Abstract
Background
The aim of this study is to analyze sex-specific readmission rates, etiology, and predictors of readmission after transcatheter aortic valve replacement (TAVR). Readmissions after TAVR are common, contributing to increased health care utilization and costs. Many factors have been discovered as predictors of readmission; however, sex-specific disparities in readmission rates are limited.
Methods
Between January 2012 and September 2015, adult patients after TAVR were identified using appropriate international classifications of diseases, ninth revision, clinical modification from the National Readmission Database. Incidence of unplanned 30-days readmission rate was the primary outcome of this study. In addition, this study includes sex-specific etiology and predictors of readmissions. Multivariate logistic regression was performed to analyze adjusted readmission rates. Hierarchical 2-level logistic models were used to evaluate predictors of readmission.
Results
Readmission rate at 30 days was 17.3%, with slightly higher readmission rates in women (OR 1.09; CI: 1.01–1.19, p < 0.001) after multivariate adjusted analysis. Noncardiac causes were responsible for most readmissions in both genders. Etiologies for readmissions such as arrhythmias, pulmonary complications, and infections were slightly higher in women, whereas heart failure and bleeding complications were higher in men. History of heart failure, atrial fibrillation, prior pacemaker, and renal failure significantly strongly predicted readmissions in both genders.
Conclusion
Women undergoing TAVR have slightly higher 30-day all-cause readmission rates. These results indicate that women require more attention compared to men to prevent 30-day readmission. In addition, risk stratification for men and women based on predictors will help identify high-risk men and women for readmissions.
Keywords: Sex, Transcatheter aortic valve replacement, Readmissions, Predictors
1. Introduction
The transcatheter aortic valve replacement (TAVR) has been increasingly utilized as an intervention for the management of symptomatic intermediate- and high-risk severe aortic stenosis, and with utilization rates expected to increase exponentially worldwide.1, 2 Several factors have led to better outcomes in TAVR in recent years, including the increase in procedural volume and operator experience, the technical and procedural refinements, besides improved patient's selection.3 However, there is an ongoing urge for further improvements in outcomes, specifically readmission rates, as readmissions are associated with higher financial burden and adversely affects quality of life.4 Thirty-day readmission rate is an important quality metric measure used for cardiovascular diseases and procedures such as heart failure, myocardial infarction, percutaneous coronary intervention, and coronary artery bypass grafting.5 A recent study by Kolte et al demonstrated 30-day readmission rates for TAVR was estimated to be 17.9%; however, gender-specific readmission rates were not shown.4 In addition, Khera et al have generated the risk tool to predict a 30-day readmission rate for TAVR patients, which once validated, we believe it would be of a great value especially in patient's selection.6 Although nine factors including anemia, atrial fibrillation, chronic liver disease, chronic lung disease, chronic kidney disease, end-stage renal disease on dialysis, length of stay 5 days or more, acute kidney injury, and discharge disposition were used to generate the aforementioned risk tool, other important factors such as the effect of gender on outcomes was left behind.6 Gender was an important factor for readmission and was included in predictions of readmission with other interventional procedures.7
In this study, we analyzed sex-specific difference in readmission rates after TAVR. In addition, we studied sex-specific differences in etiology and predictors to better understand target high-risk patients. This study can potentially help reduce readmission rates and associated financial burdens.
2. Methods
2.1. Data source
This study utilized Nationwide Readmission Database (NRD) from January 2012 to September 2015. The NRD is part of the all-payer databases established by the Agency for Healthcare Research and Quality for the Healthcare Cost and Utilization Project. The NRD represents ~50% of all US hospitalizations. It includes discharge records of patients treated in the 21 states of the US hospitals, excluding rehabilitation and long-term acute care facilities. Discharge weights are provided to calculate national estimates. The NRD contains verified patient linkage numbers that could be used to track a patient across hospitals within a state. However, the patient linkage numbers do not track the same person from 1 year into the following year. Patients were tracked using variable “NRD_visitlink,” and time between 2 admissions was calculated by subtracting variable “NRD_DaysToEvent.” This study was deemed exempt by the Institutional Review Board as the NRD is a publicly available data that contains deidentified database. More details regarding NRD data have been published earlier.4, 8
2.2. Study population
We identified patients who underwent TAVR procedure using International Classification of Diseases, Ninth Edition, Clinical Modification (ICD-9-CM) procedure codes 35.05 and 35.06 from the NRD database, which has been utilized previously.4, 9 We included hospitalizations from January 2012 to September 2015 as ICD-10-CM codes were utilized after September 2015. Hospitalization records were excluded if (1) discharge month was December for years 2012–2014 and September for year 2015 because 30-day readmission data would not be available; (2) subject died during the index hospitalization; and (3) age <18 years, and 4) subjects with missing age, gender, and death information (Supplement Figure 1). Similar methods were used previously.4, 8
2.3. Outcomes
The primary outcome was the rate of all-cause unplanned readmission within 30 days of hospitalization with TAVR in men and in women. We reviewed the primary diagnosis of each readmission record for men and women and grouped them into clinically meaningful categories to determine the main cause of readmission. This strategy has been utilized previously.4 Causes of readmissions were classified as cardiac and noncardiac. We also examined secondary in-hospital outcomes such as length of stay and disposition in both men and women cohort.
2.4. Patient and hospital characteristics
Baseline patient characteristics included demographics such as age, median household income by ZIP code, primary expected payer, weekend versus weekday admission, and other relevant comorbidities (e.g., obesity, congestive heart failure, hypertension, diabetes, smoking, dyslipidemia, known coronary artery disease, prior percutaneous coronary intervention, prior myocardial infarction, prior coronary artery bypass grafting, atrial fibrillation, prior permanent pacemaker, prior implantable cardioverter defibrillator, renal failure, chronic liver disease, chronic lung disease) and in-hospital procedures such as coronary angiography, percutaneous coronary intervention, and mechanical circulatory support. We used “cm_” variables provided by Healthcare Cost and Utilization Project to identify different comorbidities which use ICD-9-CM diagnoses and the diagnosis-related group in effect on the discharge date. These comorbidities are not directly related to the principal diagnosis or the main reason for admission and are likely to have originated before the hospital stay.10 ICD-9-CM codes used to identify other comorbidities and in-hospital procedures are given in Supplementary Table 1. Hospital-related characteristics, such as bed size (small, medium, and large), location (urban vs rural), and teaching status, were also included.
2.5. Statistical analysis
Baseline patient and hospital characteristics, comorbidities, in-hospital procedures, and in-hospital outcomes were compared between patients with and without 30-day readmission using Pearson χ2 test for categorical variables and Student's t-test for continuous variables.
SAS 9.4 (SAS Institute Inc., Cary, North Carolina) was used for analyses. Categorical variables were presented as frequencies and percentages, whereas continuous variables as mean ± standard deviations or median (interquartile range) depending on their distribution. Hierarchical 2-level logistic models with hospital ID as random effect were used to evaluate predictors of readmission for men and women. Multivariate models for readmission included patient-level variables such as age, median household income (higher income quartile vs lowest income quartile), primary payer (private insurance [including Health Maintenance Organization] and self-pay versus Medicaid/Medicare), all comorbidities, in-hospital procedures, and all hospital level variables as explained previously. A 2-sided value of p < 0.05 was set for statistical significance in all analyses.
3. Results
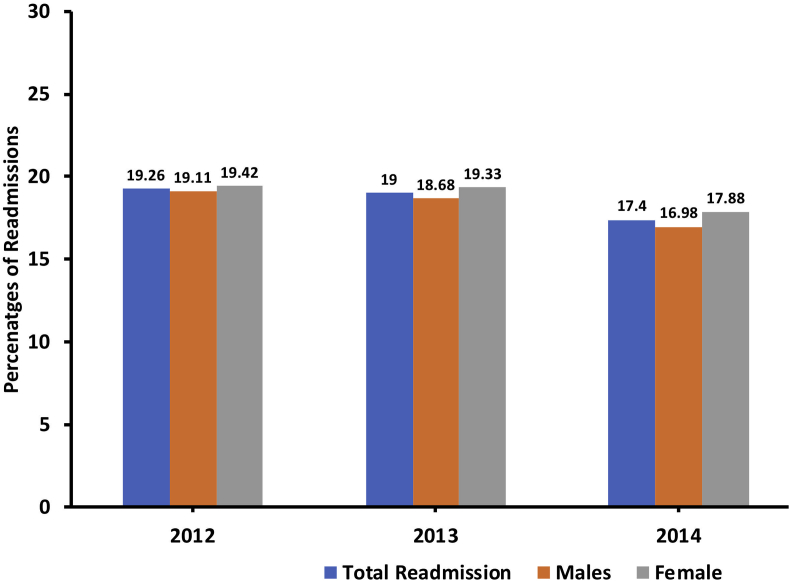
Between January 2012 and September 2015, a total of 26,233 patients were included in this study. Prevalence of TAVR was comparable in men and in women (53% vs. 47%). From the study population, 4532 (17.2%) patients were readmitted. Total readmission rate trended down from 2012 to 2015 (19.3%–16.1%, Ptrend<0.001). Total readmission rate was slightly higher in women (17.1% in men and 18% in women, p < 0.001). This readmission rate trended down in men (19.1%–15.5%, Ptrend<0.001) as well in women (19.4%–16.8%, Ptrend<0.001) (Fig. 1).
Fig. 1.
All-cause readmission rates in overall TAVR patients and further stratified by men and women. Ptrend value for all <0.001. TAVR, transcatheter aortic valve replacement.
Cardiac causes were responsible for 38.3% of the readmissions in men and 35.8% in women, among which heart failure was the most prevalent (23.5% in men vs. 21.9% in women), followed by arrhythmias (6.2% in men vs. 6.8% in women). Other common reasons for readmissions were pulmonary complications and infections, both slightly higher in women than men. Bleeding and renal complications were also among the major reasons for readmission to the hospital (Supplement Figure 2 and 3).
Women were slightly older in this study (80.6 vs. 81.8 years, p < 0.001). There were differences in baseline characteristics in men and in women. Women have higher prevalence of obesity (13.9% vs 18.2%, p < 0.001), heart failure (6.8% vs 7.5%, p = 0.003), and hypertension (80% vs. 80.8%, p = 0.006), whereas other comorbidities were higher in men. Women more frequently underwent TAVR using transapical approach as opposed to transfemoral approach and required more blood transfusions than men (15.6% vs 23.4%, p < 0.001). However, men required more mechanical circulatory support (1.6% vs. 1.0%, p < 0.001). No statistically significant difference was noted in the utilization of coronary angiography and percutaneous coronary intervention (PCI) rates between both groups (Table 1). Supplementary Table 2 demonstrated gender differences based on whether they were readmitted to the hospital.
Table 1.
Demographics and baseline characteristics for patients undergoing transcatheter aortic valve replacement: Stratified by gender.
| Variables | Men (n = 13,922) | Women (n = 12,301) | Total (n = 26,223) | p value |
|---|---|---|---|---|
| Weighted Frequency | 28,432 | 25,685 | 54,117 | <0.001 |
| Mean age | 80.6 ± 12.6 | 81.8 ± 11.7 | ||
| Comorbidities | ||||
| Obesity | 13.94 | 18.17 | 15.95 | <0.001 |
| Heart failure | 6.82 | 7.46 | 7.12 | 0.004 |
| Hypertension | 79.98 | 80.85 | 80.39 | 0.011 |
| Diabetes mellitus | 37.79 | 32.32 | 35.19 | <0.001 |
| Smoking | 32.78 | 18.41 | 25.96 | <0.001 |
| Dyslipidemia | 65.41 | 62.61 | 64.08 | <0.001 |
| History of coronary artery disease | 76.33 | 59.07 | 68.14 | <0.001 |
| Prior myocardial infarction | 15.37 | 9.27 | 12.48 | <0.001 |
| Prior percutaneous coronary intervention | 22.57 | 17.07 | 19.96 | <0.001 |
| Prior coronary artery bypass grafting | 30.64 | 10.99 | 21.31 | <0.001 |
| Atrial fibrillation | 46.23 | 44.55 | 45.43 | <0.001 |
| Prior permanent pacemaker | 11.71 | 9.49 | 10.66 | <0.001 |
| Prior implantable cardioverter defibrillator | 4.6 | 1.22 | 3 | <0.001 |
| Renal failure | 40.37 | 30.09 | 35.49 | <0.001 |
| Chronic liver disease | 2.97 | 2.24 | 2.62 | <0.001 |
| Chronic lung disease | 33.96 | 32.97 | 33.49 | 0.015 |
| Procedural details | ||||
| Coronary angiography | 23.13 | 23.68 | 23.39 | 0.13 |
| Percutaneous coronary intervention | 3.62 | 3.49 | 3.56 | 0.42 |
| Mechanical circulatory support | 1.64 | 0.99 | 1.33 | <0.001 |
| Transfemoral approach | 84.48 | 81.7 | 83.16 | <0.001 |
| Transapical approach | 15.68 | 18.47 | 17 | <0.001 |
| Blood transfusion | 15.6 | 23.35 | 19.28 | <0.001 |
| Median household income category for patient's zip code | ||||
| 0-25th percentile | 19.93 | 20.14 | 20.03 | 0.01 |
| 26-50th percentile | 24.52 | 25.24 | 24.86 | |
| 51-75th percentile | 26.52 | 26.1 | 26.32 | |
| 76-100th percentile | 27.63 | 27.4 | 27.52 | |
| Primary payer | ||||
| Medicare/Medicaid | 90.74 | 94.17 | 92.37 | <0.001 |
| Private insurance | 6.39 | 4.85 | 5.66 | |
| Self-pay/others | 2.78 | 0.92 | 1.89 | |
| Admission type | ||||
| Emergency/urgent | 21.96 | 22.86 | 22.39 | 0.01 |
| Elective | 78.04 | 77.14 | 77.61 | |
| Hospital-level characteristics | ||||
| Hospital bed size | ||||
| Small | 4.17 | 4.16 | 4.17 | 0.07 |
| Medium | 13.64 | 14.33 | 13.96 | |
| Large | 82.19 | 81.51 | 81.87 | |
| Hospital teaching status | ||||
| Non-teaching | 9.1 | 9.04 | 9.07 | 0.80 |
| Teaching | 90.9 | 90.96 | 90.93 | |
| Admission day | ||||
| Weekdays | 94.13 | 94.51 | 94.31 | 0.057 |
| Weekend | 5.87 | 5.49 | 5.69 | |
The bold items are the major variables which has sub-variables.
There were 3 cardiac conditions associated with increased risk of readmission including heart failure (OR 3.44 in men, 3.65 in women), followed by the presence of prior permanent pacemaker (OR 1.39 in men, 1.32 in women), and atrial fibrillation (OR 1.17 in men, 1.36 in women), p < 0.001 for all. Concerning noncardiac causes, renal failure (OR 1.41 in men, 1.26 in women, p < 0.001 for both) and the need for blood transfusion (OR 1.31 in men, 1.14 in women, p < 0.001 for both) predicted readmission in both genders. While diabetes predicted readmissions only in women (OR 1.19, p < 0.001), chronic lung disease (OR 1.24, p < 0.001) predicted readmissions only in men (Table 2).
Table 2.
Predictors of readmissions for transcatheter aortic valve replacement: Stratified by gender.
| Variables | Men |
Women |
||||||
|---|---|---|---|---|---|---|---|---|
| Odds ratio | Lower limit | Upper limit | p value | Odds ratio | Lower limit | Upper limit | p value | |
| Age | 0.99 | 0.99 | 1.00 | 0.51 | 0.99 | 0.98 | 0.99 | 0.04 |
| Obesity | 0.81 | 0.70 | 0.93 | 0.004 | 0.77 | 0.68 | 0.87 | <0.001 |
| Heart failure | 3.44 | 3.01 | 3.93 | <0.001 | 3.65 | 3.15 | 4.22 | <0.001 |
| Hypertension | 0.78 | 0.69 | 0.87 | <0.001 | 0.85 | 0.75 | 0.95 | 0.005 |
| Diabetes mellitus | 1.06 | 0.95 | 1.20 | 0.29 | 1.19 | 1.08 | 1.31 | <0.001 |
| Smoking | 0.94 | 0.85 | 1.04 | 0.25 | 0.94 | 0.83 | 1.07 | 0.35 |
| Dyslipidemia | 0.75 | 0.68 | 0.82 | <0.001 | 0.85 | 0.78 | 0.93 | <0.001 |
| History of coronary artery disease | 0.89 | 0.80 | 0.98 | 0.023 | 0.97 | 0.88 | 1.06 | 0.51 |
| Prior myocardial infarction | 0.87 | 0.77 | 0.97 | 0.015 | 1.06 | 0.89 | 1.26 | 0.50 |
| Prior percutaneous coronary intervention | 1.10 | 0.97 | 1.24 | 0.13 | 1.09 | 0.95 | 1.26 | 0.22 |
| Prior coronary artery bypass grafting | 0.96 | 0.87 | 1.07 | 0.49 | 0.97 | 0.81 | 1.15 | 0.72 |
| Atrial fibrillation | 1.17 | 1.07 | 1.29 | <0.001 | 1.36 | 1.23 | 1.50 | <0.001 |
| Prior permanent pacemaker | 1.39 | 1.24 | 1.57 | <0.001 | 1.32 | 1.16 | 1.49 | <0.001 |
| Prior implantable cardioverter defibrillator | 1.20 | 0.98 | 1.48 | 0.08 | 1.00 | 0.72 | 1.40 | 0.99 |
| Renal failure | 1.41 | 1.29 | 1.55 | <0.001 | 1.26 | 1.13 | 1.40 | <0.001 |
| Chronic liver disease | 1.14 | 0.88 | 1.46 | 0.32 | 1.13 | 0.77 | 1.65 | 0.52 |
| Chronic lung disease | 1.24 | 1.13 | 1.36 | <0.001 | 1.08 | 0.98 | 1.20 | 0.11 |
| Procedural details | ||||||||
| Coronary angiography | 0.62 | 0.55 | 0.70 | <0.001 | 0.55 | 0.48 | 0.63 | <0.001 |
| Percutaneous coronary intervention | 1.00 | 0.76 | 1.32 | 0.98 | 0.81 | 0.62 | 1.07 | 0.13 |
| Mechanical circulatory support | 0.78 | 0.55 | 1.11 | 0.17 | 0.87 | 0.54 | 1.340 | 0.56 |
| Blood transfusion | 1.31 | 1.16 | 1.48 | <0.001 | 1.14 | 1.15 | 1.17 | <0.001 |
| Transfemoral approach vs. transapical approach | 0.62 | 0.53 | 0.71 | <0.001 | 0.57 | 0.49 | 0.66 | <0.001 |
| Median household income category for patient's zip code | ||||||||
| 0-25th percentile | Reference | Reference | Reference | Reference | Reference | Reference | ||
| 26-50th percentile | 0.96 | 0.82 | 1.13 | 0.64 | 0.96 | 0.82 | 1.12 | 0.59 |
| 51-75th percentile | 1.03 | 0.88 | 1.21 | 0.68 | 0.90 | 0.77 | 1.05 | 0.17 |
| 76-100th percentile | 1.00 | 0.86 | 1.18 | 0.97 | 0.97 | 0.83 | 1.14 | 0.76 |
| Primary payer | ||||||||
| Medicare/Medicaid | Reference | Reference | Reference | Reference | Reference | Reference | ||
| Private insurance | 0.79 | 0.66 | 0.96 | 0.015 | 0.83 | 0.63 | 1.09 | 0.17 |
| Self-pay/others | 0.53 | 0.39 | 0.73 | <0.001 | 0.88 | 0.60 | 1.28 | 0.51 |
| Hospital-level characteristics | ||||||||
| Hospital bed size | ||||||||
| Small | Reference | Reference | Reference | Reference | Reference | Reference | ||
| Medium | 0.80 | 0.60 | 1.05 | 0.11 | 0.75 | 0.58 | 0.98 | 0.033 |
| Large | 0.61 | 0.47 | 0.79 | <0.001 | 0.65 | 0.52 | 0.82 | <0.001 |
| Hospital teaching status | ||||||||
| Nonteaching | Reference | Reference | Reference | Reference | Reference | Reference | ||
| Teaching | 0.47 | 0.40 | 0.56 | <0.001 | 0.51 | 0.43 | 0.61 | <0.001 |
After multivariate adjustment, odds of 30-day readmission were significantly higher in women (OR 1.09; CI: 1.01–1.19, p < 0.001). After index admissions, women had higher odds of discharge to short- or long-term facilities (OR 1.61, p < 0.001) rather than home. Women also had higher odds of hospital stay for more than five days (OR 1.61; CI: 1.50–1.72 p < 0.001). Table 3 displays the adjusted outcomes based on gender (Table 3).
Table 3.
Adjusted outcomes for transcatheter aortic valve replacement.
| Outcomes | Odds ratio | Lower limit | Upper limit | p value |
|---|---|---|---|---|
| 30 days readmission | ||||
| Men | Reference | Reference | Reference | Reference |
| Women | 1.09 | 1.01 | 1.19 | <0.001 |
| Disposition | ||||
| Home | ||||
| Men | Reference | Reference | Reference | Reference |
| Women | 0.62 | 0.58 | 0.67 | <0.001 |
| Long-/short-term facility | ||||
| Men | Reference | Reference | Reference | Reference |
| Women | 1.61 | 1.51 | 1.72 | <0.001 |
| Length of stay during index hospitalization >5 days | ||||
| Men | Reference | Reference | Reference | Reference |
| Women | 1.61 | 1.50 | 1.72 | <0.001 |
4. Discussion
All-cause readmission rates at 30-days were slightly higher in women as compared with men who underwent TAVR from 2012 to 2015 in the United States. This study demonstrated that all-cause readmission rates associated with TAVR has been slowly decreasing in men as well as in women as expected. This analysis also highlighted that cardiac etiology, infections, pulmonary etiology, and bleeding were not the most common reasons for readmissions. Cardiac etiology and bleeding were more common in men as compared with women, whereas pulmonary etiology and infections were more common in women as compared with men. In different cardiac etiologies for readmissions, heart failure and arrhythmias were the most common reasons for readmissions in both genders. History of heart failure, atrial fibrillation, prior pacemaker, and renal failure significantly predicted readmissions in both genders. Readmissions rates were significantly lower in patients with private insurance, and patients admitted to the large-bed hospitals or teaching hospitals in men as well in women. This is the all-comers, largest-to-date analysis comparing readmission rates in male and female patients who underwent TAVR.
Patients in both genders presented with different risk profile on index admission. Women presented with slightly higher age as compared with men. More women were obese and had higher heart failure and hypertension. Women more commonly underwent TAVR using transapical approach when compared with men. We are not entirely sure about higher transapical approach in women. These results are in line with previous studies showing higher prevalence of NYHA III/IV class and utilization of nontransfemoral approaches for TAVR in women; however, this study had few women with renal failure undergoing TAVR.11 Aligned with previous data, readmission rates within 30 days were ~17% with TAVR possibly due to reduction in complication rates and improvement in technology.4, 12, 13 Nearly, two-fifth patients were readmitted with cardiac cause which is comparable with previously published studies.14, 15 Infections and pulmonary causes were the other most common reasons for readmission in men and in women which is shown by previous studies.15 Readmission rates were slightly higher in women at 30 days, which is in contrast to a previously published study which showed no difference at 30-days readmission rates between men and women.16 The difference was minimal and we are not sure if this is clinically important. Nonetheless, there are several reasons for this: 1) In previous studies, women were deemed to be frailer than men by heart teams.11 Poor frailty is significantly associated with morbidity and mortality.17 This study did not include frailty score as we do not control for variables. 2) In line with previously published articles, more women underwent transapical approach which is associated with worse outcomes as compared with transfemoral approach.11, 18 Typically, patients undergoing transapical TAVR are sicker and they have complex peripheral vascular disease which was not captured in this study.4 3) Need for blood transfusion was significantly higher in women than in men. Smaller body surface area, smaller peripheral arteries in women, and sheath to femoral artery ratio more than 1 in small peripheral vessels may contribute to it.11, 19 Previous studies demonstrated higher 30-day vascular complications and major bleeding in women undergoing TAVR.16, 20 Postprocedure blood transfusion was an independent predictor of readmission of patients with heart failure who underwent TAVR in previous studies.14, 21
Heart failure on presentation significantly predicted readmissions rates in men and in women, prevalence of which was slightly higher in women on index admission. These patients have heart failure partly due to pressure-overload–induced left-sided cardiac hypertrophy.22 However, pulmonary hypertension–developed secondary to severe aortic stenosis could play a role in progression of heart failure even after TAVR.23 NYHA class III/IV is independently associated with 1-year mortality as well.24 Presence of kidney disease was associated with higher readmission rates, which was demonstrated in multiple previous studies.14, 15 We recommend a nephrology consultation, limited use of contrast agent, and elimination of nephrotoxic agents to reduce readmissions. Atrial fibrillation and permanent pacemaker were another significant predictor for readmission in both genders. Atrial fibrillation is shown to be an independent predictor to increase morbidity and mortality.14, 21, 25 Atrial fibrillation can contribute to myocardial remodeling and fibrosis which can accelerate ventricular aging and ultimately readmissions.26 Chronic lung disease in men was shown to be an independent predictor and diabetes in women was shown to be an independent predictor in this study, and the reason for this difference is largely unknown. Chronic lung disease and chronic kidney disease have shown to be independent predictors of poor outcomes in previous studies.4, 27 As mentioned previously, nontransfemoral approach has been associated with higher readmissions.4, 14 Postprocedure blood transfusion in both genders predicted readmission as demonstrated in multiple previous studies.14, 24 Readmission rates were lower in male patients with private insurance when compared with Medicare/Medicaid. Finally, readmission rates were lower in men as well as women who were admitted to the teaching and large-bed hospital.
To improve 30-day readmission rates, a multidisciplinary approach may help based on the comorbidity present on admission which can predict short- and long-term readmission rates as shown in this study and previous studies.11, 14, 24 In addition, we propose performing this procedures at higher volume centers as they tend to have better outcomes and lower readmissions rates.28 Early postdischarge follow-up for high-risk men and women can reduce readmission rates. More prospective studies are needed demonstrating long-term readmission incidence and etiology in these patients to confirm these results. Better understanding of predictors may help reducing readmission rates associated with TAVR in the future.
There are several limitations which might affect the results of this study. First, this is a retrospective study using NRD which may have coding errors, and readmission to a hospital in another state was not tracked. Second, we do not have information on the severity or frailty as we do not have Society of Thoracic Surgeons score or Kansas City Cardiomyopathy Questionnaire (KCCQ12), valve type, or medical therapy after discharge. Third, no information is available on the type of valve which can impact outcomes and readmissions.29 Fourth, we do not have information on longitudinal outcomes; however, previous study demonstrated better 1-year survival rates in women as compared with men.11, 16 This might be associated with less baseline comorbidities on presentation which is demonstrated in our study. Fifth, we have included data up to 2015 which mainly utilized first-generation valves with larger sheath size. This might be one of the reasons for higher complications as this is almost obsolete in 2019. Nonetheless, this is the all-comers, largest till-date study demonstrating sex-specific differences in patients undergoing TAVR.
In conclusion, women undergoing TAVR have slightly higher 30-day all-cause readmission rates. These results indicate that women require slightly more attention compared to men to prevent 30-day readmission rates. In addition, risk stratification for men and women based on predictors will help identify high-risk men and women for readmissions.
Conflicts of interest
All authors have none to declare.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ihj.2019.09.004.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Nishimura R.A., Otto C.M., Bonow R.O. AHA/ACC focused update of the 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American college of cardiology/American heart association task force on clinical practice guidelines. Circulation. 2017;135(25):e1159–e1195. doi: 10.1161/CIR.0000000000000503. [DOI] [PubMed] [Google Scholar]
- 2.Mylotte D., Osnabrugge R.L.J., Windecker S. Transcatheter aortic valve replacement in Europe: adoption trends and factors influencing device utilization. J Am Coll Cardiol. 2013;62(3):210–219. doi: 10.1016/j.jacc.2013.03.074. [DOI] [PubMed] [Google Scholar]
- 3.Beohar N., Kirtane A.J., Blackstone E. Trends in complications and outcomes of patients undergoing transfemoral transcatheter aortic valve replacement: experience from the PARTNER continued access registry. JACC Cardiovasc Interv. 2016;9(4):355–363. doi: 10.1016/j.jcin.2015.10.050. [DOI] [PubMed] [Google Scholar]
- 4.Kolte D., Khera S., Sardar M.R. Thirty-day readmissions after transcatheter aortic valve replacement in the United States: insights from the Nationwide readmissions database. Circ Cardiovasc Interv. 2017;10(1) doi: 10.1161/CIRCINTERVENTIONS.116.004472. [DOI] [PubMed] [Google Scholar]
- 5.Hospital Readmissions Reduction Program (HRRP) Center for Medicare and Medicaid Services. 2016. https://www.cms.gov/medicare/medicare-fee-for-service-payment/acuteinpatientpps/readmissions-reduction-program.html [Google Scholar]
- 6.Khera S. 2018. Late-Breaking Clinical Science II: Derivation of a Simple Risk Tool to Predict 30-day Readmission after Transcatheter Aortic Valve Replacement. Presented at: Society for Cardiovascular Angiography and Interventions Scientific Sessions; April 25-28. San Diego. [Google Scholar]
- 7.Lam L., Ahn H.J., Okajima K. Gender differences in the rate of 30-day readmissions after percutaneous coronary intervention for acute coronary syndrome. Women's Health Issues. 2019;29(1):17–22. doi: 10.1016/j.whi.2018.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arora S., Lahewala S., Tripathi B. Causes and predictors of readmission in patients with atrial fibrillation undergoing catheter ablation: a national population-based cohort study. J Am Heart Assoc. 2018;7(12) doi: 10.1161/JAHA.118.009294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Patel N., Doshi R., Kalra R., Bajaj N.S., Arora G., Arora P. Costs of transcatheter aortic valve replacement: implications of proposed Medicare cuts. JACC Cardiovasc Interv. 2018;11(6):610–612. doi: 10.1016/j.jcin.2018.01.234. [DOI] [PubMed] [Google Scholar]
- 10.Healthcare Cost and utilization Project (HCUP) comorbidity software V. Available at: https://www.hcup-us.ahrq.gov/toolssoftware/comorbidity/comorbidity.jsp. Accessed January 1, 2019.
- 11.Chandrasekhar J., Dangas G., Yu J. Sex-based differences in outcomes with transcatheter aortic valve therapy: TVT registry from 2011 to 2014. J Am Coll Cardiol. 2016;68(25):2733–2744. doi: 10.1016/j.jacc.2016.10.041. [DOI] [PubMed] [Google Scholar]
- 12.Holmes D.R., Jr., Nishimura R.A., Grover F.L. Annual outcomes with transcatheter valve therapy: from the STS/ACC TVT registry. J Am Coll Cardiol. 2015;66(25):2813–2823. doi: 10.1016/j.jacc.2015.10.021. [DOI] [PubMed] [Google Scholar]
- 13.Vahl T.P., Kodali S.K., Leon M.B. Transcatheter aortic valve replacement 2016: a modern-day "through the looking-glass" adventure. J Am Coll Cardiol. 2016;67(12):1472–1487. doi: 10.1016/j.jacc.2015.12.059. [DOI] [PubMed] [Google Scholar]
- 14.Nombela-Franco L., del Trigo M., Morrison-Polo G. Incidence, causes, and predictors of early (</=30 Days) and late unplanned hospital readmissions after transcatheter aortic valve replacement. JACC Cardiovasc Interv. 2015;8(13):1748–1757. doi: 10.1016/j.jcin.2015.07.022. [DOI] [PubMed] [Google Scholar]
- 15.Franzone A., Pilgrim T., Arnold N. Rates and predictors of hospital readmission after transcatheter aortic valve implantation. Eur Heart J. 2017;38(28):2211–2217. doi: 10.1093/eurheartj/ehx182. [DOI] [PubMed] [Google Scholar]
- 16.Kodali S., Williams M.R., Doshi D. Sex-specific differences at presentation and outcomes among patients undergoing transcatheter aortic valve replacement: a cohort study. Ann Intern Med. 2016;164(6):377–384. doi: 10.7326/M15-0121. [DOI] [PubMed] [Google Scholar]
- 17.Martin G.P., Sperrin M., Ludman P.F. Do frailty measures improve prediction of mortality and morbidity following transcatheter aortic valve implantation? An analysis of the UK TAVI registry. BMJ Open. 2018;8(6):e022543. doi: 10.1136/bmjopen-2018-022543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Doshi R., Shah P., Meraj P.M. In-hospital outcomes comparison of transfemoral vs transapical transcatheter aortic valve replacement in propensity-matched cohorts with severe aortic stenosis. Clin Cardiol. 2018;41(3):326–332. doi: 10.1002/clc.22866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hayashida K., Lefevre T., Chevalier B. Transfemoral aortic valve implantation new criteria to predict vascular complications. JACC Cardiovasc Interv. 2011;4(8):851–858. doi: 10.1016/j.jcin.2011.03.019. [DOI] [PubMed] [Google Scholar]
- 20.Genereux P., Webb J.G., Svensson L.G. Vascular complications after transcatheter aortic valve replacement: insights from the PARTNER (Placement of AoRTic TraNscathetER Valve) trial. J Am Coll Cardiol. 2012;60(12):1043–1052. doi: 10.1016/j.jacc.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 21.Durand E., Doutriaux M., Bettinger N. Incidence, prognostic impact, and predictive factors of readmission for heart failure after transcatheter aortic valve replacement. JACC Cardiovasc Interv. 2017;10(23):2426–2436. doi: 10.1016/j.jcin.2017.09.010. [DOI] [PubMed] [Google Scholar]
- 22.Gotzmann M., Rahlmann P., Hehnen T. Heart failure in severe aortic valve stenosis: prognostic impact of left ventricular ejection fraction and mean gradient on outcome after transcatheter aortic valve implantation. Eur J Heart Fail. 2012;14(10):1155–1162. doi: 10.1093/eurjhf/hfs108. [DOI] [PubMed] [Google Scholar]
- 23.O'Sullivan C.J., Wenaweser P., Ceylan O. Effect of pulmonary hypertension hemodynamic presentation on clinical outcomes in patients with severe symptomatic aortic valve stenosis undergoing transcatheter aortic valve implantation: insights from the new proposed pulmonary hypertension classification. Circ Cardiovasc Interv. 2015;8(7):e002358. doi: 10.1161/CIRCINTERVENTIONS.114.002358. [DOI] [PubMed] [Google Scholar]
- 24.Zahn R., Gerckens U., Linke A. Predictors of one-year mortality after transcatheter aortic valve implantation for severe symptomatic aortic stenosis. Am J Cardiol. 2013;112(2):272–279. doi: 10.1016/j.amjcard.2013.03.024. [DOI] [PubMed] [Google Scholar]
- 25.Biviano A.B., Nazif T., Dizon J. Atrial fibrillation is associated with increased mortality in patients undergoing transcatheter aortic valve replacement: insights from the placement of aortic transcatheter valve (PARTNER) trial. Circ Cardiovasc Interv. 2016;9(1):e002766. doi: 10.1161/CIRCINTERVENTIONS.115.002766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Burstein B., Nattel S. Atrial fibrosis: mechanisms and clinical relevance in atrial fibrillation. J Am Coll Cardiol. 2008;51(8):802–809. doi: 10.1016/j.jacc.2007.09.064. [DOI] [PubMed] [Google Scholar]
- 27.Dvir D., Waksman R., Barbash I.M. Outcomes of patients with chronic lung disease and severe aortic stenosis treated with transcatheter versus surgical aortic valve replacement or standard therapy: insights from the PARTNER trial (placement of AoRTic TraNscathetER Valve) J Am Coll Cardiol. 2014;63(3):269–279. doi: 10.1016/j.jacc.2013.09.024. [DOI] [PubMed] [Google Scholar]
- 28.Khera S., Kolte D., Gupta T. Association between hospital volume and 30-day readmissions following transcatheter aortic valve replacement. JAMA Cardiol. 2017;2(7):732–741. doi: 10.1001/jamacardio.2017.1630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.O'Connor S.A., Morice M.C., Gilard M. Revisiting sex equality with transcatheter aortic valve replacement outcomes: a collaborative, patient-level meta-analysis of 11,310 patients. J Am Coll Cardiol. 2015;66(3):221–228. doi: 10.1016/j.jacc.2015.05.024. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.