Abstract
Background
Stroke is among the leading causes of death in Germany and one of the main reasons for handicap and disability. The risk factors for stroke include hypertension, metabolic disorders, and diabetes. An estimated 250 000 persons sustain a stroke in Germany each year. German data on the occurrence of stroke, and of recurrent stroke in particular, are still inadequate. The main objective of this study was to determine the frequency and timing of recurrent stroke.
Methods
The analyses were based on routine data of the AOK statutory health insurance fund in the German federal state of Lower Saxony. Inpatient billing and diagnosis data were used to identify initial and recurrent strokes (ICD-10 I60–I64). The derived incidence and prevalence were standardized for age and sex. The risks of recurrence and mortality were estimated with Kaplan–Meier analyses and Cox regressions.
Results
In 2010/2011, the standardized incidence of stroke was 292 per 100 000 persons per year, and the standardized prevalence was 336 per 100 000 persons. The risk of recurrence was 1.2% in the first 30 days, 3.4% within 90 days, 7.4% within 1 year, and 19.4% within 5 years. The mortality after an initial stroke was 6.8% in the first 30 days, 9.4% within 90 days, 17.0% within 1 year, and 45% within 5 years. Patients with hemorrhagic strokes had higher mortality. Treatment in a stroke unit was associated with lower mortality.
Conclusion
Patients with acute stroke should be treated in a specialized center whenever possible. After hospital discharge, stroke patients should be followed up at short intervals and any risk factors for stroke should be treated.
Stroke is one of the leading causes of death in developed countries (1). Furthermore, it ranks among the main causes of disability and invalidity in adults (2). Every year, about 243 000–260 000 persons in Germany have a stroke (3). The rates documented vary according to the type of study and the methods used. One study based on billing data from a national health insurance fund (GKV) found a 1-year prevalence of 317 cases per 100 000 population for 2007 (3); another study analyzing German diagnosis-related groups (DRG) billing data found a hospital admission rate due to stroke of 365 cases per 100 000 population in 2010 (4). On the basis of survey data the Robert Koch Institute (RKI) calculated a lifetime prevalence of 2.9%, with large differences by sex and social status (5). Similarly, estimates of the incidence of stroke events vary. The Erlangen Stroke Registry identified an incidence of 174 cases per 100 000 population for the period 1994–1996 (6). Van den Bussche et al. found an incidence of 126 cases per 100 000 population in 2006 on the basis of GKV billing data (7), while according to routine data from the AOK, a large statutory health insurance fund, the incidence was 266 cases per 100 000 population in 2008 (8). The variations can be explained to some extent by different methodological approaches and study populations.
Altogether, the currently available data on stroke rates, especially with regard to recurrent stroke, are unsatisfactory. In the study by van den Bussche et al. (7), 11.2% of the study population had a recurrence within 12 months. In the patient cohort of the Erlangen Stroke Registry, the recurrence rate was 15% over the 2-year follow-up period (9). A recent study in the USA found a recurrence risk of 9.5% within 5 years after transient ischemic attack (TIA) or mild ischemic stroke (10).
The present analysis aimed to determine the rate and the timing of recurrent stroke after an initial stroke event. Further points of interest were analysis of the incidence and prevalence of stroke events and calculation of mortality after incident stroke.
Methods
The present study is based on GKV routine health insurance data from the 2.7 million members of the AOK statutory health insurance fund in the German federal state of Lower Saxony. Routine data include various data that are collected for billing purposes (11). Routine data provide an opportunity to undertake a multitude of different analyses in the context of health services research (12– 15).
Initially, all insurance scheme members with a stroke diagnosis in 2010 and 2011 were selected. Because stroke is a severe acute illness that requires inpatient treatment as swiftly as possible, we used only inpatient diagnostic data (main diagnosis: stroke) in this study. All data relating to treatment before and after hospital admission or to partial inpatient treatment were removed to avoid the danger of classifying any follow-up treatment and referrals as new events.
The following ICD-10 main discharge diagnoses were considered as stroke events:
I60 (nontraumatic subarachnoid hemorrhage)
I61 (nontraumatic intracerebral hemorrhage)
I62 (other and unspecified nontraumatic intracranial hemorrhage)
I63 (cerebral infarction)
I64 (stroke, not specified as hemorrhage or infarction)
This definition of a stroke event has also been used by Federal Health Monitoring at the RKI and other authors (3, 7, 16, 17). Individual studies have also included TIA (3), but TIA was excluded from our analysis.
To date no standardized approach has been adopted to define stroke recurrence in studies of routine data or registries. Authors have used different criteria or have not explicitly reported the criteria. The routine-data study by van den Bussche et al., for example, used a minimum period of 7 days between discharge after the initial stroke and readmission (7). International (registry) studies have mostly used a minimum period of 21 days between initial event and recurrence. Infarction within 21 days after the initial cerebral insult is categorized as a recurrence only if a different region of the brain is affected (18– 20). These criteria were adapted in the context of our own study:
We defined an event as a recurrence only if a minimum of 21 days had elapsed between admission due to the initial cerebral insult and repeat admission due to the new event. Furthermore, the patient had to have been discharged from acute inpatient care after the initial event.
Infarction events within 21 days were categorized as recurrences only if, after discharge and repeat admission for a stroke, the patient was determined to have sustained a different type of stroke according to ICD-10 or if another region of the brain was affected.
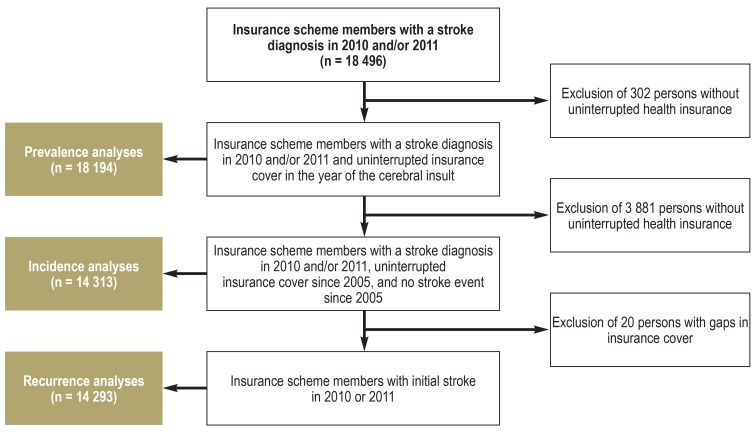
In all analyses, only those insurance scheme members were included who had continuous insurance cover throughout the relevant time period. No age limits were imposed. Only patients who had not had a stroke event in the pre-observation period from 2005 to the observed event in 2010/2011 were classified as incident cases. In the context of the long-term follow-up of patients with incident stroke, only those were included who had been continuously insured, without gaps in cover, until the end of the follow-up period (December 2016) or until termination of their insurance scheme (death or switch to another insurer). The maximum follow-up period was therefore 7 years. As this means different patient populations for the prevalence and incidence analyses, we standardized the documented incidence and prevalence rates according to the German standard population as in the 2011 census (21). Figure 1 shows how insurance scheme members were selected and the specific populations under analysis.
Figure 1.
Flow chart of data processing and analysis
The figure shows processing steps and numbers of insurance scheme members with a stroke diagnosis who were included in the respective analyses.
We used the statistics software package SPSS 25 for data evaluation and analyses. Information on the study population is presented descriptively. To determine the probability of recurrence and mortality over time, we undertook Kaplan–Meier survival analyses and Cox regression analyses. The level of significance was set at p = 0.05.
Results
Prevalence and incidence of stroke
In 2010/2011, 18 496 members of the insurance scheme experienced an initial or recurrent cerebral insult. The average age of the patients was 74 years, and 53% of those affected were women. The women were notably older than the men (77 versus 71 years). Some 81% of cases were cerebral infarctions (I63), 15% were hemorrhagic stroke (I60–I62), and 4% were stroke events not specified as hemorrhage or infarction (I64). The standardized 1-year prevalence was 336 cases per 100 000 population in 2010/2011 (336 cases per 100 000 population for 2010 and 335 cases per 100 000 population for 2011).
Altogether we found 14 313 insurance scheme members who had sustained an incident cerebral insult in 2010 or 2011. The age and sex distribution and the stroke types were almost identical with the prevalence results. The ICD-10 coding showed that 2.4% of the events were subarachnoid hemorrhage (I60), 9.3% were intracerebral hemorrhage (I61), 2.6% were other nontraumatic intracranial hemorrhages (I62), 81.2% were cerebral infarctions (I63), and 4.4% were stroke events not specified as hemorrhage or infarction (I64). Relevant underlying disorders/risk factors were observed in many cases: 69% of patients had hypertension, 33% had diabetes mellitus, 31% had hyperlipidemia, 13% had atrial fibrillation, and in 4% of patients carotid stenosis had been diagnosed in the preceding year. The standardized 1-year incidence of stroke was 292 cases per 100 000 population (290 cases/100 000 population in 2010 and 294 cases/100 000 population in 2011). Table 1 shows stroke incidence and prevalence by age and sex.
Table 1. Stroke incidence and prevalence by sex and age*.
| 2010 | 2011 | ||||||||
| Age group | N (women) | Prevalence women | N (men) | Prevalence men | N (women) | Prevalence women | N (men) | Prevalence men | |
| Prevalence | Below 50 years | 575 807 | 0.03% | 592 658 | 0.04% | 651 246 | 0.04% | 684 638 | 0.05% |
| 50 to below 55 years | 74 327 | 0.15% | 76 791 | 0.15% | 85 670 | 0.14% | 90 023 | 0.26% | |
| 55 to below 60 years | 66 939 | 0.18% | 66 371 | 0.26% | 74 500 | 0.21% | 75 936 | 0.42% | |
| 60 to below 65 years | 59 901 | 0.31% | 57 868 | 0.40% | 69 237 | 0.29% | 67 715 | 0.61% | |
| 65 to below 70 years | 57 306 | 0.46% | 50 409 | 0.58% | 58 382 | 0.48% | 52 976 | 0.84% | |
| 70 to below 75 years | 84 868 | 0.73% | 64 262 | 0.88% | 90 351 | 0.67% | 72 370 | 1.14% | |
| 75 to below 80 years | 70 767 | 1.16% | 44 137 | 1.13% | 78 104 | 1.16% | 51 355 | 1.63% | |
| 80 to below 85 years | 59 868 | 1.69% | 29 189 | 1.58% | 63 374 | 1.62% | 32 731 | 1.92% | |
| 85 to below 90 years | 42 238 | 2.30% | 12 917 | 1.98% | 43 708 | 2.13% | 14 266 | 2.32% | |
| 90 years and older | 21 963 | 2.30% | 4 641 | 2.39% | 24 389 | 2.30% | 5 543 | 2.11% | |
| Incidence | Below 50 years | 419 051 | 0.03% | 418 173 | 0.04% | 392 224 | 0.03% | 389 468 | 0.05% |
| 50 to below 55 years | 65 990 | 0.13% | 66 723 | 0.23% | 66 626 | 0.12% | 67 227 | 0.23% | |
| 55 to below 60 years | 61 144 | 0.16% | 59 277 | 0.35% | 60 378 | 0.19% | 59 147 | 0.39% | |
| 60 to below 65 years | 56 264 | 0.28% | 53 178 | 0.48% | 57 623 | 0.27% | 54 287 | 0.54% | |
| 65 to below 70 years | 54 851 | 0.39% | 47 775 | 0.79% | 49 473 | 0.43% | 43 508 | 0.75% | |
| 70 to below 75 years | 83 023 | 0.64% | 62 371 | 0.96% | 79 668 | 0.60% | 61 250 | 1.01% | |
| 75 to below 80 years | 69 595 | 1.01% | 43 180 | 1.32% | 70 904 | 1.00% | 44 515 | 1.39% | |
| 80 to below 85 years | 58 825 | 1.40% | 28 665 | 1.65% | 58 346 | 1.35% | 29 313 | 1.65% | |
| 85 to below 90 years | 41 401 | 1.99% | 12 636 | 2.03% | 40 430 | 1.88% | 12 968 | 1.93% | |
| 90 years and older | 21 422 | 1.96% | 4 512 | 2.13% | 22 729 | 1.98% | 5 018 | 1.77% | |
*Proportion of insurance scheme members, by age and sex, with an (initial) stroke
Frequency and timing of stroke recurrence
Among the 14 293 insurance scheme members with an incident stroke in 2010/2011, a total of 16 879 insult events (including initial insult) were found up to the end of the observation period (2016 at the latest). Altogether, 2145 (15%) insurance scheme members had at least one recurrence; of these, 1786 (12.1%) had one recurrence, 294 (2.1%) had two recurrences, and 52% (0.04%) had three recurrences. Thirteen insurance scheme members had four (n = 10), five (n = 2), or six (n = 1) recurrences.
The mean elapse of time between initial stroke event and recurrence was 697 days (standard deviation [SD] 643 days; 95% confidence interval [CI] 670–724 days). If another recurrence occurred, this happened after a mean interval of 450 days (SD 489 days; 95% CI 388–501 days).
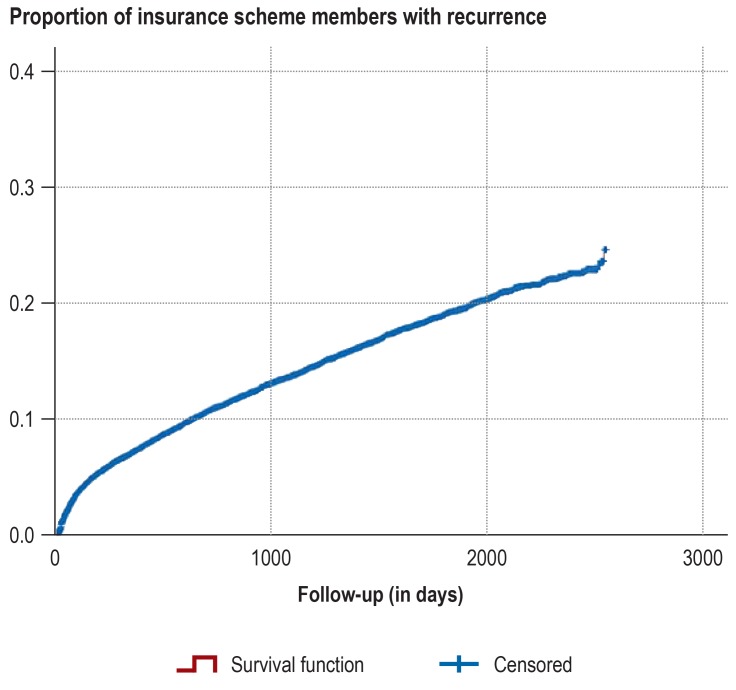
The results of the Kaplan–Meier tests (Figure 2) showed a risk of recurrence of 1.2% during the first 30 days, 3.4% within 90 days, 7.4% within 1 year, and 19.4% within 5 years. The annual risk of recurrence was 7.4% in the first year, 3.7% in the second year, 2.8% in the third year, 2.9% in the fourth year, and 2.6% in the fifth year after the initial stroke event.
Figure 2.
Recurrence rate
Proportion of insurance scheme members with a stroke recurrence in the follow-up period (x-axis: time in days, y-axis: number of insurance scheme members)
We used a complementary Cox regression to analyze the influence of stroke type on the probability of recurrence. We selected subarachnoid hemorrhage (I60) as our reference category. Age and sex were further variables. Women were found to have a lower risk of recurrence than men (hazard ratio [HR] 0.871; p = 0.002). Furthermore, the risk increased with each additional year of life (HR 1.016; p <0.001). The risk of recurrence after intracerebral hemorrhage (I61) (HR 0.838; p = 0.270) and other nontraumatic intracranial hemorrhage (I62) (HR 0.774; p = 0.184) was not significantly reduced compared with subarachnoid hemorrhage. Significantly lower probabilities of recurrence were determined for cerebral infarction (I63) (HR 0.715; p = 0.019) and stroke events not specified as hemorrhage or infarction (I64) (HR 0.683; p = 0.032).
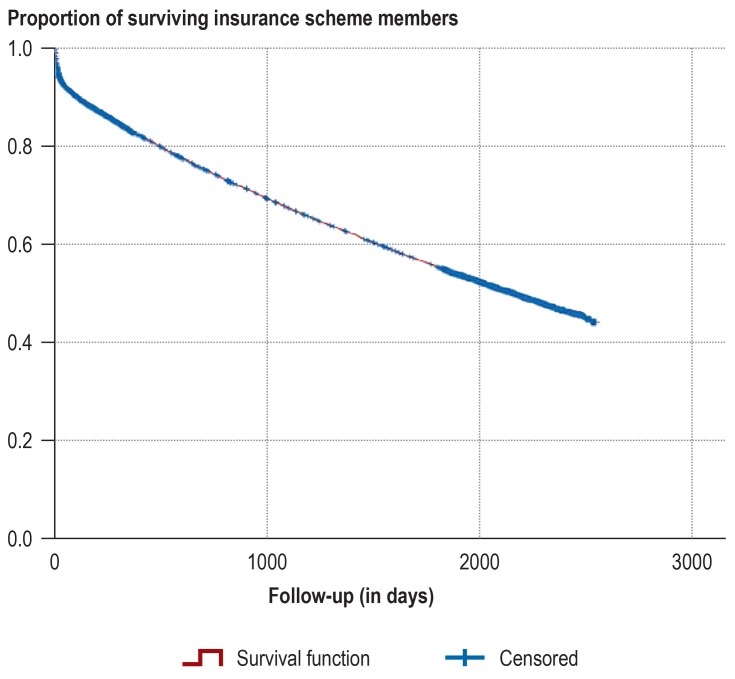
Mortality after stroke
Our Kaplan–Meier survival analyses of mortality (Figure 3) showed that 30 days after an incident stroke, 6.8% of patients had died; after 90 days, this rate had risen to 9.4%. Looking at the longer term, the 1-year and 5-year mortality rates were 17.0% and 45%. In the context of complementary Cox regression analysis with the variables age, sex, type of stroke, and type of treatment/care, the influence of stroke type on the mortality rate and the influence of care delivered in a stroke unit were studied. Women had a lower risk of death (HR 0.837; p <0.001). The mortality increased steadily with the patient’s age at the time of the initial cerebral insult (per life year) (HR 1.07; p <0.001). The risk of death was significantly lower for other nontraumatic intracranial bleeds (HR 0.653; p = 0.001), cerebral infarctions (HR 0.776; p = 0.016), and strokes not specified as hemorrhage or infarction (HR 0.768; p = 0.025) than for subarachnoid hemorrhage. The difference between mortality for intracerebral hemorrhage and for subarachnoid hemorrhage did not attain significance (HR 1.162; p = 0.175) (Table 2).
Figure 3.
Mortality after incident stroke event
Proportion of surviving insurance scheme members after incident stroke in the follow-up period (x-axis: time in days, y-axis: proportion of insurance scheme members)
Table 2. Cox regression for the outcome mortality*.
| Variable |
Significance (p value) |
Hazard ratio |
| Women (reference: men) | <0.001 | 0.837 |
| Age (per year) | <0.001 | 1.070 |
| I60 (nontraumatic subarachnoid hemorrhage) | <0.001 | Reference category |
| I61 (nontraumatic intracerebral hemorrhage) | 0.175 | 1.162 |
| I62 (other nontraumatic intracranial hemorrhage) | 0.001 | 0.653 |
| I63 (cerebral infarction) | 0.016 | 0.776 |
| I64 (stroke, not classified as hemorrhage or infarction) | 0.025 | 0.768 |
| Stroke unit care ‧(reference: no stroke unit) | <0.001 | 0.820 |
*Results of Cox regression for outcome mortality: effect of individual variables on outcome compared with reference category. Stroke unit care had been received in cases where the surgical and procedural (OPS) billing codes 8.981 (neurological complex treatment of acute stroke) or 8.98b (other neurological complex treatment of acute stroke) were used for the initial inpatient stay. In total, 7003 of the 14 293 patients had received care in a stroke unit. OPS billing code 8.981 was used in 6230 patients, code 8.98b in 773 patients.
Discussion
The present study investigated, on the basis of routine health insurance data, the incidence and prevalence of stroke, the frequency of stroke recurrence, the interval between initial insult and recurrence, and mortality after the initial stroke event. No previous studies of stroke in Germany have covered all of these aspects. Our study presents recent findings on stroke events in Germany and thus adds to the existing literature.
The results show a mean incidence and prevalence of 292 cases/100 000 population and 336 cases/100 000 population, respectively, for the period 2010/2011. The risk of recurrence was 3.4% within 90 days, 7.4% within 1 year, and 19.4% within 5 years. While the recurrence risk within the first year after a stroke is highest, it then falls up to the third year after the event and remains almost constant thereafter. The mortality risk after stroke is 6.8% after 30 days, 9.4% after 90 days, 17.0% after one year, and 45% after five years. Bleeding events were associated with higher mortality. Mortality was lower in patients who were treated in a stroke unit.
The findings on incidence and prevalence are consistent with previous estimates, although the results of the various analyses cannot be compared directly because of differences in inclusion criteria and in the age structures of the study populations (3, 4, 7– 9, 22). Furthermore, the frequency of stroke events can change over time, e.g., owing to changes in lifestyle or improved options for prevention of stroke (17, 23). Additionally, analyses have shown that stroke rates differ by social status (5). The social structures of the populations should therefore also be considered when comparing studies.
To date, little information is available on the rates of stroke recurrence in Germany. This study adds comprehensive analyses of the rates of recurrence and mortality, for individual stroke types and overall, to the current literature. Two analyses of routine data found that 11.2% and 11.4%, respectively, of stroke patients experienced a recurrence within 12 months (7, 8). Data from the Erlangen Stroke Registry show that for ischemic stroke, the risk of recurrence was 11% within 1 year and 15% within 2 years after the initial cerebral insult (9, 23). Data from registry studies in other countries are available (18, 20, 24, 25). A meta-analysis of registry studies published in 2011 found a 30-day recurrence risk of 3.1%. The cumulative risks for recurrence after 1, 5, and 10 years were 11.1%, 26.4%, and 39.2%, respectively (23). Data on the time that elapses between initial stroke and recurrence are sparse. An Asian study reported an average interval of 58 months (26).
A study of mortality after stroke based on GKV billing data showed in-hospital mortality of 7.1% and 12-month mortality of 17.4% (7). Figures from the AOK Research Institute (WIdO) showed in-hospital mortality of 11.4% and death rates of 12.7% at 30 days, 17.1% at 90 days, and 24.3% at 1 year in the year 2008 (8). Analyses of data from the Erlangen Stroke Registry determined mortality rates of 19.4% at 28 days, 28.5% at 90 days, and 37.3% at 1 year for the period 1994–1996 (6). Somewhat more recently, data from Ludwigshafen (2006/2007) showed lower rates (28-day mortality: 13.6%; 90-day mortality: 16.4%; 1-year mortality: 23.3%) (22). This distinct decrease in mortality rates is likely to be due to advances in care over time. Stroke treatment has improved substantially in recent years, not least as a result of the introduction of stroke units (27).
The principal strengths of the present study are the large sample size and the long follow-up period. However, it also features limitations arising from the use of GKV routine data. These routine statutory health insurance data include only services and diagnoses reimbursed by the GKV. The greatest disadvantage is the lack of clinical information, such as diagnostic or laboratory data, as well as details of stroke severity, quality of life, and impairments (12). Further uncertainty relates to the validity of the diagnoses. The data merely show that the billing hospital assigned a stroke diagnosis. The clinical-neurological investigations on which this diagnosis was based are unknown. Even though the indication of stroke makes incorrect coding of the diagnosis unlikely, misclassification of the different stroke types cannot be ruled out (7). Comparisons show that the classification into the different stroke types resembles that in other studies. Moreover, we may have underestimated incidence and prevalence, as stroke events that did not result in hospital treatment were not included in the analyses. Although the severity of a stroke event means it is unlikely that patients receive merely outpatient care, persons who died directly as a result of their stroke and therefore did not receive inpatient treatment were not included in the data. Similarly, recurrences that occur during the initial inpatient stay (early recurrences) cannot be reflected in routine data. Furthermore, questions arise with regard to the representativeness and generalizability of the results. In the present analysis, we evaluated data from the AOK statutory health insurance fund for Lower Saxony. By standardizing incidence and prevalence rates, we at least adjusted for some sources of bias. Slight selection bias owing to specific characteristics of the insurance clientele at a given point in time cannot be ruled out, however (2, 13, 28).
The present study investigated the rates of stroke recurrence and the incidence and prevalence of stroke events on the basis of routine health insurance data. The recurrence rate was found to be 7.4% after 1 year and 19.4% after 5 years. Specialized stroke care was associated with lower mortality. Long-term treatment and close monitoring of risk factors are essential to minimize the risk of recurrence. In view of ongoing demographic trends, stroke care will become increasingly important.
Key Messages.
This study comprises epidemiological estimates of stroke occurrence bases on a large sample.
The incidence and prevalence of stroke were 292 and 336 cases per 100 000 population in 2010/2011, consistent with previous estimates.
The risk of recurrence within 1 year is 7.4%. Contrary to expectation, the risk does not fall any further after the first 2 years.
The 1-year mortality rate of 17.0% is slightly below the figures reported in earlier studies.
Mortality was higher for hemorrhagic events than for cerebral infarctions. Patients treated in stroke units had significantly lower mortality.
Acknowledgments
Translated from the original German by Birte Twisselmann, PhD
Footnotes
Conflict of interest statement
Prof. Weissenborn has received lecture honoraria from Boehringer-Ingelheim, BMS, Pfizer, and Bayer. Furthermore, she has received funding for conducting clinical studies from Boehringer-Ingelheim, Bayer Portola, and Astra Zeneca.
The remaining authors declare that no conflict of interest exists.
References
- 1.GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1151–1210. doi: 10.1016/S0140-6736(17)32152-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Busch MA, Kuhnert R. 12-Monats-Prävalenz von Schlaganfall oder chronischen Beschwerden infolge eines Schlaganfalls in Deutschland. J Health Monit. 2017;2:70–76. [Google Scholar]
- 3.Kohler M, Deutschbein J, Peschke D, Schenk L. [Stroke occurrence in Germany—on the comparability of insurance data and registry-based data] Fortschr Neurol Psychiatr. 2014;82:627–633. doi: 10.1055/s-0034-1385231. [DOI] [PubMed] [Google Scholar]
- 4.Nimptsch U, Mansky T. Trends in acute inpatient stroke care in Germany—an observational study using administrative hospital data from 2005-2010. Dtsch Arztebl Int. 2012;109:885–892. doi: 10.3238/arztebl.2012.0885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Busch MA, Schienkiewitz A, Nowossadeck E, Gößwald A. [Prevalence of stroke in adults aged 40 to 79 years in Germany: results of the German Health Interview and Examination Survey for Adults (DEGS1)] Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2013;56:656–660. doi: 10.1007/s00103-012-1659-0. [DOI] [PubMed] [Google Scholar]
- 6.Kolominsky-Rabas PL, Sarti C, Heuschmann PU, et al. A prospective community-based study of stroke in Germany-the Erlangen Stroke Project (ESPro): incidence and case fatality at 1, 3, and 12 months. Stroke. 1998;29:2501–2506. doi: 10.1161/01.str.29.12.2501. [DOI] [PubMed] [Google Scholar]
- 7.van den Bussche H, Berger K, Kemper C, Barzel A, Glaeske G, Koller, D Inzidenz, Rezidiv, Pflegebedürftigkeit und Mortalität von Schlaganfall - Eine Sekundärdatenanalyse von Krankenkassendaten. Aktuelle Neurol. 2010;37:131–135. [Google Scholar]
- 8.Günster C. Schattauer. Stuttgart: 2010. Schlaganfallversorgung in Deutschland - Inzidenz, Wiederaufnahmen, Mortalität und Pflegerisiko im Spiegel von Routinedaten In: Versorgungs-Report 2011; pp. 147–163. [Google Scholar]
- 9.Kolominsky-Rabas PL, Weber M, Gefeller O, Neundoerfer B, Heuschmann PU. Epidemiology of ischemic stroke subtypes according to TOAST criteria: incidence, recurrence, and long-term survival in ischemic stroke subtypes: a population-based study. Stroke. 2001;32:2735–2740. doi: 10.1161/hs1201.100209. [DOI] [PubMed] [Google Scholar]
- 10.Amarenco P, Lavallée PC, Monteiro Tavares L, et al. Five-year risk of stroke after TIA or minor ischemic stroke. N Engl J Med. 2018;378:2182–2190. doi: 10.1056/NEJMoa1802712. [DOI] [PubMed] [Google Scholar]
- 11.Neubauer S, Zeidler J, Lange A, von der Schulenburg JM. Nomos. Baden-Baden: 2017. Prozessorientierter Leitfaden für die Analyse und Nutzung von Routinedaten der Gesetzlichen Krankenversicherung; pp. 17–19. [Google Scholar]
- 12.Kreis K, Neubauer S, Klora M, Lange A, Zeidler J. Status and perspectives of claims data analyses in Germany- A systematic review. Health Policy. 2016;120:213–226. doi: 10.1016/j.healthpol.2016.01.007. [DOI] [PubMed] [Google Scholar]
- 13.Ohlmeier C, Frick J, Prütz F, et al. [Use of routine data from statutory health insurances for federal health monitoring purposes] Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2014;57:464–472. doi: 10.1007/s00103-013-1912-1. [DOI] [PubMed] [Google Scholar]
- 14.Gansen FM. Health economic evaluations based on routine data in Germany: a systematic review. BMC Health Serv Res. 2018;18 doi: 10.1186/s12913-018-3080-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Neubauer S, Kreis K, Klora M, Zeidler J. Access, use, and challenges of claims data analyses in Germany. Eur J Health Econ. 2017;18:533–536. doi: 10.1007/s10198-016-0849-3. [DOI] [PubMed] [Google Scholar]
- 16.Robert Koch-Institut. Gesundheitsberichterstattung des Bundes. Berlin RKI: 2015. Gesundheit in Deutschland. [Google Scholar]
- 17.Bachus L, Eberhard S, Weißenborn K, Muschik D, Epping J, Geyer S. [Morbidity compression in stroke: longitudinal analyses on changes in the incidence of stroke] Gesundheitswesen. 2019;81:351–360. doi: 10.1055/s-0043-109860. [DOI] [PubMed] [Google Scholar]
- 18.Mohan KM, Crichton SL, Grieve AP, Rudd AG, Wolfe CDA, Heuschmann PU. Frequency and predictors for the risk of stroke recurrence up to 10 years after stroke: the South London Stroke Register. J Neurol Neurosurg Psychiatry. 2009;80:1012–1018. doi: 10.1136/jnnp.2008.170456. [DOI] [PubMed] [Google Scholar]
- 19.Hillen T, Coshall C, Tilling K, et al. Cause of stroke recurrence is multifactorial: patterns, risk factors, and outcomes of stroke recurrence in the South London Stroke Register. Stroke. 2003;34:1457–1463. doi: 10.1161/01.STR.0000072985.24967.7F. [DOI] [PubMed] [Google Scholar]
- 20.Burn J, Dennis M, Bamford J, Sandercock P, Wade D, Warlow C. Long-term risk of recurrent stroke after a first-ever stroke. The Oxfordshire Community Stroke Project. Stroke. 1994;25:333–337. doi: 10.1161/01.str.25.2.333. [DOI] [PubMed] [Google Scholar]
- 21.Gesundheitsberichterstattung des Bundes. Im Informationssystem der GBE zur Altersstandardisierung benutzte Standardbevölkerungen. www.gbe-bund.de/oowa921-install/servlet/oowa/aw92/dboowasys921.xwdevkit/xwd_init?gbe.isgbetol/xs_start_neu/&p_aid=i&p_aid=83060086&nummer=1000&p_sprache=D&p_indsp=-&p_aid=32921657 (last accessed on 5 July 2018) [Google Scholar]
- 22.Palm F, Urbanek C, Rose S, et al. Stroke incidence and survival in Ludwigshafen am Rhein, Germany: the Ludwigshafen Stroke Study (LuSSt) Stroke. 2010;41:1865–1870. doi: 10.1161/STROKEAHA.110.592642. [DOI] [PubMed] [Google Scholar]
- 23.Mohan KM, Wolfe CDA, Rudd AG, Heuschmann PU, Kolominsky-Rabas PL, Grieve AP. Risk and cumulative risk of stroke recurrence: a systematic review and meta-analysis. Stroke. 2011;42:1489–1494. doi: 10.1161/STROKEAHA.110.602615. [DOI] [PubMed] [Google Scholar]
- 24.Hata J, Tanizaki Y, Kiyohara Y, et al. Ten year recurrence after first ever stroke in a Japanese community: the Hisayama Study. J Neurol Neurosurg Psychiatry. 2005;76:368–372. doi: 10.1136/jnnp.2004.038166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Modrego PJ, Mainar R, Turull L. Recurrence and survival after first-ever stroke in the area of Bajo Aragon, Spain a prospective cohort study. J Neurol Sci. 2004;224:49–55. doi: 10.1016/j.jns.2004.06.002. [DOI] [PubMed] [Google Scholar]
- 26.Zhu R, Zu K, Shi J, Yan Q. Time interval between first ever and recurrent stroke in a population hospitalized for second stroke: a retrospective study. Neurol Asia. 2016;21:209–216. [Google Scholar]
- 27.Stroke Unit Trialists’ Collaboration. Organised inpatient (stroke unit) care for stroke. Cochrane Database Syst Rev. 2013;9 doi: 10.1002/14651858.CD000197.pub3. CD000197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jaunzeme J, Eberhard S, Geyer S. [How “representative” are SHI (statutory health insurance) data? Demographic and social differences and similarities between an SHI-insured population, the population of Lower Saxony, and that of the Federal Republic of Germany using the example of the AOK in Lower Saxony] Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2013;56:447–454. doi: 10.1007/s00103-012-1626-9. [DOI] [PubMed] [Google Scholar]