Abstract
To investigate whether Kinesio tape (KT) application improves proprioception, balance, and functional performance in patients with anterior cruciate ligament rupture (ACLr).
This retrospective analysis included 48 male patients with surgically-untreated ACLr who attended the Sports Medicine and Rehabilitation Center, Qingdao Municipal Hospital, China between June 2017 and June 2018. KT was applied to induce a detoning effect on the quadriceps muscle and toning effect on the ischiocrural muscles. Proprioception, balance, and functional performance were assessed before and 1 and 7 days after KT application using the Lysholm scale, anteroposterior shift of the tibia (APST), active angle reproduction test (AART), modified star excursion balance test (mSEBT), and single-hop distance (SHD).
KT resulted in significant improvements in Lysholm scale at 1 day (83.00 [6.50] vs. 76.00 [5.25], P < .001) and APST (8.00 [2.00] vs. 10.00 [2.00] mm, P < .001), AART (3.00 [1.00] vs. 4.00 [1.75] degrees, P < .001), SEBT (96.08 [6.62] vs. 83.92 [7.31] %, P < .001) and SHD (120.96 [6.94] vs. 106.46 [9.03] %, P < .001) at 3 hours (median [interquartile range]). However, significant deficits remained when compared with the healthy side. Except for mSEBT posterolateral direction, those effects were maintained at 7 days.
KT has benefits in people with ACLr but cannot fully compensate for functional deficits. KT could be used to assist knee strengthening during rehabilitation.
Keywords: anterior cruciate ligament, balance, function, Kinesio tape, proprioception
1. Introduction
Anterior cruciate ligament rupture (ACLr) is one of the most common sporting injuries.[1] ACLr is associated with joint instability and secondary meniscal and cartilage lesions that limit mobility and exercise capacity.[1] The functional abnormalities that occur after ACLr include a loss of proprioception and balance, a decrease in muscle power and functional performance, and changes in biomechanics.[2] Although ACL reconstruction is one of the most common operations performed in orthopedic surgery,[3] nonsurgical treatment options can also produce good outcomes.[4]
ACLr affects proprioception of the knee because of damage to proprioceptors in the joint.[5] Kinesio tape (KT) is a thin, elastic tape that is applied to the skin surface to produce toning or detoning effects on the underlying muscles with the aim of rebalancing the affected musculature after injury.[6] The use of KT has been suggested to improve proprioception, blood circulation, lymph flow, and the stability of movement after sporting injuries.[6–8] However, very few studies have examined the clinical utility of KT in patients with ACLr. A preliminary study found that the use of KT led to more rapid improvements in range of motion, thigh circumference, and knee edema after surgery, with a decrease in the use of analgesics.[9] A subsequent randomized controlled trial of KT after ACL reconstruction also reported that pain was reduced in the early postoperative period, but there were no significant effects on knee swelling, range of motion, or Lysholm-Tegner knee scale score.[10] Furthermore, a recent study concluded that the application of KT in patients with ACLr not treated surgically resulted in improvements in proprioception, gait pattern, and subjectively perceived joint function.[11]
The objective of the present retrospective study was to assess the effects of KT on proprioception, balance, and functional performance of the knee with ACLr.
2. Patients and methods
2.1. Study design and participants
This was a retrospective analysis of consecutive patients with ACLr treated at the Sports Medicine and Rehabilitation Center, Qingdao Municipal Hospital, China, between June 2017 and June 2018. The inclusion criteria were:
-
(1)
male;
-
(2)
aged 18–30 years;
-
(3)
diagnosis of ACLr based on the clinical history and results of the Lachman test, lever sign test,[12] and magnetic resonance imaging;
-
(4)
unilateral ACLr;
-
(5)
no other lesions;
-
(6)
time from injury of 1–6 months;
-
(7)
Tegner activity level scale of 5–8; and
-
(8)
receiving conservative treatment either as the primary therapy or while awaiting surgery.
The exclusion criteria were:
-
(1)
injury to the contralateral knee joint;
-
(2)
injuries to other ligaments in the ipsilateral knee joint; and
-
(3)
intolerance toward KT or its components.
The ethics committee of Qingdao Municipal Hospital approved the study. Informed consent was waived due to the retrospective study design.
2.2. Methods
Application of the KT (Kinesio Tex Classic, Kinesio Co. Ltd, Tokyo, Japan) was performed by the same experienced physiotherapist.[11] KT was applied in a Y-shape (running either side of the patella from the tibial tuberosity to the anterior inferior iliac spine) with 10% tension to induce a detoning effect on the quadriceps muscle (Fig. 1). KT was also applied in a Y-shape (from the ischial tuberosity to the medial tibial condyle and upper aspect of the fibular head) with 10% tension to induce a toning effect on the ischiocrural muscle group (Fig. 1). An additional tape was applied over the tibial tuberosity with dorsal 20% tension (Fig. 1). During follow-up, the participants were instructed not to apply heat or water to the body area containing KT.
Figure 1.

Application of Kinesio tape (KT). KT was applied in a Y-shape (running either side of the patella from the tibial tuberosity to the anterior inferior iliac spine) with 10% tension to induce a detoning effect on the quadriceps muscle (black). KT was also applied in a Y-shape (from the ischial tuberosity to the medial tibial condyle and upper aspect of the fibular head) with 10% tension to induce a toning effect on the ischiocrural muscle group (pink). An additional tape was applied over the tibial tuberosity with dorsal 20% tension (blue).
2.3. Methodology
All data were collected from the medical charts. Data were de-identified after extraction and for analysis. Data were stored in a password-protected Excel file. All data were kept for 10 years, after which the Excel file will be destroyed.
All the assessments described below were made before and 3 hours after the application of KT,[11] except for subjective self-assessment of the injured knee joint, which was made the day after KT application. In our experience, the service life of KT is around 2–3 days (by which time the tape loses some of its elasticity); for this reason, the subjective assessments were made 1 day after KT rather than 3 days after taping, as were done in a previous study.[11] Furthermore, these subjective assessments were also done 7 days after KT to observe the effects over a longer time.
Subjective self-assessment of the injured knee joint was carried out by the participants using the Lysholm scale.[12] Anteroposterior shift of the tibia (APST)[13] was measured with a KneeLax 3 joint arthrometer (Monitored Rehab Systems BV, Haarlem, Netherlands) under 30° knee flexion and 132 N.
The active angle reproduction test (AART)[14] was performed using the IsoMed 2000 isokinetic dynamometer (D. & R. Ferstl GmbH, Hemau, Germany). Each participant was seated comfortably with his vision shielded and legs dangling over the edge of the seat. The affected leg was passively extended from a starting position of 90° knee flexion to 30° knee flexion with an angular velocity of 2°/s, held in this position for 5 seconds and then repositioned to the initial position. Following a 5 seconds rest, the participant was asked to perform active knee flexion to a 30° angle. The angle reached was measured, and its difference from the target angle was recorded. The test was repeated three times, and the mean value was used for the analysis. The AART was carried out by two physiotherapists who had received identical training. This test has a fair to good reliability.[15]
For the modified star excursion balance test (mSEBT),[16] each participant was asked to place the great toe of the affected leg at the center of three lines oriented in the anterior, posteromedial, and posterolateral directions, with his hands on his hips throughout the test procedure. The patient was then asked to maintain a single leg stance on the affected leg while reaching as far as possible with the other leg to complete a single non-weight-bearing toe touch in one of the test directions before returning the reaching leg to the starting position. Weight-bearing toe touches, lifts, or shifts of any part of the stance foot, or loss of balance were considered unsuccessful trials. Every participant was allowed to practice four times in each test direction to become familiar with the trial protocol. Three successful trials were recorded for each test direction, and the mean value was used as the reaching distance for each direction. Then, the reaching distance for each direction was normalized (as a percentage) to the participant's leg length (measured from the anterosuperior iliac spine to the distal end of the medial malleolus). The overall mSEBT score was a composite value calculated as the mean of the normalized measurements for the three different directions. The mSEBT has excellent reliability.[17]
The single-hop distance (SHD)[18] was measured as follows. After 10 minutes of rest, the participant was asked to perform a single leg hop. The hop distance was measured from the toe at push-off to the heel at landing. Unsuccessful trials were defined as any part except the stance foot contacting the ground. Every participant was allowed to practice several times before the measurements were made. Three successful trials were recorded, and the mean value normalized to the participant's leg length was used as the SHD. The SHD has been shown to be valid and reliable.[19]
2.4. Statistical analysis
No sample size analysis was done. Based on similar studies, a sample size of 48 participants was set. A post hoc power analysis based on the Wilcoxon signed-rank test and the Mann–Whitney U test showed powers of 99.7% and 99.9%, respectively.
Data were analyzed using SPSS for Windows version 22 (IBM Corporation, Armonk, NY). All continuous data were tested for normality and found to be non-normally distributed. Therefore, these data are presented as median (interquartile range) and were analyzed using the Wilcoxon signed-rank test (for comparisons before and after KT) or the Mann–Whitney U test (for comparisons between legs). The Friedman test was used to evaluate the effects during different time sets. P < .05 was taken to indicate statistical significance.
3. Results
3.1. Baseline characteristics of the study participants
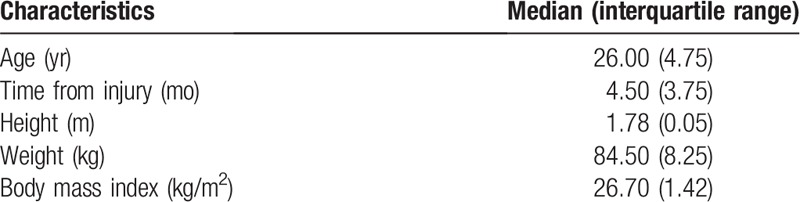
A total of 48 male patients with ACLr were included in the study. The baseline characteristics of the 48 participants are presented in Table 1. The participants were mostly young adults with some overweight.
Table 1.
Baseline characteristics of the 48 study participants.
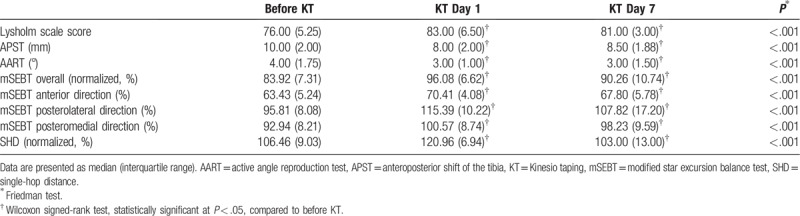
3.2. Comparison of outcome measures for the affected leg before and after KT
The Lysholm scale score, APST, AART, mSEBT, and SHD for the affected leg showed significant improvements at day 1 after KT (all P < .001), compared with the values obtained before the application of KT. At day 7 after KT, similar results were observed (all P < .001 vs. baseline) (Table 2). Taken together, the results suggest that the application of KT in participants with ACLr improves proprioception, balance, and functional performance and that the effects are maintained in time for at least 7 days.
Table 2.
Comparison of outcome measures for the affected leg before and after KT.
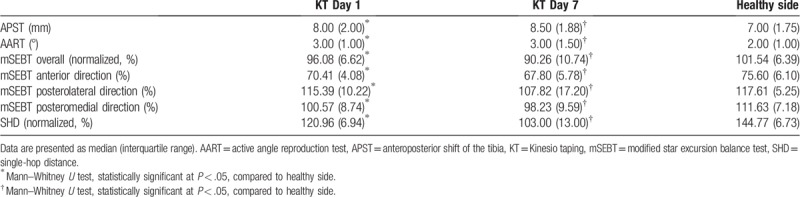
3.3. Comparison of outcome measures between the affected side after KT and the healthy side
At 1 day after the application of KT, the affected side had significantly higher values for APST (P = .008) and AART (P < .001), and significantly lower values for mSEBT overall (P < .001), mSEBT anterior direction (P < .001), mSEBT posterolateral direction (P = .001), mSEBT posteromedial direction (P < .001), and SHD (P < .001) than the healthy side without KT application. At 7 days after the application of KT, the affected side had significantly higher values for APST (P < .001) and AART (P < .001), and significantly lower values for mSEBT overall (P < .001), mSEBT anterior direction (P < .001), mSEBT posteromedial direction (P = .018), and SHD (P < .001) than the healthy side without KT application. There was no difference in mSEBT posterolateral direction at 7 days after the KT application (P = .205) (Table 3). Taken together, despite improvements after KT, the results suggest that the application of KT in participants with ACLr does not completely restore the indicators of proprioception, balance, and functional performance compared with the healthy side.
Table 3.
Comparison of outcome measures between the affected side after KT and the healthy side.
4. Discussion
The main objective of this study was to investigate whether KT improves proprioception, balance, and functional performance in patients with ACLr during the early period after its application. The positive results showed that KT improved Lysholm score, APST, AART, mSEBT, and SHD within a short time (1 day) after its application and that the effect could last for several days, but seems to decline as time goes on. Moreover, there was still significant difference between the affected side after KT application and the healthy side.
KT is an adhesive elastic tape that can be extended up to 140% of its initial length. KT was first developed by Dr Kase in the 1970s, and it has shown promise as a treatment method for musculoskeletal rehabilitation and sports injury. KT exerts various effects according to the amount of extension and taping method used, and these effects include:
-
(1)
reducing edema, inhibiting pain, and improving blood flow and lymphatic drainage[20,21];
-
(2)
stimulating proprioceptors in the skin, muscle tissue, and joint capsule and thereby improving proprioception and balance[22,23]; and
-
(3)
facilitating muscles, reducing muscle fatigue and enhancing movement performance.[24]
Although the application of KT has been demonstrated to have positive effects on pain management,[25] postural correction,[26] and lymph flow,[27] its influence on the proprioception and balance of an injured knee is still controversial. A study by Torres et al[28] found that KT in healthy participants led to immediate and short-term improvements in the threshold for movement detection, but no significant effect on joint position sense. Ahn et al[29] concluded that the use of KT on knee extensor muscles had no significant effect on joint position sense and static balance.
On the other hand, there is evidence that the KT application can improve knee proprioception and balance. Cho et al[30] determined that KT over the quadriceps had beneficial short-term effects in elderly people with osteoarthritis, with significant improvements in activity, proprioception, and pain compared with those receiving a placebo treatment. Furthermore, a crossover study of healthy elderly people performed by Simon et al[31] showed that KT application was associated with significant improvements in dynamic balance, postural stability, and knee proprioception during a 30-minute downhill path walk, as compared with non-application of KT.
There are several possible reasons for the negative outcomes of previous studies. First, the proprioceptors of healthy participants are normal; hence, KT would not be expected to produce a notable enhancement of proprioception. Indeed, most of the positive effects of KT application on proprioception observed previously were in participants with trauma.[7,23,32] Second, positive outcomes with KT are more readily detectable when proprioception function is disturbed. Third, the initial levels of proprioception and balance function can affect the outcomes of experiments. A study of healthy young male participants revealed that the effect of KT application was significant in participants with poor primary balance function but not in those with good motor control.[33]
ACLr would be expected to influence proprioception and balance functions because proprioceptors are present in the ACL. Furthermore, APST would be expected to disturb normal afferent proprioception, causing instability and pain. In our research, stretching induced by KT was able to excite proprioceptors, partly compensating for the decrease in proprioception caused by ACLr. Moreover, the detoning effect on the quadriceps muscle and toning effect on the hamstring muscles would together limit APST (as evidenced by the decrease in APST value in this study), thereby improving afferent proprioception and leading to positive outcomes. However, when the affected side after the KT application was compared with the healthy side, there were still significant differences in proprioception, balance, and functional performance. This shows that external enhancement cannot completely compensate for the loss of proprioception resulting from ACLr.
This study has some limitations. First, this was not a randomized controlled trial, and there is a risk of patient heterogeneity, so the quality of evidence is limited. Second, neither the participant nor investigator was blinded to the intervention because the tape was clearly visible, which may have introduced bias, particularly in self-reported outcomes. Third, this was a single-center study, so the generalizability of the findings is not known. Fourth, gait analysis was not performed. Multicenter randomized controlled trials are needed to confirm and extend our findings.
KT may have beneficial effects on proprioception, balance, and functional performance in people with ACLr, but it cannot completely compensate for the loss of proprioception. The application of KT during rehabilitation may be a good therapeutic option either before ACL reconstruction surgery or as a conservative treatment for ACLr.
Author contributions
Conceptualization: Qi Gao.
Investigation: Kai Liu, Jinghua Qian, Bin Ruan.
Methodology: Kai Liu, Jinghua Qian, Bin Ruan.
Writing – original draft: Kai Liu.
Writing – review & editing: Qi Gao.
Footnotes
Abbreviations: AART = active angle reproduction test, ACLr = anterior cruciate ligament rupture, APST = anteroposterior shift of the tibia, KT = Kinesio tape, mSEBT = modified star excursion balance test, SHD = single-hop distance.
How to cite this article: Liu K, Qian J, Gao Q, Ruan B. Effects of Kinesio taping of the knee on proprioception, balance, and functional performance in patients with anterior cruciate ligament rupture; a retrospective case series. Medicine. 2019;98:48(e17956).
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Siegel L, Vandenakker-Albanese C, Siegel D. Anterior cruciate ligament injuries: anatomy, physiology, biomechanics, and management. Clin J Sport Med 2012;22:349–55. [DOI] [PubMed] [Google Scholar]
- [2].Ageberg E. Consequences of a ligament injury on neuromuscular function and relevance to rehabilitation – using the anterior cruciate ligament-injured knee as model. J Electromyogr Kinesiol 2002;12:205–12. [DOI] [PubMed] [Google Scholar]
- [3].Alazzawi S, Sukeik M, Ibrahim M, et al. Surgical treatment of anterior cruciate ligament injury in adults. Br J Hosp Med (Lond) 2016;77:227–31. [DOI] [PubMed] [Google Scholar]
- [4].Monk AP, Davies LJ, Hopewell S, et al. Surgical versus conservative interventions for treating anterior cruciate ligament injuries. Cochrane Database Syst Rev 2016;4:CD011166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Çabuk H, Kuşku Çabuk F. Mechanoreceptors of the ligaments and tendons around the knee. Clin Anat 2016;29:789–95. [DOI] [PubMed] [Google Scholar]
- [6].Kase K, Wallis J, Kase T. Clinical Therapeutic Applications of the Kinesio Taping Method. Tokyo: Ken Ikai Co. Ltd; 2003. [Google Scholar]
- [7].Williams S, Whatman C, Hume PA, et al. Kinesio taping in treatment and prevention of sports injuries: a meta-analysis of the evidence for its effectiveness. Sports Med 2012;42:153–64. [DOI] [PubMed] [Google Scholar]
- [8].Halseth T, McChesney JW, Debeliso M, et al. The effects of kinesio taping on proprioception at the ankle. J Sports Sci Med 2004;3:1–7. [PMC free article] [PubMed] [Google Scholar]
- [9].Boguszewski D, Tomaszewska I, Adamczyk JG, et al. Evaluation of effectiveness of kinesiology taping as an adjunct to rehabilitation following anterior cruciate ligament reconstruction. Preliminary report. Ortop Traumatol Rehabil 2013;15:469–78. [DOI] [PubMed] [Google Scholar]
- [10].Chan MC, Wee JW, Lim MH. Does kinesiology taping improve the early postoperative outcomes in anterior cruciate ligament reconstruction? A randomized controlled study. Clin J Sport Med 2017;27:260–5. [DOI] [PubMed] [Google Scholar]
- [11].Bischoff L, Babisch C, Babisch J, et al. Effects on proprioception by Kinesio taping of the knee after anterior cruciate ligament rupture. Eur J Orthop Surg Traumatol 2018;28:1157–64. [DOI] [PubMed] [Google Scholar]
- [12].Wu YF, Chen L, Gao DW. Evaluation of four physical examinations in diagnosis of complete rupture of anterior cruciate ligament. J Shanghai Jiao Tong Univ (Med Sci) 2017;37:1513–6. [Google Scholar]
- [13].Lee HM, Cheng CK, Liau JJ. Correlation between proprioception, muscle strength, knee laxity, and dynamic standing balance in patients with chronic anterior cruciate ligament deficiency. Knee 2009;16:387–91. [DOI] [PubMed] [Google Scholar]
- [14].Miao X, Huang H, Hu X, et al. The characteristics of EEG power spectra changes after ACL rupture. PLoS One 2017;12:e0170455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Springer S, Kelman D, Brand M, et al. Knee position sense: does the time interval at the target angle affect position accuracy? J Phys Ther Sci 2017;29:1760–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Cug M, Wikstrom EA, Golshaei B, et al. The effects of sex, limb dominance, and soccer participation on knee proprioception and dynamic postural control. J Sport Rehabil 2016;25:31–9. [DOI] [PubMed] [Google Scholar]
- [17].Gribble PA, Kelly SE, Refshauge KM, et al. Interrater reliability of the star excursion balance test. J Athl Train 2013;48:621–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Fältström A, Hägglund M, Kvist J. Functional performance among active female soccer players after unilateral primary anterior cruciate ligament reconstruction compared with knee-healthy controls. Am J Sports Med 2017;45:377–85. [DOI] [PubMed] [Google Scholar]
- [19].Reid A, Birmingham TB, Stratford PW, et al. Hop testing provides a reliable and valid outcome measure during rehabilitation after anterior cruciate ligament reconstruction. Phys Ther 2007;87:337–49. [DOI] [PubMed] [Google Scholar]
- [20].Lietz-Kijak D, Kijak E, Krajczy M, et al. The impact of the use of kinesio taping method on the reduction of swelling in patients after orthognathic surgery: a pilot study. Med Sci Monit 2018;24:3736–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Rahlf AL, Braumann KM, Zech A. Kinesio taping improves perceptions of pain and function of patients with knee osteoarthritis: a randomized, controlled trial. J Sport Rehabil 2019;28:481–7. [DOI] [PubMed] [Google Scholar]
- [22].Konishi Y. Tactile stimulation with kinesiology tape alleviates muscle weakness attributable to attenuation of Ia afferents. J Sci Med Sport 2013;16:45–8. [DOI] [PubMed] [Google Scholar]
- [23].Simon J, Garcia W, Docherty CL. The effect of kinesio tape on force sense in people with functional ankle instability. Clin J Sport Med 2014;24:289–94. [DOI] [PubMed] [Google Scholar]
- [24].Lee MS. Effects of Kinesio Taping on Muscle Strength Improvement, and the Blood Markers of Muscle Fatigue and Damage. Seoul: Graduate School of Yonsei University; 2007. [Google Scholar]
- [25].Cho YT, Hsu WY, Lin LF, et al. Kinesio taping reduces elbow pain during resisted wrist extension in patients with chronic lateral epicondylitis: a randomized, double-blinded, cross-over study. BMC Musculoskelet Disord 2018;19:193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Abbasi S, Rojhani-Shirazi Z, Shokri E, et al. The effect of Kinesio taping on postural control in subjects with non-specific chronic low back pain. J Bodyw Mov Ther 2018;22:487–92. [DOI] [PubMed] [Google Scholar]
- [27].Kasawara KT, Mapa JMR, Ferreira V, et al. Effects of Kinesio taping on breast cancer-related lymphedema: a meta-analysis in clinical trials. Physiother Theory Pract 2018;34:337–45. [DOI] [PubMed] [Google Scholar]
- [28].Torres R, Trindade R, Gonçalves RS. The effect of kinesiology tape on knee proprioception in healthy subjects. J Bodyw Mov Ther 2016;20:857–62. [DOI] [PubMed] [Google Scholar]
- [29].Ahn IK, Kim YL, Bae YH, et al. Immediate effects of kinesiology taping of quadriceps on motor performance after muscle fatigued induction. Evid Based Complement Alternat Med 2015;2015:410526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Cho HY, Kim EH, Kim J, et al. Kinesio taping improves pain, range of motion, and proprioception in older patients with knee osteoarthritis: a randomized controlled trial. Am J Phys Med Rehabil 2015;94:192–200. [DOI] [PubMed] [Google Scholar]
- [31].Hosp S, Csapo R, Heinrich D, et al. Does kinesiology tape counter exercise-related impairments of balance in the elderly? Gait Posture 2018;62:167–72. [DOI] [PubMed] [Google Scholar]
- [32].Morris D, Jones D, Ryan H, et al. The clinical effects of Kinesio® Tex taping: a systematic review. Physiother Theory Pract 2013;29:259–70. [DOI] [PubMed] [Google Scholar]
- [33].Hosp S, Folie R, Csapo R, et al. Eccentric exercise, kinesiology tape, and balance in healthy men. J Athl Train 2017;52:636–42. [DOI] [PMC free article] [PubMed] [Google Scholar]


