Abstract
Objective
To determine associations between important pre-arrest and intra-arrest prognostic factors and survival after in-hospital cardiac arrest.
Design
Systematic review and meta-analysis.
Data sources
Medline, PubMed, Embase, Scopus, Web of Science, and the Cochrane Database of Systematic Reviews from inception to 4 February 2019. Primary, unpublished data from the United Kingdom National Cardiac Arrest Audit database.
Study selection criteria
English language studies that investigated pre-arrest and intra-arrest prognostic factors and survival after in-hospital cardiac arrest.
Data extraction
PROGRESS (prognosis research strategy group) recommendations and the CHARMS (critical appraisal and data extraction for systematic reviews of prediction modelling studies) checklist were followed. Risk of bias was assessed by using the QUIPS tool (quality in prognosis studies). The primary analysis pooled associations only if they were adjusted for relevant confounders. The GRADE approach (grading of recommendations assessment, development, and evaluation) was used to rate certainty in the evidence.
Results
The primary analysis included 23 cohort studies. Of the pre-arrest factors, male sex (odds ratio 0.84, 95% confidence interval 0.73 to 0.95, moderate certainty), age 60 or older (0.50, 0.40 to 0.62, low certainty), active malignancy (0.57, 0.45 to 0.71, high certainty), and history of chronic kidney disease (0.56, 0.40 to 0.78, high certainty) were associated with reduced odds of survival after in-hospital cardiac arrest. Of the intra-arrest factors, witnessed arrest (2.71, 2.17 to 3.38, high certainty), monitored arrest (2.23, 1.41 to 3.52, high certainty), arrest during daytime hours (1.41, 1.20 to 1.66, high certainty), and initial shockable rhythm (5.28, 3.78 to 7.39, high certainty) were associated with increased odds of survival. Intubation during arrest (0.54, 0.42 to 0.70, moderate certainty) and duration of resuscitation of at least 15 minutes (0.12, 0.07 to 0.19, high certainty) were associated with reduced odds of survival.
Conclusion
Moderate to high certainty evidence was found for associations of pre-arrest and intra-arrest prognostic factors with survival after in-hospital cardiac arrest.
Systematic review registration
PROSPERO CRD42018104795
Introduction
Cardiac arrest refers to cessation of mechanical heart function and effective blood circulation, and is typically considered as either out-of-hospital cardiac arrest or in-hospital cardiac arrest.1 2 Although evidence from out-of-hospital cardiac arrest is often extrapolated to in-hospital cardiac arrest, the epidemiology is different, and the determinants of success might differ accordingly.1 3 In comparison to out-of-hospital cardiac arrest, data on incidence and survival after in-hospital cardiac arrest are limited. Most studies report an incidence of one to six events per 1000 hospital admissions.4 5 Survival to discharge ranges between 12% and 25%, with increased survival recently reported.1 6 7 One year outcomes are similar, with only modest increases over the past decade.8
Prognostic factors associated with survival after in-hospital cardiac arrest are an important focus of ongoing research.2 Patients admitted to hospital have increasingly complex conditions and present unique challenges when managing in-hospital cardiac arrest. Clinicians have to rapidly process many factors related to preadmission status (including age, sex, comorbidities) and factors related to the arrest itself (whether the arrest was witnessed or monitored, initial rhythm) to determine the effectiveness of ongoing cardiopulmonary resuscitation. Additionally, clinicians need to discuss expected prognosis after in-hospital cardiac arrest with patients at the time of hospital admission to inform care plans, and whether to include cardiopulmonary resuscitation in the event of cardiac arrest.3 9 10 Patient understanding of survival after in-hospital cardiac arrest is poor, and is often influenced by popular media where unrealistic rates of survival to discharge approach 67%.11 Furthermore, when discussing inclusion of cardiopulmonary resuscitation in goals of care, clinicians rarely mention prognostic factors and likelihood of survival after in-hospital cardiac arrest.12
A greater understanding of the factors associated with successful resuscitation of patients with in-hospital cardiac arrest is needed. This information will help in developing a predictive model used in shared decision making with patients and families, and clinical decision making at the time of in-hospital cardiac arrest and after return of spontaneous circulation. Therefore, we conducted a systematic review and meta-analysis to summarise the association between pre-arrest and intra-arrest factors and survival after in-hospital cardiac arrest.
Methods
We conducted this systematic review and meta-analysis according to PROGRESS (prognosis research strategy group) recommendations,13 14 15 16 and recent guidelines for systematic reviews and meta-analyses of prognostic factors.17 The CHARMS (critical appraisal and data extraction for systematic reviews of prediction modelling studies) checklist18 was used to define and frame the study. We registered the review protocol with the PROSPERO registry (CRD42018104795).
Data sources and searches
We searched Medline, PubMed, Embase, Scopus, Web of Science, and the Cochrane Database of Systematic Reviews from inception to 4 February 2019. An experienced health sciences librarian assisted in developing the search strategy (supplemental fig 1), which was conducted using the terms “cardiac arrest,” combined with terms related to prognosis research, as recommended.17 We used the Science Citation Index to retrieve reports that cited the relevant articles identified from our search, and then entered them into PubMed and conducted further surveillance searches using the “Related Articles” feature.19
Study selection
We included all English language full text articles that described retrospective and prospective observational studies, randomised controlled trials, and quasi randomised controlled trials. Inclusion criteria for studies were based on existing standards for research among patients with in-hospital cardiac arrest1 2: enrolled mostly (≥80%) adult patients (≥16 years) with in-hospital cardiac arrest; conducted in the emergency department, hospital wards, or intensive care unit; and evaluated mortality as an outcome of interest (in-hospital, 28 day, or 30 day mortality). We excluded studies that evaluated mortality over longer or unspecified time periods; case reports and case series; studies that included only patients who received a particular treatment after cardiac arrest (such as therapeutic hypothermia or extracorporeal life support); studies that included patients with out-of-hospital cardiac arrest; and studies that failed to provide model adjusted or unadjusted odds ratios with confidence intervals, or counts for calculating unadjusted odds ratios. We contacted the corresponding authors to obtain further information when these values could not be obtained from the reported data.
We screened studies using Covidence software (Melbourne, Australia); titles were imported into Covidence directly from the search databases and duplicates removed. Two reviewers (SMF and AT) independently screened the titles and abstracts of all identified citations. Disagreement was resolved by discussion; no third party adjudication proved necessary. The same two reviewers independently assessed full texts of the selected articles after screening and again resolved any disagreement by discussion.
Data extraction and quality assessment
Two investigators (SMF and AT) abstracted the following variables: author information, year of publication, study design, study dates, definition of start points, eligibility criteria, number of patients included, and incidence of mortality. We used a predesigned data extraction sheet (supplemental table 2) to minimise transcription errors. Subsequently, for each prognostic factor, two investigators (SMF and AT) independently collected unadjusted or adjusted odds ratios for survival in each study, if available. Extraction was performed using a modified version of the CHARMS checklist for prognostic factors (CHARMS-PF).17 18 A third investigator (WC) verified all extracted data and calculated unadjusted odds ratios from counts.
Two reviewers (SMF and AT) independently assessed the risk of bias for included studies, using the QUIPS (quality in prognosis studies) tool.20 Disagreements were resolved through discussion. As our protocol indicates, we had initially intended to use a different scale for quality review, but QUIPS is recommended for risk of bias assessment in reviews of prognostic factors.17 This tool includes six potential domains for bias and applicability of the research question: study participation, study attrition, prognostic factor measurement, outcome measurement, adjustment for other prognostic factors, and statistical analysis and reporting.
Data synthesis
Many of the included studies of in-hospital cardiac arrest were extracted from large databases, including the American Heart Association National Registry of Cardiopulmonary Resuscitation (NRCPR; later renamed the Get With The Guidelines (GWTG) registry), the United Kingdom National Cardiac Arrest Audit (NCAA), and the Swedish Cardiac Arrest Registry (SCAR). For registry or large databases, we included the report with the largest number of patients for each prognostic factor. We evaluated the associated websites of these databases and searched through all of their published studies. Primary, unpublished unadjusted and adjusted odds ratios were obtained directly from the NCAA database (April 2011-March 2018) by the principal investigators (KMR, DAH, and JPN), and the data they provided exceeds the number of patients in any of the published NCAA reports.21 22 23
For the primary analysis, we present meta-analyses of adjusted odds ratios. All included studies in this primary analysis had to consider the effect of age, initial rhythm, or cause of arrest in their analyses. These variables are known to be associated with outcome after in-hospital cardiac arrest.1 2 We included meta-analyses of unadjusted values as secondary analyses. Odds ratio estimates and the corresponding confidence intervals were analysed by applying the DerSimonian-Laird random effects model24 using Review Manager (version 5.3; Copenhagen, Denmark). We assessed heterogeneity using the I2 statistic, the χ2 test for homogeneity, and visual inspection of the forest plots.
Two investigators (BR and GHG) evaluated overall certainty in pooled estimates using the GRADE (grading of recommendations assessment, development, and evaluation) approach.25 These estimates were categorised into one of four levels of certainty: high, moderate, low, or very low. In accordance with GRADE guidance for prognostic studies, cohort data start as high certainty evidence.25 A GRADE evidence profile was created using the guideline development tool (gradepro.org).
Patient and public involvement
After article completion, and at the suggestion of peer reviewers, we sought out patient representatives through our institution’s patient relations department. Patient representatives were confidentially provided with a copy of the article and asked to provide written comments on the relevance of the work, the potential impact of the work on their own decision making, any perceived shortcomings of the work, and suggestions for future research.
Results
Search results
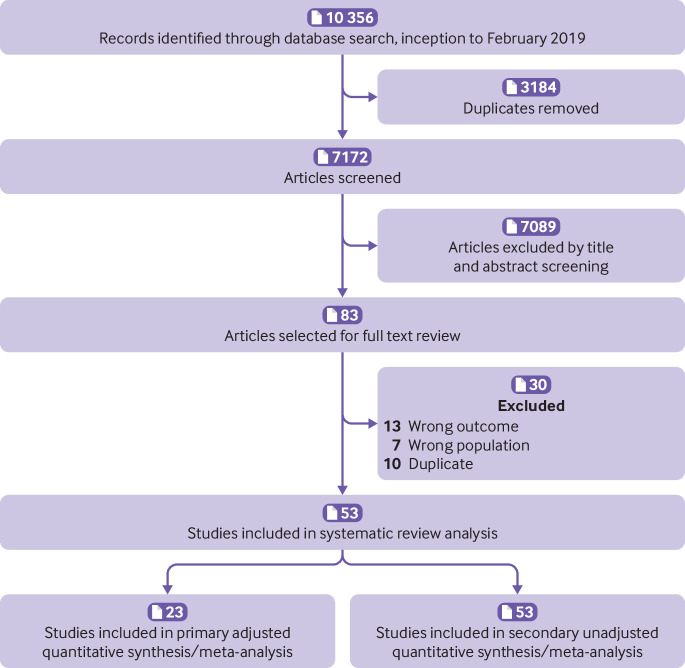
Our search identified 10 356 citations (fig 1) and after removing duplicates we screened 7172 studies, including 83 for full text review. We included 23 studies26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 in our primary meta-analysis of adjusted results, including unpublished results from 90 276 patients recorded on the NCAA database. Three studies used the NRCPR/GWTG database,29 42 44 and two used the SCAR database.26 43 The secondary analysis included an additional 30 studies.48 49 50 51 52 53 54 55 56 57 58 59 60 61 62 63 64 65 66 67 68 69 70 71 72 73 74 75 76 77
Fig 1.
Flowchart summarising evidence search and study selection
Study characteristics
Table 1 presents characteristics of studies included in the primary analysis. Supplemental table 2 displays CHARMS-PF checklist detailed characteristics of each study, and supplemental table 3 shows consistency between the included studies and the CHARMS-PF checklist requirements. Of the 23 studies included in the primary analysis, 12 (52.2%) were from North America, and six (26.1%) were from Europe. All included studies used observational designs, and 13 (56.5%) used retrospective cohort designs. Thirteen (56.5%) were multicentre studies (table 1). Supplemental table 6 presents prognostic factors included in the adjustment analyses of each study.
Table 1.
Characteristics of the 23 studies included in the primary analysis
| Description | No of studies (%) |
|---|---|
| Continent of study | |
| North America | 12 (52.2) |
| Europe | 6 (26.1) |
| Asia | 4 (17.4) |
| Australia | 1 (4.3) |
| Year of publication | |
| 1990–94 | 2 (8.7) |
| 1995–99 | 2 (8.7) |
| 2000–04 | 5 (21.7) |
| 2005–09 | 2 (8.7) |
| 2010–14 | 6 (26.1) |
| 2015–19 | 6 (26.1) |
| Study design | |
| Prospective cohort | 10 (43.5) |
| Retrospective cohort | 13 (56.5) |
| Sites | |
| Single centre | 10 (43.5) |
| Multicentre | 13 (56.5) |
Risk of bias and quality assessment
Supplemental table 7 displays quality assessments performed using the QUIPS tool. Most of the included studies were deemed to be at low risk of bias for all QUIPS domains. No studies were rated as high risk of bias in any QUIPS domain. We judged five studies to have moderate risk of bias in study participation, study attrition, or statistical reporting.21 27 30 33 64
Results of synthesis
Table 2 presents pooled adjusted odds ratios and 95% confidence intervals for the primary analysis, and GRADE level of certainty. Supplemental tables 8-9 show GRADE evidence profiles.
Table 2.
Pre-arrest and intra-arrest prognostic factors and associated odds of survival after in-hospital cardiac arrest
| Prognostic factors | Model adjusted data | ||||
|---|---|---|---|---|---|
| Studies | OR (95% CI) | P* | I2 (%) | GRADE certainty† | |
| Pre-arrest factors | |||||
| Demographics: | |||||
| Male sex | 7 | 0.84 (0.73 to 0.95) | 0.007 | 66 | Moderate |
| Age ≥60 | 3 | 0.50 (0.40 to 0.62) | <0.001 | 50 | Low |
| Age ≥70 | 2 | 0.42 (0.18 to 0.99) | 0.050 | 69 | Low |
| Comorbidities at admission: | |||||
| Active malignancy | 4 | 0.57 (0.45 to 0.71) | <0.001 | 71 | High |
| Congestive heart failure | 1 | 0.62 (0.56 to 0.68) | <0.001 | NA | Moderate |
| Chronic kidney disease | 5 | 0.56 (0.40 to 0.78) | 0.001 | 92 | High |
| COPD | 1 | 0.65 (0.58 to 0.72) | <0.001 | NA | Moderate |
| Diabetes mellitus | 1 | 0.53 (0.34 to 0.83) | 0.005 | NA | Moderate |
| Admission diagnosis: | |||||
| Acute coronary syndrome | 2 | 0.70 (0.28 to 1.78) | 0.460 | 99 | Low |
| Sepsis | 1 | 0.80 (0.70 to 0.91) | 0.001 | NA | Moderate |
| Intra-arrest factors | |||||
| Witnessed arrest | 4 | 2.71 (2.17 to 3.38) | <0.001 | 68 | High |
| Monitored patient | 6 | 2.23 (1.41 to 3.52) | <0.001 | 97 | High |
| Arrest during daytime hours | 5 | 1.41 (1.20 to 1.66) | <0.001 | 94 | High |
| Ventricular tachycardia | 4 | 3.76 (2.95 to 4.78) | <0.001 | 85 | High |
| Ventricular fibrillation | 4 | 3.68 (2.68 to 5.05) | <0.001 | 94 | High |
| Asystole | 4 | 0.42 (0.32 to 0.56) | <0.001 | 12 | High |
| Pulseless electrical activity | 2 | 0.59 (0.27 to 1.27) | 0.180 | 77 | High |
| Shockable rhythm | 12 | 5.28 (3.78 to 7.39) | <0.001 | 96 | High |
| Intubation during arrest | 5 | 0.54 (0.42 to 0.70) | <0.001 | 73 | Moderate |
| Resuscitation duration ≥15 min | 2 | 0.12 (0.07 to 0.19) | <0.001 | 27 | High |
COPD=chronic obstructive pulmonary disease; GRADE=grading of recommendations, assessment, development, and evaluation; NA=not applicable; OR=odds ratio.
P values obtained from the test for overall effect.
GRADE certainty of estimates in studies of prognosis, as described by Iorio and colleagues.25
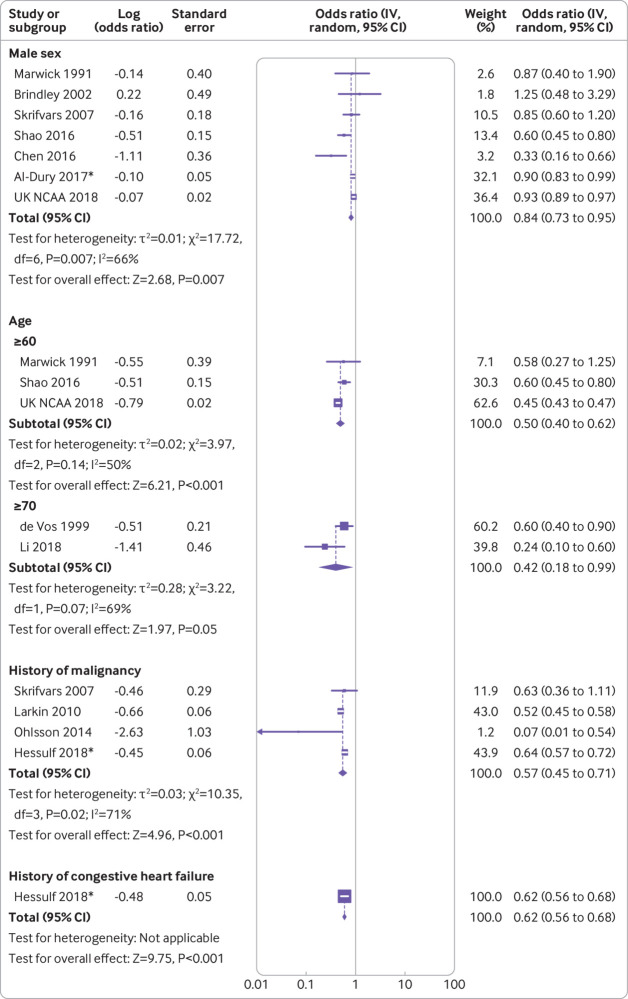
Primary analyses: pre-arrest factors
We evaluated the association between patient demographics and survival from in-hospital cardiac arrest. Figure 2 and figure 3 present forest plots.26 30 32 34 35 38 39 40 41 43 45 46 Male sex was associated with lower odds of survival (pooled odds ratio 0.84, 95% confidence interval 0.73 to 0.95, moderate certainty). We assessed the impact of age at two different thresholds: age 60 and older had a pooled odds ratio of 0.50 (0.40 to 0.62, low certainty); age 70 and older had a pooled odds ratio of 0.42 (0.18 to 0.99, low certainty).
Fig 2.
Forest plots showing pre-arrest factors and associated odds of survival after in-hospital cardiac arrest. Factors shown are male sex, age, history of malignancy and congestive heart failure. *30 day mortality
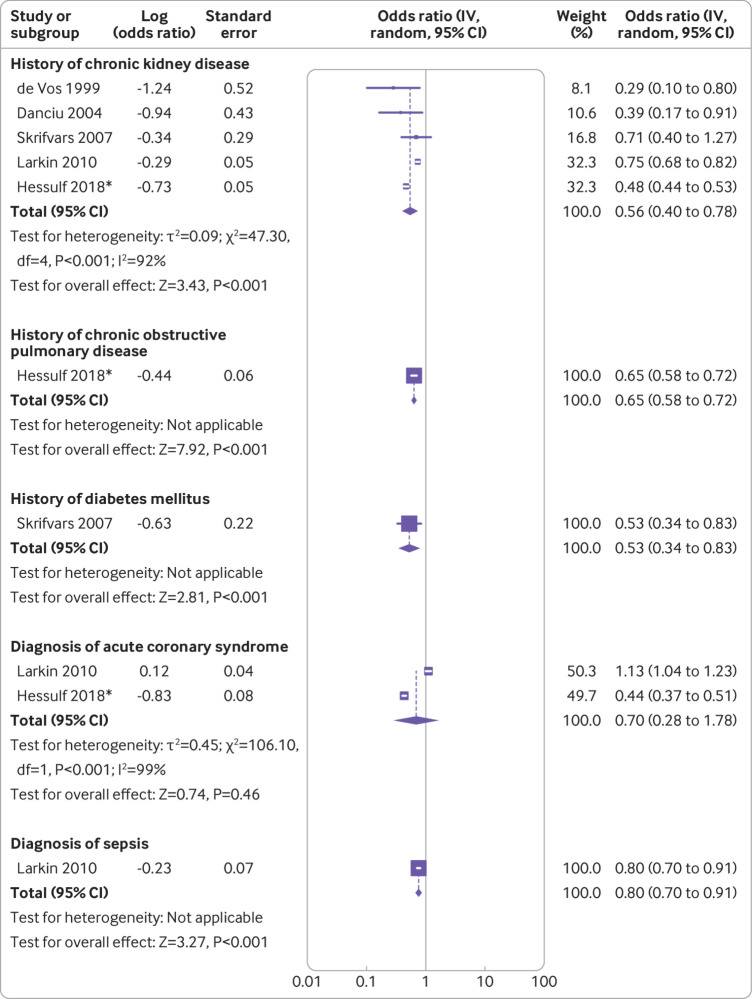
Fig 3.
Forest plots showing pre-arrest factors and associated odds of survival after in-hospital cardiac arrest. Factors shown are history of chronic kidney disease, chronic obstructive pulmonary disease, and diabetes mellitus, and diagnosis of acute coronary syndrome and sepsis. *30 day mortality
A history of malignancy was associated with a pooled odds ratio of 0.57 (95% confidence interval 0.45 to 0.71, high certainty) for survival from in-hospital cardiac arrest, and chronic kidney disease had a pooled odds ratio of 0.56 (0.40 to 0.78, high certainty). Single studies reported associations with congestive heart failure (0.62, 0.56 to 0.68, moderate certainty),38 chronic obstructive pulmonary disease (0.65, 0.58 to 0.72, moderate certainty),38 and diabetes mellitus (0.53, 0.34 to 0.83, moderate certainty).46 A diagnosis of acute coronary syndrome had a pooled odds ratio of 0.70 (0.28 to 1.78, low certainty).
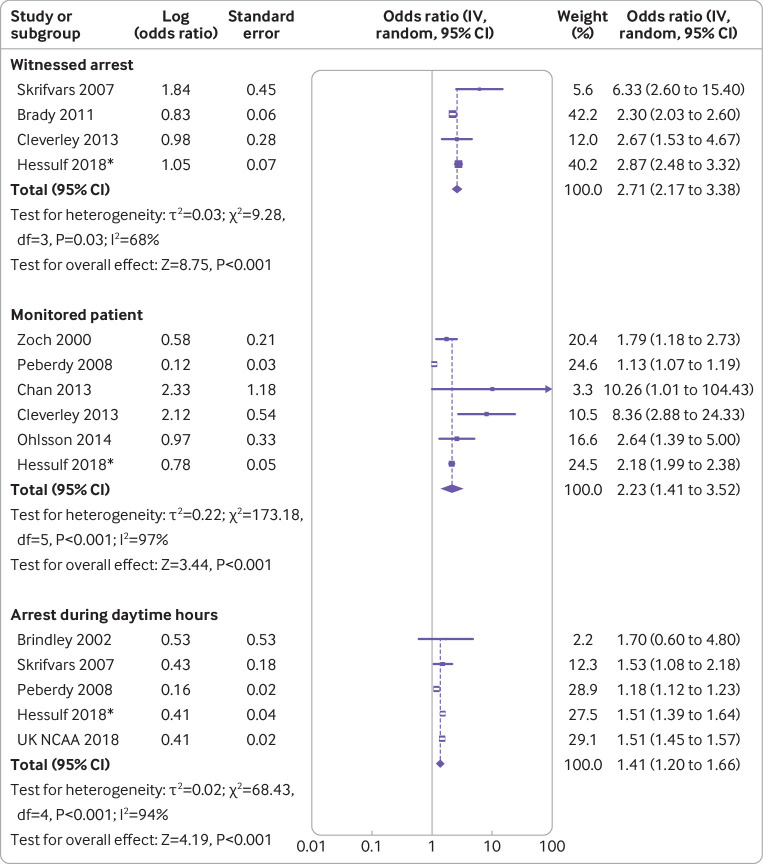
Primary analyses: intra-arrest factors
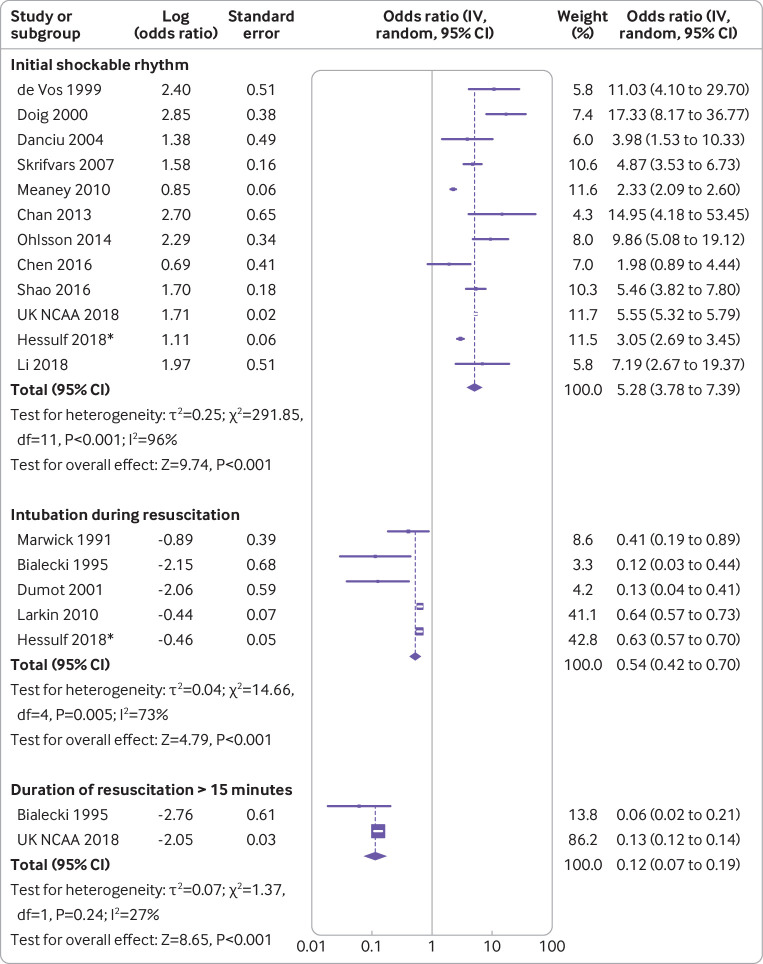
We investigated the association between intra-arrest factors and survival from in-hospital cardiac arrest. Figure 4 and figure 5 present forest plots.28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 Witnessed in-hospital cardiac arrest had a pooled odds ratio of 2.71 (95% confidence interval 2.17 to 3.38, high certainty). Arrests that took place in monitored settings (patients on telemetry) had a pooled odds ratio of 2.23 (1.41 to 3.52, high certainty). In-hospital cardiac arrest that took place during daytime hours (defined as time periods when hospitals were fully staffed, which varied among studies) had an associated pooled odds ratio of 1.41 (1.20 to 1.66, high certainty). Initial rhythm was categorised as either shockable (ventricular fibrillation or pulseless ventricular tachycardia) or non-shockable (pulseless electrical activity or asystole). An initial shockable rhythm during in-hospital cardiac arrest was associated with a pooled odds ratio of 5.28 (3.78 to 7.39, high certainty). We evaluated the prognostic impact of each rhythm (supplemental figs 14-17), which showed increased associated odds of survival among patients with any initial shockable rhythm. Tracheal intubation during in-hospital cardiac arrest was associated with a pooled odds ratio of 0.54 (0.42 to 0.70, moderate certainty). Duration of resuscitation (that is, time from arrest to return of spontaneous circulation) of at least 15 minutes had a pooled odds ratio of 0.12 (0.07 to 0.19, high certainty).
Fig 4.
Forest plots showing intra-arrest factors and associated odds of survival after in-hospital cardiac arrest. Factors shown are witnessed arrest, monitored patient, and arrest during daytime hours. *30 day mortality
Fig 5.
Forest plots showing intra-arrest factors and associated odds of survival after in-hospital cardiac arrest. Factors shown are initial shockable rhythm, intubation during resuscitation, and duration of resuscitation longer than 15 minutes. *30 day mortality
Secondary analyses
The supplemental material presents results of the secondary analyses. Supplemental table 10 shows CHARMS-PF checklist detailed characteristics of studies with only unadjusted results, and supplemental table 11 shows pooled unadjusted results. Supplemental figs 2-20 show forest plots that compare adjusted and unadjusted meta-analyses of pre-arrest and intra-arrest prognostic factors. Importantly, the direction of effect for all unadjusted analyses is in agreement with the primary adjusted analyses.
Discussion
We conducted a systematic review and meta-analysis to evaluate the association of pre-arrest and intra-arrest factors with survival after in-hospital cardiac arrest. Pre-arrest factors associated with reduced survival include male sex, increasing age, active malignancy, and chronic kidney disease. Among intra-arrest factors, we found that witnessed arrest, monitored setting, arrest during daytime hours, and shockable rhythm were associated with increased survival, while tracheal intubation during arrest and prolonged resuscitation were associated with reduced survival. These findings provide evidence of the association between important prognostic factors and odds of survival after in-hospital cardiac arrest. While clinicians have previously extrapolated data from out-of-hospital cardiac arrest to patients with in-hospital cardiac arrest,1 this study evaluated the in-hospital cardiac arrest population. The study identified risk factors that healthcare providers can consider when discussing expected prognosis with patients and making clinical decisions. Our results could be used to guide future large observational studies to derive a clinical prediction instrument for practical application. However, clinicians should exercise caution when using these results to make clinical decisions about starting or stopping resuscitation after in-hospital cardiac arrest. Nevertheless, even in the absence of an existing decision model, identification of risk factors that are associated with a poor prognosis after in-hospital cardiac arrest will probably have value for clinicians in discussions about goals of care and when to stop resuscitation.
Strengths and limitations of study
Our study involved a comprehensive search and included studies with an overall low risk of bias. We followed recent recommendations for meta-analysis of prognostic studies,17 evaluated several pre-arrest and intra-arrest prognostic factors for in-hospital cardiac arrest, and used GRADE guidelines to contextualise our findings based on overall certainty in estimates. Most of the estimates were based on moderate or high certainty evidence. Notably, we were able to include previously unpublished results from the NCAA database, and to analyse these data with published work from the NRCPC/GWTG, SCAR, and other databases to provide reliable estimates of prognostic factor association.
This review has some limitations. Firstly, our meta-analysis included only observational studies, and therefore provides associations between individual prognostic factors and survival from in-hospital cardiac arrest. Given the limitations of the literature, we were unable to assess how the combination of these factors might be used to influence clinical decision making. Therefore, clinicians should be cautious when combining these findings to make clinical decisions about starting or stopping resuscitation. Our results could be used to guide future large observational studies to derive a clinical prediction instrument for practical application. However, even in the absence of a decision model that could be used for accurate risk stratification, identification of risk factors associated with poor prognosis could be useful for clinicians when discussing goals of care with patients, and when making clinical decisions about stopping resuscitation after in-hospital cardiac arrest. Our study should be considered in that context.
Secondly, we evaluated short term survival as our primary outcome because this was the outcome most commonly reported in the literature.3 However, associations between prognostic factors and neurological outcome at discharge or long term survival are unknown and potentially could be more important to patients and caregivers. While neurological outcome was evaluated in some included studies, different scales were used, and so meta-analysis was not possible.
Thirdly, many of the factors we evaluated (namely age, sex, and comorbidities) are non-modifiable, but understanding their impact is valuable. It is important to emphasise the non-modifiable nature of these prognostic factors to patients when discussing advanced directives that relate to cardiopulmonary resuscitation after in-hospital cardiac arrest.
Finally, our study is limited by statistical and clinical heterogeneity. Statistical heterogeneity (assessed by I2) was markedly high in meta-analyses of several prognostic factors. While high heterogeneity suggests that we cannot be certain about the magnitude of effect size, the direction of effect size was clear for each factor, and visual inspection of forest plots did not reveal any important inconsistencies among included studies. Reliance upon the I2 statistic alone for quantifying the magnitude of heterogeneity in meta-analyses is problematic.78 In our study, the high I2 values were caused by a combination of several large national registry studies with small variability of effect estimates and smaller studies with larger variability. For this reason, the GRADE approach assesses statistical heterogeneity using a combination of factors, including I2, but also overlap of point estimates and overlap of 95% confidence intervals.79 After we evaluated all these measures of statistical heterogeneity, we felt it was appropriate to present the meta-analyses despite the high I2 values.
There is also clinical heterogeneity among studies with regard to some of the prognostic factors (for example, “monitoring” was referred to as continuous telemetry in some studies, while in others it included telemetry in addition to pulse oximetry). However, it is more likely that unknown confounders could have influenced the point estimates for individual studies. Furthermore, the clinical relevance of this heterogeneity is unknown. For example, the difference between telemetry alone versus telemetry and pulse oximetry might not be shown to be clinically significant. These sources of heterogeneity should be taken into account when the study results are evaluated.
Patient and public involvement
The patients involved in reviewing this study indicated that the study was of great importance to them and that identifying prognostic factors associated with outcome from in-hospital cardiac arrest was directly relevant to their care. All patients stated that, before reviewing the study, they had minimal knowledge of outcomes after in-hospital cardiac arrest, and were surprised to learn that overall outcomes were poor. They stated that the findings of this study allowed them to contextualise the likelihood of survival after in-hospital cardiac arrest, and that they would consider these results in their own decisions about cardiopulmonary resuscitation. One patient stated that neurological outcome was of particular importance, and that future research should prioritise neurological outcome as the primary outcome after in-hospital cardiac arrest.
Comparison with other studies
While pre-arrest factors are typically patient specific and non-modifiable, they show important associations that could help when considering expected prognosis and risk stratification. We found moderate certainty evidence that male sex was associated with reduced odds of survival after in-hospital cardiac arrest. Existing literature on out-of-hospital cardiac arrest has investigated the association between patient sex and survival, and found improved survival among female patients80; however the explanation for this finding is unclear. Female patients might benefit from specific hormones (namely oestrogen) and the effect of these hormones on their cardiovascular risk profile.81 82 Coronary occlusion in women is associated with stronger vagal activation, and therefore reduced potential for dysrhythmic events and decreased oxygen consumption.83 Our study suggests that this difference between sexes for out-of-hospital cardiac arrest extends to in-hospital cardiac arrest, but the underlying mechanisms remain unclear.
We found that increasing age and prevalence of certain comorbidities (malignancy and chronic kidney disease) were associated with reduced odds of survival after in-hospital cardiac arrest. Hirlekar and colleagues showed the association between increasing age and mortality from in-hospital cardiac arrest in the SCAR database.84 In addition to the higher prevalence of comorbidities in this population, older patients undergo less aggressive intervention, and survival from in-hospital cardiac arrest appears to decrease in a dose-response manner.85 We also found that patients with active cancer had lower associated survival from in-hospital cardiac arrest. The GWTG registry found that approximately 14% of patients in their cohort had advanced cancer, and that survival was markedly lower in this population even after taking into account resuscitation performance and patient directed limits in care.86 Increasing age and comorbidity burden are related to frailty, which describes a state of physiological decline and vulnerability.87 Future research should aim to investigate the association between frailty and outcomes after in-hospital cardiac arrest to help clinicians make a more accurate prognosis for patients admitted to hospital.88
While all of these pre-arrest factors are non-modifiable, discussing them with patients could be valuable when considering the inclusion of cardiopulmonary resuscitation in goals of care. Non-modifiable risk factors are particularly important because providing preventative care before in-hospital cardiac arrest or critical care after cardiac arrest will probably not alter patient outcome.89 90 Therefore, clinicians can talk with patients about these individual prognostic factors and poor survival after in-hospital cardiac arrest, even in the absence of a clinical decision model. Patients often have a poor understanding of outcome after in-hospital cardiac arrest, and this can be influenced by popular media.11 However, patients (particularly older patients) have found it helpful when clinicians provide statistics associated with poor survival after in-hospital cardiac arrest; when presented with such data, patients are more likely to decide against cardiopulmonary resuscitation.91 This view was also prevalent in the feedback provided by patients who reviewed our study, even though clinicians might not be surprised by our results. Therefore, our findings about pre-arrest prognostic factors could be helpful when clinicians discuss goals of care with patients.
We investigated intra-arrest factors to further our understanding about variables that influence prognosis after in-hospital cardiac arrest. We found high certainty evidence that patients who had in-hospital cardiac arrest in a monitored setting (that is, with telemetry) had increased odds of survival. This is not only because of immediate recognition, but also potentially because patients on continuous telemetry are more likely to have advanced haemodynamic monitoring devices in place.3 Witnessed arrest was also associated with improved survival after in-hospital cardiac arrest compared with unwitnessed arrest, also based on high certainty evidence. This finding has been consistently reported in the literature related to out-of-hospital cardiac arrest,92 and probably reflects reduced latency to cardiopulmonary resuscitation. Interestingly, we also found that in-hospital cardiac arrest during daytime hours was associated with improved survival. Hospital staffing (physicians, nurses, and allied health workers) is reduced at night time and during weekends, and these time periods have been associated with increased mortality.93 94
Other important intra-arrest variables were found to be associated with survival. Unsurprisingly, we found high certainty evidence that initial rhythm was associated with outcome after in-hospital cardiac arrest. Shockable rhythms (ventricular fibrillation or ventricular tachycardia) were associated with higher odds of survival because they are more likely to accompany a primary cardiac cause, and because of the effectiveness of early defibrillation. In the out-of-hospital cardiac arrest literature, survival from a shockable rhythm greatly exceeds survival after pulseless electrical activity or asystole75 95; our results for in-hospital cardiac arrest also show this trend. We found that prolonged duration of resuscitation (≥15 minutes) was associated with reduced survival after in-hospital cardiac arrest. As the duration of resuscitation increases, the likelihood of response to cardiac arrest interventions decreases, and the prolonged ischaemic time will probably result in irreversible organ dysfunction, even if return of spontaneous circulation is eventually achieved.2
Finally, we found that tracheal intubation during in-hospital cardiac arrest was associated with lower odds of survival, although this finding was based on moderate certainty evidence. This was the only potentially modifiable prognostic factor that was found. This association might be because of “resuscitation time bias,” because prolonged resuscitation could be associated with an increased number of interventions and worse outcome.96 However, this same finding was reported in a large cohort study that controlled for duration of resuscitation.48 Additionally, two recent randomised trials in patients with out-of-hospital cardiac arrest found that insertion of supraglottic airway devices resulted in at least comparable, if not superior, survival and neurological outcome as tracheal intubation.97 98 Future randomised trials on tracheal intubation during in-hospital cardiac arrest might provide more data on the optimal airway management strategy during in-hospital cardiac arrest.
Conclusions and policy implications
We evaluated pre-arrest and intra-arrest factors associated with survival after in-hospital cardiac arrest. Of the pre-arrest factors, male sex, increasing age, active malignancy, and chronic kidney disease were associated with reduced survival. Of the intra-arrest factors, witnessed arrest, monitored setting, cardiac arrest during daytime hours, and shockable rhythm were associated with increased survival, while tracheal intubation and prolonged resuscitation were associated with reduced survival. These findings provide evidence of associations between important prognostic factors and survival after in-hospital cardiac arrest.
What is already known about this topic
In-hospital cardiac arrest is associated with low survival rates
Much of our clinical understanding of in-hospital cardiac arrest is deduced from the extensive literature on out-of-hospital cardiac arrest
Understanding pre-arrest and intra-arrest prognostic factors associated with survival after in-hospital cardiac arrest is an important area of research
What this study adds
Of the pre-arrest factors, increasing age, male sex, active malignancy, and chronic kidney disease were associated with reduced survival after in-hospital cardiac arrest
Of the intra-arrest factors, witnessed arrest, monitored setting, arrest during daytime hours, and shockable rhythm were associated with increased survival after in-hospital cardiac arrest; increased duration of resuscitation and tracheal intubation were associated with reduced survival
The study identified important prognostic factors associated with outcome after in-hospital cardiac arrest, which could be used when discussing expected prognosis and advanced directives with patients
Acknowledgments
The authors wish to thank Maxime Le, Susan Rich, and other patient representatives (wishing to remain anonymous) who reviewed our study and provided critical feedback and patient perspectives on its findings.
Web extra.
Extra material supplied by authors
Web appendix: Electronic appendix
Contributors: SMF, AT, and JJP conceived the study idea. SMF, AT, WC, BR, and JJP coordinated the systematic review. SMF and AT designed the search strategy. SMF and AT screened abstracts and full texts. SMF, AT, and WC acquired the data and judged risk of bias in the studies. KMR, DAH, and JPN provided original data. WC performed the data analyses. BR and GHG created the GRADE evidence profiles. SMF, AT, WC, BR, MT, CV, KMR, DAH, JPN, KK, DIM, GHG, and JJP interpreted the data analysis and critically revised the manuscript. All authors have had the opportunity to review the final manuscript, and provided their permission to publish the manuscript. All authors agree to take responsibility for the work. AT and WC contributed equally. SMF is guarantor. The corresponding author attests that all listed authors meet authorship criteria, and that no others meeting the criteria have been omitted.
Funding: None received.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval: Not applicable.
Data sharing: The study protocol was registered with PROSPERO (CRD42018104795). For individual study data, please see online supplement.
The lead author (SMF) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned have been explained.
References
- 1. Andersen LW, Holmberg MJ, Berg KM, Donnino MW, Granfeldt A. In-hospital cardiac arrest: a review. JAMA 2019;321:1200-10. 10.1001/jama.2019.1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Morrison LJ, Neumar RW, Zimmerman JL, et al. American Heart Association Emergency Cardiovascular Care Committee, Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, and Council on P Strategies for improving survival after in-hospital cardiac arrest in the United States: 2013 consensus recommendations: a consensus statement from the American Heart Association. Circulation 2013;127:1538-63. 10.1161/CIR.0b013e31828b2770. [DOI] [PubMed] [Google Scholar]
- 3. Moskowitz A, Holmberg MJ, Donnino MW, Berg KM. In-hospital cardiac arrest: are we overlooking a key distinction? Curr Opin Crit Care 2018;24:151-7. 10.1097/MCC.0000000000000505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hodgetts TJ, Kenward G, Vlackonikolis I, et al. Incidence, location and reasons for avoidable in-hospital cardiac arrest in a district general hospital. Resuscitation 2002;54:115-23. 10.1016/S0300-9572(02)00098-9 [DOI] [PubMed] [Google Scholar]
- 5. Sandroni C, Nolan J, Cavallaro F, Antonelli M. In-hospital cardiac arrest: incidence, prognosis and possible measures to improve survival. Intensive Care Med 2007;33:237-45. 10.1007/s00134-006-0326-z. [DOI] [PubMed] [Google Scholar]
- 6. Nolan JP, Ferrando P, Soar J, et al. Increasing survival after admission to UK critical care units following cardiopulmonary resuscitation. Crit Care 2016;20:219. 10.1186/s13054-016-1390-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Zhu A, Zhang J. Meta-analysis of outcomes of the 2005 and 2010 cardiopulmonary resuscitation guidelines for adults with in-hospital cardiac arrest. Am J Emerg Med 2016;34:1133-9. 10.1016/j.ajem.2016.03.008. [DOI] [PubMed] [Google Scholar]
- 8. Schluep M, Gravesteijn BY, Stolker RJ, Endeman H, Hoeks SE. One-year survival after in-hospital cardiac arrest: a systematic review and meta-analysis. Resuscitation 2018;132:90-100. 10.1016/j.resuscitation.2018.09.001. [DOI] [PubMed] [Google Scholar]
- 9. Barry MJ, Edgman-Levitan S. Shared decision making—pinnacle of patient-centered care. N Engl J Med 2012;366:780-1. 10.1056/NEJMp1109283. [DOI] [PubMed] [Google Scholar]
- 10. Mentzelopoulos SD, Slowther AM, Fritz Z, et al. Ethical challenges in resuscitation. Intensive Care Med 2018;44:703-16. 10.1007/s00134-018-5202-0. [DOI] [PubMed] [Google Scholar]
- 11. Diem SJ, Lantos JD, Tulsky JA. Cardiopulmonary resuscitation on television. Miracles and misinformation. N Engl J Med 1996;334:1578-82. 10.1056/NEJM199606133342406. [DOI] [PubMed] [Google Scholar]
- 12. Tulsky JA, Chesney MA, Lo B. How do medical residents discuss resuscitation with patients? J Gen Intern Med 1995;10:436-42. 10.1007/BF02599915. [DOI] [PubMed] [Google Scholar]
- 13. Hemingway H, Croft P, Perel P, et al. PROGRESS Group Prognosis research strategy (PROGRESS) 1: a framework for researching clinical outcomes. BMJ 2013;346:e5595. 10.1136/bmj.e5595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Riley RD, Hayden JA, Steyerberg EW, et al. PROGRESS Group Prognosis Research Strategy (PROGRESS) 2: prognostic factor research. PLoS Med 2013;10:e1001380. 10.1371/journal.pmed.1001380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Steyerberg EW, Moons KG, van der Windt DA, et al. PROGRESS Group Prognosis Research Strategy (PROGRESS) 3: prognostic model research. PLoS Med 2013;10:e1001381. 10.1371/journal.pmed.1001381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hingorani AD, Windt DA, Riley RD, et al. PROGRESS Group Prognosis research strategy (PROGRESS) 4: stratified medicine research. BMJ 2013;346:e5793. 10.1136/bmj.e5793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Riley RD, Moons KGM, Snell KIE, et al. A guide to systematic review and meta-analysis of prognostic factor studies. BMJ 2019;364:k4597. 10.1136/bmj.k4597. [DOI] [PubMed] [Google Scholar]
- 18. Moons KG, de Groot JA, Bouwmeester W, et al. Critical appraisal and data extraction for systematic reviews of prediction modelling studies: the CHARMS checklist. PLoS Med 2014;11:e1001744. 10.1371/journal.pmed.1001744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Sampson M, Shojania KG, McGowan J, et al. Surveillance search techniques identified the need to update systematic reviews. J Clin Epidemiol 2008;61:755-62. 10.1016/j.jclinepi.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 20. Hayden JA, van der Windt DA, Cartwright JL, Côté P, Bombardier C. Assessing bias in studies of prognostic factors. Ann Intern Med 2013;158:280-6. 10.7326/0003-4819-158-4-201302190-00009. [DOI] [PubMed] [Google Scholar]
- 21. Nolan JP, Soar J, Smith GB, et al. National Cardiac Arrest Audit Incidence and outcome of in-hospital cardiac arrest in the United Kingdom National Cardiac Arrest Audit. Resuscitation 2014;85:987-92. 10.1016/j.resuscitation.2014.04.002. [DOI] [PubMed] [Google Scholar]
- 22. Harrison DA, Patel K, Nixon E, et al. National Cardiac Arrest Audit Development and validation of risk models to predict outcomes following in-hospital cardiac arrest attended by a hospital-based resuscitation team. Resuscitation 2014;85:993-1000. 10.1016/j.resuscitation.2014.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Robinson EJ, Smith GB, Power GS, et al. Risk-adjusted survival for adults following in-hospital cardiac arrest by day of week and time of day: observational cohort study. BMJ Qual Saf 2016;25:832-41. 10.1136/bmjqs-2015-004223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177-88. 10.1016/0197-2456(86)90046-2 [DOI] [PubMed] [Google Scholar]
- 25. Iorio A, Spencer FA, Falavigna M, et al. Use of GRADE for assessment of evidence about prognosis: rating confidence in estimates of event rates in broad categories of patients. BMJ 2015;350:h870. 10.1136/bmj.h870. [DOI] [PubMed] [Google Scholar]
- 26. Al-Dury N, Rawshani A, Israelsson J, et al. Characteristics and outcome among 14,933 adult cases of in-hospital cardiac arrest: a nationwide study with the emphasis on gender and age. Am J Emerg Med 2017;35:1839-44. 10.1016/j.ajem.2017.06.012. [DOI] [PubMed] [Google Scholar]
- 27. Ballew KA, Philbrick JT, Caven DE, Schorling JB. Predictors of survival following in-hospital cardiopulmonary resuscitation. A moving target. Arch Intern Med 1994;154:2426-32. 10.1001/archinte.1994.00420210060007 [DOI] [PubMed] [Google Scholar]
- 28. Bialecki L, Woodward RS. Predicting death after CPR. Experience at a nonteaching community hospital with a full-time critical care staff. Chest 1995;108:1009-17. 10.1378/chest.108.4.1009 [DOI] [PubMed] [Google Scholar]
- 29. Brady WJ, Gurka KK, Mehring B, Peberdy MA, O’Connor RE, American Heart Association’s Get with the Guidelines (formerly, NRCPR) Investigators In-hospital cardiac arrest: impact of monitoring and witnessed event on patient survival and neurologic status at hospital discharge. Resuscitation 2011;82:845-52. 10.1016/j.resuscitation.2011.02.028. [DOI] [PubMed] [Google Scholar]
- 30. Brindley PG, Markland DM, Mayers I, Kutsogiannis DJ. Predictors of survival following in-hospital adult cardiopulmonary resuscitation. CMAJ 2002;167:343-8. [PMC free article] [PubMed] [Google Scholar]
- 31. Chan JC, Wong TW, Graham CA. Factors associated with survival after in-hospital cardiac arrest in Hong Kong. Am J Emerg Med 2013;31:883-5. 10.1016/j.ajem.2013.02.005. [DOI] [PubMed] [Google Scholar]
- 32. Chen CT, Chiu PC, Tang CY, et al. Prognostic factors for survival outcome after in-hospital cardiac arrest: an observational study of the oriental population in Taiwan. J Chin Med Assoc 2016;79:11-6. 10.1016/j.jcma.2015.07.011. [DOI] [PubMed] [Google Scholar]
- 33. Cleverley K, Mousavi N, Stronger L, et al. The impact of telemetry on survival of in-hospital cardiac arrests in non-critical care patients. Resuscitation 2013;84:878-82. 10.1016/j.resuscitation.2013.01.038. [DOI] [PubMed] [Google Scholar]
- 34. Danciu SC, Klein L, Hosseini MM, Ibrahim L, Coyle BW, Kehoe RF. A predictive model for survival after in-hospital cardiopulmonary arrest. Resuscitation 2004;62:35-42. 10.1016/j.resuscitation.2004.01.035. [DOI] [PubMed] [Google Scholar]
- 35. de Vos R, Koster RW, De Haan RJ, Oosting H, van der Wouw PA, Lampe-Schoenmaeckers AJ. In-hospital cardiopulmonary resuscitation: prearrest morbidity and outcome. Arch Intern Med 1999;159:845-50. 10.1001/archinte.159.8.845 [DOI] [PubMed] [Google Scholar]
- 36. Doig CJ, Boiteau PJ, Sandham JD. A 2-year prospective cohort study of cardiac resuscitation in a major Canadian hospital. Clin Invest Med 2000;23:132-43. [PubMed] [Google Scholar]
- 37. Dumot JA, Burval DJ, Sprung J, et al. Outcome of adult cardiopulmonary resuscitations at a tertiary referral center including results of “limited” resuscitations. Arch Intern Med 2001;161:1751-8. 10.1001/archinte.161.14.1751 [DOI] [PubMed] [Google Scholar]
- 38. Hessulf F, Karlsson T, Lundgren P, et al. Factors of importance to 30-day survival after in-hospital cardiac arrest in Sweden: a population-based register study of more than 18,000 cases. Int J Cardiol 2018;255:237-42. 10.1016/j.ijcard.2017.12.068. [DOI] [PubMed] [Google Scholar]
- 39. Larkin GL, Copes WS, Nathanson BH, Kaye W. Pre-resuscitation factors associated with mortality in 49,130 cases of in-hospital cardiac arrest: a report from the National Registry for Cardiopulmonary Resuscitation. Resuscitation 2010;81:302-11. 10.1016/j.resuscitation.2009.11.021. [DOI] [PubMed] [Google Scholar]
- 40. Li H, Wu TT, Liu PC, et al. Characteristics and outcomes of in-hospital cardiac arrest in adults hospitalized with acute coronary syndrome in China. Am J Emerg Med 2018;37:1301-6. 10.1016/j.ajem.2018.10.003. [DOI] [PubMed] [Google Scholar]
- 41. Marwick TH, Case CC, Siskind V, Woodhouse SP. Prediction of survival from resuscitation: a prognostic index derived from multivariate logistic model analysis. Resuscitation 1991;22:129-37. 10.1016/0300-9572(91)90003-H [DOI] [PubMed] [Google Scholar]
- 42. Meaney PA, Nadkarni VM, Kern KB, Indik JH, Halperin HR, Berg RA. Rhythms and outcomes of adult in-hospital cardiac arrest. Crit Care Med 2010;38:101-8. 10.1097/CCM.0b013e3181b43282. [DOI] [PubMed] [Google Scholar]
- 43. Ohlsson MA, Kennedy LM, Juhlin T, Melander O. Evaluation of pre-arrest morbidity score and prognosis after resuscitation score and other clinical variables associated with in-hospital cardiac arrest in southern Sweden. Resuscitation 2014;85:1370-4. 10.1016/j.resuscitation.2014.07.009. [DOI] [PubMed] [Google Scholar]
- 44. Peberdy MA, Ornato JP, Larkin GL, et al. National Registry of Cardiopulmonary Resuscitation Investigators Survival from in-hospital cardiac arrest during nights and weekends. JAMA 2008;299:785-92. 10.1001/jama.299.7.785. [DOI] [PubMed] [Google Scholar]
- 45. Shao F, Li CS, Liang LR, et al. Incidence and outcome of adult in-hospital cardiac arrest in Beijing, China. Resuscitation 2016;102:51-6. 10.1016/j.resuscitation.2016.02.002. [DOI] [PubMed] [Google Scholar]
- 46. Skrifvars MB, Castrén M, Aune S, Thoren AB, Nurmi J, Herlitz J. Variability in survival after in-hospital cardiac arrest depending on the hospital level of care. Resuscitation 2007;73:73-81. 10.1016/j.resuscitation.2006.08.022. [DOI] [PubMed] [Google Scholar]
- 47. Zoch TW, Desbiens NA, DeStefano F, Stueland DT, Layde PM. Short- and long-term survival after cardiopulmonary resuscitation. Arch Intern Med 2000;160:1969-73. 10.1001/archinte.160.13.1969 [DOI] [PubMed] [Google Scholar]
- 48. Andersen LW, Granfeldt A, Callaway CW, et al. American Heart Association’s Get With The Guidelines–Resuscitation Investigators Association between tracheal intubation during adult in-hospital cardiac arrest and survival. JAMA 2017;317:494-506. 10.1001/jama.2016.20165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Andréasson AC, Herlitz J, Bång A, et al. Characteristics and outcome among patients with a suspected in-hospital cardiac arrest. Resuscitation 1998;39:23-31. 10.1016/S0300-9572(98)00120-8 [DOI] [PubMed] [Google Scholar]
- 50. Bedell SE, Delbanco TL, Cook EF, Epstein FH. Survival after cardiopulmonary resuscitation in the hospital. N Engl J Med 1983;309:569-76. 10.1056/NEJM198309083091001. [DOI] [PubMed] [Google Scholar]
- 51. Cohn AC, Wilson WM, Yan B, et al. Analysis of clinical outcomes following in-hospital adult cardiac arrest. Intern Med J 2004;34:398-402. 10.1111/j.1445-5994.2004.00566.x. [DOI] [PubMed] [Google Scholar]
- 52. Cooper S, Janghorbani M, Cooper G. A decade of in-hospital resuscitation: outcomes and prediction of survival? Resuscitation 2006;68:231-7. 10.1016/j.resuscitation.2005.06.012. [DOI] [PubMed] [Google Scholar]
- 53. Dodek PM, Wiggs BR. Logistic regression model to predict outcome after in-hospital cardiac arrest: validation, accuracy, sensitivity and specificity. Resuscitation 1998;36:201-8. 10.1016/S0300-9572(98)00012-4 [DOI] [PubMed] [Google Scholar]
- 54. Ebell MH, Kruse JA, Smith M, Novak J, Drader-Wilcox J. Failure of three decision rules to predict the outcome of in-hospital cardiopulmonary resuscitation. Med Decis Making 1997;17:171-7. 10.1177/0272989X9701700207. [DOI] [PubMed] [Google Scholar]
- 55. George AL, Jr, Folk BP, 3rd, Crecelius PL, Campbell WB. Pre-arrest morbidity and other correlates of survival after in-hospital cardiopulmonary arrest. Am J Med 1989;87:28-34. 10.1016/S0002-9343(89)80479-6 [DOI] [PubMed] [Google Scholar]
- 56. Huang CH, Chen WJ, Ma MH, Chang WT, Lai CL, Lee YT. Factors influencing the outcomes after in-hospital resuscitation in Taiwan. Resuscitation 2002;53:265-70. 10.1016/S0300-9572(02)00024-2 [DOI] [PubMed] [Google Scholar]
- 57. Karetzky M, Zubair M, Parikh J. Cardiopulmonary resuscitation in intensive care unit and non-intensive care unit patients. Immediate and long-term survival. Arch Intern Med 1995;155:1277-80. 10.1001/archinte.1995.00430120054007 [DOI] [PubMed] [Google Scholar]
- 58. Marik PE, Craft M. An outcomes analysis of in-hospital cardiopulmonary resuscitation: the futility rationale for do not resuscitate orders. J Crit Care 1997;12:142-6. 10.1016/S0883-9441(97)90044-7 [DOI] [PubMed] [Google Scholar]
- 59. Ofoma UR, Basnet S, Berger A, Kirchner HL, Girotra S, American Heart Association Get With the Guidelines – Resuscitation Investigators Trends in survival after in-hospital cardiac arrest during nights and weekends. J Am Coll Cardiol 2018;71:402-11. 10.1016/j.jacc.2017.11.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. O’Keeffe S, Redahan C, Keane P, Daly K. Age and other determinants of survival after in-hospital cardiopulmonary resuscitation. Q J Med 1991;81:1005-10. 10.1093/qjmed/81.3.1005 [DOI] [PubMed] [Google Scholar]
- 61. Patrick A, Rankin N. The in-hospital Utstein style: use in reporting outcome from cardiac arrest in Middlemore Hospital 1995-1996. Resuscitation 1998;36:91-4. 10.1016/S0300-9572(98)00006-9 [DOI] [PubMed] [Google Scholar]
- 62. Peters R, Boyde M. Improving survival after in-hospital cardiac arrest: the Australian experience. Am J Crit Care 2007;16:240-6, quiz 247. [PubMed] [Google Scholar]
- 63. Piscator E, Hedberg P, Göransson K, Djärv T. Survival after in-hospital cardiac arrest is highly associated with the Age-combined Charlson Co-morbidity Index in a cohort study from a two-site Swedish University hospital. Resuscitation 2016;99:79-83. 10.1016/j.resuscitation.2015.11.023. [DOI] [PubMed] [Google Scholar]
- 64. Radeschi G, Mina A, Berta G, et al. Piedmont IHCA Registry Initiative Incidence and outcome of in-hospital cardiac arrest in Italy: a multicentre observational study in the Piedmont Region. Resuscitation 2017;119:48-55. 10.1016/j.resuscitation.2017.06.020. [DOI] [PubMed] [Google Scholar]
- 65. Rakić D, Rumboldt Z, Carević V, et al. Approach to Sudden Cardiac Death Study Investigators In-hospital cardiac arrest and resuscitation outcomes: rationale for sudden cardiac death approach. Croat Med J 2005;46:907-12. [PubMed] [Google Scholar]
- 66. Roberts D, Landolfo K, Light RB, Dobson K. Early predictors of mortality for hospitalized patients suffering cardiopulmonary arrest. Chest 1990;97:413-9. 10.1378/chest.97.2.413 [DOI] [PubMed] [Google Scholar]
- 67. Robinson GR, 2nd, Hess D. Postdischarge survival and functional status following in-hospital cardiopulmonary resuscitation. Chest 1994;105:991-6. 10.1378/chest.105.4.991 [DOI] [PubMed] [Google Scholar]
- 68. Rosenberg M, Wang C, Hoffman-Wilde S, Hickam D. Results of cardiopulmonary resuscitation. Failure to predict survival in two community hospitals. Arch Intern Med 1993;153:1370-5. 10.1001/archinte.1993.00410110070011 [DOI] [PubMed] [Google Scholar]
- 69. Rozenbaum EA, Shenkman L. Predicting outcome of inhospital cardiopulmonary resuscitation. Crit Care Med 1988;16:583-6. 10.1097/00003246-198806000-00003 [DOI] [PubMed] [Google Scholar]
- 70. Sandroni C, Ferro G, Santangelo S, et al. In-hospital cardiac arrest: survival depends mainly on the effectiveness of the emergency response. Resuscitation 2004;62:291-7. 10.1016/j.resuscitation.2004.03.020. [DOI] [PubMed] [Google Scholar]
- 71. Schultz SC, Cullinane DC, Pasquale MD, Magnant C, Evans SR. Predicting in-hospital mortality during cardiopulmonary resuscitation. Resuscitation 1996;33:13-7. 10.1016/S0300-9572(96)00986-0 [DOI] [PubMed] [Google Scholar]
- 72. Skogvoll E, Isern E, Sangolt GK, Gisvold SE. In-hospital cardiopulmonary resuscitation. 5 years’ incidence and survival according to the Utstein template. Acta Anaesthesiol Scand 1999;43:177-84. 10.1034/j.1399-6576.1999.430210.x [DOI] [PubMed] [Google Scholar]
- 73. Sowden GR, Robins DW, Baskett PJ. Factors associated with survival and eventual cerebral status following cardiac arrest. Anaesthesia 1984;39:39-43. 10.1111/j.1365-2044.1984.tb09452.x [DOI] [PubMed] [Google Scholar]
- 74. Taffet GE, Teasdale TA, Luchi RJ. In-hospital cardiopulmonary resuscitation. JAMA 1988;260:2069-72. 10.1001/jama.1988.03410140081027 [DOI] [PubMed] [Google Scholar]
- 75. Tortolani AJ, Risucci DA, Rosati RJ, Dixon R. In-hospital cardiopulmonary resuscitation: patient, arrest and resuscitation factors associated with survival. Resuscitation 1990;20:115-28. 10.1016/0300-9572(90)90047-I [DOI] [PubMed] [Google Scholar]
- 76. van Walraven C, Forster AJ, Stiell IG. Derivation of a clinical decision rule for the discontinuation of in-hospital cardiac arrest resuscitations. Arch Intern Med 1999;159:129-34. 10.1001/archinte.159.2.129 [DOI] [PubMed] [Google Scholar]
- 77. van Walraven C, Forster AJ, Parish DC, et al. Validation of a clinical decision aid to discontinue in-hospital cardiac arrest resuscitations. JAMA 2001;285:1602-6. 10.1001/jama.285.12.1602 [DOI] [PubMed] [Google Scholar]
- 78. Borenstein M, Higgins JP, Hedges LV, Rothstein HR. Basics of meta-analysis: I2 is not an absolute measure of heterogeneity. Res Synth Methods 2017;8:5-18. 10.1002/jrsm.1230. [DOI] [PubMed] [Google Scholar]
- 79. Guyatt GH, Oxman AD, Kunz R, et al. GRADE Working Group GRADE guidelines: 7. Rating the quality of evidence–inconsistency. J Clin Epidemiol 2011;64:1294-302. 10.1016/j.jclinepi.2011.03.017. [DOI] [PubMed] [Google Scholar]
- 80. Bougouin W, Mustafic H, Marijon E, et al. Gender and survival after sudden cardiac arrest: a systematic review and meta-analysis. Resuscitation 2015;94:55-60. 10.1016/j.resuscitation.2015.06.018. [DOI] [PubMed] [Google Scholar]
- 81. Noppens RR, Kofler J, Hurn PD, Traystman RJ. Dose-dependent neuroprotection by 17beta-estradiol after cardiac arrest and cardiopulmonary resuscitation. Crit Care Med 2005;33:1595-602. 10.1097/01.CCM.0000169884.81769.F7 [DOI] [PubMed] [Google Scholar]
- 82. Kitamura T, Iwami T, Nichol G, et al. Utstein Osaka Project Reduction in incidence and fatality of out-of-hospital cardiac arrest in females of the reproductive age. Eur Heart J 2010;31:1365-72. 10.1093/eurheartj/ehq059. [DOI] [PubMed] [Google Scholar]
- 83. Airaksinen KE, Ikäheimo MJ, Linnaluoto M, Tahvanainen KU, Huikuri HV. Gender difference in autonomic and hemodynamic reactions to abrupt coronary occlusion. J Am Coll Cardiol 1998;31:301-6. 10.1016/S0735-1097(97)00489-0 [DOI] [PubMed] [Google Scholar]
- 84. Hirlekar G, Karlsson T, Aune S, et al. Survival and neurological outcome in the elderly after in-hospital cardiac arrest. Resuscitation 2017;118:101-6. 10.1016/j.resuscitation.2017.07.013. [DOI] [PubMed] [Google Scholar]
- 85. van Gijn MS, Frijns D, van de Glind EM, C van Munster B, Hamaker ME. The chance of survival and the functional outcome after in-hospital cardiopulmonary resuscitation in older people: a systematic review. Age Ageing 2014;43:456-63. 10.1093/ageing/afu035. [DOI] [PubMed] [Google Scholar]
- 86. Bruckel JT, Wong SL, Chan PS, Bradley SM, Nallamothu BK. Patterns of resuscitation care and survival after in-hospital cardiac arrest in patients with advanced cancer. J Oncol Pract 2017;13:e821-30. 10.1200/JOP.2016.020404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Bagshaw SM, Stelfox HT, McDermid RC, et al. Association between frailty and short- and long-term outcomes among critically ill patients: a multicentre prospective cohort study. CMAJ 2014;186:E95-102. 10.1503/cmaj.130639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Smith RJ, Reid DA, Santamaria JD. Frailty is associated with reduced prospect of discharge home after in-hospital cardiac arrest. Intern Med J 2018;49:978-85. 10.1111/imj.14159. [DOI] [PubMed] [Google Scholar]
- 89. Kyeremanteng K, Downar J. Why is it so hard to stop doing things that are unwanted, non-beneficial, or unsustainable? Lancet Respir Med 2019;7:558-60. 10.1016/S2213-2600(19)30169-9. [DOI] [PubMed] [Google Scholar]
- 90. Stelfox HT, Bourgault AM, Niven DJ. De-implementing low value care in critically ill patients: a call for action-less is more. Intensive Care Med 2019;45:1443-6. 10.1007/s00134-019-05694-y. [DOI] [PubMed] [Google Scholar]
- 91. Murphy DJ, Burrows D, Santilli S, et al. The influence of the probability of survival on patients’ preferences regarding cardiopulmonary resuscitation. N Engl J Med 1994;330:545-9. 10.1056/NEJM199402243300807. [DOI] [PubMed] [Google Scholar]
- 92. Sasson C, Rogers MA, Dahl J, Kellermann AL. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes 2010;3:63-81. 10.1161/CIRCOUTCOMES.109.889576. [DOI] [PubMed] [Google Scholar]
- 93. Needleman J, Buerhaus P, Pankratz VS, Leibson CL, Stevens SR, Harris M. Nurse staffing and inpatient hospital mortality. N Engl J Med 2011;364:1037-45. 10.1056/NEJMsa1001025. [DOI] [PubMed] [Google Scholar]
- 94. Pronovost PJ, Angus DC, Dorman T, Robinson KA, Dremsizov TT, Young TL. Physician staffing patterns and clinical outcomes in critically ill patients: a systematic review. JAMA 2002;288:2151-62. 10.1001/jama.288.17.2151 [DOI] [PubMed] [Google Scholar]
- 95. Stiell IG, Wells GA, Field B, et al. Ontario Prehospital Advanced Life Support Study Group Advanced cardiac life support in out-of-hospital cardiac arrest. N Engl J Med 2004;351:647-56. 10.1056/NEJMoa040325. [DOI] [PubMed] [Google Scholar]
- 96. Andersen LW, Grossestreuer AV, Donnino MW. “Resuscitation time bias”—a unique challenge for observational cardiac arrest research. Resuscitation 2018;125:79-82. 10.1016/j.resuscitation.2018.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Benger JR, Kirby K, Black S, et al. Effect of a strategy of a supraglottic airway device vs tracheal intubation during out-of-hospital cardiac arrest on functional outcome: the AIRWAYS-2 randomized clinical trial. JAMA 2018;320:779-91. 10.1001/jama.2018.11597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Wang HE, Schmicker RH, Daya MR, et al. Effect of a strategy of initial laryngeal tube insertion vs endotracheal intubation on 72-hour survival in adults with out-of-hospital cardiac arrest: a randomized clinical trial. JAMA 2018;320:769-78. 10.1001/jama.2018.7044. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Web appendix: Electronic appendix