Abstract
Acquired immune deficiency syndrome (AIDS) has become the leading cause of death among adolescents (aged 10–19) in sub-Saharan Africa. Less than 20% of African adolescents know their human immunodeficiency virus (HIV) status, whereas HIV testing remains the gateway to care. To end the AIDS epidemic by 2030 according to the Joint United Nations Programme on HIV/AIDS target, it is necessary to introduce scalable HIV testing strategies specific to different settings such as age groups, populations, and geographical areas. Demonstrated evidence on HIV self-testing (HIVST) in sub-Saharan Africa settings is reported, including data among adolescents. The All In initiative, which is the current international platform for the fight against HIV in adolescents is a good opportunity to address the challenge of HIV testing, including HIVST. Adapted strategies of HIVST such as (i) implementation of several listening and recreation centers for adolescents, (ii) door-to-door HIVST approach, and (iii) reducing the age of consent is urgently needed to promote HIV testing among adolescents living in Africa.
Keywords: Adolescent, human immunodeficiency virus self-testing, sub-Saharan African
INTRODUCTION
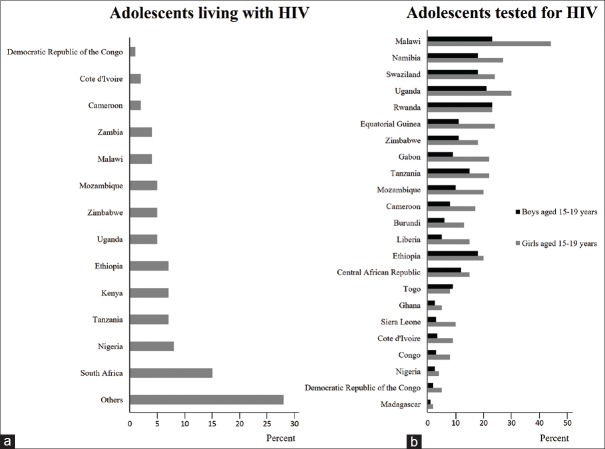
Globally, an estimated 2.1 million adolescents between 10 and 19 years were living with human immunodeficiency virus (HIV) in 2016, while an adolescent is infected with HIV every 2 min.1,2 Acquired immune deficiency syndrome (AIDS) has become the leading cause of death among adolescents (aged 10–19) in sub-Saharan Africa, mainly due to the lack of access to care.3 In sub-Saharan Africa, HIV testing being the gateway to care remains deficient among adolescents. Furthermore, <20% of African adolescents know their HIV status, while 90% of HIV-positive adolescents in the world live in sub-Saharan Africa [Figure 1a].1,2 Nearly, 80% of all new HIV infections among adolescent girls aged 15–19 in 2015 were living in Africa,2 as well as approximately 170 adolescents are infected with HIV each day in the Western and Central regions.4 To end the AIDS epidemic by 2030 according to the Joint United Nations Programme on HIV/AIDS (UNAIDS) target,1 it is necessary to introduce scalable strategies specific to different settings such as age groups, populations, and geographical areas. HIV self-testing (HIVST) recommended by the WHO since 2016 as an additional approach to existing HIV testing services is an innovative strategy to be implemented among adolescents to promote HIV testing.3,5
Figure 1.
(a) Adolescents living with human immunodeficiency virus in African countries in 2016; (b) Adolescents aged 15–19 who have been tested for human immunodeficiency virus in sub-Saharan Africa in 20141,3
Response against human immunodeficiency virus for adolescents
While the HIV-testing rate was very low and disproportionate among adolescents in 2014 [Figure 1b], UNICEF and UNAIDS launched the All In platform in February 2015 to galvanize global action toward HIV among adolescents.6 The All In initiative provides three targets for the year 2020 as follows: (i) reduce new HIV infections among adolescents by at least 75%; (ii) reduce AIDS-related deaths among adolescents by at least 65%; and (iii) end stigma and discrimination.6 The low levels of testing among adolescent populations at higher risk of exposure to HIV underscore the urgent need to focus on quality of, and investment in, adolescent HIV programs.
Barriers to human immunodeficiency virus testing among adolescents
Pitfalls of HIV testing in health-care facilities include fears over loss of privacy and confidentiality.7 Furthermore, HIV stigma and discrimination are a well-known barrier to access HIV testing and treatment for all people, of all ages, but the dynamics for adolescents who live in a context of dependency are not fully understood.8,9 The age of consent is also a barrier to HIV testing. In sub-Saharan Africa, the age of consent to access HIV testing without parental consent varies across countries but is mostly between 16 and 18 years [Figure 2].6 The age of consent should be de facto decreased to allow adolescents the autonomy to be tested. Thus, the first “C” of the WHO “5Cs” (Consent, Confidentiality, Counseling, Correct Test Results, and Connection) of HIV testing services will be respected. In this perspective, Kenya and Lesotho lowered the age of consent for HIV testing from 18 to 15 and 15 to 12, respectively.6 Nevertheless, HIV testing in adolescents, especially if they are not accompanied by an adult referent, which should be done with caution and associated with pre-test and post-test counseling adapted to the specificities of adolescence.10 In contrast, several studies show that peer support or family-based support can eliminate psychological and social barriers, create a supportive environment and sensitize adolescents to HIV testing.11,12
Figure 2.
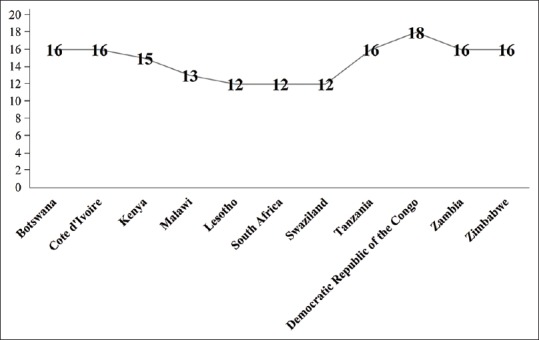
The age of consent to access human immunodeficiency virus testing without parental consent in sub-Saharan Africa 2016 in sub-Saharan African countries6
Furthermore, some populations of adolescents, including adolescents involved in sex commerce, adolescents who inject drugs, transgender adolescents, and gay and bisexual adolescent males are considered as much more vulnerable, pointing to the necessity of specific intervention for HIV prevention and HIVST in these neglected groups.13
Evidence of human immunodeficiency virus self-testing among adolescents
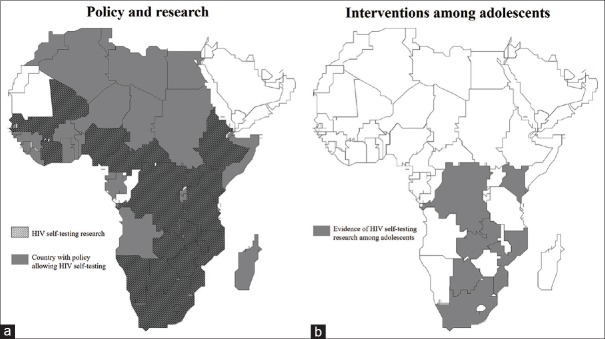
Currently, many African countries have policies supporting HIVST. Demonstrated evidence on HIVST in sub-Saharan Africa settings is reported in the literature [Figure 3a12,14,15 including HIVST data in adolescents [Figure 3b].12,14,15 The WHO has outlined various sector channels through which self-test kits could be distributed, including community-based, facility-based, and over-the-counter and Internet-based approaches.5 Furthermore, directly assisted and unassisted HIVST are two delivery approaches varying in level and type of provided support.5 In Malawi, the highest rate of uptake of directly assisted community-based HIVST was among adolescents.16
Figure 3.
(a) African countries supporting policy, research program; (b) Specific interventions among adolescents on human immunodeficiency virus self-testing in 201912,13,14
Impact of gender norms on human immunodeficiency virus self-testing among adolescents
A recent rigorous evidence of a 3-month intervention of door-to-door distribution of HIVST in Zambia demonstrated increased knowledge of HIV status among young adults aged 16–29 years.17 This effect was driven among men, but unpredictably not among women, suggesting differential effectiveness of the intervention by gender.17 On the other hand, HIV incidence in sub-Saharan Africa is high among adolescent girls and female young people aged 15–24. This group incidentally is at the highest risk of HIV because they are very often victims of gender-based violence, poverty-related prostitution, procuring, cultural norms sustaining gender disparities in access to education and healthcare, especially in relation with reproductive health.1,4 Furthermore, slight differences in acceptability and feasibility of HIVST observed in Democratic Republic of the Congo between adolescent boys versus girls may affect the uptake of HIVST.12 Very often, the consideration of gender issues is limited to focusing on women as the main target of the programs (prevention of mother-to-child transmission, and income-generating activities) without taking into account, the impact of these intervention modalities on gender relations. Conversely, men are still as far removed from testing and care centers, and constitute <20% of the active lines of HIV associations in sub-Saharan Africa.1,3 The difference of genre concerning HIVST in adolescents should be evaluated in each setting to highlight specific intervention in Africa.
Challenges and solutions
Although the need seems to be clear to increase the rate of HIV testing among African adolescents, interventions are disproportionate between East and Southern Africa versus West and Central Africa.4 Context-dependent operational studies on the acceptability, feasibility, preference, and uptake of HIVST among adolescents are needed in sub-Saharan Africa, especially in the West and Central Africa. Research institutions, nongovernmental organizations for development, governments, donors, and all stakeholders must become involved in operationalizing HIVST among adolescents living in Africa. Thus, targeted interventions can be proposed in sub-Saharan Africa to promote access to HIVST as follows: (i) implementation of several listening and listening centers for adolescents which are important to allow supervised distribution of self-test kits and to eliminate psychological and social barriers;8(ii) door-to-door HIVST approach which constitutes an innovative way to distribute the self-test kit among adolescent; (iii) m-Health including social media platforms in local languages to raise awareness and to present the video-based instructions for use of the HIVST; (iv) advocacy with ministries of health for the implementation of policies facilitating HIVST among adolescents, in particular by changing the age of consent for HIV testing, and hence that young people aged 12 and over could receive an independent HIV testing in good conditions; and (v) facilitating the delegation of tasks allowing community health workers to facilitate access to HIVST by adolescents in a community-based approach.
In Nigeria, there is a policy allowing HIVST, and three products for HIVST have received national regulatory approval in 2019.18 Nigeria views the HIVST as a possible mechanism help to increase HIV testing uptake and capture otherwise undiagnosed HIV cases.19 In a recent survey, the majority (54.8%) of interviewed researchers, academics, journalists, community advocates, activists, and HIV policy-makers and programmers supported the introduction of HIVST.20 However, a significant number of respondents was concerned about the possible risk associated with self-testing, especially suicide and partner violence, as well as about poor linkages to care.20 Furthermore, many adolescent girls in Nigeria do not test for HIV despite being at high risk, and HIVST could constitute a problematic challenge.21 Whatever, introduction of HIVST in Nigeria would need to be paired with intense media campaigns and education about its use.
CONCLUSION
Current HIV testing strategies for adolescents are the most often inappropriate in sub-Saharan Africa. The All In initiative is a good opportunity to address the challenge of HIV testing including HIVST and adapt strategies for the AIDS response among adolescents. The adapted strategy of HIVST is urgently needed to promote HIV testing among adolescents living in Africa in ending AIDS by 2030.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.UNAIDS. Ending the AIDS Epidemic for Adolescents, with Adolescents. [Last accessed on 2019 Mar 23]. Available from: http://www.unaids.org/sites/default/files/media_asset/ending-AIDS-epidemic-adolescents_en.pdf .
- 2.UNICEF. Every Three Minutes Teenage Girl Infected HIV Unicef. UNICEF. 2018. [Last accessed on 2019 Mar 23]. Available from: https://www.unicef.org/fr/press-releases/every-three-minutes-teenage-girl-infected-hiv-unicef .
- 3.UNAIDS. Global AIDS Monitoring 2019, Indicators for Monitoring the 2016 Political Declaration on Ending AIDS. UNAIDS. 2018. [Last accessed on 2019 Mar 23]. Available from: http://www.unaids.org/sites/default/files/media_asset/global-aids-monitoring_en.pdf .
- 4.UNAIDS & UNICEF. Step Up the Pace: Towards an AIDS-Free Generation in West and Central Africa. UNAIDS and UNICEF. 2017. Dec, [Last accessed 2019 Mar 23]. Available from: https://www.unicef.org/publications/files/Step_Up_the_Pace_West_and_Central_Africa.pdf .
- 5.World Health Organization. HIV and Adolescents: guidance for HIV Testing and Counselling and Care for Adolescents Living with HIV: recommendations for a Public Health Approach and Considerations for Policymakers and Managers. Geneva: World Health Organization; [Lst accessed on 2019 Mar 25]. Available from: http://www.who.int/iris/handle/10665/94334 . [Google Scholar]
- 6.UNAIDS. Progress Report: All in to End the Adolescent AIDS Epidemic. UNAIDS. 2016. [Last accessed on 2019 Apr 10]. Available from: http://www.unaids.org/sites/default/files/media_asset/ALLIN2016ProgressReport_en.pdf .
- 7.Kalichman SC, Simbayi LC. HIV testing attitudes, AIDS stigma, and voluntary HIV counselling and testing in a black township in Cape town, South Africa. Sex Transm Infect. 2003;79:442–7. doi: 10.1136/sti.79.6.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.MacQueen KM. Young people, HIV, and life goals. J Int AIDS Soc. 2017;20:22267. doi: 10.7448/IAS.20.1.22267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fielden SJ, Chapman GE, Cadell S. Managing stigma in adolescent HIV: Silence, secrets and sanctioned spaces. Cult Health Sex. 2011;13:267–81. doi: 10.1080/13691058.2010.525665. [DOI] [PubMed] [Google Scholar]
- 10.Msellati P, Ateba Ndongo F, Hejoaka F, Nacro B. Impediments to HIV testing in HIV-infected children and teenagers in Africa: Look for them where they are! Med Sante Trop. 2016;26:10–4. doi: 10.1684/mst.2015.0519. [DOI] [PubMed] [Google Scholar]
- 11.Zvandiri A. Engaging Adolescents in HIV Treatment and Care: Approaches for Improved Service Delivery. Session at 18th International Conference on AIDS and STIs in Africa; Novembr 29 – December 4, 2015; Harare, Zimbabwe. [Google Scholar]
- 12.Tonen-Wolyec S, Batina-Agasa S, Muwonga J, Mboumba Bouassa RS, Kayembe Tshilumba C, Bélec L. Acceptability, feasibility, and individual preferences of blood-based HIV self-testing in a population-based sample of adolescents in Kisangani, democratic republic of the Congo. PLoS One. 2019;14:e0218795. doi: 10.1371/journal.pone.0218795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.AVERT. Young People, HIV and AIDS. [Last accessed on 2019 Jul 24]. Available from: https://www.avert.org/professionals/hiv-social-issues/key-affected-populations/young-people .
- 14.Hector J, Davies MA, Dekker-Boersema J, Aly MM, Abdalad CC, Langa EB, et al. Acceptability and performance of a directly assisted oral HIV self-testing intervention in adolescents in rural Mozambique. PLoS One. 2018;13:e0195391. doi: 10.1371/journal.pone.0195391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Smith P, Wallace M, Bekker LG. Adolescents' experience of a rapid HIV self-testing device in youth-friendly clinic settings in Cape town South Africa: A cross-sectional community based usability study. J Int AIDS Soc. 2016;19:21111. doi: 10.7448/IAS.19.1.21111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Choko AT, MacPherson P, Webb EL, Willey BA, Feasy H, Sambakunsi R, et al. Uptake, accuracy, safety, and linkage into care over two years of promoting annual self-testing for HIV in Blantyre, Malawi: A community-based prospective study. PLoS Med. 2015;12:e1001873. doi: 10.1371/journal.pmed.1001873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mulubwa C, Hensen B, Phiri MM, Shanaube K, Schaap AJ, Floyd S, et al. Community based distribution of oral HIV self-testing kits in Zambia: A cluster-randomised trial nested in four HPTN 071 (PopART) intervention communities. Lancet HIV. 2019;6:e81–e92. doi: 10.1016/S2352-3018(18)30258-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.HIVST. Policy & Regulations for HIVST. [Last accessed on 2019 Jul 24]. Available from: http://www.hivst.org/policy-regulations-for-hivst-1 .
- 19.Brown B, Folayan MO, Imosili A, Durueke F, Amuamuziam A. HIV self-testing in Nigeria: Public opinions and perspectives. Glob Public Health. 2015;10:354–65. doi: 10.1080/17441692.2014.947303. [DOI] [PubMed] [Google Scholar]
- 20.Tun W, Vu L, Dirisu O, Sekoni A, Shoyemi E, Njab J, et al. Uptake of HIV self-testing and linkage to treatment among men who have sex with men (MSM) in Nigeria: A pilot programme using key opinion leaders to reach MSM. J Int AIDS Soc. 2018;21(Suppl 5):e25124. doi: 10.1002/jia2.25124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Iwelunmor J, Blackstone S, Jennings L, Converse D, Ehiri J, Curley J. Determinants of HIV testing and receipt of test results among adolescent girls in Nigeria: The role of assets and decision-making. Int J Adolesc Med Health. 2018 doi: 10.1515/ijamh-2017-0152. pii:/j/ijamhahead-of-print/ijamh-2017-0152/ijamh-2017-0152.xml. [DOI] [PubMed] [Google Scholar]