Abstract
It is common to measure continuous outcomes using different scales (eg, quality of life, severity of anxiety or depression), therefore these outcomes need to be standardized before pooling in a meta-analysis. Common methods of standardization include using the standardized mean difference, the odds ratio derived from continuous data, the minimally important difference, and the ratio of means. Other ways of making data more meaningful to end users include transforming standardized effects back to original scales and transforming odds ratios to absolute effects using an assumed baseline risk. For these methods to be valid, the scales or instruments being combined across studies need to have assessed the same or a similar construct
Summary points.
When an outcome is measured using several scales (eg, quality of life or severity of anxiety or depression), it requires standardization to be pooled in a meta-analysis
Common methods of standardization include using the standardized mean difference, converting continuous data to binary relative and absolute association measures, the minimally important difference, the ratio of means, and transforming standardized effects back to original scales
The underlying assumption in all these methods is that the different scales measure the same construct
Clinical scenario
A child and her parent present to the clinic to discuss anxiety symptoms that the child has had for over a year. The therapist talks with the parent and child about the possibility of starting a selective serotonin reuptake inhibitor (SSRI). A systematic review comparing SSRIs with placebo has shown that SSRIs reduce anxiety symptoms by a standardized mean difference (SMD) of −0.65 (95% confidence interval −1.10 to −0.21).1 2 The therapist finds these results difficult to interpret and not easy to explain to the parent and child.
The problem
Outcomes of importance to patients such as quality of life and severity of anxiety or depression are often measured using different scales. These scales can have different signaling questions, units, or direction. For example, when comparing the effect of two cancer treatments on quality of life, trials can present their results using the short form health survey 36, the short form health survey 12, the European quality of life five dimensions, or others. Trials may also present their results as binary outcomes (proportion of patients who had improved quality of life in each trial arm). Decision makers need to know the best estimate of the impact of interventions on quality of life. The best estimate for decision makers is usually the pooled estimate (that is, from a meta-analysis), which has the highest precision (narrower confidence intervals).
Pooling outcomes across studies is challenging because they are measured using different scales. Pooling the results of each scale independently is undesirable because it does not allow all the available evidence to be included and can lead to imprecise estimates (only a few studies would be included in each analysis, leading to an overall small sample size and wide confidence intervals). As long as the different scales represent the same construct (eg, severity of anxiety), pooling outcomes across studies is needed.
In this guide, we describe several approaches for meta-analyzing outcomes measured using multiple scales. The methods used can be applied before the meta-analysis (to individual study estimates that are then meta-analyzed), after the meta-analysis and generation of the SMD, or they can be based on individual trial summary statistics and established minimally important differences (MIDs) for all instruments.3 We present a simplified approach focused on the general concepts of the SMD, the ratio of means (ROM), the MID, and conversion to relative and absolute binary measures.
For each approach, we describe the method used and the associated assumptions (fig 1). We apply these methods to a dataset of five randomized trials comparing SSRIs with placebo (table 1). These trials used different anxiety scales and one trial presented its results as a binary outcome. We use this dataset to show the common approaches described in this guide and how the clinical scenario was addressed by providing an interpretation (a narrative) to convey the results to end users such as clinicians and patients.
Fig 1.
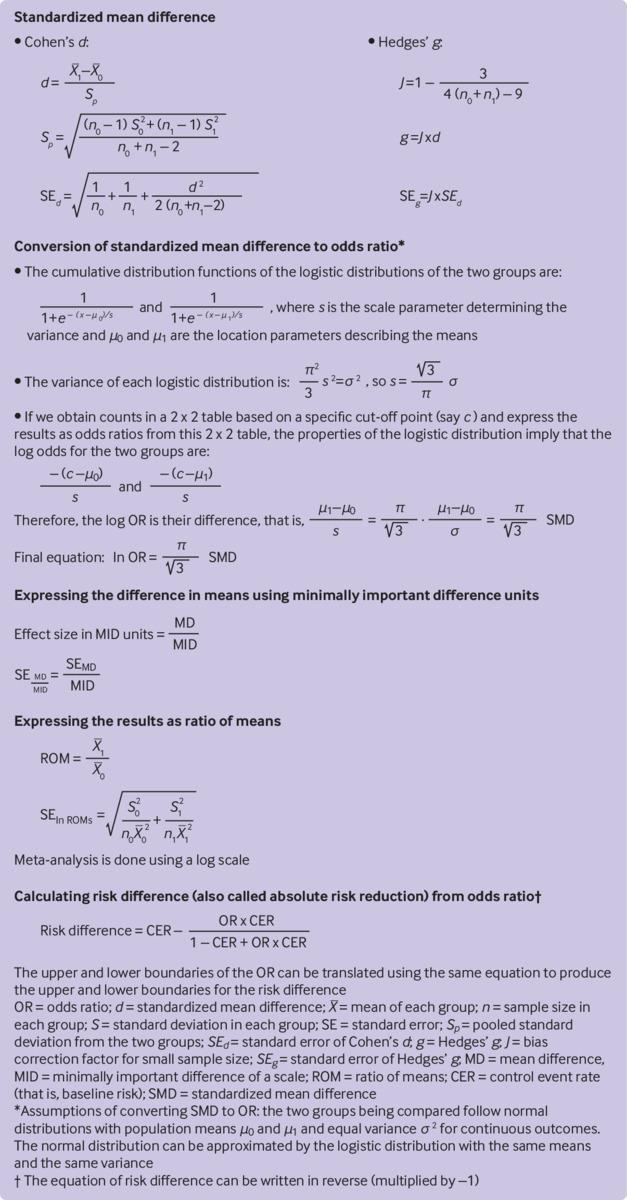
Calculations for the different methods used to standardize outcomes measured using different scales
Table 1.
Data from five trials evaluating SSRIs for childhood anxiety (fictitious)
| Trial | SSRIs | Placebo | Scale | |||
|---|---|---|---|---|---|---|
| Sample size | Mean (SD) | Sample size | Mean (SD) | |||
| Trials presenting results as continuous outcomes: | ||||||
| Trial 1 | 100 | 8 (4) | 100 | 12 (3) | Pediatric anxiety rating scale | |
| Trial 2 | 250 | 7.5 (3) | 250 | 11 (2) | Pediatric anxiety rating scale | |
| Trial 3 | 200 | 20 (15) | 200 | 35 (15) | Screen for child anxiety related emotional disorders | |
| Trial 4 | 150 | 21 (11) | 150 | 31 (12) | Screen for child anxiety related emotional disorders | |
| Trial presenting results as binary outcomes: | ||||||
| Trial 5 | 300 | 150* | 300 | 100* | No scale data | |
SSRI=selective serotonin reuptake inhibitor.
Number who improved.
SMD
A common approach for combining outcomes from studies that used different scales is to standardize the outcomes (that is, express outcomes in multiples of standard deviations), which makes the outcomes unitless (or have the same unit, the standard deviation). This approach consists of dividing the mean difference between the intervention and control in each study by the study’s pooled standard deviation of the two groups, which allows the studies to be combined and a pooled SMD to be generated. The SMD is justified based on one of the following two arguments. Firstly, outcome measures across studies may be interpreted as linear transformations of each other. Secondly, the SMD may be considered to be the difference between two distributions of distinct clusters of scores, even if these distributions did not measure exactly the same outcomes.4 Therefore, for the standard deviation to be used as a scaling factor, between-study variation in standard deviations is assumed to only reflect differences in measurement scales and not differences in the reliability of outcome measures or variability among study populations.5 However, this assumption cannot always be met. For example, when a meta-analysis includes pragmatic and explanatory trials, pragmatic trials are expected to have more variation in the study population and higher standard deviations.5
Figure 1 shows two commonly used methods to derive the SMD: Cohen’s d and Hedges’ g. Hedges’ g includes a correction for small sample size.6 Small sample size can lead to biased overestimation of the SMD.4 The SMD method can be complemented by three additional approaches.
Provide a judgment about size of effect
Meta-analysts can provide end users with the commonly used arbitrary cut-off points for the magnitude of a standardized effect. SMD cut-off points of 0.20, 0.50, and 0.80 can be considered to represent a small, moderate, and large effect, respectively.7
Transform SMD to odds ratio
Continuous outcome measures such as the SMD can be converted to odds ratios. Although several approaches are available, the most commonly used method is to multiply the SMD by π/√3 (about 1.81) to produce the natural logarithm of the odds ratio.8 9 This conversion from the SMD to the odds ratio can be performed by some statistical software packages.4 The main advantage of this approach is the ability to combine studies that present the outcome in a binary fashion (that is, number of responders) with studies that present the results on a continuous scale. Figure 1 presents the assumptions and an explanation for this approach.
Interpretation of this odds ratio is challenging. The Cochrane Handbook for Systematic Reviews of Interventions 5 implies that the odds ratio refers to an improvement by some unspecified amount. Based on the characteristics of logistic distribution, which indicate that the calculated odds ratio is invariant to the cut-off point (fig 1), we propose that this odds ratio can be interpreted as follows: the ratio of the odds of patients with a measure higher than any specific cut-off point to those with a lower measure. Therefore, this odds ratio applies to any cut-off point of the continuous data. The cut-off point defining the magnitude of improvement on the various anxiety scales can be determined by practitioners to represent a meaningful change.
Back transform SMD to an original scale
SMDs can be made more clinically relevant by translating them back to scales with which clinicians are more familiar. This rescaling is done by simply multiplying the SMD generated from the meta-analysis by the standard deviation of the specific scale. The results are then given in the natural units of a scale, which allows a more intuitive interpretation by end users. The standard deviation used here is the pooled standard deviation of baseline scores in one of the included trials (the largest or most representative) or the average value from several of the trials, or from a more representative observational study.5
It is also possible to perform this rescaling on the results of each individual trial before conducting the meta-analysis; the meta-analysis can then be performed using the transformed values.3
Box 1 shows the SMD based methods applied to the example of anxiety in children.
Box 1. Standardized mean difference (SMD) based methods applied to the example of selective serotonin reuptake inhibitors (SSRIs) for anxiety in children*.
SMD
Method: the first four trials in table 1 provide the mean, standard deviation, and sample size for each study arm; however, the trials used two different scales. Data from each trial are standardized by dividing the difference in means by the pooled standard deviation (pooled from the intervention and control groups). The odds ratio from the fifth trial is 2.00 (95% confidence interval 1.44 to 2.78) by using the equation ln(odds ratio)=π/√3(fig 1) and multiplying by –1 (because the odds ratio is for improvement whereas the scales measure anxiety symptoms, and a higher score suggests worsening of symptoms). This odds ratio is converted to an SMD of –0.38 (95% confidence interval –0.56 to –0.20). SMDs of all five trials were pooled in a random effects meta-analysis to give a final SMD of –0.97 (95% confidence interval –1.34 to –0.59)
Interpretation:
Compared with no treatment, SSRIs reduce anxiety symptoms by 0.97 standard deviations of anxiety scales
Compared with no treatment, the reduction in anxiety symptoms associated with SSRIs is consistent with a large effect
Odds ratio derived from SMD
Method: this pooled SMD of the five trials can also be expressed as an odds ratio using the equation ln(odds ratio)=π/√3(fig 1); that is, an odds ratio of 5.75 (95% confidence interval 2.90 to 11.35)
Interpretation: the odds of improvement in anxiety symptoms after taking SSRIs are approximately six times higher compared with not taking SSRIs
Transformation to natural units
Method: the SMD can be transformed back to the natural units of the Pediatric Anxiety Rating Scale by multiplying it by the pooled standard deviation (pooled from the intervention and control groups in a trial that used this scale). This standard deviation can be obtained from the largest trial or as an average of the pooled standard deviations of the two trials, which here is 2.91. This multiplication gives a mean reduction of –2.81 (95% confidence interval –3.90 to –1.71)
Interpretation: compared with no treatment, SSRIs reduce anxiety symptoms by approximately three points on the Pediatric Anxiety Rating Scale
*All analyses use the DerSimonian-Laird random effect model (presuming that the assumptions of this model are met). For simplicity, the end-of-trial means in the two groups are compared (rather than comparing the change in means in the two groups).
MID
The MID is defined as “the smallest difference in score in the outcome of interest that informed patients or informed proxies perceive as important, either beneficial or harmful, and which would lead the patient or clinician to consider a change in the management.”10 Meta-analysts might consider expressing the outcomes of each study using MID units and then pooling the results (which now have the same unit, the MID) in the meta-analysis. Figure 1 shows the formula for this expression.
One advantage of the MID approach is to reduce heterogeneity (often a lower I2 value, which is the proportion of heterogeneity not attributable to chance11). Such heterogeneity observed with the SMD approach would have been caused by variability in the standard deviation across studies.12 A second advantage is that a more intuitive interpretation can be made by clinicians and patients.12 This approach requires the availability of published MID values for the scales used in the various studies. MIDs are determined using either anchor based methods (correlating the scale with other measures or clinical classifications that are independent and well established) or distribution based methods (MID is based either on variation between or within individuals, or the standard error of measurement).13 The MID is estimated to range from 0.20 to 0.50 standard deviations.13
Box 2 shows the MID based method applied to the example of anxiety in children.
Box 2. Minimally important difference (MID) method applied to the example of selective serotonin reuptake inhibitors (SSRIs) for anxiety in children*.
Method: assuming that the smallest change a patient can feel on the Pediatric Anxiety Rating Scale and on the Screen for Child Anxiety Related Emotional Disorders is 5 and 10 points, respectively, the mean difference in each study is divided by the corresponding MID to obtain the difference between the two groups in MID units. The standard error of the difference in MID units is then calculated (fig 1). The differences in MID units from each study are meta-analyzed using the random effects model to give a difference of –0.98 (95% confidence interval –1.27 to –0.69)
Interpretation: compared with no treatment, the reduction in anxiety symptoms associated with SSRI use is 0.98 of the minimal amount of improvement that a patient can feel
*All analyses use the DerSimonian-Laird random effect model (presuming that the assumptions of this model are met). For simplicity, the end-of-trial means in the two groups are compared (rather than comparing the change in means in the two groups).
ROM
Another simple and potentially attractive way to present the results of continuous outcomes is as a ROM, also called a response ratio in ecological research.14 When the means of the first group are divided by the mean of the second group, the resulting percentage is theoretically unitless. This percentage is easy to understand and can be combined across studies that have used different outcome instruments. Pooling is done on the log scale.15 Figure 1 shows the formula for this expression.
The ROM can also be imputed directly from the pooled SMD by using the simple equation ln(ROM)=0.392×SMD. This equation was derived empirically from 232 meta-analyses by using linear regression between the two measures (however, the coefficient of determination of that model was only R 2=0.62).16 The ROM is less frequently used in meta-analyses in medicine.
Box 3 shows the ROM based method applied to the example of anxiety in children.
Box 3. Ratio of means (ROM) method applied to the example of selective serotonin reuptake inhibitors (SSRIs) for anxiety in children*.
Method: in each study, the mean of anxiety symptoms in the group that received SSRIs is divided by the mean in the placebo group, giving a ROM. The standard error of the ROM is then calculated (fig 1). The natural logarithms of ROMs from each study are meta-analyzed using the random effects model and then exponentiated to give a pooled ROM of 0.66 (95% confidence interval 0.61 to 0.70)
Interpretation: the average scores on anxiety symptom scales for patients who used SSRIs are 66% of the average symptom scores for patients who did not use SSRIs (thus better)
*All analyses use the DerSimonian-Laird random effect model (presuming that the assumptions of this model are met). For simplicity, the end-of trial-means in the two groups are compared (rather than comparing the change in means in the two groups).
Conversion to binary relative and absolute measures
Various methods are available to convert continuous outcomes to probabilities, relative risks, risk differences, and odds ratios of treatment response and number needed to treat.3 17 For clinical decision making and guideline development, trade-offs of the desirable and undesirable effects of the intervention are facilitated by such conversion.18 19
We have described a common method for this conversion (multiplying the SMD by π/√3). This odds ratio can be converted to a risk difference (also called absolute risk reduction) or number needed to treat. Figure 1 shows the calculation for this conversion. The number needed to treat is the inverse of the risk difference. Other methods are available to convert SMD directly to risk difference and number needed to treat.3 17
Decision makers need to specify the source of the baseline risk, which can be derived from well conducted observational studies that enroll individuals similar to the target population. A less desirable but easy option is to obtain this baseline risk from the control arms of the trials included in the same meta-analysis (as a mean or median risk across trials). Another option is to derive the baseline risk from a risk prediction model, if available.20 Multiple baseline risks can be presented to decision makers so that different recommendations can be made for different populations. Software from the GRADE (grading of recommendations, assessment, development, and evaluation) Working Group (GRADEPro, McMasters University, Hamilton, Ontario, Canada) enables different absolute effects to be calculated and presented to help decision makers.21
Box 4 shows how the absolute effect is generated for the example of anxiety in children.
Box 4. Absolute effect generation.
Method: the odds ratio derived from the standardized mean difference in previous steps was used as the relative effect of selective serotonin reuptake inhibitors (SSRIs) (other ways to derive the odds ratio can also be used). A baseline risk (here, the likelihood of symptom improvement without SSRIs) is obtained from the placebo arm of the fifth trial: 100/300=0.33 (this baseline risk can also be derived from a better source that shows the clinical course of anxiety in children without treatment). By using the odds ratio and the baseline risk (fig 1), the resultant risk difference is 0.41
Interpretation: in 100 patients with anxiety who do not receive treatment, 33 will improve. However, when 100 patients with anxiety receive SSRIs, 74 will improve (difference of 41 attributable to treatment with SSRIs).
Discussion
Continuous outcomes such as quality of life scores, arthritis activity, and severity of anxiety or depression are important to patients and critical for making treatment choices. Meta-analysis of these outcomes provides more precise estimates for decision making but is challenged when individual studies use multiple instruments with different scales and units. Several methods are available to deal with this issue and include using the SMD, back transformation of the SMD to natural units, converting the SMD to an odds ratio, using MID units, using the ROM, or converting continuous outcomes to absolute effects using a baseline risk appropriate for the target population.
Each of these methods has statistical or conceptual limitations. The SMD is often associated with heterogeneity because of variation in the standard deviations across trials and has also been reported to be biased towards the null.12 22 The variance of the SMD, which impacts meta-analysis weights, is not independent of the magnitude of the SMD, as can be seen in the equation shown in figure 1. Larger SMDs tend to have larger variances and thus lower weights in inverse variance weighted meta-analysis, which may be another limitation.12 22 23
By using the MID, some of these statistical challenges may be reduced; however, the MID is not always known for many scales. When the SMD is converted to an odds ratio, empirical evaluation shows that at least four of five available methods have performed well and were consistent with each other (intraclass correlation coefficients were ≥0.90).17 Nevertheless, the assumptions of these methods vary and may not always be met. When the effect size is extreme, the conversion to an odds ratio may be poor. Some conversion methods can be considered exact methods using the normal distribution, which makes the resultant odds ratio dependent on the cut-off point17 and further complicates intuitive interpretation.
When results are converted to natural units (to the scale most familiar to end users), linear transformation may not be valid when the instruments have different measurement scales.3 Although the ROM has reasonable statistical properties,22 its assumptions are not always met (such as having outcome measures with natural units and natural zero values).4 The ROM cannot be used with change data, which can have a negative value.3 The ROM is also criticized for having a multiplicative nature, which is appealing for clinicians and patients because treatments are often discussed in these terms, but this interpretation may not be appropriate.24 The limitation of having different ROMs calculated in studies with similar absolute change is shared with other relative association measures (such as odds ratio and relative risk). Although methods for establishing certainty in baseline risk have been proposed, they have not been widely used.25
Not all of the described methods have been implemented in the commonly used meta-analysis software packages and may require statistical coding. It is important to reiterate that for any of these methods to be valid, the scales or instruments being combined across studies need to have assessed the same or a similar construct.
Contributors: All authors contributed to the design of the manuscript and interpretation of the data. MHM developed the first draft and ZW, HC, and LL critically revised the manuscript and approved the final version. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. MHM is the guarantor.
Funding: This research did not receive any specific grant from any funding agency in the public, commercial, or not-for-profit sector. HC is supported in part by the National Library of Medicine (R21 LM012197, R21 LM012744), and the National Institute of Diabetes and Digestive and Kidney Diseases (U01 DK106786). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Wang Z, Whiteside SPH, Sim L, et al. Comparative Effectiveness and Safety of Cognitive Behavioral Therapy and Pharmacotherapy for Childhood Anxiety Disorders: A Systematic Review and Meta-analysis. JAMA Pediatr 2017;171:1049-56. 10.1001/jamapediatrics.2017.3036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang Z, Whiteside SPH, Sim L, et al. Anxiety in Children. Rockville (MD): Agency for Healthcare Research and Quality (US); 2017 Aug. Report No.: 17-EHC023-EF. www.ncbi.nlm.nih.gov/books/NBK476277/
- 3. Thorlund K, Walter SD, Johnston BC, Furukawa TA, Guyatt GH. Pooling health-related quality of life outcomes in meta-analysis-a tutorial and review of methods for enhancing interpretability. Res Synth Methods 2011;2:188-203. 10.1002/jrsm.46. [DOI] [PubMed] [Google Scholar]
- 4. Borenstein M, Hedges L, Higgins J, et al. Introduction to Meta-analysis. John Wiley and Sons, 2009. 10.1002/9780470743386. [DOI] [Google Scholar]
- 5. Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Wiley-Blackwell, 2008. 10.1002/9780470712184. [DOI] [Google Scholar]
- 6. Hedges L, Olkin I. Statistical Methods for Meta-Analysis. Academic Press, 1985. [Google Scholar]
- 7. Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed Lawrence Erlbaum Associates, 1988. [Google Scholar]
- 8. Chinn S. A simple method for converting an odds ratio to effect size for use in meta-analysis. Stat Med 2000;19:3127-31. [DOI] [PubMed] [Google Scholar]
- 9. Hasselblad V, Hedges LV. Meta-analysis of screening and diagnostic tests. Psychol Bull 1995;117:167-78. 10.1037/0033-2909.117.1.167 [DOI] [PubMed] [Google Scholar]
- 10. Schünemann HJ, Puhan M, Goldstein R, Jaeschke R, Guyatt GH. Measurement properties and interpretability of the Chronic respiratory disease questionnaire (CRQ). COPD 2005;2:81-9. 10.1081/COPD-200050651 [DOI] [PubMed] [Google Scholar]
- 11. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60. 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Johnston BC, Thorlund K, Schünemann HJ, et al. Improving the interpretation of quality of life evidence in meta-analyses: the application of minimal important difference units. Health Qual Life Outcomes 2010;8:116. 10.1186/1477-7525-8-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Guyatt GH, Osoba D, Wu AW, Wyrwich KW, Norman GR, Clinical Significance Consensus Meeting Group Methods to explain the clinical significance of health status measures. Mayo Clin Proc 2002;77:371-83. 10.4065/77.4.371. [DOI] [PubMed] [Google Scholar]
- 14. Hedges LV, Gurevitch J, Curtis P. The meta-analysis of response ratio in experimental ecology. Ecology 1999;80:1150-6 10.1890/0012-9658(1999)080[1150:TMAORR]2.0.CO;2. [DOI] [Google Scholar]
- 15.Morton S, Murad M, O’Connor E, et al. Quantitative Synthesis—An Update. Methods Guide for Comparative Effectiveness Reviews. AHRQ Publication No 18-EHC007-EF Rockville, MD: Agency for Healthcare Research and Quality www.ncbi.nlm.nih.gov/books/NBK519365/ 2018
- 16. Friedrich JO, Adhikari NK, Beyene J. Ratio of means for analyzing continuous outcomes in meta-analysis performed as well as mean difference methods. J Clin Epidemiol 2011;64:556-64. 10.1016/j.jclinepi.2010.09.016. [DOI] [PubMed] [Google Scholar]
- 17. da Costa BR, Rutjes AW, Johnston BC, et al. Methods to convert continuous outcomes into odds ratios of treatment response and numbers needed to treat: meta-epidemiological study. Int J Epidemiol 2012;41:1445-59. 10.1093/ije/dys124. [DOI] [PubMed] [Google Scholar]
- 18. Murad MH, Montori VM, Walter SD, Guyatt GH. Estimating risk difference from relative association measures in meta-analysis can infrequently pose interpretational challenges. J Clin Epidemiol 2009;62:865-7. 10.1016/j.jclinepi.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 19. Murad MH, Montori VM, Ioannidis JP, et al. How to read a systematic review and meta-analysis and apply the results to patient care: users’ guides to the medical literature. JAMA 2014;312:171-9. 10.1001/jama.2014.5559. [DOI] [PubMed] [Google Scholar]
- 20. Guyatt GH, Eikelboom JW, Gould MK, et al. Approach to outcome measurement in the prevention of thrombosis in surgical and medical patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012;141(Suppl):e185S-94S. 10.1378/chest.11-2289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Miller SA, Wu RKS, Oremus M. The association between antibiotic use in infancy and childhood overweight or obesity: a systematic review and meta-analysis. Obes Rev 2018;19:1463-75. 10.1111/obr.12717. [DOI] [PubMed] [Google Scholar]
- 22. Friedrich JO, Adhikari NK, Beyene J. The ratio of means method as an alternative to mean differences for analyzing continuous outcome variables in meta-analysis: a simulation study. BMC Med Res Methodol 2008;8:32. 10.1186/1471-2288-8-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Van Den Noortgate W, Onghena P. Estimating the mean effect size in meta-analysis: bias, precision, and mean squared error of different weighting methods. Behav Res Methods Instrum Comput 2003;35:504-11. 10.3758/BF03195529 [DOI] [PubMed] [Google Scholar]
- 24. Shrier I, Christensen R, Juhl C, Beyene J. Meta-analysis on continuous outcomes in minimal important difference units: an application with appropriate variance calculations. J Clin Epidemiol 2016;80:57-67. 10.1016/j.jclinepi.2016.07.012. [DOI] [PubMed] [Google Scholar]
- 25. Spencer FA, Iorio A, You J, et al. Uncertainties in baseline risk estimates and confidence in treatment effects. BMJ 2012;345:e7401. 10.1136/bmj.e7401. [DOI] [PubMed] [Google Scholar]


