Abstract
Background:
Type 2 diabetes is a lifestyle-related disorder that affects around 422 million individuals in India. Integration of AYUSH (Ayurveda) with the National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke (NPCDCS) was conceived on pilot basis at Gaya, Bihar, to provide integrative treatment for non-communicable disease patients and to manage the burden of non-communicable diseases in India.
Objectives:
The objective of this study was to analyze the effect of Ayurveda intervention, lifestyle modification and Yoga in the management of type 2 diabetes under NPCDCS-AYUSH integration project.
Materials and Methods:
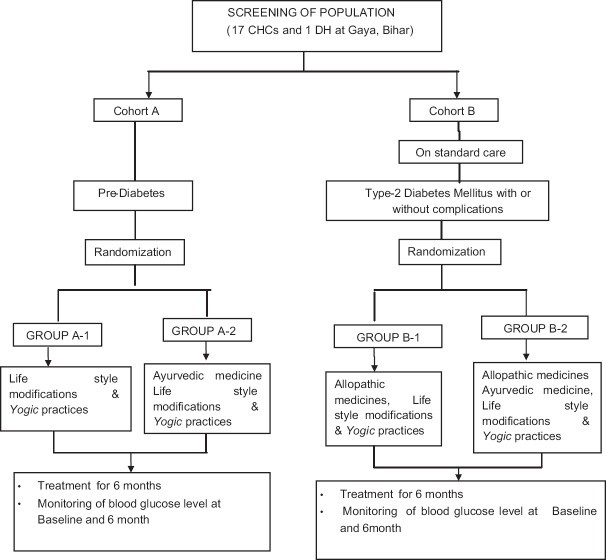
A multi-centric, open-labeled, prospective, comparative clinical study was conducted at 17 community health centers and 1 district hospital. Population over 30 years of age was screened and prediabetic or type 2 diabetic individuals were enrolled in two cohorts, i.e., pre-diabetic (Cohort A) and type 2 diabetic (Cohort B). Each cohort was further divided into two groups: Group A1 was advised for lifestyle modification and Yoga and group A2 was given Ayurveda medication in addition to lifestyle modification and Yoga. Similarly, group B1 was advised for lifestyle modification and Yoga along with allopathic medication and group B2 was given Ayurveda medication, i.e., Mamajjaka, Amalaki and Guduchi powder in addition to lifestyle modification and Yoga along with allopathic medication. Treatment was given for 6 months. Data were analyzed through paired t-test.
Results:
A significant reduction was observed in fasting blood sugar level in groups A2 and B2 (P = 0.001) and also in the postprandial blood sugar level in Groups A2 and B2 (P = 0.001). Further, improvement in subjective symptoms such as polyuria, polydipsia, polyphagia, blurred vision and weakness was found in all the groups, while non-healing ulcer does not show any improvement.
Conclusion:
The study reveals that Ayurveda intervention, i.e., Mamajjaka Churna (1 g), Amalaki Churna (3 g) and Guduchi Churna (3 g) two times a day effectively controls blood sugar level in pre-diabetic and type 2 diabetic patients and improves the disease management with lifestyle modification and Yogasana as well as with allopathic treatment.
Keywords: Ayurveda, Madhumeha, Noninsulin-dependent diabetes mellitus, Prameha, type 2 diabetes
Introduction
Non-communicable diseases (NCDs) kill 41 million people each year, equivalent to 71% of all deaths globally.[1] According to the ICMR India State-Level Disease Burden Study report “India: Health of the Nation’s States,” the estimated proportion of all deaths due to NCDs has increased from 37.09% in 1990 to 61.8% in 2016.[2] The number of people with diabetes has risen from 108 million in 1980 to 422 million in 2014. The global prevalence of diabetes among adults over 18 years of age has risen from 4.7% in 1980 to 8.55% in 2014. Almost half of all deaths were attributable to high blood glucose and occurred before the age of 70 years.[3] Physical inactivity, faulty diet, sedentary lifestyle habits and stress are the major risk factors of noninsulin-dependent diabetes. The main aim of the management of diabetes is to lower the blood glucose level either by intervention of medicine or by improving behavior of diet and lifestyle.
Ayurveda emphasized on the management of Prameha through diet and lifestyle modification (which can be correlated to diabetes).[4] Studies have also shown the effectiveness of Ayurveda intervention in the management of type 2 diabetes.[5]
Global report on diabetes (2016) by the WHO[6] and the National Health Policy (2017)[7] emphasized on the integrated management of NCDs. Keeping in view the strength of AYUSH systems for the prevention and management of NCDs by promoting healthy lifestyle, a project aimed for “Integration of AYUSH (Ayurveda) with National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke (NPCDCS)” was conceived in 2015 by the Ministry of AYUSH and Central Council for Research in Ayurvedic Sciences (CCRAS) in collaboration with Directorate General of Health Services, Ministry of Health and Family Welfare (MoHFW), for imparting health services on pilot basis in the three districts of three states, namely Bhilwara (Rajasthan), Gaya (Bihar) and Surendranagar (Gujarat).[8] The present article reports interim analysis of the patient outcome through integrated management of diabetes (from April 2016 to December 2017) at 17 community health centers (CHCs) and 1 district hospital (DH) of Gaya district.
Objectives
The objective of this study was to analyze the effect of Ayurveda intervention, lifestyle modification and Yoga in the management of type 2 diabetes under NPCDCS-AYUSH integration project.
Materials and Methods
A multicenter, open-labeled study was conducted at 17 CHCs and 1 DH in Gaya district of Bihar. A total number of 1,04,627 individuals were screened for type 2 diabetes at 17 CHCs and 1 DH between April 2016 and December 2017 and out of them, a total of 7735 participants were enrolled as prediabetic and type 2 diabetic patients for integrated management between April 2016 and December 2017. The data of all those patients who completed the management of 6 months, i.e. 3044 patients were included in the analysis. Dropped out cases were 2049 and the rest of 2642 patients were at different phases of management as it is a ongoing project.
Enrolled patients were distributed in two cohorts: pre-diabetic, i.e., Cohort A and type 2 diabetic, i.e. Cohort B. Each cohort was further divided into two groups, i.e. A1 and A2 and B1 and B2 as follows:
Group A1 was advised for lifestyle modification and Yoga
Group A2 was given Ayurveda medication, lifestyle modification and Yoga
Group B1 was advised for lifestyle modification and Yoga along with allopathic medication
Group B2 was given Ayurveda medication, lifestyle modification and Yoga along with allopathic medication.
Ethical clearance
The study protocol was approved by the Institutional Ethical Committee (15-1/IMR/RARIID/Patna/17-18/835 dated on June 10, 2017) and written informed consent was also taken before enrollment for intervention.
The case record forms (CRFs) and electronic format (E-format) were designed for recording the data of registered patients. The schematic diagram of the project is depicted in Figure 1.
Figure 1.
Scheme of categorization of patients
Diagnostic criteria
Cohort A: The Indian Diabetic Risk Score (IDRS)[9] 30–60 and adults with impaired fasting glucose as per the American Diabetes Association (ADA)[10] criteria (fasting plasma glucose [FPG] level between 100 and 125 mg/dL).
Cohort B: IDRS >60, adults with FPG ≥126 mg/dl (7.0 mmol/l), or patients with classical symptoms of hyperglycemia or hyperglycemic crisis having random plasma glucose ≥200 mg/dl (11.1 mmol/l) as per the ADA[10] criteria and patients of type 2 diabetes with or without complications on standard care of treatment.
Inclusion criteria
Cohorts A and B: Patients of either sex aged between 30 and 60 years and those who are willing to give written informed consent were included.
Exclusion criteria
Cohorts A and B: Known cases of HIV positive; type 1 diabetic individuals; patients having a history of cardiovascular diseases such as bundle branch block, transient ischemic attack, uncontrolled hypertension and stroke; patients who have undergone recent or significant abdominal surgery (e.g., gastrectomy) during the past 6 months; patients on corticosteroids and hormonal treatment; pregnant and lactating mothers and patients having any major systemic illness were excluded.
The registered patients were provided the treatment as per their study cohort for 6 months as shown in Figure 2. The laboratory investigations such as fasting blood sugar (FBS), postprandial blood sugar (PPBS) and hemoglobin A1C (HbA1C) were conducted (as per the availability of investigations facilities with state health authorities) at baseline and at the end of 6th month.
Figure 2.
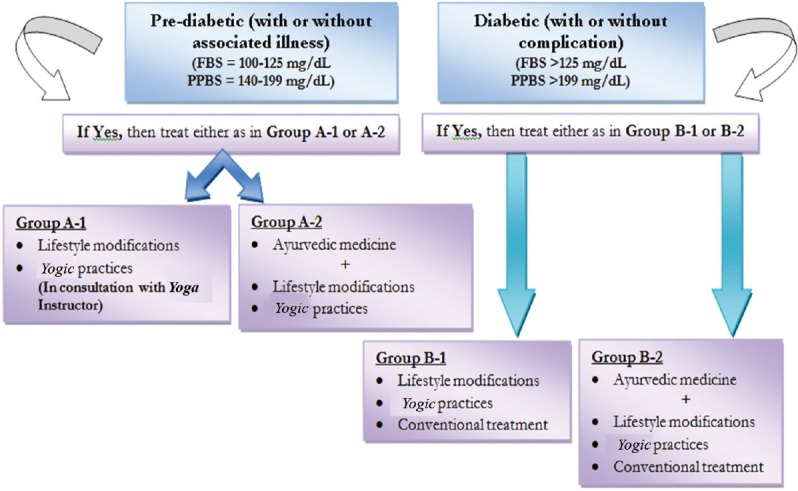
Methodology for enrollment of patients
Withdrawal criteria
Patients with irregularity in follow-up or missing consecutive three follow-ups
Noncompliance of treatment protocol
Developed any serious side effect.
Pharmacological interventions
Keeping in view of classical texts and various research studies, the Mamajjaka capsule (powdered dried whole plant of Enicostemma littorale Blume) 1 g, Amalaki Churna (powdered dried fruit of Emblica officinalis Gaertn.) 3 g and Guduchi Churna (powdered dried stem of Tinospora cordifolia (Willd.) Miers.) 3 g twice a day after meals with lukewarm water were administered for the management of type 2 diabetes. The medicines were procured from Good Manufacturing Practices (GMP) certified Ayurvedic pharmaceutical companies as per pharmacopoeial standards. The medicines were prescribed for 6 months.
The list of common allopathic medications prescribed by the allopathic physicians for type 2 diabetic patients in the study contains chlorpropamide, tolbutamide, glibenclamide, glibornuride, tolazamide, glipizide, gliclazide and metformin.
Diet and lifestyle modification
The details of the advocacy on diet and lifestyles on diabetes are shown in Table 1.
Table 1.
Details of advocacy on diet and lifestyles for pre-diabetic and type 2 diabetes patients
| Do’s | Dont’s |
|---|---|
| Intake of old harvested cereals, barley (Yava), sorghum (Jwar), whole wheat atta, bitter gourd (Karela), green leafy vegetables, garlic (Rasona), turmeric (Haridra), Aloe vera (Kumari) in vegetables (leafy) and fruits such as guava, oranges and Indian blackberry (Jammbu Phala) Timely intake of diet Regular exercise, especially walking Regular practice of Yoga, meditation, etc., under the supervision of Yoga specialist is suggested |
Sugarcane juice, jaggery, sugar, milk products Reduce intake of rice, food rich in carbohydrate and fried, or processed food Sedentary lifestyle Sleeping in the daytime and excessive sleeping Alcohol consumption Staying too long on empty stomach Cold drinks, ice cream, burger-pizza and other fast foods. |
Yogasana intervention for prediabetic and type 2 diabetes
A list of selected Asana/Kriya/Pranayama was advocated under the supervision of Yoga experts for practice by enrolled patients depending on the age and severity of disease, as mentioned in Table 2.
Table 2.
Details of Asana/Kriya/Pranayama advocated
| Yogasana | Pranayama | Kriya |
|---|---|---|
|
Surya Namaskar, Tadasana, , Sarvangasana, Halasana, Matsyasana, Ushtrasana, Gomukhasana, Ardha Matsyendrasana, Mandukasana, Paschimottanasana, Pawanmuktaasana, Bhujangasana, Shalabhasana, Dhanurasana, Vajrasana, Shavasana |
Nadi Shodhana, Suryabhedi, Bhastrika |
Kunjal, Kapalabhati, Agnisara |
Assessment criteria
Blood sugar level: As per ADA, the fasting and PPBS levels were measured at baseline and the 6th month
-
Subjective symptoms of type 2 diabetes such as polyuria, polydipsia, polyphagia, weakness, non-healing ulcer and blurred vision of the individual patients were measured on following scoring:
- Absent: 0 Mild: 1 Moderate: 2 Severe: 3
-
Changes in subjective symptoms after treatment:
- Static: No change in subjective symptoms at 6th month from baseline
- Improved: Improvement in subjective symptoms at 6th month from baseline
- Worse: Increase in severity of subjective symptoms at 6th month from baseline.
Statistical analysis
The demographic variables and chief complaints have been presented in percentage. The continuous data for blood glucose level within the group related to outcome variables were subjected to paired t-test. P <0.05 has been considered as statistically significant.
Results and Observations
Study cohort
A total of 7735 participants (56 in group A1, 1565 in group A2, 43 in group B1 and 6071 in group B2) were enrolled as prediabetic and type 2 diabetic patients for the integrated management during April 2016 to December 2017. The data of patients who had completed the management of 6 months, i.e., 3044 patients (15 in group A1, 487 in group A2, 13 in group B1 and 2529 in group B2) were included in the analysis. Dropped out cases were 2049 (13 in group A1, 546 in group A2, 7 in group B1 and 1483 in group B2) and the rest of 2642 patients (28 in group A1, 532 in group A2, 23 in group B1 and 2058 in group B2) were at different phases of management as it is a continuous running project. Figure 3 shows the outflow of patients in the study from April 2016 to December 31, 2017.
Figure 3.
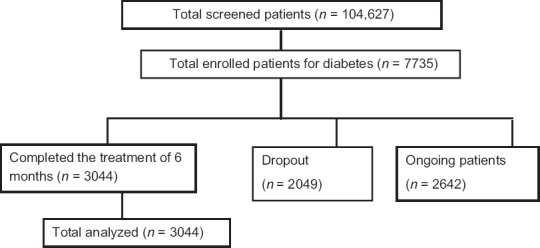
Outflow of the patients in the study
The study revealed that maximum patients (68.4%) were male in gender and the mean age of all the patients was between 45 and 54 years. About 25.4% of patients were illiterate, followed by 19.6% of patients who were educated above senior secondary. Almost 32.2% were homemakers. The baseline demographic data of the patients are summarized in Table 3.
Table 3.
Baseline characteristics of the study participants (n=3044) (Demographics)
| Variables | n (%) |
|---|---|
| Mean age (year) | 45-54 |
| Gender | |
| Male | 64.8 |
| Female | 35.2 |
| Education | |
| Illiterate | 25.4 |
| Up to primary | 14.7 |
| Up to middle | 21.7 |
| Up to senior secondary | 18.5 |
| College and above | 19.6 |
| Occupation | |
| Desk work | 14.7 |
| Field work | 28.6 |
| Homemaker | 32.2 |
| Others | 24.5 |
Effect of management of type 2 diabetes on subjective symptoms
Changes in subjective symptoms after treatment were assessed with following criteria:
Static: No change in subjective symptoms at 6th month from baseline
Improved: Improvement in subjective symptoms at 6th month from baseline
Worse: Increase in severity of subjective symptoms at 6th month from baseline.
The effect of management of type 2 diabetes on subjective symptoms is depicted in Graphs 1–6 and Table 4.
Graph 1.
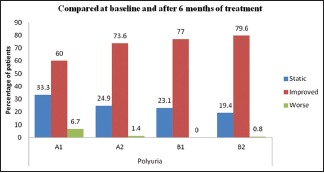
The effect of intervention on the symptom of polyuria, n=3044
Graph 6.
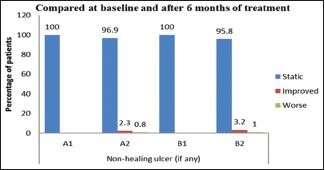
The effect of intervention on the symptom of non-healing ulcer
Table 4.
The effect of management of type 2 diabetes on subjective symptoms and signs
| Complaint | Group | Static (%) | Improved (%) | Worsened (%) |
|---|---|---|---|---|
| Polyuria | A1 | 33.3 | 60.0 | 6.7 |
| A2 | 24.9 | 73.6 | 1.4 | |
| B1 | 23.1 | 77.0 | 0.0 | |
| B2 | 19.4 | 79.6 | 0.8 | |
| Polydipsia | A1 | 40.0 | 60.0 | 0.0 |
| A2 | 23.3 | 76.0 | 0.8 | |
| B1 | 15.4 | 84.7 | 0.0 | |
| B2 | 20.7 | 78.4 | 0.9 | |
| Polyphagia | A1 | 46.7 | 46.7 | 6.6 |
| A2 | 38.8 | 59.4 | 1.8 | |
| B1 | 53.9 | 46.2 | 0.0 | |
| B2 | 34.0 | 64.8 | 1.1 | |
| Weakness | A1 | 26.6 | 73.3 | 0.0 |
| A2 | 29.1 | 68.4 | 2.4 | |
| B1 | 15.4 | 84.7 | 0.0 | |
| B2 | 22.2 | 75.4 | 1.7 | |
| Blurred vision | A1 | 46.7 | 46.7 | 6.6 |
| A2 | 64.1 | 33.5 | 2.5 | |
| B1 | 53.9 | 46.2 | 0.0 | |
| B2 | 57.6 | 39.5 | 2.8 | |
| Nonhealing ulcer (if any) | A1 | 100.0 | - | - |
| A2 | 96.9 | 2.3 | 0.8 | |
| B1 | 100.0 | - | ||
| B2 | 95.8 | 3.2 | 1.0 |
Graph 2.
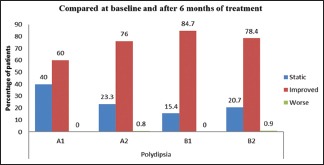
The effect of intervention on the symptom of polydipsia, n=3044
Graph 3.
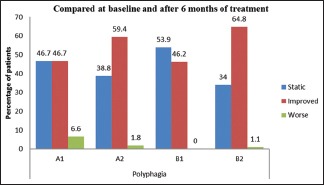
The effect of intervention on the symptom of polyphagia, n=3044
Graph 4.
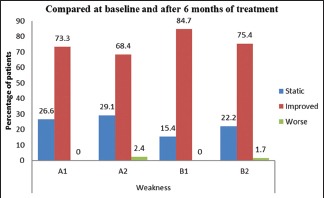
The effect of intervention on the symptom of weakness
Graph 5.
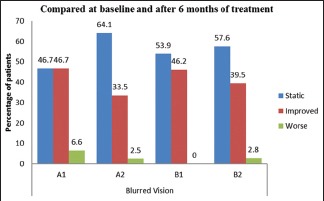
The effect of intervention on the symptom of blurred vision
Grading of the symptoms of type 2 diabetes, i.e., polyuria, polydipsia, polyphagia, weakness, blurred vision and non-healing ulcer was done at baseline and the 6th month and recorded in CRFs.
Effect of integrative management
The effect of integrative management in blood sugar level is shown in Table 5 and Graphs 7, 8. A significant reduction in the FBS level was observed from baseline to 6 months after intervention of integrative management in groups A2, B1 and B2, whereas non-significant reduction in the FBS level was observed in group A1. It was also observed that there was a significant reduction in the PPBS level from baseline to 6 months in groups A2, B1 and B2, whereas non-significant reduction in the FBS level was observed in group A1.
Table 5.
Effect on fasting blood sugar and postprandial blood sugar
| Parameters | Groups | 0 day (BT)-after 6 months (AT) | Paired differences | t | P | ||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | SEM | 95% CI of the difference | ||||||
| Lower | Upper | ||||||||
| Blood sugar fasting (mg/dl) | Group A1 | BT | 120.32 | 6.117 | 2.735 | −11.435 | 39.675 | 1.534 | 0.200 |
| AT | 106.20 | 21.534 | 9.630 | ||||||
| Group A2 | BT | 108.85 | 10.894 | 1.168 | 8.076 | 14.990 | 6.663 | <0.001 | |
| AT | 97.32 | 12.402 | 1.330 | ||||||
| Group B1 | BT | 128.80 | 28.940 | 9.152 | 2.915 | 34.685 | 2.677 | 0.025 | |
| AT | 110.00 | 13.367 | 4.227 | ||||||
| Group B2 | BT | 163.59 | 56.190 | 1.620 | 48.692 | 54.758 | 33.456 | <0.001 | |
| AT | 111.87 | 24.098 | 0.695 | ||||||
| Blood sugar postprandial (mg/dl) | Group A1 | BT | 168.85 | 43.091 | 17.592 | −47.952 | 54.985 | 0.176 | 0.867 |
| AT | 165.33 | 33.720 | 13.766 | ||||||
| Group A2 | BT | 169.13 | 21.598 | 1.619 | 19.918 | 28.974 | 10.653 | <0.001 | |
| AT | 144.68 | 24.345 | 1.8525 | ||||||
| Group B1 | BT | 205.00 | 42.834 | 14.278 | 12.494 | 64.617 | 3.412 | 0.009 | |
| AT | 166.44 | 33.313 | 11.104 | ||||||
| Group B2 | BT | 244.39 | 76.309 | 2.036 | 83.097 | 91.084 | 42.780 | <0.001 | |
| AT | 157.30 | 35.789 | 0.955 | ||||||
CI: Confidence interval, SD: Standard deviation, SEM: Standard error of mean, AT: After Treatment, BT: Before Treatment, n=3044
Graph 7.
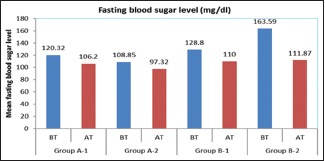
The effect of integrative management on fasting blood sugar level
Graph 8.
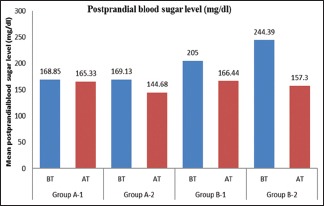
The effect of integrative management on postprandial blood sugar level
Discussion
The trial drugs, i.e., Mamajjaka, Amalaki and Guduchi were found effective in controlling FBS and PPBS levels in type 2 diabetic individuals. Mamajjaka is a folklore drug which has been practiced since long time for the management of Prameha in India. Various studies have documented the potential role of Mamajjaka in controlling blood sugar levels.[11] It possesses Bitter Taste (Tikta Rasa)[12] which is known to help in stimulating metabolism.
Amalaki and Guduchi are documented in the Ayurvedic Pharmacopoeia of India to possess anti-diabetic activity.[13,14] Further, Amalaki and Guduchi impart rejuvenating (Rasayana) effect that causes improvement in digestive functions and metabolism, thus enhancing glucose uptake by the cells. Amalaki is a rich source of Vitamin C and amino acids[15] and possesses immune-modulatory effect[16] and antioxidant activity.[17] Studies reported that Guduchi enhances glucose tolerance and lowers the blood glucose level.[18] It possesses antioxidant activity.[19]
Lifestyle modification contributes to the effect of Ayurveda medications as proper diet, abstinence of substance abuses such as tobacco and alcohol and management of daily routines will remove the causative factors of disease and help in preventing progression of disease.
Yoga has been practiced since ancient times to manage the physiology of the body. This not only improves the flexibility but also improves the function of both endocrines and exocrine glands of the body. Various studies have reported that Yoga has a positive impact in the management of type 2 diabetes. Different Asanas such as Surya Namaskara and Tadasana help in insulin production and improve digestive fire. Cleansing process in Yoga Kriya like Kapalnbhati and Agnisara stimulates pancreatic cells and improves their efficiency.[20]
Subjective symptoms of type 2 diabetes, i.e. polyuria, polydipsia, polyphagia, blurred vision, and weakness showed improvement in all the groups. This was possibly due to elimination of causative factors through lifestyle modification and improvement in physiology through Yogic practices. Further, pharmacological intervention controls the blood sugar levels and thus, relief in subjective symptoms was observed. Few patients felt improvement in vision which may be due to retinopathy changes which are nonreversible. Fewer people perceived an improvement in non-healing ulcer. This is possibly because of requirement of localized treatment of the ulcer tissue.
On comparing the P values of the four groups in FBS, it was observed that though lifestyle and Yoga have a positive impact over the disease management, the groups having medical intervention in the form of Ayurveda or allopathic medicine, i.e. groups A2, B1 and B2 performed better than group A1. This implies that lifestyle and Yoga can prevent disease progression through removal of causative and aggravating factors, but pharmacological intervention is required to manage the disease. Yoga regulates eating pattern and leads to medication adherence.[20] Diet plays an important role in the management of every disease as medicine is effective only in the presence of proper diet.[21]
Similarly, groups having Ayurveda medication, i.e., groups A2 and B2 showed better treatment outcome than group B1 which is having allopathic medicine along with lifestyle and Yoga in diseased cases. This signifies that type 2 diabetic patients responded better to Ayurveda medications, i.e., Mamajjaka, Amalaki and Guduchi in the current study. The reasons for better response may be multi-modal action of Ayurveda medications which not only relieve the symptoms but also stimulate the glands, rejuvenate the cells, and improve the uptake of glucose in the body and may probably increase insulin sensitivity. Similar observations were also observed during analysis of PPBS levels.
This highlights the importance of management of type 2 diabetes through integrative approach with Ayurveda medications that help to correct the vitiated Dosha and help in improving metabolism as reflected through the laboratory parameters and subjective parameters. Thus, Ayurveda intervention exhibits potential for integrative management along with lifestyle modifications, Yoga and allopathic anti-diabetic agents.
The acceptance of Ayurveda intervention was overwhelming among population as depicted by large proportion of participants in groups A2 and B2, where Ayurveda medication was prescribed. Further, a number of participants in the groups without Ayurveda medications were very less. The reason may be the inclination of individuals for pharmacological treatment of type 2 diabetes mellitus.
Limitations of the study
The laboratory investigations such as serum insulin HbA1C, fasting and PPBS are the key factors in diagnosis and analysis of the result of the study, but there was restricted availability of in-house and outsourced laboratory facilities at every CHCs well in time.
Conclusion
The study reveals that Ayurveda intervention, i.e. Mamajjaka Churna (1 g), Amalaki Churna (3 g) and Guduchi Churna (3 g) two times/day effectively controls blood sugar level in pre-diabetic and type 2 diabetic patients and improves the disease management with lifestyle modification and Yogasana as well as with allopathic treatment.
Way forward
Further studies should be carried out for the assessment of quality of life during integrative management
The present study shows an increased flow of participants in groups having medical intervention. This implies a psychological aspect of taking some medication along with lifestyle modification and Yoga for the treatment of type 2 diabetes. Hence, to get comparable number of participants in each group, further studies may be planned with a placebo in those groups where only lifestyle modification and Yoga had been prescribed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.World Health Organization. Media Centre. Non Communicable Diseases, Key Facts. Geneva: World Health Organization; 2017. [Last accessed on 2017 Jun 21]. Available from: http://www.whoint/mediacentre/factsheets/fs355/en/ [Google Scholar]
- 2.Indian Time Lifestyle Diseases in India. Press Information Bureau on Lifestyle Diseases in India, Ministry of health and Family Welfare. Government of India; 2018. Jul 31, [Last accessed on 2019 Mar 28]. Available from: http://pib.nic.in/newsite/PrintRelease.aspx?relid=181254 . [Google Scholar]
- 3.World Health Organization. News Room, Key Facts on Diabetes. Geneva: World Health Organization; 2018. Oct 30, [Last accessed on 2019 Mar 28]. Available from: https://www.who.int/news-room/fact-sheets/detail/Diabetes . [Google Scholar]
- 4.Guddoye G, Vyas M. Role of diet and lifestyle in the management of Madhumeha. Ayu J. 2013;34:167–73. doi: 10.4103/0974-8520.119672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Panda AK, Ratha KK, Rao MM. Efficacy of ayurveda formulation ayush-82 (IME-9) in newly diagnosed type 2 diabetics: Retrospective analysis of individual data. J Tradit Med Clin Natur. 2017;6:250. [Google Scholar]
- 6.World Health Organization. Global Report on Diabetes. Geneva: World Health Organization; 2016. [Last accessed on 2019 Mar 28]. Available from: https://appswhoint/iris/bitstream/handle/10665/204871/9789241565257_engpdf;jsessionid=CED989698 77EE5310607A3D169502AC7?sequence=1 . [Google Scholar]
- 7.National Health Policy. Non Communicable Diseases. New Delhi: Ministry of Health and Family Welfare, Government of India; 2017. [Last accessed on 2019 Mar 28]. p. 13. Available from: www.nhp.gov.in/NHPfiles/national_health_policy_2017.pdf . [Google Scholar]
- 8.Singh R, Ota S, Khanduri S, Rani S, Bhadula A, Sharma R, et al. Integration of ayush (AYURVEDA and yoga) with national programme for prevention and control of cancer, diabetes, cardiovascular diseases and stroke (NPCDCS): An appraisal of central council for research in ayurvedic sciences research and development initiatives. J Res Ayurvedic Sci. 2018;2:27–36. [Google Scholar]
- 9.Joshi SR. Indian diabetes risk score. J Assoc Physicians India. 2005;53:755–7. [PubMed] [Google Scholar]
- 10.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33(Suppl 1):S62–9. doi: 10.2337/dc10-S062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Surse YS, Raut A, Phartale VD, Shinde KP. Controlled clinical evaluation of “mamajjak choorna” in sthula madhumeha Viza-Viz type 2 diabetes mellitus. Int J Ayurveda Pharm Res. 2017;5:26–31. [Google Scholar]
- 12.Tanna SP, Patgiri B, Shukla VJ, Prajapati PK. Pharmaceutical standardization of mamajjaka (Enicostemma littorale Auct. non Bl) Ghana Ayu. 2012;33:294–8. doi: 10.4103/0974-8520.105255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Anonymous. The Ayurvedic Pharmacopoeia of India. Part. I., Vol. 1. New Delhi: Department of AYUSH, Government of India Ministry of Health and Family Welfare; 1990. pp. 5–8. [Google Scholar]
- 14.Anonymous. The Ayurvedic Pharmacopoeia of India. Part. I., Vol. I. New Delhi: Department of AYUSH, Government of India Ministry of Health and Family Welfare; 1990. pp. 53–5. [Google Scholar]
- 15.Anonymous. The Wealth of India, Dictionary of Indian Raw Materials and Industrial Products, First Supplement Series, Raw Materials. D-1. Vol. 3. Reprinted edition. New Delhi: National Institute of Science Communication and Information Resource; 2009. pp. 75–8. [Google Scholar]
- 16.Suja RS, Nair AM, Sujith S, Preethy J, Deepa AK. Evaluation of immunomodulatory potential' of Emblica officinalis fruit pulp extract in mice. Indian J Anim Res. 2009;43(2):103–6. [Google Scholar]
- 17.Jeena JK, Kuttan, Ramadasan Antioxidant activity of Emblica officinalis. J Clin Biochem Nutr. 1995;19:63–70. [Google Scholar]
- 18.Gupta SS, Varma SC, Garg VP, Rai M. Antidiabetic effect of Tinospora cordifolia. I. effect on fasting blood sugar level, glucose tolerence and adrenaline induced hyperglycemia. Indian J Exp Biol. 1967;55:733–45. [PubMed] [Google Scholar]
- 19.Stanely Mainzen Prince P, Menon VP. Antioxidant action of Tinospora cordifolia root extract in alloxan diabetic rats. Phytother Res. 2001;15:213–8. doi: 10.1002/ptr.707. [DOI] [PubMed] [Google Scholar]
- 20.Raveendran AV, Deshpandae A, Joshi SR. Therapeutic role of yoga in type 2 diabetes. Endocrinol Metab (Seoul) 2018;33:307–17. doi: 10.3803/EnM.2018.33.3.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pandey K. Commentator. Vaidya Jivanam of Lolimbaraja. Ch. 1. Ver. 10. 2nd ed. Varanasi: Chaukhamba Sanskrit Series Office; 1947. p. 4. [Google Scholar]