ABSTRACT
A 52-year-old man with a cough, high fever, and inappetence was diagnosed with thoracic empyema on computed tomography at a local hospital. He had undergone continuous thoracic drainage for a spontaneous esophageal rupture that occurred 17 years earlier. He developed left thoracic empyema 2, 14 and 17 years following the initial esophageal rupture that improved with conservative therapy each time. The most recent episode of thoracic empyema also resolved with conservative therapy. However, he was referred to our hospital for further examination and more complete surgical treatment for recurrent thoracic empyema. Gastrointestinal endoscopy showed a scar from the previous esophageal rupture in the lower esophagus. We considered that recurrent esophageal rupture may have caused repeated episodes of thoracic empyema based on endoscopic findings and his past history and elected to perform subtotal esophagectomy to provide a complete cure. A left transthoracic esophagectomy with a left lower lung lobectomy and gastric tube reconstruction via a retrosternal route were performed. A latissimus dorsi muscle flap was used to eliminate the dead space after lower lung lobectomy to prevent recurrent thoracic empyema. The bronchial stump was covered with a pedicled intercostal muscle flap to prevent leakage from the stump. Minor leakage from the esophagogastrostomy site developed during the postoperative course but resolved with conservative therapy. The patient was transferred to the previous hospital on the 36th postoperative day. Four years after surgery, he had good oral intake and nutritional status without any evidence of recurrent thoracic empyema.
Key Words: thoracic empyema, spontaneous esophageal rupture
INTRODUCTION
Spontaneous esophageal rupture is a relatively rare clinical condition, and early diagnosis and treatment are of great importance to prevent the development of life-threatening mediastinitis and thoracic empyema. Although many reports of various treatments for esophageal rupture during the acute phase have been published,1 only a few reports have described the subsequent course after esophageal rupture and discussed recurrent esophageal rupture.2-5 In addition, there are no reports of repeated episodes of thoracic empyema after spontaneous esophageal rupture.
Herein, we report a case of recurrent episodes of thoracic empyema after spontaneous esophageal rupture that was successfully treated with a left transthoracic subtotal esophagectomy and lower lung lobectomy.
CASE PRESENTATION
A 52-year-old man with a cough, high fever, inappetence, and a history of diabetes mellitus was diagnosed with thoracic empyema on computed tomography (CT) at another hospital. He had undergone continuous thoracic drainage for spontaneous esophageal rupture seventeen years earlier. He developed left thoracic empyema 2 and 14 and 17 years following the initial esophageal rupture that improved with conservative therapy, including fasting, antibiotics, and continuous thoracic drainage, each time. The patient experienced another episode of left thoracic empyema that improved with similar conservative therapy. However, the patient was referred to our hospital for further examination and more complete surgical treatment for recurrent thoracic empyema three months after the onset of this episode.
Gastrointestinal endoscopy showed a depression that appeared to be a scar from a rupture in the left wall of the lower esophagus (Fig 1a). Esophagography revealed a bulge of contrast medium in the left wall of the lower esophagus but no contrast extravasation from the esophagus (Fig 1b). CT showed an abscess along the mediastinum extending from the left lower pleural cavity (Fig 2a). Moreover, a funicular structure that continued from the left lower esophageal wall to the abscess cavity was identified as a fistula (Fig 2b). CT performed at the onset of the third and fourth episodes of thoracic empyema showed an intrathoracic abscess with niveau formation (Fig 3a, c). We considered that recurrent esophageal rupture may have caused repeated episodes of thoracic empyema based on the examination findings and his past history and elected to perform subtotal esophagectomy to provide a complete cure.
Fig. 1.
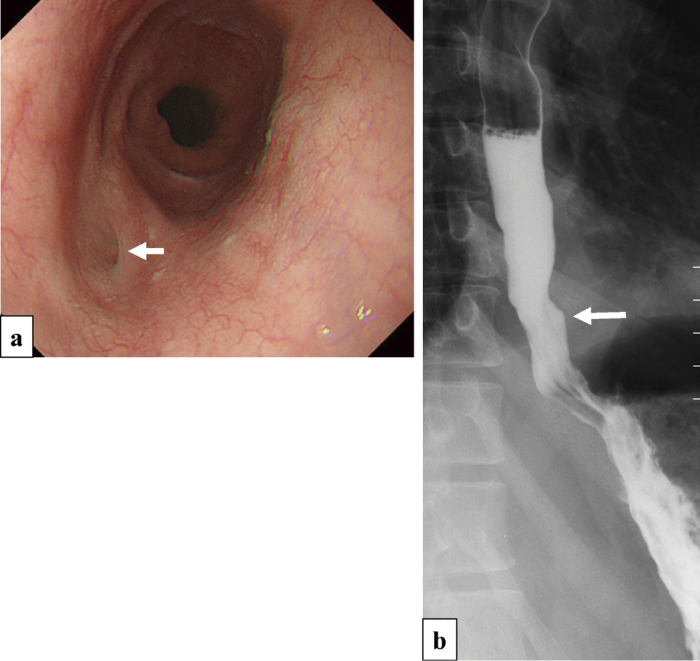
Endoscopic findings and esophagography after the fourth episode
Fig. 1a: Gastrointestinal endoscopy showing a depression that seemed to be a scar of an esophageal rupture in the left wall of the lower esophagus (white arrow).
Fig. 1b: Esophagography showing a bulge of contrast medium at the depression presumed to be a fistula without contrast extravasation from the esophagus (white arrow).
Fig. 2.

CT image after the fourth episode
Fig. 2a: Contrast-enhanced coronal CT image showing an abscess along the mediastinum in the left lower pleural cavity.
Fig. 2b: CT showing a fistula from the abscess (white arrows) that continued through the mediastinum from the thoracic cavity to the esophagus (white arrowheads).
Fig. 3.
A change of chest CT image from the third to the fourth episode
Fig. 3a: CT performed at the onset of the third episode showing an intrathoracic abscess with niveau formation.
Fig. 3b: CT performed four months after the fourth episode showing resolved niveau formation with a small amount of encapsulated liquid in the bottom of the lung.
Fig. 3c: CT performed at the onset of the fourth episode showing an intrathoracic abscess with niveau formation.
A left posterolateral thoracotomy was performed through the fifth intercostal space, and a latissimus dorsi muscle flap based inferiorly and an intercostal muscle flap were created (Fig 4a, b). The left lung was adherent, and approximately 30 ml of purulent material was drained from the abscess cavity. The culture result of this purulent material was negative. The left lower lung lobe was considerably atrophied due to chronic inflammation, and the lower esophagus, left lower lung lobe, and abscess cavity were clumped together. Therefore, the left lower lobe that was integrated with the abscess wall was removed with the esophagus (Fig 4c). The fistula could not be identified due to the adhesions. The esophagus was transected just below bifurcation of the trachea. The remnant upper thoracic esophagus was pulled out to the neck by manual dissection via a cervical approach. The left bronchial stump was covered with a pedicled intercostal muscle flap to prevent bronchial stump leakage, and a latissimus dorsi muscle flap was used to eliminate the dead space after lower lung lobectomy with abscess wall resection through the 9th intercostal space to prevent recurrent thoracic empyema (Fig 4d). Esophageal reconstruction was performed using a gastric conduit via a retrosternal route.
Fig. 4.

Operative findings
Fig. 4a: Creation of a latissimus dorsi muscle flap (white arrow).
Fig. 4b: Thoracotomy with a pedicled intercostal muscle flap (arrow).
Fig. 4c: Removal of the left lower lung lobe that was integrated with the abscess wall and the esophagus.
Fig. 4d: Use of a latissimus dorsi muscle flap to eliminate the dead space after lower lung lobectomy with abscess wall resection (white arrow); use of a pedicled intercostal muscle flap to cover the bronchial stump (white arrowhead).
Histological examination of the resected specimen revealed disruption of the muscularis mucosa in the depression that appeared to be a scar resulting from an esophageal rupture with fibrosis and foreign body deposits (Fig 5). Further exploration to determine the presence or absence of a fistula could not be performed because the resected specimen was crushed. Minor leakage from the esophagogastrostomy site developed during the postoperative course but resolved with conservative therapy. Oral intake began on the 28th postoperative day. The patient was transferred to the previous hospital on the 36th postoperative day. Four years after surgery, he had good oral intake and nutritional status without any evidence of recurrent thoracic empyema.
Fig. 5.

Histological findings of the resected specimen
Histological examination of the resected specimen revealing disruption of the muscularis mucosa in the depression that appeared to be a scar resulting from an esophageal rupture with fibrosis and foreign body deposits (between the black arrows).
DISCUSSION
Spontaneous esophageal rupture is a relatively rare disease. Recurrence of spontaneous rupture is extremely rare. To the best of our knowledge, only ten patients with recurrent spontaneous esophageal rupture have been described, and all those patients experienced a second spontaneous rupture.2-4 There are no previous reports of repeated episodes of thoracic empyema after spontaneous esophageal rupture, such as in this case. During this episode, the presence of esophageal rupture could not be directly proven, and the possibility of a lung fistula and exacerbation of a residual abscess could not be ruled out. It is highly probable that air entered the abscess from the esophagus, as evidenced by visualization of an intrathoracic abscess with niveau formation on CT images at the onset of the third and fourth episodes. When a lung fistula develops, purulent material in the abscess enters the respiratory tract; therefore, pneumonia is can occur. However, such findings were not observed during the third and fourth episodes in this patient. Regarding exacerbation of a residual abscess, Streptococcus mitis and Citrobacter koseri were detected by culture of the purulent material drained from the thoracic abscess during the third episode. Citrobacter koseri is a gas-producing bacterium; thus, the fourth episode was possibly caused by an exacerbation of chronic empyema. However, considering endoscopic and CT finding, we speculated that recurrent esophageal rupture occurred at the onset of the third and fourth episodes, which caused the repeated episodes of thoracic empyema.
The cause of recurrent spontaneous esophageal rupture has been reported to be associated with gastroesophageal reflux,6 alcohol consumption,2,4,7,8 and antiphospholipid antibody syndrome.3 This patient had no history of alcohol intake, reflux esophagitis or symptoms. Esophageal mobility disorders have been reported to be related to spontaneous esophageal rupture,9 and this patient had mild dysphagia before surgery. Although esophageal manometry was not performed in this patient, an esophageal motility disorder could possibly have been the cause of recurrent esophageal rupture. In addition, diabetes mellitus may prevent fistulas from healing completely.
A simple suture closure is generally performed for spontaneous esophageal rupture, but it is desirable to reinforce the primary sutured site in ruptures that occur more than 24 hours prior to surgery. The tissues that can be used for reinforcement include the gastric fundus,10 a pedicled omental flap,11 an elevated diaphragmatic pedicle graft,12 or a rhomboid and latissimus dorsi muscle flap.13 In this case, ligation or excision of the fistula and covering of the defect with a latissimus dorsi muscle flap were considered. However, it was impossible to separate the esophagus, left lower lung, and abscess cavity due to the dense adhesions caused by chronic thoracic empyema, and this pathogenesis might have been in the esophagus itself; thus, we decided to perform a subtotal esophagectomy to provide a complete cure. A left lower lung lobectomy along with resection of the wall of the abscess cavity in the left pleural space was also performed because the presence of an atrophic left lower lung lobe integrated with the abscess wall might have led to repeated thoracic empyema. An omental flap accompanied by a gastric conduit reconstructed via a posterior mediastinal route was deemed to be used to eliminate the dead space after lower lung lobectomy with abscess wall resection to prevent recurrent thoracic empyema. However, considering the patient’s past history and that refractory fistula formation was likely to occur, a retrosternal route was chosen. A latissimus dorsi muscle flap created during thoracotomy was used to eliminate the dead space. Postoperative CT revealed no dead space. The bronchial stump was covered with a pedicled intercostal muscle flap to prevent bronchial leakage.
Fortunately, this patient was completely cured by esophagectomy and left lower lung lobectomy with resection of the abscess wall. However, because the esophageal fistula could not be histologically proven and the defect in the esophageal wall was repaired by fibrosis, perhaps the esophagus could have been preserved.
CONCLUSION
Repeated thoracic empyema after spontaneous esophageal rupture is very rare, but this patient was successfully treated with a left transthoracic esophagectomy, lower lung lobectomy, gastric tube reconstruction via a retrosternal route, and a latissimus dorsi muscle flap to eliminate dead space.
COMPETING INTERESTS
The authors declare that they have no competing interests.
REFERENCES
- 1).de Schipper JP, Pull ter Gunne AF, Oostvogel HJ, van Laarhoven CJ. Spontaneous rupture of the oesophagus: Boerhaave's syndrome in 2008. Literature review and treatment algorithm. Dig Surg. 2009;26(1):1–6. [DOI] [PubMed]
- 2).Wang SC, Scott WW, Jr. Recurrent spontaneous esophageal rupture managed with esophageal stenting. Ann Thorac Surg. 2016;102(1):e5–6. [DOI] [PubMed]
- 3).Naitoh H, Fukuchi M, Kiriyama S, et al. Recurrent, spontaneous esophageal ruptures associated with antiphospholipid antibody syndrome: report of a case. Int Surg. 2014;99(6):842–845. [DOI] [PMC free article] [PubMed]
- 4).Ieta K, Oki A, Teshigahara K, et al. Recurrent spontaneous esophageal rupture. Clin J Gastroenterol. 2013;6(1):33–37. [DOI] [PubMed]
- 5).D'Journo XB, Doddoli C, Avaro JP, et al. Long-term observation and functional state of the esophagus after primary repair of spontaneous esophageal rupture. Ann Thorac Surg. 2006;81(5):1858–1862. [DOI] [PubMed]
- 6).Khan OA, Barlow CW, Weeden DF, Amer KM. Recurrent spontaneous esophageal rupture. Eur J Cardiothorac Surg. 2005;28(1):178–179. [DOI] [PubMed]
- 7).Reeder LB, Warren SE, Ferguson MK. Recurrent spontaneous perforation of the esophagus. Ann Thorac Surg. 1995;59(1):221–222. [DOI] [PubMed]
- 8).Lujan HJ, Lin PH, Boghossian SP, Yario RF, Tatooles CJ. Recurrent spontaneous rupture of the esophagus: an unusual late complication of Boerhaave’s syndrome. Surgery. 1997;122(3):634–636. [DOI] [PubMed]
- 9).Salo JA, Seppala KM, Pitkaranta PP, Kivilaakso EO. Spontaneous rupture and functional state of the esophagus. Surgery. 1992;112(5):897–900. [PubMed]
- 10).Symbas PN, Hatcher CR, Jr., Harlaftis N. Spontaneous rupture of the esophagus. Ann Surg. 1978;187(6):634–640. [DOI] [PMC free article] [PubMed]
- 11).Sabanathan S, Eng J, Richardson J. Surgical management of intrathoracic oesophageal rupture. Br J Surg. 1994;81(6):863–865. [DOI] [PubMed]
- 12).Kotsis L, Agocs L. The effectiveness of diaphragmatic pedicled grafts in esophageal injuries and wall reconstruction. Eur J Cardiothorac Surg. 1998;14(2):218–220. [DOI] [PubMed]
- 13).Richardson JD, Tobin GR. Closure of esophageal defects with muscle flaps. Arch Surg. 1994;129(5):541–547; discussion 547–548. [DOI] [PubMed]



