Abstract
Background:
There is an increasing appreciation of the cardiovascular implications of nonalcoholic fatty liver disease with advanced fibrosis (NAFLD-fibrosis). However, data regarding stroke risk are limited. We sought to investigate whether NAFLD-fibrosis is associated with stroke in addition to heart disease.
Methods:
We performed a cross-sectional study using data from the United States National Health and Nutrition Examination Survey (2005–2014). After excluding participants with competing causes of liver disease, the Fibrosis-4 score (FIB-4) and NAFLD Fibrosis Score (NFS) were calculated. First, we used a composite measure to classify participants: NAFLD-fibrosis was defined as having at least one score above its validated cut-off. Second, we also used the FIB-4 and NFS scores individually. The key outcome was prevalent stroke, and we also evaluated heart disease; both were self-reported. Multivariable logistic regression assessed the association between NAFLD-fibrosis and these outcomes while adjusting for demographic variables and cardiovascular risk factors.
Results:
We identified 1,653 participants with NAFLD-fibrosis from a sample of 27,040 participants. In total, 753 had prior stroke. An association between NAFLD-fibrosis and stroke was seen when using the FIB-4 score (OR 1.87, 95% CI 1.00–3.50) but not the NFS (OR 1.31, 95% CI 0.92–1.87). NAFLD-fibrosis was associated with heart disease (OR 1.46, 95% CI 1.06–2.01) using the composite measure and both scores individually.
Conclusions:
NAFLD-fibrosis may be associated with stroke in addition to heart disease, with differences depending on the measure used to define NAFLD-fibrosis.
Keywords: Stroke, cerebrovascular disease, liver disease, epidemiology, risk factors
1. Introduction
Nonalcoholic fatty liver disease (NAFLD) is a worldwide epidemic with a global prevalence of 25%.1 NAFLD represents a spectrum of disease that ranges from isolated steatosis in nonalcoholic fatty liver to nonalcoholic steatohepatitis (steatosis plus histologic inflammation and hepatocyte injury), which can lead to fibrosis and eventually cirrhosis.2 Although NAFLD has been associated with cardiovascular disease broadly,3–7 some studies suggest that shared risk factors may account for potential associations with cardiovascular diseases.8, 9 Indeed, a Mendelian randomization study found that liver fat content may not be casually associated with ischemic heart disease.10 Instead, recent studies found that NAFLD with advanced fibrosis (NAFLD-fibrosis), and not isolated nonalcoholic fatty liver per se, is associated with both cardiovascular disease and cardiovascular mortality.6, 11–14 While a specific association with stroke has not clearly emerged,15–18 there is limited evidence that liver fibrosis may be associated with ischemic stroke19 and cerebral microhemorrhages.20 Additionally, we and others have previously shown that cirrhosis is associated with stroke.21, 22 However, these studies were limited by their use of imprecise administrative claims data and included individuals with very advanced, decompensated liver disease. Whether validated, biologically-informed measures of NAFLD-fibrosis are associated with stroke at the population level is not known. Therefore, we sought to assess whether measures of NAFLD-fibrosis are associated with stroke, in addition to heart disease, in a large, population-based sample using data from the United States National Health and Nutrition Examination Survey (NHANES).
2. Materials and Methods
2.1. Study Design
We performed a cross-sectional study using continuous survey data from five biannual survey cycles spanning 2005 to 2014. The NHANES data are collected by the United States National Center for Health Statistics, Centers for Disease Control and Prevention using a multistage, probability cluster survey method to generate nationally representative statistics for the US population. Participants undergo standardized interview, physical examination, and biological specimen collection in mobile examination centers.23 Data collection for NHANES was approved by the National Center for Health Statistics Research Ethics Review Board, and written informed consent was obtained from participants; the study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki. Analysis of de-identified data from the survey is exempt from United States federal regulations for the protection of human research participants. The data that support the findings of this study are publicly available at https://www.cdc.gov/nchs/nhanes. JG had full access to all the data in the study and takes responsibility for its integrity and the data analysis.
2.2. Population
We included adult participants 21 years of age and older enrolled in NHANES from 2005 to 2014. Participants with missing age, ethnicity, sex, liver function test values, platelet count values, cardiovascular disease history information, and alcohol use history were excluded. In keeping with prior analyses of NAFLD in NHANES and in order to minimize the contribution of common competing causes of chronic liver disease or abnormalities in liver chemistries,24 we excluded pregnant women, participants with laboratory evidence of viral hepatitis (B or C), possible acute liver injury, self-reported excessive alcohol consumption, and use of medications associated with liver steatosis. Evidence of viral hepatitis included positive tests for hepatitis B core antibody and hepatitis C antibody. Aminotransferase levels greater than 500 U/l were considered evidence of possible acute liver injury at the time of collection. Excessive alcohol consumption was defined as >21 standard drinks per week for men and >14 standard drinks per week for women.2 Participants reporting use of valproic acid, amiodarone, methotrexate, and tamoxifen were excluded because these medications are associated with hepatic steatosis.
2.3. Exposures
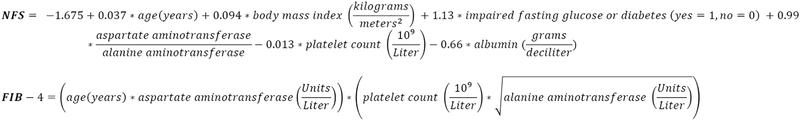
Several non-invasive, serum-based clinical scores have been developed and validated to identify advanced fibrosis in NAFLD and have been used previously in the analysis of NHANES data.13, 25 We calculated two scores for each participant: The Nonalcoholic Fatty Liver Disease Fibrosis Score (NFS) and the Fibrosis-4 (FIB-4) score.26, 27 These scores are calculated from demographic variables, anthropometric data, and laboratory data (Figure 1). The cut-offs used to assess underlying advanced fibrosis were NFS > 0.676 and FIB-4 > 3.25.25 The specificity of these cutoffs, compared to liver biopsy (gold standard), for detection of advanced fibrosis in NAFLD exceeds 90%.28 First, we categorized participants as having NAFLD-fibrosis if they had at least one score above its cut-off were categorized as NAFLD-fibrosis. We then also used each score individually, as validated.
Fig. 1.
Formulae for liver fibrosis scores
Nonalcoholic fatty liver disease with advanced fibrosis was ascertained using the Nonalcoholic Fatty Liver Disease – Fibrosis Score (NFS) and Fibrosis-4 (FIB-4) score.
Covariates included demographic variables, anthropometric data, clinical history, and laboratory data. Demographic variables included age, sex, ethnicity, the poverty-ratio index (ratio of family income to the local poverty threshold by which an index of <100% denotes poverty), health insurance (uninsured versus insured), and educational attainment (≤12th grade education versus >12th grade education). Physical inactivity was defined as the absence of at least moderate physical activity within the 30 days prior to the NHANES interview. Hypertension was defined as self-reported diagnosis, blood pressure > 140/90 mm Hg, or use of anti-hypertensive medications. Diabetes mellitus was defined as self-reported diagnosis, hemoglobin A1c ≥ 6.5%, or use of diabetes medications. Dyslipidemia was defined as self-reported diagnosis, total serum cholesterol ≥ 240 mg/dl, or use of cholesterol lowering (statin) medications. Obesity was defined as a body mass index of ≥ 30 kg/meters2. Smoking was categorized as current smoking versus not current smoking.
2.4. Outcomes
The key outcome was stroke. The outcome of prevalent stroke was defined based on participants’ responses to the following survey question: “Has a doctor or other health professional ever told you that you had a stroke”. The additional outcome was heart disease, which was defined as affirmative responses to similar questions regarding myocardial infarction, coronary revascularization procedures, angina, and congestive heart failure. A composite outcome of major cardiovascular disease was also included, which encompassed both stroke and heart disease. The measures of self-reported stroke and myocardial infarction have been shown to be reasonably accurate in the United States general population and have been used in prior epidemiological studies using data from NHANES.29–31
2.5. Statistical Analyses
Survey-weighted estimates of prevalence of baseline demographic characteristics and comorbidities were calculated. Estimates were weighted using NHANES cycle-specific weights to account for oversampling and nonresponse rates, and data for five biannual cycles were merged into one 10-year pooled dataset. Descriptive statistics were generated using survey procedures. Participant characteristics were compared across exposure groups using the chi-squared test and t-test as appropriate. We used multivariable logistic regression to estimate the odds ratios and 95% confidence intervals (OR, 95% CI) for the association between liver disease and self-reported stroke, in addition to heart disease and major cardiovascular disease, in three models. Sampling weights were used to account for the complex, multi-staged sampling design of NHANES. Model 1 was unadjusted. Model 2 was adjusted for age, sex, education, insurance, poverty, and physical inactivity, and Model 3 was additionally adjusted for hypertension, diabetes, dyslipidemia, smoking, and obesity. Model 3 accounted for statin use because the definition of dyslipidemia reflected statin use. In post-hoc analyses, we repeated Model 3 without inclusion of dyslipidemia in case dyslipidemia is a mediator in the pathway. The threshold of statistical significance was set at α = 0.05. Statistical analyses were performed using SAS software, version 9.4 (SAS Institute Inc., Cary, NC).
3. Results
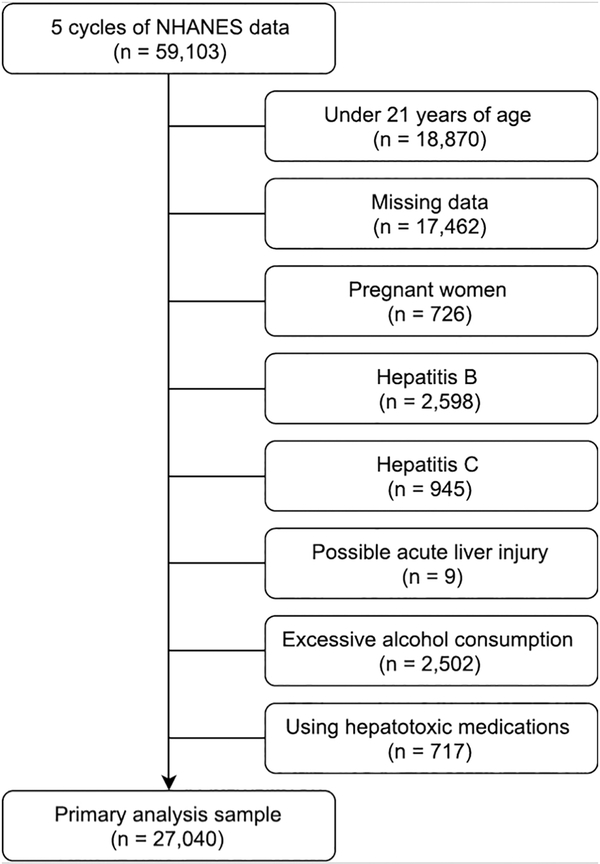
Our study sample consisted of 27,040 participants after exclusions (Figure 2). Of these, 1,653 participants (6.1%) had at least one non-invasive fibrosis score above its respective high probability cut-off and was thus categorized as having possible NAFLD-fibrosis. Among these participants, the NFS and FIB-4 scores were above cut-offs for 89% and 26%, respectively. Participants with NAFLD-fibrosis were older, more often men, and had a greater burden of cardiovascular risk factors than participants without NAFLD-fibrosis (Table 1). In the total sample, 753 (2.8%) participants reported prevalent stroke, 1,815 (6.7%) reported prevalent heart disease, and 2,282 (8.4%) reported prevalent major cardiovascular disease. The prevalence of these outcomes were greater in participants with NAFLD-fibrosis as compared to those without: stroke (11% vs 2%), heart disease (30% vs 5%), and major cardiovascular disease (36% vs 7%).
Fig. 2.
Participant flow diagram for primary analysis of nonalcoholic fatty liver disease with advanced fibrosis
Participants under the age of 21 and those with missing data were excluded. In addition, participants were excluded if they were pregnant women, had laboratory evidence of hepatitis B or hepatitis C infection, had laboratory evidence of acute liver injury at the time of blood analysis, reported excessive alcohol consumption, and/or reported using medications associated with liver steatosis. Some participants had multiple reasons for exclusion.
Table 1.
Characteristics of Participants, Stratified by NAFLD-fibrosis
| Characteristic* | N AFLD-fibrosis† (N = 1,653) |
Without NAFLD- fibrosis (N = 25,387) |
|---|---|---|
| Age, mean (SE, IQR), y | 65.5 (0.5, 57.0–76.4) | 45.9 (0.3, 31.6–57.4) |
| Female | 840 (51%) | 13,145 (52%) |
| Race‡ | ||
| White | 852 (75%) | 11,834 (70%) |
| African American or Non-Hispanic Black | 418 (14%) | 4,702 (10%) |
| Hispanic | 329 (9%) | 6,506 (14%) |
| Other | 54 (3%) | 2,345 (6%) |
| Poverty Income Ratio Index < 100%§ | 184 (12%) | 3,232 (14%) |
| Uninsured | 123 (7%) | 4,866 (19%) |
| ≤12th grade education§ | 1,255 (76%) | 21,254 (84%) |
| Physical inactivity‖ | 1,328 (80%) | 13,849 (55%) |
| Hypertension# | 1,345 (81%) | 8,794 (35%) |
| Diabetes** | 1,115 (67%) | 2,043 (8%) |
| Dyslipidemia†† | 1,192 (72%) | 14,393 (57%) |
| Current smoking§ | 154 (9%) | 4,959 (20%) |
| Body mass index ≥ 30 kg/meters2§ | 1,152 (70%) | 8,760 (35%) |
Abbreviations: NAFLD-fibrosis, nonalcoholic fatty liver disease with advanced fibrosis; SE, standard error;
IQR, interquartile range.
Data are reported as number (%) except as otherwise specified.
Possible NAFLD-fibrosis was defined as having a Nonalcoholic Fatty Diver Disease Fibrosis score (NFS) > 0.676 and/or Fibrosis-4 (FIB-4) score > 3.25.
As reported by participants.
Data were missing for 8% of participants for poverty and <1% for education, smoking, and obesity. The values provided are for participants with available data.
Absence of at least moderate physical activity within last 30 days.
BP >140/90 mm Hg, on antihypertensive medications, or self-report.
Hemoglobin A1C ≥6.5%, on diabetes mellitus medications, or self-report.
Total serum cholesterol ≥240 mg/dL, on lipid lowering medications, or self-report.
When using both scores together in a composite measure to define NAFLD-fibrosis, NAFLD-fibrosis was associated with increased odds of stroke (OR 5.75, 95% CI 4.66–7.09) in the unadjusted model (Model 1). The associations were progressively attenuated after adjustment for demographics, physical inactivity, and cardiovascular risk factors in Models 2 and 3 (Table 2). After adjustment for all covariates in Model 3, the association for stroke (OR 1.35, 95% CI 0.96–1.90) was not statistically significant. Then, we used the fibrosis scores individually. When NAFLD-fibrosis was defined using the FIB-4 score, an association with stroke was observed (OR 1.87, 95% CI 1.00–3.50) in the most adjusted model. This was not the case when using the NFS (OR 1.31, 95% CI 0.92–1.87). The direction of effect and effect size was similar regardless of how we defined NAFLD-fibrosis.
Table 2.
Associations between NALFD-fibrosis and Self-report of Prevalent Stroke, Heart Disease, and Major Cardiovascular Disease
| Outcome and Exposure* | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| Stroke | |||
| NAFLD-fibrosis composite† | 5.75 (4.66–7.09) | 1.86 (1.45–2.39) | 1.35 (0.96–1.90) |
| FIB-4 > 3.25 | 6.54 (3.81–11.22) | 1.69 (0.96–2.97) | 1.87 (1.00–3.50) |
| NFS > 0.676 | 5.79 (4.79–7.01) | 1.96 (1.56–2.47) | 1.31 (0.92–1.87) |
| Heart disease‡ | |||
| NAFLD-fibrosis composite | 7.63 (6.20–9.83) | 2.44 (1.95–3.05) | 1.46 (1.06–2.01) |
| FIB-4 > 3.25 | 6.94 (5.04–9.56) | 1.58 (1.11–2.25) | 1.79 (1.23–2.61) |
| NFS > 0.676 | 7.88 (6.21–9.99) | 2.70 (2.07–3.53) | 1.48 (1.02–2.17) |
| Major cardiovascular disease§ | |||
| NAFLD-fibrosis composite | 7.81 (6.60–9.25) | 2.50 (2.02–3.04) | 1.53 (1.14–2.05) |
| FIB-4 > 3.25 | 7.20 (5.12–10.11) | 1.60 (1.15–2.24) | 1.81 (1.26–2.60) |
| NFS > 0.676 | 7.96 (6.64–9.53) | 2.27 (2.15–3.36) | 1.52 (1.09–2.11) |
Abbreviations: NAFLD-fibrosis, nonalcoholic fatty liver disease with advanced fibrosis; NFS, Nonalcoholic Fatty Liver Disease Fibrosis score; FIB-4, fibrosis-4 score.
Results of multivariable analysis are reported as the odds ratio (95% confidence interval). Model 1 is unadjusted; Model 2 is adjusted for age, sex, race/ethnicity, insurance status, poverty, education, and physical inactivity. Model 3 is additionally adjusted for hypertension, diabetes, dyslipidemia, smoking, and obesity.
In the primary analysis, possible NAFLD-fibrosis was defined as NFS > 0.676 and/or FIB-4 > 3.25.
Heart disease was defined as a composite of myocardial infarction, coronary revascularization procedure, angina, and congestive heart failure.
Major cardiovascular disease was defined as a composite of stroke, myocardial infarction, coronary revascularization procedure, angina, and congestive heart failure.
Similarly, the composite measure of NAFLD-fibrosis was associated with heart disease (OR 7.63, 95% CI 6.20–9.83) and major cardiovascular disease (OR 7.81, 95% CI 6.60–9.25) in unadjusted models. After adjustment for all covariates in Model 3, NAFLD-fibrosis remained associated with heart disease (OR 1.46, 95% CI 1.06–2.01) and major cardiovascular disease (OR 1.53, 95% CI 1.14–2.05). The results were consistent when using each fibrosis score individually (Table 2). In post-hoc analyses, the results of Model 3 for stroke, heart disease, and major cardiovascular disease did not meaningfully change when dyslipidemia was not adjusted for (data not shown).
4. Discussion
In this cross-sectional analysis of a contemporary population-based sample, NAFLD-fibrosis was associated with prevalent stroke in addition to heart disease; however, associations were attenuated after adjustment for demographics and cardiovascular risk factors. In most adjusted models, NAFLD-fibrosis was associated with stroke when using the FIB-4 score but not the NFS.
Prior data regarding the association between NAFLD-fibrosis and stroke were sparse. Our findings are consistent with a case-control study that studied the association between liver fibrosis – assessed by transient elastography, an ultrasound-based measure of fibrosis – and stroke.19 They found that the degree of liver fibrosis was associated with an increased risk of stroke; however, their findings were not definitive because controls were selected from healthy patients undergoing health screening, whereas cases were evaluated for liver fibrosis at the time of stroke. To our knowledge, no prior studies used validated scores calculated from routinely collected health care data. NAFLD-fibrosis, when defined using the FIB-4 score, was associated with an increased odds of stroke. The discrepant results between different scores may be due to the FIB-4 score’s greater predictive value.26 The largely consistent effect sizes and direction of effect across adjusted models, regardless of how NAFLD-fibrosis was defined, supports an association between NAFLD-fibrosis and stroke in our study. However, marked attenuation in effect size was seen with incremental adjustment for vascular risk factors. Given the possibility of residual confounding, the magnitude and precision of the observed effect sizes should be interpreted with caution. Taken together, these data suggest that liver fibrosis may be independently associated with stroke, in addition to previously known associations with heart disease.
These findings are generally consistent with a growing body of literature regarding the overall risk of cardiovascular disease in participants with chronic liver disease. At one end of the spectrum, NAFLD, on the whole, has been previously associated with cardiovascular disease but not specifically stroke.4, 5, 7, 15–17, 32 However, recent data suggest that an increased risk of cardiovascular disease is seen primarily in participants with advanced degrees of liver fibrosis (e.g., histologic nonalcoholic steatohepatitis).6, 11, 13, 14 For example, a recent analysis of the Multi-Ethnic Study of Atherosclerosis found magnetic resonance liver imaging evidence of fibrosis to be associated with prevalent cardiovascular disease outcomes.14 Our findings regarding stroke are therefore consistent with data regarding cardiovascular outcomes broadly.
An association between NAFLD-fibrosis and stroke is likely multifactorial. First, a dose-dependent association between degree of liver fibrosis measured on transient elastography and cerebral microhemorrhages suggests that small vessel disease or coagulopathy may be implicated.20 Second, NAFLD, in particular the more advanced nonalcoholic steatohepatitis, is associated with systemic inflammation33, 34 and vascular inflammation.35 Third, NAFLD has been associated with increased atherosclerosis,3, 36–39 including carotid artery atherosclerosis.40 Fourth, advanced liver disease is associated with a mixed coagulopathy,41 which may have ramifications for both thrombotic and hemorrhagic stroke risk. Last, it should be noted that NAFLD-spectrum disorders are heterogeneous; stroke and cardiovascular risk may differ based on whether an individual’s liver disease is genetically or metabolically driven.42
Our study builds on prior studies in part by leveraging non-invasive serum-based scores for NAFLD-fibrosis and in a diverse, nationally-representative, population-based sample. Our findings should be interpreted in light of two important methodological considerations. First, NAFLD-fibrosis was ascertained using non-invasive scores that account for a heterogeneous group of variables, ranging from demographics to laboratory values. This may account for the variable accuracy of these scores25, 28 and in turn explain why we found that each score accounted for a different proportion of the overall sample of participants with NAFLD-fibrosis. However, the high specificity of the scores and the overall consistency of the results of the multivariable models is reassuring. Similarly, while common competing causes of liver disease were excluded, individuals may have underreported alcohol use such that there was misclassification error. Although the use of these non-invasive scores introduces the possibility of misclassification error, misclassification of the exposures was likely non-differential, which would be expected to have attenuated the observed associations. Second, stroke and other cardiovascular diseases were ascertained by self-report, so we lack information on stroke type, etiology, and severity. Specifically, ischemic and hemorrhagic stroke cannot be differentiated in NHANES. Given prior evidence that the association between advanced liver disease and stroke may be stronger for hemorrhagic stroke than ischemic stroke,21, 22 the effect size of the association between NAFLD-fibrosis and stroke in adjusted models may have been attenuated in part by the inclusion of ischemic stroke alongside hemorrhagic stroke. Further study with more precise ascertainment of NAFLD-fibrosis and stroke types is necessary to clarify and confirm our findings.
Several additional limitations warrant discussion. First, this was an observational, cross-sectional study such that the temporality of the association between NAFLD-fibrosis and outcomes cannot be assessed. Second, because only non-institutionalized participants who can respond to surveys are included in NHANES, it is possible that our sample included healthier participants with less severe strokes and heart disease. Third, although our sample included 10 years of NHANES data, the analysis with stroke as an outcome may have been underpowered because stroke was less prevalent than heart disease. Last, as discussed earlier, there was marked attenuation of effect size after adjustment for vascular risk factors. This may reflect the presence of confounding and limits confidence with respect to the magnitude and precision of the effect sizes we report. However, we believe the risk of bias from confounding was at least in part mitigated by our use of NHANES data, which allowed comprehensive assessment of cardiovascular risk factors based on self-report, medication use, and clinical and laboratory data.
Among participants in a nationally representative sample of U.S. adults, NAFLD-fibrosis was associated with prevalent stroke, in addition to heart disease, albeit with heterogeneity depending on the measure used to define NAFLD-fibrosis. Prospective study using precise measures of liver disease and stroke are needed to better understand the implications of chronic liver disease for stroke.
Highlights:
Advanced liver fibrosis in nonalcoholic fatty liver disease leads to worse outcomes.
Associations with heart disease had previously been identified.
We analyzed nationally-representative health survey data to study stroke.
An association with stroke was also identified.
Sources of Funding:
This study was supported by National Institute of Neurological Disorders and Stroke grant T32NS07153 (PI: Elkind, Trainee: Parikh), and National Heart, Lung, and Blood Institute grant K23HL136891 (VanWagner). The funding sources had no involvement in study design, analysis and interpretation of data, writing of the manuscript, or in the decision to submit the article for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of interest:
none.
5. References
- 1.Younossi ZM, Koenig AB, Abdelatif D, et al. Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64:73–84 [DOI] [PubMed] [Google Scholar]
- 2.Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67:328–357. [DOI] [PubMed] [Google Scholar]
- 3.Mellinger JL, Pencina KM, Massaro JM, et al. Hepatic steatosis and cardiovascular disease outcomes: An analysis of the Framingham Heart Study. J Hepatol. 2015;63:470–476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stepanova M, Younossi ZM. Independent association between nonalcoholic fatty liver disease and cardiovascular disease in the US population. Clin Gastroenterol Hepatol. 2012;10:646–650 [DOI] [PubMed] [Google Scholar]
- 5.Wu S, Wu F, Ding Y, et al. Association of non-alcoholic fatty liver disease with major adverse cardiovascular events: A systematic review and meta-analysis. Sci Rep. 2016;6:33386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ekstedt M, Hagström H, Nasr P, et al. Fibrosis stage is the strongest predictor for disease-specific mortality in NAFLD after up to 33 years of follow-up. Hepatology. 2015;61:1547–1554 [DOI] [PubMed] [Google Scholar]
- 7.Targher G, Byrne CD, Lonardo A, et al. Non-alcoholic fatty liver disease and risk of incident cardiovascular disease: A meta-analysis. J Hepatol. 2016;65:589–600 [DOI] [PubMed] [Google Scholar]
- 8.Di Costanzo A, D’Erasmo L, Polimeni L, et al. Non-alcoholic fatty liver disease and subclinical atherosclerosis: A comparison of metabolically- versus genetically-driven excess fat hepatic storage. Atherosclerosis. 2017;257:232–239 [DOI] [PubMed] [Google Scholar]
- 9.Pisto P, Santaniemi M, Bloigu R, et al. Fatty liver predicts the risk for cardiovascular events in middle-aged population: A population-based cohort study. BMJ Open. 2014;4:e004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lauridsen BK, Stender S, Kristensen TS, et al. Liver fat content, non-alcoholic fatty liver disease, and ischaemic heart disease: Mendelian randomization and meta-analysis of 279 013 individuals. Eur Heart J. 2018;39:385–393 [DOI] [PubMed] [Google Scholar]
- 11.Le MH, Devaki P, Ha NB, et al. Prevalence of non-alcoholic fatty liver disease and risk factors for advanced fibrosis and mortality in the United States. PLoS One. 2017;12:e0173499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Angulo P, Kleiner DE, Dam-Larsen S, et al. Liver fibrosis, but no other histologic features, is associated with long-term outcomes of patients with nonalcoholic fatty liver disease. Gastroenterology. 2015;149:389–397.e310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim D, Kim WR, Kim HJ, et al. Association between noninvasive fibrosis markers and mortality among adults with nonalcoholic fatty liver disease in the United States. Hepatology. 2013;57:1357–1365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ostovaneh MR, Ambale-Venkatesh B, Fuji T, et al. Association of liver fibrosis with cardiovascular diseases in the general population: The Multi-Ethnic Study of Atherosclerosis (MESA). Circ Cardiovasc Imaging. 2018;11:e007241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moshayedi H, Ahrabi R, Mardani A, et al. Association between non-alcoholic fatty liver disease and ischemic stroke. Iran J Neurol. 2014;13:144–148 [PMC free article] [PubMed] [Google Scholar]
- 16.Ying I, Saposnik G, Vermeulen MJ, et al. Nonalcoholic fatty liver disease and acute ischemic stroke. Epidemiology. 2011;22:129–130 [DOI] [PubMed] [Google Scholar]
- 17.Hamaguchi M, Kojima T, Takeda N, et al. Nonalcoholic fatty liver disease is a novel predictor of cardiovascular disease. World J Gastroenterol. 2007;13:1579–1584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alexander KS, Zakai NA, Lidofsky SD, et al. Non-alcoholic fatty liver disease, liver biomarkers and stroke risk: The Reasons for Geographic and Racial Differences in Stroke cohort. PLoS One. 2018;13:e0194153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim SU, Song D, Heo JH, et al. Liver fibrosis assessed with transient elastography is an independent risk factor for ischemic stroke. Atherosclerosis. 2017;260:156–162 [DOI] [PubMed] [Google Scholar]
- 20.Kim YD, Song D, Heo JH, et al. Relationship between cerebral microbleeds and liver stiffness determined by transient elastography. PLoS One. 2015;10:e0139227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Parikh NS, Navi BB, Schneider Y, et al. Association between cirrhosis and stroke in a nationally representative cohort. JAMA Neurol. 2017;74:927–932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wu HY, Lin CS, Yeh CC, et al. Cirrhosis patients’ stroke risks and adverse outcomes: Two nationwide studies. Atherosclerosis. 2017;263:29–35 [DOI] [PubMed] [Google Scholar]
- 23.National Center for Health Statistics. National Health and Nutrition Examination Survey. (NHANES): questionnaires, datasets, and related documentation. https://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm. Accessed July 1, 2018.
- 24.Kabbany MN, Conjeevaram Selvakumar PK, et al. Prevalence of nonalcoholic steatohepatitis-associated cirrhosis in the United States: An analysis of National Health and Nutrition Examination Survey data. Am J Gastroenterol. 2017;112:581–587 [DOI] [PubMed] [Google Scholar]
- 25.Xiao G, Zhu S, Xiao X, et al. Comparison of laboratory tests, ultrasound, or magnetic resonance elastography to detect fibrosis in patients with nonalcoholic fatty liver disease: A meta-analysis. Hepatology. 2017 [DOI] [PubMed] [Google Scholar]
- 26.Shah AG, Lydecker A, Murray K, et al. Comparison of noninvasive markers of fibrosis in patients with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2009;7:1104–1112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Angulo P, Hui JM, Marchesini G, et al. The NAFLD Fibrosis score: A noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology. 2007;45:846–854 [DOI] [PubMed] [Google Scholar]
- 28.McPherson S, Stewart SF, Henderson E, et al. Simple non-invasive fibrosis scoring systems can reliably exclude advanced fibrosis in patients with non-alcoholic fatty liver disease. Gut. 2010;59:1265–1269 [DOI] [PubMed] [Google Scholar]
- 29.Okura Y, Urban LH, Mahoney DW, et al. Agreement between self-report questionnaires and medical record data was substantial for diabetes, hypertension, myocardial infarction and stroke but not for heart failure. J Clin Epidemiol. 2004;57:1096–1103 [DOI] [PubMed] [Google Scholar]
- 30.Lin MP, Ovbiagele B, Markovic D, et al. “Life’s simple 7” And long-term mortality after stroke. J Am Heart Assoc. 2015;4(11). doi: 10.1161/JAHA.114.001470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shah NS, Huffman MD, Ning H, et al. Trends in myocardial infarction secondary prevention: The National Health and Nutrition Examination Surveys (NHANES), 1999–2012. J Am Heart Assoc. 2015;4(4). doi: 10.1161/JAHA.114.001709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Targher G, Bertolini L, Padovani R, et al. Prevalence of nonalcoholic fatty liver disease and its association with cardiovascular disease among type 2 diabetic patients. Diabetes Care. 2007;30:1212–1218 [DOI] [PubMed] [Google Scholar]
- 33.Al Rifai M, Silverman MG, Nasir K, et al. The association of nonalcoholic fatty liver disease, obesity, and metabolic syndrome, with systemic inflammation and subclinical atherosclerosis: The Multi-Ethnic Study of Atherosclerosis (MESA). Atherosclerosis. 2015;239:629–633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Targher G, Bertolini L, Scala L, et al. Non-alcoholic hepatic steatosis and its relation to increased plasma biomarkers of inflammation and endothelial dysfunction in non-diabetic men. Role of visceral adipose tissue. Diabet Med. 2005;22:1354–1358 [DOI] [PubMed] [Google Scholar]
- 35.Lee HJ, Lee CH, Kim S, et al. Association between vascular inflammation and non-alcoholic fatty liver disease: Analysis by 18f-fluorodeoxyglucose positron emission tomography. Metabolism. 2017;67:72–79 [DOI] [PubMed] [Google Scholar]
- 36.VanWagner LB, Ning H, Lewis CE, et al. Associations between nonalcoholic fatty liver disease and subclinical atherosclerosis in middle-aged adults: The Coronary Artery Risk Development In young Adults Study. Atherosclerosis. 2014;235:599–605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sinn DH, Kang D, Chang Y, et al. Non-alcoholic fatty liver disease and progression of coronary artery calcium score: A retrospective cohort study. Gut. 2017;66:323–329 [DOI] [PubMed] [Google Scholar]
- 38.Wong VW, Wong GL, Yeung JC, et al. Long-term clinical outcomes after fatty liver screening in patients undergoing coronary angiogram: A prospective cohort study. Hepatology. 2016;63:754–763 [DOI] [PubMed] [Google Scholar]
- 39.Kim J, Lee DY, Park SE, et al. Increased risk for development of coronary artery calcification in subjects with non-alcoholic fatty liver disease and systemic inflammation. PLoS One. 2017;12:e0180118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Madan SA, John F, Pyrsopoulos N, et al. Nonalcoholic fatty liver disease and carotid artery atherosclerosis in children and adults: A meta-analysis. Eur J Gastroenterol Hepatol. 2015;27:1237–1248 [DOI] [PubMed] [Google Scholar]
- 41.Tripodi A, Primignani M, Chantarangkul V, et al. An imbalance of pro- vs anti-coagulation factors in plasma from patients with cirrhosis. Gastroenterology. 2009;137:2105–2111 [DOI] [PubMed] [Google Scholar]
- 42.Lonardo A, Ballestri S, Targher G. “Not all forms of nafld were created equal”. Do metabolic syndrome-related nafld and pnpla3-related nafld exert a variable impact on the risk of early carotid atherosclerosis? Atherosclerosis. 2017;257:253–255 [DOI] [PubMed] [Google Scholar]