Abstract
Female sex workers (FSWs) experience syndemic factors (e.g., polydrug use, hazardous alcohol consumption, client-perpetrated violence, depression, and sexually transmitted infections) that often heighten vulnerability to HIV and limit healthcare utilization. We hypothesized that syndemic factors will limit FSWs’ uptake of pre-exposure prophylaxis (PrEP). From 2016-2017, 295 HIV-negative FSWs were enrolled in a behavioral HIV prevention trial in Tijuana and Ciudad Juarez, Mexico, underwent STI testing, and completed surveys on syndemic factors and perceived barriers to PrEP use. Syndemic scores (0-5) were calculated by summing syndemic factors. Latent class analysis (LCA) was used to identify homogeneous classes with respect to perceived barriers to PrEP use. We identified four classes: (1) perceived healthcare access barriers (8.3%), (2) perceived financial barriers (18.7%), (3) high level of perceived barriers (19.9%), and (4) low level of perceived barriers (53.0%) to PrEP use. Those experiencing three (adjusted odds ratio [aOR]=3.63, 95% confidence interval [CI]=1.24-10.67) and four or five (aOR=6.30, 95% CI=1.70-23.35) syndemic factors had a higher odds of membership in the class characterized by a high level of perceived barriers than in the class characterized by a low level of perceived barriers. Addressing syndemic factors may maximize PrEP’s impact among FSWs along Mexico’s northern border.
Keywords: HIV, pre-exposure prophylaxis, latent class analysis, syndemic theory, female sex workers, Mexico
Introduction
Female sex workers (FSWs) are disproportionately affected by HIV in low- and middle-income countries (LMICs) (Baral et al., 2012). Marginalized women, including FSWs, often experience syndemic or co-occurring substance use, violence, and mental illness (Meyer, Springer, & Altice, 2011), which can interact synergistically to heighten HIV risk (Singer, 2000). Violence, for instance, can increase HIV risk by fostering power differentials that limit women’s ability to negotiate condom use (Gielen et al., 2007; Maman, Campbell, Sweat, & Gielen, 2000). Substance-involved women often experience elevated rates of intimate partner violence (IPV) (El-Bassel, Gilbert, Wu, Go, & Hill, 2005; El-Bassel, Terlikbaeva, & Pinkham, 2010) and women with a history of IPV are more likely to experience depression (Illangasekare, Burke, Chander, & Gielen, 2013). Further, among FSWs, increased vulnerability to HIV has been linked to substance use and experiences of client-perpetrated violence (CPV) (Maher et al., 2011; Shannon et al., 2009).
Female-controlled HIV prevention strategies, such as pre-exposure prophylaxis (PrEP) (Baeten et al., 2012; Choopanya et al., 2013; Grant et al., 2010; Thigpen et al., 2012), that empower women to take control of their sexual health may be particularly beneficial among syndemic-affected women, including FSWs. However, given that healthcare is often less accessible to these women (Lichtenstein, 2006) and syndemic factors have been linked to decreased HIV care engagement among substance-involved women (Mizuno et al., 2015), PrEP uptake may be limited among syndemic-affected FSWs.
Several barriers to PrEP use among high-risk women, including FSWs, have been identified such as cost, stigma, medical mistrust, interpersonal dynamics (e.g., male partners disapproving of their partners’ PrEP use) (Auerbach, Kinsky, Brown, & Charles, 2015; Goparaju et al., 2017; van der Straten, Stadler, Montgomery, et al., 2014), and adherence challenges due to substance use (Galea et al., 2011; Van der Elst et al., 2013). However, little is known about the heterogeneity in patterns of perceived barriers to PrEP use among FSWs or which patterns, if addressed, might maximize PrEP use among syndemic-affected FSWs’ in LMICs like Mexico.
Tijuana and Ciudad Juarez are economically disadvantaged Mexico-United States (US) border cities situated along major drug trafficking routes with quasi-legal sex trade industries (Bucardo et al., 2005; Strathdee et al., 2012). In Tijuana, FSWs are required to have a permit and undergo routine HIV screening. However, many FSWs who use illicit drugs and practice street-based sex work are systematically excluded from such programs because they are less accessible to the local authorities that enforce these regulations (Gaines et al., 2013). HIV prevalence among FSWs in these cities is approximately 30 times higher than Mexico’s national HIV prevalence (6% vs. 0.2%), with a higher HIV burden among FSWs who inject drugs (12.3%) (Patterson et al., 2008; Secretaria de Salud, 2005; Strathdee et al., 2008). Overlapping experiences of violence, substance use, and depression among FSWs in this region exacerbate HIV risk (Ulibarri et al., 2013; Ulibarri et al., 2014; Ulibarri et al., 2011), and may also limit their access to healthcare (Lichtenstein, 2006; Mizuno et al., 2015), which could similarly inhibit their future PrEP uptake.
The purpose of this study was to help inform interventions to maximize PrEP’s impact among syndemic-affected FSWs along Mexico’s northern border and other similar LMICs. We used latent class analysis (LCA) (Goodman, 1974a, 1974b; Lazarsfeld & Henry, 1968) to identify classes of FSWs based on their patterns of perceived barriers to PrEP use. To evaluate our hypothesis that syndemic-affected FSWs face unique barriers to PrEP use, we examined whether class membership was associated with co-occurring hazardous alcohol consumption, polydrug use, depression, CPV, and sexually transmitted infections (STIs).
Methods
Study Design and Population.
Proyecto PrEParado (Project PrEPared) was embedded in a HIV prevention trial (Trial Registration: NCT02447484) conducted among HIV-negative FSWs in Tijuana and Ciudad Juarez examining the efficacy of a text messaging intervention to maintain the impact of a sexual risk reduction counseling session (Strathdee et al., 2013; Vera et al., 2012). As previously described (Patterson et al., 2018; Pines et al., 2019; Pines et al., 2018), 602 FSWs (302 Tijuana; 300 Ciudad Juarez) were recruited into the trial (March 2016-January 2017) from known sex work locations (e.g., bars, street corners). Eligibility criteria included: cisgender female, ≥18 years-old, HIV-negative, self-identification as a sex worker, exchanging sex for money, drugs or other goods (past month), condom-unprotected vaginal/anal sex with a male client (past month), willingness to receive treatment if STI-positive, and cellular telephone ownership. Proyecto PrEParado was a cross-sectional study (July 2016-January 2017) conducted among 313 (163 Tijuana; 150 Ciudad Juarez) participants when they returned for their STI test results within approximately one month post-enrollment (Pines et al., 2019).
Study Procedures.
At enrollment, participants provided written informed consent and underwent HIV/STI testing, including (1) rapid HIV: Advance Quality Anti-HIV 1&2 (InTec Products, Inc); (2) rapid syphilis: Advance Quality Anti-TP (InTec Products, Inc); (3) confirmatory HIV: Architect HIV Ag/Ab Combo, Abbott, Geenius™ HIV ½ Supplemental Assay (Bio-Rad); (4) confirmatory syphilis: BD Macro-Vue™ rapid plasma regain (RPR) (Becton, Dickinson and Company) and Architect Syphilis Treponemal assay (Abbott); and (5) chlamydia and gonorrhea: Aptima Combo 2@ Assay (Hologic). Participants received rapid HIV/STI test results, and then completed the baseline survey, participated in the sexual risk reduction counseling session, and were randomized (1:1) to the intervention or control group. Participants returned within approximately one month to receive their confirmatory HIV/syphilis test and STI test results. All STI-positive participants were offered free treatment, and HIV-positive participants were referred to local clinics for free HIV care. At that visit, participants also completed the Proyecto PrEParado survey. All surveys were interviewer-administered using computer-assisted personal-interviewing. Study procedures were approved by ethics committees at the University of California, San Diego, Xochicalco University in Tijuana, and SADEC-FEMAP in Ciudad Juarez.
Data Collection
Baseline Survey.
Data were collected on socio-demographics: age, highest level of education, and average monthly income in Mexican pesos. Moderate or severe depression was assessed via the 21-item Beck Depression Inventory (Cronbach’s alpha=0.93) and defined as a score of ≥20 (Beck, Steer, & Carbin, 1988; Beck, Ward, Mendelson, Mock, & Erbaugh, 1961). Alcohol use in the past year was measured using the 10-item Alcohol Use Disorders Identification Test (AUDIT), with AUDIT scores ≥8 defined as hazardous alcohol consumption (Saunders, Aasland, Babor, de la Fuente, & Grant, 1993). Data were collected on illicit drug use in the past month (heroin; methamphetamine; cocaine; inhalants; ecstasy; tranquilizers; barbiturates), and polydrug use was defined as using two or more substances. CPV was defined as ever experiencing physical (“Have you ever been physically abused by a client?”) or sexual (“Since you became a sex worker, how many different times have you been forced or coerced into having sex against your will with a client?”) violence from clients.
Proyecto PrEParado Survey.
First, participants received information on PrEP products in development (i.e., potential effectiveness, side effects, and the importance of adherence and routine screening for HIV/STIs while using PrEP). Next, participants indicated via 5-point Likert scale responses (strongly disagree to strongly agree) the extent to which they agree with 30 statements about why they would not use PrEP. Statements were developed based on previous research (Doggett et al., 2015; Galea et al., 2011; Mack et al., 2014; Minnis et al., 2013; Robertson et al., 2013; Syvertsen et al., 2014; Van der Elst et al., 2013; van der Straten, Stadler, Luecke, et al., 2014; van der Straten, Stadler, Montgomery, et al., 2014; Ye et al., 2014) and assessed perceived barriers to PrEP use across five domains: (1) product attributes, (2) individual perceptions and capacity, (3) interpersonal dynamics, (4) healthcare access, and (5) stigma (Supplemental Table 1).
Statistical Analysis
To ensure that baseline and Proyecto PrEParado data were collected within a reasonably close time frame to facilitate their combined analysis, analyses were restricted to participants who completed their Proyecto PrEParado survey within 3 months of enrollment (N=295).
Descriptive Analysis.
Using SAS 9.3 (SAS Institute, Inc., Cary, NC), we examined the prevalence of perceived barriers to PrEP use and syndemic factors (hazardous alcohol consumption, polydrug use, depression, CPV, STIs). We calculated a syndemic score (0-5) by summing the number of factors reported. Then, we assessed the co-occurrence of syndemic factors using bivariate logistic regression.
Latent Class Analysis.
We conducted an LCA using Latent Gold v5.1 (Vermunt & Magidson, 2016) to identify homogeneous subgroups of FSWs with respect to patterns of perceived barriers to PrEP use. LCA examines response patterns from observed variables and probabilistically assigns individuals with similar patterns to homogeneous classes that represent categories of a latent variable (Goodman, 1974a, 1974b; Lazarsfeld & Henry, 1968). Indicators measuring barriers to PrEP use were dichotomized (0=strongly disagree, disagree, or neither agree nor disagree; 1=agree or strongly agree). Using these 30 binary indicators, we fit a series of models with one to five classes. For each model, we used 100 random starting values to facilitate the identification of a maximum likelihood (ML) solution (Vermunt & Magidson, 2016). Due to the sparseness of our data (230 possible response patterns), we were unable to identify an ML solution for models with more than two classes.
To facilitate the identification of an ML solution, we reduced the amount of unknown information (Collins & Lanza, 2010) by considering only 11 indicators in our LCA (Supplemental Material; Supplemental Table 1) and again fit a series of models with one to five classes, 100 random starting values, and Bayesian priors (1.0) to stabilize parameter estimation (Vermunt & Magidson, 2016). To select our final model, we considered: (1) fit statistics (prioritizing models with lower values for Akaike’s information criteria [AIC] and sample size-adjusted Bayesian information criteria [BIC]), (2) entropy as a measure of classification certainty, (3) class separation (uniqueness of response patterns across classes), (4) homogeneity within classes (similarity in response patterns), and (5) the meaningfulness of the identified classes (Collins & Lanza, 2010; Vermunt & Magidson, 2016). To examine the extent to which the local independence assumption underlying LCA might be violated, we examined bivariate residuals (BVR) and considered models that allow for local dependence between pairs of indicators with statistically significant relationships (i.e., BVR>3.84) (Vermunt & Magidson, 2016; Hagenaars, 1988).
Next, we examined the association between class membership and our covariates of interest (i.e., syndemic factors and syndemic score) using Vermunt’s bias-adjusted three-step approach (Vermunt, 2010). After selecting our final model (Step 1), we used the estimated posterior probabilities of class membership to assign participants to one of the four classes using the proportional assignment method (Step 2). Then, we used multinomial logistic regression to model class membership as a function of our covariates of interest (Step 3) using Vermunt’s ML method to correct for classification errors in Step 2 and a robust variance estimator to obtain unbiased parameter estimates and standard errors, respectively (Bakk, Oberski, & Vermunt, 2014; Vermunt, 2010). We ran seven separate multinomial logistic regression models: (1-5) each syndemic factor, (6) syndemic score as a nominal variable (to examine the relationship between the number of syndemic factors and class membership), and (7) syndemic score as an ordinal variable (to detect a linear trend in the relationship between the number of syndemic factors and class membership). Each model was adjusted for age and education.
Results
Syndemic Factors.
There was a high prevalence of hazardous alcohol consumption in the past year (46.1%), lifetime CPV (36.3%), depression (35.9%), polydrug use in the past month (28.8%), and STIs (19.0%) (Table 1). One-fifth of the sample did not have any of these factors (21.4%), while 27.5% had one, 25.1% had two, 17.3% had three, 7.5% had four, and 1.4% had five (median syndemic score=2; Interquartile range [IQR]=1-3). Six of ten possible distinct associations among syndemic factors were associated with one another, suggesting a moderate level of clustering (Table 2).
Table 1.
Sociodemographics and syndemic factors among FSWs in Tijuana and Ciudad Juarez, Mexico (N=295).
| n (%) | |
|---|---|
| Sociodemographics | |
| Tijuana study site | 145 (49.2) |
| Completed secondary school | 130 (44.1) |
| Average monthly income ≥3,500 pesos (~172 USD) | 206 (69.8) |
| Median age in years (IQR) | 38 (30, 46) |
| Age in years | |
| 18 - 29 | 71 (24.1) |
| 30 - 39 | 92 (31.2) |
| ≥40 | 132 (44.8) |
| Syndemic Factors | |
| Hazardous alcohol consumption (past year)a | 136 (46.1) |
| Lifetime client perpetrated violenceb | 107 (36.3) |
| Depressionc | 106 (35.9) |
| Polydrug use (past month)d | 85 (28.8) |
| Tested STI-positivee | 56 (19.0) |
| Chlamydia | 41 (13.9) |
| Gonorrhea | 21 (7.1) |
| Active syphilis (antibody titers ≥1:8) | 10 (3.4) |
| Median syndemic score (IQR)f | 2 (1, 3) |
| Number of syndemic factors | |
| 0 | 63 (21.4) |
| 1 | 81 (27.5) |
| 2 | 74 (25.1) |
| 3 | 51 (17.3) |
| 4 | 22 (7.5) |
| 5 | 4 (1.4) |
Percentages may not sum to 100 due to rounding or omission of one category for binary variables.
Abbreviations: FSW=female sex worker; IQR=interquartile range; STI=sexually transmitted infection; USD=United States dollars.
Alcohol Use Disorder Identification Test score ≥8.
Lifetime experience of physical abuse or sexual violence perpetrated by a client.
Moderate or severe depression defined as a score ≥20 on the Beck Depression Inventory II (BDI-II).
Use of ≥2 illicit drugs (heroin; methamphetamine; cocaine; inhalants; ecstasy; tranquilizers; barbiturates) in the past month.
Tested positive for chlamydia, gonorrhea, or active syphilis.
Syndemic score = sum of syndemic factors (range: 0 to 5).
Table 2.
Bivariate associations between syndemic factors among FSWs in Tijuana and Ciudad Juarez, Mexico (N=295).
| Hazardous alcohol consumption (past year) OR (95% CI) |
Polydrug use (past month) OR (95% CI) |
Depression OR (95% CI) |
Lifetime client perpetrated violence OR (95% CI) |
|
|---|---|---|---|---|
| Hazardous alcohol consumption (past year)a | - | - | - | - |
| Polydrug use (past month)b | 1.38 (0.83, 2.28) | - | - | - |
| Depressionc | 1.62 (1.00, 2.62) | 2.75 (1.63, 4.62) | - | - |
| Lifetime client perpetrated violenced | 1.67 (1.04, 2.69) | 2.18 (1.30, 3.65) | 2.07 (1.26, 3.38) | - |
| Tested STI-positivee | 1.33 (0.74, 2.37) | 1.64 (0.89, 3.03) | 2.97 (1.64, 5.39) | 1.07 (0.59, 1.95) |
Abbreviations: CI=confidence interval; FSW=female sex worker; OR=odds ratio; STI=sexually transmitted infection.
Alcohol Use Disorder Identification Test score ≥8.
Use of ≥2 illicit drugs (heroin; methamphetamine; cocaine; inhalants; ecstasy; tranquilizers; barbiturates; cocaine and heroin together; methamphetamine and heroin together) in the past month.
Moderate or severe depression defined as a score ≥20 on the Beck Depression Inventory II (BDI-II).
Lifetime experience of physical abuse or sexual violence perpetrated by a client.
Tested positive for chlamydia, gonorrhea, or active syphilis.
Perceived Barriers to PrEP Use.
The most common perceived barrier was “I do not have enough money to pay for PrEP” (30.2%), followed by “PrEP does not provide complete protection against HIV”, “I am worried I will lose clients if I use PrEP because they will assume I am HIV+”, and “Accessing PrEP and regular HIV testing will be more difficult since healthcare clinics have limited hours of operation” (23.4%) (Supplemental Table 1).
Classes of FSWs.
Based on fit statistics (Table 3), the five-class model appeared to fit the data best (i.e., lowest AIC and BIC values). However, BVRs from all models suggested a violation of the local independence assumption (Supplemental Table 2). To account for the relationships between indicators with BVRs >3.84 in the three-, four-, and five-class models, we relaxed the local independence assumption by re-fitting these models with direct effects between these indicators. AIC and BIC values associated with these three models improved, but their entropy values decreased slightly. Although the three-class model with direct effects had the lowest AIC and BIC values, it also had the lowest entropy. After considering class separation, homogeneity within classes, and the meaningfulness of the identified classes for the four- and five-class models with direct effects (Supplemental Table 3), which had similar AIC, BIC, and entropy values, we selected the four-class model with direct effects as our final model.
Table 3.
Model fit information across LCA models with one to five classes using 11 binary indicators (N=295).
| LCA Model | Log Likelihood | AIC | Adjusted-BIC | Entropy |
|---|---|---|---|---|
| 1-class | −1683.12 | 3388.24 | 3393.92 | 1.00 |
| 2-class | −1276.56 | 2599.12 | 2610.98 | 0.92 |
| 3-class | −1233.31 | 2536.61 | 2554.66 | 0.86 |
| 4-class | −1197.85 | 2489.70 | 2513.94 | 0.86 |
| 5-class | −1174.90 | 2467.80 | 2498.23 | 0.87 |
| 3-class with DE | −1174.61 | 2435.22 | 2457.39 | 0.77 |
| 4-class with DE | −1183.52 | 2465.03 | 2490.30 | 0.85 |
| 5-class with DE | −1168.74 | 2457.48 | 2488.42 | 0.85 |
Abbreviations: AIC=Akaike’s information criteria; BIC=Bayesian information criteria; DE=direct effects; LCA=latent class analysis.
After examining item-response probabilities for each class in our final model, we labeled the classes: low level of perceived barriers to PrEP use (53.0%), high level of perceived barriers to PrEP use (19.9%), perceived financial barriers to PrEP use (18.7%), and perceived healthcare access barriers to PrEP use (8.3%) (Figure 1). FSWs in the low level of perceived barriers class had a low probability of endorsing any of the barriers and served as the reference group in subsequent analyses.
Figure 1. Item-response probabilities across classes of FSWs in Tijuana and Ciudad Juarez, Mexico with varying patterns of perceived barriers to PrEP use as identified via latent class analysis (N=295).
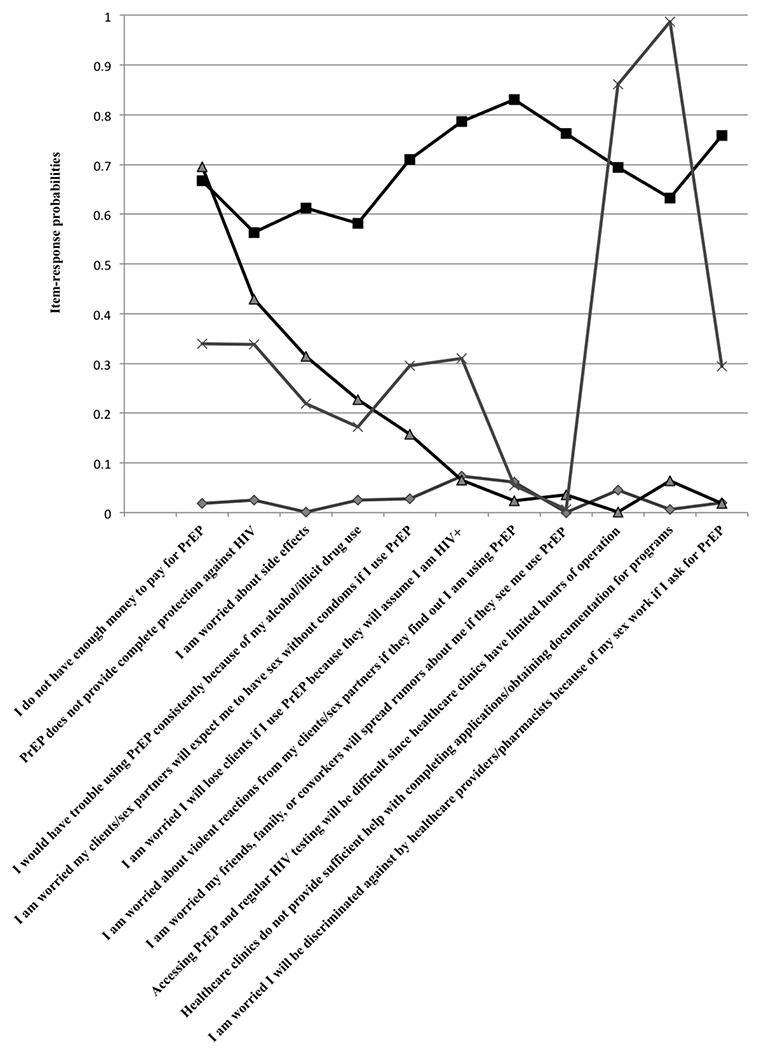
Identified classes consist of FSWs with a low-level of perceived barriers (diamond; 53.0%), a high level of perceived barriers (square; 19.9%), perceived financial barriers (triangle; 18.7%), and perceived health care access barriers (cross; 8.3%). Abbreviations: FSW=female sex workers; PrEP=pre-exposure prophylaxis.
Syndemic Factors and Class Membership.
Compared to membership in the low level of perceived barriers class, the odds of membership in the high level of perceived barriers class were higher for those with three (aOR=3.63, 95% CI=1.24-10.67) and four or five (aOR=6.30, 95% CI=1.70-23.35) syndemic factors (Table 4). There was also a linear trend in the relationship between the number of syndemic factors and membership in that class (aOR=1.46, 95% CI=1.13-1.89), and a marginally non-significant trend for membership in the classes characterized by financial (aOR=1.28, 95% CI=0.96-1.71) and healthcare access (aOR=1.43, 95% CI=0.94-2.19) barriers. The odds of membership in the financial and high level of perceived barriers classes were higher for those with depression (aOR=3.77, 95% CI=1.74-8.18 and aOR=3.71, 95% CI=1.90-7.26, respectively) and STIs (aOR=4.18, 95% CI=1.67-10.47 and aOR=3.10, 95% CI=1.35-7.10, respectively). Those who reported polydrug use had a higher odds of membership in the perceived healthcare access barriers class (aOR=2.70, 95% CI=1.04-7.04).
Table 4.
Adjusted associations between syndemic factors and syndemic scores and class membership among FSWs in Tijuana and Ciudad Juarez, Mexico (N=295).
| Class 2 | Class 3 | Class 4 | |
|---|---|---|---|
|
High Level of Perceived Barriers to PrEP Use AOR (95% CI)a |
Perceived Financial Barriers to PrEP Use AOR (95% CI)a |
Perceived Healthcare Access Barriers to PrEP Use AOR (95% CI)a |
|
| Syndemic factors | |||
| Hazardous alcohol consumption (past year)b | 1.07 (0.57, 2.01) | 0.61 (0.29, 1.27) | 1.19 (0.46, 3.05) |
| Polydrug use (past month)c | 1.52 (0.76, 3.04) | 1.54 (0.70, 3.43) | 2.70 (1.04, 7.04) |
| Depressiond | 3.71 (1.90, 7.26) | 3.77 (1.74, 8.18) | 2.02 (0.69, 5.87) |
| Lifetime client perpetrated violencee | 1.21 (0.64, 2.29) | 0.66 (0.30, 1.48) | 1.55 (0.59, 4.05) |
| Tested STI-positivef | 3.10 (1.35, 7.10) | 4.18 (1.67, 10.47) | 1.57 (0.33, 7.40) |
| Nominal syndemic score | |||
| 0 syndemic conditions | Ref | Ref | Ref |
| 1 | 1.95 (0.72, 5.32) | 1.57 (0.53, 4.62) | 1.76 (0.41, 7.49) |
| 2 | 1.29 (0.45, 3.67) | 1.45 (0.47, 4.48) | 1.19 (0.25, 5.53) |
| 3 | 3.63 (1.24, 10.67) | 2.46 (0.74, 8.23) | 2.61 (0.45, 15.00) |
| 4 or 5 syndemic conditions | 6.30 (1.70, 23.35) | 2.95 (0.59, 14.71) | 5.72 (0.89, 36.63) |
| Ordinal syndemic score | |||
| # syndemic conditions | 1.46 (1.13, 1.89) | 1.28 (0.96, 1.71) | 1.43 (0.94, 2.19) |
Abbreviations: AOR=adjusted odds ratio; CI=confidence interval; FSW=female sex worker; PrEP=pre-exposure prophylaxis; STI=sexually transmitted infection.
Reference group = low level of perceived barriers to PrEP use.
Adjusted for age in years and education (completed secondary school vs. less than secondary school).
Alcohol Use Disorder Identification Test score ≥8.
Use of ≥2 illicit drugs (heroin; methamphetamine; cocaine; inhalants; ecstasy; tranquilizers; barbiturates) in the past month.
Moderate or severe depression defined as a score ≥20 on the Beck Depression Inventory II (BDI-II).
Lifetime experience of physical abuse or sexual violence perpetrated by a client.
Tested positive for chlamydia, gonorrhea, or active syphilis.
Discussion
Most participants endorsed few barriers to PrEP use, suggesting that PrEP uptake may be high within this population. However, some participants’ patterns of perceived barriers indicate that multiple, financial, and healthcare access barriers may pose challenges to PrEP implementation. Further, over half of the sample experienced syndemic factors, suggesting that syndemic risk is common among FSWs in the Mexico-US border region.
Consistent with our main hypothesis, we found that FSWs with more syndemic factors may face the greatest barriers to PrEP uptake. In our model considering nominal syndemic scores, we found that those experiencing three to five syndemic factors had a higher odds of membership in the high level of perceived barriers class. Although this trend was only observed for FSWs experiencing three or more syndemic factors, findings from our model considering ordinal syndemic scores suggest that the odds of membership in this class increase linearly with the number of syndemic factors. While ordinal syndemic scores were marginally associated with membership in the perceived healthcare access and financial barriers to PrEP use classes, this trend was not observed in our model considering nominal syndemic scores, which may be due to the small prevalence of FSWs in those classes.
Depression was associated with membership in the financial and high level of perceived barriers classes. This is consistent with prior research highlighting depression as a barrier to health and social service utilization among FSWs (Kurtz, Surratt, Kiley, & Inciardi, 2005; Weissman et al., 1995). Depression has also been linked to lower self-efficacy for managing self-care and reduced engagement in healthcare services among FSWs (Hong, Li, Fang, & Zhao, 2007; Kurtz, Surratt, Kiley, & Inciardi, 2005). Moreover, research suggests that many FSWs enter sex work out of economic necessity (Bucardo et al., 2004), and such extreme poverty may heighten depression risk and act as a barrier to healthcare utilization.
Being STI-positive was associated with membership in the financial and high level of perceived barriers classes. FSWs who tested STI-positive (excluding HIV) may not have considered themselves at high-risk of HIV, and therefore may not have perceived PrEP to be beneficial. This underscores the need for PrEP programs to emphasize the link between STI and HIV acquisition, and the benefits of routine STI screening (Scott & Klausner, 2016). Polydrug use was the only factor associated with membership in the healthcare access barriers class. This maps onto previous work demonstrating that substance use acts as a barrier to treatment access among HIV-positive FSWs (Chakrapani, Newman, Shunmugam, Kurian, & Dubrow, 2009).
Limitations.
Given the cross-sectional and hypothetical nature of this study, the classes and associated factors identified may differ from those in the context of actual PrEP delivery. Non-random sampling was used to recruit FSWs, which may limit the generalizability of our findings. Our analysis relies on self-reported information on sensitive behaviors (e.g., substance use), which may have led to under-reporting. It is also possible that participants felt obliged to over-state their willingness to use PrEP in the context of an interviewer-administered survey. Finally, due to the sparseness of our data, we were unable to stratify by city.
Conclusions.
Taken together, our findings suggest efforts to address syndemic factors may enhance future PrEP uptake and maximize its impact among syndemic-affected FSWs. Importantly, prior research among clients of FSWs in this region demonstrated that a sexual risk reduction intervention attenuated the impact of syndemic risk factors on condom-unprotected sex (Pitpitan et al., 2015), suggesting that similar interventions may enhance PrEP use among syndemic-affected FSWs.
Supplementary Material
References
- Auerbach JD, Kinsky S, Brown G, & Charles V (2015). Knowledge, attitudes, and likelihood of pre-exposure prophylaxis (PrEP) use among US women at risk of acquiring HIV. AIDS Patient Care STDS, 29(2), 102–110. doi: 10.1089/apc.2014.0142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baeten JM, Donnell D, Ndase P, Mugo NR, Campbell JD, Wangisi J, … Katabira E (2012). Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med, 2012(367), 399–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baral S, Beyrer C, Muessig K, Poteat T, Wirtz AL, Decker MR, … Kerrigan D (2012). Burden of HIV among female sex workers in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Infect Dis, 12(7), 538–549. doi: 10.1016/s1473-3099(12)70066-x [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, & Carbin MG (1988). Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review, 8(1), 77–100. doi: 10.1016/0272-7358(88)90050-5 [DOI] [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, & Erbaugh J (1961). An inventory for measuring depression. Arch Gen Psychiatry, 4, 561–571. [DOI] [PubMed] [Google Scholar]
- Bucardo J, Brouwer KC, Magis-Rodríguez C, Ramos R, Fraga M, Perez SG, … Strathdee SA (2005). Historical trends in the production and consumption of illicit drugs in Mexico: Implications for the prevention of blood borne infections. Drug Alcohol Depend, 79(3), 281–293. doi: 10.1016/j.drugalcdep.2005.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bucardo J, Semple SJ, Fraga-Vallejo M, Davila W, & Patterson TL (2004). A qualitative exploration of female sex work in Tijuana, Mexico. Arch Sex Behav, 33(4), 343–351. doi: 10.1023/B:ASEB.0000028887.96873.f3 [DOI] [PubMed] [Google Scholar]
- Chakrapani V, Newman PA, Shunmugam M, Kurian AK, & Dubrow R (2009). Barriers to free antiretroviral treatment access for female sex workers in Chennai, India. AIDS patient care and STDs, 23(11), 973–980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choopanya K, Martin M, Suntharasamai P, Sangkum U, Mock PA, Leethochawalit M, … Vanichseni S (2013). Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir Study): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet, 381(9883), 2083–2090. doi: 10.1016/s0140-6736(13)61127-7 [DOI] [PubMed] [Google Scholar]
- Collins LM, & Lanza ST (2010). Latent Class and Latent Transition Analysis: John Wiley & Sons, Inc. [Google Scholar]
- Doggett EG, Lanham M, Wilcher R, Gafos M, Karim QA, & Heise L (2015). Optimizing HIV prevention for women: a review of evidence from microbicide studies and considerations for gender-sensitive microbicide introduction. Journal of the International AIDS Society, 18(1), 20536. doi: 10.7448/IAS.18.1.20536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Bassel N, Gilbert L, Wu E, Go H, & Hill J (2005). Relationship between drug abuse and intimate partner violence: a longitudinal study among women receiving methadone. Am J Public Health, 95(3), 465–470. doi: 10.2105/ajph.2003.023200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Bassel N, Terlikbaeva A, & Pinkham S (2010). HIV and women who use drugs: double neglect, double risk. The Lancet, 376(9738), 312–314. doi: 10.1016/S0140-6736(10)61026-4 [DOI] [PubMed] [Google Scholar]
- Gaines TL, Rusch ML, Brouwer KC, Goldenberg SM, Lozada R, Robertson AM, … & Patterson TL (2013). Venue-level correlates of female sex worker registration status: a multilevel analysis of bars in Tijuana, Mexico. Global public health, 8(4), 405–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea JT, Kinsler JJ, Salazar X, Lee SJ, Giron M, Sayles JN, … Cunningham WE (2011). Acceptability of pre-exposure prophylaxis as an HIV prevention strategy: barriers and facilitators to pre-exposure prophylaxis uptake among at-risk Peruvian populations. Int J STD AIDS, 22(5), 256–262. doi: 10.1258/ijsa.2009.009255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gielen AC, Ghandour RM, Burke JG, Mahoney P, McDonnell KA, & O’Campo P (2007). HIV/AIDS and intimate partner violence: intersecting women’s health issues in the United States. Trauma Violence Abuse, 8(2), 178–198. doi: 10.1177/1524838007301476 [DOI] [PubMed] [Google Scholar]
- Goodman LA (1974a). The analysis of systems of qualitative variables when some of the variables are unobservable. Part IA modified latent structure approach. American Journal of Sociology, 79(5), 1179–1259. [Google Scholar]
- Goodman LA (1974b). Exploratory latent structure analysis using both identifiable and unidentifiable models. Biometrika, 61(2), 215–231. [Google Scholar]
- Goparaju L, Praschan NC, Warren-Jeanpiere L, Experton LS, Young MA, & Kassaye S (2017). Stigma, Partners, Providers and Costs: Potential Barriers to PrEP Uptake among US Women. J AIDS Clin Res, 8(9). doi: 10.4172/2155-6113.1000730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, … Glidden DV (2010). Preexposure Chemoprophylaxis for HIV Prevention in Men Who Have Sex with Men. New England Journal of Medicine, 363(27), 2587–2599. doi: 10.1056/NEJMoa1011205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagenaars JA (1988). Latent structure models with direct effects between indicators: local dependence models. Sociological Methods & Research, 16(3), 379–405. [Google Scholar]
- Hong Y, Li X, Fang X, & Zhao R (2007). Depressive symptoms and condom use with clients among female sex workers in China. Sexual Health, 4(2), 99–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Illangasekare S, Burke J, Chander G, & Gielen A (2013). The syndemic effects of intimate partner violence, HIV/AIDS, and substance abuse on depression among low-income urban women. J Urban Health, 90(5), 934–947. doi: 10.1007/s11524-013-9797-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurtz SP, Surratt HL, Kiley MC, & Inciardi JA (2005). Barriers to health and social services for street-based sex workers. Int J Health Care Poor Underserved, 16. doi: 10.1353/hpu.2005.0038 [DOI] [PubMed] [Google Scholar]
- Lazarsfeld PF, & Henry NW (1968). Latent structure analysis. Houghton Mifflin Co. [Google Scholar]
- Lichtenstein B (2006). Domestic violence in barriers to health care for HIV-positive women. AIDS Patient Care STDS, 20(2), 122–132. doi: 10.1089/apc.2006.20.122 [DOI] [PubMed] [Google Scholar]
- Mack N, Evens EM, Tolley EE, Brelsford K, Mackenzie C, Milford C, … Kimani J (2014). The importance of choice in the rollout of ARV-based prevention to user groups in Kenya and South Africa: a qualitative study. Journal of the International AIDS Society, 17(3Suppl 2), 19157. doi: 10.7448/IAS.17.3.19157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maher L, Mooney-Somers J, Phlong P, Couture M-C, Stein E, Evans J, … Page K (2011). Selling sex in unsafe spaces: sex work risk environments in Phnom Penh, Cambodia. Harm Reduction Journal, 8, 30 10.1186/1477-7517-8-30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maman S, Campbell J, Sweat MD, & Gielen AC (2000). The intersections of HIV and violence: directions for future research and interventions. Soc Sci Med, 50(4), 459–478. [DOI] [PubMed] [Google Scholar]
- Meyer JP, Springer SA, & Altice FL (2011). Substance Abuse, Violence, and HIV in Women: A Literature Review of the Syndemic. Journal of Women’s Health, 20(7). doi: 10.1089/jwh.2010.2328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minnis AM, Gandham S, Richardson BA, Guddera V, Chen BA, Salata R, … Hendrix CW (2013). Adherence and acceptability in MTN 001: a randomized cross-over trial of daily oral and topical tenofovir for HIV prevention in women. AIDS Behav, 17(2), 737–747. doi: 10.1007/s10461-012-0333-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mizuno Y, Purcell DW, Knowlton AR, Wilkinson JD, Gourevitch MN, & Knight KR (2015). Syndemic Vulnerability, Sexual and Injection Risk Behaviors, and HIV Continuum of Care Outcomes in HIV-Positive Injection Drug Users. AIDS Behav, 19(4), 684–693. doi: 10.1007/s10461-014-0890-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson TL, Semple SJ, Staines H, Lozada R, Orozovich P, Bucardo J, … Strathdee SA (2008). Prevalence and Correlates of HIV Infection among Female Sex Workers in Two Mexico-U.S. Border Cities. The Journal of infectious diseases, 197(5), 728–732. doi: 10.1086/527379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson TL, Semple SJ, Abramovitz D, Harvey-Vera A, Pines HA, Verdugo S, … & Strathdee SA (2018). Impact of time perspectives on texting intervention to reduce HIV/STI transmission among female sex workers in Tijuana and Ciudad Juarez, Mexico. Journal of behavioral medicine, 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pines HA, Strathdee SA, Hendrix CW, Bristow CC, Harvey-Vera A, Magis-Rodríguez C, … & Patterson TL (2019). Oral and vaginal HIV pre-exposure prophylaxis product attribute preferences among female sex workers in the Mexico-US border region. International journal of STD & AIDS, 30(1), 45–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pines HA, Semple SJ, Strathdee SA, Hendrix CW, Harvey-Vera A, Gorbach PM, … & Patterson TL (2018). Vaginal washing and lubrication among female sex workers in the Mexico-US border region: implications for the development of vaginal PrEP for HIV prevention. BMC public health, 18(1), 1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pitpitan EV, Strathdee SA, Semple SJ, Chavarin CV, Magis-Rodriguez C, & Patterson TL (2015). Buffering syndemic effects in a sexual risk-reduction intervention for male clients of female sex workers: results from a randomized controlled trial. American journal of public health, 105(9), 1866–1871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson AM, Syvertsen JL, Martinez G, Rangel MG, Palinkas LA, Stockman JK, … Strathdee SA (2013). Acceptability of vaginal microbicides among female sex workers and their intimate male partners in two Mexico-U.S. border cities: a mixed methods analysis. Global public health, 8(5), 619–633. doi: 10.1080/17441692.2012.762412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, & Grant M (1993). Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption--II. Addiction, 88(6), 791–804. [DOI] [PubMed] [Google Scholar]
- Scott HM, & Klausner JD (2016). Sexually transmitted infections and pre-exposure prophylaxis: challenges and opportunities among men who have sex with men in the US. AIDS Res Ther, 13, 5. doi: 10.1186/s12981-016-0089-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Secretaria de Salud, Centro Nacional para la Prevencion y el Control del VIH y el SIDA (CENSIDA). (2005).
- Shannon K, Strathdee SA, Shoveller J, Rusch M, Kerr T, & Tyndall MW (2009). Structural and Environmental Barriers to Condom Use Negotiation With Clients Among Female Sex Workers: Implications for HIV-Prevention Strategies and Policy. American Journal of Public Health, 99(4), 659–665. 10.2105/AJPH.2007.129858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer M (2000). A dose of drugs, a touch of violence, a case of AIDS: conceptualizing the SAVA syndemic. Free Inquiry in Creative Sociology, 28(1), 13–24. [Google Scholar]
- Strathdee SA, Magis-Rodriguez C, Mays VM, Jimenez R, & Patterson TL (2012). The emerging HIV epidemic on the Mexico-U.S. border: an international case study characterizing the role of epidemiology in surveillance and response. Ann Epidemiol, 22(6), 426–438. doi: 10.1016/j.annepidem.2012.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strathdee SA, Philbin MM, Semple SJ, Pu M, Orozovich P, Martinez G, … Patterson TL (2008). Correlates of injection drug use among female sex workers in two Mexico-U.S. border cities. Drug Alcohol Depend, 92(1–3), 132–140. doi: 10.1016/j.drugalcdep.2007.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strathdee SA, Abramovitz D, Lozada R, Martinez G, Rangel MG, Vera A, … & Patterson TL (2013). Reductions in HIV/STI incidence and sharing of injection equipment among female sex workers who inject drugs: results from a randomized controlled trial. PloS one, 8(6), e65812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Syvertsen JL, Robertson Bazzi AM, Scheibe A, Adebajo S, Strathdee SA, & Wechsberg WM (2014). The promise and peril of pre-exposure prophylaxis (PrEP): using social science to inform prep interventions among female sex workers. Afr J Reprod Health, 18(3 Spec No), 74–83. [PMC free article] [PubMed] [Google Scholar]
- Thigpen MC, Kebaabetswe PM, Paxton LA, Smith DK, Rose CE, Segolodi TM, … Brooks JT (2012). Antiretroviral Preexposure Prophylaxis for Heterosexual HIV Transmission in Botswana. New England Journal of Medicine, 367(5), 423–434. doi: 10.1056/NEJMoa1110711 [DOI] [PubMed] [Google Scholar]
- Ulibarri MD, Hiller SP, Lozada R, Rangel MG, Stockman JK, Silverman JG, & Ojeda VD (2013). Prevalence and characteristics of abuse experiences and depression symptoms among injection drug-using female sex workers in Mexico. J Environ Public Health, 2013, 631479. doi: 10.1155/2013/631479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ulibarri MD, Strathdee SA, Lozada R, Magis-Rodriguez C, Amaro H, O’Campo P, & Patterson TL (2014). Prevalence and correlates of client-perpetrated abuse among female sex workers in two Mexico-U.S. border cities. Violence against women, 20(4), 427–445. doi: 10.1177/1077801214528582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ulibarri MD, Strathdee SA, Ulloa EC, Lozada R, Fraga MA, Magis-Rodríguez C, … Patterson TL (2011). Injection Drug Use as a Mediator Between Client-perpetrated Abuse and HIV Status Among Female Sex Workers in Two Mexico-US Border Cities. AIDS Behav, 15(1), 179–185. doi: 10.1007/s10461-009-9595-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van der Elst EM, Mbogua J, Operario D, Mutua G, Kuo C, Mugo P, … Sanders EJ (2013). High acceptability of HIV pre-exposure prophylaxis but challenges in adherence and use: qualitative insights from a phase I trial of intermittent and daily PrEP in at-risk populations in Kenya. AIDS Behav, 17(6), 2162–2172. doi: 10.1007/s10461-012-0317-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Straten A, Stadler J, Luecke E, Laborde N, Hartmann M, Montgomery ET, & on behalf of the, V.-C. S. T. (2014). Perspectives on use of oral and vaginal antiretrovirals for HIV prevention: the VOICE-C qualitative study in Johannesburg, South Africa. Journal of the International AIDS Society, 17(3Suppl 2), 19146. doi: 10.7448/IAS.17.3.19146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Straten A, Stadler J, Montgomery E, Hartmann M, Magazi B, Mathebula F, … Soto-Torres L (2014). Women’s Experiences with Oral and Vaginal Pre-Exposure Prophylaxis: The VOICE-C Qualitative Study in Johannesburg, South Africa. PLoS One, 9(2), e89118. doi: 10.1371/journal.pone.0089118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vera A, Abramovitz D, Lozada R, Martinez G, Rangel MG, Staines H, … & Strathdee SA (2012). Mujer Mas Segura (Safer Women): a combination prevention intervention to reduce sexual and injection risks among female sex workers who inject drugs. BMC Public Health, 12(1), 653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vermunt JK (2010). Latent class modeling with covariates: Two improved three-step approaches. Political analysis, 18(4), 450–469. [Google Scholar]
- Vermunt JK, Magidson J. Technical Guide for Latent GOLD 5.1: Basic, Advanced, and Syntax. Belmont, MA: Statistical Innovations Inc; 2016. [Google Scholar]
- Weissman G, Melchior L, Huba G, Altice F, Booth R, Cottler L, … et al. (1995). Women living with substance abuse and HIV disease: medical care access issues. J Am Med Womens Assoc (1972), 50(3–4), 115–120. [PubMed] [Google Scholar]
- WHO Guidelines Approved by the Guidelines Review Committee. (2016) Consolidated Guidelines on HIV Prevention, Diagnosis, Treatment and Care for Key Populations -2016 Update. Geneva: World Health Organization. [PubMed] [Google Scholar]
- Ye L, Wei S, Zou Y, Yang X, Abdullah AS, Zhong X, … Huang A (2014). HIV pre-exposure prophylaxis interest among female sex workers in Guangxi, China. PLoS One, 9(1), e86200. doi: 10.1371/journal.pone.0086200 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


