Abstract
Ipilimumab is effective for patients with melanoma, but not for those with less immunogenic tumors. We report a phase II trial of ipilimumab with concurrent or sequential stereotactic ablative radiation therapy to metastatic lesions in the liver or lung (). Ipilimumab (every 3 weeks for 4 doses) was given with radiotherapy begun during the first dose (concurrent) or one week after the second dose (sequential) and delivered as 50 Gy in 4 fractions or 60 Gy in 10 fractions to metastatic liver or lung lesions. In total, 106 patients received ≥1 cycle of ipilimumab with radiation. Median follow-up was 10.5 months. Median progression-free survival time was 2.9 months (95% confidence interval 2.45–3.40) and median overall survival time was not reached. Rates of clinical benefit of nonirradiated tumor volume were 26% overall, 28% for sequential versus 20% for concurrent therapy (P=0.250) and 31% for lung versus 14% for liver metastases (P=0.061). The sequential lung group had the highest rate of clinical benefit at 42%. There were no differences in treatment-related adverse events between groups. Exploratory analysis of non-targeted lesions revealed that lesions receiving low-dose radiation were more likely to respond than those that received no radiation (31% vs 5%, P=0.0091).
Keywords: Stereotactic ablative radiation therapy, ipilimumab, radiotherapy, immunotherapy, cancer
Introduction
Improved understanding of the immune system’s role in cancer has reinvigorated research on the interplay between radiation and immunotherapies in cancer. Preclinical evidence has shown that radiation can increase T-cell priming and tumor-specific antigen presentation (1,2). Checkpoint inhibitors such as the CTLA4 antagonist ipilimumab prime the immune system and prevent T-cell exhaustion. Combining the tumor-specific immunogenic properties of local radiation therapy with the systemic effects of immunotherapy can significantly reduce disease outside the radiation field, a phenomenon known as the abscopal effect (3).
Although synergistic effects of radiation and immunotherapy have been amply demonstrated in preclinical models (2–5), to our knowledge clinical trials have yet to address critical factors such as the most effective sequence of therapies and radiation dosage. High-dose hypofractionated radiation in the form of stereotactic ablative radiotherapy (SABR) can cause immunogenic cell death, although higher doses can lead to increased toxicity (6,7). We previously addressed such concerns in the phase I portion of our phase I/II study of combining SABR with ipilimumab ()(8). Here, we present our phase II findings from a 5-arm nonrandomized phase II “basket” trial of SABR with either concurrent or sequential CTLA4 blockade with ipilimumab for patients with liver or lung metastases from non-melanoma cancers after previous failure of standard therapies.
Methods
Patients
Eligible patients were ≥18 years old with histologic confirmation of non-melanoma, metastatic cancer with at least one metastatic lesion in the liver, lung, or adrenal glands amenable to SABR and at least one additional non-contiguous lesion. Prior receipt of radiation to the same lung or liver field was allowed at the discretion of the treating physician. All patients were required to have a baseline performance status score of ≤2 on the Eastern Cooperative Oncology Group (ECOG) scale (Karnofsky score of ≥60). Patients with brain metastases or those requiring emergent treatment were excluded.
Trial Design and Treatment
In this single-institution phase II parallel-treatment study, patients were assigned to one of the five treatment groups based on tumor size and location. All participants received ipilimumab at a dose of 3 mg/kg given every 21 days for a total of 4 doses. Patients assigned to Groups 1 or 2 received concurrent or sequential ipilimumab with SABR to 50 Gy given in 4 fractions (corresponding to 60 Gy to the gross tumor volume [GTV]) to 1 liver lesion. Patients assigned to Groups 3 or 4 received concurrent or sequential ipilimumab with SABR to 50 Gy in 4 fractions (60 Gy to the GTV) to 1 lung lesion. The fifth group (for tumors that could not be treated safely with 50 Gy in 4 fractions, i.e., large or centrally located tumors) received sequential ipilimumab and SABR for lung, liver, or adrenal lesions to a total dose of 60 Gy (to the GTV) in 10 fractions. Therapy was considered concurrent when the SABR was begun within 1 day after the first dose of ipilimumab; therapy was sequential when SABR was begun 7–10 days after the second dose of ipilimumab.
Data were analyzed after the phase II portion of the trial had fully accrued and all patients had a minimum follow-up time of 3 months. The primary endpoint, assessed upon completion of the phase II portion of the trial, was toxicity. Secondary endpoints included in-field (RT treated lesions) and out-of-field (lesions that received no intentional RT) responses, which we separately (for both in-field and out-of-field lesions) analyzed according to the Immune-Related Response Criteria (irRC) guidelines (9), progression-free survival (PFS), and overall survival (OS). Adverse events were scored per the Common Terminology Criteria for Adverse Events (CTCAE) v 4.0 and were evaluated by medical and radiation oncologists.
Response Assessments
Disease response and progression were evaluated according to the irRC (9). We evaluated global response (i.e., complete response [CR], partial response [PR], or stable disease [SD] of both irradiated and un-irradiated lesions), in-field response (response of only the irradiated lesions), and out-of-field response (response of only the non-irradiated lesions). Tumor growth and disease progression were assessed according to the irRC at the end of every second study cycle and at 2–3 months after completion of the last ipilimumab cycle. The imaging modality used in these assessments was the same as that used before treatment, typically computed tomography (CT) of the chest, abdomen, or pelvis or positron emission tomography (PET/CT).
Trial Oversight
The study protocol and amendments were approved by MD Anderson’s institutional review board. All patients provided written informed consent before enrollment.
Statistical Analysis
The endpoints for this parallel-arm “basket” trial were toxicity and out-of-field response. “Clinical benefit” was defined as CR, PR, or SD in accordance with the irRC system. Each patient’s best response was selected for analysis. Toxicity and efficacy were compared between the concurrent-therapy versus the concurrent-therapy groups with Pearson chi-squared or Fisher exact tests. To compare sequential versus concurrent therapy, the plan was to recruit 60 patients to a sequential group and 40 patients to a concurrent group, which allowed 80% power using a two-sided alpha of 5%. Time-to-event analyses were done with the Kaplan-Meier method. PFS and OS intervals were measured from the date of enrollment to the event of interest.
Results
Patient Characteristics
A total of 119 patients were enrolled from September 2014 through March 2017; 13 of these patients were excluded (2 did not meet the eligibility criteria, 7 withdrew consent, 1 died before starting treatment, 1 did not receive financial clearance, and 2 were erroneously registered twice) (Supplementary Fig. S1). The remaining 106 patients (89%) all received at least one cycle of ipilimumab; 60 patients (57%) received all 4 ipilimumab cycles, and 98 patients (92%) completed the radiation treatment.
The median age of the 106 treated patients was 60 years (range 20–82); 50 (47%) were men and 56 (53%) women (Supplementary Table S1). The most common tumor histologic types were adenocarcinoma (n=57, 54%) followed by squamous cell carcinoma (n=13, 12%), and the most common primary tumor sites were lung (n=30 [28%]), gastrointestinal tract (n=20 [19%]) and head and neck (n=19 [18%]). Ninety-seven patients (91%) had received prior systemic therapy (median 3, range 0–8); 66 (62%) had received prior radiation therapy for metastatic disease; and 17 patients (16%) had received prior immunotherapy (Supplementary Table S1).
Toxicity
Adverse events attributable to either radiation or immunotherapy are shown in Table 1. All events recorded were grade ≤3 by CTCAE v 4.0; no patient experienced grade 4 or 5 treatment-related toxicity. Among all grade 3 events, the most common was diarrhea (6 patients [6%]), followed by ALT/AST elevation and skin rash (5 patients [5%]). Four patients experienced grade 3 respiratory-related events (2 dyspnea, 1 chest pain, 1 pneumonitis) in the lung-lesion treatment groups (2 in the concurrent group and 2 in the sequential group).
Table 1.
Toxicity probably or definitely related to radiation or immunotherapy*
| Grade 1–2 | -----------------------------------------------Grade 3----------------------------------------------- | ||||||
|---|---|---|---|---|---|---|---|
| Characteristics | All Patients (n=106) | All Patients (n=106) | Group 1: Liver 50/4** Concurrent (n=20) | Group 2: Liver 50/4 Sequential (n=22) | Group 3: Lung 50/4 Concurrent (n=21) | Group 4: Lung 50/4 Sequential (n=24) | Group 5: Liver, Lung, or Adrenal 60/10 Sequential (n=19) |
| ALT/AST elevation | 5 (4.7%) | 5 (4.7%) | 1 (0.9%) | 0 | 0 | 1 (0.9%) | 3 (2.8%) |
| Bilirubin elevation | – | 2 (1.8%) | 0 | 2 (1.8%) | 0 | 0 | 0 |
| Colitis | 1 (0.9%) | 2 (1.8%) | 0 | 1 (0.9%) | 0 | 0 | 1 (0.9%) |
| Cholecystitis | – | 1 (0.9%) | 0 | 0 | 0 | 1(0.9%) | 0 |
| Diarrhea | 17 (16%) | 6 (5.6%) | 0 | 1 (0.9%) | 0 | 0 | 5 (4.7%) |
| Constipation | 2 (1.8%) | 1 (0.9%) | 0 | 0 | 0 | 0 | 1 (0.9%) |
| Fatigue | 34 (32%) | 1 (0.9%) | 0 | 1 (0.9%) | 0 | 0 | 0 |
| Fever | 6 (5.6%) | 1 (0.9%) | 0 | 0 | 0 | 0 | 1 (0.9%) |
| Pain | 13 (12%) | 2 (1.8%) | 0 | 1 (0.9%) | 1 (0.9%) | 0 | 0 |
| Pancreatitis/lipase elevation | – | 1 (0.9%) | 1 (0.9%) | 0 | 0 | 0 | 0 |
| Pituitary hypophysitis | – | 3 (2.8%) | 0 | 1 (0.9%) | 0 | 1 (0.9%) | 1 (0.9%) |
| TSH elevation | 3 (2.8%) | 1 (0.9%) | 0 | 0 | 0 | 1 (0.9%) | 0 |
| Pneumonitis | 2 (1.8%) | 1 (0.9%) | 0 | 0 | 0 | 1 (0.9%) | 0 |
| Chest pain | – | 1 (0.9%) | 0 | 0 | 1 (0.9%) | 0 | 0 |
| Dyspnea | 12 (11%) | 2 (1.8%) | 0 | 0 | 1 (0.9%) | 1 (0.9%) | 0 |
| Rash, maculopapular | 32 (30%) | 5 (4.7%) | 0 | 3 (2.8%) | 2 (1.8%) | 0 | 0 |
| Upper muscle weakness | 4 (3.7%) | 1 (0.9%) | 0 | 0 | 1 (0.9%) | 0 | 0 |
| Sensory neuropathy | 9 (8.5%) | – | – | – | – | – | – |
No patient experienced grade 4 or 5 toxicity probably or definitely related to treatment.
Indicates the radiation dose (in Gy) / number of fractions.
Abbreviations: ALT, alanine aminotransferase; AST, aspartate aminotransferase; TSH, thyroid-stimulating hormone.
Outcomes
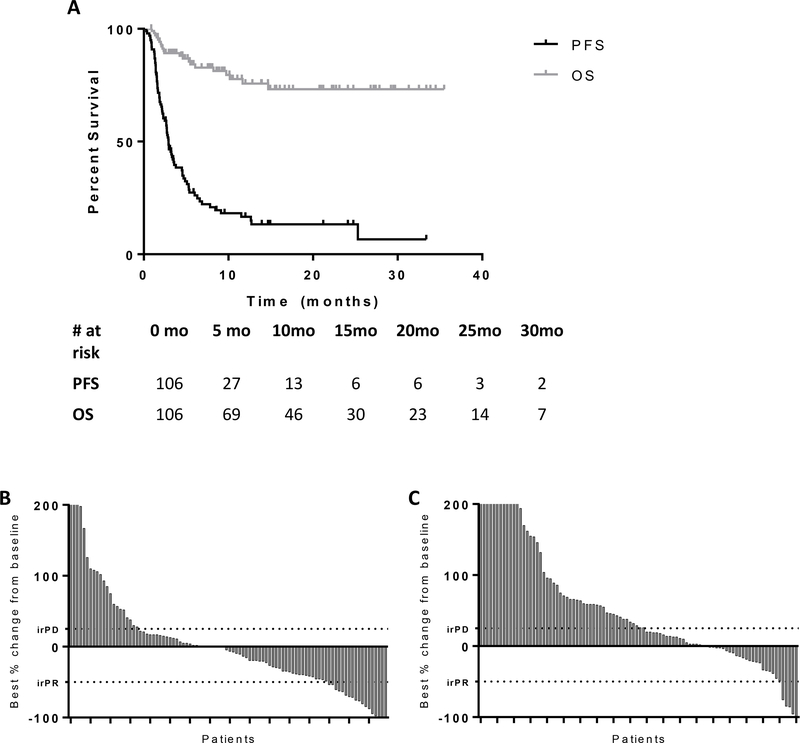
Among all 106 evaluable patients, the median follow-up time was 10.5 months, the median PFS time was 2.93 months (95% confidence interval [CI], 2.45–3.40), and the median OS time was not reached (Fig. 1A). The 1-year, 2-year, and 3-year OS rates were 76% (95% CI 67.4–87.1), 73% (95% CI 64.3–85.6), and 73% (95% CI 64.3–85.6). The best responses of in-field (irradiated) and out-of-field (unirradiated) disease sites are shown in Figure 1B and 1C. As expected, irradiated lesions were reasonably controlled (radiation-induced fibrosis may have precluded accurate analysis), and even unirradiated lesions responded well in about one-third of cases (Fig. 1C).
Figure 1.
A, Overall survival (OS) and progression-free survival (PFS) for the 106 evaluable patients. B, change in volume of targeted (irradiated) lesion with best response during protocol C, change in volume of single unirradiated lesion with best response per patient, during protocol. For reference, cut-off points from the Immune-Related Response Criteria (irRC) guidelines are provided in the waterfall plots for partial response (irPR) and progressive disease (irPD).
Clinical benefit, defined by the irRC as CR, PR, or SD lasting 6 months or more, was achieved by 26% of the 95 patients with evaluable images. Table 2 reports the complete outcomes of all patients and Supplemental Table S2 provides a breakdown of responses by stereotactic target site and histology. Patients who received sequential ipilimumab and SABR to 50 Gy in 4 fractions to lung metastases had the highest clinical benefit rate at 42% (95% CI, 20.3–66.5), whereas patients who received concurrent ipilimumab and radiation to 50 Gy in 4 fractions to liver lesions had the lowest at 5%. The clinical benefit rate among treated for lung lesions was 31% as compared with 14% for those treated for liver lesions (P=0.061); clinical benefit rates were 28% for those who received sequential treatment versus 20% for those who received concurrent treatment (P=0.250) (Table 2).
Table 2.
Response Rates of Unirradiated Tumors by Treatment, Target, or Treatment Sequence
| irRC Response Category, n (%) | |||||
|---|---|---|---|---|---|
| CR | PR | SD | PD | P Value* | |
| All patients | 2 (2) | 7 (7) | 16(17) | 70 (74) | |
| By treatment group | |||||
| Liver 50/4 concurrent | 0 | 1 (5) | 0 | 18 (95) | |
| Liver 50/4 sequential | 0 | 1 (6) | 4 (24) | 12 (70) | |
| Lung 50/4 concurrent | 1 (5) | 2 (9) | 4 (19) | 14 (67) | |
| Lung 50/4 sequential | 1 (5) | 1 (5) | 6 (32) | 11 (58) | |
| Liver or lung 60/10 sequential | 0 | 2 (11) | 2 (11) | 15 (78) | |
| By stereotactic target | 0.061 | ||||
| Liver | 0 | 3 (6) | 4 (11) | 36 (83) | |
| Lung | 2 (5) | 4 (7) | 12 (25) | 34 (63) | |
| By treatment sequence | 0.250 | ||||
| Concurrent | 1 (2) | 3 (8) | 4 (10) | 32 (80) | |
| Sequential | 1 (2) | 4 (7) | 12 (22) | 38 (69) | |
Abbreviations: irRC, Immunotherapy-Related Response Criteria; CR, complete response; PR, partial response; SD, stable disease; PD, progressive disease; SCC, Squamous cell carcinoma.
Reported P value compares clinical benefit (defined as CR, PR, or SD) at 6 months between the concurrent therapy versus sequential therapy groups.
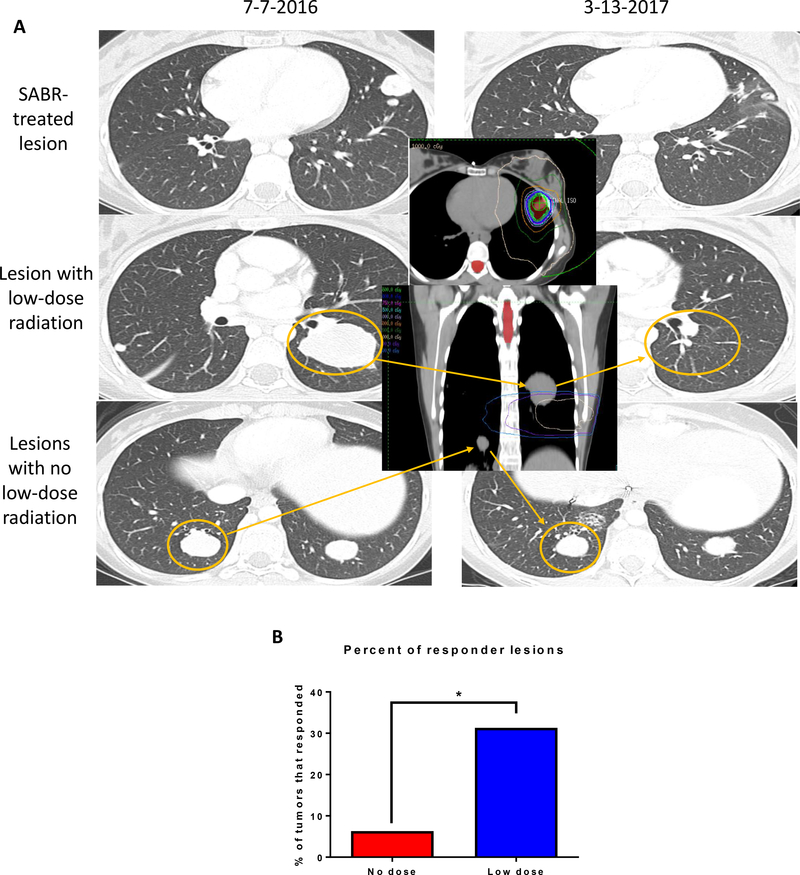
Low-Dose Radiation and Out-of-Field Responses
Following the occurrence of mixed responses in several patients, it was anecdotally observed that many responding lesions received low-dose radiation, whereas other tumors (in the same patient) that had received no radiation either stayed stable or grew. As a result, we undertook an exploratory analysis regarding the effect of low-dose radiation on out-of-field responses. Although out-of-field response was a prespecified endpoint of this trial, low-dose radiation was not delivered intentionally, and rather was solely related to anatomic proximity to another irradiated site. While there may have been marginal shifts of lesion position between planning and treatment, which would affect the precise amount of low-dose radiation received, we believe this is only a small limitation of our analysis.
Responses of a representative patient with metastatic fibrolamellar hepatocellular carcinoma are shown in Figure 2A. That patient received ipilimumab with sequential SABR to 50 Gy in 4 fractions to a metastatic lesion in the left upper lobe of the lung. Imaging 6 months after SABR revealed not only response in the irradiated lesions, but near-complete resolution of a large lesion in the left lower lobe (Fig. 2A, middle row). As depicted in the treatment plan (Fig. 2A, inset), the large lesion was outside the SABR field but was exposed to low-dose radiation. However, two other lesions completely outside the low-dose field did not respond (Fig. 2A, bottom row). To investigate further, we analyzed the percentage of unirradiated lesions in all patients with a tumor response (defined per the irRC as a decrease in tumor volume of ≥50% from baseline), and found that 31% of lesions that received low-dose radiation (i.e., 5–10 Gy) responded, whereas only 5% of lesions that received no radiation responded (P=0.0091) (Fig. 2B).
Figure 2.
A, Scans from a patient with fibrolamellar hepatocellular carcinoma who received sequential radiation and ipilimumab to a metastatic lesion in the left upper lobe of the lung. At 6 months after treatment, the in-field lesion (i.e., that which received SABR 50 Gy in 4 fractions) had completely resolved (top row). A large lesion that received low-dose radiation (mean dose 305 cGy) also resolved (middle row), but several other lesions in the lower lungs, outside the radiation field, did not respond (bottom row). B, Responding out-of-field lesions that that received low-dose radiation (n=16) or no low-dose radiation (n=95). Response was defined as a decrease in tumor volume of at least 50%. Fisher’s exact P=0.0091.
Discussion
The results of this phase II trial demonstrate that administration of SABR and ipilimumab (concurrently or sequentially) is safe and effective for patients with metastatic cancer. These prospective results add to the growing literature demonstrating interactions between these two modalities, and should serve as the basis for many future investigations looking to exploit the immune system for anti-tumoral benefits.
The results of this study mirror encouraging recent publications. Formenti and colleagues studied chemotherapy-refractory metastatic non-small cell lung cancer and observed improved responses with ipilimumab and radiotherapy (objective response 18%, disease control 31%) as compared to figures of ipilimumab alone (10). These are similar to the objective response of 13% as documented in a recent phase I study by Luke et al (11), which utilized pembrolizumab.
Previously, we found higher percentage of peripheral CD8+ T cells and in the CD8+/CD4+ ratio after the first 1 to 2 doses of ipilimumab and SABR among patients who achieved clinical benefit. Clinical benefit was also associated with an increased proportion of CD8+ T cells expressing 4–1BB and PD1. Our previous results also showed that sequencing of therapy did not promote differences in T cell activation, but substantial differences were observed after hepatic versus lung irradiation. Hepatic radiation was associated with increased percentages of CD8+ T cells expressing ICOS, GITR, and LAG3 and increased percentages of CD4+ Treg cells expressing 4–1BB, GITR, TIM-3, and PD1 (8). Although our current trial was not powered to address other endpoints such as concurrent versus sequential therapy (suggesting that dedicated studies with longer follow-up are required) (12–14), a stronger trend herein for clinical benefit in lung lesions (relative to liver) merits discussion. Due to the design of this trial, patients in Groups 1 and 2 (liver-targeted radiation) all had liver metastases at baseline, but only a fraction of patients in Groups 3 and 4 (lung-targeted radiation) had liver metastases at baseline (Supplemental Table S3). Because this is merely an anecdotal observation, mechanisms must be further elucidated. For instance, it is possible that tumor biological factors associated with seeding the hepatic parenchyma are associated with reduced immunogenicity and/or even prognosis; however, just as important may be factors inherent to the liver cytoarchitecture and/or microenvironment. Additionally, whether particular immune checkpoint agents and/or SABR dosing play a role in this phenomenon also remain unresolved. Hence, in the absence of known mechanisms or modifying factors, there are few evidence-based measures that may be taken in efforts to manipulate one of several factors designed to improve response rates of liver disease.
The finding with regard to low-dose radiation also beckons a presumptive and speculative explanation, which is also not firmly backed by a high-quality evidence base. Radiation in this trial could have augmented the immune response via two unique mechanisms: in one mechanism, high-dose radiation would cause release of tumor neoantigens that assist in T-cell priming and repertoire diversity (1), and in the other mechanism, low-dose radiation would address the tumor stroma and microenvironment so as to allow activated T cells to penetrate the tumor. Preclinical studies have shown that low-dose radiation (i.e., ≤2 Gy/fraction) can stimulate residential immune cells and enable T-cell homing (15,16). This immune modulation provided by low-dose radiation has been posited before but has not been shown in a clinical setting (17). Additionally other strategies, such as ADscopal, which consists of partially irradiating large tumors, have also shown to stimulate responses which further provides rationale for low-doses of radiation(18). However, we believe the combination of high and low radiation doses with immunotherapy may synergistically generate tumor-specific immune responses with enhanced systemic antitumor outcomes.
One of the major obstacles for immunotherapy is the tumor stroma and associated macrophages, which causes T-cell anergy and prevents T-cells from migrating into the tumor (19). Our post hoc analysis that revealed non-targeted lesions receiving low-dose radiation were more likely to respond could reflect the ability of low-dose radiation to reprogram the tumor microenvironment to directly stimulate or activate incoming immune cells (15,16,20,21). The abundance of tumor promoting M2 macrophages in the tumor microenvironment leads to the production of immune inhibitory cytokines such as IL-4, TGF-β, and the vascular endothelial growth factor (VEGF). Preclinical findings recently revealed that low-dose radiation can shift the tumor microenvironment towards an M1/Th1 phenotype through induced nitric oxide synthase (iNOS) production (22). We believe the combination of high-dose radiation (which “primes” T cells), low-dose radiation at secondary sites (which “pulls in” and activates T cells), and systemic immunotherapy, results in a response that is distinctly different from the traditional abscopal response, in which distant sites are not exposed to radiation. However, in the absence of further evidence for this “low dose” phenomenon, these mechanisms and explanations must remain theoretical.
With regard to radiation dosage, few reports of outcomes after hypofractionated radiation with immunotherapy are available at this time, although some preclinical evidence suggests that delivering higher doses may be more immunogenic than delivering the same dose in multiple smaller fractions (1, 23). In a preclinical study, murine colon tumors showed complete remission when treated with a single radiation dose of 30 Gy, but a 3 Gy x 10 day fraction scheme failed to induce remission of the tumor and resulted in decreased survival and metastatic spread, along with marked reduction of CD8+ T-cells in the tumor infiltrate (23). Higher doses of radiation have also been associated with increased MHC class I expression (1). However, Vanpouille-Box and colleagues reported that Trex1, a DNA exonuclease, is activated by radiation doses ranging 12 to 18 Gy (in different cell lines) in a single fraction, but not by using radiation fractions with doses below this threshold (24). Activation of Trex1 resulted in the degradation of cytosolic DNA, which is essential in activating the cGAS-STING pathway to induce secretion of interferon-β, dendritic cell activation, CD8+ T-cell priming, and abscopal responses (24). Therefore, treating a tumor with a dose of radiation above the threshold for Trex1 induction would lead to insufficient dendritic cell recruitment and blunted CD8+ T-cell activation, resulting in reduced abscopal tumor responses in conjunction with immune checkpoint inhibitors. However, it is important to note that the threshold for Trex1 induction varies by cell line and dose thresholds for primary human tumors will likely differ. Further clinical studies are required to elucidate the optimal dose and fractionation for the variety of tumor types in this trial, and the dose used in this trial (12.5 Gy per fraction) may have exceeded the Trex1 induction threshold for some tumor types. In sum, hypofractionated radiation is double-edged in that it may simultaneously up-regulate and down-regulate immune responses via different pathways, an important consideration for future trials.
Another important consideration in interpreting our results is the nature of this non-traditional, nonrandomized “basket” trial design, in which the participants had heterogeneous primary tumor types, treatment timing, and irradiated sites. Although the heterogeneity of our patients could be viewed as a weakness, the primary purpose of this trial was to assess the safety and effectiveness of combining ipilimumab with radiation therapy. For these purposes, a diverse study cohort is actually a strength in that it shows that this combination was indeed safe and effective for many types of tumor histologic types. Another way in which the heterogeneity of our patients could be viewed as a strength was the large number of patients who achieved SD or PR, considering that most had already experienced disease progression during first- and second-line therapies before enrolling in this trial. This diversity, coupled with the limited numbers of patients (about 20) per treatment arm, may have contributed to the lack of statistical significance in our findings. However, randomization in this 5-arm study was not possible; two groups received radiation to lung tumors, two groups to liver tumors, and a fifth group had tumors that were too large or too centrally located to safely undergo SABR.
Supplementary Material
Synopsis.
This phase II trial of ipilimumab with stereotactic radiotherapy describes satisfactory outcomes and low toxicities, lending support to further investigation of combined-modality therapy for metastatic cancers.
Acknowledgments
This work was supported by the family of M. Adnan Hamed, the Susan and Peter Goodwin Foundation, Mabuchi Research fund, and the Orr Family Foundation (to MD Anderson Cancer Center’s Thoracic Radiation Oncology program), and the Wiegand Foundation. We also have support the from the MD Anderson Knowledge Gap award, Doctors Cancer Foundation Grant, The Lung Cancer Research Foundation, and the Cancer Center Support (Core) Grant CA016672 from the National Cancer Institute (to The University of Texas MD Anderson Cancer Center).
Support: Bristol Myers Squibb provided funding and access to ipilimumab; and other support was provided by the Cancer Center Support (Core) Grant CA016672 from the National Cancer Institute, National Institutes of Health to The University of Texas MD Anderson Cancer Center.
Declaration of Interest
JWW, JYC, DRG and DSH have received research grants from Bristol-Myers Squibb. JWW and DRG have received grants from Merck. JWW has also received research support from GlaxoSmithKline, Nanobiotix, Mavu Pharma, and Checkmate Pharmaceuticals; he also is a co-founder of Healios, MolecularMatch, and OncoResponse; he is on the scientific advisor board of Reflexion Medical, MolecularMatch, OncoResponse, Mavu Pharma, and Alpine Immune Sciences; he also serves as an advisor to Astra Zeneca, Merck, MolecularMatch, Incyte, Aileron, and Nanobiotix. JWW has the following patents; MP470 (amuvatinib), MRX34 regulation of PDL1, XRT technique to overcome immune resistance. MD Anderson Cancer Center has a trademark for RadScopal™. DSH has received grants from Merck, Daichii-Sanko, Esai, Adaptimmune, AbbVie, AstraZeneca, Genmab, Infinifty, Kite, Kyowa, Medimmune, Molecular Template, and Novartis. DSH has received travel accommodations from Mirna and LOXO; he has a consulting/advisory role for Bayer, Baxter, Janssen, MolecularMatch and Guidepoint Global. JWW and DSH have ownership interest in OncoResponse. VAP and RD are advisory board members for Bristol-Myers Squibb. VS has received research grants from Novartis, Bayer, Roche/Genentech, LOXO, and Blueprint Medicines. JYC is a shareholder of Global Oncology One. EM is the principal investigator on another Bristol-Myers Squibb trial. PS is a consultant for Merck and Astellas, and owns stock in Jounce, Kite Pharma, Constellation, and Neon.
References
- 1.Reits EA, Hodge JW, Herberts CA, Groothuis TA, Chakraborty M, Wansley EK, et al. Radiation modulates the peptide repertoire, enhances MHC class I expression, and induces successful antitumor immunotherapy. The Journal of experimental medicine 2006;203(5):1259–71 doi 10.1084/jem.20052494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Twyman-Saint Victor C, Rech AJ, Maity A, Rengan R, Pauken KE, Stelekati E, et al. Radiation and dual checkpoint blockade activate non-redundant immune mechanisms in cancer. Nature 2015;520(7547):373–7 doi 10.1038/nature14292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Demaria S, Ng B, Devitt ML, Babb JS, Kawashima N, Liebes L, et al. Ionizing radiation inhibition of distant untreated tumors (abscopal effect) is immune mediated. International journal of radiation oncology, biology, physics 2004;58(3):862–70 doi 10.1016/j.ijrobp.2003.09.012. [DOI] [PubMed] [Google Scholar]
- 4.Demaria S, Kawashima N, Yang AM, Devitt ML, Babb JS, Allison JP, et al. Immune-mediated inhibition of metastases after treatment with local radiation and CTLA-4 blockade in a mouse model of breast cancer. Clinical cancer research : an official journal of the American Association for Cancer Research 2005;11(2 Pt 1):728–34. [PubMed] [Google Scholar]
- 5.Lee Y, Auh SL, Wang Y, Burnette B, Wang Y, Meng Y, et al. Therapeutic effects of ablative radiation on local tumor require CD8+ T cells: changing strategies for cancer treatment. Blood 2009;114(3):589–95 doi 10.1182/blood-2009-02-206870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chang JY, Li QQ, Xu QY, Allen PK, Rebueno N, Gomez DR, et al. Stereotactic ablative radiation therapy for centrally located early stage or isolated parenchymal recurrences of non-small cell lung cancer: how to fly in a “no fly zone”. International journal of radiation oncology, biology, physics 2014;88(5):1120–8 doi 10.1016/j.ijrobp.2014.01.022. [DOI] [PubMed] [Google Scholar]
- 7.Timmerman R, McGarry R, Yiannoutsos C, Papiez L, Tudor K, DeLuca J, et al. Excessive toxicity when treating central tumors in a phase II study of stereotactic body radiation therapy for medically inoperable early-stage lung cancer. Journal of clinical oncology : official journal of the American Society of Clinical Oncology 2006;24(30):4833–9 doi 10.1200/JCO.2006.07.5937. [DOI] [PubMed] [Google Scholar]
- 8.Tang C, Welsh JW, de Groot P, Massarelli E, Chang JY, Hess KR, et al. Ipilimumab with Stereotactic Ablative Radiation Therapy: Phase I Results and Immunologic Correlates from Peripheral T Cells. Clinical cancer research : an official journal of the American Association for Cancer Research 2017;23(6):1388–96 doi 10.1158/1078-0432.CCR-16-1432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wolchok JD, Hoos A, O’Day S, Weber JS, Hamid O, Lebbe C, et al. Guidelines for the evaluation of immune therapy activity in solid tumors: immune-related response criteria. Clinical cancer research : an official journal of the American Association for Cancer Research 2009;15(23):7412–20 doi 10.1158/1078-0432.CCR-09-1624. [DOI] [PubMed] [Google Scholar]
- 10.Formenti SC, Rudqvist NP, Golden E, Cooper B, Wennerberg E, Lhuillier C, et al. Radiotherapy induces responses of lung cancer to CTLA-4 blockade. Nature medicine 2018;24(12):1845–51 doi 10.1038/s41591-018-0232-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Luke JJ, Lemons JM, Karrison TG, Pitroda SP, Melotek JM, Zha Y, et al. Safety and Clinical Activity of Pembrolizumab and Multisite Stereotactic Body Radiotherapy in Patients With Advanced Solid Tumors. Journal of clinical oncology : official journal of the American Society of Clinical Oncology 2018;36(16):1611–8 doi 10.1200/jco.2017.76.2229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cushman TR, Caetano MS, Welsh JW, Verma V. Overview of ongoing clinical trials investigating combined radiotherapy and immunotherapy. Immunotherapy 2018;10(10):851–0 doi 10.2217/imt-2018-0019. [DOI] [PubMed] [Google Scholar]
- 13.Verma V, Cushman TR, Selek U, Tang C, Welsh JW. Safety of Combined Immunotherapy and Thoracic Radiation Therapy: Analysis of 3 Single-Institutional Phase I/II Trials. International journal of radiation oncology, biology, physics 2018;101(5):1141–8 doi 10.1016/j.ijrobp.2018.04.054. [DOI] [PubMed] [Google Scholar]
- 14.Verma V, Cushman TR, Tang C, Welsh JW. Toxicity of radiation and immunotherapy combinations. Advances in radiation oncology 2018;3(4):506–11 doi 10.1016/j.adro.2018.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bogdandi EN, Balogh A, Felgyinszki N, Szatmari T, Persa E, Hildebrandt G, et al. Effects of low-dose radiation on the immune system of mice after total-body irradiation. Radiat Res 2010;174(4):480–9 doi 10.1667/RR2160.1. [DOI] [PubMed] [Google Scholar]
- 16.Safwat A The role of low-dose total body irradiation in treatment of non-Hodgkin’s lymphoma: a new look at an old method. Radiother Oncol 2000;56(1):1–8. [DOI] [PubMed] [Google Scholar]
- 17.Hodge JW, Guha C, Neefjes J, Gulley JL. Synergizing radiation therapy and immunotherapy for curing incurable cancers. Opportunities and challenges. Oncology (Williston Park) 2008;22(9):1064–84. [PMC free article] [PubMed] [Google Scholar]
- 18.Lemons JM, Luke JJ, Janisch L, Hseu R, Melotek JM, Chmura SJ. The ADscopal Effect? Control of Partially Irradiated Versus Completely Irradiated Tumors on a Prospective Trial of Pembrolizumab and SBRT Per NRG-BR001. International Journal of Radiation Oncology • Biology • Physics 2017;99(2):S87 doi 10.1016/j.ijrobp.2017.06.209. [DOI] [Google Scholar]
- 19.Peranzoni E, Lemoine J, Vimeux L, Feuillet V, Barrin S, Kantari-Mimoun C, et al. Macrophages impede CD8 T cells from reaching tumor cells and limit the efficacy of anti-PD-1 treatment. Proceedings of the National Academy of Sciences of the United States of America 2018;115(17):E4041–e50 doi 10.1073/pnas.1720948115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim RK, Kim MJ, Seong KM, Kaushik N, Suh Y, Yoo KC, et al. Beneficial effects of low dose radiation in response to the oncogenic KRAS induced cellular transformation. Scientific reports 2015;5:15809 doi 10.1038/srep15809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Matsubara J, Turcanu V, Poindron P, Ina Y. Immune effects of low-dose radiation: short-term induction of thymocyte apoptosis and long-term augmentation of T-cell-dependent immune responses. Radiat Res 2000;153(3):332–8. [DOI] [PubMed] [Google Scholar]
- 22.Klug F, Prakash H, Huber PE, Seibel T, Bender N, Halama N, et al. Low-dose irradiation programs macrophage differentiation to an iNOS(+)/M1 phenotype that orchestrates effective T cell immunotherapy. Cancer cell 2013;24(5):589–602 doi 10.1016/j.ccr.2013.09.014. [DOI] [PubMed] [Google Scholar]
- 23.Filatenkov A, Baker J, Mueller AM, Kenkel J, Ahn GO, Dutt S, et al. Ablative Tumor Radiation Can Change the Tumor Immune Cell Microenvironment to Induce Durable Complete Remissions. Clinical cancer research : an official journal of the American Association for Cancer Research 2015;21(16):3727–39 doi 10.1158/1078-0432.CCR-14-2824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vanpouille-Box C, Alard A, Aryankalayil MJ, Sarfraz Y, Diamond JM, Schneider RJ, et al. DNA exonuclease Trex1 regulates radiotherapy-induced tumour immunogenicity. Nature communications 2017;8:15618 doi 10.1038/ncomms15618. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.