Abstract
Background:
Laser systems are a common treatment choice for onychomycosis. They exert their effects on inhibiting the growth of the fungus by selective photothermolysis but efficacy is dependent on the specific type of apparatus used. To systematically review the available published literature on the curative effects and safety of laser treatment for onychomycosis.
Methods:
Databases including PubMed, web of science, China National Knowledge Internet (CNKI), WanFang Database and VIP were searched systematically to identify relevant articles published up to July 2018. Potentially relevant articles were sourced, assessed against eligibility criteria by 2 researchers independently and data were extracted from included studies. A meta-analysis was performed using R software.
Results:
Thirty-five articles involving 1723 patients and 4278 infected nails were included. Meta-analysis of data extracted from these studies revealed that: the overall mycological cure rate was 63.0% (95%CI 0.53-0.73); the mycological cure rate associated with the 1064-nm Nd: YAG laser was 63.0% (95%CI 0.51-0.74); and that of CO2 lasers was 74.0% (95%CI 0.37-0.98). The published data indicate that laser treatment is relatively safe, but can cause tolerable pain and occasionally lead to bleeding after treatment.
Conclusion:
Laser treatment of onychomycosis is effective and safe. The cumulative cure rate of laser treatment was significantly higher for CO2 lasers than other types of laser. Laser practitioners should be made aware of potential adverse effects such as pain and bleeding.
Keywords: laser, Nd-YAG laser, CO2 laser, onychomycosis, single rate, systematic review
1. Introduction
Onychomycosis is a chronic fungal infection of the nail that may involve the nail bed, plate or matrix. It is difficult to cure and relapses are common. The condition is caused by dermatophytes, principally Trichophyton rubrum, Trichophyton mentagrophytes and Candida albicans.[1] Clinical classification is performed according to the specific site of infection and includes superficial white onychomycosis, proximal subungual onychomycosis, distal and lateral subungual onychomycosis and total dystrophic onychomycosis. Of these, distal and lateral subungual onychomycosis are the most common.[2] Traditional treatments for onychomycosis comprise topical, oral, mechanical and chemical therapies.[3] Topical drug treatments are not usually successful because they are unable to penetrate the nail plate.[4,5] Oral antifungal agents can produce adverse reactions due to a significant risk of liver and kidney toxicity and drug interactions occurring within the body.[6] Topical antifungal treatments can be more effective when combined with surgical removal or chemical dissolution of the nail plate.[7] In 1984, Apfelberg[8] began using laser treatment for onychomycosis, and since that time laser treatments such as long-pulsed 1064-nm Nd: YAG lasers, short-pulsed 1064-nm Nd: YAG lasers, CO2 lasers and lasers with wavelengths of 870 nm, 930 nm and 1320 nm have begun to emerge as new therapies for the treatment of onychomycosis.[9] Compared with topical and oral therapies, laser treatment offers a more promising therapy for the treatment of the condition in diabetics, elderly patients with drug intolerance, and those with liver and kidney disease.[10] However, available evidence concerning its efficacy for the treatment of onychomycosis is contradictory.[11] We therefore conducted a meta-analysis of data extracted from available published studies on laser treatment in the context of onychomycosis, in order to evaluate the efficacy and safety of the available different laser devices. It was anticipated that the results would inform and guide future clinical application of laser treatment technologies for onychomycosis.
2. Materials and methods
All data of this study were collected from published trials, so an additional ethical approval is not necessary.
2.1. Search strategy and eligibility criteria
The study was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. We searched electronic databases (PubMed, Web of Science) for studies published up to July 2018 using the Mesh terms “laser, onychomycosis” and “laser, tinea unguium”. We also searched electronic Chinese databases (CNKI, WanFang Database and VIP) for studies published up to July 2018 using the Chinese keywords “laser, onychomycosis,” and “laser and onychomycosis”. The inclusion criteria for the study were as follows:
-
(1)
Randomized Controlled Trial (RCT) or clinical study in which the onychomycosis group received only laser treatment;
-
(2)
onychomycosis diagnosed by mycological examination;
-
(3)
study purpose related to the efficacy of laser treatment for onychomycosis;
-
(4)
patients had not been treated with systematic antifungal drugs during the preceding 6 months and exhibited no abnormal clinical manifestations associated with other skin diseases such as psoriasis or lichen planus; (4) the treatment group was treated by laser and the control group comprised either a blank control, self-control, and/or laser treatment combined with other treatment options; and
-
(5)
mycological cure rate and clinical cure rate of diseased nail reported. Since clinical cure rates can vary markedly with different treatments, a meta-analysis of mycological cure rates was performed.
The exclusion criteria were as follows:
-
(1)
case reports;
-
(2)
duplicate publications
-
(3)
conference papers, systematic reviews, and meta-analyses
-
(4)
studies in which the laser treated group also received other forms of treatment.
2.2. Study selection
Articles were initially assessed by title and abstract only. Those not meeting the inclusion criteria were excluded; duplicate publications were also excluded. Full-text of the remaining articles was retrieved and assessed to determine eligibility for inclusion in the study. Study selection and data extraction were done independently by two reviewers, and the final results were crosschecked. Disagreements were discussed and resolved with consensus or an additional advice was asked to provide by a third reviewer.
2.3. Data extraction
Relevant information was extracted from publications meeting the inclusion/exclusion criteria by the 2 independent researchers. Extracted data included the lead author, year of publication, method of laser treatment, duration of treatment, identified fungi, duration of treatment, number of infected nails, mycological and clinical cure rates in treatment and control groups, duration of follow-up, quality assessment scores (Jadad/methodological index for non-randomized studies (MINORS)).
2.4. Quality assessment
The quality of RCT studies was evaluated according to the Jadad scale,[12] and the quality of clinical-control articles was evaluated according to the MINORS scale.[13] In brief, the studies were assessed with respect to the following aspects: randomization, allocation concealment, blinding, baseline comparability, loss to follow-up, grade, and were scored from 0 to 5 (0 being the lowest quality and 5 being the highest quality). The MINORS scale contains 12 items: a clearly stated aim, inclusion of consecutive patients, prospective collection of data, endpoints appropriate to the study aim, unbiased assessment of the study endpoint, appropriate follow-up period, loss to follow-up less than 5%, prospective calculation of required sample size, an adequate control group, contemporary groups, baseline equivalence of patient groups and adequate statistical analyses. Each item is scored from 0 to 2 and the first eight relate specifically to non-randomized studies.
2.5. Statistical analysis
A meta-analysis of the efficacy of laser treatment of onychomycosis was performed using extracted data from included studies. Analyses were conducted using R software combined with the clinical/mycological cure rates and its 95% CI. Chi-squared tests were performed to determine the heterogeneity of the outcome data from the included studies. Subsequent quantitative analyses of heterogeneity were performed by calculation of I-squared values; where P < .1 and/or I2 > 50%, heterogeneity existed between the data and the combined analysis was performed using a random effects model. Otherwise, a fixed effect model was used. In the subgroup analysis, the chi-squared test was used to identify differences between subgroups. The potential for publication bias was assessed by construction of a funnel plot. Publication bias was considered likely to exist where P < .05.
3. Results
3.1. Characteristics of the included studies
The systematic search of the literature identified 681 potentially relevant articles. After removing duplicate publications, 104 articles remained and were subjected to preliminary screening of abstracts (Fig. 1). Following the exclusion of descriptive studies and studies that included other therapies in addition to laser treatment, 35 articles remained that met the eligibility criteria. These 35 articles involved 1723 patients and 4278 diseased nails. The specific data extracted from each of these articles are shown in Table 1 . The studies included 5 RCTs. The quality assessment results of the 35 included studies according to the Jadad and MINORS quality evaluation criteria are also presented in Table 1 .
Figure 1.
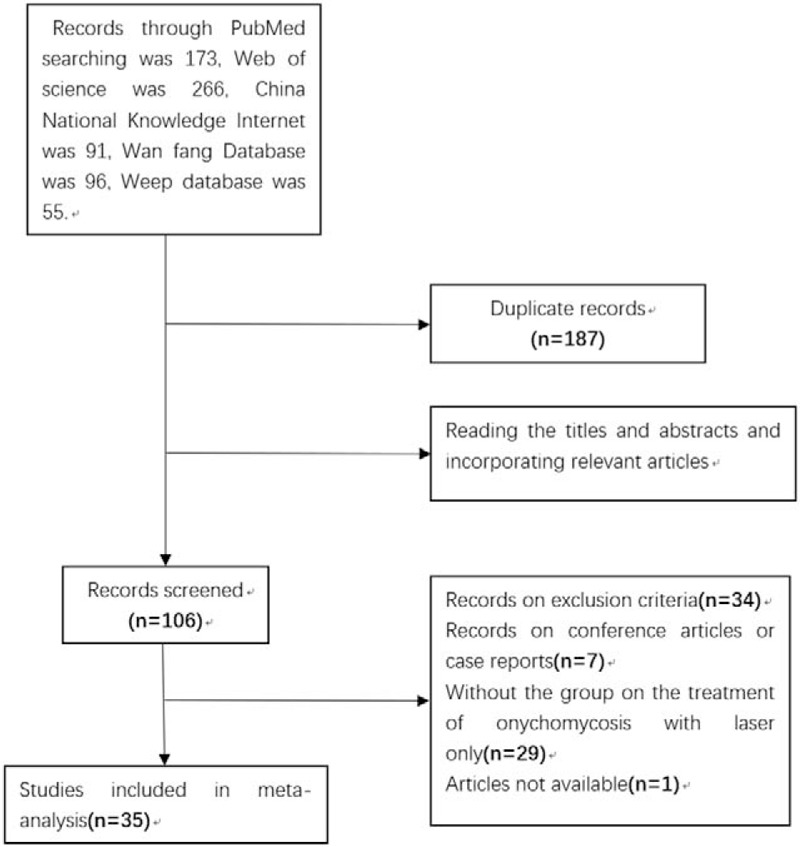
PRISMA flow chart of study identification and selection.
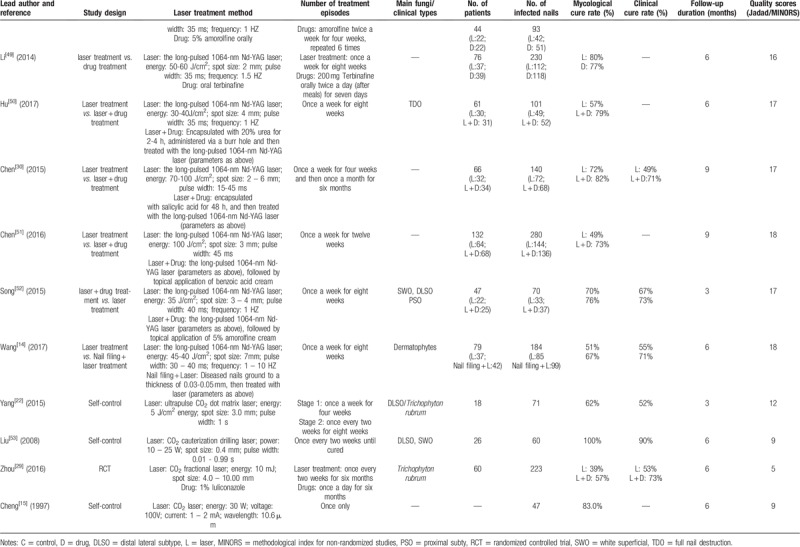
Table 1.
Characteristics of studies included in the meta-analysis.
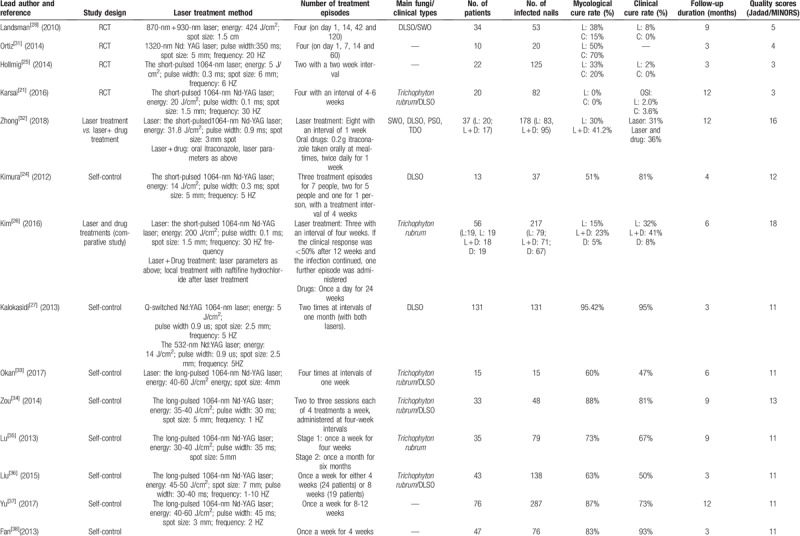
Table 1 (Continued).
Characteristics of studies included in the meta-analysis.
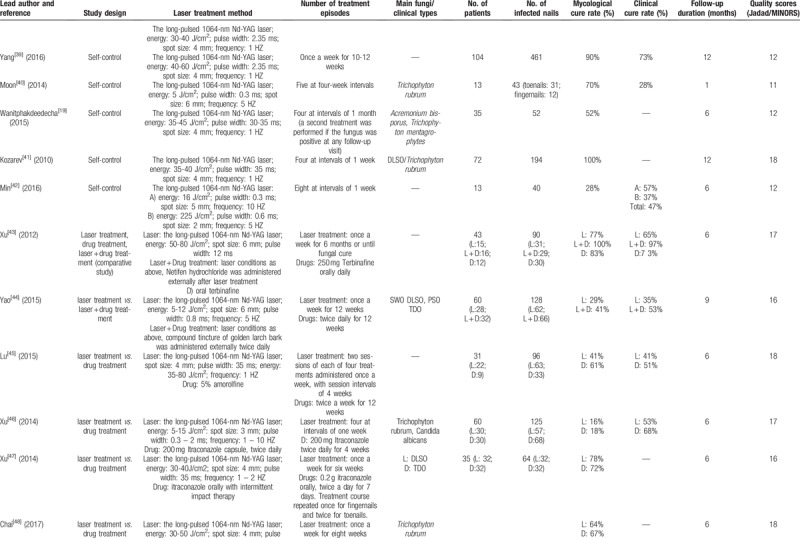
Table 1 (Continued).
Characteristics of studies included in the meta-analysis.
3.2. Meta-analysis of extracted data on laser treatment of onychomycosis
The results of the meta-analysis are shown in Figure 2. All 35 included studies reported the efficacy of laser treatment on onychomycosis. There was statistical heterogeneity among the data from the different studies (P < .01, I2 > 50%), so the random effects model (REM) was used for data analysis. The results of this analysis revealed that the overall mycological cure rate of laser treatment was 63.0% (95% CI 0.53-0.73), as shown in Figure 2. The percentage cure rates of the various subtypes of laser treatment methodology employed in the included studies are shown in Figure 3. The mycological cure rate of long pulse width 1064-nm Nd:YAG laser treatment was 71.0% (95% CI 0.62-0.80); the mycological cure rate of short pulse width 1064-nm Nd:YAG laser treatment was 21.0% (95% CI 0.05 - 0.44); the mycological cure rate of CO2 fractional laser treatment was 45.0% (95% CI 0.32-0.58); and the mycological cure rate of perforated CO2 laser treatment was 95.0% (95% CI 0.67-1.00).
Figure 2.
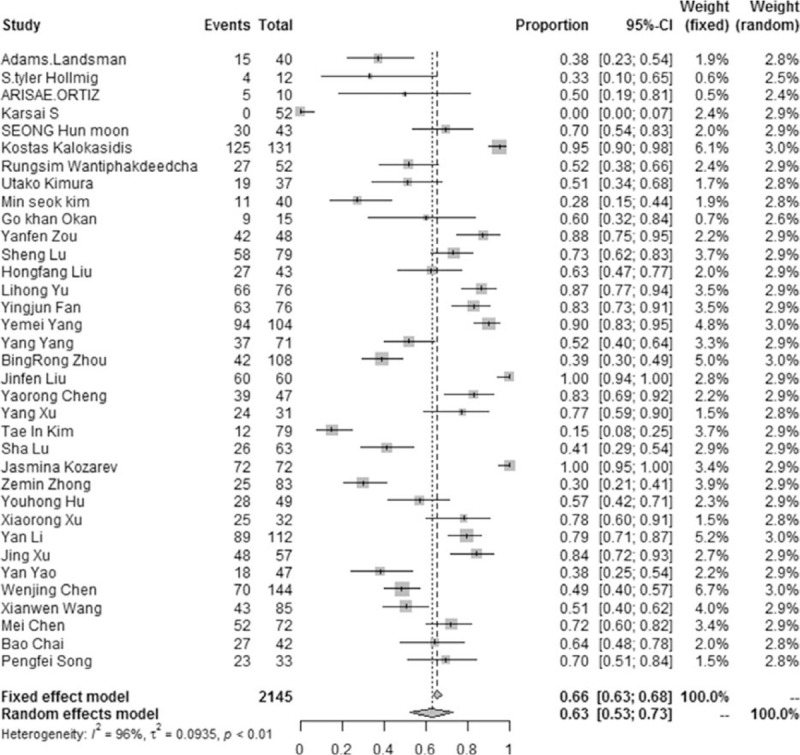
Results (forest plot) of meta-analysis of data extracted from studies on the efficacy of laser treatment for curing onychomycosis.
Figure 3.
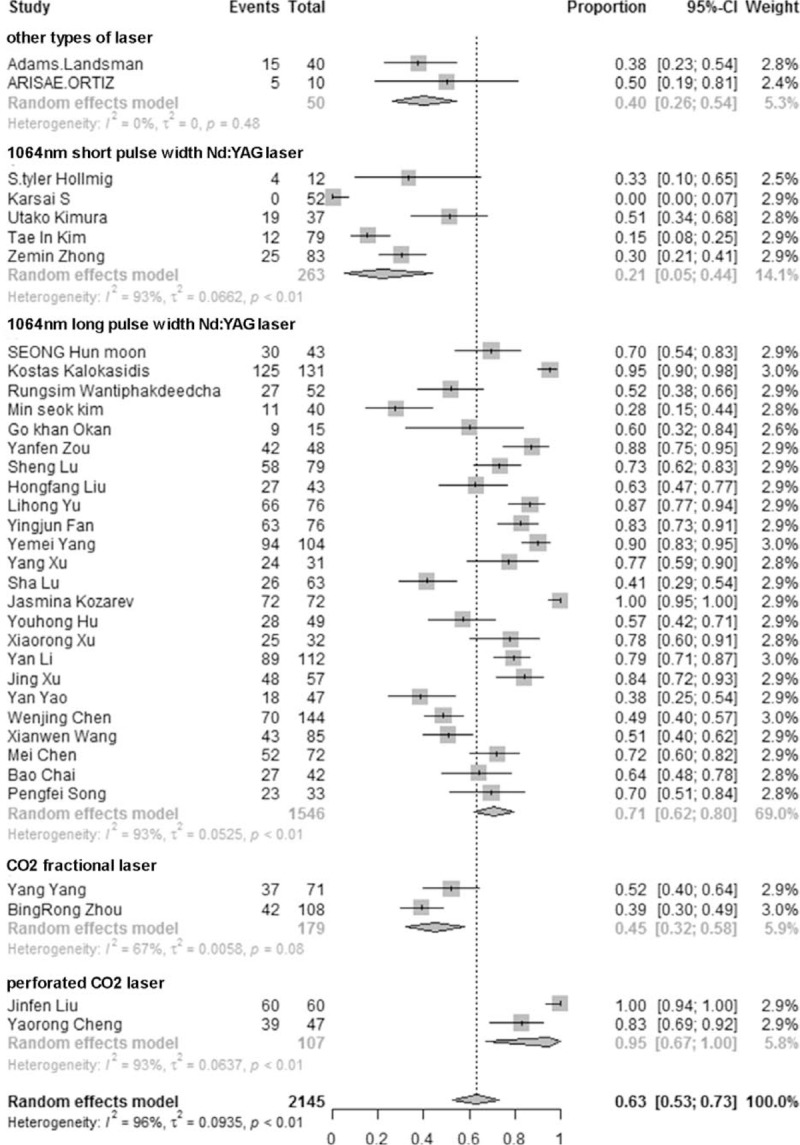
Comparison of the percentage cure rates of different types of laser treatment: 1064-nm Nd: YAG laser (long pulse and short pulse) treatment, CO2 laser treatment (fractional and perforated) with 870-nm and 930-nm lasers, and other types of laser treatment.
3.3. Adverse effects
Among the 35 included studies, 1 reported that the affected nails were filed to a thickness of 0.03 to 0.05 mm prior to laser treatment. In one study, subsequent hemorrhage occurred after treatment and subsided after 2 weeks.[14] After reducing the laser energy density, there was no evidence of bleeding.[14] Laser treatment with CO2 resulted in a larger wound on the nail deck and nail bed and the formation brown eschar, which can readily hemorrhage.[15] The majority of patients in the included studies reported experiencing a mild to moderate burning sensation during laser treatment, which was tolerable. There were no serious adverse reactions.
3.4. Publication bias
The constructed funnel plot is presented in Figure 4. There was no evidence of obvious publication bias among the included studies.
Figure 4.
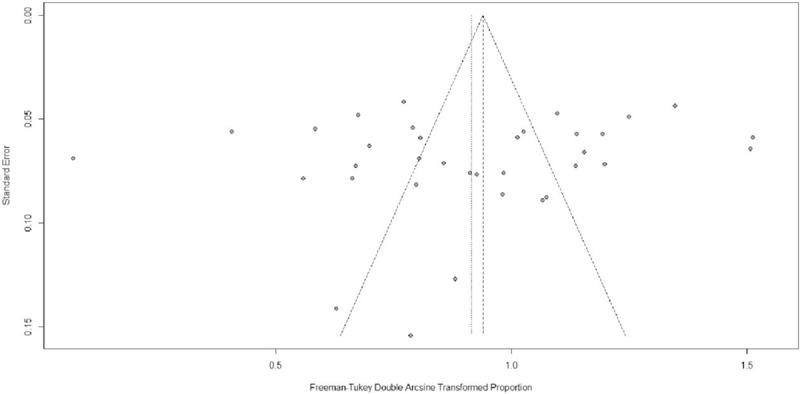
Funnel plot of studies evaluating the effects of laser treatment on onychomycosis, to assess publication bias.
4. Discussion:
The meta-analysis performed in this study was conducted on data extracted from 35 articles, including 5 RCT studies, 1723 patients and 4278 diseased nails. The included studies did not show evidence of publication bias and the risk of selective reporting was determined as being low. The majority of the included studies were scored as being of medium quality or above. In general, the analysis revealed that the efficacy of laser treatment of onychomycosis was approximately 63%. In comparison, the mycological efficacy of itraconazole pulse therapy and continuous terbinafine therapy for the treatment of onychomycosis were 79.6% and 84.8%, respectively.[16] Thus, the overall efficacy of laser treatment was moderately lower than that of conventional oral drug treatments, but it produced less reported side effects, such as damage to the liver and kidney or gastrointestinal reactions.[17] Further, the data suggested that laser treatment appeared to be more suitable for certain population subgroups, such as children, the elderly and pregnant women.
The efficacy of CO2 laser-treatment was found to be slightly higher than that of 1064-nm Nd: YAG laser treatment for curing onychomycosis. This may be because whilst the 1064-nm laser inhibits the growth of the fungus, the CO2 laser can increase the localized temperature and gasify and decompose the infected tissue and have a sterilizing effect.[18] However, differences between the number of included cases within each of these treatment groups may have influenced the result. The long-pulsed 1064-nm Nd:YAG laser exhibited better efficacy than the short-pulsed 1064-nm Nd:YAG laser. Rungsima et al considered the long-pulsed 1064-nm laser to be more easily absorbed by melanocytes, giving rise to better therapeutic results.[19] The cytoderm of Trichophyton fungi contains a large amount of melanin, and the absorption spectrum of its chromophore is 1064 nm. This means that the long-pulsed 1064-nm Nd:YAG laser can act directly on the chromophore, resulting in a localized increase in temperature and subsequent destruction of the fungi. On the other hand, the short-pulsed 1064-nm Nd:YAG laser acts on the diseased nail, causing tiny bubbles to form and producing sonic shock waves which can significantly inhibit the growth of the fungal colony.[20] Karsai et al reported that short-pulsed 1064-nm Nd:YAG laser treatment had no effect on either the mycological cure rate or on clinical improvement of onychomycosis caused by T. rubrum. It may be that the longer follow-up period of the RCT study (12 months) led to a relatively high recurrence rate or that there was a decrease in the number of potential target chromophores which affected (reduced) the laser-tissue interaction.[21]
The present analysis also revealed that the efficacy of CO2 perforated laser treatment was superior to that of CO2 fractional laser treatment in curing onychomycosis. Among the analyzed studies, the cure rate produced by CO2 fractional laser treatment was 45%, while the cure rate of CO2 perforated laser treatment was 95%. Further, the bacteriostatic and sterilizing effects of CO2 laser treatment did not appear to produce the types of side effects reported for the conventional oral drug therapies. On this basis, Yang et al considered that the efficacy of fractional CO2 laser treatment could be improved by extending the duration of treatment.[22] Because of its photothermal effect, perforated CO2 laser treatment can gasify and entirely decompose the infected tissue, which is likely to achieve a better long-term effect due to improved sterilization. However, compared to CO2 fractional laser treatment, CO2 perforated laser treatment produces a higher localized temperature, which can be difficult to control in terms of the depth of laser penetration into the tissue, and which can therefore result in larger wounds, forming a brown eschar and higher risk of bleeding. It is therefore necessary to avoid excessive pursuit of curative effects where the treatment itself may cause excessive clinical damage of the nail bed and deck.
The efficacy of laser treatment in curing onychomycosis depends significantly on the health condition of the patient and on the course of treatment being completed. Carney et al showed that grinding of the diseased nail before treatment in order achieve a thickness of less than 2 mm was conducive to laser penetration.[23] Where more than 50% of the diseased nail is affected, malnutrition of the nail and/or invasion of the nail matrix have a detrimental effect on the prognosis following laser treatment. In all except five of the included articles,[15,24,25,26,27] the laser treatment was repeated at least 4 times. It is therefore considered that changing the treatment duration and the total length of the treatment course could improve the mycological cure rate and clinical efficacy of laser treatment of onychomycosis. In addition to the 1064-nm Nd:YAG laser and CO2 laser, Landsman et al used 870-nm and a 930-nm lasers to treat severe onychomycosis and this produced a mycological cure rate of only 38%.[28] Ortiz et al used a 1320-nm Nd:YAG laser to treat onychomycosis but reported that this produced a lower curative efficacy than the control group.[17] For this reason, 1064-nm Nd:YAG lasers and CO2 lasers are more commonly used than 1320-nm Nd:YAG lasers. It is worth noting that many studies found that the mycological and clinical efficacy of laser treatment combined with topical drugs was significantly higher than that produced by laser treatment alone,[29,30] which may be related to the effects of laser treatment in enabling the drugs to penetrate deeper into the nail deck. Yang et al similarly reported that the combination of oral drug therapy and laser treatment was more effective than administering laser treatment or drug therapy alone.[30]
The results of the present study have certain limitations: The methods employed in the included studies were heterogeneous. The subjects included in the studies also differed in basic characteristics such as age, duration of disease and duration of follow-up. Because of these differences, despite the present analysis more randomized controlled trials are needed to verify the findings regarding the efficacy of laser treatment for onychomycosis.
5. Conclusion
Laser treatment (using a 1064-nm Nd: YAG laser or perforated CO2 laser) for the treatment of onychomycosis has a high mycological cure rate and high safety record, and can be used successfully for the treatment and cure of onychomycosis.
Author contributions
Data curation: Weiwei Ma, Chenchen Si.
Formal analysis: Chenchen Si, Juan Liu, Yang Xu.
Methodology: Lorna Martin Kasyanju Carrero, Hou-fang Liu, Xu-Feng Yin.
Writing – original draft: Weiwei Ma.
Writing – review & editing: Bingrong Zhou.
Footnotes
Abbreviations: CNKI = china national knowledge internet, RCT = randomized controlled trial, REM = random effects model, MINORS = methodological index for non-randomized studies.
How to cite this article: Ma W, Si C, Kasyanju Carrero LM, Liu HF, Yin XF, Liu J, Xu Y, Zhou B. Laser treatment for onychomycosis: a systematic review and meta-analysis. Medicine. 2019;98:48(e17948).
WM and CS contribute equally to the manuscript.
This work was supported by grants from the China National Natural Science Foundation (81573072) and the Priority Academic Program Development (PAPD) of Jiangsu Higher Education Institutions. Bingrong Zhou is funded by the project of key youth medical talent of Jiangsu Province (QNNRC 2016583) and outstanding young backbone teachers of Nanjing Medical University (2017).
The authors have no conflicts of interest to disclose.
References
- [1].Sigurgeirsson B, Baran R. The prevalence of onychomycosis in the global population – A literature study. J Eur Acad Dermatol Venereol 2015;28:1480–91. [DOI] [PubMed] [Google Scholar]
- [2].Hay RJ, Baran R. Onychomycosis: Aproposed revision of the clinical classification. J Am Acad Dermatol 2011;65:1219. [DOI] [PubMed] [Google Scholar]
- [3].Crawford F, Young P, Godfrey C, et al. Oral treatments for toenail onychomycosis: a systematic review. Arch Dermatol 2002;138:811–6. [DOI] [PubMed] [Google Scholar]
- [4].Elewski BE. A full “cure” for onychomycosis is not always possible. Arch Dermatol 1999;135:852–3. [DOI] [PubMed] [Google Scholar]
- [5].Gupta AK. Ciclopirox nail lacquer: a brush with onychomycosis. Cutis 2001;68:13–6. [PubMed] [Google Scholar]
- [6].Katz HI. Drug interactions of the newer oral antifungal agents. Brit J Dermatol 1999;141:26–32. [DOI] [PubMed] [Google Scholar]
- [7].Grover C, Bansal S, Nanda S, et al. Combination of surgical avulsion and topical therapy for single nail onychomycosis: a randomized controlled trial. Brit J Dermatol 2007;157:364–8. [DOI] [PubMed] [Google Scholar]
- [8].Apfelberg DB, Rothermel E, Widtfeldt A, et al. Preliminary report on use of carbon dioxide laser in podiatry. J Am Podiatry Assoc 1984;74:509–13. [DOI] [PubMed] [Google Scholar]
- [9].Ledon JA, Savas J, Franca K, et al. Laser and light therapy for onychomycosis: a systematic review. Laser Med Sci 2014;29:823–9. [DOI] [PubMed] [Google Scholar]
- [10].Ortiz AE, Avram MM, Wanner MA. A review of lasers and light for the treatment of onychomycosis. Laser Surg Med 2014;46:117–24. [DOI] [PubMed] [Google Scholar]
- [11].Bristow IR. The effectiveness of lasers in the treatment of onychomycosis: a systematic review. J Foot Ankle Res 2014;7:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 1996;17:1–2. [DOI] [PubMed] [Google Scholar]
- [13].Slim K, Nini ED, Kwiatkowski F, et al. Methodological index for non-randomized studies (minors): development and validation of a new instrument. Anz J Surg 2003;73:712–6. [DOI] [PubMed] [Google Scholar]
- [14].Wang XW, Chen JH, Chen CX, et al. The observation of efficacy of the long-pulsed 1064-nm Nd: YAG laser combined with filing nails away treatment for onychomycosis. J Diagn Therap Dermato-venereol 2017;6:398–402. [Google Scholar]
- [15].Cheng YR, Wang CY, Cao LF, et al. Clinical observation of CO2 laser treatment for onychomycosis. Chin J Dermatovenereol 1997;53–4. [Google Scholar]
- [16].Wang L, Li W, Xue HH, et al. Systematic evaluation of efficacy and safety of antifungal drugs in the treatment of onychomycosis. Med Pharmaceut J Chin People's Liber Army 2016;01: 62-65+95. [Google Scholar]
- [17].Ortiz AE, Truong S, Serowka K, et al. A 1,320-nm Nd: YAG laser for improving the appearance of onychomycosis. Dermatol Surg 2014;40:1356–60. [DOI] [PubMed] [Google Scholar]
- [18].Xu J, Zhuo FL, Zhang RN, et al. The progress in laser treatment for onychomycosis. Chin J Laser Med Surg 2013;41–4. [Google Scholar]
- [19].Wanitphakdeedecha R, Thanomkitti K, Bunyaratavej S, et al. Efficacy and safety of 1064-nm Nd:YAG laser in treatment of onychomycosis. J Dermatol Treat 2015;27:75–9. [DOI] [PubMed] [Google Scholar]
- [20].Hochman LG. Laser treatment of onychomycosis using a novel 0.65-millisecond pulsed Nd:YAG 1064-nm laser. J Cutaneous Laser Therap 2011;13:2–5. [DOI] [PubMed] [Google Scholar]
- [21].Karsai S, Jäger M, Oesterhelt A, et al. Treating onychomycosis with the short-pulsed 1064-nm-Nd: YAG laser: results of a prospective randomized controlled trial. J Eur Acad Dermatol 2017;31:175–80. [DOI] [PubMed] [Google Scholar]
- [22].Yang Y, Liu H, Yang RY, et al. The observation of efficacy of Ultrapulse CO2 fractional laser treatment for onychomycosis. Chin J Dermatol 2015;526–30. [Google Scholar]
- [23].Carney C, Cantrell W, Warner J, et al. Treatment of onychomycosis using a submillisecond 1064-nm neodymium:yttrium-aluminum-garnet laser. J Am Acad Dermatol 2013;69:578–82. [DOI] [PubMed] [Google Scholar]
- [24].Kimura U, Takeuchi K, Kinoshita A, et al. Treating onychomycoses of the toenail: clinical efficacy of the sub-millisecond 1,064 nm Nd: YAG laser using a 5 mm spot diameter. J Drugs Dermatol 2012;11:496–504. [PubMed] [Google Scholar]
- [25].Hollmig ST, Rahman Z, Henderson MT, et al. Lack of efficacy with 1064-nm neodymium: yttrium-aluminum-garnet laser for the treatment of onychomycosis: a randomized, controlled trial. J Am Acad Dermatol 2014;70:911–7. [DOI] [PubMed] [Google Scholar]
- [26].Kim TI, Shin MK, Jeong K, et al. A randomised comparative study of 1064 nm Neodymium-doped yttrium aluminium garnet (Nd:YAG) laser and topical antifungal treatment of onychomycosis. Mycoses 2016;59:803–10. [DOI] [PubMed] [Google Scholar]
- [27].Kalokasidis K, Onder M, Trakatelli M, et al. The Effect of Q-Switched Nd:YAG 1064 nm/532 nm Laser in the Treatment of Onychomycosis In Vivo. Dermatol Res Pract 2013;2013:1–0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Landsman AS, Robbins AH. Treatment of mild, moderate, and severe onychomycosis using 870- and 930-nm light exposure: some follow-up observations at 270 days. J Am Podiatr Med Assoc 2012;102:169–71. [DOI] [PubMed] [Google Scholar]
- [29].Zhou BR, Lu Y, Permatasari F, et al. The efficacy of fractional carbon dioxide (CO2) laser combined with luliconazole 1% cream for the treatment of onychomycosis. Medicine 2016;95:e5141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Chen M, Zhang JD, Dong ZB. The assessment of efficacy of the long-pulsed 1064-nm Nd: YAG Laser combined with Salicylic acid treatment for onychomycosis. China J Leprosy Skin Dis 2015;685–8. [Google Scholar]
- [31].Ortiz AE, Truong S, Serowka K, et al. A 1320-nm Nd: YAG laser for improving the appearance of onychomycosis. Dermatol Surg 2014;40:1356–60. [DOI] [PubMed] [Google Scholar]
- [32].Zhong ZM, Yang YM, Zhou ST, et al. The 0.9ms-pulsed 1064-nm Nd: YAG laser treatment for toenail mycosis. J South Med Univ 2018;358–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Okan G, Tarikci N, Gokdemir G. The effect of long-pulsed Nd: YAG laser for the treatment of onychomycosis. J Am Podiat Med Assn 2017;107:54–9. [DOI] [PubMed] [Google Scholar]
- [34].Zou YF, Ye TL, Zhong QL, et al. Clinical observation on 33 cases of onychomycosis treated with the long-pulsed 1064-nm Nd: YAG laser. Chin J Dermatovenereol 2014;581–3. [Google Scholar]
- [35].Lu S, Zhang Z, Fei Y, et al. Observation of efficacy of long pulse width Nd: YAG laser treatment for onychomycosis. Chin J Dermatol 2013;46:105–8. [Google Scholar]
- [36].Liu HF, Huang LN, Chen YJ, et al. Observation of efficacy of the long-pulsed 1064-nm Nd: YAG Laser treatment for onychomycosis with different courses. J Diagn Therap Dermato-venereol 2015;22:185–8. [Google Scholar]
- [37].Yu LH, Wang YJ, Fang QH, et al. Observation of efficacy of Nd: YAG Laser treatment for onychomycosis. Chin Health Nutr 2017;27:112–3. [Google Scholar]
- [38].Fing J. Observation of the efficacy of the long-pulsed 1064-nm Nd: YAG Laser treatment for onychomycosis. Chin J Modern Drug Appl 2013;7:50–1. [Google Scholar]
- [39].Yang YM, Zhou ST, Hu YX, et al. The efficacy and safety of the long-pulsed 1064-nm Width Nd: YAG laser treatment for toenail mycosis. J South Med Univ 2016;36:693–6. [PubMed] [Google Scholar]
- [40].Moon SH, Hur H, Oh YJ, et al. Treatment of onychomycosis with a 1,064-nm long-pulsed Nd: YAG laser. J Cosmet Laser Ther 2014;16:165–70. [DOI] [PubMed] [Google Scholar]
- [41].Kozarev J, Vižintin Z. Novel laser therapy in treatment of onychomycosis. J Laser Health Acad 2010;1:1–9. [Google Scholar]
- [42].Kim MS, Jung JY, Cho EB, et al. The effectiveness of 1,064-nm long-pulsed Nd: YAG laser in the treatment of severe onychomycosis. J Cosmet Laser Ther 2016;18:317–22. [DOI] [PubMed] [Google Scholar]
- [43].Xu Y, Miao X, Zhou B, et al. Combined oral terbinafine and long-pulsed 1064-nm Nd. Dermatol Surg 2014;40:1201–7. [DOI] [PubMed] [Google Scholar]
- [44].Yao Y, Wang XH. Clinical Observation on 60 Cases of toenail mycosis in elderly patients treated with the long-pulsed 1064-nm Nd: YAG Laser combined with compound tincture of golden larch bark. Pract Geriatr 2015;10:810–3. [Google Scholar]
- [45].Lu S, Zhang J, Liang Y, et al. The efficacy and prognostic factors for long pulse neodymium: yttrium-aluminum-garnet laser treatment on onychomycosis: a pilot study. Ann Dermatol 2016;28:406–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Xu J, Zhuo FL, Zhang RN, et al. Short-term efficacy analysis of 1064-nm Nd: YAG laser combined with itraconazole treatment for mild to moderate onychomycosis. Chin J Mycol 2014;9:20–3. [Google Scholar]
- [47].Xu XR, Lai AM, Zheng JB, et al. The observation of efficacy of 1064-nm Nd: YAG laser treatment for onychomycosis. China Trop Med 2014;14:1246–8. [Google Scholar]
- [48].Chai B, Wang P, Xu LH, et al. The study of efficacy of the long-pulsed 1064-nm Nd: YAG Laser treatment for onychomycosis. Guangdong Trace Element Sci 2017;24:17–22. [Google Scholar]
- [49].Li Y, Yu S, Xu J, et al. Comparison of the efficacy of long-pulsed Nd: YAG laser intervention for treatment of onychomycosis of toenails or fingernails. J Drugs Dermatol 2014;13:1258–63. [PubMed] [Google Scholar]
- [50].Hu YH, Tu XS, Yi QY, et al. The effect of 20% urea-encapsulated on the long-pulsed 1064-nm Nd: YAG Laser treatment for onychomycosis. Chin J Aesth Med 2017;26:106–8. [Google Scholar]
- [51].Chen WJ, Ilyur M, Zou XH, et al. The evaluation of efficacy of the long-pulsed 1064-nm Nd: YAG Laser combined with concentrated benzoic acid ointment treatment for onychomycosis. Xinjiang Med J 2016;46:1152–5. [Google Scholar]
- [52].Song PF, Xu J, Qin H, et al. The evaluation of efficacy of the long-pulsed 1064-nm Nd: YAG Laser combined with amorofen treatment for onychomycosis. J Diagnos Therap Dermato-venereol 2015;22:432–4. [Google Scholar]
- [53].Liu JF. The observation of efficacy of 26 cases of CO2 laser treatment for onychomycosis. Chin J Mycol 2008;03:289–91. [Google Scholar]


