Abstract
Background Volar locking plates with a central notch were designed to reduce the risk of flexor pollicis longus (FPL) tendon irritation after volar plating for distal radius fractures.
Objective The purpose of this study was to evaluate the course of the FPL tendon after FPL-plate osteosynthesis to identify a plate position that avoids an impingement with the FPL tendon.
Patients and Methods Nineteen patients treated with volar plating using an FPL plate for a distal radius fracture were evaluated. Transverse ultrasound images were used to assess whether the profile of the FPL tendon lied within the plate notch. The position of the FPL tendon on transverse ultrasound images was transferred onto postoperative dorsovolar X-ray images to define an FPL tendon corridor for a plate position not interfering with the FPL tendon.
Results The FPL tendon was aligned inside the plate notch completely in three cases, partially in 11 cases, and missed the notch in five cases. An FPL corridor was defined at the level of the watershed line with all FPL tendons being completely (74%) or partially (26%) aligned inside that corridor. There was a moderate correlation between the plate notch being positioned inside this corridor and the FPL tendon being positioned inside the plate notch ( r = 0.49; p = 0.033).
Conclusion It seems advantageous to place the plate notch within a corridor parallel to the radial shaft between the ulnar edge of the scaphoid tubercle and the scapholunate interval for the FPL tendon protection.
Level of Evidence This is Level IV study.
Keywords: flexor pollicis longus, distal radius fracture, tendon rupture, Soong classification, ultrasound
Displaced distal radius fractures can be treated successfully by volar locking plates. Fracture lines distal to the watershed line as in shear type fractures require a distal plate position to buttress the articular fragments sufficiently. Distally placed, the plate can irritate the flexor tendons which course close to the volar radial rim. Especially, irritation or lesions of the flexor pollicis longus (FPL) and deep flexor tendon of the index finger are reported in 0.3 to 12% because of a direct tendon–plate contact. 1 2 3 4 Tendon rupture can occur as early as 3 months 1 or even after 10 years postoperatively 5 without previous complaints. 6
Known reasons for these tendon complications are a “lift-off” of the plate, protruding screws, poor fracture reduction, a loss of reduction, a distal plate position, the plate design, or a wrong application of the plate. 1 2 7 8 9
The position of the plate in accordance to the watershed line can be classified according to Soong et al in the sagittal view. 2 10 If the distal rim of the plate is in line with the watershed line (Soong 1) or exceeds the line volarly (Soong 2), the FPL tendon can rub on the distal rim of the plate and, therefore, irritate or tear. 2 10
Therefore, it should be tried to position the plate below the watershed line (Soong 0) to reduce any risk for tendon irritation. However, a distal plate position is necessary in distal fracture lines to stabilize the fragments. Therefore, industry developed a volar locking plate with a central notch to minimize the risk of plate interference with the FPL tendon ( Fig. 1 ).
Fig. 1.
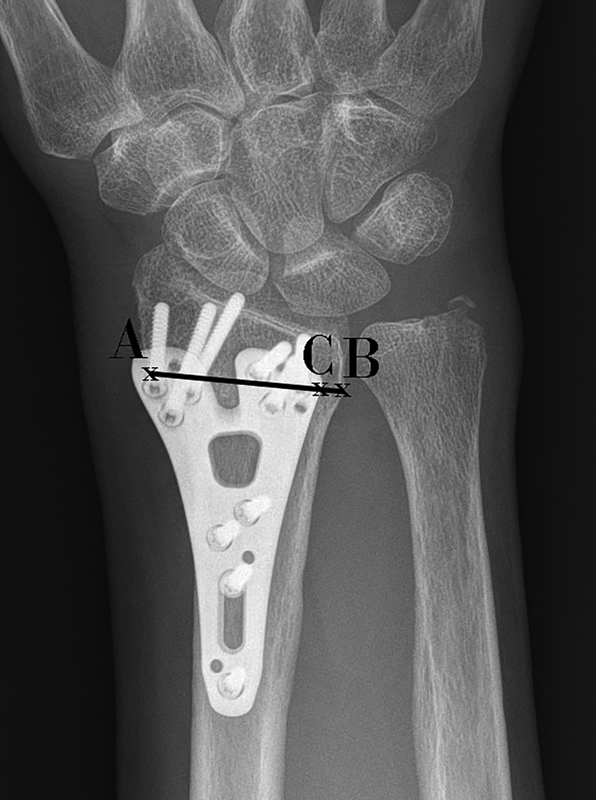
Radial width measured at the level of the largest plate width (A–B). The distance between the ulnar edge of the plate to the sigmoid notch (C–B). The plate notch is not aligned adequately according to the FPL tendon corridor. FPL, flexor pollicis longus.
It is recommended to position the plate along the ulnar corner of the radius to address the unstable ulnar facet fragment. However, it remains unclear if the FPL tendon would run within the plate notch. Furthermore, the adequate position of the plate notch not interfering with the course of the FPL tendon is not known sufficiently.
Therefore, the aim of this study was to evaluate the course of the FPL tendon after FPL-plate osteosynthesis to identify a plate position that avoids an impingement with the FPL tendon.
Patients and Methods
Nineteen patients (14 females, 5 males) with a mean age of 57 years (27–74 years) treated with volar plating using an angle-stable FPL plate (Medartis, Basel, Switzerland) for a distal radius fracture (nondominant wrist 63.2%) between March 2015 and September 2016 were evaluated retrospectively. Surgery was performed within 9.6 days (standard deviation [SD] = 6.3 days) after trauma. An ultrasound investigation was conducted because of unspecified wrist complaints between 1 and 17 months after plate osteosynthesis to detect possible flexor tendon irritations.
Inclusion criteria were a minimum age of 18 years, available postoperative X-ray images, ultrasound images, and surgical treatment with this specified implant. Institutional review board approval was granted by means of a general waiver for studies with retrospective data analysis (local research ethics committee, BLINDED, February 20 2009).
The used FPL plate has a central notch with a width of approximately 4 mm on its bottom side. The width is approximately 7 mm on its upper side because of the embankment angle with a smooth and oblique transition. Plate thickness is 2 mm. The ulnar plate end reaches more distal than the radial one.
Three hand surgeons performed plating using a volar approach. Fracture reduction and angular correction were controlled by fluoroscopy. The plate position was intended to address the main fragments with at least two locking screws placed subchondrally to the articular surface. The surgeons decided on the amount of achievable alignment. Usually, an adequate alignment was considered if there was > 15-degree radial inclination, 0-degree sagittal tilt, and 0-mm ulnar variance. The pronator quadratus muscle was refixed whenever possible. The part of the plate protruding distal to the watershed line remained uncovered.
The distance between the fracture line and the radiocarpal joint was measured on sagittal preoperative computed tomography (CT) scans at the lunate facet. The radial inclination, the dorsal tilt, and the ulnar variance were measured on postoperative dorsovolar and lateral X-ray images to assess fracture reduction. A standard dorsovolar wrist projection was conducted with the arm position in 90-degree shoulder abduction, 90-degree elbow flexion, neutral forearm rotation, and the middle finger in line with the long axis of the forearm. A true dorsovolar wrist X-ray was defined showing no or minimal superimposition of the distal radioulnar joint.
Plate Position in Relation to the Radius
The sagittal plate position was evaluated according to Soong et al 2 to assess a volar plate protrusion at the distal radial rim. However, the Soong classification does not exactly reflect the plate design because the ulnar plate part extends more distal than the radial one in the lateral projection. Radial width was measured on the postoperative dorsovolar X-ray images at the level of the largest plate width. The distance between the ulnar edge of the plate and sigmoid notch was measured at the same level. These measurements were undertaken for analysis of the placement of the plate in relation to the radius to assess a potential variability in positioning possibilities ( Fig. 1 ).
Radioulnar FPL Tendon Position in Relation to the Radius and the Plate Notch
An Epiq 7G ultrasound (Philipps, Amsterdam, the Netherlands) with an L18–5 ultrasound head or an iU22 ultrasound (Philipps) with an L17–5 ultrasound head were used for evaluation.
Transverse ultrasound images were used to evaluate whether the profile of the FPL tendon lied within the plate notch or missed it. Any overlap of the FPL tendon with the plate was assessed as a percentage in relation to the FPL tendon diameter. The thickness of the FPL tendon was measured at the height of the distal plate position and correlated to the radial width.
The position of the FPL tendon in relation to plate landmarks on the transverse ultrasound image was transferred and estimated onto postoperative dorsovolar X-ray images. The width of the FPL tendon and its position in relation to the plate sparing on ultrasound images was drawn onto postoperative dorsovolar X-ray images showing the same width of the tendon and position in relation to the plate sparing on the X-ray images ( Fig. 2 ). The radial or ulnar plate sparing border in relation to the width of the FPL tendon was used for an adequate orientation on ultrasound images and transfer of the FPL tendon position on X-ray images.
Fig. 2.

(A–D) A 70-year-old patient sustained a distal radius refracture after a fall and was treated surgically with an FPL-plate fixation after previous surgical treatment of an impaction syndrome a decade ago. ( A and B ) The plate notch was positioned according to the FPL tendon corridor (red lines). The lateral X-ray images shows Soong grade 2 plate position. (C) The transverse ultrasound image showed that the FPL tendon was within the FPL tendon–plate notch with its whole diameter. (D) Consequently, the longitudinal ultrasound image does not show any FPL tendon–plate contact or gliding restrain. The transmission of the position of the FPL tendon in relation to plate landmarks of the transverse ultrasound image onto the postoperative dorsovolar X-ray image is shown in turquoise color in A and C. FPL, flexor pollicis longus.
By this method, an FPL tendon corridor could be defined using anatomical landmarks on dorsovolar X-ray images. The position of the plate notch was evaluated in relation to this corridor. This position was grouped as follows: (1) a complete alignment, (2) a partial alignment, and (3) no alignment of the plate notch within the FPL tendon corridor. The frequency of the position of the FPL tendon within the plate notch was evaluated depending on the position of the plate notch within the corridor ( Table 1 ).
Table 1. Frequency and relationship of the plate notch within the FPL tendon corridor and the FPL tendon position within the plate notch.
| Plate notch aligned within the corridor | Plate notch partially aligned within the corridor | Plate notch missing the corridor | Total | |
|---|---|---|---|---|
| The FPL tendon inside the plate notch | 3 | 0 | 0 | 3 |
| The FPL tendon partially inside the plate notch | 6 | 4 | 1 | 11 |
| The FPL tendon missing the plate notch | 1 | 3 | 1 | 5 |
| Total | 10 | 7 | 2 | 19 |
Abbreviation: FPL, flexor pollicis longus.
FPL Tendon in Relation to a Plate Contact
A tendon–plate contact with a gliding restraint can be clearly visualized with a longitudinal ultrasound view. 6 11 Longitudinal ultrasound images were used to measure any tendon–plate contact. A tendon gliding restraint was evaluated with passive flexion of the interphalangeal joint of the thumb. A deformation of the tendon was interpreted as a gliding restraint.
The position of the FPL tendon within the plate notch, as well as any tendon–plate contact, was related to the Soong classification.
CT, X-ray, and ultrasound images were evaluated with the Impax EE software (Agfa Healthcare, Bonn, Germany).
Statistical Evaluation
Statistical evaluation was performed using SPSS Version 23 (IBM, Armonk, NY). Clinical and radiological parameters are given as absolute frequencies and percentages or means and SDs appropriate to data distribution. Due to skewed data distribution, statistical analysis was performed using nonparametric methods. The association between the position of the FPL tendon within the plate notch and the radial width and the distance of the plate to the sigmoid notch was assessed using the Mann–Whitney U -test. Correlation hypothesis were analyzed using Spearman's rank correlations. Statistical significance was set at p < 0.05.
Results
Adequate realignment of the distal radius could be achieved ( Table 2 ).
Table 2. Postoperative fracture alignment.
| Alignment parameter | Value |
|---|---|
| Distance between the fracture line and the radiocarpal joint | 8.2 mm (SD = 2.5 mm) |
| Volar tilt (degree) | 3.3 (SD = 3.4) |
| Radial inclination | 20.0 (SD = 3.7) |
| Ulnar variance | −0.2 mm (SD = 1.3 mm) |
Abbreviation: SD, standard deviation.
Plate Position in Relation to the Radius
A Soong 0 plate position was seen in five cases, Soong 1 in nine cases and Soong 2 in five cases ( Table 3 ). Mean radial width was 30.2 mm (SD = 3.6 mm; range: 25.4–37.7 mm) at the height of the largest plate width representing 121% (SD = 14%; range: 102–150%) of the plate width (25 mm). The distance between the ulnar plate edge and the sigmoid notch was 3.0 mm (SD = 3.0 mm; range: 0.0–13.2 mm). There was no association between the position of the FPL tendon within the plate notch and the radial width ( p = 0.391) or the distance of the plate to the sigmoid notch ( p = 0.622).
Table 3. Frequency of the position of the FPL tendon in regard to the plate notch and a gliding restraint depending on the Soong classification ( n = 19) .
| FPL tendon within plate notch | Soong 0 n (%) |
Soong 1 n (%) |
Soong 2 n (%) |
|---|---|---|---|
| Yes | 4 (80.0) | 6 (66.7) | 4 (80.0) |
| No | 1 (20.0) | 3 (33.3) | 1 (20.0) |
| Total | 5 | 9 | 5 |
| FPL tendon–plate contact/gliding restraint |
Soong 0
n (%) |
Soong 1
n (%) |
Soong 2
n (%) |
| Yes | 0 (0.0) | 3 (33.3) | 2 (40.0) |
| No | 5 (100.0) | 6 (66.7) | 3 (60.0) |
| Total | 5 | 9 | 5 |
Abbreviation: FPL, flexor pollicis longus .
Radioulnar FPL Tendon Position in Relation to the Radius and the Plate Notch
The frequency of the position of the FPL tendon in regard to the plate notch is shown in Fig. 3 .
Fig. 3.

FPL tendon position in regard to the plate notch. Position A (whole tendon within the plate notch): three cases (16%); position B (partial tendon–plate overlap radially): one case (5%); position C (partial tendon–plate overlap ulnarly): 10 cases (53%); position D (whole tendon–plate overlap ulnarly): five cases (26%). FPL, flexor pollicis longus.
The FPL tendon thickness was 4.9 mm (SD = 0.7 mm; range: 3.8–6.4 mm). There was a moderate correlation between the FPL tendon thickness and the radial width ( r = 0.50; p = 0.030).
Matching the evaluated FPL tendon position using ultrasound onto postoperative X-ray images, revealed that the FPL tendon at the level of the watershed line lies within a corridor formed by two longitudinal lines parallel to the radius, one starting at the ulnar border of the scaphoid tubercle and the second one at the scapholunate interval in a neutral wrist position ( Fig. 4 ).
Fig. 4.

The FPL tendon corridor (two longitudinal lines parallel to the radius: one starting at the ulnar side of the scaphoid tubercle and the other one at the scapholunate interval in a neutral wrist position). FPL, flexor pollicis longus.
Fourteen cases (73.7%) showed a complete FPL tendon position within this corridor while five cases (26.3%) showed a partial one. The tendons showing a partial position within this corridor exceeded its borders by a maximum of 2 mm radially and 3 mm ulnarly.
The plate notch was positioned within this corridor with its whole width in 10/19 cases (52.6%), partially in 7/19 cases (36.8%), and missed the corridor in 2/19 cases (10.5%; Table 1 ).
Four of five (80%) cases in which the FPL tendon missed the plate notch showed that the whole plate notch was not adequately aligned within this corridor. All three cases with the whole FPL tendon, positioned inside the notch, showed full alignment of the plate notch within this corridor ( Table 1 ). There was a moderate correlation between the plate notch being positioned inside the corridor and the FPL tendon being positioned inside the plate notch ( r = 0.49; p = 0.033).
FPL Tendon in Relation to a Plate Contact
Longitudinal ultrasound images showed a direct FPL tendon–plate contact in five cases (26.3%). Table 3 shows the frequency of the position of the FPL tendon inside the plate notch and any tendon–plate contact in relation to the Soong classification. All patients with an FPL tendon–plate contact showed a concomitant gliding restraint.
Fig. 2 shows an exemplary case of an optimal alignment for FPL protection in a Soong 2 plate position.
Discussion
The FPL tendon runs inside the carpal tunnel and turns around the scaphoid tubercle toward the thumb. To estimate the course of the FPL tendon during surgery under intensifier control, this study analyzed the potential course of the FPL tendon out of postoperative X-ray and ultrasound data. A specific postoperative FPL tendon corridor could be defined ( Fig. 4 ) for a neutral wrist position.
This study could demonstrate that the FPL plate can be positioned distally near the watershed line respecting the course of the FPL tendon as 14 out of 19 FPL tendons were lying completely or partially within the plate notch ( Fig. 3 ). Three cases showed an FPL tendon position with its full tendon diameter coursing within the plate notch. However, most FPL tendons (11/19 cases) showed a partial tendon–plate overlap.
One reason for a partial tendon–plate overlap is the fact that the notch width is similar to the diameter of the FPL tendon. The mean FPL tendon diameter in this cohort was 4.9 mm, similar to Oura et al (4.2 mm). 12
A second reason for a partial overlap might obviously be a suboptimal plate position in regard to the FPL tendon position, which could be seen in nine cases ( Table 2 ). Because the FPL tendon runs inside the described corridor, it seems necessary to align the whole plate notch along this corridor for tendon protection.
Plate positioning inside this corridor might not always be possible or desired because addressing the ulnar fragment remains the primary goal. Moreover, only wider radii showed a potential variability of the radioulnar plate position due to the fact that the radial width (30.2 mm; SD = 3.6 mm) was mostly not too much larger than the plate width. Therefore, the distance between the ulnar plate edge and the sigmoid notch could only be altered in wider radii. This implies that there will be a higher variability for plate positioning for thinner tendons and wider radii than for thicker tendons and narrower radii.
A third reason for a partial overlap is the fact that evaluations were only performed in neutral wrist positions. However, the ulnoradial FPL position can change up to 3 mm, depending on the wrist and finger position showing a maximal ulnodorsal shift from a radiovolar position in wrist extension with finger flexion. 13 14 Additionally, the plate notch seemed to limit the ulnar shift if the FPL tendon showed a tendon–plate contact. 14 In summary, the wrist position might change the amount of partial tendon–plate overlap.
A distally positioned plate can be regarded as a main risk factor for a tendon–plate contact. 6 11 15 However, less cases of FPL tendon–plate contacts were seen in a distal plate position than expected ( Table 3 ). Former findings showed that tendon lesions only occurred in Soong 1 and 2, 2 10 and that plate removal was mainly necessary in these cases. 16 These findings might imply that the FPL tendon is not at risk in cases of Soong 0 but might be for Soong 1 and 2 plate positions. Because three Soong 2 cases showed the FPL tendon inside the plate notch, it might be hypothesized that plate designs with a notch can reduce or prevent tendon–plate contact ( Fig. 2 ).
Longitudinal ultrasound images showed a direct FPL tendon–plate contact with a concomitant gliding restraint in a quarter of the patients. A plate contact with a concomitant gliding restraint is possible on either, the radial and ulnar side. Yet, due to the plate design and the FPL tendon course, a tendon position over the radial part is rare and usually not to be expected. The ulnar part of this plate reaches more distally than the radial one, which needs to be taken into account when assessing the plate position and any potential tendon–plate conflict on X-ray images. Because of this plate-length discrepancy, the Soong classification is less suitable for depicting potential tendon–plate conflicts.
All patients with a tendon–plate contact showed a concomitant gliding restraint. For the authors, a gliding restraint reflects the situation of a pressure load deforming capacity of the tendon. The use of the FPL plate might give the option to unload this pressure by shifting the tendon into the plate notch. The notch width of 4 mm is bordered by a smooth embankment angle, which increases the area of reduced friction to 7 mm minimizing an FPL tendon–plate conflict beyond the radiologically visible gap. Therefore, the plate notch design might reduce friction even if the FPL tendon is positioned only partially inside the notch. Nevertheless, the FPL tendon showed an alteration of a natural tendon gliding and, therefore, demonstrated a potential risk for irritation.
Although a recent study showed a different FPL position in a neutral and functional wrist position, 14 there is one major point, which needs to be taken into account. Finger flexion leads to a transverse shift of the FPL tendon. In some cases, the tendon glided from radial to ulnar into the plate sparing and further ulnar movement was restricted by the ulnar edge of the sparing. In other cases, the tendon glided from ulnar over the ulnar edge into the sparing causing a potential transverse friction which might lead to tendon irritations and rupture. 14 However, a longitudinal friction between the FPL tendon and the plate also exists during thumb flexion/extension movements that may contribute to tendon irritation and rupture. To reduce this risk, an optimal plate sparing position underneath the FPL tendon might help to reduce load peaks, if the fracture and the radius size allow variable plate positions. The presented study is a help for surgeons to intraoperatively position the plate sparing to potentially reduce the risk of friction of the FPL tendon.
Limitations
The limitations of this study are the small sample size and the retrospective character. The evaluation of the FPL tendon corridor was only indirect by comparison of two imaging modalities. Therefore, the FPL tendon course could just be estimated. Anatomical variations, wrist and finger positions 13 14 17 as well as X-ray rotation can also alter results and contribute to cases with a partial position of the tendon within the described corridor. Surgical fracture reduction and fixation might also change the position of the FPL tendon, potentially leading to a more ulnar position postoperatively than in healthy wrists. 13 15 17 Finally, the clinical relevance of the tendon deformation and gliding restraint remains unclear and further research is necessary. This study did not evaluate specific wrist complains in regard to different FPL tendon positions.
Conclusion
In conclusion, it seems advantageous to place the FPL tendon–plate notch within a corridor parallel to the radial shaft between the ulnar edge of the scaphoid tubercle and the scapholunate interval. The plate notch can hereby be placed underneath the course of the FPL tendon if the fracture and width of the distal radius allow for selective plate placement. Plate designs sparing the FPL tendon seem to be especially useful in cases of a distal plate position (Soong 1 and 2) to protect the FPL tendon from any tendon–plate interference.
Conflict of Interest M.G. declares that he is a member of the advisory board of Medartis. The other authors declare no potential conflict of interests with respect to the research, authorship, and/or publication of this article. M.G. has nothing to disclose.
Note
Institutional review board approval was granted by means of a general waiver for studies with retrospective data analysis (local research ethics committee, Medical University Innsbruck, February 20, 2009).
References
- 1.Drobetz H, Kutscha-Lissberg E. Osteosynthesis of distal radial fractures with a volar locking screw plate system. Int Orthop. 2003;27(01):1–6. doi: 10.1007/s00264-002-0393-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Soong M, Earp B E, Bishop G, Leung A, Blazar P. Volar locking plate implant prominence and flexor tendon rupture. J Bone Joint Surg Am. 2011;93(04):328–335. doi: 10.2106/JBJS.J.00193. [DOI] [PubMed] [Google Scholar]
- 3.Casaletto J A, Machin D, Leung R, Brown D J. Flexor pollicis longus tendon ruptures after palmar plate fixation of fractures of the distal radius. J Hand Surg Eur Vol. 2009;34(04):471–474. doi: 10.1177/1753193408100964. [DOI] [PubMed] [Google Scholar]
- 4.Figl M, Weninger P, Jurkowitsch J, Hofbauer M, Schauer J, Leixnering M. Unstable distal radius fractures in the elderly patient--volar fixed-angle plate osteosynthesis prevents secondary loss of reduction. J Trauma. 2010;68(04):992–998. doi: 10.1097/TA.0b013e3181b99f71. [DOI] [PubMed] [Google Scholar]
- 5.Monda M K, Ellis A, Karmani S. Late rupture of flexor pollicis longus tendon 10 years after volar buttress plate fixation of a distal radius fracture: a case report. Acta Orthop Belg. 2010;76(04):549–551. [PubMed] [Google Scholar]
- 6.Kadoma C, Takahara M, Maruyama M, Satake H, Takagi M. Ultrasonographic assessment of the flexor pollicis longus tendon after plate fixation. Orthopedics. 2017;40(01):e104–e108. doi: 10.3928/01477447-20161017-01. [DOI] [PubMed] [Google Scholar]
- 7.Selvan D R, Machin D G, Perry D, Simpson C, Thorpe P, Brown D J. The role of fracture reduction and plate position in the aetiology of flexor pollicis longus tendon rupture after volar plate fixation of distal radius fractures. Hand (N Y) 2015;10(03):497–502. doi: 10.1007/s11552-014-9735-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Limthongthang R, Bachoura A, Jacoby S M, Osterman A L. Distal radius volar locking plate design and associated vulnerability of the flexor pollicis longus. J Hand Surg Am. 2014;39(05):852–860. doi: 10.1016/j.jhsa.2014.01.038. [DOI] [PubMed] [Google Scholar]
- 9.Asadollahi S, Keith P P. Flexor tendon injuries following plate fixation of distal radius fractures: a systematic review of the literature. J Orthop Traumatol. 2013;14(04):227–234. doi: 10.1007/s10195-013-0245-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kitay A, Swanstrom M, Schreiber J J et al. Volar plate position and flexor tendon rupture following distal radius fracture fixation. J Hand Surg Am. 2013;38(06):1091–1096. doi: 10.1016/j.jhsa.2013.03.011. [DOI] [PubMed] [Google Scholar]
- 11.Kara A, Celik H, Bankaoglu M, Oc Y, Bulbul M, Sugun T S. Ultrasonic evaluation of the flexor pollicis longus tendon following volar plate fixation for distal radius fractures. J Hand Surg Am. 2016;41(03):374–380. doi: 10.1016/j.jhsa.2015.11.022. [DOI] [PubMed] [Google Scholar]
- 12.Oura K, Oka K, Kawanishi Y, Sugamoto K, Yoshikawa H, Murase T. Volar morphology of the distal radius in axial planes: a quantitative analysis. J Orthop Res. 2015;33(04):496–503. doi: 10.1002/jor.22780. [DOI] [PubMed] [Google Scholar]
- 13.Nanno M, Kodera N, Tomori Y, Takai S. Transverse ultrasound assessment of the flexor pollicis longus tendon movement on the distal radius during wrist and finger motion in distal radius fracture with volar plating. J Med Ultrason (2001) 2016;43(01):29–36. doi: 10.1007/s10396-015-0670-0. [DOI] [PubMed] [Google Scholar]
- 14.Schlickum L, Quadlbauer S, Pezzei C, Stophasius E, Hausner T, Leixnering M. Three-dimensional kinematics of the flexor pollicis longus tendon in relation to the position of the FPL plate and distal radius width. Arch Orthop Trauma Surg. 2019;139(02):269–279. doi: 10.1007/s00402-018-3081-z. [DOI] [PubMed] [Google Scholar]
- 15.Agnew S P, Ljungquist K L, Huang J I. Danger zones for flexor tendons in volar plating of distal radius fractures. J Hand Surg Am. 2015;40(06):1102–1105. doi: 10.1016/j.jhsa.2015.02.026. [DOI] [PubMed] [Google Scholar]
- 16.Nelitz M. Femoral derotational osteotomies. Curr Rev Musculoskelet Med. 2018;11(02):272–279. doi: 10.1007/s12178-018-9483-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nanno M, Kodera N, Tomori Y, Takai S. Ultrasonographic movement of the flexor pollicis longus tendon before and after removal of a volar plate for the distal radius fracture. J Orthop Surg (Hong Kong) 2018;26(01):2.309499018760131E15. doi: 10.1177/2309499018760131. [DOI] [PubMed] [Google Scholar]


