Abstract
Introduction
The dihydroorotate dehydrogenase (DHODH) inhibitors leflunomide and teriflunomide are immunomodulatory agents approved to treat rheumatoid arthritis (RA) and multiple sclerosis, respectively, and are actively being investigated as therapeutic agents for other immune-related diseases; however, both structurally related compounds have a number of potentially serious adverse effects. Vidofludimus, a new selective second-generation DHODH inhibitor, is chemically distinct from leflunomide/teriflunomide and appears to exhibit a distinct safety profile.
Objective
The aim of the COMPONENT study was to assess the efficacy, safety, and pharmacokinetics of vidofludimus in the treatment of patients with active RA on a background therapy of methotrexate. This report focuses solely on the safety results of the COMPONENT trial.
Methods
Patients received once-daily oral vidofludimus (N = 122) or placebo (N = 119) along with their standard of care methotrexate treatment for 13 weeks. Efficacy endpoints were assessed. Safety parameters were monitored throughout treatment and at follow-up. Plasma concentrations of vidofludimus were measured.
Results
The primary efficacy endpoint, American College of Rheumatology 20 (ACR20) responder rate at 13 weeks, demonstrated numerical superiority in the treatment group compared with placebo; however, it did not reach statistical significance. Nonetheless, the COMPONENT study yielded important safety and pharmacokinetic data that could provide important information regarding the use of vidofludimus in other clinical trials, not only for RA but also for other autoimmune diseases. A safety profile for vidofludimus similar to placebo was obtained in this RA patient population. This includes similar rates of the adverse events of diarrhea, alopecia, neutropenia, and elevated liver enzymes, all of which are known drug-related adverse events reported for leflunomide and teriflunomide. A potential pharmacokinetic interaction between vidofludimus and methotrexate was observed.
Conclusions
Vidofludimus demonstrated a positive safety profile, making it a promising candidate for the treatment of a variety of immune-related diseases.
Trial Registrations
ClinicalTrials.gov identifier: NCT01010581.
Key Points
| The second-generation dihydroorotate dehydrogenase (DHODH) inhibitor vidofludimus exhibits a favorable safety profile. |
| In the COMPONENT trial for rheumatoid arthritis (RA), vidofludimus did not exhibit higher rates of many of the adverse effects known to occur with the US FDA-approved DHODH inhibitors leflunomide and teriflunomide. |
| The high selectivity for DHODH and lack of off-target effects of vidofludimus positions it as a promising selective immunomodulatory agent for use in a number of different immune-related diseases. |
Introduction
Rheumatoid arthritis (RA) is a painful and highly debilitating chronic inflammatory disease characterized by progressive destruction of the joints, deformity, disability, and premature death. Current treatment includes palliative anti-inflammatory agents (e.g. nonsteroidal anti-inflammatory drugs and corticosteroids), biologic response modifiers that selectively inhibit cytokines that contribute to disease pathogenesis, and disease-modifying antirheumatic drugs (DMARDs) such as methotrexate and leflunomide [1]. DMARDs, particularly methotrexate, are the frontline treatment in early RA [2]. However, DMARD monotherapy is often insufficient to halt disease progression and combination therapy using drugs with different mechanisms of action may be used [1].
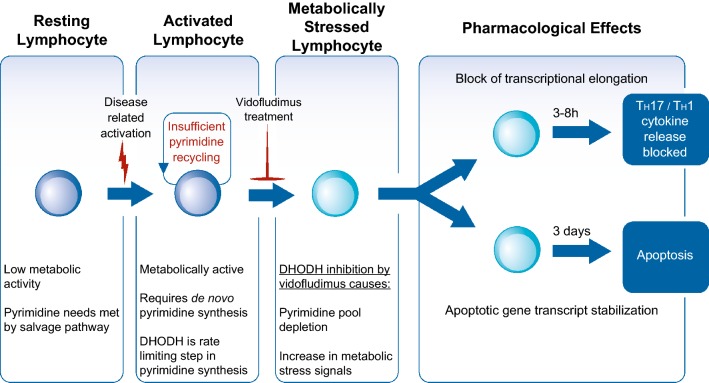
One approach to the treatment of RA and other immune-related diseases is to inhibit human dihydroorotate dehydrogenase (DHODH), the enzyme that catalyzes the rate-limiting step in pyrimidine synthesis. It is well established that inhibitors of DHODH show immunomodulatory activity, which is most pronounced on T cells [3–8], with T helper (Th) 1 and Th17 cells acting as important contributors to the inflammatory processes of RA [9]. DHODH inhibitors exhibit an immunomodulatory effect that is selective towards metabolically highly activated and rapidly proliferating lymphocytes [10], which require de novo synthesis to meet their needs for pyrimidines, an essential component of nucleic acids. DHODH inhibition in these cells leads to inhibition of transcriptional elongation, cell cycle arrest, and apoptosis. In contrast, resting and normal-acting lymphocytes do not depend on de novo synthesis, instead satisfying their pyrimidine requirements through the DHODH-independent salvage pathway. In activated lymphocytes, the metabolic stress in response to DHODH inhibition leads to a reduction of proinflammatory cytokine release, including interleukin (IL)-17 (IL-17A and IL-17F) and interferon (IFN)-γ, and to increased apoptosis (Fig. 1) [11–13].
Fig. 1.
DHODH inhibition by vidofludimus inhibits cytokine release and promotes apoptosis in activated lymphocytes. DHODH dihydroorotate dehydrogenase
There are currently two DHODH inhibitors approved by the US FDA—leflunomide (Arava®, approved for use in RA and psoriatic arthritis) and teriflunomide [Aubagio®, approved for use in multiple sclerosis (MS)]. Leflunomide is a prodrug that is rapidly converted in the body to its active metabolite, teriflunomide [14]; thus, both drugs share the same mechanism of action. The two compounds are believed to act by both inhibiting T-cell proliferation and decreasing activation of B cells, resulting in reduction of the autoantibodies that are thought to be at the root of their respective disease indications [15–17].
While leflunomide is widely used in treating RA, either as a monotherapy or in combination with methotrexate [18], the class of DHODH inhibitors to which both leflunomide and teriflunomide belong have been the subject of numerous safety concerns since their approval by the FDA. Postmarket surveillance includes reports of a variety of drug-related adverse reactions, including elevated liver enzymes and hepatotoxicity, peripheral neuropathy, vasculitis, hypertension, alopecia, pruritus, nausea, and diarrhea [16, 19–28]. In one prospective study evaluating leflunomide treatment in 136 RA patients, 65% of patients experienced at least one adverse event (AE) related to leflunomide, and nearly 37% discontinued the drug for such reasons [29]. Similarly, a 3-year retrospective study found that in RA patients initiating DMARD treatment, those receiving leflunomide demonstrated a higher discontinuation rate, largely due to AEs, including occurrence of neutropenia [30]. Furthermore, when taken in combination with methotrexate, the cumulative dose of leflunomide has been shown to correlate with liver fibrosis [31].
In 2010, the FDA placed a boxed warning on the label of Arava after concluding that leflunomide was associated with the development of severe liver injury in patients using the drug [32]. This was based on the FDA’s review of AE reporting, which identified 49 cases of severe liver injury, including 14 cases of fatal liver failure, between August 2002 and May 2009. As treatment with Aubagio leads to plasma concentrations of teriflunomide similar to what is seen with Arava, the FDA also placed a boxed warning on the approved labeling text for Aubagio based on the expectation of similar risks [33].
Vidofludimus is a novel chemical class of orally available DHODH inhibitors with no structural similarity to other known drugs, including leflunomide and teriflunomide. Vidofludimus, in both its free acid form and its calcium salt formulation (vidofludimus calcium), has undergone clinical trials for a variety of immune-related indications. Both formulations depend on the same active substance (vidofludimus) in vivo, and thus the two formulations share the same mechanism of action, pharmacology, and toxicology. The safety of both vidofludimus and vidofludimus calcium has been investigated in healthy volunteers and patients with different immune-mediated diseases. Based on the known selective immunomodulatory effect of DHODH inhibitors, vidofludimus has been considered therapeutically promising for a number of indications. Vidofludimus has undergone trials in patients with inflammatory bowel disease (IBD), including Crohn’s disease (CD) and ulcerative colitis (UC) [34], and RA [35] (ClinicalTrials.gov identifiers: NCT00820365 and NCT01010581), and vidofludimus calcium is currently undergoing trials, or has trials planned, for UC, primary sclerosing cholangitis (PSC), and MS [36] (ClinicalTrials.gov identifiers: NCT03341962, NCT03722576, and NCT03846219). Although ongoing studies remain blinded, it is estimated that to date more than 500 patients and healthy volunteers have been exposed to vidofludimus or vidofludimus calcium [36].
In this publication, we report the safety data of vidofludimus from a phase II trial in patients with RA (the COMPONENT trial; ClinicalTrials.gov Identifier: NCT01010581). This was a randomized, double-blind, placebo-controlled study to evaluate the efficacy, safety, and pharmacokinetics (PK) of vidofludimus 35 mg compared with placebo on methotrexate background therapy in subjects with RA. The primary endpoint of the trial was the rate of responders showing a 20% improvement in American College of Rheumatology criteria (ACR20) [37] after 13 weeks of treatment. While the ACR20 responder rate was higher in the vidofludimus group than in the placebo group, it did not reach statistical significance. Despite the failed primary efficacy endpoint in the indication of RA, the study has yielded important insights into the safety of vidofludimus. The pharmaceutical industry has been criticized for not reporting data from failed trials, the results from which can inform clinical practice and give insights into the safety and pharmacology of other agents in that class [38]. Furthermore, the World Health Organization has taken the position that negative and inconclusive results from clinical trials should be published [39].
The authors feel strongly that the safety results from the COMPONENT trial are relevant for current studies of vidofludimus calcium (IMU-838) in PSC, UC, and MS, as well as for any future studies of this novel class of DHODH inhibitors. Indeed, DHODH inhibitors have been proposed as potential therapeutic agents for a variety of autoimmune diseases [40–43] and as antitumor agents [44, 45], and are currently undergoing clinical trials for a number of such indications.
In this study, we report a comprehensive summary of the safety data of the COMPONENT trial. Establishment of a positive safety profile is likely to facilitate the study of the DHODH inhibitor vidofludimus as a promising selective immunomodulatory agent for the treatment of a variety of immune-mediated diseases.
Methods
Overall Study Design
The COMPONENT study was a phase II clinical trial to assess the safety and efficacy of vidofludimus in combination with methotrexate in patients with RA who were not responding sufficiently to methotrexate monotherapy. The study was a randomized, double blind, placebo-controlled, parallel group, multicenter study performed at 29 sites in Bulgaria, Czech Republic, Poland, and Romania. The primary objective was to evaluate the efficacy of once-daily oral vidofludimus (35 mg) in combination with methotrexate compared with methotrexate monotherapy after 13 weeks of treatment. Secondary objectives were to evaluate the safety profile of vidofludimus when administered in combination with methotrexate, and to assess the trough plasma concentrations of vidofludimus.
Patients with active RA were enrolled and randomized into two treatment arms (133 patients per arm), receiving either once-daily vidofludimus or placebo in combination with the patient’s current established stable once-weekly dose of methotrexate, which varied from 10 to 25 mg. Folic acid (5 mg) was taken once weekly to offset the effects of methotrexate-induced folate deficiency. Patients received the study medication for a period of 13 weeks. During the study period, patients underwent an initial screening visit at the investigative site, eight study visits (at day 1 and weeks 1, 2, 3, 4, 6, 8, and 13), and a follow-up visit at week 15 to assess safety.
At study visits 3–8, procedures performed included vital signs (blood pressure and pulse), a 12-lead electrocardiogram (ECG), assessment of efficacy parameters, safety laboratory parameters (hematology, clinical chemistry, and urinalysis), blood sampling for plasma vidofludimus concentration, and documentation of AEs. At the week 15 follow-up visit, vital signs, documentation of AEs, and safety laboratory testing were performed. Urine dipstick testing to check for erythrocytes in the urine was performed daily by patients during the study.
Inclusion and Exclusion Criteria
Males and females 18 years of age or older with active RA of functional classes I, II, or III according to the ACR criteria for the classification of global functional status in RA [46], and who had received weekly doses of methotrexate (10–25 mg/week) for a minimum of 3 months prior to day 1 dosing, were eligible for the study. Methotrexate dosage must have been stable for at least 6 weeks. Patients may have received up to 10 mg/day of oral prednisolone or corticosteroid equivalent.
Reasons for exclusion were active RA of functional class IV; non-pharmacological treatment (physical therapy), cardiac arrhythmia or other significant ECG finding; congestive heart failure; uncontrolled hypertension; low hemoglobin, white blood cell count, or platelet count; uncontrolled asthma; history of acute infection with human immunodeficiency virus (HIV), hepatitis B or C; elevated liver enzymes or serum creatinine; low glomerular filtration rate; renal disease or conditions after kidney transplantation; history or existence of urolithiasis; hematuria; psychiatric illness; active tuberculosis; known or suspected immunodeficiency; history of malignancy (past 5 years); inadequate contraception, pregnancy, or lactation; history of serious drug sensitivity; and history of alcohol or drug dependence, or history of heavy smoking. Patients were also prohibited from participating if they had received vaccination with live attenuated viruses within 4 weeks prior to study start or had participated in another investigational drug or vaccine study within the last 3 months. The following were prohibited within 4 weeks prior to dosing: sulfasalazine, hydroxychloroquine, and corticosteroids > 10 mg/day. Patients who had received leflunomide or cyclophosphamide required a 180-day washout period prior to day 1 dosing. Cyclosporine, abatacept, etanercept, adalimumab, infliximab, and rituximab required a 60-day washout period, while oral or injectable gold, azathioprine, penicillamine, anakinra, or parenteral or intra-articular corticosteroids required a 30-day washout period.
Patient Stratification
The safety set includes all patients who were randomized and received any amount of study drug. The full analysis set is a subset of the safety set and includes all patients who were randomized and received any amount of study drug and who had minimum efficacy data available (defined as at least one post-baseline efficacy observation of any of the primary or secondary efficacy parameters at visit 3 or later).
Efficacy Endpoints
The primary efficacy analysis was based on the ACR20 responder rate after 13 weeks of treatment. The ACR20 calculation was based on the following variables: tender joint count (TJC), swollen joint count (SJC), C-reactive protein (CRP), patient’s pain on a visual analog scale (VAS), patient’s global assessments of disease activity on a VAS, physician’s global assessments of disease activity on a VAS, and Health Assessment Questionnaire–Disability Index. The ACR20 was defined as 20% improvement in TJC, SJC, and three of the last five items. Secondary efficacy variables included ACR50; ACR70; 28-joint count disease activity score (DAS28) with CRP and erythrocyte sedimentation rate (ESR); responder rates for DAS28 (CRP) and DAS28 (ESR); morning stiffness; patient’s assessment of pain and patient’s assessment of disease activity using a VAS; rheumatoid factor; patient’s and physician’s global assessments of efficacy; and withdrawals due to lack of efficacy.
Safety Assessment
The criteria to evaluate safety were AEs, changes from baseline in safety laboratory values (hematology, clinical chemistry, and urinalysis), changes from baseline in vital signs (blood pressure and heart rate), 12-lead ECG findings, and patient’s and physician’s global assessments of tolerability. Treatment-emergent AEs (TEAEs) and serious AEs (SAEs) were coded using MedDRA, version 12.0.1 A TEAE was defined as an AE occurring or worsening after the first study treatment and up through the follow-up visit. AEs occurring or worsening after the follow-up visit were also defined as treatment emergent if they were considered to be study drug related.
Hematology results included hematocrit, hemoglobin, mean corpuscular volume, mean corpuscular hemoglobin, mean corpuscular hemoglobin concentration, red blood cell (RBC) count, total and differential leukocyte count, platelet count, and coagulation tests (prothrombin time and partial thromboplastin time). Clinical chemistry testing included sodium, potassium, chloride, inorganic phosphorus, calcium, creatine phosphokinase, lactate dehydrogenase, total protein, albumin, albumin/globulin ratio, fasting glucose, cholesterol, triglycerides, creatinine, uric acid, urea, total and conjugated bilirubin, and liver enzymes [alanine aminotransferase (ALT), aspartate aminotransferase (AST), γ-glutamyl transferase (GGT), and alkaline phosphatase (ALP)].
Urinalysis results included pH, urobilinogen, erythrocytes, leukocytes, protein, ketones, bilirubin, nitrite, and glucose. Urinalysis results (except pH values) were categorized as negative, positive but normal, abnormal but not clinically significant, or abnormal and clinically significant. Urine pH values were recorded as numeric value and categorized as either normal, abnormal but not clinically significant, or abnormal and clinically significant. Daily urine dipstick results were characterized as normal, elevated (+), highly elevated (++), or extremely highly elevated (+++).
Vital signs (blood pressure and heart rate) were evaluated as changes from baseline. The summary ECG assessments were categorized as normal, abnormal but not clinically significant, or abnormal and clinically significant. Individual values of heart rate and PQ, QRS, QT, and QTc (Bazett’s correction) intervals were determined. Patient’s and physician’s global assessment of tolerability was rated on a scale of 1–5 (very good, good, moderate, poor, or very poor).
All safety data were evaluated and summarized using descriptive statistics only.
Analysis of Plasma Concentration of Vidofludimus
Blood samples were taken at baseline and at 2 weeks (visit 3), 4 weeks (visit 5), 8 weeks (visit 7), and 13 weeks (visit 8). Blood samples were taken before daily dosing of study medication. Plasma concentrations of vidofludimus were analyzed by liquid chromatography with tandem mass spectrometry and represented the steady-state trough levels of vidofludimus. The median PK concentrations over all time points were calculated for each patient in the vidofludimus arm. A non-parametric Jonckheere–Terpstra test [47] was used to determine whether there was any relationship between vidofludimus trough values and increasing methotrexate concentrations.
Results
Patient Demographics, Medical History, Methotrexate Doses
A total of 266 patients were randomized to either the vidofludimus or placebo groups, with 133 patients in each study arm. A total of 213 patients completed the study, with 53 withdrawals—26 in the vidofludimus arm and 27 in the placebo arm, mostly due to withdrawn consent. The safety set (N = 241) included 122 patients in the treatment group and 119 in the placebo arm, with a mean age of 57 years. The set was composed of 83% female patients and 17% male patients. This is representative of the natural distribution of RA in the population and no effort was made to equalize sex distribution. Full demographic data of the safety set are shown in Table 1. Within the safety set, 5.4% of patients were categorized as class I, 61.4% as class II, and 33.2% as class III for global functional status in RA. Patients categorized as class IV were excluded from the study by design. Overall mean time since first diagnosis was 8.4 years and the mean time since first methotrexate treatment was 4.2 years.
Table 1.
Demographic data of the safety set in the COMPONENT trial
| Vidofludimus (N = 122) | Placebo (N = 119) | Total (N = 241) | |
|---|---|---|---|
| Sex | |||
| Female | 101 (82.8%) | 99 (83.2%) | 200 (83.0%) |
| Male | 21 (17.2%) | 20 (16.8%) | 41 (17.0%) |
| Race | |||
| Caucasian | 122 (100.0%) | 119 (100.0%) | 241 (100.0%) |
| Age (years) | |||
| Mean (SD) | 56.4 (10.6) | 56.9 (10.1) | 56.6 (10.3) |
| Median | 57 | 58 | 57 |
| Minimum | 21 | 29 | 21 |
| Maximum | 81 | 77 | 81 |
| Weight (kg) | |||
| Mean (SD) | 71.5 (14.9) | 73.6 (14.8) | 72.5 (14.9) |
| Median | 70 | 73 | 71 |
| Minimum | 49 | 44 | 44 |
| Maximum | 126 | 117 | 126 |
| Height (cm) | |||
| Mean (SD) | 164.0 (8.2) | 164.0 (6.7) | 164.0 (7.5) |
| Median | 164 | 164 | 164 |
| Minimum | 140 | 146 | 140 |
| Maximum | 192 | 185 | 192 |
| BMI (kg/m2) | |||
| Mean (SD) | 26.6 (5.0) | 27.4 (5.5) | 27.0 (5.3) |
| Median | 26 | 27 | 26 |
| Minimum | 18 | 18 | 18 |
| Maximum | 40 | 46 | 46 |
BMI body mass index, N number of patients, SD standard deviation
Patients in both arms were assigned a weekly dose of methotrexate of between 10 and 25 mg, based on their current ongoing standard of care methotrexate dose; 37.8% received 10 mg, 34.0% received between 12.5 and 15 mg, and 28.2% were assigned doses between 17.5 and 25 mg. Within the full analysis set, a statistically significant effect of methotrexate dose on the plasma concentration of vidofludimus was observed (Fig. 2), with median trough values per patient being lower with increasing methotrexate concentrations (p = 0.023). However, there was no statistically significant influence of methotrexate dose on the overall rate of TEAEs between the vidofludimus and placebo arms (10 mg: 56.8% vs. 51.1%; 12.5–15 mg: 63.8% vs. 60.0%; 17.5–25 mg: 45.2% vs. 67.6%).
Fig. 2.
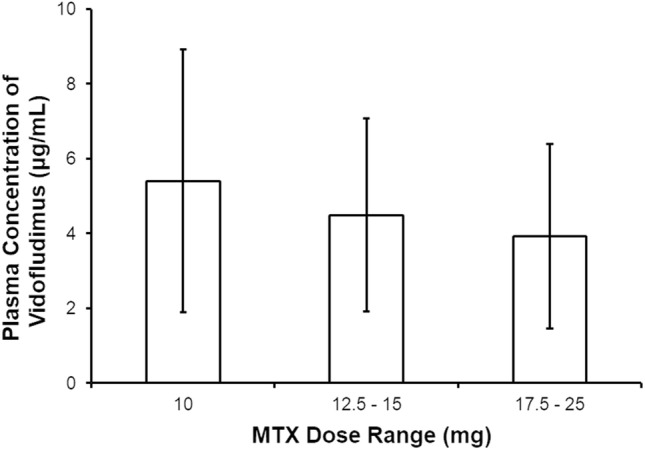
Median plasma trough concentration of vidofludimus per patient over all visits by weekly methotrexate dose group. Data are presented as mean ± SD. Analysis based on the Jonckheere–Terpstra test consistently showed that vidofludimus median trough values per patient were significantly lower with increasing methotrexate concentrations (p = 0.023). SD standard deviation
Efficacy
Complete efficacy results of the COMPONENT trial have been made public elsewhere [35] and are summarized here. While the primary endpoint of ACR20 responder rate at 13 weeks was not statistically significant over placebo (50.8% vs. 44.8%; p = 0.365), the metric demonstrated numerical superiority over placebo throughout the study and statistical significance at the 8-week time point (46.7% vs. 31.9%; p = 0.024). Overall, the study demonstrated a trend of beneficial effects in patients with RA treated with vidofludimus versus placebo. ACR50 (26.7% vs. 17.2%) and ACR70 (11.7% vs. 6.0%) responder rates at 13 weeks were higher in the treatment arm. The time to ACR20 response was significantly (p < 0.05) shorter in the vidofludimus group compared with placebo (median 56 vs. 92 days). The DAS28 (CRP) response rate of vidofludimus was significantly higher compared with placebo at week 4 (55.0% vs. 41.3%; p = 0.038), but did not reach statistical significance at week 13 (60.9% vs. 56.9%; p = 0.597). There were also numerically greater mean changes from baseline in inflammatory markers such CRP and ESR. One limitation of this study lies in its relatively small size and short duration. It is possible that the potentially clinically important trends seen will require a larger and/or longer study to reach statistical significance. Another limitation lies in the heterogeneity of the background standard of care methotrexate treatment. In some patients, onset of methotrexate therapy was relatively recent and may have contributed to a higher placebo response than anticipated. Perhaps more importantly, PK analysis showed that in patients receiving weekly methotrexate doses of 17.5 mg or higher (which was applicable for 25.4% of patients receiving vidofludimus), there was an approximately 20% decrease in serum trough levels of vidofludimus. This apparent PK interaction may have led to a reduced exposure to vidofludimus for these patients.
Adverse Events (AEs)
Of the 241 patients in the safety set, 57.7% experienced one or more TEAEs during the study (Table 2). A similar percentage in the vidofludimus (56.6%) and placebo (58.8%) arms experienced at least one TEAE, with 14.8% (vidofludimus arm) and 24.4% (placebo arm) experiencing an AE that was considered related to vidofludimus or placebo. Overall, eight patients (3.3%) experienced a TEAE that led to discontinuation of vidofludimus or placebo—three (2.5%) in the vidofludimus arm and five (4.2%) in the placebo group. None of the discontinuations in the vidofludimus arm were thought to be due to study drug.
Table 2.
Overall adverse event profile by study arm
| Adverse event | Vidofludimus (N = 122) | Placebo (N = 119) | Total (N = 241) |
|---|---|---|---|
| Any TEAE | 69 (56.6) | 70 (58.8) | 139 (57.7) |
| Any SAE | 1 (0.8) | 1 (0.8) | 2 (0.8) |
| Any TEAE related to: | |||
| Vidofludimus or placebo | 18 (14.8) | 29 (24.4) | 47 (19.5) |
| Methotrexate | 16 (13.1) | 18 (15.1) | 34 (14.1) |
| Folic acid | 7 (5.7) | 2 (1.7) | 9 (3.7) |
| Any study drug | 22 (18.0) | 30 (25.2) | 52 (21.6) |
| Any TEAE leading to withdrawal of: | |||
| Vidofludimus or placebo | 3 (2.5) | 5 (4.2) | 8 (3.3) |
| Methotrexate | 1 (0.8) | 1 (0.8) | 2 (0.8) |
| Folic acid | 1 (0.8) | 1 (0.8) | 2 (0.8) |
| Death | 0 (0.0) | 0 (0.0) | 0 (0.0) |
Data are expressed as n (%)
N number of patients, SAE serious adverse event, TEAE treatment-emergent adverse event
Common Treatment-Emergent AEs
Hematology, clinical chemistry, urinalysis, vital signs, and ECG values all remained stable over time, and no consistent differences or trends between the treatment groups were noted. Tolerability was judged as high and was similar in both arms, with 79.5% of patients in the vidofludimus arm and 78.2% in the placebo arm responding either ‘good’ or ‘very good’ in the patient’s global assessment of tolerability.
Among the TEAEs, most were of mild or moderate severity. In the vidofludimus arm, 45.9% of patients experienced a mild AE and 22.1% experienced a moderate AE. In the placebo arm, mild or moderate AEs occurred in 48.7% and 24.4% of patients, respectively. The most frequently affected system organ class (SOC) was infections and infestations, experienced by 22.1% of patients in the vidofludimus arm and 30.3% of patients in the placebo arm (Table 3). The most frequent single TEAE overall was headache, experienced by 15.6% of patients in the vidofludimus arm and 16.8% in the placebo arm (Table 4). The most frequent TEAEs that occurred at least twice as frequently in the vidofludimus arm than in the placebo arm included upper abdominal pain, increased ALP, and hypertension (each experienced by 3.3% of patients in the vidofludimus arm vs. 0.8% of patients in the placebo arm); pyrexia and cystitis (each 2.5% vs. 0.8%); and dyspepsia and oropharyngeal pain (each 2.5% vs. 0.0%). The most frequent TEAEs experienced at least twice as frequently in the placebo arm than in the vidofludimus arm included vomiting, respiratory tract infection, sinusitis, and musculoskeletal stiffness (each experienced by 2.5% of patients in the placebo arm vs. 0.0% of patients in the vidofludimus arm); and upper respiratory tract infection (7.6% vs. 1.6%).
Table 3.
Most frequent treatment-emergent adverse events by system organ class (frequency > 2.0% in either treatment arm)
| TEAEs by MedDRA SOC | Vidofludimus (N = 122) | Placebo (N = 119) | Total (N = 241) |
|---|---|---|---|
| Infections and infestations | 27 (22.1) | 36 (30.3) | 63 (26.1) |
| Nervous system disorders | 22 (18.0) | 24 (20.2) | 46 (19.1) |
| Musculoskeletal and connective tissue disorders | 19 (15.6) | 16 (13.4) | 35 (14.5) |
| Gastrointestinal disorders | 18 (14.8) | 15 (12.6) | 33 (13.7) |
| Investigations | 10 (8.2) | 8 (6.7) | 18 (7.5) |
| Skin and subcutaneous tissue disorders | 8 (6.6) | 4 (3.4) | 12 (5.0) |
| Respiratory, thoracic and mediastinal disorders | 7 (5.7) | 5 (4.2) | 12 (5.0) |
| Metabolism and nutrition disorders | 3 (2.5) | 6 (5.0) | 9 (3.7) |
| General disorders and administration site conditions | 6 (4.9) | 5 (4.2) | 11 (4.6) |
| Renal and urinary disorders | 6 (4.9) | 5 (4.2) | 11 (4.6) |
| Vascular disorders | 4 (3.3) | 3 (2.5) | 7 (2.9) |
| Psychiatric disorders | 4 (3.3) | 1 (0.8) | 5 (2.1) |
| Eye disorders | 3 (2.5) | 2 (1.7) | 5 (2.1) |
| Ear and labyrinth disorders | 1 (0.8) | 3 (2.5) | 4 (1.7) |
| Hepatobiliary disorders | 1 (0.8) | 3 (2.5) | 4 (1.7) |
Data are expressed as n (%)
MedDRA Medical Dictionary for Regulatory Activities, N number of patients, SOC system organ class, TEAEs treatment-emergent adverse events
Table 4.
Most frequent treatment-emergent adverse events by preferred term (frequency > 2.0% in either treatment arm)
| MedDRA SOC | TEAEs by MedDRA preferred term | Vidofludimus (N = 122) | Placebo (N = 119) | Total (N = 241) |
|---|---|---|---|---|
| Gastrointestinal disorders | Diarrhea | 7 (5.7) | 7 (5.9) | 14 (5.8) |
| Nausea | 4 (3.3) | 5 (4.2) | 9 (3.7) | |
| Abdominal pain upper | 4 (3.3) | 1 (0.8) | 5 (2.1) | |
| Dyspepsia | 3 (2.5) | 0 (0.0) | 3 (1.2) | |
| Vomiting | 0 (0.0) | 3 (2.5) | 3 (1.2) | |
| General disorders and administration site conditions | Pyrexia | 3 (2.5) | 1 (0.8) | 4 (1.7) |
| Infections and infestations | Nasopharyngitis | 8 (6.6) | 6 (5.0) | 14 (5.8) |
| Urinary tract infection | 6 (4.9) | 7 (5.9) | 13 (5.4) | |
| Upper respiratory tract infection | 2 (1.6) | 9 (7.6) | 11 (4.6) | |
| Pharyngitis | 3 (2.5) | 4 (3.4) | 7 (2.9) | |
| Viral infection | 3 (2.5) | 2 (1.7) | 5 (2.1) | |
| Cystitis | 3 (2.5) | 1 (0.8) | 4 (1.7) | |
| Respiratory tract infection | 0 (0.0) | 3 (2.5) | 3 (1.2) | |
| Sinusitis | 0 (0.0) | 3 (2.5) | 3 (1.2) | |
| Investigations | Blood alkaline phosphatase increased | 4 (3.3) | 1 (0.8) | 5 (2.1) |
| Musculoskeletal and connective tissue disorders | Rheumatoid arthritis | 8 (6.6) | 7 (5.9) | 15 (6.2) |
| Arthralgia | 5 (4.1) | 4 (3.4) | 9 (3.7) | |
| Musculoskeletal stiffness | 0 (0.0) | 3 (2.5) | 3 (1.2) | |
| Nervous system disorders | Headache | 19 (15.6) | 20 (16.8) | 39 (16.2) |
| Respiratory, thoracic and mediastinal disorders | Oropharyngeal pain | 3 (2.5) | 0 (0.0) | 3 (1.2) |
| Vascular disorders | Hypertension | 4 (3.3) | 1 (0.8) | 5 (2.1) |
Data are expressed as n (%)
MedDRA Medical Dictionary for Regulatory Activities, N number of patients, SOC system organ class, TEAEs treatment-emergent adverse events
Overall, 4.1% of patients (five in each arm) reported a TEAE considered severe. Severe TEAEs in the vidofludimus arm included RA, pneumonia, viral infection, arthralgia, renal amyloidosis, and chronic renal failure. Severe TEAEs in the placebo arm included headache, herpes zoster, RA, dysuria, hematuria, and uterine dilation and curettage.
Serious AEs
There were two patients (one patient each in the vidofludimus and placebo arms) with at least one SAE reported during the study. One patient in the vidofludimus arm experienced three SAEs (pneumonia, secondary renal amyloidosis, and chronic renal failure) and was withdrawn from all study drugs. This patient was hospitalized and recovered from the pneumonia. At the time of the follow-up visit, the patient had not recovered from renal amyloidosis, deemed to be caused by a concomitant disease, and chronic renal failure. One patient in the placebo arm experienced two SAEs (hemiparesis and hypertensive crisis), requiring withdrawal of placebo, but no change in methotrexate dose or folic acid. This patient was hospitalized and recovered from the hypertensive crisis. The hemiparesis resolved with sequelae. None of the five SAEs were considered to be related to any study medication. No deaths were reported during the study.
AEs of Special Interest
Infections and Infestations
An increase in the susceptibility to infections is a general concern for therapies involving immunomodulators [48, 49]. While the most commonly affected SOC in the COMPONENT trial was infections and infestations (see Table 3), no increase of TEAEs in this SOC were observed (22.1% of patients in the vidofludimus arm vs. 30.3% in the placebo arm). Viral infections were uncommon and occurred at similar rates in both arms (see Table 4).
Hepatobiliary Events
Based on safety data from the DHODH inhibitors leflunomide and teriflunomide, AEs in the hepatobiliary disorders SOC were identified as AEs of special interest. However, such AEs were rare and overall did not occur more frequently in the vidofludimus arm compared with the placebo arm. The overall rate of hepatobiliary events was 4.9% in the vidofludimus arm and 5.9% in the placebo arm (Table 5).
Table 5.
All hepatobiliary treatment-emergent adverse events
| Hepatobiliary TEAEs by MedDRA SOC | Hepatobiliary TEAEs by MedDRA Preferred Term | Vidofludimus (N = 122) | Placebo (N = 119) | Total (N = 241) |
|---|---|---|---|---|
| Hepatobiliary disorders | 1 (0.8) | 3 (2.5) | 4 (1.7) | |
| Biliary colic | 0 (0.0) | 1 (0.8) | 1 (0.4) | |
| Hepatic pain | 0 (0.0) | 1 (0.8) | 1 (0.4) | |
| Hepatic steatosis | 0 (0.0) | 1 (0.8) | 1 (0.4) | |
| Hepatocellular injury | 1 (0.8) | 0 (0.0) | 1 (0.4) | |
| Investigations (hepatobiliary related) | 5 (4.1) | 4 (3.4) | 9 (3.7) | |
| Blood alkaline phosphatase increased | 4 (3.3) | 1 (0.8) | 5 (2.1) | |
| γ-Glutamyltransferase increased | 1 (0.8) | 1 (0.8) | 2 (0.8) | |
| Alanine aminotransferase increased | 0 (0.0) | 1 (0.8) | 1 (0.4) | |
| Hepatic enzyme increased | 0 (0.0) | 1 (0.8) | 1 (0.4) |
Data are expressed as n (%)
MedDRA Medical Dictionary for Regulatory Activities, N number of patients, SOC system organ class, TEAEs treatment-emergent adverse events
Hematuria
Based on early studies with high doses of vidofludimus, AEs of the renal and urinary disorders SOC, in particular hematuria, were of special interest. AEs in this SOC were uncommon and occurred with approximately the same frequency in both arms of the study (Table 6). Based on the known high rate of false-positive results in urine dipstick measurements [50], the determination of hematuria was based on findings from microscopic examination of urinary sediment and the likely clinical significance of those results. RBCs in the urine may be deemed clinically insignificant for a number of reasons, including improper urine collection, infection not considered secondary to drug-induced damage, menstruation, vigorous exercise, viral illness, trauma, or a recent urologic procedure [51]. Findings of RBCs in the urine were only considered as an AE of hematuria when assessed as clinically significant and when either five or more RBCs per high power field are present in at least two consecutive specimens [52] or the finding has diagnostic or therapeutic consequences. Table 7 shows the frequency of all positive urine dipstick results and all positive urine sediment analysis results for erythrocytes. The frequency of positive dipstick reads, as well as positive urine sediment analysis, did not differ between treatment arms and only one AE of hematuria per arm occurred during the study.
Table 6.
All renal and urinary treatment-emergent adverse events
| Renal and urinary TEAEs by MedDRA SOC | Renal and urinary TEAEs by MedDRA preferred term | Vidofludimus (N = 122) | Placebo (N = 119) | Total (N = 241) |
|---|---|---|---|---|
| Renal and urinary disorders | 6 (4.9) | 5 (4.2) | 11 (4.6) | |
| Hematuria | 1 (0.8) | 1 (0.8) | 2 (0.8) | |
| Bladder pain | 1 (0.8) | 0 (0.0) | 1 (0.4) | |
| Dysuria | 0 (0.0) | 1 (0.8) | 1 (0.4) | |
| Hemorrhage urinary tract | 0 (0.0) | 1 (0.8) | 1 (0.4) | |
| Ketonuria | 1 (0.8) | 0 (0.0) | 1 (0.4) | |
| Leukocyturia | 1 (0.8) | 0 (0.0) | 1 (0.4) | |
| Nephrolithiasis | 0 (0.0) | 1 (0.8) | 1 (0.4) | |
| Nocturia | 1 (0.8) | 0 (0.0) | 1 (0.4) | |
| Renal amyloidosis | 1 (0.8) | 0 (0.0) | 1 (0.4) | |
| Renal failure | 0 (0.0) | 1 (0.8) | 1 (0.4) | |
| Renal failure chronic | 1 (0.8) | 0 (0.0) | 1 (0.4) | |
| Renal pain | 0 (0.0) | 1 (0.8) | 1 (0.4) |
Data are expressed as n (%)
MedDRA Medical Dictionary for Regulatory Activities, N number of patients, SOC system organ class, TEAEs treatment-emergent adverse events
Table 7.
All positive urine dipstick and urine sediment analysis results
| Positive urinary erythrocyte results | Vidofludimus (N = 122) | Placebo (N = 119) | Total (N = 241) |
|---|---|---|---|
| Urine dipstick analysis | |||
| Elevated (+) | 33 (27.0) | 26 (21.8) | 59 (24.5) |
| Highly elevated (++) | 15 (12.3) | 15 (12.6) | 30 (12.4) |
| Extremely elevated | 8 (6.6) | 7 (5.9) | 15 (6.2) |
| Urine sediment analysis | |||
| Positive but normal | 63 (51.6) | 58 (48.7) | 121 (50.2) |
| Abnormal but not clinically significant | 35 (28.7) | 31 (26.1) | 66 (27.4) |
| Abnormal and clinically significant | 3 (2.5) | 2 (1.7) | 5 (2.1) |
Data are expressed as n (%)
N number of patients
Diarrhea, Alopecia, and Neutropenia
Along with hepatotoxicity, diarrhea, alopecia, and neutropenia are common and clinically relevant adverse effects of leflunomide and teriflunomide. In the COMPONENT study, there was no increased rate of diarrhea in the vidofludimus group compared with placebo, and alopecia and neutropenia were rare and did not occur at a significantly higher rate in the vidofludimus arm compared with placebo (Table 8).
Table 8.
All treatment-emergent adverse events involving diarrhea, alopecia, or neutropenia
| MedDRA SOC | MedDRA preferred term | Vidofludimus (N = 122) | Placebo (N = 119) | Total (N = 241) |
|---|---|---|---|---|
| Gastrointestinal disorders | Diarrhea | 7 (5.7) | 7 (5.9) | 14 (5.8) |
| Skin and subcutaneous tissue disorders | Alopecia | 1 (0.8) | 0 (0.0) | 1 (0.4) |
| Blood and lymphatic system disorders | White blood cell disorder | 0 (0.0) | 1 (0.8) | 1 (0.4) |
| Investigations | Neutrophil count abnormal | 0 (0.0) | 1 (0.8) | 1 (0.4) |
Data are expressed as n (%)
MedDRA Medical Dictionary for Regulatory Activities, N number of patients, SOC system organ class
Discussion
DHODH inhibitors are an important class of oral immunomodulatory drugs. Both leflunomide, as Arava for the treatment of RA, and its active metabolite teriflunomide, as Aubagio for MS, have been approved by the FDA. Leflunomide has shown some activity for a variety of other immune diseases, including juvenile idiopathic arthritis [53, 54], systemic lupus erythematosus (SLE) [16, 19], lupus nephritis [55], Sjogren’s syndrome [56], ankylosing spondylitis [57], dermatomyositis [58], and Wegener’s granulomatosis [59, 60]. Nonetheless, both leflunomide and teriflunomide have been the subject of significant safety concerns, including black box warnings by the FDA that limit their attractiveness as therapeutic agents for new clinical trials.
Vidofludimus is a novel and chemically distinct DHODH inhibitor that has undergone clinical trials for the treatment of RA and IBD. In the COMPONENT trial in patients with active RA, while the treatment group showed numerical superiority over control for a number of efficacy parameters, the primary efficacy endpoint of the trial was not met. However, important safety and tolerability information can be gleaned from that study.
During this study, the safety profile of vidofludimus was similar to that of the placebo group. In the set of patients (N = 241) receiving any study drug, most TEAEs were of mild or moderate severity. Five patients in each arm reported a severe TEAE, none of which were attributed to any study drug. Most TEAEs occurred with similar frequencies in both arms of the study and no pattern was noted with regard to TEAE frequency and methotrexate dose group. Some adverse effects occurred more often in the treatment group compared with controls, however their occurrences were low, and no clear conclusions can be drawn. Most of these TEAEs were assessed by investigators as unlikely to be related to any study drug, with only a single case of cystitis determined to be probably related to vidofludimus.
Infections and infestation did not occur at a higher rate following vidofludimus compared with placebo treatment. Notably, some of the more common and serious adverse effects of leflunomide and teriflunomide, such as neutropenia, alopecia, and diarrhea [24, 27, 61], occurred at a low rate in the COMPONENT trial and their rate was similar in both arms, with no increased rate in the vidofludimus treatment arm. The patient’s global assessment of tolerability showed that most patients in both treatment arms overwhelmingly considered the treatment tolerability as good or very good, and only 3% of patients discontinued treatment with vidofludimus due to an AE.
Interaction with Methotrexate
An effect of methotrexate dose on plasma levels of vidofludimus was noted during the study. This may have led to those in the higher methotrexate group of the vidofludimus arm receiving subtherapeutic exposure to the drug. Cytochrome P450 enzymes are not involved in metabolism of methotrexate [62], however methotrexate is known to be a substrate for the breast cancer resistance protein (BCRP) [63]. BCRP, an ATP-binding cassette efflux transporter, mediates renal and hepatobiliary elimination of drugs and xenobiotics [64] and is recognized as one of the key transport proteins mediating many drug–drug interactions.
Vesicular transport inhibition assays showed that human BCRP activity was potently inhibited by vidofludimus, with a half maximal inhibitory concentration (IC50) of 0.02 μM.2 Interestingly, while both leflunomide and teriflunomide are high affinity substrates for BCRP [65], vidofludimus was found not to be a substrate of BCRP in initial preclinical studies.3 While coadministration of methotrexate with BCRP inhibitors can result in methotrexate toxicity [62], in this study, combination therapy of methotrexate with vidofludimus did not lead to a different AE profile compared with placebo. However, methotrexate doses of 17.5 mg/week or higher slightly lowered trough levels of vidofludimus, and it is possible that BCRP transport competition may have contributed to this PK interaction. Although this result demonstrated statistical significance, the study design of the COMPONENT trial did not fulfill the criteria for interaction studies, and the negative association between methotrexate dose and vidofludimus plasma levels should be interpreted with caution.
Drug-Induced Liver Injury
Based on FDA-mandated warnings regarding leflunomide and teriflunomide, hepatobiliary events were considered AEs of clinical interest. The FDA’s boxed warnings on Arava (leflunomide) and Aubagio (teriflunomide) highlight the risk of severe liver injury, including fatal liver failure. This was based on a review of almost 7 years of AE reporting data on Arava use and the structural relatedness of the two compounds.
However, in the COMPONENT trial, hepatobiliary AEs were rare and, overall, did not occur more frequently in the vidofludimus arm compared with the placebo arm. Furthermore, evaluation of liver enzymes throughout the trial demonstrated no adverse effects on liver function attributed to treatment with vidofludimus.
Although there was no clinical indication of hepatotoxicity of vidofludimus in this trial, it is worth noting that in a phase IIa study of 116 RA patients evaluating the efficacy and safety of vidofludimus (20 or 35 mg) monotherapy or placebo (EudraCT Number: 2006-003142-42), one patient treated with vidofludimus 35 mg, who had documented increases in ALT, AST, GGT, and blood bilirubin, developed hepatitis 4 weeks after the end of treatment. This SAE was judged to be related to study drug. The patient had a history of Gilbert’s syndrome, a genetic liver disorder characterized by 70–80% reduced UGT1A1 activity. UGT1A1 is an enzyme of the glucuronidation pathway that transforms small lipophilic molecules, such as corticosteroids, bilirubin, hormones, and drugs, into water-soluble, excretable metabolites. Inhibition of UGT1A1 can cause mild hyperbilirubinemia, which normally has no serious consequences. In in vitro assays, vidofludimus has been shown to weakly inhibit UGT1A1,4 which is not clinically relevant under normal conditions. However, the weak UGT1A1 activity in patients with Gilbert’s syndrome may be exacerbated, leading to high levels of unconjugated bilirubin, elevated liver enzymes, and hepatitis.
Thus, careful analysis of hepatic events and laboratory data from this and previous clinical trials with vidofludimus do not indicate an elevated hepatotoxic potential of vidofludimus. As vidofludimus is structurally unrelated to leflunomide/teriflunomide, the liver toxicity may be an off-target effect of leflunomide rather than being due to DHODH inhibition itself. However, patients with Gilbert’s syndrome seem to be at higher risk for hepatobiliary events and the use of vidofludimus should be avoided until more data are available.
Hematuria
Vidofludimus interacts with DHODH by fitting sterically in the binding site of its native substrate, orotate. The human urate transporter 1 (URAT-1) has been shown to mediate uptake of orotate in the kidney [66]. Thus, it is not surprising that vidofludimus has been demonstrated to sterically inhibit the URAT-1 transport system.5 A member of the organic anion transporter family, URAT-1 mediates the reabsorption of uric acid from primary urine, maintaining urate homeostasis. Inhibition of URAT-1 leads to reduced serum urate levels and increased uric acid concentration in the urine. The DHODH inhibitors teriflunomide [67] and leflunomide [68] are also known to increase renal uric acid clearance and reduce serum uric acids levels, suggesting that both also act as uricosuric agents and block renal tubular reabsorption of urate.
Findings in the two phase I trials with vidofludimus have indicated that daily doses ≥ 70 mg may cause an increased rate of hematuria. A possible mechanism may be through this inhibition of URAT-1. High uric acid concentrations in the urine, when combined with low urine pH, may allow microcrystals to form. Such microcrystals may cause microscopic damage to the blood vessels within the urinary tract and may eventually lead to hematuria. All subsequent phase II trials of vidofludimus use doses well below 70 mg. Results in these trials, including the COMPONENT trial reported here, demonstrate that the frequency of RBC/hemoglobin-positive urinary results in the vidofludimus 35 mg and placebo groups were similar and no increased hematuria has been observed. Nonetheless, RBCs in urine should be carefully monitored and caution should be exercised using vidofludimus in patients with known conditions or medications leading to hyperuricemia.
Off-target Effects: Diarrhea, Alopecia, and Neutropenia
While the FDA-approved DHODH inhibitors and the investigational drug vidofludimus have a number of similarities, namely their mechanism of action, they have vastly different safety profiles. A number of characteristic adverse effects have been observed for leflunomide and teriflunomide that have not been observed with the structurally unrelated vidofludimus. In addition to liver toxicity and elevated liver enzymes, which require careful monitoring throughout the duration of therapy, some of the most common adverse reactions to the current FDA-approved DHODH inhibitors include diarrhea, alopecia, and neutropenia, which have led to high rates of treatment discontinuation [69].
In clinical studies of teriflunomide, alopecia was the most common cause of discontinuation because of AEs [33, 70], and real-world adherence studies of MS patients demonstrate that teriflunomide patients had a more than twofold increased risk for discontinuation compared with fingolimod patients [71]. These adverse effects may complicate their long-term use in other immune-related conditions. For instance, while leflunomide has shown efficacy in CD, its adverse effect of diarrhea is not acceptable in an IBD patient population [22]. In the COMPONENT study, neither diarrhea nor alopecia were observed at a higher rate as a consequence of therapy with vidofludimus compared with placebo.
The therapeutic use of many immunosuppressive agents is often limited by myelosuppression resulting from the non-specific antiproliferative effects on the immune cell population [72–75]. One of the key advantages of DHODH inhibitors is thought to be their specificity for activated, rapidly proliferating lymphocytes. Despite that fact, clinical trials and postmarket surveillance have identified neutropenia, a reduction in neutrophil count that can cause risk of serious infection, as a potential adverse effect for both leflunomide and teriflunomide. On the other hand, in preclinical studies, vidofludimus has been shown not to induce neutropenia or generalized leukopenia [76], and no instance of an increased rate of neutropenia has been observed in clinical studies using either vidofludimus or vidofludimus calcium.
This seemingly paradoxical occurrence of neutropenia, as well as the adverse reactions of diarrhea and alopecia, may be due to the many known off-target effects of leflunomide/teriflunomide [77–83]. Both leflunomide and teriflunomide have been shown to have a number of effects outside of their inhibition of DHODH. At clinically relevant concentrations, leflunomide has been shown to inhibit the tyrosine kinase activity of epidermal growth factor receptors (EGFRs), IL-2 receptors, and the Src-related tyrosine kinases p56lck and p59fyn. It has also been shown to act as an agonist for the aryl hydrocarbon receptor, which affects a number of processes involved in cell growth and differentiation. Teriflunomide was screened against 600 known kinases. This screen identified 55 kinases that were inhibited > 50% [84], some at clinically relevant concentrations. These off-target effects on kinases are likely the source of many of the unwanted in vivo effects of leflunomide and teriflunomide. On the other hand, vidofludimus is highly selective for DHODH, with no relevant inhibitory effects when tested against a panel of more than 100 protein kinases at concentrations up to 100 μM [36], approximately seven times the mean trough levels seen in the COMPONENT trial at week 8 (13.9 μM). The favorable safety profile of vidofludimus demonstrates that these undesirable adverse reactions are not a class effect of DHODH inhibitors, and is likely due, at least in part, to its lack of off-target effects and high selectivity of vidofludimus.
Anti-Viral Activity
As with all long-term use of immunomodulators, an increase in susceptibility to bacterial, viral, and fungal infections is a general concern [85, 86]. These agents can also trigger reactivation of otherwise harmless latent viruses such as the JC virus, which can cause progressive multifocal leukoencephalopathy (PML). PML is a rare but often fatal condition that is strongly linked to immunosuppressive therapy for conditions such as HIV infection, lymphomas and leukemias, and organ transplant [87, 88]. More recently, it has been seen in patients undergoing treatment for autoimmune diseases such as RA, CD, SLE, psoriasis, and MS [88–92]. However, despite the immunomodulatory effects of vidofludimus, the incidence of infections and infestation, and notably virus reactivations, was similar to placebo. This is consistent with in vitro studies showing that vidofludimus exerted antiviral effects. Vidofludimus effectively inhibited the replication of HIV and human cytomegalovirus (hCMV) at low micromolar concentrations in human peripheral blood mononuclear cells or fibroblasts infected with the respective virus. The activity against hCMV was in the range of ganciclovir [36], which is used in clinical practice to treat hCMV infections. Evidence from preclinical and clinical studies indicates that leflunomide and/or teriflunomide exert a similar antiviral effect, impacting the replication of a broad range of viruses, including herpes simplex virus-1 [93], hCMV [94–97], respiratory syncytial virus [98, 99], and BK virus [100–102].
Thus, it appears that the combination of selective immunosuppressive activity and antiviral activity may be a hallmark of DHODH inhibition. Since de novo pyrimidine synthesis is required to meet the demands of not only rapidly proliferating lymphocytes but also virus-infected cells, the DHODH inhibition by vidofludimus, teriflunomide, and leflunomide may explain the observed antiviral activity of the compounds. This may make inhibitors of DHODH a preferred immunomodulatory agent for the treatment of autoimmune diseases given the apparent protective effects against virus infection and reactivation.
Conclusion
The novel DHODH inhibitor vidofludimus demonstrated a positive safety profile in the COMPONENT trial for patients with RA. Many of the adverse effects that mar the safety profiles of the FDA-approved DHODH inhibitors leflunomide and teriflunomide, including alopecia, diarrhea, neutropenia, and hepatobiliary disorders, were observed at a similar rate following vidofludimus treatment compared with placebo. This is believed to be due to the high selectivity of vidofludimus for DHODH and a distinct absence of off-target effects. These data, along with its selective immunomodulatory activity and its demonstrated antiviral effects make vidofludimus a promising therapeutic candidate for clinical testing in a wide variety of immune-related diseases.
Acknowledgements
The authors wish to thank all patients, site staff, and investigators who participated in the COMPONENT study. Writing and editing support was provided by Richard R. McKay, PhD, of Full Spectrum Scientific LLC (East Windsor, NJ, USA).
Compliance with Ethical Standards
Funding
The COMPONENT study was funded by 4SC AG, the original developer of vidofludimus.
Contributors
All authors had full access to the study data, were involved in data interpretation, participated in manuscript preparation, and approved the final version for submission.
Conflict of interest
Hella Kohlhof, Manfred Groeppel, and Daniel Vitt were all employed by 4SC AG, the study sponsor, during the time the COMPONENT study was conducted. All authors are current employees of, and hold stock in, Immunic AG, which owns the rights to vidofludimus at this time. All authors are co-inventors for patents or patent applications covering vidofludimus.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This study received ethical approval from the Institutional Review Board or independent Ethics Committee at each site, and was approved by national regulatory agencies. Written informed consent was obtained from all participants prior to enrollment in the study.
Footnotes
MedDRA® (Medical Dictionary for Regulatory Activities) terminology is the international medical terminology developed under the auspices of the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH). The MedDRA trademark is registered by the International Federation of Pharmaceutical Manufacturers and Associations on behalf of the ICH.
Internal data on file with Immunic AG.
Internal data on file with Immunic AG.
Internal data on file with Immunic AG.
Internal data on file with Immunic AG.
References
- 1.Smolen JS, Aletaha D, McInnes IB. Rheumatoid arthritis. Lancet. 2016;388(10055):2023–2038. doi: 10.1016/S0140-6736(16)30173-8. [DOI] [PubMed] [Google Scholar]
- 2.Combe B, Landewe R, Lukas C, Bolosiu HD, Breedveld F, Dougados M, et al. EULAR recommendations for the management of early arthritis: report of a task force of the European Standing Committee for International Clinical Studies Including Therapeutics (ESCISIT) Ann Rheum Dis. 2007;66(1):34–45. doi: 10.1136/ard.2005.044354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Greene S, Watanabe K, Braatz-Trulson J, Lou L. Inhibition of dihydroorotate dehydrogenase by the immunosuppressive agent leflunomide. Biochem Pharmacol. 1995;50(6):861–867. doi: 10.1016/0006-2952(95)00255-x. [DOI] [PubMed] [Google Scholar]
- 4.Williamson RA, Yea CM, Robson PA, Curnock AP, Gadher S, Hambleton AB, et al. Dihydroorotate dehydrogenase is a high affinity binding protein for A77 1726 and mediator of a range of biological effects of the immunomodulatory compound. J Biol Chem. 1995;270(38):22467–22472. doi: 10.1074/jbc.270.38.22467. [DOI] [PubMed] [Google Scholar]
- 5.Chong AS-F, Rezai K, Gebel HM, Finnegan A, Foster P, Xu X, et al. Effects of leflunomide and other immunosuppressive agents on T cell proliferation in vitro. Transplantation. 1996;61(1):140–145. doi: 10.1097/00007890-199601150-00026. [DOI] [PubMed] [Google Scholar]
- 6.Davis JP, Cain GA, Pitts WJ, Magolda RL, Copeland RA. The immunosuppressive metabolite of leflunomide is a potent inhibitor of human dihydroorotate dehydrogenase. Biochemistry. 1996;35(4):1270–1273. doi: 10.1021/bi952168g. [DOI] [PubMed] [Google Scholar]
- 7.Löffler M, Jockel J, Schuster G, Becker C. Dihydroorotat-ubiquinone oxidoreductase links mitochondria in the biosynthesis of pyrimidine nucleotides. Mol Cell Biochem. 1997;174(1–2):125–129. [PubMed] [Google Scholar]
- 8.Löffler M, Grein K, Knecht W, Klein A, Bergjohann U. Dihydroorotate dehydrogenase. Profile of a novel target for antiproliferative and immunosuppressive drugs. Adv Exp Med Biol. 1998;431:507–513. [PubMed] [Google Scholar]
- 9.Lubberts E. IL-17/Th17 targeting: on the road to prevent chronic destructive arthritis? Cytokine. 2008;41(2):84–91. doi: 10.1016/j.cyto.2007.09.014. [DOI] [PubMed] [Google Scholar]
- 10.Klotz L, Eschborn M, Lindner M, Liebmann M, Herold M, Janoschka C, et al. Teriflunomide treatment for multiple sclerosis modulates T cell mitochondrial respiration with affinity-dependent effects. Sci Transl Med. 2019;11(490):eaao5563. doi: 10.1126/scitranslmed.aao5563. [DOI] [PubMed] [Google Scholar]
- 11.Fitzpatrick LR, Deml L, Hofmann C, Small JS, Groeppel M, Hamm S, et al. 4SC-101, a novel immunosuppressive drug, inhibits IL-17 and attenuates colitis in two murine models of inflammatory bowel disease. Inflamm Bowel Dis. 2010;16(10):1763–1777. doi: 10.1002/ibd.21264. [DOI] [PubMed] [Google Scholar]
- 12.Fitzpatrick LR, Small JS, Doblhofer R, Ammendola A. Vidofludimus inhibits colonic interleukin-17 and improves hapten-induced colitis in rats by a unique dual mode of action. J Pharmacol Exp Ther. 2012;342(3):850–860. doi: 10.1124/jpet.112.192203. [DOI] [PubMed] [Google Scholar]
- 13.Tan JL, Fogley RD, Flynn RA, Ablain J, Yang S, Saint-André V, et al. Stress from nucleotide depletion activates the transcriptional regulator HEXIM1 to suppress melanoma. Mol Cell. 2016;62(1):34–46. doi: 10.1016/j.molcel.2016.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Breedveld FC, Dayer J-M. Leflunomide: mode of action in the treatment of rheumatoid arthritis. Ann Rheum Dis. 2000;59(11):841–849. doi: 10.1136/ard.59.11.841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Siemasko KF, Chong AS, Williams JW, Bremer EG, Finnegan A. Regulation of B cell function by the immunosuppressive agent leflunomide. Transplantation. 1996;61(4):635–642. doi: 10.1097/00007890-199602270-00020. [DOI] [PubMed] [Google Scholar]
- 16.Remer CF, Weisman MH, Wallace DJ. Benefits of leflunomide in systemic lupus erythematosus: a pilot observational study. Lupus. 2001;10(7):480–483. doi: 10.1191/096120301678416033. [DOI] [PubMed] [Google Scholar]
- 17.Cada DJ, Demaris K, Levien TL, Baker DE. Teriflunomide. Hosp Pharm. 2013;48(3):231–240. doi: 10.1310/hpj4803-231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kunkel G, W Cannon G. Leflunomide in the treatment of rheumatoid arthritis. Expert Rev Clin Immunol. 2006;2(1):17–31. doi: 10.1586/1744666X.2.1.17. [DOI] [PubMed] [Google Scholar]
- 19.Tam L-S, Li EK, Wong C-K, Lam CW, Szeto C-C. Double-blind, randomized, placebo-controlled pilot study of leflunomide in systemic lupus erythematosus. Lupus. 2004;13(8):601–604. doi: 10.1191/0961203304lu1067sr. [DOI] [PubMed] [Google Scholar]
- 20.Wang H, Cui T, Hou F, Ni Z, Chen X, Lu F, et al. Induction treatment of proliferative lupus nephritis with leflunomide combined with prednisone: A prospective multi-centre observational study. Lupus. 2008;17(7):638–644. doi: 10.1177/0961203308089408. [DOI] [PubMed] [Google Scholar]
- 21.Alcorn N, Saunders S, Madhok R. Benefit–risk assessment of leflunomide. Drug Saf. 2009;32(12):1123–1134. doi: 10.2165/11316650-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 22.Günendi Z, Benli E, Göğüş F, Atalay F. Long term use of leflunomide as a cause of severe diarrhea? Arch Rheumatol. 2010;25(1):41–43. [Google Scholar]
- 23.Aithal GP. Hepatotoxicity related to antirheumatic drugs. Nat Rev Rheumatol. 2011;7:139–150. doi: 10.1038/nrrheum.2010.214. [DOI] [PubMed] [Google Scholar]
- 24.O’Connor P, Wolinsky JS, Confavreux C, Comi G, Kappos L, Olsson TP, et al. Randomized trial of oral teriflunomide for relapsing multiple sclerosis. N Engl J Med. 2011;365(14):1293–1303. doi: 10.1056/NEJMoa1014656. [DOI] [PubMed] [Google Scholar]
- 25.Keen HI, Conaghan PG, Tett SE. Safety evaluation of leflunomide in rheumatoid arthritis. Expert Opin Drug Saf. 2013;12(4):581–588. doi: 10.1517/14740338.2013.798299. [DOI] [PubMed] [Google Scholar]
- 26.Wu G-C, Xu X-D, Huang Q, Wu H. Leflunomide: friend or foe for systemic lupus erythematosus? Rheumatol Int. 2013;33(2):273–276. doi: 10.1007/s00296-012-2508-z. [DOI] [PubMed] [Google Scholar]
- 27.O’Connor P, Comi G, Freedman MS, Miller AE, Kappos L, Bouchard J-P, et al. Long-term safety and efficacy of teriflunomide: nine-year follow-up of the randomized TEMSO study. Neurology. 2016;86(10):920–930. doi: 10.1212/WNL.0000000000002441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Duquette A, Frenette AJ, Doré M. Chronic diarrhea associated with high teriflunomide blood concentration. Rheumatol Ther. 2016;3(1):179–185. doi: 10.1007/s40744-016-0025-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Van Roon EN, Jansen TLTA, Mourad L, Houtman PM, Bruyn GAW, Griep EN, et al. Leflunomide in active rheumatoid arthritis: a prospective study in daily practice. Br J Clin Pharmacol. 2004;57(6):790–797. doi: 10.1111/j.1365-2125.2004.02075.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bettembourg-Brault I, Gossec L, Pham T, Gottenberg JE, Damiano J, Dougados M. Leflunomide in rheumatoid arthritis in daily practice: treatment discontinuation rates in comparison with other DMARDs. Clin Exp Rheumatol. 2006;24(2):168–171. [PubMed] [Google Scholar]
- 31.Lee S-W, Park H-J, Kim BK, Han K-H, Lee S-K, Kim SU, et al. Leflunomide increases the risk of silent liver fibrosis in patients with rheumatoid arthritis receiving methotrexate. Arthritis Res Ther. 2012;14(5):R232. doi: 10.1186/ar4075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.US FDA. FDA Drug Safety Communication: New boxed warning for severe liver injury with arthritis drug Arava (leflunomide). US FDA; 13 Jul 2010.
- 33.US FDA. FDA Approved Labeling and Full Prescribing Information for Aubagio (teriflunomide). US FDA; 12 Sep 2012.
- 34.Herrlinger KR, Diculescu M, Fellermann K, Hartmann H, Howaldt S, Nikolov R, et al. Efficacy, safety and tolerability of vidofludimus in patients with inflammatory bowel disease: the ENTRANCE study. J Crohn’s Colitis. 2013;7(8):636–643. doi: 10.1016/j.crohns.2012.09.016. [DOI] [PubMed] [Google Scholar]
- 35.Sierakowski S, Dietrich B, Hentsch B, Ammendola A. Efficacy, safety and pharmacokinetics of vidofludimus, a novel oral immunomodulator, in patients with active rheumatoid arthritis on methotrexate background therapy: The COMPONENT study. American College of Rheumatology/Association of Rheumatology Health Professionals (ACR/ARHP) Annual Meeting, Chicago; 2011.
- 36.Kohlhof H. IMU-838 in inflammatory bowel disease: New oral treatment with promising safety profile. GI Inflammatory Diseases Summit; June 24–26, Boston; 2019.
- 37.Felson DT, Anderson JJ, Boers M, Bombardier C, Furst D, Goldsmith C, et al. American College of Rheumatology. Preliminary definition of improvement in rheumatoid arthritis. Arthritis Rheumatol. 1995;38(6):727–735. doi: 10.1002/art.1780380602. [DOI] [PubMed] [Google Scholar]
- 38.Hwang TJ, Carpenter D, Lauffenburger JC, Wang B, Franklin JM, Kesselheim AS. Failure of investigational drugs in late-stage clinical development and publication of trial results. JAMA Intern Med. 2016;176(12):1826–1833. doi: 10.1001/jamainternmed.2016.6008. [DOI] [PubMed] [Google Scholar]
- 39.The World Health Organization. WHO Statement on Public Disclosure of Clinical Trial Results. April 9, 2015.
- 40.Fragoso YD, Brooks JBB. Leflunomide and teriflunomide: altering the metabolism of pyrimidines for the treatment of autoimmune diseases. Expert Rev Clin Pharmacol. 2015;8(3):315–320. doi: 10.1586/17512433.2015.1019343. [DOI] [PubMed] [Google Scholar]
- 41.Wang Y, Li K, Gao D, Luo G, Zhao Y, Wang X, et al. Combination therapy of leflunomide and glucocorticoids for the maintenance of remission in patients with IgG4-related disease: a retrospective study and literature review. Intern Med J. 2017;47(6):680–689. doi: 10.1111/imj.13430. [DOI] [PubMed] [Google Scholar]
- 42.Vijaysekharan K, Punatar S, Bonda A, Mohite A, Shanmugam K, Nayak L, et al. Leflunomide: is it the game changer in musculoskeletal chronic graft versus host disease? Indian J Hematol Blood Transfus. 2018;34(3):566–567. doi: 10.1007/s12288-018-0929-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yao X, Wu Y, Jiang J, Chen X, Liu D, Hu P. A population pharmacokinetic study to accelerate early phase clinical development for a novel drug, teriflunomide sodium, to treat systemic lupus erythematosus. Eur J Pharm Sci. 2019;136:104942. doi: 10.1016/j.ejps.2019.05.020. [DOI] [PubMed] [Google Scholar]
- 44.Zhang C, Chu M. Leflunomide: a promising drug with good antitumor potential. BBRC. 2018;496(2):726–730. doi: 10.1016/j.bbrc.2018.01.107. [DOI] [PubMed] [Google Scholar]
- 45.Lolli ML, Sainas S, Pippione AC, Giorgis M, Boschi D, Dosio F. Use of human dihydroorotate dehydrogenase (hDHODH) inhibitors in autoimmune diseases and new perspectives in cancer therapy. Recent Patents Anticancer Drug Discov. 2018;13(1):86–105. doi: 10.2174/1574892812666171108124218. [DOI] [PubMed] [Google Scholar]
- 46.Hochberg MC, Chang RW, Dwosh I, Lindsey S, Pincus T, Wolfe F. The American College of Rheumatology 1991 revised criteria for the classification of global functional status in rheumatoid arthritis. Arthritis Rheumatol. 1992;35(5):498–502. doi: 10.1002/art.1780350502. [DOI] [PubMed] [Google Scholar]
- 47.Ali A, Rasheed A, Siddiqui AA, Naseer M, Wasim S, Akhtar W. Non-parametric test for ordered medians: the Jonckheere Terpstra test. Int J Stat Med Res. 2015;4:203–207. [Google Scholar]
- 48.Swoger JM, Regueiro M. Stopping, continuing, or restarting immunomodulators and biologics when an infection or malignancy develops. Inflamm Bowel Dis. 2014;20(5):926–935. doi: 10.1097/MIB.0000000000000002. [DOI] [PubMed] [Google Scholar]
- 49.Celius EG. Infections in patients with multiple sclerosis: implications for disease-modifying therapy. Acta Neurol Scand. 2017;136(S201):34–36. doi: 10.1111/ane.12835. [DOI] [PubMed] [Google Scholar]
- 50.Simerville JA, Maxted WC, Pahira JJ. Urinalysis: a comprehensive review. Am Fam Physician. 2005;71(6):1153–1162. [PubMed] [Google Scholar]
- 51.Sharp VJ, Lee DK, Askeland EJ. Urinalysis: case presentations for the primary care physician. Am Fam Physician. 2014;90(8):542–547. [PubMed] [Google Scholar]
- 52.Grossfeld GD, Wolf JS, Jr, Litwan MS, Hricak H, Shuler CL, Agerter DC, et al. Asymptomatic microscopic hematuria in adults: summary of the AUA best practice policy recommendations. Am Fam Physician. 2001;63(6):1145–1154. [PubMed] [Google Scholar]
- 53.Silverman E, Mouy R, Spiegel L, Jung LK, Saurenmann RK, Lahdenne P, et al. Leflunomide or methotrexate for juvenile rheumatoid arthritis. N Engl J Med. 2005;352(16):1655–1666. doi: 10.1056/NEJMoa041810. [DOI] [PubMed] [Google Scholar]
- 54.Silverman E, Spiegel L, Hawkins D, Petty R, Goldsmith D, Schanberg L, et al. Long-term open-label preliminary study of the safety and efficacy of leflunomide in patients with polyarticular-course juvenile rheumatoid arthritis. Arthritis Rheumatol. 2005;52(2):554–562. doi: 10.1002/art.20861. [DOI] [PubMed] [Google Scholar]
- 55.Tam LS, Li EK, Wong CK, Lam CWK, Li WC, Szeto CC. Safety and efficacy of leflunomide in the treatment of lupus nephritis refractory or intolerant to traditional immunosuppressive therapy: an open label trial. Ann Rheum Dis. 2006;65(3):417–418. doi: 10.1136/ard.2005.044248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.van Woerkom JM, Kruize AA, Geenen R, van Roon EN, Goldschmeding R, Verstappen SMM, et al. Safety and efficacy of leflunomide in primary Sjögren’s syndrome: a phase II pilot study. Ann Rheum Dis. 2007;66(8):1026–1032. doi: 10.1136/ard.2006.060905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Haibel H, Rudwaleit M, Braun J, Sieper J. Six months open label trial of leflunomide in active ankylosing spondylitis. Ann Rheum Dis. 2005;64(1):124–126. doi: 10.1136/ard.2003.019174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Boswell JS, Costner MI. Leflunomide as adjuvant treatment of dermatomyositis. J Am Acad Dermatol. 2008;58(3):403–406. doi: 10.1016/j.jaad.2007.08.014. [DOI] [PubMed] [Google Scholar]
- 59.Metzler C, Miehle N, Manger K, Iking-Konert C, de Groot K, Hellmich B, et al. Elevated relapse rate under oral methotrexate versus leflunomide for maintenance of remission in Wegener’s granulomatosis. Rheumatology. 2007;46(7):1087–1091. doi: 10.1093/rheumatology/kem029. [DOI] [PubMed] [Google Scholar]
- 60.Bremer JP, Ullrich S, Laudien M, Gross WL, Lamprecht P. Methotrexate plus leflunomide for the treatment of relapsing Wegener’s granulomatosis. A retrospective uncontrolled study. Clin Exp Rheumatol. 2010;28(1 Suppl 57):67–71. [PubMed] [Google Scholar]
- 61.Smolen JS, Kalden JR, Scott DL, Rozman B, Kvien TK, Larsen A, et al. Efficacy and safety of leflunomide compared with placebo and sulphasalazine in active rheumatoid arthritis: a double-blind, randomised, multicentre trial. European Leflunomide Study Group. Lancet. 1999;353(9149):259–266. doi: 10.1016/s0140-6736(98)09403-3. [DOI] [PubMed] [Google Scholar]
- 62.Breedveld P, Zelcer N, Pluim D, Sönmezer Ö, Tibben MM, Beijnen JH, et al. Mechanism of the pharmacokinetic interaction between methotrexate and benzimidazoles: potential role for breast cancer resistance protein in clinical drug–drug interactions. Cancer Res. 2004;64(16):5804–5811. doi: 10.1158/0008-5472.CAN-03-4062. [DOI] [PubMed] [Google Scholar]
- 63.Volk EL, Schneider E. Wild-type breast cancer resistance protein (BCRP/ABCG2) is a methotrexate polyglutamate transporter. Cancer Res. 2003;63(17):5538–5543. [PubMed] [Google Scholar]
- 64.Mao Q, Unadkat JD. Role of the breast cancer resistance protein (BCRP/ABCG2) in drug transport-an update. AAPS J. 2014;17(1):65–82. doi: 10.1208/s12248-014-9668-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kis E, Nagy T, Jani M, Molnár É, Jánossy J, Ujhellyi O, et al. Leflunomide and its metabolite A771726 are high affinity substrates of BCRP: implications for drug resistance. Ann Rheum Dis. 2009;68(7):1201–1207. doi: 10.1136/ard.2007.086264. [DOI] [PubMed] [Google Scholar]
- 66.Miura D, Anzai N, Jutabha P, Chanluang S, He X, Fukutomi T, et al. Human urate transporter 1 (hURAT1) mediates the transport of orotate. J Physiol Sci. 2011;61(3):253–257. doi: 10.1007/s12576-011-0136-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.US FDA, Center for Drug Evaluation and Research. CDER clinical pharmacology and biopharmaceutics review of teriflunomide.
- 68.Perez-Ruiz F, Nolla JM. Influence of leflunomide on renal handling of urate and phosphate in patients with rheumatoid arthritis. J Clin Rheumatol. 2003;9(4):215–218. doi: 10.1097/01.rhu.0000081470.31167.8b. [DOI] [PubMed] [Google Scholar]
- 69.Hopkins AM, Wiese MD, Proudman SM, O’Doherty CE, Upton RN, Foster DJR. Genetic polymorphism of CYP1A2 but not total or free teriflunomide concentrations is associated with leflunomide cessation in rheumatoid arthritis. Br J Clin Pharmacol. 2016;81(1):113–123. doi: 10.1111/bcp.12760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.US FDA. FDA approved labeling and full prescribing information for Arava (leflunomide). US FDA; 2015.
- 71.Johnson KM, Zhou H, Lin F, Ko JJ, Herrera V. Real-world adherence and persistence to oral disease-modifying therapies in multiple sclerosis patients over 1 year. J Manag Care Spec Pharm. 2017;23(8):844–852. doi: 10.18553/jmcp.2017.23.8.844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Connell WR, Kamm MA, Ritchie JK, Lennard-Jones JE. Bone marrow toxicity caused by azathioprine in inflammatory bowel disease: 27 years of experience. Gut. 1993;34(8):1081–1085. doi: 10.1136/gut.34.8.1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lewis JD, Abramson O, Pascua M, Liu L, Asakura LM, Velayos FS, et al. Timing of myelosuppression during thiopurine therapy for inflammatory bowel disease: implications for monitoring recommendations. Clin Gastroenterol Hepatol. 2009;7(11):1195–1201. doi: 10.1016/j.cgh.2009.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hou JK, Kramer JR, Richardson P, Sansgiry S, El-Serag HB. Myelosuppression monitoring after immunomodulator initiation in veterans with inflammatory bowel disease: a national practice audit. Aliment Pharmacol Ther. 2012;36(11–12):1049–1056. doi: 10.1111/apt.12075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Lam NC, Ghetu MV, Bieniek ML. Systemic lupus erythematosus: primary care approach to diagnosis and management. Am Fam Physician. 2016;94(4):284–294. [PubMed] [Google Scholar]
- 76.Kulkarni OP, Sayyed SG, Kantner C, Ryu M, Schnurr M, Sárdy M, et al. 4SC-101, a novel small molecule dihydroorotate dehydrogenase inhibitor, suppresses systemic lupus erythematosus in MRL-(Fas)lpr mice. Am J Pathol. 2010;176(6):2840–2847. doi: 10.2353/ajpath.2010.091227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Mattar T, Kochhar K, Bartlett R, Bremer EG, Finnegan A. Inhibition of the epidermal growth factor receptor tyrosine kinase activity by leflunomide. FEBS Lett. 1993;334(2):161–164. doi: 10.1016/0014-5793(93)81704-4. [DOI] [PubMed] [Google Scholar]
- 78.Nikcevich DA, Finnegan A, Chong ASF, Williams JW, Bremer EG. Inhibition of Interleukin 2 (IL-2)-stimulated tyrosine kinase activity by leflunomide. Agents Actions. 1994;41(2):C279–C282. [Google Scholar]
- 79.Xu X, Williams JW, Bremer EG, Finnegan A, Chong AS-F. Inhibition of protein tyrosine phosphorylation in T cells by a novel immunosuppressive agent, leflunomide. J Biol Chem. 1995;270(21):12398–12403. doi: 10.1074/jbc.270.21.12398. [DOI] [PubMed] [Google Scholar]
- 80.Elder RT, Xu X, Williams JW, Gong H, Finnegan A, Chong AS. The immunosuppressive metabolite of leflunomide, A77 1726, affects murine T cells through two biochemical mechanisms. J Immunol. 1997;159(1):22–27. [PubMed] [Google Scholar]
- 81.Siemasko K, Chong AS-F, Jäck H-M, Gong H, Williams JW, Finnegan A. Inhibition of JAK3 and STAT6 tyrosine phosphorylation by the immunosuppressive drug leflunomide leads to a block in IgG1 production. J Immunol. 1998;160(4):1581–1588. [PubMed] [Google Scholar]
- 82.Manna SK, Aggarwal BB. Immunosuppressive leflunomide metabolite (A77 1726) blocks TNF-dependent nuclear factor-κB activation and gene expression. J Immunol. 1999;162(4):2095–2102. [PubMed] [Google Scholar]
- 83.O’Donnell EF, Saili KS, Koch DC, Kopparapu PR, Farrer D, Bisson WH, et al. The anti-inflammatory drug leflunomide is an agonist of the aryl hydrocarbon receptor. PLoS One. 2010;5(10):e13128. doi: 10.1371/journal.pone.0013128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Buettner R, Morales CJ, Caserta E, Viola D, Palmer JM, Wu X, et al. Leflunomide inhibits c-Myc signaling and impairs myeloma cell growth. Blood. 2017;130(Suppl 1):4426. [Google Scholar]
- 85.Orlicka K, Barnes E, Culver EL. Prevention of infection caused by immunosuppressive drugs in gastroenterology. Ther Adv Chronic Dis. 2013;4(4):167–185. doi: 10.1177/2040622313485275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Wingerchuk DM, Carter JL. Multiple sclerosis: current and emerging disease-modifying therapies and treatment strategies. Mayo Clin Proc. 2014;89(2):225–240. doi: 10.1016/j.mayocp.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 87.Palazzo E, Yahia SA. Progressive multifocal leukoencephalopathy in autoimmune diseases. Joint Bone Spine. 2012;79(4):351–355. doi: 10.1016/j.jbspin.2011.11.002. [DOI] [PubMed] [Google Scholar]
- 88.Berger JR. Classifying PML risk with disease modifying therapies. Mult Scler Relat Disord. 2017;12:59–63. doi: 10.1016/j.msard.2017.01.006. [DOI] [PubMed] [Google Scholar]
- 89.US FDA. Communication About an Ongoing Safety Review of CellCept (mycophenolate mofetil) and Myfortic (mycophenolic acid). US FDA; 10 Apr 2008.
- 90.US FDA. FDA Statement on the Voluntary Withdrawal of Raptiva (efalizumab) from the U.S. Market. US FDA; 8 Apr 2009.
- 91.US FDA. FDA Approved Labeling and Full Prescribing Information for Rituxan (rituximab). US FDA; Feb 2010.
- 92.US FDA. FDA Drug Safety Communication: New risk factor for Progressive Multifocal Leukoencephalopathy (PML) associated with Tysabri (natalizumab). US FDA; 20 Jan 2012.
- 93.Knight DA, Hejmanowski AQ, Dierksheide JE, Williams JW, Chong AS, Waldman WJ. Inhibition of herpes simplex virus type 1 by the experimental immunosuppressive agent leflunomide. Transplantation. 2001;71(1):170–174. doi: 10.1097/00007890-200101150-00031. [DOI] [PubMed] [Google Scholar]
- 94.Chong AS, Zeng H, Knight DA, Shen J, Meister GT, Williams JW, et al. concurrent antiviral and immunosuppressive activities of leflunomide in vivo. Am J Transpl. 2006;6(1):69–75. doi: 10.1111/j.1600-6143.2005.01152.x. [DOI] [PubMed] [Google Scholar]
- 95.Avery RK, Mossad SB, Poggio E, Lard M, Budev M, Bolwell B, et al. Utility of leflunomide in the treatment of complex cytomegalovirus syndromes. Transplantation. 2010;90(4):419–426. doi: 10.1097/TP.0b013e3181e94106. [DOI] [PubMed] [Google Scholar]
- 96.Chacko B, John GT. Leflunomide for cytomegalovirus: bench to bedside. Transpl Infect Dis. 2012;14(2):111–120. doi: 10.1111/j.1399-3062.2011.00682.x. [DOI] [PubMed] [Google Scholar]
- 97.Morita S, Shinoda K, Tamaki S, Kono H, Asanuma H, Nakagawa K, et al. Successful low-dose leflunomide treatment for ganciclovir-resistant cytomegalovirus infection with high-level antigenemia in a kidney transplant: a case report and literature review. J Clin Virol. 2016;82:133–138. doi: 10.1016/j.jcv.2016.07.015. [DOI] [PubMed] [Google Scholar]
- 98.Davis IC, Lazarowski ER, Hickman-Davis JM, Fortenberry JA, Chen F-P, Zhao X, et al. Leflunomide prevents alveolar fluid clearance inhibition by respiratory syncytial virus. Am J Respir Crit Care Med. 2006;173(6):673–682. doi: 10.1164/rccm.200508-1200OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Cox Dunn MC, Knight DA, Waldman WJ. Inhibition of respiratory syncytial virus in vitro and in vivo by the immunosuppressive agent leflunomide. Antivir Ther. 2011;16(3):309–317. doi: 10.3851/IMP1763. [DOI] [PubMed] [Google Scholar]
- 100.Williams JW, Javaid B, Kadambi PV, Gillen D, Harland R, Thistlewaite JR, et al. Leflunomide for polyomavirus type BK nephropathy. N Engl J Med. 2005;352(11):1157–1158. doi: 10.1056/NEJM200503173521125. [DOI] [PubMed] [Google Scholar]
- 101.Bernhoff E, Tylden GD, Kjerpeseth LJ, Gutteberg TJ, Hirsch HH, Rinaldo CH. Leflunomide inhibition of BK virus replication in renal tubular epithelial cells. J Virol. 2010;84(4):2150–2156. doi: 10.1128/JVI.01737-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Nesselhauf N, Strutt J, Bastani B. Evaluation of leflunomide for the treatment of BK viremia and biopsy proven BK nephropathy: a single center experience. J Nephropathol. 2016;5(1):34–37. doi: 10.15171/jnp.2016.06. [DOI] [PMC free article] [PubMed] [Google Scholar]