Abstract
Objective
This study aims to determine the correlation between the duration of cardiopulmonary resuscitation (CPR) and the return of spontaneous circulation (ROSC) in an in-hospital cardiac arrest cohort.
Methods
All patients (age ≥ 17 years) who underwent CPR at our institution from 2015 to 2017 were included. The primary endpoint was ROSC or death. A total of 88 patients were included in the study. The Pearson correlation of CPR duration with the establishment of ROSC was calculated using the IBM SPSS, version 25.
Results
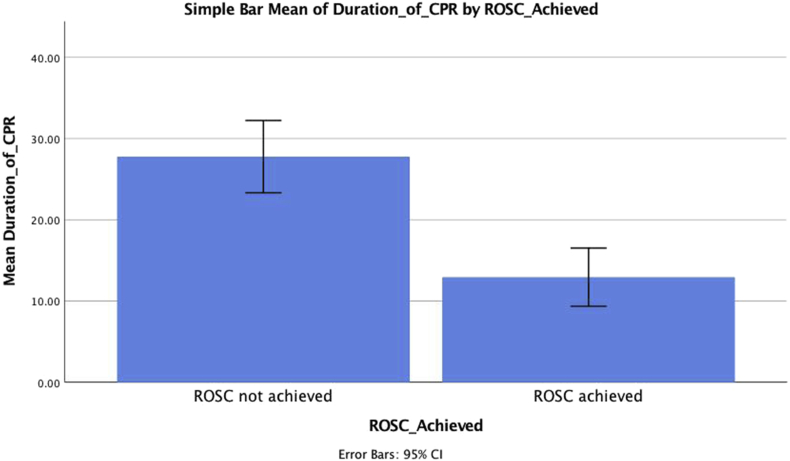
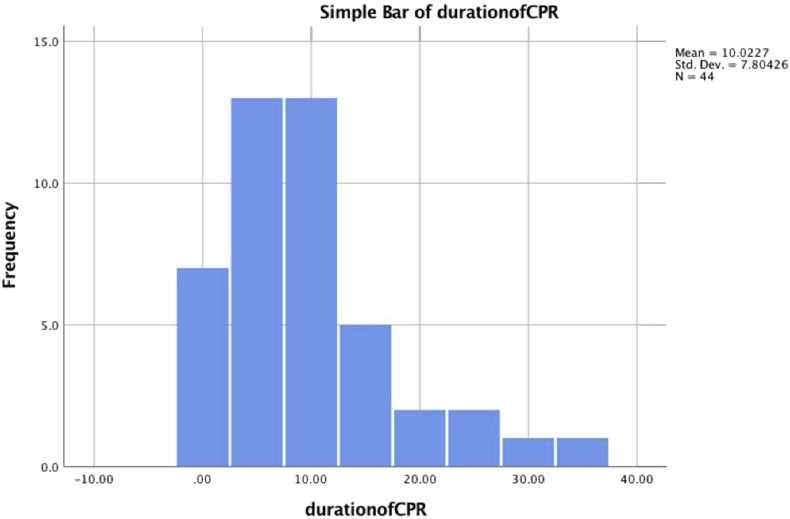
In all, 88 patients who received CPR, 55% (n = 48) experienced ROSC and survived. The remaining 45% (n = 40) of the total and 56% (n = 27) of those with ROSC died during the same hospitalization (Fig. 1). Among the 48 patients with ROSC, the documented duration of their CPR was about 10 min on average in comparison with 27.5 min CPR for patients who did not achieve ROSC (Fig. 2). Among all the patients, there was a negative correlation between the duration of the CPR and the establishment of ROSC. This is shown in Fig. 3.
Conclusion
Our study shows that CPR duration is inversely associated with the establishment rates of ROSC. Most of the benefits of CPR can be achieved in the first 15 min, and a further increase in the duration of CPR provides a minimal gain. Still, survival was achievable till 38 min in some cases, and the ideal duration of resuscitation should remain a bedside decision taking into consideration the whole clinical picture.
Keywords: Cardiopulmonary resuscitation, Cardiology, Blood circulation
1. Introduction
Cardiopulmonary resuscitation (CPR) is one of the greatest advances in modern medicine. It is an important temporary intervention to keep the brain oxygenated in patients who suffer from cardiac arrest.1 Every year, there are an estimated 200,000 in-hospital cardiac arrests in the United States.2,3 There are also an estimated 370,00–750,000 cases of in-hospital CPR administered in the United States yearly.4 The American Heart Association (AHA) estimates that the survival rate for cardiac arrest is estimated to be around 50% in cases, where the CPR is administered within 3–5 min. However, this survival decreases by 7–10% with each minute that defibrillation is delayed.1 Ever since Kouwenhoven introduced chest compressions in 1960, there have been a number of changes and advancements in the CPR technique. The survival rate, however, has not changed very significantly since then.1,2
Various studies have reported a range of 7–26% survival after in-hospital cardiac resuscitation (IHCR).5,6 Cooper et al. performed a large 10-year review of IHCR and showed that even though the initial survival was 38.6% immediately after CPR, this rate decreased significantly to 24.7%, 15.9%, and 11.3% when examined again at 24 h, at the time of discharge, and at 12 months.7 Similar studies were reported by other authors as well.8,9 The post-CPR survival after IHCR is affected by numerous factors.1 Some of them being increased age, sex, duration of CPR time till initiation of CPR, general health and associated comorbidities, quality of CPR, presence of trained staff, and effective communication.10 Cooper et al. reported an inverse relationship between the outcome of CPR and the duration of CPR and age.7 Rakic et al. reported better outcomes in younger patients, those who had a witnessed arrest, and patients with Vfib and Vtach. Others also reported better outcomes in if prompt CPR was initiated.5
So, what should be the optimal duration of CPR? CPR has been reported to be associated with greater rates of anoxic brain injury and poor survival.11 There are no current recommendations regarding when to stop CPR, and it should be individualized according to the patient and comorbidities. This study was undertaken to assess the effect of the duration of CPR on survival in patients with an in-hospital cardiac arrest. Prehospital CPR efforts are usually beneficial if carried out effectively up to 40 min.12 However, its impact on in-hospital cardiac arrest and survival remains unknown.13 This study aims to determine the correlation between the duration of CPR and the return of spontaneous circulation (ROSC) in an in-hospital cohort.
2. Materials and methods
All patients (age ≥ 17 years) who received CPR at our institution (Abington Jefferson Health) after an in-hospital cardiac arrest between 2015 and 2017 were included in this retrospective study. A total of 88 patients were identified and included in this study. The primary endpoint was the ROSC or death. This was compared with the duration of CPR done. The time from event onset to initiation of CPR was not more than a minute in any of the witnessed arrests, and for the most part, it was within 30 s. Other important variables that were studied include the outcomes of CPR, the type of initial rhythm on telemetry, and the location of cardiac arrest. Various clinical characteristics, duration of CPR, and outcomes were noted. These data were analyzed using IBM SPSS, version 25. This study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration.
3. Results
The mean age of the included patients was 71.4 years (range of 17–94 years). The duration of CPR was compared with the age of the patients using Pearson correlation, and there was a very weak correlation (0.07) that was not statistically significant (p = 0.5) (Table 1).
Table 1.
Pearson correlation depicting a weak negative correlation between duration of CPR and immediate ROSC that is not statistically significant.
| ROSC_Achieved | Duration_of_CPR | ||
|---|---|---|---|
| ROSC_Achieved | Pearson Correlation | 1 | −.496a |
| Sig. (2-tailed) | 0.000 | ||
| N | 88 | 88 | |
| Duration_of_CPR | Pearson Correlation | −.496a | 1 |
| Sig. (2-tailed) | 0.000 | ||
| N | 88 | 88 | |
CPR, cardiopulmonary resuscitation; ROSC, return of spontaneous circulation.
Correlation is significant at the 0.01 level (2-tailed).
Our patient population included 72% (n = 63) males and 28% (n = 25) females. 58.7% (n = 37) of the males achieved ROSC, while 41.3% (n = 26) did not. On the other hand, 44% (n = 11) of the females achieved ROSC, while 56% (n = 14) did not. The duration of CPR received in male patients was 20.31 ± 1.99 min (mean ± standard error) with a standard deviation of 15.81, while in female patients, it was 18.08 ± 2.55 min (mean ± standard error) with a standard deviation of 12.75. The difference between these two groups however was not statistically different, p = 0.53.
In all, 88 patients who received CPR, 55% (n = 48) experienced ROSC and survived the initial postresuscitation period (Fig. 1). The remaining 45% (n = 40) of the total patients and an additional 56% (n = 27) of those who achieved ROSC died during the same hospitalization in the post-ROSC period (Fig. 2). The difference in the duration of CPR between the group that achieved ROSC initially and the group that did not achieve ROSC was further analyzed. Data are mean ± standard deviation, unless otherwise stated. An independent samples t-test was run to determine if there were differences in the duration in patients who achieved ROSC and those that did not achieve ROSC and to see of this difference was statistically different. There was homogeneity of variances, as assessed by Levene's test for equality of variances with p > 0.05 (p = 0.39).
Fig. 1.
Mean duration of CPR in both groups. CPR, cardiopulmonary resuscitation.
Fig. 2.
Duration of CPR required to achieve ROSC in all the patients. Only four patients achieved ROSC after more than 20 min of CPR. CPR, cardiopulmonary resuscitation; ROSC, return of spontaneous circulation.
The mean duration of CPR in patients who achieved ROSC was 12.93 ± 12.33; on the other hand, the mean duration of CPR in patients who did not achieve ROSC was 27.77 ± 13.91. The mean duration of CPR in patients who did not achieve ROSC was 14.83 higher than patients who did achieve ROSC initially. There was a statistically significant difference in mean durations of CPR between the two groups, with patients who did not achieve ROSC receiving 14.83 ± 2.79 more minutes of CPR, [95% confidence interval (CI), 9.27–20.40], t(86) = 5.30, p = 0.00 (Table 2).
Table 2.
Independent sample t-test, comparing the duration of CPR in both groups.
| Groups | Mean duration of CPR | Std deviation | p value |
|---|---|---|---|
| ROSC achieved | 12.93 | 12.33 | t(86) = 5.30, p = 0.00 |
| ROSC not achieved | 27.77 | 13.91 |
CPR, cardiopulmonary resuscitation; ROSC, return of spontaneous circulation.
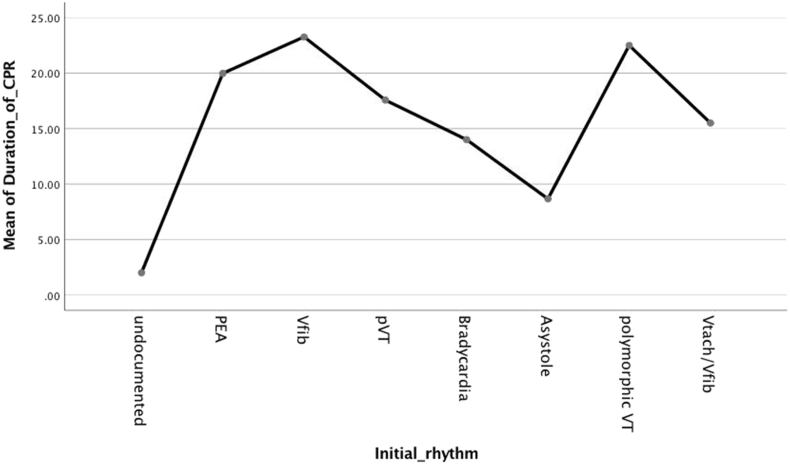
Among all the patients, there was a negative correlation between the duration of the CPR and the establishment of ROSC. This is shown in Fig. 3.
Fig. 3.
One-way ANOVA depicting the duration of CPR in different rhythms. CPR, cardiopulmonary resuscitation; ANOVA, analysis of variance.
The duration of CPR was also compared in patients who had a cardiac arrest in the intensive care unit (ICU) vs. out of the ICU. 55.86 (n = 49) patients had an arrest in the ICU, while 44.31 (n = 39) patients had an arrest out of the ICU. The mean duration of CPR in patients who had an arrest in the ICU was 21.12 ± 1.96 (mean ± standard error) with a standard deviation of 13.74; on the other hand, the mean duration of CPR in patients who had an arrest out of the ICU was 17.87 ± 2.62 (mean ± standard error) with a standard deviation of 16.38. The mean duration of CPR in patients who had an arrest in the ICU was 3.25 ± 3.21 (mean ± standard error) higher than patients who had an arrest out of the ICU. This difference was not statistically different (95% CI, −9.63 to 3.13), t(86) = −1.01, p = 0.31.51% of the patients (n = 25) in the ICU achieved ROSC, against 49% (n = 24) who did not achieve ROSC. On the other hand, 59% (n = 23) of the patients in the non-ICU setting achieved ROSC as against 41% (n = 16) who did not achieve ROSC.
In our study, most of the cardiac arrests were witnessed 94.31% (n = 83) with 5.69% (n = 5) of the cardiac arrests which were unwitnessed. 55.4% (n = 46) of witnessed cardiac arrest patients achieved ROSC, while 44.6% (n = 37) of witnessed cardiac arrest patients did not achieve ROSC. On the other hand, 40% (n = 2) of the unwitnessed cardiac arrest patients did achieve ROSC, while 60% (n = 3) of the unwitnessed cardiac arrest patients did not achieve ROSC. The duration of CPR received was also compared between the two groups. The duration of CPR received in patients with witnessed arrest was 19.36 ± 1.61 (mean ± standard error) with a standard deviation of 14.67, while those that had an unwitnessed arrest received 25.00 ± 9.24 (mean ± standard error) with a standard deviation of 20.66 of CPR. The difference between these two groups however was not statistically different, p = 0.41.
Finally, effect of the type of initial rhythm on achieving ROSC and the duration of CPR received with each rhythm was checked. 51% (n = 25) of the patients with Pulseless electrical activity (PEA) achieved ROSC, and 49% (n = 24) did not achieve ROSC initially. 26% (n = 4) of the patients with Vfib achieved ROSC, while 73% (n = 11) of the patients did not achieve ROSC. 42% (n = 3) patients with pulseless Vtach achieved ROSC, while 57.1% (n = 4) did not receive ROSC initially. 66.6% (n = 2) patients with asystole achieved ROSC, while 33.3% (n = 1) did not. 50% (n = 4) patients with polymorphic Vtach achieved ROSC, while 50% (n = 4) did not achieve ROSC. Furthermore, the duration of CPR received for each of the different rhythms was analyzed using a one-way analysis of variance. It revealed no statistically significant difference in the times of CPR received for any of the rhythms when compared with each other, (p = 0.60).
4. Discussion
In our study, the total sample size was 88 with 71.59% males (n = 63) and 28.41% females (n = 25). 58.7% (n = 37) of the males achieved ROSC, while 41.3% (n = 26) did not. On the other hand, 44% (n = 11) of the females achieved ROSC, while 56% (n = 14) did not. The number of females achieving ROSC was lower; however, this does not take into account the type of rhythm and any underlying comorbidities. Also, there was no statistical difference in the duration of CPR received by both the sexes. Based on previous studies, sudden cardiac death is more common in men than in women, but on the other hand, the incidence of ventricular fibrillation is less in women which is considered a favorable rhythm.14 Our study, however, was too small to draw any conclusion about the outcome of CPR in male and female. The mean age of our patient population was 71.94 years (17–94). It has been seen that the outcomes of CPR worsen, and the rate of sudden cardiac death increases particularly after the age of 45 years.15 Our study did not show any correlation between age and duration of CPR. We believe this may have been because of the fact that these patients groups may have differed in comorbidities and the cause or setting of the cardiac arrest too may have played a role in the duration of CPR and the outcomes.
One of the most important prognostic factors regarding the outcome of CPR is the duration it was administered. The main aim of this study was to look at how long CPR was attempted and its correlation with achieving ROSC. A study by Goldberger ZD et al. looked at over 64000 patients who suffered a cardiac arrest while in hospital.16 It demonstrated ROSC in about half of the patients, and the mean time to ROSC was about 12 min. Another study also demonstrates achievement of ROSC in about half of their sample.13 In our study, overall, the average duration of CPR lasted 19.68 min with a minimum of 0 min and a maximum of 67 min. The return of spontaneous circulation was achieved in 54.55% of the cases (n = 48) in our study. We further looked at the duration of CPR in patients who achieved ROSC and those who did not. The mean duration of CPR received in patients who achieved ROSC was 12.93 ± 1.7; on the other hand; the mean duration of CPR in patients who did not achieve ROSC was 27.77 ± 2.1.
The mean duration of CPR in patients who did not achieve ROSC was 14.83 ± 2.79 higher than patients who did achieve ROSC initially, and this difference was statistically different. This implies that the best results achieved with CPR were usually within 15 min and that CPR more than 25 min generally have a poor outcome. Our study did have some outliers, and five patients did achieve ROSC at 25 min or more of CPR. 80% (n = 4) of these patients, however, died in the immediate post-ROSC, indicating that even if they achieve ROSC, they have poorer outcomes. Our results are fairly consistent with the studies mentioned above.13,16
It is also important to analyze how the survival rates at different time intervals after ROSC were achieved. The study by Rohlin O et al shows that in patients who achieved ROSC, greater than 50% of those lived for at least 30 days.13 In our study, we looked at the subgroup who had achieved ROSC (n = 48), and we studied the survival after ROSC. First, we evaluated how many patients survived the immediate post-ROSC period after achieving ROSC. 41.67% (n = 20) patients survived, while 58.33% (n = 28) died in the immediate post-ROSC period. Of the patients who had survived, 25% (n = 5) subsequently died within a week. Overall, only 15 out of 88 patients in our study actually survived up to discharge, and they were not studied after their discharge.
It is very difficult to study the effect of the duration of CPR on survival because of a lot of confounding factors and patient-to-patient variability. Most of the patients in our study had a lot of comorbidities, and this does not take into account the acute changes in patients’ health status before their cardiac arrest. About 65% of the patients had hypertension, 58% of the patients had hyperlipidemia and 42% of the patients had prior coronary artery disease. So, more than half of the patients had risk factors for an adverse cardiac event. We did analyze the differences in CPR durations in patients with different comorbidities, including hypertension, hyperlipidemia and CAD, but we did not find any statistically significant difference in CPR duration in both groups. However, the general trend in the most of the studies is that the longer the duration of CPR, the worse the outcome is. Our study is consistent with this.
The authors also took a look at the setting where the cardiac arrests took place, and the majority were in a medical intensive care unit (MICU) setting, 55.86% (n = 49), and the rest 44.31% (n = 39) were on the general medical floor. It has also been noticed that the mortality from in-hospital cardiac arrest is further trending downward, and it has decreased more than out of hospital cardiac arrest; however, even in the in-hospital arrests, the department or location also affects outcome.15 In our study, slightly more patients in the non-ICU group achieved ROSC (59% vs. 51%), and the mean duration of CPR received was also 3.25 min more on average. This may have been because of the fact that non-ICU patients tend to be less sick in general. This difference, however, was not statistically different.
In-hospital cardiac arrests are mostly witnessed as the patients are usually monitored, and medical assistance is available instantly in the form of CPR and defibrillation. Rakić D et al. looked at a population of approximately 32 thousand patients in a hospital with cardiac arrest and found that 76.7% were witnessed.5 In another study 73% of patients who had an in-hospital cardiac arrest were witnessed and monitored.17 It was also noted that with a witnessed arrest, the odds of survival to discharge and neurological outcomes are better.17 In our study, the cardiac arrests were mostly witnessed 94.31% (n = 83) with 5.69% (n = 5) of the cardiac arrests which were unwitnessed. 55% of the patients with a witnessed arrest achieved ROSC as compared with 40% of the unwitnessed patients. However, the duration of CPR received was not statistically different.
It is also important to discuss the etiologies of cardiac arrest. The most common cause is coronary artery disease which is responsible for about 60–70% of cardiac arrests.18 A study by Spaulding CM et al. looked at the incidence of coronary occlusion in patients who came in with out-of-hospital sudden cardiac arrest. They found that almost half of their sample indeed had coronary artery occlusion.19 Other causes can include structural heart disease which is responsible for about 10% of deaths.18,20 Without structural heart disease, sudden cardiac death can be due to arrhythmias such as Wolff-Parkinson-White syndrome, Long QT syndrome, and Brugada syndrome. These account for about 5–10% of cases.21,22 There can also be “noncardiac” cardiac arrests due to other causes. Some of them include pulmonary emboli, trauma, drug intoxication, and intracranial hemorrhage.23 Heart failure is also a cause of sudden cardiac death, and it is associated with ventricular arrhythmias, asystole, and electromechanical dissociation.24 At the beginning of resuscitation, in our study, we analyzed if the cardiac arrest was presumed to be cardiac in etiology. 30.68% (n = 27) were thought to be cardiac in etiology, while the rest 69.32% (n = 61) were not.
Meaney PA et al looked at EKG rhythms and the effect on survival. They analyzed approximately 50000 cardiac arrest events. The most frequent rhythms were asystole and PEA at 39% and 37%, respectively. Pulseless ventricular tachycardia was seen in 7%, and ventricular fibrillation was seen in 17% of patients.25 The types of initial rhythms during the cardiac arrest were also noted in our study and are presented below (Table 3), PEA being the most common.
Table 3.
The frequency of different types of rhythms found in our patients.
| Rhythm | Percentage |
|---|---|
| Pulseless electrical activity (n = 49) | 55.68% |
| Ventricular fibrillation (n = 15) | 17.04% |
| Pulseless ventricular tachycardia (n = 9) | 10.23% |
| Asystole (n = 8) | 0.91% |
| Uncommon: | |
| Bradycardia (n = 3) | |
| Polymorphic ventricular tachycardia (n = 2) | 16.14% |
| Vtach/Vf (n = 1) | |
| Undocumented (n = 1) | |
During the cardiac arrest, the Vfib, and pulseless Vtach were both shocked. The undocumented rhythm was not shocked telling us that it was not Vfib or pulseless Vtach.
The use of IV amiodarone is demonstrated in the ALIVE26 and ARREST27 trials that demonstrated its efficacy in out of hospital cardiac arrests. It was this thought that this can also be applied to in-hospital cardiac arrests and subsequently added to the AHA ACLS guidelines. Another trial looked at IV amiodarone administration in the in-hospital setting and found that it provided no survival benefit.28 In our patients, amiodarone was administered 23.86% of the time (n = 21) following ACLS recommendations.
5. Limitations
The age range of our patients was very wide, with patients as young as 17 and as old as 80 years; therefore, we did not find any trend of CPR duration with age. In general, as the age would increase especially above 70 years, we would expect a longer duration of CPR required and worsening outcomes; however, this was not true in all cases. We could not find any significant effect of CPR duration and co-morbidities because of the relatively lower sample size. Our study was likely underpowered because of this.
6. Conclusion
Our study shows that CPR duration is inversely associated with the establishment rates of ROSC. Most of the benefits of CPR can be achieved in the first 10 to 15 min, and a further increase in the duration of CPR provides a minimal gain. Still, survival was achievable till 38 min in some cases, and the ideal duration of resuscitation should remain a bedside decision taking into consideration the whole clinical picture.
Financial disclosure or funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
All authors have none to declare.
Informed consent
Informed consent was taken from all the patients.
Ethics
IRB was approved by the institution.
Acknowledgment
None to declare.
References
- 1.Nasiripour A.A., MasoudiAsl I., Fathi E. The relationship of CPR success and time of patients' referring to emergency department. J Mil Med. 2012 Apr 15;14(1):21–25. [Google Scholar]
- 2.Timerman A., Sauaia N., Piegas L.S. Prognostic factors of the results of cardiopulmonary resuscitation in a cardiology hospital. Arq Bras Cardiol. 2001 Aug;77(2):152–160. doi: 10.1590/s0066-782x2001000800006. [DOI] [PubMed] [Google Scholar]
- 3.Khan A.M., Kirkpatrick J.N., Yang L. American Heart Association's Get with the Guidelines-Resuscitation (GWTG-R) Investigators. Age, sex, and hospital factors are associated with the duration of cardiopulmonary resuscitation in hospitalized patients who do not experience sustained return of spontaneous circulation. J Am Heart Assoc. 2014 Dec 17;3(6) doi: 10.1161/JAHA.114.001044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sandroni C., Nolan J., Cavallaro F. In-hospital cardiac arrest: incidence, prognosis and possible measures to improve survival. Intensive Care Med. 2007 Feb 1;33(2):237–245. doi: 10.1007/s00134-006-0326-z. [DOI] [PubMed] [Google Scholar]
- 5.Rakić D., Rumboldt Z., Carević V. In-hospital cardiac arrest and resuscitation outcomes: rationale for sudden cardiac death approach. Croat Med J. 2005 Dec 1;46(6) [PubMed] [Google Scholar]
- 6.Ehlenbach W.J., Barnato A.E., Curtis J.R. Epidemiologic study of in-hospital cardiopulmonary resuscitation in the elderly. N Engl J Med. 2009 Jul 2;361(1):22–31. doi: 10.1056/NEJMoa0810245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cooper S., Janghorbani M., Cooper G. A decade of in-hospital resuscitation: outcomes and prediction of survival? Resuscitation. 2006 Feb 1;68(2):231–237. doi: 10.1016/j.resuscitation.2005.06.012. [DOI] [PubMed] [Google Scholar]
- 8.Peberdy M.A., Kaye W., Ornato J.P. NRCPR Investigators. Cardiopulmonary resuscitation of adults in the hospital: a report of 14 720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003 Sep 1;58(3):297–308. doi: 10.1016/s0300-9572(03)00215-6. [DOI] [PubMed] [Google Scholar]
- 9.Miranzadeh S., Adib-Hajbaghery M., Hosseinpour N. A prospective study of survival after in-hospital cardiopulmonary resuscitation and its related factors. Trauma Mon. 2016 Feb;21(1) doi: 10.5812/traumamon.31796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eftychiou C.H., Georgiou M.A., Andreou A.N. Nicosia General Hospital cardiac arrest team: first year's practice and outcomes of in-hospital resuscitation. Hellenic J Cardiol. 2009;50(4):264–268. [PubMed] [Google Scholar]
- 11.Sekhon M.S., Ainslie P.N., Griesdale D.E. Clinical pathophysiology of hypoxic ischemic brain injury after cardiac arrest: a “two-hit” model. Crit Care. 2017 Dec;21(1):90. doi: 10.1186/s13054-017-1670-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nagao K., Nonogi H., Yonemoto N. Duration of prehospital resuscitation efforts after out-of-hospital cardiac arrest. Circulation. 2016 Apr 5;133(14):1386–1396. doi: 10.1161/CIRCULATIONAHA.115.018788. [DOI] [PubMed] [Google Scholar]
- 13.Rohlin O., Taeri T., Netzereab S. Duration of CPR and impact on 30-day survival after ROSC for in-hospital cardiac arrest—a Swedish cohort study. Resuscitation. 2018 Nov 1;132:1–5. doi: 10.1016/j.resuscitation.2018.08.017. [DOI] [PubMed] [Google Scholar]
- 14.Kim C., Fahrenbruch C.E., Cobb L.A. Out-of-hospital cardiac arrest in men and women. ACC Curr J Rev. 2002;3(11):72. doi: 10.1161/hc4701.099784. [DOI] [PubMed] [Google Scholar]
- 15.Adabag A.S., Luepker R.V., Roger V.L. Sudden cardiac death: epidemiology and risk factors. Nat Rev Cardiol. 2010 Apr;7(4):216. doi: 10.1038/nrcardio.2010.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goldberger Z.D., Chan P.S., Berg R.A. American heart association get with the guidelines—resuscitation (formerly the national registry of cardiopulmonary resuscitation) investigators. Duration of resuscitation efforts and survival after in-hospital cardiac arrest: an observational study. The Lancet. 2012 Oct 27;380(9852):1473–1481. doi: 10.1016/S0140-6736(12)60862-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brady W.J., Gurka K.K., Mehring B. In-hospital cardiac arrest: impact of monitoring and witnessed event on patient survival and neurologic status at hospital discharge. Resuscitation. 2011 Jul 1;82(7):845–852. doi: 10.1016/j.resuscitation.2011.02.028. [DOI] [PubMed] [Google Scholar]
- 18.Zheng Z.J., Croft J.B., Giles W.H. Sudden cardiac death in the United States, 1989 to 1998. Circulation. 2001 Oct 30;104(18):2158–2163. doi: 10.1161/hc4301.098254. [DOI] [PubMed] [Google Scholar]
- 19.Spaulding C.M., Joly L.M., Rosenberg A. Immediate coronary angiography in survivors of out-of-hospital cardiac arrest. N Engl J Med. 1997 Jun 5;336(23):1629–1633. doi: 10.1056/NEJM199706053362302. [DOI] [PubMed] [Google Scholar]
- 20.Eckart R.E., Scoville S.L., Campbell C.L. Sudden death in young adults: a 25-year review of autopsies in military recruits. Ann Intern Med. 2004 Dec 7;141(11):829–834. doi: 10.7326/0003-4819-141-11-200412070-00005. [DOI] [PubMed] [Google Scholar]
- 21.Priori S.G. Survivors of out-of-hospital cardiac arrest with apparently normal heart: need for definition and standardized clinical evaluation. Circulation. 1997;95(1):265–272. doi: 10.1161/01.cir.95.1.265. [DOI] [PubMed] [Google Scholar]
- 22.Chugh S.S., Kelly K.L., Titus J.L. Sudden cardiac death with apparently normal heart. Circulation. 2000 Aug 8;102(6):649–654. doi: 10.1161/01.cir.102.6.649. [DOI] [PubMed] [Google Scholar]
- 23.Kuisma M., Alaspää A. Out-of-hospital cardiac arrests of non-cardiac origin: epidemiology and outcome. Eur Heart J. 1997 Jul 1;18(7):1122–1128. doi: 10.1093/oxfordjournals.eurheartj.a015407. [DOI] [PubMed] [Google Scholar]
- 24.Saour B., Smith B., Yancy C.W. Heart failure and sudden cardiac death. Card electrophysiol clin. 2017 Dec 1;9(4):709–723. doi: 10.1016/j.ccep.2017.07.010. [DOI] [PubMed] [Google Scholar]
- 25.Meaney P.A., Nadkarni V.M., Kern K.B. Rhythms and outcomes of adult in-hospital cardiac arrest. Crit Care Med. 2010 Jan 1;38(1):101–108. doi: 10.1097/CCM.0b013e3181b43282. [DOI] [PubMed] [Google Scholar]
- 26.Dorian P., Cass D., Schwartz B. Amiodarone as compared with lidocaine for shock-resistant ventricular fibrillation. N Engl J Med. 2002 Mar 21;346(12):884–890. doi: 10.1056/NEJMoa013029. [DOI] [PubMed] [Google Scholar]
- 27.Kudenchuk P.J., Cobb L.A., Copass M.K. Amiodarone for resuscitation after out-of-hospital cardiac arrest due to ventricular fibrillation. N Engl J Med. 1999 Sep 16;341(12):871–878. doi: 10.1056/NEJM199909163411203. [DOI] [PubMed] [Google Scholar]
- 28.Pollak P.T., Wee V., Al-Hazmi A. The use of amiodarone for in-hospital cardiac arrest at two tertiary care centres. Can J Cardiol. 2006 Mar 1;22(3):199–202. doi: 10.1016/s0828-282x(06)70896-0. [DOI] [PMC free article] [PubMed] [Google Scholar]