Abstract
Research on visual perception in schizophrenia suggests a deficit in motion processing. Specifically, difficulties with discriminating motion speed are commonly reported. However, speed discrimination tasks typically require participants to make judgments about the difference between two stimuli in a two-interval forced choice (2IFC) task. Such tasks not only tap into speed processing mechanisms, but also rely on higher executive functioning including working memory and attention which has been shown to be compromised in schizophrenia. We used the Flash Lag illusion to examine speed processing in patients with schizophrenia. Based on previous research showing a strong dependence between motion speed and the illusion magnitude, we expected a deficit in speed processing to alter this relationship. A motion processing deficit in patients would also predict overall reductions in perceived lag. We found the magnitude and speed dependence of the Flash Lag illusion to be similar in patients and controls. Together, the findings suggest no general abnormality in motion speed processing in schizophrenia.
Keywords: Schizophrenia, Motion perception, Flash lag effect
1. Introduction
Recent studies on visual processing in schizophrenia demonstrate numerous perceptual deficits (Cutting and Dunne, 1986; Phillipson and Harris, 1985; Waters et al., 2014; Bunney Jr et al., 1999; Kantrowitz et al., 2009; Butler et al., 2008; Butler and Javitt, 2005; Butler et al., 2003; Silverstein, 2016; Yoon et al., 2010; Uhlhaas et al., 2005; Uhlhaas and Mishara, 2006; Thoenes and Oberfeld, 2017; O'donnell et al., 2002; Notredame et al., 2014). In particular, evidence suggests a deficit in motion perception that might underlie other disruptions in behaviour associated with the disorder (Chen et al., 1999a; Chen et al., 2003; Chen et al., 2004; Chen, 2011; Tadin et al., 2006; Kim et al., 2005; Kim et al., 2006; Spencer et al., 2013). For instance, it has been reported that patients exhibit difficulties in discriminating biological motion from non-biological motion (Kim et al., 2005; Okruszek et al., 2015; Spencer et al., 2013) that might underlie some social cognitive impairments (Couture et al., 2006; Fett et al., 2011; Green et al., 2015). Patients also show impairments in apparent motion perception which have been linked to positive and disorganization symptoms (Tschacher et al., 2008; Sanders et al., 2013). In addition, patients are reported to exhibit higher coherence thresholds for detecting global motion direction (Chen et al., 2003; Carter et al., 2017; Li, 2002; Chen et al., 2005; Slaghuis et al., 2007; Stuve et al., 1997), which might generally impede daily functioning in dynamic visual environments.
Research on motion perception in schizophrenia suggests a severe deficit in global motion processing (Carter et al., 2017; Bennett et al., 2016; Chen et al., 2003; Brittain et al., 2010), while local processing seems to be relatively intact (Carter et al., 2017; Chen et al., 2003). This indicates a functional impairment in higher-order motion areas like V5/MT+ (Britten et al., 1993; Zeki, 1974; Albright, 1984; Pasternak et al., 1985; Van Essen et al., 1981; Dumoulin et al., 2000; van Kemenade et al., 2014), consistent with a cortical lower limit to visual dysfunction in schizophrenia (Tibber et al., 2013; Yang et al., 2013; Kaliuzhna et al., 2019; Palmer et al., 2018b; Palmer et al., 2018a; Silverstein, 2016; Yoon et al., 2009; Yoon et al., 2010; Seymour et al., 2013; Dakin et al., 2005; Keane et al., 2012; Tadin et al., 2006; Butler et al., 2008; Carter et al., 2017; Uhlhaas et al., 2006; Uhlhaas and Mishara, 2006). Also in support of this is evidence from functional magnetic resonance imaging (fMRI) suggesting hypofunction in V5/MT+ in schizophrenia (Lencer et al., 2005; Stuve et al., 1997).
The most consistent finding of a motion processing deficit in schizophrenia is an impairment in speed discrimination (Clementz et al., 2007; Chen, 2011; Chen et al., 2004; Chen et al., 1999b; Chen et al., 1999a; Chen et al., 2003; Bidwell et al., 2006; Chen et al., 2006; Kim et al., 2006; Hong et al., 2009; Brenner et al., 2003). Speed processing deficits have been linked to V5/MT+ dysfunction and smooth pursuit deficits, commonly reported with the disorder (Stuve et al., 1997; O'Driscoll and Callahan, 2008; Lencer et al., 2005). In a typical motion discrimination task, participants observe two successive motion stimuli and decide whether the first or second stimulus is moving faster. Patients consistently exhibit higher velocity discrimination thresholds than controls, meaning they require larger speed differences to successfully distinguish the two stimuli. This deficit is shown to be present irrespective of the type of moving targets used (Chen et al., 1999b; Kim et al., 2006; Clementz et al., 2007; Hong et al., 2009) and is most prominent at intermediate speeds (e.g., 10°/s) (Chen et al., 1999b; Chen et al., 1999a).
While current evidence suggests speed processing abnormalities exist in schizophrenia, studies employing speed discrimination tasks may be confounded by the presence of a more generalised deficit associated with the disorder. For instance, a working memory deficit (Forbes et al., 2009; Lee and Park, 2005; Conklin et al., 2000; Goldman-Rakic, 1994; Landrø et al., 2001; Meda et al., 2009; Park and Gooding, 2014) or attention deficit (Fioravanti et al., 2012; Fioravanti et al., 2005; Chen and Faraone, 2000) could account for findings of poor task performance in schizophrenia, which might otherwise appear to indicate a specific speed processing impairment. In the typical two-interval forced choice (2IFC) speed discrimination task, participants are required to make a comparison between two stimuli (Chen et al., 1999a; Chen et al., 2004; Chen et al., 2006; Chen et al., 2005; Kim et al., 2006; Clementz et al., 2007; Hong et al., 2009). Such judgments not only require the engagement of speed processing mechanisms, but rely on intact working memory and focussed attention to make an accurate comparison. Thus, poor performance by patients in such tasks could be due to a cognitive deficit related to poor working memory or an attention deficit rather than a speed processing deficit per se.
To circumvent the confounding effects of a generalised deficit on task performance, recent research has used visual illusions to examine the integrity of visual processing in schizophrenia (Dakin et al., 2005; Kaliuzhna et al., 2019; Palmer et al., 2018b; Tibber et al., 2013; Yang et al., 2013; Tadin et al., 2006; Chen et al., 2008; Koethe et al., 2009; Tschacher et al., 2006; Crawford et al., 2010; Norton et al., 2008; Notredame et al., 2014; Dima et al., 2010; Dima et al., 2009; Keane et al., 2013; Keane et al., 2016; Uhlhaas et al., 2006; Kantrowitz et al., 2009; Letourneau and Lavoie, 1973; Letourneau, 1974). Visual illusions are usually well validated and known to probe the functional integrity of a relatively narrow range of mechanisms. Also, because they have typically been tested under multiple stimulus manipulations in healthy participants, they can be used to predict specific hypothesis-consistent patterns of performance from patients that are different from controls and what would be expected from a generalised deficit (Silverstein and Keane, 2011b). However, of the many reports of motion processing deficits in schizophrenia, only few studies have used visual illusions (Tschacher et al., 2006; Crawford et al., 2010; Tschacher et al., 2008; Sanders et al., 2013; Yang et al., 2013; Tadin et al., 2006) and no study has specifically examined the processing of motion speed.
The Flash Lag illusion (FLI) is a robust visual illusion that is heavily dependent on motion speed (Krekelberg and Lappe, 2001; Eagleman and Sejnowski, 2007; Arnold et al., 2009; Brenner and Smeets, 2000; Sarich et al., 2007; Chappell and Mullen, 2010; Hubbard, 2014; Khan and Timney, 2007; Linares and Lopez-Moliner, 2007; Linares et al., 2009; Watanabe et al., 2001; Nijhawan et al., 2004; Nijhawan, 1994; Nijhawan, 2002; Shioiri et al., 2010; Whitney et al., 2000). It is observed when a flashed bar is presented in physical alignment with a moving target but appears to lag behind the moving target (Nijhawan, 1994). It is consistently shown that the size of the FLI increases linearly with the speed of the moving target (Hubbard and Bharucha, 1988, Hubbard, 1990, Krekelberg and Lappe, 1999, Nijhawan, 1994), making it an excellent tool to assess the integrity of speed processing mechanisms without requiring participants to discriminate between motion speeds directly, as is the case in most speed discrimination experiments.
Examining speed perception in schizophrenia using the FLI eliminates the confounding factors commonly associated with 2IFC speed discrimination tasks, such as high working memory demands. Importantly, it allows for careful testing of specific patterns of performance that would be predicted from a speed processing deficit. Specifically, an impairment in speed processing would predict a weaker relationship between FLI magnitude and motion speed (i.e., slope and goodness of fit) compared to controls. That is, a selective deficit in speed processing would be evidenced by a statistically significant interaction between motion speed and group, being most evident at intermediate speeds as the research suggests (Chen et al., 1999b; Chen et al., 1999a). Also, the use of the FLI allows for predictions about a specific motion deficit or general attention deficit to be pitted against each other. For instance, research in healthy participants shows that disruption to motion area V5/MT+ reduces perceived lag (Maus et al., 2012). We would, thus, predict that a motion deficit in schizophrenia results in reduced FLIs compared to controls. On the other hand, limited attentional resources have been shown to increase FLIs in healthy participants (Sarich et al., 2007; Hayes and Freyd, 2002; Shioiri et al., 2010; Baldo and Namba, 2002; Baldo et al., 2002). Hence, if performance is affected by an attention deficit in patients, we would expect to observe larger FLIs in this group.
Currently, it is also unclear whether speed processing deficits in schizophrenia impact other aspects of functioning in dynamic visual environments. Some evidence suggests patients experience twice as many car accidents compared to other drivers (Edlund et al., 1989; Lipskaya-Velikovsky et al., 2013). The Flash Lag illusion demonstrates that judgments of the relative position between stationary and moving objects are affected by motion speed. By examining how speed processing deficits affect other visual judgments, the current study aids our understanding of how such deficits might contribute to other impairments in daily functioning (Green et al., 2008; Javitt, 2009).
2. Materials and methods
2.1. Participants
Eighteen outpatients who met the DSM-IV criteria for schizophrenia and 21 healthy controls recruited from the general population performed the experiment. The two groups were matched on mean age (patients 33.3 yo (SD = 5.6), controls 33.7 yo (SD = 6.4), gender (50% female)) and years of education (patients 15.8 y (SD = 4.2), controls 15.4 (SD = 3.7)). At the time of testing all patients were stable, had a mean illness duration of 9 years (SD = 6.9) and received antipsychotic medication (Chlorpromazine equivalent: 282 mg/day; SD = 256.7). An experienced psychiatrist conducted the clinical interview and administered the Positive and Negative Symptoms Scale (Kay et al., 1987). At the time of testing, the patients were stable and symptom severity was low: the mean positive symptom score was 11.9 (SD = 4.6), the negative score was 13.9 (SD = 5.2), with a general score of 24.8 (SD = 7.9). All participants had normal or corrected-to-normal visual acuity. Participants gave written informed consent to take part in the experiment and the study was approved by the Charité Universitätsmedizin Berlin Medical Ethics Review Committee.
2.2. Procedure
Stimuli were presented on a gamma corrected 48-cm Samtron CRT colour monitor (resolution 1024 × 768; 100 Hz) using Matlab and the Psychophysics Toolbox (Pelli, 1997; Brainard, 1997). Subjects were seated in a darkened experimental booth with a chin rest 57 cm from the CRT monitor. Subjects practiced with 10 trials before completing the main experiment.
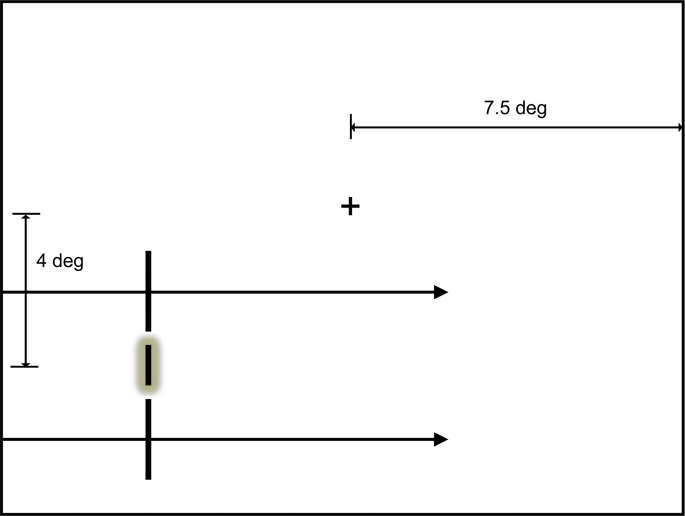
Our procedure closely followed (Whitney et al., 2000). The moving stimulus comprised a pair of vertically aligned white (34.5 cd/m2) target bars translating horizontally 4° below a white fixation point on a grey background. Each target bar subtended 0.50° in width and 2° in height (Fig. 1) and moved concurrently at one of 10 speeds (3, 5, 7, 9, 11, 13, 15, 20, 25, 30°/s). The distance between the two bars (2°) was constant.
Fig. 1.
Schematic of the stimulus display for measuring the Flash Lag illusion. The moving target consists of two vertically aligned vertical bars moving from left to right. The flashed object consists of a vertical bar which is briefly flashed in the gap within the moving target bars when they are aligned. The position of the flashed object appears to lag behind the position of the moving target.
The moving bars were presented within a 15° horizontal window (within 7.5° of fixation). The bars always moved from left to the right. Each trial began by an initial translation (>3.5°) of the moving bars, after which another white bar (subtending 0.50° in width and 1° in height) was flashed for one video frame (16.7 ms) between the moving target bars.
We used a set of interleaved adaptive staircase procedures, where participants were asked on each trial to indicate whether they perceived the flash to precede or follow the moving target bars. The horizontal position of the flash relative to the moving bars was updated after each trial. On the first trial of each speed condition, the flash and target bars were horizontally aligned. On every subsequent trial, the position of the flashed bar relative to the moving bars was updated (by an increment of 0.5° for the first 3 trials and 0.25° on subsequent trials, see Cornsweet Tom, 1962). The extent of apparent lag (FLI) was determined as the flash setting that appeared spatially aligned with the moving bars (based on the average of the last two reversals of the staircase over the 15 trials for a given speed condition). For example, when the flash was physically aligned with the moving bars, it would have appeared to lag behind the bars. In order to offset this apparent lag, the flash had to be presented ahead of the moving bars. This offset was calculated for each participant under each speed condition.
3. Data analysis
All analyses were performed using JASP (JASP Team, 2018, Version 0.9) software.
We first used a classical frequentist approach to analyze our results. We then applied Bayesian statistics in order to determine whether our null effects were genuine evidence for the null hypothesis relative to the alternative hypotheses. Bayes Factors (BF10) were calculated using a default Cauchy prior width of 0.707 and were interpreted using established guidelines (Lee and Wagenmakers, 2013; Jeffreys, 1961).
4. Results
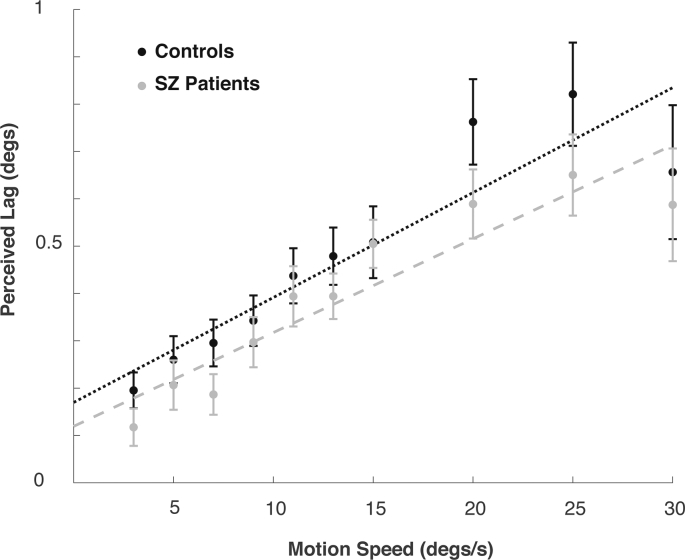
An ANOVA was used to determine whether there were any group differences in the size of the FLI in our sample. The analysis returned a very strong significant main effect of speed (Fig. 2) with all participants showing a linear increase in FLI with increasing speed (F(1,37) = 26.77, p < 0.001, ηp2 = 0.420; BF10 > 100). This is consistent with previous research (Hubbard and Bharucha, 1988; Hubbard, 1990; Krekelberg and Lappe, 1999; Nijhawan, 1994; Wojtach et al., 2008). Importantly, our analysis did not reveal a significant main effect of group (F(1,37) = 0.419, p = 0.522, ηp2 = 0.011, BF10 = 0.346), nor evidence for an interaction between speed and group (p = 0.496), which would indicate a deficit in motion speed processing in schizophrenia. Bayesian statistics indicated “strong” evidence against an interaction (BF10 = 0.045). The slope (mean SZ: 0.019, HC: 0.022; p = 0.324) and R2 goodness of fit (mean SZ: 0.49, HC: 0.45; p = 0.852) of the linear functions did not differ between patients and controls.
Fig. 2.
Average extent to which participants with and without schizophrenia perceived the moving stimulus ahead of the flash at 10 target speeds. Error bars represent standard error.
Correlations of line slope with PANNS scores failed to show any relationship between an individual's illness severity and the influence of motion speed on perceived lag (positive scores: R2 = 0.047, p = 0.878; negative scores: R2 = −0.032, p = 0.917; general scores: R2 = 0.08, p = 0.799; total score: R2 = −0.093, p = 0.763).
5. Discussion
Research on visual perception in schizophrenia consistently reports an impairment in motion speed processing (Clementz et al., 2007; Chen, 2011; Chen et al., 2004; Chen et al., 1999b; Chen et al., 1999a; Chen et al., 2003; Bidwell et al., 2006; Chen et al., 2006; Kim et al., 2006; Hong et al., 2009; Brenner et al., 2003). However, the typical task used to assess speed processing in schizophrenia is a 2IFC speed discrimination task, which may be susceptible to the effects of a more generalised deficit (e.g., including limited working memory function and attention resources). The aim of this study was to use the Flash Lag illusion to indirectly probe the integrity of speed processing mechanisms in patients with schizophrenia. Previous research on the Flash Lag illusion in healthy adults shows there is a strong linear relationship between the speed of the moving target and the magnitude of the perceived lag. We expected that if patients exhibited difficulties in processing motion speed, this relationship would be altered. Based on previous research (Maus et al., 2012), we also predicted that a motion deficit would reduce the overall size of the Flash Lag illusion. The results of this study suggest no such abnormality in motion speed processing in schizophrenia. We found no group differences in overall illusion magnitude or dependence on motion speed.
Despite previous reports of a speed discrimination deficit in schizophrenia (Chen, 2011; Clementz et al., 2007; Wang et al., 2009), the characteristic speed dependence of the Flash Lag illusion observed from our patients indicates intact speed processing in this group. The majority of previous research reporting speed processing deficits has assessed velocity thresholds using a 2IFC task. In the typical speed discrimination task, participants are required to make a comparative judgement of two motion speeds presented in separate temporal intervals. Thus, speed estimations calculated for the first motion stimulus must be maintained in working memory until the second motion stimulus is presented. Given that schizophrenia is heavily associated with working memory deficits (Lee and Park, 2005; Meda et al., 2009; Goldman-Rakic, 1994; Conklin et al., 2000; Forbes et al., 2009), it is possible that poor performance on these 2IFC tasks reflect difficulties in working memory rather than a speed processing deficit per se. In the current study, participants were not required to make judgments of stimuli presented in two separate intervals, reducing any confound associated with a working memory deficit. Instead, they were asked to make much simpler judgments about the relative position of a stationary object and moving target. Thus, our failure to find a weaker relationship between FLI magnitude and motion speed in schizophrenia suggests intact speed processing in this group. These findings are in line with other visual illusion studies showing no visual impairments in schizophrenia (King et al., 2017; Grzeczkowski et al., 2018; Tibber et al., 2013; Yang et al., 2013; Palmer et al., 2018b; Kaliuzhna et al., 2019) and highlight the importance of examining perception in this group using a range of experimental tasks. Our results are also in accordance with some earlier studies on motion processing in schizophrenia that report no differences between patients and controls (Keane et al., 2018b; Tso et al., 2013; Keane et al., 2018a). Specifically, it has been suggested that previously documented motion processing deficits might be a result of lower IQ in patients with schizophrenia. IQ was not assessed in the present sample. However, both groups were matched on years of education, suggesting comparable IQ levels. Thus, our results might differ from previous research that observed motion processing deficits in schizophrenia due to an IQ level confound.
Another confounding factor that could influence task performance on 2IFC tasks is a general attention deficit (Fioravanti et al., 2012; Fioravanti et al., 2005; Chen and Faraone, 2000). The task employed in this study arguably recruits less attentional resources than the typical 2IFC speed discrimination task, and may thus be more sensitive to detecting a specific deficit in speed processing. Importantly, our study made clear predictions about the pattern of results expected if an attention deficit were to influence task performance. Previous research in healthy adults shows that limited attention results in larger FLIs (Sarich et al., 2007; Hayes and Freyd, 2002; Shioiri et al., 2010; Baldo and Namba, 2002; Baldo et al., 2002). Our study showed a trend in the opposite direction. This may indicate that patients in our study might exhibit generally good cognitive function. Unfortunately, no cognitive battery was used in our study to assess patients' general cognitive ability. It should be noted, that because an attention deficit in schizophrenia and a motion-processing deficit are expected to result in opposing effects on the FLI, the lack of difference between the two groups could theoretically result from the two deficits “cancelling each other out”. However, this is unlikely, as a specific speed processing deficit predicts larger differences between the groups at intermediate speeds (~10°/s) (Chen, 2011).
The mild illness severity of our patients may explain our failure to detect an abnormality in motion processing, which may have otherwise been evident in a more acute sample. Indeed, previous work indicates that perceptual deficits could be present only in patients with pronounced symptomatology (Keane et al., 2013; Silverstein, 2016). It should be noted that we did observe a trend towards a reduced Flash Lag illusion in our patients, which would be indicative of a specific deficit in motion processing in schizophrenia (Tibber et al., 2013; Keane et al., 2013; Silverstein et al., 2013; Tschacher et al., 2006). However, such a dependence on illness state and symptom severity would be at odds with findings that suggests speed discrimination deficits are not directly associated with clinical manifestations in patients, but also present in biological relatives (Chen et al., 1999a). Moreover, we saw no relationship between individual differences in PANSS measures and FLI magnitude (however, this, too, could be related to the fact that patients were generally asymptomatic, thus exhibiting little variation).
Visual integration deficits have recently been suggested as a fundamental feature of schizophrenia (Butler et al., 2008; Carter et al., 2017; Silverstein et al., 2000; Silverstein and Keane, 2011a; Silverstein et al., 2009). Motion processing is heavily dependent on the integration of information over time. Although our data provide no evidence for a general integration deficit, other research suggests patients with schizophrenia have difficulties in discriminating motion direction (Chen et al., 2003; Carter et al., 2017; Li, 2002; Chen et al., 2005; Slaghuis et al., 2007; Stuve et al., 1997) or biological motion from non-biological motion (Kim et al., 2005; Okruszek et al., 2015; Spencer et al., 2013). Many of these studies employ a 2IFC task. After controlling for confounds associated with 2IFC judgments, it may be the case that integration deficits are shown to only manifest at higher levels of cognition, for example when temporal order judgments are made (Capa et al., 2014; Thoenes and Oberfeld, 2017; Zhou et al., 2018; Foucher et al., 2007; Giersch et al., 2008; Norton et al., 2008) or when stimuli are backward masked (Schechter et al., 2003; Butler et al., 2003; McClure, 2001; Slaghuis, 2004; Bakanidze et al., 2013; Herzog et al., 2013). Thus, it will be important for future experiments to assess aspects of motion processing across a wide range of tasks within the same patient cohort (Grzeczkowski et al., 2018; Yang et al., 2013).
Declaration of competing interest
Authors declare no conflict of interest.
Acknowledgements
This research was funded by the Alexander von Humboldt Foundation, the Australian Research Council Centre of Excellence in Cognition and its Disorders and the Swiss National Science Foundation. MK was funded by an Early Postdoc. Mobility Grant of the Swiss National Science Foundation. KS was funded by an Alexander von Humboldt Foundation Fellowship. We thank Markus Lappe, Derek Arnold, Jeff Foster, John Cass and Serje Robidoux for their comments on the interpretation of our findings.
References
- Albright T.D. Direction and orientation selectivity of neurons in visual area MT of the macaque. J. Neurophysiol. 1984;52:1106–1130. doi: 10.1152/jn.1984.52.6.1106. [DOI] [PubMed] [Google Scholar]
- Arnold D.H., Ong Y., Roseboom W. Simple differential latencies modulate, but do not cause the flash-lag effect. J. Vis. 2009;9:4. doi: 10.1167/9.5.4. [DOI] [PubMed] [Google Scholar]
- Bakanidze G., Roinishvili M., Chkonia E., Kitzrow W., Richter S., Neumann K., Herzog M., Brand A., Puls I. Association of the nicotinic receptor α7 subunit gene (CHRNA7) with schizophrenia and visual backward masking. Frontiers in psychiatry. 2013;4:133. doi: 10.3389/fpsyt.2013.00133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baldo M.V.C., Namba J. The attentional modulation of the flash-lag effect. Braz. J. Med. Biol. Res. 2002;35:969–972. doi: 10.1590/s0100-879x2002000800014. [DOI] [PubMed] [Google Scholar]
- Baldo M.V., Kihara A.H., Namba J., Klein S.A. Evidence for an attentional component of the perceptual misalignment between moving and flashing stimuli. Perception. 2002;31:17–30. doi: 10.1068/p3302. [DOI] [PubMed] [Google Scholar]
- Bennett D., Dluzniak A., Cropper S.J., Partos T., Sundram S., Carter O. Selective impairment of global motion integration, but not global form detection, in schizophrenia and bipolar affective disorder. Schizophrenia research: cognition. 2016;3:11–14. doi: 10.1016/j.scog.2015.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bidwell L.C., Holzman P.S., Chen Y. Aging and visual motion discrimination in normal adults and schizophrenia patients. Psychiatry Res. 2006;145:1–8. doi: 10.1016/j.psychres.2005.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brainard D.H. The psychophysics toolbox. Spat. Vis. 1997;10:433–436. [PubMed] [Google Scholar]
- Brenner E., Smeets J.B. Motion extrapolation is not responsible for the flash–lag effect. Vis. Res. 2000;40:1645–1648. doi: 10.1016/s0042-6989(00)00067-5. [DOI] [PubMed] [Google Scholar]
- Brenner C.A., Wilt M.A., Lysaker P.H., Koyfman A., O’donnell B.F. Psychometrically matched visual-processing tasks in schizophrenia spectrum disorders. J. Abnorm. Psychol. 2003;112:28. [PubMed] [Google Scholar]
- Brittain P., Surguladze S., Mckendrick A. Backward and forward visual masking in schizophrenia and its relation to global motion and global form perception. Schizophr. Res. 2010;124:134–141. doi: 10.1016/j.schres.2010.07.008. [DOI] [PubMed] [Google Scholar]
- Britten K.H., Shadlen M.N., Newsome W.T., Movshon J.A. Responses of neurons in macaque MT to stochastic motion signals. Vis. Neurosci. 1993;10:1157–1169. doi: 10.1017/s0952523800010269. [DOI] [PubMed] [Google Scholar]
- Bunney W.E., Jr., Hetrick W.P., Bunney B.G., Patterson J.V., Jin Y., Potkin S.G., Sandman C.A. Structured interview for assessing perceptual anomalies (SIAPA) Schizophr. Bull. 1999;25:577–592. doi: 10.1093/oxfordjournals.schbul.a033402. [DOI] [PubMed] [Google Scholar]
- Butler P.D., Javitt D.C. Early-stage visual processing deficits in schizophrenia. Current opinion in psychiatry. 2005;18:151. doi: 10.1097/00001504-200503000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler P.D., Desanti L.A., Maddox J., Harkavy-Friedman J.M., Amador X.F., Goetz R.R., Javitt D.C., Gorman J.M. Visual backward-masking deficits in schizophrenia: relationship to visual pathway function and symptomatology. Schizophr. Res. 2003;59:199–209. doi: 10.1016/s0920-9964(01)00341-3. [DOI] [PubMed] [Google Scholar]
- Butler P.D., Silverstein S.M., Dakin S.C. Visual perception and its impairment in schizophrenia. Biol. Psychiatry. 2008;64:40–47. doi: 10.1016/j.biopsych.2008.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capa R.L., Duval C.Z., Blaison D., Giersch A. Patients with schizophrenia selectively impaired in temporal order judgments. Schizophr. Res. 2014;156:51–55. doi: 10.1016/j.schres.2014.04.001. [DOI] [PubMed] [Google Scholar]
- Carter O., Bennett D., Nash T., Arnold S., Brown L., Cai R., Allan Z., Dluzniak A., Mcanally K., Burr D. Sensory integration deficits support a dimensional view of psychosis and are not limited to schizophrenia. Transl. Psychiatry. 2017;7:e1118. doi: 10.1038/tp.2017.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chappell M., Mullen K.T. The Magnocellular visual pathway and the flash-lag illusion. J. Vis. 2010;10:24. doi: 10.1167/10.11.24. [DOI] [PubMed] [Google Scholar]
- Chen Y. Abnormal visual motion processing in schizophrenia: a review of research progress. Schizophr. Bull. 2011;37:709–715. doi: 10.1093/schbul/sbr020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen W.J., Faraone S.V. Sustained attention deficits as markers of genetic susceptibility to schizophrenia. Am. J. Med. Genet. 2000;97:52–57. doi: 10.1002/(sici)1096-8628(200021)97:1<52::aid-ajmg7>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- Chen Y., Nakayama K., Levy D.L., Matthysse S., Holzman P.S. Psychophysical isolation of a motion-processing deficit in schizophrenics and their relatives and its association with impaired smooth pursuit. Proc. Natl. Acad. Sci. 1999;96:4724–4729. doi: 10.1073/pnas.96.8.4724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y., Palafox G.P., Nakayama K., Levy D.L., Matthysse S., Holzman P.S. Motion perception in schizophrenia. Arch. Gen. Psychiatry. 1999;56:149–154. doi: 10.1001/archpsyc.56.2.149. [DOI] [PubMed] [Google Scholar]
- Chen Y., Nakayama K., Levy D., Matthysse S., Holzman P. Processing of global, but not local, motion direction is deficient in schizophrenia. Schizophr. Res. 2003;61:215–227. doi: 10.1016/s0920-9964(02)00222-0. [DOI] [PubMed] [Google Scholar]
- Chen Y., Levy D.L., Sheremata S., Holzman P.S. Compromised late-stage motion processing in schizophrenia. Biol. Psychiatry. 2004;55:834–841. doi: 10.1016/j.biopsych.2003.12.024. [DOI] [PubMed] [Google Scholar]
- Chen Y., Bidwell L.C., Holzman P.S. Visual motion integration in schizophrenia patients, their first-degree relatives, and patients with bipolar disorder. Schizophr. Res. 2005;74:271–281. doi: 10.1016/j.schres.2004.04.002. [DOI] [PubMed] [Google Scholar]
- Chen Y., Levy D.L., Sheremata S., Holzman P.S. Bipolar and schizophrenic patients differ in patterns of visual motion discrimination. Schizophr. Res. 2006;88:208–216. doi: 10.1016/j.schres.2006.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y., Grossman E.D., Bidwell L.C., Yurgelun-Todd D., Gruber S.A., Levy D.L., Nakayama K., Holzman P.S. Differential activation patterns of occipital and prefrontal cortices during motion processing: evidence from normal and schizophrenic brains. Cognitive, Affective, & Behavioral Neuroscience. 2008;8:293–303. doi: 10.3758/cabn.8.3.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clementz B.A., Mcdowell J.E., Dobkins K.R. Compromised speed discrimination among schizophrenia patients when viewing smooth pursuit targets. Schizophr. Res. 2007;95:61–64. doi: 10.1016/j.schres.2007.05.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conklin H.M., Curtis C.E., Katsanis J., Iacono W.G. Verbal working memory impairment in schizophrenia patients and their first-degree relatives: evidence from the digit span task. Am. J. Psychiatr. 2000;157:275–277. doi: 10.1176/appi.ajp.157.2.275. [DOI] [PubMed] [Google Scholar]
- Cornsweet Tom N. The Staircase-Method in Psychophysics. American Journal of Psychology. 1962;75:485–491. [PubMed] [Google Scholar]
- Couture S.M., Penn D.L., Roberts D.L. The functional significance of social cognition in schizophrenia: a review. Schizophr. Bull. 2006;32:S44–S63. doi: 10.1093/schbul/sbl029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crawford T., Hamm J., Kean M., Schmechtig A., Kumari V., Anilkumar A., Ettinger U. The perception of real and illusory motion in schizophrenia. Neuropsychologia. 2010;48:3121–3127. doi: 10.1016/j.neuropsychologia.2010.06.027. [DOI] [PubMed] [Google Scholar]
- Cutting J., Dunne F. The nature of the abnormal perceptual experiences at the onset of schizophrenia. Psychopathology. 1986;19:347–352. doi: 10.1159/000284459. [DOI] [PubMed] [Google Scholar]
- Dakin S., Carlin P., Hemsley D. Weak suppression of visual context in chronic schizophrenia. Curr. Biol. 2005;15:R822–R824. doi: 10.1016/j.cub.2005.10.015. [DOI] [PubMed] [Google Scholar]
- Dima D., Roiser J.P., Dietrich D.E., Bonnemann C., Lanfermann H., Emrich H.M., Dillo W. Understanding why patients with schizophrenia do not perceive the hollow-mask illusion using dynamic causal modelling. Neuroimage. 2009;46:1180–1186. doi: 10.1016/j.neuroimage.2009.03.033. [DOI] [PubMed] [Google Scholar]
- Dima D., Dietrich D.E., Dillo W., Emrich H.M. Impaired top-down processes in schizophrenia: a DCM study of ERPs. NeuroImage. 2010;52:824–832. doi: 10.1016/j.neuroimage.2009.12.086. [DOI] [PubMed] [Google Scholar]
- Dumoulin S.O., Bittar R.G., Kabani N.J., Baker Jr C.L., Le Goualher G., Pike G.B., Evans A.C. A new anatomical landmark for reliable identification of human area V5/MT: a quantitative analysis of sulcal patterning. Cereb. Cortex. 2000;10:454–463. doi: 10.1093/cercor/10.5.454. [DOI] [PubMed] [Google Scholar]
- Eagleman D.M., Sejnowski T.J. Motion signals bias localization judgments: a unified explanation for the flash-lag, flash-drag, flash-jump, and Frohlich illusions. J. Vis. 2007;7:3. doi: 10.1167/7.4.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edlund M.J., Conrad C., Morris P. Accidents among schizophrenic outpatients. Compr. Psychiatry. 1989;30:522–526. doi: 10.1016/0010-440x(89)90082-5. [DOI] [PubMed] [Google Scholar]
- Fett A.-K.J., Viechtbauer W., Penn D.L., Van Os J., Krabbendam L. The relationship between neurocognition and social cognition with functional outcomes in schizophrenia: a meta-analysis. Neurosci. Biobehav. Rev. 2011;35:573–588. doi: 10.1016/j.neubiorev.2010.07.001. [DOI] [PubMed] [Google Scholar]
- Fioravanti M., Carlone O., Vitale B., Cinti M.E., Clare L. A meta-analysis of cognitive deficits in adults with a diagnosis of schizophrenia. Neuropsychol. Rev. 2005;15:73–95. doi: 10.1007/s11065-005-6254-9. [DOI] [PubMed] [Google Scholar]
- Fioravanti M., Bianchi V., Cinti M.E. Cognitive deficits in schizophrenia: an updated metanalysis of the scientific evidence. BMC psychiatry. 2012;12:64. doi: 10.1186/1471-244X-12-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes N., Carrick L., Mcintosh A., Lawrie S. Working memory in schizophrenia: a meta-analysis. Psychol. Med. 2009;39:889–905. doi: 10.1017/S0033291708004558. [DOI] [PubMed] [Google Scholar]
- Foucher J.R., Lacambre M., Pham B.-T., Giersch A., Elliott M. Low time resolution in schizophrenia: lengthened windows of simultaneity for visual, auditory and bimodal stimuli. Schizophr. Res. 2007;97:118–127. doi: 10.1016/j.schres.2007.08.013. [DOI] [PubMed] [Google Scholar]
- Giersch A., Lalanne L., Corves C., Seubert J., Shi Z., Foucher J., Elliott M.A. Extended visual simultaneity thresholds in patients with schizophrenia. Schizophr. Bull. 2008;35:816–825. doi: 10.1093/schbul/sbn016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman-Rakic P.S. The Frontal Loves and Neuropsychiatric Illness. Washington, DC. 1994. Working memory dysfunction in schizophrenia; pp. 71–82. [Google Scholar]
- Green M.F., Butler P.D., Chen Y., Geyer M.A., Silverstein S., Wynn J.K., Yoon J.H., Zemon V. Perception measurement in clinical trials of schizophrenia: promising paradigms from CNTRICS. Schizophr. Bull. 2008;35:163–181. doi: 10.1093/schbul/sbn156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green M.F., Horan W.P., Lee J. Social cognition in schizophrenia. Nat. Rev. Neurosci. 2015;16:620. doi: 10.1038/nrn4005. [DOI] [PubMed] [Google Scholar]
- Grzeczkowski L., Roinishvili M., Chkonia E., Brand A., Mast F.W., Herzog M.H., Shaqiri A. Is the perception of illusions abnormal in schizophrenia? Psychiatry Res. 2018;270:929–939. doi: 10.1016/j.psychres.2018.10.063. [DOI] [PubMed] [Google Scholar]
- Hayes A.E., Freyd J.J. Representational momentum when attention is divided. Vis. Cogn. 2002;9:8–27. [Google Scholar]
- Herzog M.H., Roinishvili M., Chkonia E., Brand A. Schizophrenia and visual backward masking: a general deficit of target enhancement. Front. Psychol. 2013;4:254. doi: 10.3389/fpsyg.2013.00254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong L.E., Turano K.A., O’neill H.B., Hao L., Wonodi I., Mcmahon R.P., Thaker G.K. Is motion perception deficit in schizophrenia a consequence of eye-tracking abnormality? Biol. Psychiatry. 2009;65:1079–1085. doi: 10.1016/j.biopsych.2008.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hubbard T.L. Cognitive representation of linear motion: possible direction and gravity effects in judged displacement. Mem. Cogn. 1990;18:299–309. doi: 10.3758/bf03213883. [DOI] [PubMed] [Google Scholar]
- Hubbard T.L. The flash-lag effect and related mislocalizations: findings, properties, and theories. Psychol. Bull. 2014;140:308. doi: 10.1037/a0032899. [DOI] [PubMed] [Google Scholar]
- Hubbard T.L., Bharucha J.J. Judged displacement in apparent vertical and horizontal motion. Percept. Psychophys. 1988;44:211–221. doi: 10.3758/bf03206290. [DOI] [PubMed] [Google Scholar]
- Javitt D.C. When doors of perception close: bottom-up models of disrupted cognition in schizophrenia. Annu. Rev. Clin. Psychol. 2009;5:249–275. doi: 10.1146/annurev.clinpsy.032408.153502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeffreys H. The Clarendon Press; Oxford: 1961. The Theory of Probability. [Google Scholar]
- Kaliuzhna M., Stein T., Rusch T., Sekutowicz M., Sterzer P., Seymour K.J. No evidence for abnormal priors in early vision in schizophrenia. Schizophrenia research. 2019;210:245–254. doi: 10.1016/j.schres.2018.12.027. [DOI] [PubMed] [Google Scholar]
- Kantrowitz J.T., Butler P.D., Schecter I., Silipo G., Javitt D.C. Seeing the world dimly: the impact of early visual deficits on visual experience in schizophrenia. Schizophr. Bull. 2009;35:1085–1094. doi: 10.1093/schbul/sbp100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kay S.R., Fiszbein A., Opler L.A. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr. Bull. 1987;13:261–276. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- Keane B.P., Silverstein S.M., Barch D.M., Carter C.S., Gold J.M., Kovács I., Macdonald A.W., Ragland J.D., Strauss M.E. The spatial range of contour integration deficits in schizophrenia. Exp. Brain Res. 2012;220:251–259. doi: 10.1007/s00221-012-3134-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keane B.P., Silverstein S.M., Wang Y., Papathomas T. Reduced depth inversion illusions in schizophrenia are state-specific and occur for multiple object types and viewing conditions. J. Abnorm. Psychol. 2013;122:506. doi: 10.1037/a0032110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keane B.P., Silverstein S.M., Wang Y., Roché M.W., Papathomas T.V. Seeing more clearly through psychosis: depth inversion illusions are normal in bipolar disorder but reduced in schizophrenia. Schizophr. Res. 2016;176:485–492. doi: 10.1016/j.schres.2016.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keane B., Peng Y., Demmin D., Silverstein S., Lu H. Evidence that low IQ, but not schizophrenia, impairs motion integration. J. Vis. 2018;18:51. [Google Scholar]
- Keane B.P., Peng Y., Demmin D., Silverstein S.M., Lu H. Intact perception of coherent motion, dynamic rigid form, and biological motion in chronic schizophrenia. Psychiatry Res. 2018;268:53–59. doi: 10.1016/j.psychres.2018.06.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan S.A., Timney B. Alcohol slows interhemispheric transmission, increases the flash-lag effect, and prolongs masking: evidence for a slowing of neural processing and transmission. Vis. Res. 2007;47:1821–1832. doi: 10.1016/j.visres.2007.03.008. [DOI] [PubMed] [Google Scholar]
- Kim J., Doop M.L., Blake R., Park S. Impaired visual recognition of biological motion in schizophrenia. Schizophr. Res. 2005;77:299–307. doi: 10.1016/j.schres.2005.04.006. [DOI] [PubMed] [Google Scholar]
- Kim D., Wylie G., Pasternak R., Butler P.D., Javitt D.C. Magnocellular contributions to impaired motion processing in schizophrenia. Schizophr. Res. 2006;82:1–8. doi: 10.1016/j.schres.2005.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King D.J., Hodgekins J., Chouinard P.A., Chouinard V.-A., Sperandio I. A review of abnormalities in the perception of visual illusions in schizophrenia. Psychon. Bull. Rev. 2017;24:734–751. doi: 10.3758/s13423-016-1168-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koethe D., Kranaster L., Hoyer C., Gross S., Neatby M.A., Schultze-Lutter F., Ruhrmann S., Klosterkötter J., Hellmich M., Leweke F.M. Binocular depth inversion as a paradigm of reduced visual information processing in prodromal state, antipsychotic-naive and treated schizophrenia. Eur. Arch. Psychiatry Clin. Neurosci. 2009;259:195. doi: 10.1007/s00406-008-0851-6. [DOI] [PubMed] [Google Scholar]
- Krekelberg B., Lappe M. Temporal recruitment along the trajectory of moving objects and the perception of position. Vis. Res. 1999;39:2669–2679. doi: 10.1016/s0042-6989(98)00287-9. [DOI] [PubMed] [Google Scholar]
- Krekelberg B., Lappe M. Neuronal latencies and the position of moving objects. Trends Neurosci. 2001;24:335–339. doi: 10.1016/s0166-2236(00)01795-1. [DOI] [PubMed] [Google Scholar]
- Landrø N.I., Pape–Ellefsen E., Hagland K.O., Odland T. Memory deficits in young schizophrenics with normal general intellectual function. Scand. J. Psychol. 2001;42:459–465. doi: 10.1111/1467-9450.00259. [DOI] [PubMed] [Google Scholar]
- Lee J., Park S. Working memory impairments in schizophrenia: a meta-analysis. J. Abnorm. Psychol. 2005;114:599. doi: 10.1037/0021-843X.114.4.599. [DOI] [PubMed] [Google Scholar]
- Lee M.D., Wagenmakers E.-J. Cambridge University Press; Cambridge: 2013. Bayesian Cognitive Modeling: A Practical Course. [Google Scholar]
- Lencer R., Nagel M., Sprenger A., Heide W., Binkofski F. Reduced neuronal activity in the V5 complex underlies smooth-pursuit deficit in schizophrenia: evidence from an fMRI study. Neuroimage. 2005;24:1256–1259. doi: 10.1016/j.neuroimage.2004.11.013. [DOI] [PubMed] [Google Scholar]
- Letourneau J.E. The Oppel-Kundt and the Müller-Lyer illusions among schizophrenics. Percept. Mot. Skills. 1974;39:775–778. doi: 10.2466/pms.1974.39.2.775. [DOI] [PubMed] [Google Scholar]
- Letourneau J.E., Lavoie G. The Poggendorff illusion among paranoid and simple schizophrenic patients. American Journal of Optometry & Archives of American Academy of Optometry. 1973;50:944–948. doi: 10.1097/00006324-197312000-00003. [DOI] [PubMed] [Google Scholar]
- Li C.-S.R. Impaired detection of visual motion in schizophrenia patients. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2002;26:929–934. doi: 10.1016/s0278-5846(02)00207-5. [DOI] [PubMed] [Google Scholar]
- Linares D., Lopez-Moliner J. Absence of flash-lag when judging global shape from local positions. Vis. Res. 2007;47:357–362. doi: 10.1016/j.visres.2006.10.013. [DOI] [PubMed] [Google Scholar]
- Linares D., Holcombe A.O., White A.L. Where is the moving object now? Judgments of instantaneous position show poor temporal precision (SD = 70 ms) J. Vis. 2009;9:9. doi: 10.1167/9.13.9. [DOI] [PubMed] [Google Scholar]
- Lipskaya-Velikovsky L., Kotler M., Weiss P., Kaspi M., Gamzo S., Ratzon N. Car driving in schizophrenia: can visual memory and organization make a difference? Disabil. Rehabil. 2013;35:1734–1739. doi: 10.3109/09638288.2012.753116. [DOI] [PubMed] [Google Scholar]
- Maus G.W., Ward J., Nijhawan R., Whitney D. The perceived position of moving objects: transcranial magnetic stimulation of area MT+ reduces the flash-lag effect. Cereb. Cortex. 2012;23:241–247. doi: 10.1093/cercor/bhs021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClure R.K. The visual backward masking deficit in schizophrenia. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2001;25:301–311. doi: 10.1016/s0278-5846(00)00166-4. [DOI] [PubMed] [Google Scholar]
- Meda S.A., Stevens M.C., Folley B.S., Calhoun V.D., Pearlson G.D. Evidence for anomalous network connectivity during working memory encoding in schizophrenia: an ICA based analysis. PLoS One. 2009;4 doi: 10.1371/journal.pone.0007911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nijhawan R. Motion extrapolation in catching. Nature. 1994;370(6487):256–257. doi: 10.1038/370256b0. [DOI] [PubMed] [Google Scholar]
- Nijhawan R. Neural delays, visual motion and the flash-lag effect. Trends Cogn. Sci. 2002;6:387–393. doi: 10.1016/s1364-6613(02)01963-0. [DOI] [PubMed] [Google Scholar]
- Nijhawan R., Watanabe K., Khurana B., Shimojo S. Compensation of neural delays in visual-motor behaviour: no evidence for shorter afferent delays for visual motion. Vis. Cogn. 2004;11:275–298. [Google Scholar]
- Norton D., Ongur D., Stromeyer Iii C., Chen Y. Altered ‘three-flash’illusion in response to two light pulses in schizophrenia. Schizophr. Res. 2008;103:275–282. doi: 10.1016/j.schres.2008.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Notredame C.-E., Pins D., Deneve S., Jardri R. What visual illusions teach us about schizophrenia. Front. Integr. Neurosci. 2014;8:63. doi: 10.3389/fnint.2014.00063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’donnell B.F., Potts G.F., Nestor P.G., Stylianopoulos K.C., Shenton M.E., Mccarley R.W. Spatial frequency discrimination in schizophrenia. J. Abnorm. Psychol. 2002;111:620. doi: 10.1037//0021-843x.111.4.620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Driscoll G.A., Callahan B.L. Smooth pursuit in schizophrenia: a meta-analytic review of research since 1993. Brain Cogn. 2008;68:359–370. doi: 10.1016/j.bandc.2008.08.023. [DOI] [PubMed] [Google Scholar]
- Okruszek Ł., Haman M., Kalinowski K., Talarowska M., Becchio C., Manera V. Impaired recognition of communicative interactions from biological motion in schizophrenia. PLoS One. 2015;10 doi: 10.1371/journal.pone.0116793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmer C.J., Caruana N., Clifford C.W., Seymour K.J. Adaptive sensory coding of gaze direction in schizophrenia. R. Soc. Open Sci. 2018;5 doi: 10.1098/rsos.180886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmer C.J., Caruana N., Clifford C.W.G., Seymour K.J. Perceptual integration of head and eye cues to gaze direction in schizophrenia. R. Soc. Open Sci. 2018;5 doi: 10.1098/rsos.180885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park S., Gooding D.C. Working memory impairment as an endophenotypic marker of a schizophrenia diathesis. Schizophrenia Research: Cognition. 2014;1:127–136. doi: 10.1016/j.scog.2014.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pasternak T., Schumer R., Gizzi M., Movshon J. Abolition of visual cortical direction selectivity affects visual behavior in cats. Exp. Brain Res. 1985;61:214–217. doi: 10.1007/BF00235638. [DOI] [PubMed] [Google Scholar]
- Pelli D.G. The VideoToolbox software for visual psychophysics: transforming numbers into movies. Spat. Vis. 1997;10:437–442. [PubMed] [Google Scholar]
- Phillipson O., Harris J. Perceptual changes in schizophrenia: a questionnaire survey. Psychol. Med. 1985;15:859–866. doi: 10.1017/s0033291700005092. [DOI] [PubMed] [Google Scholar]
- Sanders L.L.O., De Millas W., Heinz A., Kathmann N., Sterzer P. Apparent motion perception in patients with paranoid schizophrenia. Eur. Arch. Psychiatry Clin. Neurosci. 2013;263:233–239. doi: 10.1007/s00406-012-0344-5. [DOI] [PubMed] [Google Scholar]
- Sarich D., Chappell M., Burgess C. Dividing attention in the flash-lag illusion. Vis. Res. 2007;47:544–547. doi: 10.1016/j.visres.2006.09.029. [DOI] [PubMed] [Google Scholar]
- Schechter I., Butler P.D., Silipo G., Zemon V., Javitt D.C. Magnocellular and parvocellular contributions to backward masking dysfunction in schizophrenia. Schizophr. Res. 2003;64:91–101. doi: 10.1016/s0920-9964(03)00008-2. [DOI] [PubMed] [Google Scholar]
- Seymour K., Stein T., Sanders L.L.O., Guggenmos M., Theophil I., Sterzer P. Altered contextual modulation of primary visual cortex responses in schizophrenia. Neuropsychopharmacology. 2013;38:2607. doi: 10.1038/npp.2013.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shioiri S., Yamamoto K., Oshida H., Matsubara K., Yaguchi H. Measuring attention using flash-lag effect. J. Vis. 2010;10:10. doi: 10.1167/10.10.10. [DOI] [PubMed] [Google Scholar]
- Silverstein S.M. The Neuropsychopathology of Schizophrenia. Springer; 2016. Visual perception disturbances in schizophrenia: a unified model. [DOI] [PubMed] [Google Scholar]
- Silverstein S.M., Keane B.P. Perceptual organization impairment in schizophrenia and associated brain mechanisms: review of research from 2005 to 2010. Schizophr. Bull. 2011;37:690–699. doi: 10.1093/schbul/sbr052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverstein S.M., Keane B.P. Vision science and schizophrenia research: toward a re-view of the disorder editors’ introduction to special section. Schizophr. Bull. 2011;37:681–689. doi: 10.1093/schbul/sbr053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverstein S.M., Kovács I., Corry R., Valone C. Perceptual organization, the disorganization syndrome, and context processing in chronic schizophrenia. Schizophr. Res. 2000;43:11–20. doi: 10.1016/s0920-9964(99)00180-2. [DOI] [PubMed] [Google Scholar]
- Silverstein S.M., Berten S., Essex B., Kovacs I., Susmaras T., Little D.M. An fMRI examination of visual integration in schizophrenia. J. Integr. Neurosci. 2009;8:175–202. doi: 10.1142/s0219635209002113. [DOI] [PubMed] [Google Scholar]
- Silverstein S.M., Keane B.P., Wang Y., Mikkilineni D., Paterno D., Papathomas T.V., Feigenson K. Effects of short-term inpatient treatment on sensitivity to a size contrast illusion in first-episode psychosis and multiple-episode schizophrenia. Front. Psychol. 2013;4:466. doi: 10.3389/fpsyg.2013.00466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slaghuis W.L. Spatio-temporal luminance contrast sensitivity and visual backward masking in schizophrenia. Exp. Brain Res. 2004;156:196–211. doi: 10.1007/s00221-003-1771-3. [DOI] [PubMed] [Google Scholar]
- Slaghuis W.L., Holthouse T., Hawkes A., Bruno R. Eye movement and visual motion perception in schizophrenia II: global coherent motion as a function of target velocity and stimulus density. Exp. Brain Res. 2007;182:415–426. doi: 10.1007/s00221-007-1003-3. [DOI] [PubMed] [Google Scholar]
- Spencer J.M., Sekuler A.B., Bennett P.J., Christensen B.K. Contribution of coherent motion to the perception of biological motion among persons with schizophrenia. Front. Psychol. 2013;4:507. doi: 10.3389/fpsyg.2013.00507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuve T., Friedman L., Jesberger J., Gilmore G., Strauss M., Meltzer H. The relationship between smooth pursuit performance, motion perception and sustained visual attention in patients with schizophrenia and normal controls. Psychol. Med. 1997;27:143–152. doi: 10.1017/s0033291796004230. [DOI] [PubMed] [Google Scholar]
- Tadin D., Kim J., Doop M.L., Gibson C., Lappin J.S., Blake R., Park S. Weakened center-surround interactions in visual motion processing in schizophrenia. J. Neurosci. 2006;26:11403–11412. doi: 10.1523/JNEUROSCI.2592-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thoenes S., Oberfeld D. Meta-analysis of time perception and temporal processing in schizophrenia: differential effects on precision and accuracy. Clin. Psychol. Rev. 2017;54:44–64. doi: 10.1016/j.cpr.2017.03.007. [DOI] [PubMed] [Google Scholar]
- Tibber A., Elaine J., Bobin T., Antonova E., Seabright A., Wright B., Carlin P., Shergill S.S., Dakin S.C. Visual surround suppression in schizophrenia. Front. Psychol. 2013;4:88. doi: 10.3389/fpsyg.2013.00088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tschacher W., Schuler D., Junghan U. Reduced perception of the motion-induced blindness illusion in schizophrenia. Schizophr. Res. 2006;81:261–267. doi: 10.1016/j.schres.2005.08.012. [DOI] [PubMed] [Google Scholar]
- Tschacher W., Dubouloz P., Meier R., Junghan U. Altered perception of apparent motion in schizophrenia spectrum disorder. Psychiatry Res. 2008;159:290–299. doi: 10.1016/j.psychres.2007.04.005. [DOI] [PubMed] [Google Scholar]
- Tso I.F., Carp J., Taylor S.F., Deldin P.J. Role of visual integration in gaze perception and emotional intelligence in schizophrenia. Schizophr. Bull. 2013;40:617–625. doi: 10.1093/schbul/sbt058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uhlhaas P.J., Mishara A.L. Perceptual anomalies in schizophrenia: integrating phenomenology and cognitive neuroscience. Schizophr. Bull. 2006;33:142–156. doi: 10.1093/schbul/sbl047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uhlhaas P.J., Phillips W.A., Silverstein S.M. The course and clinical correlates of dysfunctions in visual perceptual organization in schizophrenia during the remission of psychotic symptoms. Schizophr. Res. 2005;75:183–192. doi: 10.1016/j.schres.2004.11.005. [DOI] [PubMed] [Google Scholar]
- Uhlhaas P.J., Phillips W.A., Mitchell G., Silverstein S.M. Perceptual grouping in disorganized schizophrenia. Psychiatry Res. 2006;145:105–117. doi: 10.1016/j.psychres.2005.10.016. [DOI] [PubMed] [Google Scholar]
- Van Essen D., Maunsell J., Bixby J. The middle temporal visual area in the macaque: myeloarchitecture, connections, functional properties and topographic organization. J. Comp. Neurol. 1981;199:293–326. doi: 10.1002/cne.901990302. [DOI] [PubMed] [Google Scholar]
- Van Kemenade B.M., Seymour K., Christophel T.B., Rothkirch M., Sterzer P. Decoding pattern motion information in V1. cortex. 2014;57:177–187. doi: 10.1016/j.cortex.2014.04.014. [DOI] [PubMed] [Google Scholar]
- Wang J., Brown R., Dobkins K.R., Mcdowell J.E., Clementz B.A. Diminished parietal cortex activity associated with poor motion direction discrimination performance in schizophrenia. Cereb. Cortex. 2009;20:1749–1755. doi: 10.1093/cercor/bhp243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watanabe K., Nijhawan R., Khurana B., Shimojo S. Perceptual organization of moving stimuli modulates the flash-lag effect. J. Exp. Psychol. Hum. Percept. Perform. 2001;27:879. doi: 10.1037//0096-1523.27.4.879. [DOI] [PubMed] [Google Scholar]
- Waters F., Collerton D., Ffytche D.H., Jardri R., Pins D., Dudley R., Blom J.D., Mosimann U.P., Eperjesi F., Ford S. Visual hallucinations in the psychosis spectrum and comparative information from neurodegenerative disorders and eye disease. Schizophr. Bull. 2014;40:S233–S245. doi: 10.1093/schbul/sbu036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitney D., Murakami I., Cavanagh P. Illusory spatial offset of a flash relative to a moving stimulus is caused by differential latencies for moving and flashed stimuli. Vis. Res. 2000;40:137–149. doi: 10.1016/s0042-6989(99)00166-2. [DOI] [PubMed] [Google Scholar]
- Wojtach W.T., Sung K., Truong S., Purves D. An empirical explanation of the flash-lag effect. Proc. Natl. Acad. Sci. 2008;105:16338–16343. doi: 10.1073/pnas.0808916105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang E., Tadin D., Glasser D.M., Hong S.W., Blake R., Park S. Visual context processing in schizophrenia. Clin. Psychol. Sci. 2013;1:5–15. doi: 10.1177/2167702612464618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoon J.H., Rokem A.S., Silver M.A., Minzenberg M.J., Ursu S., Ragland J.D., Carter C.S. Diminished orientation-specific surround suppression of visual processing in schizophrenia. Schizophr. Bull. 2009;35:1078–1084. doi: 10.1093/schbul/sbp064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoon J.H., Maddock R.J., Rokem A., Silver M.A., Minzenberg M.J., Ragland J.D., Carter C.S. GABA concentration is reduced in visual cortex in schizophrenia and correlates with orientation-specific surround suppression. J. Neurosci. 2010;30:3777–3781. doi: 10.1523/JNEUROSCI.6158-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeki S. Cells responding to changing image size and disparity in the cortex of the rhesus monkey. J. Physiol. 1974;242:827–841. doi: 10.1113/jphysiol.1974.sp010736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou H.-Y., Cai X.-L., Weigl M., Bang P., Cheung E.F., Chan R.C. Multisensory temporal binding window in autism spectrum disorders and schizophrenia spectrum disorders: a systematic review and meta-analysis. Neurosci. Biobehav. Rev. 2018;86:66–76. doi: 10.1016/j.neubiorev.2017.12.013. [DOI] [PubMed] [Google Scholar]