0.59 (P < .001). Figure 1B illustrates the similar relationship between census tract-level PICU bed-day rate and child poverty rate (r = 0.47; P < .001).
FIGURE 1.
A, PICU admission rate. B, PICU IPBD rate. Scatter plots demonstrate the relationships between PICU use measures and neighborhood poverty. Each point is an individual census tract. PICU admission rate and neighborhood poverty are strongly positively correlated (upper; r = 0.59; P < .001), as are PICU bed-day rate and neighborhood poverty (lower; r = 0.47; P < .001). Both axes are on the log10 scale.
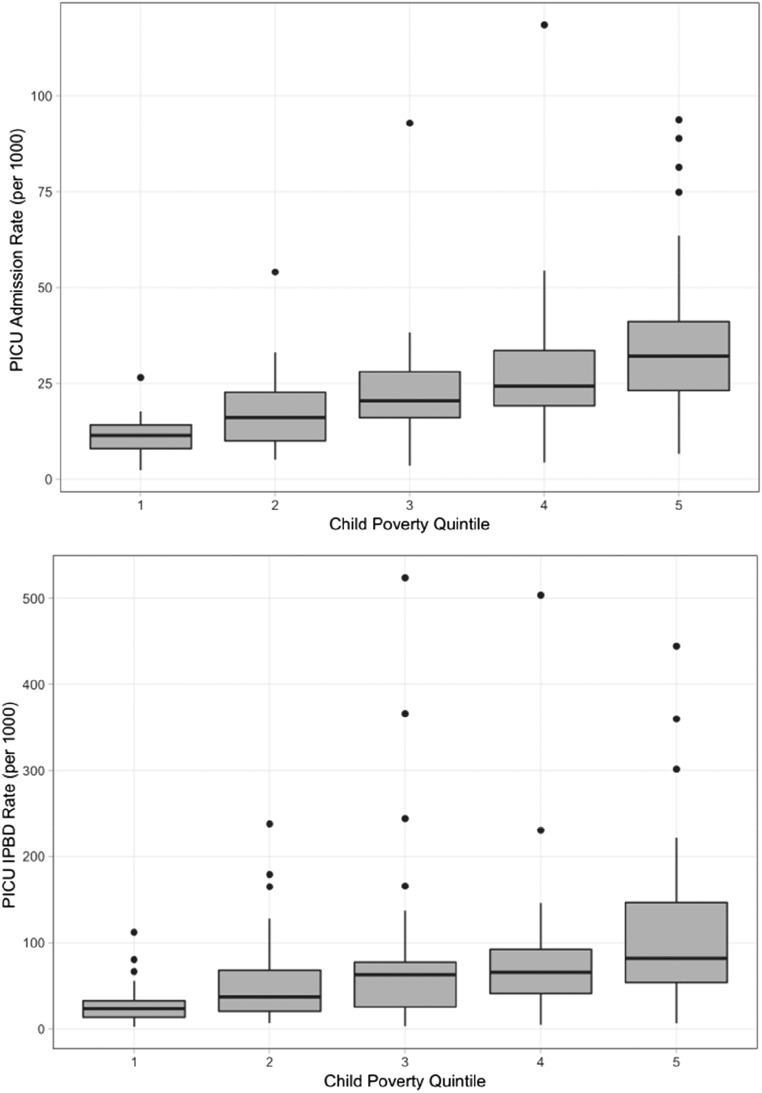
We next categorized census tracts according to child poverty rates, from lowest poverty (Quintile 1) to highest poverty (Quintile 5), as depicted in Fig 2. Although analysis of continuous data provided us with more power to illustrate the correlation between PICU use and neighborhood child poverty, condensing the analysis from 220 tracts into quintiles allowed us to make discrete comparisons between low- and high-poverty communities across the county. Figure 2A illustrates the distribution of census tract admission rates across each poverty quintile. The county-wide PICU admission rate was 20.6 admissions per 1000 children over the study period. Quintile 1 had a median admission rate of 11.3 admissions per 1000 children, which increased to 32.0 per 1000 children in Quintile 5 (P < .001). Figure 2B illustrates PICU bed-day rates across quintiles. The county-wide PICU bed-day rate was 55.3 days per 1000 children. Quintile 1 had a median PICU bed-day rate of 23.4 days per 1000 children, which increased to 81.9 days per 1000 children in Quintile 5 (P < .001).
FIGURE 2.
A, PICU admission rate. B, PICU IPBD rate. Plots of PICU admission and bed-day rates by poverty quintile are shown. Census tracts were aggregated into quintiles based on child poverty rate from lowest (Quintile 1) to highest (Quintile 5). Bold horizontal lines represent the median admission (upper figure) and PICU bed-day (lower figure) rates in each quintile (P < .0001 for both variables), whereas gray boxes represent the interquartile range. Whiskers represent 1.5 times the interquartile range for each quintile, and dots represent census tracts that were outliers.
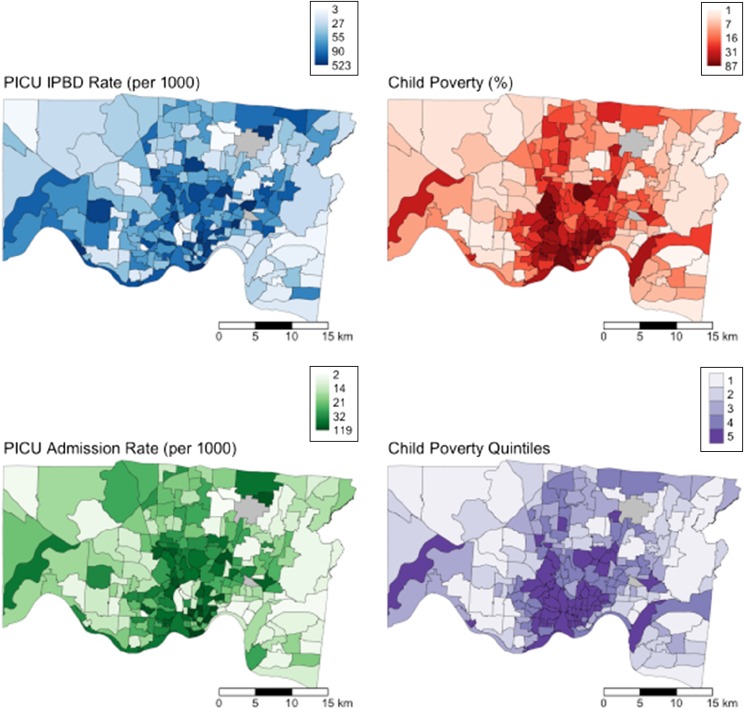
Finally, we visualized geospatial patterns of each PICU use outcome and child poverty. The panels in Fig 3 depict the large degree of overlap between these measures. In each map, darker shades indicate higher rates of each variable; gradations are continuous rather than quintile based. The figure in the lower right illustrates how the tracts aggregated into the 5 poverty-based quintiles. This figure also illustrates how areas with higher rates of PICU use and poverty were not uniformly distributed throughout the county; clusters of both were observed in Cincinnati’s urban core.
FIGURE 3.
Maps of Greater Cincinnati demonstrating PICU bed-day (upper left), child poverty (upper right), and PICU admission rates (lower left) of census tracts. Shades correspond to the rank, rather than the absolute number, of each continuous variable. Poverty quintiles (lower right) range from Quintile 1 (lowest poverty; lightest shade) to Quintile 5 (highest poverty; darkest shade).
Discussion
Our study evaluated pediatric intensive care use patterns in Cincinnati and the surrounding Hamilton County over a multiyear period. We found significant correlations between neighborhood child poverty rates and neighborhood rates of PICU use, providing further evidence of income-based disparities in the need for intensive care services. By our estimates, if all children in Hamilton County required PICU care at rates equivalent to children in the quintile with the lowest rates of child poverty, there would have been nearly 2000 fewer PICU admissions and nearly 8000 fewer PICU bed days during our study period, which is almost 22 child-years of time our region’s children could have avoided spending in the PICU.
The disproportionate burden of critical illness on low-income children affects the physical, mental, emotional, and financial health of children and families in ways that are both obvious and subtle. As stated previously, evidence suggests that lower-income children are more ill when they arrive to the PICU and may be more likely to die before PICU or hospital discharge. Even when children survive a PICU stay, their quality of life may subsequently be diminished compared with their experience before admission; they may also experience lower functioning and quality of life compared with same-age controls who did not experience a PICU stay.15–17,24–26 Although there is not currently evidence to suggest that this “post-intensive care syndrome” is more likely to develop in lower-income children after a PICU admission, the disproportionate burden of critical illness in lower-income children also results in increased exposure to the risks of its subsequent effects.
The impact of a PICU stay on a family is also substantial. The medical and nonmedical financial costs of a hospital admission may be especially catastrophic for the already financially distressed family27,28 and may be worsened by the comparatively higher costs of a PICU admission. Lower-income earners commonly have jobs that tend to have less work flexibility,28,29 causing these parents the added distress of having to choose between dedicating time to earning income or being with their critically ill child. The inequitable acute and longer-term burdens of critical illness on low-income children, families, and communities merit focused investigation and action.
Although research has begun to explore the relationships between poverty and pediatric intensive care needs, it has largely, although not exclusively, used a patient-level frame. We suggest that taking a neighborhood-level view of poverty-related health disparities, as some authors have done, may support both public health– and health system–based approaches to pattern recognition and preventive strategies aimed at disparity reduction.1,30–37 We also agree with authors who argue that worse health outcomes seen in higher-poverty neighborhoods represent more than just the aggregate of individual health risks, behaviors, and disparities.38–40 Delineating the complex, intersectional relationships between individual demographic variables; patient and family health risk factors, assets, and exposures; health infrastructure of communities; and cultural and community health norms and practices offers a broader and more nuanced understanding of health inequity and the roots of disparities. Our data support the potential value of identifying high-risk neighborhoods or “hot spots” to inform future community-hospital partnership interventions. Our findings also provide important context for future studies that will seek to explore disparities in PICU use using a multilevel approach.
Mechanisms by which a physical and social environment may influence need for pediatric intensive care become apparent when examining features common in high-poverty, racially segregated neighborhoods.5,6,16,30–45 Higher-poverty neighborhoods may lack health care infrastructure equivalent to that found in lower-poverty neighborhoods (eg, fewer or more distant points of care access or a limited number of providers who accept public insurance).46,47 Physical living conditions and a more distressed social environment likely also contribute.30,40–44 For example, dilapidated, substandard, or overcrowded housing; environmental pollution; a lack of safe public spaces for play and recreation; and increased exposure to tobacco smoke may increase a child’s risk of injury or exposure to allergens, toxins, or infections.6,35,40–44 Neighborhoods with higher poverty rates bear a greater burden of community violence, which may directly affect a child’s need for critical care by way of injury5,32,42–44,48; community violence (along with the aforementioned exposures) also serves as a toxic stressor, which can affect health in ways that are becoming increasingly well characterized.11,30,45,49–52 Even if a neighborhood does not have comparatively higher crime rates, the perception of poor neighborhood safety can affect the physical health of residents,53 as can the chronic sense of social devaluation based on socioeconomic status, race, or place of residence.38,39 When experienced within the health care system, this sense of social devaluation may create a community culture in which care is not routinely sought or is sought late in the course of illness even if resources are physically and financially available.
The intensive care setting provides a unique platform for evaluating the contribution of poverty to childhood illness. When examining disparities in admissions across the general inpatient ward, it is occasionally argued that identified disparities in use are rooted, at least in part, in providers’ “social concerns” about particular patients or families; for example, a provider may be more likely to admit rather than discharge a low-income patient from the emergency department on the basis of perceptions about access to follow-up care or adherence to a medication regimen even if that patient is less ill compared with a child from a higher-income family. Data do not support this argument,54–56 and we further argue that even if it is true, this is a symptom of rather than an explanation for income-based disparity. Nonetheless, the more severe physiologic derangements typically observed in children who are ill enough to be admitted to an ICU57,58 serve to remove this potential social confounder, isolating relationships between childhood illness and poverty.
There are important limitations to our study. First, although we chose to focus on in-county admissions given that nearly all children admitted from within Hamilton County are admitted to CCHMC,23 this resulted in single-center data from 1 county. There are also still in-county patients we may have missed who used intensive care services at other centers, although we suspect this number is small. The racial and economic makeup of Hamilton County is also not necessarily generalizable, with a racial composition that is different from the United States as a whole and slightly higher poverty levels than the national average.31,59 Third, we used census tracts as a surrogate marker for neighborhood, and although this provided standardized measures for our study, the accepted geographic and social boundaries of residential neighborhoods may not precisely correlate with census tract divisions. That said, analyses of disparities between neighborhoods as defined by communities has also been described, with analogous relationships between poverty and health care use being observed.44
At present, our study examines only disparities in CCHMC PICU admissions and bed days; clinical outcomes were not a component of this investigation. Future research will assess for disparities in the severity of illness on presentation, clinical courses, and dispositions of critically ill children by poverty level of their residential neighborhoods, as defined by census tracts and/or community-defined boundaries. Additional directions include exploration of whether particular diagnoses (eg, lower respiratory infection, trauma, and perhaps even sepsis) drive the disparities observed in critical care use between low- and high-poverty communities. These data may be particularly useful to inform targeted intervention efforts (eg, community outreach on asthma recognition and management in certain neighborhoods or bolstering discharge processes for families from other high-risk neighborhoods).
Finally, there were some high-poverty tracts within Hamilton County that did not have a high rate of PICU use and, conversely, had comparatively lower-poverty tracts that demonstrated high PICU use. Evaluating which characteristics of these communities may help to shield children from critical illness or confer elevated risk could also help in focusing intervention efforts.
Conclusions
Children who live in poverty in the United States have inferior health outcomes compared with those who live in more privileged communities. Our study suggests that these inequities include a disproportionate burden of critical illness. Further delineating the extent of that burden, including contributory disease states and outcomes of critical illness, is important future work. Understanding how physical and cultural environments within communities contribute to need for intensive care may reveal opportunities for interventions that promote health equity across health systems, including in the ICU.
Glossary
- ACS
American Community Survey
- CCHMC
Cincinnati Children’s Hospital Medical Center
- EHR
electronic health record
- IPBD
inpatient bed-day
Footnotes
Dr Andrist drafted the initial manuscript, revised the manuscript, and contributed to the study design and statistical analyses; Drs Riley and Beck conceptualized the study, contributed to the study design, and reviewed and revised the manuscript; Dr Brokamp was principally responsible for the statistical analyses and figures, is a cocreator of the geospatial software used in the project, and reviewed and revised the manuscript; Mr Taylor designed and implemented the data collection tools used in the electronic medical record; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported through the National Institutes of Health (NIH 1K23AI112916). Funders played no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the article. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Slain KN, Shein SL, Stormorken AG, Broberg MCG, Rotta AT. Outcomes of children with critical bronchiolitis living in poor communities. Clin Pediatr (Phila). 2018;57(9):1027–1032 [DOI] [PubMed] [Google Scholar]
- 2.Beck AF, Huang B, Simmons JM, et al. . Role of financial and social hardships in asthma racial disparities. Pediatrics. 2014;133(3):431–439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beck AF, Huang B, Auger KA, et al. . Explaining racial disparities in child asthma readmission using a causal inference approach. JAMA Pediatr. 2016;170(7):695–703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Williams DR, Sternthal M, Wright RJ. Social determinants: taking the social context of asthma seriously. Pediatrics. 2009;123(suppl 3):S174–S184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hakmeh W, Barker J, Szpunar SM, Fox JM, Irvin CB. Effect of race and insurance on outcome of pediatric trauma. Acad Emerg Med. 2010;17(8):809–812 [DOI] [PubMed] [Google Scholar]
- 6.Ong T, Schechter M, Yang J, et al. ; EPIC Study Group . Socioeconomic status, smoke exposure, and health outcomes in young children with cystic fibrosis. Pediatrics. 2017;139(2):e20162730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Attenello FJ, Ng A, Wen T, et al. . Racial and socioeconomic disparities in outcomes following pediatric cerebrospinal fluid shunt procedures. J Neurosurg Pediatr. 2015;15(6):560–566 [DOI] [PubMed] [Google Scholar]
- 8.Piatt JH., Jr Pediatric spinal injury in the US: epidemiology and disparities. J Neurosurg Pediatr. 2015;16(4):463–471 [DOI] [PubMed] [Google Scholar]
- 9.Rossen LM. Neighbourhood economic deprivation explains racial/ethnic disparities in overweight and obesity among children and adolescents in the U.S.A. J Epidemiol Community Health. 2014;68(2):123–129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pomerantz WJ, Dowd MD, Buncher CR. Relationship between socioeconomic factors and severe childhood injuries. J Urban Health. 2001;78(1):141–151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Felitti VJ, Anda RF, Nordenberg D, et al. . Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245–258 [DOI] [PubMed] [Google Scholar]
- 12.Johnson SB, Riis JL, Noble KG. State of the art review: poverty and the developing brain. Pediatrics. 2016;137(4):e20153075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Children’s Defense Fund Ending child poverty now: overview. 2017. Available at: https://www.childrensdefense.org/policy/resources/overview/. Accessed March 1, 2019
- 14.Council on Community Pediatrics Poverty and child health in the United States. Pediatrics. 2016;137(4):e20160339. [DOI] [PubMed] [Google Scholar]
- 15.Epstein D, Reibel M, Unger JB, et al. . The effect of neighborhood and individual characteristics on pediatric critical illness. J Community Health. 2014;39(4):753–759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cassidy LD, Lambropoulos D, Enters J, et al. . Health disparities analysis of critically ill pediatric trauma patients in Milwaukee, Wisconsin. J Am Coll Surg. 2013;217(2):233–239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lopez AM, Tilford JM, Anand KJ, et al. . Variation in pediatric intensive care therapies and outcomes by race, gender, and insurance status. Pediatr Crit Care Med. 2006;7(1):2–6 [DOI] [PubMed] [Google Scholar]
- 18.Colvin JD, Zaniletti I, Fieldston ES, et al. . Socioeconomic status and in-hospital pediatric mortality. Pediatrics. 2013;131(1). Available at: www.pediatrics.org/cgi/content/full/131/1/e182 [DOI] [PubMed] [Google Scholar]
- 19.Beck AF, Riley CL, Taylor SC, Brokamp C, Kahn RS. Pervasive income-based disparities in inpatient bed-day rates across conditions and subspecialties. Health Aff (Millwood). 2018;37(4):551–559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bosnjakovic E. INSIGHT Database. Columbus, OH: Ohio Hospital Association; 2009 [Google Scholar]
- 21.Census Bureau American FactFinder. 2018. Available at: https://factfinder.census.gov/faces/nav/jsf/pages/searchresults.xhtml?refresh=t. Accessed October 9, 2019
- 22.Brokamp C, Wolfe C, Lingren T, Harley J, Ryan P. Decentralized and reproducible geocoding and characterization of community and environmental exposures for multi-site studies. J Am Med Inform Assoc. 2018;25(3):309–314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.US Census Bureau American Community Survey 5-year estimates. Hamilton County, OH. 2016. Available at: https://censusreporter.org/profiles/05000US39061-hamilton-county-ohva. Accessed October 9, 2019
- 24.Herrup EA, Wieczorek B, Kudchadkar SR. Characteristics of postintensive care syndrome in survivors of pediatric critical illness: a systematic review. World J Crit Care Med. 2017;6(2):124–134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Als LC, Picouto MD, Hau SM, et al. . Mental and physical well-being following admission to pediatric intensive care. Pediatr Crit Care Med. 2015;16(5):e141–e149 [DOI] [PubMed] [Google Scholar]
- 26.Polic B, Mestrovic J, Markic J, et al. . Long-term quality of life of patients treated in paediatric intensive care unit. Eur J Pediatr. 2013;172(1):85–90 [DOI] [PubMed] [Google Scholar]
- 27.Cohen RA, Kirzinger WK. Financial burden of medical care: a family perspective. NCHS Data Brief. 2014;142(142):1–8 [PubMed] [Google Scholar]
- 28.Chang LV, Shah AN, Hoefgen ER, et al. ; H2O Study Group . Lost earnings and nonmedical expenses of pediatric hospitalizations. Pediatrics. 2018;142(3):e20180195. [DOI] [PubMed] [Google Scholar]
- 29.Lundeen A; Tax Foundation. Most common jobs by income bracket. 2014. Available at: https://taxfoundation.org/most-common-jobs-income-bracket/. Accessed March 1, 2019
- 30.Beck AF, Huang B, Ryan PH, et al. . Areas with high rates of police-reported violent crime have higher rates of childhood asthma morbidity. J Pediatr. 2016;173:175–182.e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Beck AF, Florin TA, Campanella S, Shah SS. Geographic variation in hospitalization for lower respiratory tract infections across one county. JAMA Pediatr. 2015;169(9):846–854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Beard JH, Morrison CN, Jacoby SF, et al. . Quantifying disparities in urban firearm violence by race and place in Philadelphia, Pennsylvania: a cartographic study. Am J Public Health. 2017;107(3):371–373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cooper RA, Cooper MA, McGinley EL, Fan X, Rosenthal JT. Poverty, wealth, and health care utilization: a geographic assessment. J Urban Health. 2012;89(5):828–847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Winkleby MA, Cubbin C. Influence of individual and neighbourhood socioeconomic status on mortality among black, Mexican-American, and white women and men in the United States. J Epidemiol Community Health. 2003;57(6):444–452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yousey-Hindes KM, Hadler JL. Neighborhood socioeconomic status and influenza hospitalizations among children: New Haven County, Connecticut, 2003-2010. Am J Public Health. 2011;101(9):1785–1789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Riley C, Maxwell A, Parsons A, Andrist E, Beck AF. Disease prevention & health promotion: what’s critical care got to do with it? Transl Pediatr. 2018;7(4):262–266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Susser M, Susser E. Choosing a future for epidemiology: II. From black box to Chinese boxes and eco-epidemiology. Am J Public Health. 1996;86(5):674–677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kothari CL, Paul R, Dormitorio B, et al. . The interplay of race, socioeconomic status and neighborhood residence upon birth outcomes in a high black infant mortality community. SSM Popul Health. 2016;2:859–867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Braveman PA, Heck K, Egerter S, et al. . The role of socioeconomic factors in Black-White disparities in preterm birth. Am J Public Health. 2015;105(4):694–702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cubbin C, LeClere FB, Smith GS. Socioeconomic status and injury mortality: individual and neighbourhood determinants. J Epidemiol Community Health. 2000;54(7):517–524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Beck AF, Huang B, Chundur R, Kahn RS. Housing code violation density associated with emergency department and hospital use by children with asthma. Health Aff (Millwood). 2014;33(11):1993–2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gielen AC, Shields W, McDonald E, et al. . Home safety and low-income urban housing quality. Pediatrics. 2012;130(6):1053–1059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.O’Campo P, Rao RP, Gielen AC, Royalty W, Wilson M. Injury-producing events among children in low-income communities: the role of community characteristics. J Urban Health. 2000;77(1):34–49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Beck AF, Moncrief T, Huang B, et al. . Inequalities in neighborhood child asthma admission rates and underlying community characteristics in one US county. J Pediatr. 2013;162(2):574–580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Attar BK, Guerra NG, Tolan PH. Neighborhood disadvantage, stressful life events, and adjustment in urban elementary-school children. J Clin Child Psychol. 1994;23(4):391–400 [Google Scholar]
- 46.Bodenheimer T, Pham HH. Primary care: current problems and proposed solutions. Health Aff (Millwood). 2010;29(5):799–805 [DOI] [PubMed] [Google Scholar]
- 47.Strickland BB, Jones JR, Ghandour RM, Kogan MD, Newacheck PW. The medical home: health care access and impact for children and youth in the United States. Pediatrics. 2011;127(4):604–611 [DOI] [PubMed] [Google Scholar]
- 48.Carter PM, Cook LJ, Macy ML, et al. ; Pediatric Emergency Care Applied Research Network (PECARN) . Individual and neighborhood characteristics of children seeking emergency department care for firearm injuries within the PECARN network. Acad Emerg Med. 2017;24(7):803–813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Evans GW, English K. The environment of poverty: multiple stressor exposure, psychophysiological stress, and socioemotional adjustment. Child Dev. 2002;73(4):1238–1248 [DOI] [PubMed] [Google Scholar]
- 50.Purtle J, Harris E, Compton R, et al. . The psychological sequelae of violent injury in a pediatric intervention. J Pediatr Surg. 2014;49(11):1668–1672 [DOI] [PubMed] [Google Scholar]
- 51.Johnson SB, Riley AW, Granger DA, Riis J. The science of early life toxic stress for pediatric practice and advocacy. Pediatrics. 2013;131(2):319–327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hillis SD, Mercy JA, Saul JR. The enduring impact of violence against children. Psychol Health Med. 2017;22(4):393–405 [DOI] [PubMed] [Google Scholar]
- 53.Ziersch AM, Baum FE, Macdougall C, Putland C. Neighbourhood life and social capital: the implications for health. Soc Sci Med. 2005;60(1):71–86 [DOI] [PubMed] [Google Scholar]
- 54.MacFaul R, Glass EJ, Jones S. Appropriateness of paediatric admission. Arch Dis Child. 1994;71(1):50–58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lovejoy FH Jr, Carper JM, Janeway CA, Kosa J. Unnecessary and preventable hospitalizations: report on an internal audit. J Pediatr. 1971;79(5):868–872 [DOI] [PubMed] [Google Scholar]
- 56.Kemper KJ. Medically inappropriate hospital use in a pediatric population. N Engl J Med. 1988;318(16):1033–1037 [DOI] [PubMed] [Google Scholar]
- 57.American Academy of Pediatrics Committee on Hospital Care and Section on Critical Care; Society of Critical Care Medicine Pediatric Section Admission Criteria Task Force. Guidelines for developing admission and discharge policies for the pediatric intensive care unit. American Academy of Pediatrics. Committee on Hospital Care and Section of Critical Care. Society of Critical Care Medicine. Pediatric Section Admission Criteria Task Force. Pediatrics. 1999;103(4, pt 1):840–842 [PubMed] [Google Scholar]
- 58.Rosenberg DI, Moss MM; American College of Critical Care Medicine of the Society of Critical Care Medicine . Guidelines and levels of care for pediatric intensive care units. Crit Care Med. 2004;32(10):2117–2127 [DOI] [PubMed] [Google Scholar]
- 59.Semega JL, Fontenot KR, Kollar MA; United States Census Bureau. Income and poverty in the United States: 2016. Report number P60-259. Available at: https://www.census.gov/content/dam/Census/library/publications/2017/demo/P60-259.pdf. Accessed October 3, 2019