Abstract
Background
Antimicrobial resistance has become one of the most severe global threats to human and veterinary Medicine. colistin is an effective therapeutic agent against multi-drug-resistant pathogens. However, the discovery of transferable plasmids that confer resistance to colistin (mcr-1) has led to challenges in medical science. This study describes the role of wild birds in the harbouring and environmental spread of colistin-resistant bacteria, which could pose a potential hazard to human and animal health.
Methods
In total, 140 faecal samples from wild birds (migratory and resident birds) were tested. Twenty surface water samples were collected from the area in which wild bird trapping was conducted, and 50 human stool samples were collected from individuals residing near the surface water sources and farm buildings. Isolation and identification of Enterobacteriaceae and Pseudomonas aeruginosa from the different samples were performed using conventional culture techniques and biochemical identification. PCR amplification of the mcr genes was performed in all positive isolates. Sequencing of mcr-1 genes from three randomly selected E. coli carrying mcr-1 isolates; wild birds, water and humans was performed.
Result
The bacteriological examination of the samples showing isolates of Escherichia coli, Klebsiella pneumoniae, Klebsiella oxytoca and P. aeruginosa. The results of multiplex PCR of the mcr genes revealed that E. coli was the most prevalent gram-negative bacterium harbouring the mcr genes, whereas a low prevalence was observed for K. pneumoniae. The prevalence of mcr-1 in resident birds, migratory birds, water sources and humans were 10.4, 20,16.6 and 9.6% while the prevalence of mcr-2 were 1.4, 3.6, 11.1 and 9.6%, respectively. Sequencing of the mcr-1 gene from the three E. coli carrying mcr-1 isolates indicated a possible correlation between the wild bird and surface water isolates.
Conclusion
The detection of mcr-1-positive bacteria in wild birds in Egypt indicates the possible environmental dissemination of this gene through bird activity. The impact of the interaction between domestic and wild animals on public health cannot be overlooked.
Keywords: Wild bird, Enterobacteriaceae, P. aeruginosa, mcr genes, Egypt
Background
Antimicrobial resistance (AMR) has become one of the most severe global threats to human and veterinary medicine. This crisis has been catalysed by the rapid emergence of carbapenemase-producing Enterobacteriaceae expressing enzymes such as KPC-2 (Klebsiella pneumoniae carbapenemase-2) and NDM-1 (New Delhi metallo-β-lactamase-1) [1, 2].
Colistin is considered the last resort for the treatment of severe infections caused by multi-drug-resistant bacteria. Thus, the global increase in carbapenemase-producing Enterobacteriaceae has resulted in the overuse of colistin with the inevitable risk of emerging resistance [3].
Recently, resistance to colistin has been linked to not only chromosomal mutations but also plasmid-mediated mechanisms [4, 5]. Unfortunately, the presence of colistin resistance on mobile genetic elements poses a significant public health risk, as these elements can spread rapidly via horizontal transfer [6]. A transferable plasmid that confers resistance to colistin (movable colistin resistance 1, mcr-1) was first discovered in Escherichia coli, K. pneumoniae and Pseudomonas aeruginosa strains from China between April 2011 and November 2014 [7]. In addition, the mcr-1 gene has also been observed on plasmids containing other AMR genes, such as genes encoding carbapenemases [8, 9] and extended-spectrum β-lactamases [10–12]. Many studies have attributed the emergence and silent dissemination of plasmid genes involved in polymyxin resistance to the current use of colistin as an antibiotic growth promoter (AGP) in livestock [13].
The presence of bacteria of potential zoonotic importance among migratory and non-migratory wild birds has public health significance. The bird migration provides a mechanism for the establishment of new endemic foci of disease at great distances from the site of acquisition of and infection [14]. Therefore, migratory and non-migratory wild birds could serve as reservoirs of resistant bacteria and genetic factors associated with AMR [15].
Although the origin of bacterial resistance genes in wild animals remains unclear, as wildlife are not exposed to antibiotics directly, contact with sewage or animal manure might a possible source [16]. Moreover, contact with water and feeding habits seem to be the main factors affecting the transmission of resistant bacteria from humans or veterinary sources to wild animals [17, 18]. This gap in knowledge highlights the complexity of bacterial resistance in wild animals, which act as reservoirs and vectors of resistant bacterial pathogens, and the possible interspecies transmission among humans, domestic animals, the environment, and wildlife [17]. Therefore, new health problems in wildlife populations have emerged, and novel reservoirs of zoonotic diseases have formed.
The aim of this study was to obtain a detailed understanding of the possibility that migratory and non-migratory wild birds can harbour and spread colistin-resistant bacteria, which could pose a potential risk to human and animal health by transmission of antimicrobial-resistant strains to waterways and environmental sources through faecal deposits.
Materials and methods
Sample preparation
A total of 140 faecal samples were collected from 80 resident wild birds (20 hooded crows, 20 cattle egrets, 20 rock pigeons and 20 laughing dove) and 60 migratory waterfowls (20 shoveler ducks, 20 Cotte ducks and 20 green-winged teal ducks) were collected from Giza, Cairo, El-Sharkia, El-Ismailia and Port-said governorates in Egypt (Fig. 1) during the period from August 2017 to January 2018. Modified traps were used to capture wild birds and migratory waterfowls during winter migration. After trapping, faecal swabs were taken, and the birds were released. The swabs were then placed in 2 ml of sterile saline (0.9% NaCl) and stored in an ice box until being transported to the laboratory.
Fig. 1.

Location of sampling points in Egypt
Twenty Surface water samples from 20 different sources (1 from each) were collected in sterile glass bottles in the area in which wild-bird trapping was conducted. Upon arrival, all water samples were filtered using a membrane filtration method, which was carried out according to American Public Health Association (APHA) [19]. In this procedure, 100-ml water samples were drawn through a vacuum filtration apparatus containing a sterile filter membrane with a pore size of 0.45 μm (Sartorius, France), which retained bacteria, and then, the filters were vortexed in peptone broth to recover the bacteria. After removing the filters, the bacteria were cultivated at 37 °C for 24 h.
Fifty human stool specimens were gathered from apparently healthy farmers residing near the surface water sources and farm buildings in the area in which wild-bird trapping was conducted. Samples were taken with sterile swabs, and the swabs were transferred to tubes containing trypticase soy broth and incubated at 37 °C for 24 h.
Bacterial isolation and identification
A loopful of all the previously inoculated broths was cultured on eosin methylene blue (EMB) agar (Oxoid, Oxoid Ltd., London) for isolation of Enterobacteriaceae other than salmonellae. Pseudomonas agar base with CN supplement (Oxoid) was used for the selective isolation of P. aeruginosa. All the inoculated plates were incubated aerobically at 37 °C for 24 h. Suspected colonies were picked and examined for morphological and culture characteristics according to Quinn et al. [20].
The API 20E and API 20NE kits (BioMerieux, France) were used according to the manufacturer’s instructions to detect the biochemical profiles of the isolated Enterobacteriaceae and P. aeruginosa, respectively.
Molecular identification mcr-1 and mcr-2
All isolates obtained from the examined samples were subjected to genotyping using multiplex polymerase chain reaction (PCR) according to Cavaco et al. [21].
The template DNA used consisted of boiled lysates prepared from the isolates. In brief, a loopful of culture was suspended in 100 μl of sterile TE buffer, boiled for 10 min at 100 °C, and centrifuged for 5 min at 6000×g. The extracted DNA was stored at − 20 °C until use.
PCR was performed on the extracted DNA, wherein two genes were targeted as described in Table (1). PCR amplification was performed using 2 μl of the DNA template, 25 μl of 2× DreamTaq DNA PCR Master Mix (Thermo Scientific, Waltham, USA), and 2 μl of each primer at a concentration of 2 μM, and nuclease-free water was added up to 50 μl.
Additionally, PCR reaction was done using E. coli carrying mcr-1 (ID: 2012-60-1176-27) and E. coli containing mcr-2 (ID: KP37) as a positive control, while water sample was used as a negative control.
The thermal profile of the reaction was as follows: initial denaturation at 94 °C for 15 min, 25 cycles of denaturation at 94 °C for 30 s, annealing at 58 °C for 90 s, and extension at 72 °C for 60 s, followed by a final extension step at 72 °C for 10 min.
Then, gel electrophoresis of the amplified PCR product was performed on a 1.5% agarose gel, which was visualized under ultraviolet light.
Sequence analysis
The amplified fragments of mcr-1 gene from E. coli carrying mcr-1 isolates that randomly selected from migratory bird, human and water in the same locality were purified using the QIAquick Gel Extraction Kit (QIAGEN, Germany) according to the manufacturer’s instructions and sequenced at Promega Lab Technology (Germany) using the forward and reverse primers of the mcr-1 gene listed in Table 1.
Table 1.
List of primer pairs used for the mcr-1 and mcr-2 genes in this study
The gene sequences have been deposited in the National Center for Biotechnology Information (NCBI) GenBank database under the accession numbers MK 530689, MK 620991, MK 620992 for the water, human stool, and migratory bird-derived sequences, respectively.
The genes sequenced in this study were compared with the sequences available in the public domain using the NCBI BLAST server. Publicly available gene sequences were downloaded from NCBI GenBank and aligned using CLUSTALW in BioEdit version 7.0.1.4. Phylogenetic analysis was performed with MEGA version 7 using the neighbour-joining approach. The bootstrap consensus tree was estimated from 1000 replicates.
Ethics statement
Protocols for the collection of samples were conducted in accordance with applicable legislation of the Institutional Animal Care and Use Committee, of the Faculty of Veterinary Medicine, Cairo University, Egypt.
Oral consent was obtained from each abattoir worker participated in the study upon information on the use of hand swab samples.
Result
In total, 140 wild birds were sampled. Bacteriological examination revealed that all the wild birds sampled carried members of the family Enterobacteriaceae, including E. coli, K. pneumoniae, and Klebsiella oxytoca. P. aeruginosa, as a non-Enterobacteriaceae species, was also isolated (Table 2). The occurrence of isolated bacterial species varied among host types (Table 3). Moreover, E. coli, K. pneumoniae, K. oxytoca and P. aeruginosa were also isolated from water and stool samples.
Table 2.
Prevalence of the bacteria isolated from wild birds, water and humans
| Sample | Total number | Isolated bacteria | ||||
|---|---|---|---|---|---|---|
| E. coli | K. pneumoniae | K. oxytoca | P. aeruginosa | |||
| Resident birds | Hooded crow | 20 | 12 (60%) | 4 (20%) | 1 (5%) | 1 (5%) |
| Cattle egret | 20 | 9 (45%) | 1 (5%) | 0 (0%) | 0 (0%) | |
| Rock pigeon | 20 | 10 (50%) | 3 (15%) | 1 (25%) | 3 (15%) | |
| Laughing dove | 20 | 11 (55%) | 11 (55%) | 2 (10%) | 4 (20%) | |
| Total | 80 | 33 (41.2%) | 22 (27.5%) | 4 (5%) | 8 (10%) | |
| Migratory birds | Shoveler duck. | 20 | 9 (45%) | 4 (20%) | 1 (5%) | 6 (30%) |
| Cotte duck | 20 | 12 (60%) | 3 (15%) | 2 (10%) | 2 (10%) | |
| Green-winged teal duck | 20 | 8 (40%) | 2 (10%) | 3 (15%) | 3 (15%) | |
| Total | 60 | 29 (48.3%) | 9 (15%) | 6 (10%) | 11 (18.3%) | |
| Water | 20 | 7 (35%) | 7 (35%) | 1 (5%) | 3 (15%) | |
| Humans | 50 | 10 (20%) | 15 (30%) | 2 (4%) | 4 (8%) | |
Table 3.
Frequencies of colistin resistance genes among different bacterial isolates from different isolation sources
| Sample | Total isolates | Colistin resistance genes | |||
|---|---|---|---|---|---|
| mcr-1 | mcr-2 | Both | |||
| Resident birds | E. coli | 33 | 3 (9.1%) | 0 | 0 |
| K. pneumoniae | 22 | 1 (4.5%) | 0 | 0 | |
| K. oxytoca | 4 | 0 | 0 | 0 | |
| P. aeruginosa | 8 | 3 (37.5%) | 1 (12.5%) | 0 | |
| Total | 67 | 7 (10.4%) | 1 (1.4%) | 0 | |
| Migratory birds | E. coli | 29 | 6 (20.6%) | 1 (3.4%) | 1 (3.4%) |
| K. pneumoniae | 9 | 2 (22.2%) | 1 (11.1%) | 1 (11.1%) | |
| K. oxytoca | 6 | 0 | 0 | 0 | |
| P. aeruginosa | 11 | 3 (27.2%) | 0 | 0 | |
| Total | 55 | 11 (20%) | 2 (3.6%) | 2 (3.6%) | |
| Water | E. coli | 7 | 2 (28.5%) | 1 (14.2%) | 0 |
| K. pneumoniae | 7 | 1 (14.2%) | 1 (14.2%) | 0 | |
| K. oxytoca | 1 | 0 | 0 | 0 | |
| P. aeruginosa | 3 | 0 | 0 | 0 | |
| Total | 18 | 3 (16.6%) | 2 (11.1%) | 0 | |
| Humans | E. coli | 10 | 1 (10%) | 1 (10%) | 0 |
| K. pneumoniae | 15 | 1 (6.6%) | 2 (13.3%) | 1 (6.6%) | |
| K. oxytoca | 2 | 0 | 0 | 0 | |
| P. aeruginosa | 4 | 0 | 0 | 0 | |
| Total | 31 | 2 (6.4%) | 3 (9.6%) | 1 (3.2%) | |
The mcr genes were detected in various E. coli, K. pneumoniae and P. aeruginosa isolates recovered from resident birds and migratory birds, while in this study, the mcr-1 and mcr-2 genes were detected in only E. coli and K. pneumoniae isolates from water sources and human stool samples. In this study, E. coli was the most prevalent gram-negative bacterial species harbouring the mcr genes, whereas a low prevalence was observed in K. pneumoniae and no mcr genes isolated from K. oxytoca.
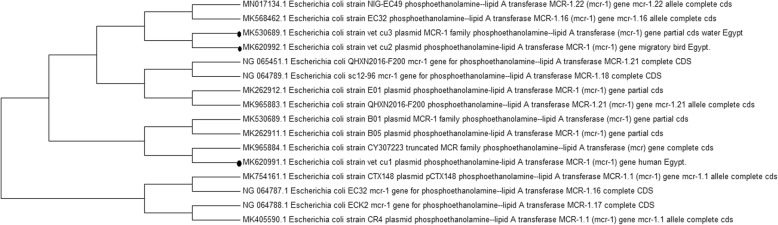
Comparing the sequences of the mcr-1 gene revealed 100% homology between the selected isolates from the wild bird and water isolates, and lack of homology with the human isolate as shown in Fig. 2.
Fig. 2.
Neighbour joining tree showing the relationship between the nucleotide sequences of the partial coding regions of mcr-1 gene. The studied sequences were remark by bullets. The Evolutionary analysis was performed with MEGA version 7
Discussion
The emergence of new infectious diseases in wildlife [24, 25] and the potential threat of these diseases as zoonoses has increased the general interest in birds as vectors of pathogens and their role in disease epidemiology. The lifestyles of migratory birds allow them to carry and disseminate pathogenic and resistant microorganisms across country borders.
In this study, bacteriological examination of resident and migratory birds revealed the presence of E. coli, K. pneumoniae, K. oxytoca and P. aeruginosa. In addition, these bacteria were also recovered from water and human samples.
Special consideration for crows was consistent with Lee et al. [26] who showed that the house crow usually lives close to humans. This bird occupies different ecological niches, including household areas, city dumps, hospital dumps, and water sources such as lakes, ponds, and rivers. Many bird species have been found to carry antibiotic-resistant bacteria. Resistant E. coli have been isolated from ducks, geese [17, 27], cormorants [28, 29], birds of prey [30], gulls [31], doves [32], and passerines [33].
When tracking the source of the mcr-1 gene in previous studies, it was closely related to human activities and movement, while environmental dissemination of this gene was rarely considered and much less the role that migratory birds might play in the process [34, 35].
The first known occurrence of the mcr-1 gene was in E. coli carried by a wild migratory bird, namely, the European herring gull (Larus argentatus) [36], and the first detection of mcr-1 was in colistin-resistant extended-spectrum β-lactamase-producing E. coli (ESBL-E. coli) isolated from the wild transboundary migratory waterfowl species Fulica atra from Pakistan, Asia [37].
The current study showed that mcr genes were detected in E. coli, K. pneumoniae and P. aeruginosa from resident birds and migratory birds (Table 2). The prevalence of mcr-1 in resident birds, migratory birds were 10.4, 20% while the prevalence of mcr-2 were 1.4, 3.6%, respectively. This occurrence of mcr genes in bacterial isolates of resident and migratory birds was surprising. This is because these findings were much higher than that obtained by Ruzauskas et al., [36] who found that the percentage of mcr-1 gene were really low (0.85%) in 117 E. coli isolates recovered from 160 European herring gulls.
E. coli remains the most prevalent gram-negative bacterium harbouring the mcr gene, and these results are consistent with Skov and Monnet [38]. whereas low prevalence was observed in K. pneumoniae; however, the latter pathogen is a leading cause of nosocomial infections globally.
The emergence of resistant bacteria in wildlife may be related to the passage of antibiotic resistance genes to the environment [39]. The possibility of water contamination by bird faeces should be considered an important risk factor for the transmission of resistant bacteria [40, 41].
In this study, the mcr-1 and mcr-2 genes isolated from water sources were 16.6 and 11.1, respectively and these genes were detected only from in E. coli and K. pneumoniae isolates. This result agreed with Wu et al. [41] who detected the mcr-1 gene in three colistin-resistant E. coli isolates, among which two were isolated from river water and one from egret faeces.
The occurrence of mcr genes in bacteria isolated from farmers residing near the area from which surface water and wild bird sampling conducted was confirmed in our study. The persistence of mcr-1 in the human GI tract microflora can cause further contamination of water systems through disposal of waste water containing human faeces [42].
There is no doubt that human intervention plays a substantial role in the development of AMR, as there is a linear correlation between the use of antibiotics and the development of resistance [43]. The zoonotic potential of mcr-1-carrying bacteria has been indicated by many studies [42, 44, 45]. In addition, the dissemination of mcr-carrying bacteria from wild birds and other livestock animals to humans could occur via the food chain or direct contact with animals as well as through contamination of fresh and seawater systems [10, 46].
To determine the correlation between wild birds, water sources and humans, phylogenetic analysis using mcr-1 genes isolated from these sources was performed. The sequences of the mcr-1 genes revealed 100% homology between the sequences from water source and wild-bird isolates, and no homology with human isolates as shown in Fig. 2. This finding indicated the dissemination of this gene between both sources. Moreover, this finding confirmed the role of wild birds in antibiotic resistance as they consider a potential spreader of antibiotic resistance through the ability to migrate long distances in short periods of time and its effect on the environment contamination.
Most of the existing research results have revealed that the dissemination of environmental AMR is closely related to anthropogenic factors. Bacteria seldom develop AMR in regions free from antibiotic pressure and human activities [47]. Moreover, scientists have speculated that migratory animals, especially migratory birds, may carry resistant bacteria or genes and transport them to regions far from anthropogenic influences [48].
The clear limitation of this study was only three isolates were sequenced. Further studies on colistin-resistance co-exists with other resistance patterns (such as carbapenem-resistance) is planned.
Conclusion
This study is the first to detect of mcr-1-positive bacteria in wild birds in Egypt, indicating the possibility of environmental dissemination of this gene through bird activity. In addition to their impact on the environment, the levels of resistance in wild birds tend to correlate with the degree of contact with human activities as they easily accumulate human and environmental bacteria. Zoonotic infections caused by bacteria carrying mcr-1 highlight the urgent need to limit the use of colistin in agriculture and veterinary practices.
Acknowledgements
The authors would like to thank all the slaughterhouse workers in the investigated Egyptian abattoirs for their kind cooperation during sample collection.
Authors’ contributions
All authors contributed to the collection of samples, the molecular detection of the target genes, the analysis and interpretation of the data, as well as writing the manuscript. All authors read and approved the final manuscript.
Funding
The authors declare that they did not receive any funding or grants to support their research.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Ethics approval and consent to participate
The study was conducted according to ethical guidelines approved by the Faculty of Veterinary Medicine, Cairo University. There were no experiments on human participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Zeinab S. Ahmed, Email: Zeinab.ahmed.vet@yahoo.com
Esraa A. Elshafiee, Email: esraa_elshafiee@cu.edu.eg
Hanan S. Khalefa, Email: hanansaad0@gmail.com
Mona Kadry, Email: Vet_moony@yahoo.com.
Dalia A. Hamza, Email: daliahamza@cu.edu.eg
References
- 1.KumarasamyKk TM, Tr W, Bagaria J, Butt F, Balakrishnan R, Krishnan P. Emergence of a new antibiotic resistance mechanism in India, Pakistan, and the UK: a molecular, biological, and epidemiological study. Lancet Infect Dis. 2010;10:597–602. doi: 10.1016/S1473-3099(10)70143-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Munoz-Price LS, Poirel L, Bonomo RA, Schwaber MJ, Daikos GL, Cormican M, Kumarasamy K. Clinical epidemiology of the global expansion of Klebsiella pneumoniae carbapenemases. Lancet Infect Dis. 2013;13:785–796. doi: 10.1016/S1473-3099(13)70190-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Center for Disease Dynamics, Economics & Policy (CDDEP). 2015. ResistanceMap. Accessed on August 20, 2015. Retrieved from www.cddep.org/projects/resistancemap and www.resistancemap.org
- 4.Olaitan AO, Morand S, Rolain J-M. Mechanisms of polymyxin resistance: acquired and intrinsic resistance in bacteria. Front Microbiol. 2014;5:643. [DOI] [PMC free article] [PubMed]
- 5.Lee J-Y, Choi M-J, Choi HJ, Ko KS. preservation of acquired colistin resistance in gram-negative bacteria. Antimicrob. Agents Chemother. 2016;60:609–612. doi: 10.1128/AAC.01574-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carattoli A. Plasmids and the spread of resistance. Int J Med Microbiol. 2013;303:298–304. doi: 10.1016/j.ijmm.2013.02.001. [DOI] [PubMed] [Google Scholar]
- 7.Liu YY, Wang Y, Walsh TR, Yi LX, Zhang R, Spencer J, Yu LF. Emergence of plasmid-mediated colistin resistance mechanism mcr-1 in animals and human beings in China: a microbiological and molecular biological study. Lancet Infect Dis. 2016;16:161–168. doi: 10.1016/S1473-3099(15)00424-7. [DOI] [PubMed] [Google Scholar]
- 8.Poirel L, Kieffer N, Liassine N, Thanh D, Nordmann P. Plasmidmediatedcarbapenem and colistin resistance in a clinical isolate of Escherichia coli. Lancet Infect Dis. 2016;16:281. doi: 10.1016/S1473-3099(16)00006-2. [DOI] [PubMed] [Google Scholar]
- 9.Du H, Chen L, Tang Y-W, Kreiswirth BN, Rolain J-M. Emergence of the mcr-1 colistin resistance gene in carbapenem-resistant Enterobacteriaceae. Lancet Infect Dis. 2016;16:287–288. doi: 10.1016/S1473-3099(16)00056-6. [DOI] [PubMed] [Google Scholar]
- 10.Zhang XF, Doi Y, Huang X, Li HY, Zhong LL, Zeng KJ, et al. Possible transmission of mcr-1-harboring Escherichia coli between companion animals and human. Emerg Infect Dis. 2016;22:1679–1681. doi: 10.3201/eid2209.16046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Falgenhauer L, Waezsada SE, Yao Y, Imirzalioglu C, Käsbohrer A, Roesler U, Chakraborty T. Colistin resistance gene mcr-1 in extended-spectrum β- lactamase-producing and carbapenemase-producing gram-negative bacteria in Germany. Lancet Infect Dis. 2016;16:282–283. doi: 10.1016/S1473-3099(16)00009-8. [DOI] [PubMed] [Google Scholar]
- 12.Haenni Marisa, Poirel Laurent, Kieffer Nicolas, Châtre Pierre, Saras Estelle, Métayer Véronique, Dumoulin Romain, Nordmann Patrice, Madec Jean-Yves. Co-occurrence of extended spectrum β lactamase and MCR-1 encoding genes on plasmids. The Lancet Infectious Diseases. 2016;16(3):281–282. doi: 10.1016/S1473-3099(16)00007-4. [DOI] [PubMed] [Google Scholar]
- 13.Dominguez JE, Redondo LM, Figueroa Espinosa RA, Cejas D, Gutkind GO, Chacana PA, Di Conza JA, Fernández Miyakawa ME. Simultaneous Carriage of mcr-1 and Other Antimicrobial Resistance Determinants in Escherichia coli From Poultry. Front Microbiol. 2018;9:1679. doi: 10.3389/fmicb.2018.01679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kurt D, Jennifer K, James S, Sanjay K. Bird migration and emerging zoonoses. Clin Med Res. 2002;1(1):5–12. [Google Scholar]
- 15.Dolejska M, Bierosova B, Kohoutova L, Literak I, Cizek A. Antibiotic-resistant Salmonella and Escherichia coli isolates with integrons and extended-spectrum beta-lactamases in surface water and sympatric black-headed gulls. J ApplMicrobiol. 2009;106:1941–1950. doi: 10.1111/j.1365-2672.2009.04155.x. [DOI] [PubMed] [Google Scholar]
- 16.Wellington EMH, Boxall ABA, Cross P, Feil EJ, Gaze WH, Hawkey PM, Johnson-Rollings AS, Jones DL, Lee NM, Otten W, Thomas CM, Williams AP. The role of the natural environment in the emergence of antibiotic resistance in gram-negative bacteria. Lancet Infect Dis. 2013;13(2):155–165. doi: 10.1016/S1473-3099(12)70317-1. [DOI] [PubMed] [Google Scholar]
- 17.Cole D, Drum DJ, Stalknecht DE, White DG, Lee MD, Ayers S, Sobsey M, Maurer JJ. Free-living Canada geese and antimicrobial resistance. Emerg Infect Dis. 2005;11:935–938. doi: 10.3201/eid1106.040717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kozak GK, Boerlin P, Janecko N, Reid-Smith RJ, Jardine C. Antimicrobial resistance in Escherichia coli isolates from swine and wild small mammals in the proximity of swine farms and in natural environments in Ontario. Appl Environ Microbiol. 2009;75:559–566. doi: 10.1128/AEM.01821-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.American Public Health Association (APHA) Standard methods for the examination of water and wastewater. 15. Washington: American Public Health Association; 1981. [Google Scholar]
- 20.Quinn PJ, Markey BK, Carter ME, Donnelly WJ, Leonard FG. Veterinary Microbiology and Microbial Diseases. 1. USA: Wiley-Blackwell Science; 2002. [Google Scholar]
- 21.Cavaco LM, Mordhorst H, Hendriksen R. PCR for plasmid-mediated Colistin resistance genes: mcr-1 and mcr-2 (Multiplex) Denmark: Protocol optimized at National Food Institute; 2016. [Google Scholar]
- 22.Liu Yi-Yun, Wang Yang, Walsh Timothy R, Yi Ling-Xian, Zhang Rong, Spencer James, Doi Yohei, Tian Guobao, Dong Baolei, Huang Xianhui, Yu Lin-Feng, Gu Danxia, Ren Hongwei, Chen Xiaojie, Lv Luchao, He Dandan, Zhou Hongwei, Liang Zisen, Liu Jian-Hua, Shen Jianzhong. Emergence of plasmid-mediated colistin resistance mechanism MCR-1 in animals and human beings in China: a microbiological and molecular biological study. The Lancet Infectious Diseases. 2016;16(2):161–168. doi: 10.1016/S1473-3099(15)00424-7. [DOI] [PubMed] [Google Scholar]
- 23.Xavier BB, Lammens C, Ruhal R, Kumar-Singh S, Butaye P, Goossens H, Malhotra-Kumar S. Identification of a novel plasmid-mediated colistin-resistance gene, mcr2, in Escherichia coli, Belgium, June 2016. EuroSurveill. 2016;21(27). 10.2807/1560-7917.ES.2016.21.27.30280. [DOI] [PubMed]
- 24.Alexander DJ. A review of avian influenza in different bird species. Vet Microbiol. 2003;74:3–13. doi: 10.1016/S0378-1135(00)00160-7. [DOI] [PubMed] [Google Scholar]
- 25.Capua I, Alexander DJ. Avian influenza and human health. ActaTropica. 2002;83:1–6. doi: 10.1016/s0001-706x(02)00050-5. [DOI] [PubMed] [Google Scholar]
- 26.Lee HY, Stephen A, Sushela D, Mala M. Detection of protozoan and bacterial pathogens of public health importance in faeces of Corvus spp. (large-billed crow) Trop Biomed. 2008;25:1349. [PubMed] [Google Scholar]
- 27.Fallacara DM, Monahan CM, Morishita TY, Wack RF. Fecal shedding and antimicrobial susceptibility of selected bacterial pathogens and a survey of intestinal parasites in free-living waterfowl. Avian Dis. 2001;45:128–135. doi: 10.2307/1593019. [DOI] [PubMed] [Google Scholar]
- 28.Dobbin G, Hariharan H, Daoust PY, Hariharan S, Heaney S, Coles M, et al. Bacterial flora of free-living double-crested cormorant (Phalacrocoraxauritus) chicks on Prince Edward Island, Canada, with reference to enteric bacteria and antibiotic resistance. Comp ImmunolMicrobiol Infect Dis. 2005;28:71–82. doi: 10.1016/S0147-9571(04)00059-1. [DOI] [PubMed] [Google Scholar]
- 29.Rose JM, Gast RJ, Bogomolni A, Ellis JC, Lentell BJ, Touhey K, et al. Occurrence and patterns of antibiotic resistance in vertebrates off the northeastern United States coast. FEMS Microbiol Ecol. 2009;67:421–431. doi: 10.1111/j.1574-6941.2009.00648.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Costa D, Poeta P, Saenz Y, Vinue L, Coelho AC, Matos M, et al. Mechanisms of antibiotic resistance in Escherichia coli isolates recovered from wild animals. Microb Drug Resist. 2008;14:71–77. doi: 10.1089/mdr.2008.0795. [DOI] [PubMed] [Google Scholar]
- 31.Poeta P, Radhouani H, Igrejas G, Goncalves A, Carvalho C, Rodrigues J, et al. Seagulls of the Berlengas natural reserve of Portugal as carriers of fecal Escherichia coli harboring CTXM and TEM extended-spectrum beta-lactamases. Appl Environ Microbiol. 2008;74:7439–7441. doi: 10.1128/AEM.00949-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Radimersky T, Frolkova P, Janoszowska D, Dolejska M, Svec P, Roubalova E, et al. Antibiotic resistance in faecal bacteria (Escherichia coli, Enterococcus spp.) in feral pigeons. J ApplMicrobiol. 2010;109:1687–1695. doi: 10.1111/j.1365-2672.2010.04797.x. [DOI] [PubMed] [Google Scholar]
- 33.Blanco G, Lemus JA, Grande J. Microbial pollution in wildlife: linking agricultural manuring and bacterial antibiotic resistance in red-billed choughs. Environ Res. 2009;109:405–412. doi: 10.1016/j.envres.2009.01.007. [DOI] [PubMed] [Google Scholar]
- 34.Arcilla MS, van Hattem JM, Matamoros S, Melles DC, Penders J, de Jong MD, et al. Dissemination of the mcr-1 colistin resistance gene. Lancet Infect Dis. 2016;16:147–149. doi: 10.1016/S1473-3099(15)00541-1. [DOI] [PubMed] [Google Scholar]
- 35.Fernandes MR, Moura Q, Sartori L, Silva KC, Cunha MP, Esposito F, et al. Silent dissemination of colistin-resistant Escherichia coli in South America could contribute to the global spread of the mcr-1 gene. Euro Surveill. 2016;21:1–6. doi: 10.2807/1560-7917.ES.2016.21.17.30214. [DOI] [PubMed] [Google Scholar]
- 36.Ruzauskas M, Lina V. Detection of the mcr-1 gene in Escherichia coli prevalent in the migratory bird species Larusargentatus. J AntimicrobChemother. 2016;71:2333–2334. doi: 10.1093/jac/dkw245. [DOI] [PubMed] [Google Scholar]
- 37.Mohsin M, Raza S, Roschanski N, Schaulfler K, Guenther S. First description of plasmid-mediated colistin-resistant extended-spectrum β-lactamase-producing Escherichia coli in a wild migratory bird from Asia. Int J Antimicrob Agents. 2016;48:463–464. doi: 10.1016/j.ijantimicag.2016.07.001. [DOI] [PubMed] [Google Scholar]
- 38.Skov RL, Monnet DL. Plasmid-mediated colistin resistance (mcr1 gene): three months later, the story unfolds. Euro Surveill. 2016;21(9):30155. [DOI] [PubMed]
- 39.Robinson TP, Bu DP, Carrique-Mas J, Fe’vre EM, Gilbert M, Grace D, Hay SI, Jiwakanon J, Kakkar M, Kariuki S, Laxminarayan R, Lubroth J, Magnusson U, Ngoc PT, Van Boeckel TP, Woolhouse ME. ESBLS AND CARBAPENEMASES IN WILD BIRDS 5 Downloaded by Washington Univ from www.liebertpub.com at 05/22/18. For personal use only. Antibiotic resistance is the quintessential One Health issue. Trans R Soc Trop Med Hyg. 2016;110:377–380. doi: 10.1093/trstmh/trw048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Radhouani H, Poeta P, Goncalves A, Pacheco R, Sargo R, Igrejas G. Wild birds as biological indicators of environmental pollution: antimicrobial resistance patterns of Escherichia coli and enterococci isolated from common buzzards (Buteobuteo) J Med Microbiol. 2012;61:837–843. doi: 10.1099/jmm.0.038364-0. [DOI] [PubMed] [Google Scholar]
- 41.Wu J, Huang Y, Rao D, Zhang Y, Yang K. Evidence for environmental dissemination of antibiotic resistance mediated by wild birds. Front Microbiol. 2018;9:745. doi: 10.3389/fmicb.2018.00745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chen K, Chan E, Xie M, Ye L, Dong N, Chen S. Widespread distribution of mcr-1 bearing bacteria in the ecosystem, 2015 to 2016. Euro Surveill. 2017;22:17–00206. doi: 10.2807/1560-7917.ES.2017.22.39.17-00206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sun L, Klein EY, Laxminarayan R. Seasonality and temporal correlation between community antibiotic use and resistance in the United States. Clin Infect Dis. 2012;55:687–694. doi: 10.1093/cid/cis509. [DOI] [PubMed] [Google Scholar]
- 44.Schwarz S, Johnson AP. Transferable resistance to colistin: a new but old threat. J Antimicrob Chemother. 2016;71:2066–2070. doi: 10.1093/jac/dkw274. [DOI] [PubMed] [Google Scholar]
- 45.Feng Youjun. Transferability of MCR-1/2 Polymyxin Resistance: Complex Dissemination and Genetic Mechanism. ACS Infectious Diseases. 2018;4(3):291–300. doi: 10.1021/acsinfecdis.7b00201. [DOI] [PubMed] [Google Scholar]
- 46.Zurfuh K, Poirel L, Nordmann P, Nuesch-Inderbinen M, Hachler H, Stephan R. Occurrence of the plasmid-borne mcr-1 colistin resistance gene in extended-spectrum-beta-lactamase-producing Enterobacteriaceae in river water and imported vegetable samples in Switzerland. Antimicrob Agents Chemother. 2016;60:2594–2595. doi: 10.1128/aac.00066-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Skurnik D. Effect of human vicinity on antimicrobial resistance and integrons in animal faecal Escherichia coli. Journal of Antimicrobial Chemotherapy. 2006;57(6):1215–1219. doi: 10.1093/jac/dkl122. [DOI] [PubMed] [Google Scholar]
- 48.Allen HK, Donato J, Wang HH, Cloud-Hansen KA, Davies J, Handelsman J. Call of the wild: antibiotic resistance genes in natural environments. Nat Rev Microbiol. 2010;8:251–259. doi: 10.1038/nrmicro2312. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analysed during this study are included in this published article.