Abstract
The 2019 online pre-exposure prophylaxis (PrEP) user survey in the United Kingdom was conducted to assess HIV PrEP access, and user characteristics. One in five respondents continued experiencing difficulties accessing PrEP; users were almost exclusively gay or bisexual men at high risk of HIV. The majority obtained PrEP through health service clinics and rated PrEP positively. High STI rates were reported among users. Renal and sexual health checks are advised for those sourcing PrEP privately.
Keywords: PrEP, HIV, United Kingdom, men who have sex with men, MSM, sexually transmitted infections
Pre-exposure prophylaxis (PrEP) has been available in the United Kingdom (UK) through online purchase since Autumn 2015, National Health Service (NHS)-funded programmes via sexual health clinics in Scotland and Wales since July 2017, a health service funded trial in England since October 2017 and a risk reduction clinic in Northern Ireland since July 2018. We conducted an online survey to assess PrEP access in the UK, to capture experiences of people living in the UK who are using or report being unable to obtain PrEP since January 2017, and to estimate an upper limit of the number of current users in the UK.
Survey population
For this survey, a current PrEP user was defined as someone reporting to have taken their first PrEP tablet in July 2019 or earlier and their last PrEP tablet in January 2019 or later.
From 17 May to 1 July 2019, 2,389 participants recruited through the iWantPrEPNow mailing list, social media and Grindr completed the survey. Compared with previous survey years [1], the addition of recruitment through Grindr was new for 2019 (26%; n = 627); sampling changes could have affected observed behaviour differences compared with previous years. Those accessing the survey through Grindr had similar demographics to the total survey sample, except that fewer were living in England (88%; 554/627) and London (32%; 202/627). Participants were eligible for the survey if they were living in the UK and had tried to access or used PrEP since January 2017. Almost all (94%; n = 2,242) identified as exclusively gay and/or bisexual men and the majority (85%; n = 2,041) reported white ethnicity (Table 1). Half of respondents were aged 25–39 years (50%; n = 1,202). The majority (94%; n = 2,241) were living in England, while 3% (n = 73) were living in Scotland, 2% (n = 41) in Wales and 1% (n = 24) in Northern Ireland. Of participants, 78% (n = 1,856) had used PrEP since January 2017 and 94% (n = 1,742) of these were current PrEP users. Of respondents, 114 reported using PrEP since January 2017, but were not current users.
Table 1. PrEP user survey: Demographics, sexual behaviour and experiences among current PrEP users and those unable to obtain PrEP, United Kingdom, 2019 (n = 2,275).
| Characteristic | Current PrEP usera (n = 1,742) | Tried but unable to obtain PrEP since 2017 (n = 533) | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Demographics | |||||
| Gender identity | Man (including trans man) | 1,716 | 98.5 | 517 | 97.0 |
| Non-binary/In another way | 20 | 1.1 | 10 | 1.9 | |
| Woman (including trans woman) | 3 | 0.2 | 3 | 0.6 | |
| Not reported | 3 | 0.2 | 3 | 0.6 | |
| Sexual orientationb | Gay man | 1,622 | 93.1 | 445 | 83.5 |
| Bisexual | 110 | 6.3 | 75 | 14.1 | |
| Queer | 70 | 4.0 | 27 | 5.1 | |
| Heterosexual | 8 | 0.5 | 8 | 1.5 | |
| Gay woman | 0 | 0.0 | 1 | 0.2 | |
| Not reported | 23 | 1.3 | 10 | 1.9 | |
| Ethnicity | White | 1,488 | 85.4 | 460 | 86.3 |
| Asian | 106 | 6.1 | 28 | 5.3 | |
| Mixed | 50 | 2.9 | 12 | 2.3 | |
| Black | 45 | 2.6 | 17 | 3.2 | |
| Other | 38 | 2.2 | 11 | 2.1 | |
| Not reported | 15 | 0.9 | 5 | 0.9 | |
| Age group (years) | < 20–29 | 318 | 18.3 | 161 | 30.2 |
| 30–39 | 650 | 37.3 | 161 | 30.2 | |
| 40–49 | 455 | 26.1 | 115 | 21.6 | |
| ≥ 50 | 315 | 18.1 | 95 | 17.8 | |
| Not reported | 4 | 0.2 | 1 | 0.2 | |
| How respondent heard about surveyc | Through mailing list/email | 917 | 52.6 | 195 | 36.6 |
| Other (including through Grindr) | 450 | 25.8 | 240 | 45.0 | |
| Social media (Twitter, Facebook, Instagram) | 312 | 17.9 | 88 | 16.5 | |
| Through a friend | 46 | 2.6 | 4 | 0.8 | |
| Not reported | 17 | 1 | 6 | 1.1 | |
| Sexual behaviours | |||||
| Condomless anal/vaginal sex in the past 6 months | Yes | 1,670 | 95.9 | 435 | 81.6 |
| No | 68 | 3.9 | 94 | 17.6 | |
| Not reported | 4 | 0.2 | 4 | 0.8 | |
|
Number of condomless anal/vaginal sex partners in the past 6 months
(n = 1,670 for current PrEP users and n = 435 for those unable to obtain PrEP) |
One | 137 | 8.2 | 99 | 22.8 |
| Two to four | 510 | 30.5 | 195 | 44.8 | |
| Five to ten | 437 | 26.2 | 78 | 17.9 | |
| More than ten | 571 | 34.2 | 55 | 12.6 | |
| Not reported | 15 | 0.9 | 8 | 1.8 | |
|
Number of condomless anal/vaginal sex partners in the past 6 months on HIV treatment or PrEP
(n = 1,670 for current PrEP users and n = 435 for those unable to obtain PrEP) |
I don't know | 643 | 38.5 | 123 | 28.3 |
| None | 101 | 6.0 | 93 | 21.4 | |
| One or more | 909 | 54.4 | 210 | 48.3 | |
| Not reported | 17 | 1.0 | 9 | 2.1 | |
| Used drugs just before or during sex in the past year | Yes | 1,105 | 63.4 | 268 | 50.3 |
| Yes (chemsex)d | 724 | 41.6 | 85 | 15.9 | |
| No | 612 | 35.1 | 262 | 49.2 | |
| Not reported | 25 | 1.4 | 3 | 0.6 | |
| Experiences | |||||
| Feel satisfied with sex life | Agree/strongly agree | 1,221 | 70.1 | 225 | 42.2 |
| Neither agree or disagree | 324 | 18.6 | 160 | 30.0 | |
| Disagree/strongly disagree | 197 | 11.3 | 148 | 27.8 | |
| Has being on PrEP affected your life | Yes - PrEP has only had a good effect on my life | 1,310 | 75.2 | NA | NA |
| Yes - PrEP has had a variable effect on my life | 203 | 11.7 | NA | NA | |
| Yes - PrEP has only had a bad effect on my life | 4 | 0.2 | NA | NA | |
| No - PrEP has not affected my life | 185 | 10.6 | NA | NA | |
| Not reported | 40 | 2.3 | NA | NA | |
| Has felt differently treated while using PrEP | Yes | 300 | 17.2 | NA | NA |
| No | 1,440 | 82.7 | NA | NA | |
| Not reported | 2 | 0.1 | NA | NA | |
|
From whom has felt treated differently byb
(n = 300) |
Acquaintances and/or strangers | 126 | 42.0 | NA | NA |
| Dates | 118 | 39.3 | NA | NA | |
| Healthcare provider | 79 | 26.3 | NA | NA | |
| Partners | 76 | 25.3 | NA | NA | |
| Friends | 71 | 23.7 | NA | NA | |
| Family/other | 27 | 9.0 | NA | NA | |
| Not reported | 2 | 0.7 | NA | NA | |
NA: not applicable; PrEP: Pre-exposure prophylaxis.
a Current PrEP users defined as reporting taking their first PrEP tablet in July 2019 or earlier and their last PrEP tablet in January 2019 or later.
b For this question, respondents could pick multiple answers.
c Compared with previous years, 2019 survey participants were recruited from Grindr in addition to other recruitment methods.
d Chemsex was defined as using one or a combination of the following drugs before or during sex: crystal methamphetamine, mephedrone and gamma hydroxybutyrate/gamma-Butyrolactone (GHB/GBL).
Sourcing, experiences and prevalence of PrEP users
Among current users, 62% (1,081/1,742) last sourced PrEP through a trial or programme, including 55% (949/1,742) through the English Impact trial and the remaining either through another trial or a sexual health clinic in Scotland, Wales or Northern Ireland, while 37% (638/1,742) last sourced privately, either through online purchase, buying privately from a clinic, through a friend/re-seller, using PEP as PrEP or obtaining while travelling abroad (Table 2). A small proportion (16%) reported sharing or selling PrEP, most (61%) having originally sourced it online. Of current PrEP users, 75% took PrEP daily and 25% opted for other dosing regimens. The majority (75%) reported PrEP having only had a positive effect on their life (Box), although 17% reported feeling they had been treated differently while using PrEP, most commonly (42%) by acquaintances and/or strangers.
Table 2. PrEP user survey: Sourcing among those unable to obtain PrEP and sourcing, sharing, dosing, sexual health and renal function testing among current PrEP users, United Kingdom, 2019 (n = 2,275).
| Characteristic | n | % | |
|---|---|---|---|
| Participants who tried but were unable to obtain PrEP since January 2017 (n = 533) | |||
| Tried to source PrEP froma | From a sexual health clinic in England as part of the Impact trial | 385 | 72.2 |
| Buying from the Internet | 141 | 26.5 | |
| Other (including from a friend, when abroad, using PEP for PrEP, from a person reselling a supply, another trial) | 126 | 23.6 | |
| Sexual health clinic in Scotland, Wales or Northern Ireland | 22 | 4.1 | |
| Buying privately from a clinic | 16 | 3.0 | |
| Not reported | 14 | 2.6 | |
| Current PrEP usersb (n = 1,742) | |||
| Sourcing, sharing and dosing | |||
| Last sourced PrEP fromc | From a sexual health clinic in England as part of the Impact trial | 949 | 54.5 |
| Buying from the Internet | 538 | 30.9 | |
| Sexual health clinic in Scotland, Wales or Northern Ireland | 103 | 5.9 | |
| Buying privately from a clinic | 64 | 3.7 | |
| Other (including from a friend, when abroad, using PEP for PrEP, from a person reselling a supply, another trial) | 83 | 4.8 | |
| Not reported | 5 | 0.3 | |
| Ever shared/sold PrEP intended/bought by yourself | Yes | 279 | 16.0 |
| No | 1,460 | 83.8 | |
| Not reported | 3 | 0.2 | |
|
How this shared/sold PrEP was originally obtaineda
(n = 279) |
Bought from Internet | 170 | 60.9 |
| From a sexual health clinic in England as part of the Impact trial | 76 | 27.2 | |
| Other (incl. from a friend, when abroad, using PEP for PrEP, from a person reselling a supply, another trial) | 21 | 7.5 | |
| Sexual health clinic in Scotland, Wales or Northern Ireland | 9 | 3.2 | |
| Bought privately from a clinic | 3 | 1.1 | |
| Dosing strategy last time used PrEP | Daily | 1,303 | 74.8 |
| Other dosing regimen (including event-based, intermittently, one-off) | 439 | 25.2 | |
| Sexual health and renal function testing | |||
| Number of HIV tests in the last 12 months | None | 7 | 0.4 |
| One | 107 | 6.2 | |
| Two | 226 | 13.2 | |
| Three or more | 1,375 | 80.1 | |
| Not reported | 27 | 1.5 | |
|
Setting of last HIV testd
(n = 1,740) |
Sexual health clinic | 1,523 | 87.5 |
| Other setting (including self-sampling, self-testing service and GP) | 211 | 12.1 | |
| Not reported | 6 | 0.3 | |
| Number of STI tests (excluding HIV) in last 12 months | None | 203 | 11.7 |
| One | 168 | 9.6 | |
| Two | 208 | 11.9 | |
| Three or more | 1,153 | 66.2 | |
| Not reported | 10 | 0.6 | |
| STI diagnosis in last 12 months | Yes | 882 | 50.6 |
| No | 850 | 48.8 | |
| Not reported | 10 | 0.6 | |
|
STI(s) diagnosed in last 12 monthsa,
e
(n = 882) |
Gonorrhoea | 575 | 65.2 |
| Chlamydia | 537 | 60.9 | |
| Other | 239 | 27.1 | |
| Not Reported | 2 | 0.2 | |
| If ever obtained PrEP privately, had a renal function test before starting/while taking PrEP f | Yes | 654 | 37.5 |
| No | 660 | 37.9 | |
| Not Reported | 428 | 24.6 | |
GP: general practitioner; NR: not reported; PEP: post-exposure prophylaxis; PrEP: pre-exposure prophylaxis; STI: sexually transmitted infection.
a For this question, respondents could pick multiple answers.
b Current PrEP users defined as reporting taking their first PrEP tablet in July 2019 or earlier and their last PrEP tablet in January 2019 or later.
c Trial/programme sourcing PrEP users defined as PrEP users who last sourced their PrEP either through the Impact trial in England, another trial, or a sexual health clinic in Scotland, Wales or Northern Ireland. Privately sourcing PrEP users defined as PrEP users who last sourced PrEP either through online purchase, buying privately from a clinic, through a friend/re-seller, using PEP as PrEP or obtaining while travelling abroad.
d This question was only asked of respondents who reported ever having an HIV test.
e This question was only asked of respondents reporting STI diagnoses in the last 12 months.
f This question was asked of all PrEP users, but among current PrEP users last sourcing privately (n = 638), 325 (50.9%) responded ‘Yes’ to having a renal function test, 271 (42.5%) ‘No’ and 42 (6.5%) were not reported.
Box. Examples of current PrEP users’ comments on the positive effects of PrEP on their lives and how they felt they were treated differently, PrEP user survey, United Kingdom, 2019.
| Positive effect on life from PrEP comments: |
| ‘The reduced stress. Even when I use condoms, I felt worried that I could get HIV. It definitely hasn't changed my behaviour, I still have as much or as little sex as I would have before. But this has helped me worry less, and also be more happy in myself knowing that I can take some control.’ ‘Lack of fear around all sexual encounters now. Regardless of how safe I was in the past, I always felt there was a 'chance' I could have contracted HIV. Now that chance is so statistically low it's removed any angst around sex.’ ‘I know that I am protected whatever happens. I don't have to rely totally on condoms not failing and I don't have the weeks of anxiety wondering “what if”.’ ‘Much less anxiety about contracting HIV, more STI screenings.’ ‘The relief from the fear of contracting HIV is enormous. I never thought I could have sex without that lingering fear.’ ‘No impending sense of doom when attending for routine STD checks.’ |
| Feeling treated differently from using PrEP comments: |
| ‘A lot of people assume I am always looking for unprotected sex and am promiscuous. This is completely false - I use PrEP as an added layer of protection.’ ‘Expectation of unprotected sex as I am on PrEP. People feel that condoms aren't necessary anymore.’ ‘Either positively, being seen as more health conscious and responsible, or negatively, assuming PrEP-users are more promiscuous.’ ‘I have been slut-shamed for using PrEP on hook-up apps. A doctor thought I had HIV because I was on PrEP.’ ‘Almost every healthcare professional I’ve disclosed to about taking PrEP assume I’m HIV Positive’ ‘I do not feel advocacy from healthcare providers and experience a level of judgement.’ |
PrEP: Pre-exposure prophylaxis; STD: sexually transmitted disease; STI: sexually transmitted infection.
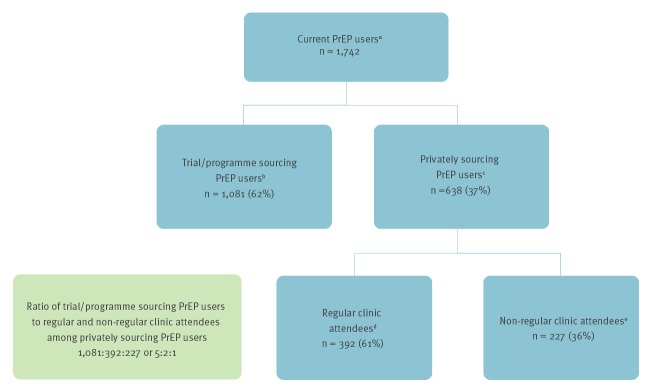
For each private PrEP user who was a non-regular clinic attendee, defined as reporting to have less than two HIV tests in the last 12 months, regardless of setting, there were two private users who were regular clinic attendees, defined as reporting having two or more HIV tests in the last 12 months at a sexual health clinic, and five trial/programme PrEP users (Figure). Using this 1:2:5 ratio, the upper limit of UK PrEP users is estimated to be one-seventh more than the numbers being monitored in clinics.
Figure.
Ratio of current PrEP users sourcing through a trial/programme to those sourcing privately who are regular or non-regular clinic attendees, United Kingdom, 2019 (n = 1,742)
PrEP: pre-exposure prophylaxis.
a Current PrEP users defined as reporting taking their first PrEP tablet in July 2019 or earlier and their last PrEP tablet in January 2019 or later.
b Trial/programme sourcing PrEP users defined as PrEP users who last sourced their PrEP either through the Impact trial in England, another trial, or a sexual health clinic in Scotland, Wales or Northern Ireland.
c Privately sourcing PrEP users defined as PrEP users who last sourced PrEP either through online purchase, buying privately from a clinic, through a friend/re-seller, using PEP as PrEP or obtaining while travelling abroad.
d Regular clinic attendee defined as reporting having two or more HIV tests in the last 12 months at a sexual health clinic.
e Non-regular clinic attendee defined as reporting to have less than two HIV tests in the last 12 months, regardless of setting.
Sexual behaviour and sexual health
Condomless sex in the past 6 months was reported by 96% of current PrEP users, with a third of these reporting more than ten condomless sex partners (Table 1). Almost a half (45%) reported that either none of these partners were on HIV treatment or PrEP or that they were unsure. In the past year, 63% reported using drugs just before or during sex and 42% reported chemsex.
Of current PrEP users sourcing through trial/programmes 77% (836/1,081), reported three or more STI tests and 92% (994/1,081) three or more HIV tests in the last year. Around a half (56%, 609/1,081) reported an STI diagnosis in the same period, most commonly gonorrhoea (68%, 412/609) and chlamydia (60%; 368/609). Among private users, 48% (308/638) reported three or more STI tests and 58% (367/638) three or more HIV tests in the last year, with 41% (263/638) reporting STI diagnoses.
While all people sourcing PrEP through trial/programmes would have had renal function tests, only 51% (325/638) of current private users reported having one before starting or while taking PrEP, even though two-thirds of private users were regular clinic attendees (Figure).
Challenges accessing pre-exposure prophylaxis (PrEP)
One in five (22%; 533/2,389) participants reported trying unsuccessfully to obtain PrEP since January 2017. Most (72%) tried to source through the Impact trial and over a quarter (27%) from online retailers (Table 2). Compared with current users, a higher proportion of those unable to access PrEP were aged under 30 years (30% vs 18%), reported bisexual sexual orientation (14% vs 6%) and accessed the survey through other means, including Grindr (45% vs 26%) (Table 1). Rates of condomless sex were also high (82%) among those unable to access PrEP and 13% reported more than ten condomless sex partners. Half reported being unsure or that none of these partners were on HIV treatment or PrEP, and 50% reported using drugs just before or during sex in the past year.
Only 42% of non-users reported feeling satisfied with their sex life, compared with 70% of current PrEP users and smaller proportions of non-users reported chemsex in the past year compared with PrEP current users (16% vs 42%).
Discussion
Since 2015, steady declines in new HIV diagnoses have been observed among UK GBM [2,3]. This followed the steady scale up of HIV testing over the past decade, the shortening of time to treatment initiation and the recent increase in PrEP use [4-8]. There were around 12,700 people accessing PrEP across England, Wales and Scotland through health service trials and programmes at the end of 2018 [6-8]. From our ratio of users sourcing through a trial/programme and privately (Figure), we estimate up to 7,600 others are sourcing PrEP privately. Of concern, we show that half of individuals sourcing PrEP privately are not undergoing baseline and ongoing renal function assessments, despite the majority being regular clinic attendees.
Our findings confirm that current PrEP users are at high-risk of exposure to HIV; the majority reported condomless sex with multiple partners and sexualised drug use, and many also reported condomless sex with partners of unknown HIV status or HIV treatment or PrEP status. The high STI rates reported in current PrEP users in this survey are consistent with recent reports in other countries [9,10] and may reflect more frequent testing. Services providing PrEP should consider how they can mitigate STI risk through integrating PrEP provision with STI screening and treatment to enhance STI control [11]. A high proportion of current users reported taking daily PrEP despite previous published evidence that event-based oral PrEP is highly effective in preventing HIV [12-14]. PrEP had a strong positive effect on the lives of users and the majority were satisfied with their sex life.
Although PrEP is highly effective for HIV prevention, PrEP availability and scale-up across Europe has been slow and uneven to date, and the ‘gap’ between self-reported use and expressed need is large across European countries [15]. Additionally, our survey highlights high demand for PrEP and a larger PrEP ‘gap’ than expected, with around one in five individuals in need of PrEP but unable or unsure of how to access publicly funded PrEP. Many of them were at high risk of HIV and would have benefited from PrEP and the proportion unable to access PrEP is similar to findings from the PrEP user survey conducted in the previous year [1], despite recent increases in the number of Impact trial places. However, this survey asked about experiences since January 2017 so the finding may be an expression of intermittent capping of trial places and capacity strains at trial clinics [8]. As other European countries are implementing pilot PrEP programmes or localised schemes, this report illustrates the value of estimating the true scale of PrEP need.
Finally, while knowledge of PrEP among UK GBM is among the highest in Europe [16], a small but appreciable number of users reported a knowledge gap among healthcare providers, including negative judgements. Greater awareness among health professionals is required to ensure these experiences do not undermine access or adherence to PrEP.
Acknowledgements
We would like to acknowledge survey respondents for taking time to participate in our survey.
Conflict of interest: None declared.
Authors’ contributions: All authors were involved in the development of the PrEP User Survey and contributed important intellectual content to this manuscript. COH was scientific lead for the survey at Public Health England and was responsible for creating the online survey and carrying out data analysis and interpretation. COH also drafted the manuscript, incorporated author comments, and was responsible for the final draft to be published. All authors commented on the manuscript and approved the final draft. VD, NG, WN, SC, GO and LS provided key input into the survey design and interpretation of results. GO and WN were responsible for survey recruitment. NG, VD and WN contributed to the analysis design and manuscript writing.
References
- 1.Cairns G. Nearly a quarter of people who want PrEP currently can’t get it, UK survey finds. Nam aidsmap. London; NAM; 25 June 2018. [Accessed 7 Aug 2019]. Available from: https://www.aidsmap.com/news/jun-2018/nearly-quarter-people-who-want-prep-currently-cant-get-it-uk-survey-finds
- 2.Nash SDS, Croxford S, Guerra L, Lowndes C, Connor N, Gill ON. Progress towards ending the HIV epidemic in the United Kingdom - 2018 report. London: Public Health England; 2018. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/821273/Progress_towards_ending_the_HIV_epidemic_in_the_UK.pdf
- 3.Public Health England (PHE). Health Protection Report: Volume 13 Number 31. Trends in new HIV diagnoses and in people receiving HIV-related care in the United Kingdom: data to the end of December 2018. London: Public Health England; 6 September 2019. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/835084/hpr3119_hiv18-v2.pdf
- 4.Ogaz D, Miltz AR, Desai S, Saunders J, Charlett A, Gill ON. Preparing for PrEP in England: prevalence and incidence of HIV and bacterial STIs. Conference on Retroviruses and Opportunistic Infections; Mar 4–7 2019; Seattle, United States. [Google Scholar]
- 5.Gill ON, Ogaz D, Blomquist P, Khawam J, Kirwan P, Brizzi F, et al. The fall in HIV infections in MSM in England during 2012 through 2016: When did it begin and what caused it? IUSTI World and European Congress; 2018; Dublin, Ireland. [Google Scholar]
- 6.Health Protection Scotland (HPS) and Information Services Division (ISD). Implementation of HIV PrEP in Scotland: First Year Report. Edinburgh and Glasgow: HPS and ISD; February 2019.Available from: https://www.hps.scot.nhs.uk/web-resources-container/implementation-of-hiv-prep-in-scotland-first-year-report/
- 7.Communicable Disease Surveillance Centre (CDSC). Pre-exposure prophylaxis for HIV (PrEP) provision in Wales. 1st July 2017 to 31st December 2018. Public Health Wales; February 2019.Available from: http://www.wales.nhs.uk/sitesplus/documents/888/PrEP_activity%2007022019_v1_.pdf
- 8.National Health Service England (NHSE). PrEP Impact Trial Update – October 2019. Available from: https://www.england.nhs.uk/commissioning/spec-services/npc-crg/blood-and-infection-group-f/f03/prep-trial-updates/
- 9. Serpa JA, Huynh GN, Nickell JB, Miao H. HIV Pre-Exposure Prophylaxis and Increased Incidence of Sexually Transmitted Infections in the United States. Clin Infect Dis. 2019;ciz552. 10.1093/cid/ciz552 [DOI] [PubMed] [Google Scholar]
- 10. Traeger MW, Cornelisse VJ, Asselin J, Price B, Roth NJ, Willcox J, et al. Association of HIV Preexposure Prophylaxis With Incidence of Sexually Transmitted Infections Among Individuals at High Risk of HIV Infection. JAMA. 2019;321(14):1380-90. 10.1001/jama.2019.2947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ong J. STIs incidence and prevalence in PrEP programmes – highlights from a systematic review. 10th International AIDS Society Conference on HIV Science (IAS 2019); 21 Jul 2019; Mexico City,Mexico. [Google Scholar]
- 12. Molina JM, Charreau I, Spire B, Cotte L, Chas J, Capitant C, et al. Efficacy, safety, and effect on sexual behaviour of on-demand pre-exposure prophylaxis for HIV in men who have sex with men: an observational cohort study. Lancet HIV. 2017;4(9):e402-10. 10.1016/S2352-3018(17)30089-9 [DOI] [PubMed] [Google Scholar]
- 13.Molina JM, Charreau I, Spire B, Cotte L, Pialoux G, Capitant C, et al. On demand PrEP with oral TDF-FTC in MSM: results of the ANRS Ipergay Trial. Conference on Retroviruses and Opportunistic Infections; Feb 22-25 2015; Seattle, United States. [Google Scholar]
- 14. BHIVA/BASHH BHIVA/BASHH guidelines on the use of HIV pre-exposure prophylaxis (PrEP) 2018. HIV Med. 2019;20(Suppl 2):s2-80. 10.1111/hiv.12718 [DOI] [PubMed] [Google Scholar]
- 15. Hayes R, Schmidt AJ, Pharris A, Azad Y, Brown AE, Weatherburn P, et al. Estimating the ‘PrEP Gap’: how implementation and access to PrEP differ between countries in Europe and Central Asia in 2019. Euro Surveill. 2019;24(41):1900598. 10.2807/1560-7917.ES.2019.24.41.1900598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.The EMIS Network. EMIS-2017 – The European Men-Who-Have-Sex-With-Men Internet Survey. Key findings from 50 countries. Stockholm: European Centre for Disease Prevention and Control; 2019. Available from: https://www.ecdc.europa.eu/sites/default/files/documents/European-MSM-internet-survey-2017-findings.pdf