Abstract
Objective
Hypertension is the most important risk factor for cardiovascular morbidity and mortality. There is limited data on hypertension prevalence in India. This study was conducted to estimate the prevalence of hypertension among Indian adults.
Methods
A national level survey was conducted with fixed one-day blood pressure measurement camps across 24 states and union territories of India. Hypertension was defined as systolic blood pressure (BP) ≥140 mmHg or a diastolic BP ≥90 mmHg or on treatment for hypertension. The prevalence was age- and gender-standardized according to the 2011 census population of India.
Results
Blood pressure was recorded for 180,335 participants (33.2% women; mean age 40.6 ± 14.9 years). Among them, 8,898 (4.9%), 99,791 (55.3%), 35,694 (11.9%), 23,084 (12.8%), 9,989 (5.5%), and 2,878 (1.6%) participants were of the age group 18–19, 20–44, 45–54, 55–64, 65–74, and ≥ 75 years, respectively. Overall prevalence of hypertension was 30.7% (95% confidence interval [CI]: 30.5, 30.9) and the prevalence among women was 23.7% (95% CI: 23.3, 24). Prevalence adjusted for 2011 census population and the WHO reference population was 29.7% and 32.8%, respectively.
Conclusion
There is a high prevalence of hypertension, with almost one in every three Indian adult affected.
Keywords: Hypertension, India, Prevalence
Abbreviations: BP, Blood pressure; CSI, Cardiological Society of India; DBP, Diastolic blood pressure; JNC7, Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; NFHS, National Family Health Survey; NCD, noncommunicable disease; SBP, Systolic blood pressure
1. Introduction
Cardiovascular diseases remain the top cause of global mortality, with an estimated 17.9 million attributed deaths in 2016 (31% of global deaths).1 Hypertension is consistently related to the development of ischemic heart disease, heart failure, stroke, and chronic kidney disease; an estimated 57% and 24% of stroke and coronary artery disease-related deaths, respectively are due to hypertension.2, 3, 4, 5 According to the global burden of diseases estimate 2015, it is the most important cause of mortality as well as the loss of disability-adjusted life years.6
Since the early 1950s, there have been many studies in India reporting the prevalence of hypertension across various geographic, occupational, and linguistic groups.7, 8, 9, 10, 11, 12, 13 Analysis of worldwide data for estimation of the global prevalence of hypertension in 2005 highlighted the lack of a national study investigating the prevalence in India.14 There is also heterogeneity among the present studies in the method of measuring blood pressure (BP) (mercury and aneroid or electronic machines), the definition of hypertension, and enrollment of participants.
This survey was conducted to estimate the prevalence of hypertension among Indian adults.
2. Materials and methods
2.1. Study setting
The study was conducted as a part of Cardiac Prevent 2015—under the aegis of the Cardiological Society of India. On 21 September 2015, from 9am to 5pm, we measured the BP of consecutive adult participants (age ≥18 years) attending the BP camp across 24 states and union territories of India. All participants gave informed written consent.
2.2. Hypertension definition
Hypertension was defined according to the Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7).15
2.3. Blood pressure measurement and data collection
BP was measured using automated oscillometric machines. Before measuring BP, the participant should not have taken tea or coffee in the last 10 min and should have been seated for at least 5 min. Individuals with BP reading ≥140/90 mmHg had their BP remeasured after 3 min; the average of the two BP measurements was recorded. The average BP was rounded off to the nearest whole number. We recorded a self-reported history of hypertension, diabetes, and use of antihypertensive medications. A printed report of BP measurement was provided to the patient. Individual site coordinators were responsible for data collection which was fed real-time into an online portal designed by the Cardiological Society of India. An independent auditor (not involved in data collection) reviewed and verified the number of participants from each site.
2.4. Statistical analysis
Total prevalence was age- and gender-standardized according to 2011 census population of India.16 Distribution of BP across the four classifications (normal, prehypertension, Stage I hypertension and Stage 2 hypertension) was calculated across six mutually exclusive age groups (18–19, 20–44, 45–54, 55–64, 65–74, and ≥ 75 years). Hypertension prevalence was also calculated according to the World Health Organization (WHO) world standard population for the year 2000–2025; as recommended by the World Hypertension League.17,18 All analyses were performed using STATA V15.0 (College Station, TX, USA) statistical software.
3. Results
Across 24 states and union territories of India a total of 180,335 participants [120,425 (66.8%) men and 59,910 (33.2%) women] with mean age 40.6 ± 14.9 years were surveyed. 8,898 (4.9%), 99,791 (55.3%), 35,694 (11.9%), 23,084 (12.8%), 9,989 (5.5%), and 2,878 (1.6%) subjects belonged to age group 18–19, 20–44, 45–54, 55–64, 65–74, and ≥ 75 years respectively. Prevalence of self-reported hypertension and diabetes was 15.9% and 10.1%, respectively.
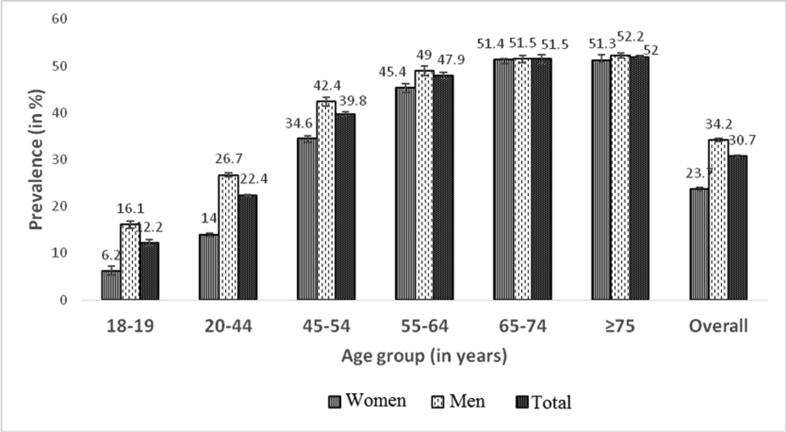
Overall prevalence of hypertension was 30.7% (95% confidence interval [CI]: 29.7, 32.8). Prevalence increased with age; with more men having hypertension in each age group, except in those with age ≥65 years, where almost equal percentage of men and women had hypertension (Table 1 and Fig. 1). Prevalence adjusted for 2011 census population of India was 29.7%; prevalence adjusted for the WHO reference population was 32.8%.
Table 1.
Prevalence of hypertension.
| Age (years) | Men (n = 120,425) | Women (n = 59,910) | Total (n = 180,335) |
|---|---|---|---|
| 18–19 (n = 8,898) | 16.1 (15.1, 17.0) | 6.2 (5.4, 7.0) | 12.2 (11.5, 12.9) |
| 20–44 (n = 99,791) | 26.7 (26.4, 27.1) | 14 (13.6, 14.4) | 22.4 (22.2, 22.7) |
| 45–54 (n = 35,694) | 42.4 (41.8, 43) | 34.6 (33.7, 35.4) | 39.8 (39.4, 40.3) |
| 55–64 (n = 23,084) | 49.0 (48.2, 49.9) | 45.4 (44.2, 46.5) | 47.9 (47.2, 48.5) |
| 65–74 (n = 9,989) | 51.5 (50.3, 52.7) | 51.4 (49.6, 53.3) | 51.5 (50.5, 52.4) |
| ≥75 (n = 2,878) | 52.2 (50.1, 54.4) | 51.3 (47.8, 54.8) | 52.0 (50.2, 53.8) |
| Total (n = 180,335) | 34.2 (33.9, 34.5) | 23.7 (23.3, 24.0) | 30.7 (30.5, 30.9) |
Data as percentage (95% confidence interval).
Fig. 1.
Prevalence of hypertension, according to age group and gender.
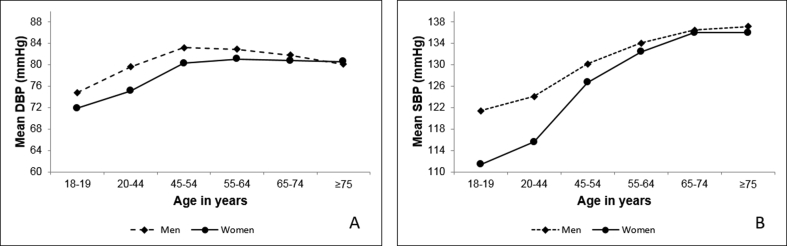
Both systolic BP (SBP) and diastolic BP (DBP) were higher among men than women across all age groups (Fig. 1). Mean SBP and DBP according to age group is given in Table 2. Mean SBP and DBP increased with increasing age in both genders till age 65 years after which it reached a plateau (Fig. 2A and B).
Table 2.
Mean systolic and diastolic blood pressure.
| Men | Women | Total | |
|---|---|---|---|
| Age (years) | 41.1 ± 15 (29–52) | 39.7 ± 14.7 (27–50) | 40.6 ± 14.9 (28–51) |
| Mean SBP (mmHg) | |||
| 18–19 | 121.4 ± 15 (110–130) | 111.4 ± 12.4 (102–120) | 117.5 ± 14.9 (110–127) |
| 20–44 | 124.1 ± 15.1 (114–130) | 115.6 ± 15.0 (108–122) | 121.2 ± 15.6 (110–130) |
| 45–54 | 130.2 ± 18.2 (120–140) | 126.7 ± 18.0 (113–140) | 129.0 ± 18.2 (119–140) |
| 55–64 | 134.1 ± 19.5 (120–144) | 132.4 ± 19.3 (120–140) | 133.6 ± 19.5 (120–143) |
| 65–74 | 136.5 ± 20.4 (120–150) | 136.0 ± 21.2 (120–149.5) | 136.4 ± 20.7 (120–150) |
| ≥75 | 137.2 ± 21.4 (120–150) | 136.0 ± 22.7 (120–148) | 136.8 ± 21.8 (120–150) |
| Total | 127.5 ± 17.5 (117–138) | 120.8 ± 18.2 (110–130) | 125.3 ± 18.0 (110–135) |
| Mean DBP (mmHg) | |||
| 18–19 | 74.8 ± 11 (69–80) | 71.9 ± 9.6 (66–80) | 73.7 ± 10.6 (68–80) |
| 20–44 | 79.6 ± 10.9 (70–86) | 75.1 ± 10.4 (70–80) | 78.1 ± 10.9 (70–84) |
| 45–54 | 83.2 ± 11.7 (77–90) | 80.3 ± 10.9 (70–90) | 82.2 ± 11.5 (75–90) |
| 55–64 | 82.9 ± 11.6 (76–90) | 81.1 ± 11.0 (73–90) | 82.4 ± 11.4 (76–90) |
| 65–74 | 81.8 ± 11.9 (74–90) | 80.8 ± 11.9 (70–90) | 81.5 ± 11.9 (72–90) |
| ≥75 | 80.1 ± 12.4 (70–90) | 80.6 ± 12.9 (70–90) | 80.2 ± 12.5 (70–90) |
| Total | 80.6 ± 11.4 (72–90) | 77.0 ± 11.0 (70–81) | 79.5 ± 11.4 (70–87) |
Data as mean ± standard deviation (25th to 75th percentile).
SBP: systolic blood pressure; DBP: diastolic blood pressure.
Fig. 2.
A. Mean systolic blood pressure (SBP) across age groups. B. Mean diastolic blood pressure (DBP) across age groups.
Among those not on any antihypertensive medication, only 28.6% of participants were found to have normal BP. Most participants were in the prehypertension stage (Table 3). 42.9% in the age group of 18–19 years had prehypertension.
Table 3.
Characteristics of Indian adults by blood pressure categories.
| SBP/DBP categories among those not taking Anti-HTN medications |
Taking Anti-HTN Medication (n = 23,213) | ||||
|---|---|---|---|---|---|
| Normal BP <120/<80 mmHg |
Prehypertension 120-139/80–89 mmHg |
Stage 1 HTN 140-159/90–99 mmHg |
Stage 2 HTN ≥160/≥100 mmHg | ||
| Age (years) | |||||
| 18–19 | 3,983 (45.0) | 3,797 (42.9) | 998 (11.3) | 73 (0.8) | 47 (0.2) |
| 20–44 | 31,018 (32.6) | 44,222 (46.5) | 18,290 (19.2) | 1,674 (1.8) | 4,587 (19.8) |
| 45–54 | 6,021 (20.8) | 12,625 (43.7) | 8,744 (30.2) | 1,526 (5.3) | 6,778 (29.2) |
| 55–64 | 2,689 (16.7) | 6,566 (40.7) | 5,461 (33.8) | 1,411 (8.8) | 6,957 (30.0) |
| 65–74 | 951 (15.2) | 2,454 (39.3) | 2,094 (33.6) | 740 (11.9) | 3,750 (16.2) |
| ≥75 | 307 (17.2) | 677 (44.8) | 584 (23.0) | 216 (3.6) | 3,750 (4.7) |
| Men | 23,690 (22.6) | 49,291 (47.0) | 27,644 (26.3) | 4,358 (4.2) | 15,442 (66.5) |
| Women | 21,280 (40.8) | 21,050 (40.4) | 8,527 (16.4) | 1,282 (2.5) | 7,771 (33.5) |
| Total | 44,970 (28.6) | 70,341 (44.8) | 55,850 (23.0) | 5,640 (3.6) | 23,213 (12.9) |
Data as n (percentage). SBP: systolic blood pressure; DBP: diastolic blood pressure; HTN: hypertension.
There were 12.9% (95% CI, 12.7–13.0) subjects on antihypertensive medications. Of total 55,370 participants with hypertension, 28,614 (51.4%) were aware of their disease status. Of those who were aware, 23,213 (81.1%) were on any antihypertensive medication. Of those on medication, only 13,545 (41.6%) had BP within the target (SBP<140 mmHg and DBP<90 mmHg).
4. Discussion
We report a high prevalence of hypertension among Indian adults, with almost one in three participants having hypertension. There are around 762 million Indians ≥18 years of age in India,16 which means there are currently 234 million adults with hypertension.
A similar prevalence of 26.5% was reported by a study using health survey–based nationwide blood pressure data (n = 1,320,555).19 Data from the National Family Health Survey-4 (NFHS-4) (n = 802,927) suggest a much lower prevalence of 11.3%.20 This could be due to the overrepresentation of women (87.2% in NFHS-4 vs. 34.3% in our study) and a younger study population (15–49 years) in NFHS-4.20 Anchala et al21 reported a similar prevalence of 29.8% in their meta-analysis where they pooled results from 142 hypertension prevalence studies from 1950 to 2013, representing around 0.3 million subjects.
Trends from the noncommunicable disease (NCD) Risk factor Collaboration (NCD-RisC) suggest that from 1975 to 2015, the mean systolic and diastolic blood pressure, as well as the prevalence of hypertension in the Indian population, has remained stable.22 Studies included in this analysis varied in their methodology and population selection. This is the first time that the NFHS has collected data on noncommunicable diseases such as obesity and hypertension. In subsequent years, this data will help better understand the epidemiological trends.
We found a high prevalence of hypertension among young adults (20–44 years). The prevalence in this age group is more than twice the prevalence in a similar population in the United States (22.4% vs. 10.5%, respectively).23 This increased prevalence of hypertension and prehypertension among young Indians is being increasingly reported.24, 25, 26 This is a disturbing trend because it puts an increasing number of young Indians at an increased risk of premature mortality due to cardiovascular causes.27 Currently, Indians experience cardiovascular event–related deaths almost a decade earlier than developed countries, with cardiovascular events responsible for 52% of all deaths in those aged <70 years in India, as compared with 23% in these countries.28
The increasing trend in both systolic and diastolic BP till the fifth and the sixth decade followed by a decline in the diastolic BP observed in our study suggests that isolated systolic hypertension is the predominant form of hypertension in the elderly.29,30
We observed a higher proportion of participants who were aware, on treatment, and had controlled BP than was reported by Roy et al (51.0% vs. 38.7%, 88.0% vs. 32.3%, and 41.0% vs. 12.8% respectively).26 A probable reason could be that the population we surveyed was mostly working class and there could be a behavioral bias among those getting their BP measured, with those more educated, aware, and concerned about their health status attending the camp. The awareness of high blood pressure was, however, much lower than that reported in similar studies from Canada (83%), the USA (81%), or England (65%).31
It is estimated that around 17.6% of patients with hypertension globally live in India, which suggests an expected large increase in cardiovascular diseases burden in the near future.26,32,33 This mandates early detection and treatment, as adequate BP control can avert almost a third of all cardiovascular-related mortality.34
Homogenous data collection, real-time feeding of data in the online system, and independent review of all readings are the strengths of this study. For the first time, we report the genderwise prevalence of hypertension across age groups. There are, however, some limitations. The study may have a selection bias as the healthy volunteers usually turn up for checkups. However, the effect of this bias is likely to be small given the large sample size.
5. Conclusion
There is a very high prevalence of hypertension among Indian adults, across all age groups. In addition, there is poor awareness, treatment, and control among those with hypertension.
| What is already known? |
|
| What does this study add? |
|
Conflicts of interest
All authors have none to declare.
Acknowledgments
The investigators would like to thank Omron Healthcare India Pvt. Ltd. for providing blood pressure apparatus, Torrent Pharmaceuticals Ltd., USV Pvt. Ltd. and Zydus Pharmaceuticals Ltd. for partial financial support. RP Singh of Zydus Pharmaceuticals Ltd. provided logistic support.
Contributor Information
Sivasubramanian Ramakrishnan, Email: drramaaiims@gmail.com.
CSI-Great India BP Campaign Investigators:
J. Shivkumar Rao, B.P. Singh, B.B. Bharti, A.K. Sinha, Kartik Gupta, Sivasubramanian Ramakrishnan, Sudha Bhushan, Sunil K. Verma, Balram Bhargava, Ambuj Roy, Sandeep Bansal, Sanjay Sood, H.S. Isser, Neeraj Pandit, Ranjit K. Nath, Sanjay Tyagi, Vijay Trehan, Mohit D. Gupta, M.P. Girish, Ramandeep Ahuja, S.C. Manchanda, Arun Mohanty, Peeyush Jain, Sameer Shrivastava, I.P.S. Kalra, B.S. Sarang, H.S. Ratti, G. Bala Sahib, Rakesh Gupta, S.K. Agarwal, Amit, K.C. Goswami, V.K. Bahl, H.K. Chopra, Ashok Seth, Geevar Zachariah, P.P. Mohanan, K. Venugopal, George Koshy, Tiny Nair, N. Shyam, Anil Roby, Raju George, Sudhaya Kumar, Abdul Kader, Mathew Abraham, Sunitha Viswanathan, A. Jabir, Jaideep Menon, Govindan Unni, Cibu Mathew, PB Jayagopal Sajeev, P.K. Ashokan, Asharaf, Subroto Mandal, A.K. Pancholia, Neil Bardolei, A.K. Gupta, Neil Bardolei, Rupam Das, Dinesh Aggarwal, Amit Malviya, S.N. Routray, S.S. Mishra, Syed Manzor Ali, Parag Barward, Navreet Singh, Yashbir S. Tomar, Davinder Chaddha, Sameer Dani, Chirayu Vyas, Kinjal Bhatt, Shrenik Doshi, G.S. Wander, Satish Gupta, Chandra Bhan Meena, Santosh Sateesh, Nagendra Boopathy Senguttuvan, Geetha Subramanyam Subramanyam, Ajit Mullasari Muruganandam, Rishi Sethi, Varun Narain, R.K. Saran, Dharmendra Jain, Praveen Jain, Sudeep Kumar, P.K. Goel, Debabatra Roy, Sibananda Datta, Kajal Ganguly, M.K. Das, Soumitra Kumar, Sarat Chandra Amal Banerjee, Santanu Guha, and P.K. Deb
Appendix.
Authors of the CSI-Great India BP campaign
Andhra Pradesh: Shivkumar Rao J,
Bihar: B P Singh, B B Bharti, A K Sinha,
Delhi: Kartik Gupta, Sivasubramanian Ramakrishnan, Sudha Bhushan, Sunil K Verma, Balram Bhargava, Ambuj Roy, Sandeep Bansal, Sanjay Sood, H S Isser, Neeraj Pandit, Ranjit K Nath, Sanjay Tyagi, Vijay Trehan, Mohit D Gupta, Girish MP, Ramandeep Ahuja, S C Manchanda, Arun Mohanty, Peeyush Jain, Sameer Shrivastava, IPS Kalra, B.S. Sarang, H.S. Ratti, G. Bala Sahib, Rakesh Gupta, S K Agarwal, Amit, KC Goswami, VK Bahl, HK Chopra, and Ashok Seth
Kerala: Geevar Zachariah, PP Mohanan, K Venugopal, George Koshy, Tiny Nair, Shyam N, Anil Roby, Raju George, Sudhaya Kumar, Abdul Kader, Mathew Abraham, Sunitha Viswanathan, Jabir A, Jaideep Menon, Govindan Unni, Cibu Mathew, PB Jayagopal, Sajeev, Ashokan PK, Asharaf
Madhya Pradesh: Subroto Mandal, A K Pancholia
North-east India: Neil Bardolei, A. K. Gupta, Neil Bardolei, Rupam Das, Dinesh Aggarwal, Amit Malviya
Orissa - SN Routray, SS Mishra,
Others - Syed Manzor Ali, Parag Barward, Navreet Singh, Yashbir S Tomar, Davinder Chaddha, Sameer Dani, Chirayu Vyas, Kinjal Bhatt, Shrenik Doshi
Punjab: G S Wander
Rajasthan: Satish Gupta, Chandra Bhan Meena
Tamil Nadu: Santosh Sateesh, Nagendra Boopathy Senguttuvan, Geetha Subramanyam, Subramanyam, Ajit Mullasari, Muruganandam,
Uttar Pradesh: Rishi Sethi, Varun Narain, RK Saran, Dharmendra Jain, Praveen Jain, Sudeep Kumar, P K Goel
West Bengal and Cardiology Society of India: Debabatra Roy, Sibananda Datta, Kajal Ganguly, MK Das, Soumitra Kumar, Sarat Chandra Amal Banerjee, Santanu Guha, PK Deb,
References
- 1.WHO | Cardiovascular Diseases (CVDs). WHO. http://www.who.int/mediacentre/factsheets/fs317/en/. Accessed February 21, 2018.
- 2.Rapsomaniki E., Timmis A., George J. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1·25 million people. Lancet Lond Engl. 2014;383(9932):1899–1911. doi: 10.1016/S0140-6736(14)60685-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stokes J., Kannel W.B., Wolf P.A., D'Agostino R.B., Cupples L.A. Blood pressure as a risk factor for cardiovascular disease. The Framingham Study--30 years of follow-up. Hypertens Dallas Tex 1979. 1989;13(5 Suppl):I13–I18. doi: 10.1161/01.hyp.13.5_suppl.i13. [DOI] [PubMed] [Google Scholar]
- 4.Klag M.J., Whelton P.K., Randall B.L. Blood pressure and end-stage renal disease in men. N Engl J Med. 1996;334(1):13–18. doi: 10.1056/NEJM199601043340103. [DOI] [PubMed] [Google Scholar]
- 5.Rodgers A., Lawes C., MacMahon S. Reducing the global burden of blood pressure-related cardiovascular disease. J Hypertens Suppl Off J Int Soc Hypertens. 2000;18(1):S3–S6. [PubMed] [Google Scholar]
- 6.Steel N. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1151–1210. doi: 10.1016/S0140-6736(17)32152-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pandey R.M., Gupta R., Misra A. Determinants of urban-rural differences in cardiovascular risk factors in middle-aged women in India: a cross-sectional study. Int J Cardiol. 2013;163(2):157–162. doi: 10.1016/j.ijcard.2011.06.008. [DOI] [PubMed] [Google Scholar]
- 8.Gupta R., Pandey R.M., Misra A. High prevalence and low awareness, treatment and control of hypertension in Asian Indian women. J Hum Hypertens. 2012;26(10):585–593. doi: 10.1038/jhh.2011.79. [DOI] [PubMed] [Google Scholar]
- 9.Joshi S.R., Saboo B., Vadivale M. Prevalence of diagnosed and undiagnosed diabetes and hypertension in India--results from the Screening India's Twin Epidemic (SITE) study. Diabetes Technol Ther. 2012;14(1):8–15. doi: 10.1089/dia.2011.0243. [DOI] [PubMed] [Google Scholar]
- 10.Singh R.B., Fedacko J., Pella D. Prevalence and risk factors for prehypertension and hypertension in five Indian cities. Acta Cardiol. 2011;66(1):29–37. doi: 10.1080/ac.66.1.2064964. [DOI] [PubMed] [Google Scholar]
- 11.Chinnakali P., Mohan B., Upadhyay R.P., Singh A.K., Srivastava R., Yadav K. Hypertension in the elderly: prevalence and health seeking behavior. N Am J Med Sci. 2012;4(11):558–562. doi: 10.4103/1947-2714.103314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tripathy J.P., Thakur J.S., Jeet G., Chawla S., Jain S. Alarmingly high prevalence of hypertension and pre-hypertension in North India-results from a large cross-sectional STEPS survey. PLoS One. 2017;12(12) doi: 10.1371/journal.pone.0188619. e0188619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bhansali A., Dhandania V.K., Deepa M. Prevalence of and risk factors for hypertension in urban and rural India: the ICMR-INDIAB study. J Hum Hypertens. 2015;29(3):204–209. doi: 10.1038/jhh.2014.57. [DOI] [PubMed] [Google Scholar]
- 14.Kearney P.M., Whelton M., Reynolds K., Muntner P., Whelton P.K., He J. Global burden of hypertension: analysis of worldwide data. The lancet. 2005;365(9455):217–223. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 15.Chobanian A.V., Bakris G.L., Black H.R. The Seventh report of the Joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. J Am Med Assoc. 2003;289(19):2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 16.Census of India Website : Office of the Registrar General & Census Commissioner, India. http://www.censusindia.gov.in/2011census/population_enumeration.html. Accessed February 22, 2018.
- 17.Ahmad O.B., Boschi-Pinto C., Lopez A.D., Murray C.J., Lozano R., Inoue M. Vol. 9. Geneva World Health Organ; 2001. Age Standardization of Rates: a New WHO Standard. [Google Scholar]
- 18.Gee M.E., Campbell N., Sarrafzadegan N. Standards for the uniform reporting of hypertension in adults using population survey data: recommendations from the world hypertension League expert committee. J Clin Hypertens. 2014;16(11):773–781. doi: 10.1111/jch.12387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Geldsetzer P., Manne-Goehler J., Theilmann M. Diabetes and hypertension in India: a nationally representative study of 1.3 million adults. JAMA Intern Med. January. 2018 doi: 10.1001/jamainternmed.2017.8094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.National Family Health Survey. http://rchiips.org/nfhs/abt.html. Accessed December 16, 2018.
- 21.Anchala R., Kannuri N.K., Pant H. Hypertension in India: a systematic review and meta-analysis of prevalence, awareness, and control of hypertension. J Hypertens. 2014;32(6):1170–1177. doi: 10.1097/HJH.0000000000000146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Collaboration NCDRF Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19.1 million participants. Lancet. 2017;389(10064):37–55. doi: 10.1016/S0140-6736(16)31919-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Muntner P., Carey R.M., Gidding S. Potential US population impact of the 2017 ACC/AHA high blood pressure guideline. Circulation. 2018;137(2):109–118. doi: 10.1161/CIRCULATIONAHA.117.032582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zafar K.S., Ram V.S., Kumar M. The prevalence of hypertension among young adults in a rural population of North India. Int J Res Med Sci. 2017;5(11):4869. [Google Scholar]
- 25.Kini S., Kamath V.G., Kulkarni M.M., Kamath A., Shivalli S. Pre-hypertension among young adults (20–30 Years) in coastal villages of udupi district in southern India: an alarming scenario. PLoS One. 2016;11(4) doi: 10.1371/journal.pone.0154538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Roy A., Praveen P.A., Amarchand R. Changes in hypertension prevalence, awareness, treatment and control rates over 20 years in National Capital Region of India: results from a repeat cross-sectional study. BMJ Open. 2017;7(7) doi: 10.1136/bmjopen-2016-015639. e015639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gupta R., Xavier D. Hypertension: the most important non communicable disease risk factor in India. Indian Heart J. 2018 doi: 10.1016/j.ihj.2018.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lozano R., Naghavi M., Foreman K. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. The Lancet. 2012;380(9859):2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liu X., Rodriguez C.J., Wang K. Prevalence and trends of isolated systolic hypertension among untreated adults in the United States. J Am Soc Hypertens JASH. 2015;9(3):197–205. doi: 10.1016/j.jash.2015.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Duprez D.A. Systolic hypertension in the elderly: addressing an unmet need. Am J Med. 2008;121(3):179–184. doi: 10.1016/j.amjmed.2007.10.027. e3. [DOI] [PubMed] [Google Scholar]
- 31.Joffres M., Falaschetti E., Gillespie C. Hypertension prevalence, awareness, treatment and control in national surveys from England, the USA and Canada, and correlation with stroke and ischaemic heart disease mortality: a cross-sectional study. BMJ Open. 2013;3(8) doi: 10.1136/bmjopen-2013-003423. e003423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Danaei G., Finucane M.M., Lin J.K. National, regional, and global trends in systolic blood pressure since 1980: systematic analysis of health examination surveys and epidemiological studies with 786 country-years and 5·4 million participants. The Lancet. 2011;377(9765):568–577. doi: 10.1016/S0140-6736(10)62036-3. [DOI] [PubMed] [Google Scholar]
- 33.Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. The Lancet. 2002;360(9349):1903–1913. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 34.Sacco R.L., Roth G.A., Reddy K.S. The heart of 25 by 25: achieving the goal of reducing global and regional premature deaths from cardiovascular diseases and stroke: a modeling study from the American heart association and world heart federation. Circulation. 2016;133(23):e674–e690. doi: 10.1161/CIR.0000000000000395. [DOI] [PubMed] [Google Scholar]