Abstract
We examined whether the patient-provider relationship (PPR) is associated with Black survivors’ health outcomes and whether this association was mediated by the quality of care.
The outcome variables were survivors’ quality of care and health outcome and the predictor variable was PPR (communication, emotional support, time spent, and survivors’ shared-decision makingA sample of 223 Black cancer survivors (age 63.0±14.0 years) provided evaluable data. The most common cancer types reported by the participants were: gynecologic (32.7%), genitourinary (21.5%), and gastrointestinal cancers (11.2%). After controlling for covariates, A Structural Equation Model (SEM) showed that PPR was significantly associated with both health outcome (p=0.015) and quality of care (p=0.002). When PPR and quality of care were tested in the mediation model, the direct association between PPR and health outcome was attenuated, and it was no longer significant (b= −0.05, SE=0.11, p=0.65). However, indirectly, there was a strong association between PPR and health outcome through the quality of care (b= 0.22, SE=0.08, p=0.003), indicating full mediation.
Providers’ interpersonal relationships had a significant influence on the health of Black survivors, and this influence may be due to the increased positive perception of quality of care. The implications of these findings for further research are discussed.
Keywords: Black cancer survivors, patient-provider relationship, quality of care, health status
Introduction
Disparities in quality of care and health outcomes between Black and White populations with cancer in the United States (US) are well documented (National Center for Health Statistics 2016; DeSantis et al., 2016). A number of interpersonal factors contribute to disparities in quality of care for racial and ethnic minorities (Smedley, Stith, & Nelson, 2003). These factors consisted of providers’ and survivors’ attitudes and behaviors towards each other during clinical encounters, hereafter known as patient-provider relationship (PPR). The patient-provider relationship is multidimensional and consists of managing uncertainty, responding to emotions, making decisions, fostering healing, enabling self-management, and exchanging information/communication ( Blanch-Hartigan et al., 2016; Sabee, Koenig, Wingard, Foster, Chivers, Olsher, & Vandergriff, 2015).
Several recent studies have focused on aspects of the patient-provider relationship, specifically among White and Black survivors. Studies have analyzed PPR in an oncology setting (Baile & Aaron, 2005; Emanuel, Godinho, Steinman, & Updegraff, 2016; Levit, Balogh, Nass, & Ganz, 2013; Lin et al., 2014; Mangione, et al., 2006; Nelson, et al., 2004; Sofaer & Firminger, 2004), the providers’ impact on quality of life (Li, Matthews, Dossaji, & Fullam, 2017; Penner et al., 2016; Rains, 2007), racial and ethnic disparities in patient-provider communication (Dugdale, Epstein, & Pantilat, 1999; Fortney, Rost, Zhang, & Pyne, 2001; Sofaer & Firminger, 2004), and survivors’ perceptions about the quality of their physician’s communication (Levit et al., 2013; Robbins, Bertakis, Helms, Azari, Callahan, & Creten, 1993; Sofaer & Firminger, 2004). Recent literature reviews concluded that effective and empathic communication with the cancer patient and his or her family enhances cancer care, patient quality of life (Baile & Aaron, 2005; Bredart, Bouleuc, & Dolbeault, 2005), satisfaction with care (Baile & Aaron, 2005; Bredart et al., 2005; Hou & Shim, 2010), and medical outcomes (Baile & Aaron, 2005; Bredart et al., 2005; Ha & Longnecker, 2010).
Although these studies have furthered our understanding of patient-provider communication, studies that have examined the interactions between providers’ time spent with patients, shared decision-making, emotional support, and providers’ communication and quality of care and health outcomes in Black cancer survivors are relatively rare.
Therefore, the purpose of our study was to evaluate associations among patients’ perceptions of their PPR (communication, emotional support, shared decision-making, and time spent with patients), the quality of care they received in the last 12 months, and their perceived health status in a sample of Black patients who have a history of cancer (Black cancer survivors).
Materials and Methods
Data Source
To test the hypotheses of the study, we utilized the Health Information National Trends Survey (HINTS) [https://hints.cancer.gov/data/download-data.aspx] datasets from 2011 to 2014 and data from subsample of 223 Black cancer survivors were included in the study. Respondents were included in the study if they met the following inclusion criteria: they self-identified as Black/African Americans, they reported a history of cancer diagnosis, and they provided information regarding outcome and predictor variables
Measures
Data were collected on the demographic characteristics of the participants including age, gender, marital status, education, income, and employment. The outcome variables were based on self-reported responses on quality of care and self-rated health. The predictor variable was PPR calculated from eight items: providers’ communication with survivors; emotional support; time spent with survivors; and involvement of survivors in decision making. (see Figure 1).
Figure 1.
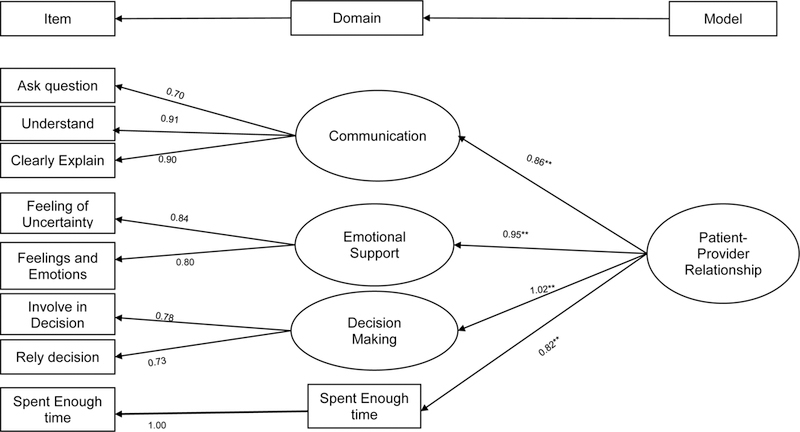
Path Diagram Displaying the CFA for Standardized Regression for PPR [χ2 (26, n = 223) = 32.25, p =.189]. CFI = .993, GFI = .977, RMSEA = .033
Statistics Analyses
Descriptive statistics were computed for demographic and clinical characteristics, self-rated quality of care, self-rated health outcome, and the PPR items. A single factor was calculated from eight items (see Figure 1). We evaluated a mediation model using a four-step evaluation approach outlined by Baron and Kenny (1986). All analyses were performed in SPSS version 25 and Amos and were weighted. Statistical significance was deemed at P<0.05.
Results
Demographics:
A subsample of 223 Black cancer survivors (age 63.0±14.0 years) provided evaluable data that were included in the analysis. Most participants were female (62.3%), unmarried (66.5%), and not working (74.9%). (see demographic characteristics in Table 1).
Table 1.
Demographics and clinical characteristics of black cancer patients
| Variable | N=223 Frequency | Percentage |
|---|---|---|
| Age | Mean=63 | S.D.=14 |
| Gender | ||
| Male | 84 | 37.7 |
| Female | 139 | 62.3 |
| Marital status | ||
| Married | 77 | 34.5 |
| Unmarried | 146 | 66.5 |
| Education | ||
| Less than high school | 32 | 14.3 |
| High school | 64 | 28.7 |
| Some college | 71 | 31.8 |
| College graduate or more | 56 | 25.1 |
| Household income | ||
| < $50,000/yr | 88 | 39.5 |
| ≥ $50,000/yr | 135 | 60.5 |
| Employment | ||
| Not working | 167 | 74.9 |
| Employed | 56 | 25.1 |
| Country of Birth | ||
| United States | 205 | 91.9 |
| Foreign | 18 | 8.1 |
| Cancer type | ||
| Gynecologic Cancer | 73 | 32.7 |
| Head and Neck | 3 | 1.3 |
| Gastrointestinal cancer | 25 | 11.2 |
| Hematologic cancer | 13 | 5.8 |
| Genitourinary Cancer | 48 | 21.5 |
| Lung | 4 | 1.8 |
| Other | 42 | 18.8 |
| Missing Data | 15 | 6.7 |
Regression models:
In model 1, the participants’ demographic variables were entered into the models, and only education (p<0.01) and sex (p<0.01) were significant predictors for self-related health outcome. The demographic variables in Model 1 accounted for 14% of the variance in participants’ health outcome (R2 =0.14). When the PPR was included in the model (Model 2), PPR significantly predicted health outcome, and the R2 value increased to 16%, indicating that a 2.4% increase in the variability of the participants’ health outcome was due to PPR (p < 0.001). In the final model, (Model 3) including the quality of care variable increased the predictive capacity of the model to 20%, indicating that quality of care accounted for additional 3.8% of the variability in the participants’ health outcome (see Table 2).
Table 2:
Summary of multiple regression analyses for covariates, Patient-Provider, and quality of care Predicting Patients Self-reported health status (n=223)
| Variable | Model 1 | Model 2 | Model 3 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| B | SE B | β | B | SE B | β | B | SE B | β | |
| Education | 0.20 | 0.07 | 0.21** | 0.22 | 0.07 | 0.23** | 0.18 | 0.07 | 0.19** |
| Sex | −0.37 | 0.14 | −0.19** | -0.38 | 0.14 | −0.19** | −0.37 | 0.13 | −0.19** |
| Marital | 0.01 | 0.14 | 0.01 | -0.02 | 0.14 | −0.01 | −0.02 | 0.14 | −0.01 |
| Employment | 0.34 | 0.16 | 0.15* | 0.30 | 0.16 | 0.14 | 0.29 | 0.16 | 0.13 |
| Born | 0.09 | 0.23 | 0.03 | 0.11 | 0.23 | 0.03 | 0.04 | 0.22 | 0.01 |
| Age | 0.01 | 0.01 | 0.12 | 0.01 | 0.01 | 0.12 | 0.01 | 0.01 | 0.10 |
| Cancer Type | 0.00 | 0.00 | 0.06 | 0.00 | 0.00 | 0.06 | 0.00 | 0.00 | 0.07 |
| Income | 0.16 | 0.14 | 0.08 | 0.14 | 0.14 | 0.07 | 0.14 | 0.13 | 0.07 |
| Patient-Provider Relationship | − | − | − | 0.03 | 0.01 | 0.16* | 0.00 | 0.02 | 0.00 |
| Quality of care | − | − | − | − | − | − | 0.27 | 0.09 | 0.25** |
| R2 | 0.14 | 0.16 | 0.20 | ||||||
| F for change in R2 | 0.14** | 0.024* | 0.038** | ||||||
Note:
p<.05.
p<.01
Mediation analyses:
The Structural Equation Model (SEM) was used to evaluate the four steps of the mediation model analyses while controlling for covariates such as age, gender, marital status, education, employment, and income. First, the standardized total effects (direct and indirect) of PPR on self-rated health outcome was significant [b =0.17, SE =0.07, p=0.015, (c1-path)] indicating a strong association between PPR and health outcome (the unmediated model). Second, PPR was directly associated with quality of care [b=0.78, SE=0.04, p=0.002, (a-path)] indicating a strong association between PPR and quality of care. Third, quality of care was also directly associated with self-rated health outcomes [b=0.28, SE=0.10, p=0.003, (b-path)], indicating a strong association between quality of care and health outcome. Fourth and finally, because the a-path and b-path were significant, mediation effects were tested using bootstrapping with bias-corrected confidence estimates. When the quality of care was added to the final model (the mediation model), the association between PPR and health outcomes was attenuated, and it was no longer significant [b=−0.05, SE=0.11, p=0.65, (c-path)], indicating no direct effect between PPR and health outcome. However, indirectly there was a strong association between PPR and health outcome through the quality of care [b=0.22, SE=0.08, p=0.003] suggesting a full mediation of quality of care on the relation between PPR and health outcome. (see Figure 2.)
Figure 2.
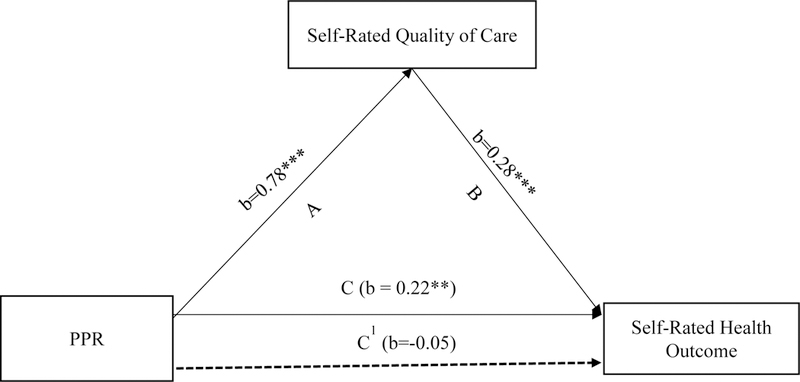
Indirect effect of PPR on self-rated health outcome through quality of care showing a full mediation.
Note: **p<.01, *** p<.001
A= indicates a pathway showing significant association between PPR and self-rated quality of care
B= indicates a pathway showing association between self-rated quality of care and self-rated health outcome
C1= indicates a pathway showing a direct association between PPR and self-rated health outcome after controlling for quality of care.
C. Showing a significant indirect association between PPR and self-rated health outcome through quality of care (full mediation).
Discussion
Our results show that quality of care is a significant mediator in the association between PPR and self-reported health in Black survivors with cancer. Overall, providers’ positive interpersonal relationship behaviors that had the greatest influence were effective communication and shared decision-making. Also, the quality of PPR is directly related to the health of survivors, accounting for 2.4% variance in the participants’ health outcome. However, quality of care significantly increases the models predicted capacity to 20% indicating that quality of care alone accounted for an additional 3.8% of the variability in the participant health outcome. Survivors who had high-quality care reported better relationships with the providers.
The most important finding of the current study is that the associations between patient-provider relationship and Black cancer survivors’ perceived health outcome are fully mediated by the perceived quality of care. This finding suggests that the amount of time providers spent with survivors, shared-decision making between survivors and providers, and emotional support survivors received from providers are strong predictors of good general health. Similarly, effective communication, including providers making sure survivors understand instructions, clearly explaining instructions, and giving survivors an opportunity to ask questions and clarify instructions are all important to Black cancer survivors’ perceived health outcome. These findings provide further evidence that quality of care is not only strongly associated with health outcome(Fortney et al., 2001; Mangione et al., 2006), but also the quality of care facilitates a better understanding of how Black cancer survivors perceived their relationship with providers and how that relationship affects their health outcome.
The results of this study showed that the majority of the survivors perceived that their providers engaged in effective communication with them by always giving them an opportunity to ask all the health-related questions they had, making sure they understood the things they needed to do to take care of their health and explaining things in a way they could understand. This finding is consistent with other studies that found survivors who engaged in good communication with their providers had better health outcomes (Baile & Aaron, 2005; Bredart et al., 2005) and helped patients managed their uncertainties (Dean & Davidson, 2018).
Many of the survivors also reported that their providers always or usually paid attention to their feelings and emotions, as well as helped them deal with feelings of uncertainty about their health. The findings of this study are congruent with the conclusion drawn by Sofaer and Firminger (2004) in their comprehensive review that better health outcomes occur when providers give support to survivors dealing with negative emotions and feelings of uncertainty. Notably, others have found that providers’ emotional support is associated with survivors’ emotional security, trust in providers, and reduction of survivors’ feelings of vulnerability and anxiety (Dean & Davidson, 2018; Sofaer & Firminger, 2004).
Furthermore, survivors had positive responses about the amount of time their provider spent with them. Many of the survivors perceived that they “usually” or “always” had positive relationships with their provider. This finding is agreement with other studies that the amount of time the physician spent in engaging survivors about their health had an important bearing on patient satisfaction (Robbins et al., 1993). While the health impact of the length of time that providers spent with their patients has been debated in the literature (Dugdale et al., 1999), the findings of this study suggest that the amount of time a provider spends with a patient explaining instructions and making sure that the patient clearly understands their medical instructions has a strong association with better health and functional status. This finding is consistent with the study by Dugdale et al (1999) that physician quality of time spent to gather information from and/or provide information to patients has a strong relationship with functional status.
Another finding worth noting is that participants’ education and gender significantly predict their health outcome. Women are more likely to report poor health outcomes compared to men, and this finding supports national data on morbidity that suggest that slightly more women than men report that they are in fair or poor health (Eberhardt et al., 2001). Participants’ education significantly predicts their perceived health outcome. This study shows that participants’ low education predicted their poor health outcome, suggesting Black survivors’ poor health outcome might be because of social (including patient-provider relationship) and economic disparities rather than biological differences (DeSantis et al., 2016) Further studies such as a longitudinal study need to be conducted to help our understanding of how health outcome disparities among Black patients are associated with social constructs.
Limitations
There are weaknesses to be considered when applying existing data to future endeavors. First, the use of existing public data limits our ability to analyze all aspects of patient-provider relationships. This study also comes with the general limitations of a cross-sectional, survey-based study. For example, there could have been responder bias in the returned surveys. Also, 91% of the Black participants in this study were born in the US, so one must be prudent when applying these data to Black individuals who are foreign-born and may have different cultural expectations of what a positive PPR looks like. Health outcome and quality of care items were measured using a single-item question only and the reliability and validity of those items are not known. However, those items have been used previously in several studies (Desai, Chewning, & Mott, 2015; Jiang & Beaudoin, 2016).
Nonetheless, there are many strengths to this study. While studies have established strong associations between PPR and positive health outcomes and patients’ satisfaction, this study accomplishes three things. (a) The findings of this study validate existing literature which links PPR to positive health outcomes. (b) The study demonstrates that quality of care is a strong mediator between PPR and survivors’ health outcomes. (c) Finally, the study expands the existing literature on PPR and quality of care to include Black cancer patients who, in many respects, are marginalized in this area of study. Even though it is well documented that Black patients disproportionately experience a heavy burden of the poor quality of care, to date studies that exclusively examine the impact of quality care on PPR and health in Black patients are rare. Our analysis leveraged the usefulness of the HINTS database, which included 223 Black cancer survivors. While this sample size is small compared to many national surveys of cancer survivors, this is a relatively large number of Black cancer survivors in a single study. This hypothesis-generating study can help guide further research into the mediation effect of quality of care using a different approach to determine health outcomes.
Future directions
The health outcome used for this study was self-reported, so future studies should use biomarkers to measure functional health outcomes. These data can inform the development of an intervention to enhance the PPR and improve patient health. Future interventions could be developed to focus on effective communication between the patient and the provider. For example, intervention could be developed to (a) encourage healthcare providers to give survivors an opportunity to ask questions during an appointment, (b) utilize a teach-back method that ensures the patient understands all given instructions, and (c) emphasize the importance of appointment duration and spend adequate time with their survivors to guarantee that the patient feels like the provider knows them “as a person” and not solely as a patient (Beach, Keruly, & Moore, 2006). In addition, in the era of managed care, providers spending more time with patients to provide high-quality care may be mutually beneficial to patients, providers, and payers. Additionally, healthcare providers should involve survivors in decision-making regarding their treatment plans, and they should provide emotional support and empathize with patients.
Conclusion
Providers’ positive interpersonal relationships—including effective communication and involvement in decision making—had a significant positive influence on the health of Black cancer survivors, and this influence may be due to the increased positive perception of quality of care. These findings can inform the development of interventions to enhance PPRs among Black cancer survivors to improve patient outcomes and self-rated health.
Acknowledgments
Funding/Support: Funding was provided by R25 CA1026185 and UG1 CA189961.
This work was supported by NCI grant R25 CA1026185 and UG1 CA189961.
Footnotes
The authors declare no potential conflicts of interest.
References
- Baile WF, & Aaron J (2005). Patient-physician communication in oncology: Past, present, and future. Current Opinion Oncology, 17(4), 331–335. 10.1097/01.cco.0000167738.49325.2c [DOI] [PubMed] [Google Scholar]
- Baron RM, & Kenny DA (1986). The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51(6), 1173–1182. 10.1037/0022-3514.51.6.1173 [DOI] [PubMed] [Google Scholar]
- Beach MC, Keruly J, & Moore RD (2006). Is the quality of the patient-provider relationship associated with better adherence and health outcomes for patients with HIV? Journal of General Internal Medicine, 21(6), 661–665. 10.1111/j.1525-1497.2006.00399.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanch-Hartigan D, Chawla N, Moser RP, Finney Rutten LJ, Hesse BW, & Arora NK (2016). Trends in cancer survivors’ experience of patient-centered communication: Results from the health information national trends survey (HINTS). Journal of Cancer Survivorship, 10(6), 1067–1077. 10.1007/s11764-016-0550-7 [DOI] [PubMed] [Google Scholar]
- Bredart A, Bouleuc C, & Dolbeault S (2005). Doctor-patient communication and satisfaction with care in oncology. Current Opinion Oncology, 17(4), 351–354. 10.1097/01.cco.0000167734.26454.30 [DOI] [PubMed] [Google Scholar]
- Dean M, & Davidson LG (2018). Previvors’ uncertainty management strategies for hereditary breast and ovarian cancer. Health Communication, 33(2), 122–130. 10.1080/10410236.2016.1250187 [DOI] [PubMed] [Google Scholar]
- Desai K, Chewning B, & Mott D (2015). Health care use amongst online buyers of medications and vitamins. Research in Social and Administrative Pharmacy, 11(6), 844–858. 10.1016/j.sapharm.2015.01.001 [DOI] [PubMed] [Google Scholar]
- DeSantis CE, Siegel RL, Sauer AG, Miller KD, Fedewa SA, Alcaraz KI, & Jemal A (2016). Cancer statistics for African Americans, 2016: Progress and opportunities in reducing racial disparities. CA: A Cancer Journal for Clinicians, 66(4), 290–308. 10.3322/caac.21340 [DOI] [PubMed] [Google Scholar]
- Dugdale DC, Epstein R, & Pantilat SZ (1999). Time and the patient–physician relationship. [Supplemental material]. Journal of General Internal Medicine, 14, 34–40. 10.1046/j.1525-1497.1999.00263.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eberhardt MS, Freid VM, Harper S, Ingram DD, Makuc DM, Pamuk E, … Prager K (2001). Health, United States, 2001, with urban and rural health chartbook Retrieved from https://www.cdc.gov/nchs/data/hus/hus01cht.pdf
- Emanuel AS, Godinho CA, Steinman C, & Updegraff JA (2016). Education differences in cancer fatalism: The role of information-seeking experiences. Journal of Health Psychology, 23(12), 1533–1544. 10.1177/1359105316664129 [DOI] [PubMed] [Google Scholar]
- Fortney J, Rost K, Zhang M, & Pyne J (2001). The relationship between quality and outcomes in routine depression care. Psychiatric Services, 52(1), 56–62. 10.1176/appi.ps.52.1.56 [DOI] [PubMed] [Google Scholar]
- Ha JF, & Longnecker N (2010). Doctor-patient communication: A review. The Ochsner Journal, 10(1), 38–43. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/21603354 [PMC free article] [PubMed] [Google Scholar]
- Hou J, & Shim M (2010). The role of provider-patient communication and trust in online sources in Internet use for health-related activities. [Supplemental material]. Journal of Health Communication, 15, 186–199. 10.1080/10810730.2010.522691 [DOI] [PubMed] [Google Scholar]
- Jiang S, & Beaudoin CE (2016). Health literacy and the internet: An exploratory study on the 2013 HINTS survey. Computers in Human Behavior, 58, 240–248. 10.1016/j.chb.2016.01.007 [DOI] [Google Scholar]
- Levit L, Balogh E, Nass S, & Ganz PA (Eds) (2013). Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis Washington, DC, Institute of Medicine, . 91–12. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK202150/ [PubMed] [Google Scholar]
- Li CC, Matthews AK, Dossaji M, & Fullam F (2017). The relationship of patient-provider communication on quality of life among African-American and White cancer survivors. Journal of Health Communication, 22(7), 584–592. 10.1080/10810730.2017.1324540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin JJ, Lake J, Wall MM, Berman AR, Salazar-Schicchi J, Powell C, … Wisnivesky JP (2014). Association of patient–provider communication domains with lung cancer treatment. Journal of Thoracic Oncology, 9(9), 1249–1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mangione CM, Gerzoff RB, Williamson DF, Steers WN, Kerr EA, Brown AF, … Selby JV (2006). The association between quality of care and the intensity of diabetes disease management programs. Annals of Internal Medicine, 145(2), 107–116. [DOI] [PubMed] [Google Scholar]
- Smedley BD, Stith AY, & Nelson AR (Eds.). (2003). Institute of Medicine Committee on understanting eliminating racial and ethnic disparities in health care. Unequal treatment: confronting racial and ethnic disparities in health care Washington (DC): National Academies Press (US) Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK220358/ [PubMed] [Google Scholar]
- National Center for Health Statistics (2016). Health, United States, 2015: With special feature on racial and ethnic health disparities Retrieved from Hyattsville, MD: https://www.ncbi.nlm.nih.gov/books/NBK367640/ [PubMed] [Google Scholar]
- Nelson DE, Kreps GL, Hesse BW, Croyle RT, Willis G, Arora NK, … Alden S (2004). The health information national trends survey (HINTS): Development, design, and dissemination. [Discussion 481-444] Journal of Health Communication, 9(5), 443–460. 10.1080/10810730490504233 [DOI] [PubMed] [Google Scholar]
- Penner LA, Dovidio JF, Gonzalez R, Albrecht TL, Chapman R, Foster T, … Eggly S (2016). The effects of oncologist implicit racial bias in racially discordant oncology interactions. Journal of Clinical Oncology, 34(24), 2874–2880. 10.1200/JCO.2015.66.3658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rains SA (2007). Perceptions of traditional information sources and use of the world wide web to seek health information: Findings from the health information national trends survey. Journal of Health Communication, 12(7), 667–680. 10.1080/10810730701619992 [DOI] [PubMed] [Google Scholar]
- Robbins JA, Bertakis KD, Helms LJ, Azari R, Callahan EJ, & Creten DA (1993). The influence of physician practice behaviors on patient satisfaction. Family Medicine, 25(1), 17–20. [PubMed] [Google Scholar]
- Sabee CM, Koenig CJ, Wingard L, Foster J, Chivers N, Olsher D, & Vandergriff I (2015). The process of interactional sensitivity coding in health care: Conceptually and operationally defining patient-centered communication. Journal of Health Communication, 20(7), 773–782. 10.1080/10810730.2015.1018567 [DOI] [PubMed] [Google Scholar]
- Sofaer S, & Firminger K (2004). Patient perceptions of the quality of health services. Annual Review of Public Health, 26(1), 513–559. 10.1146/annurev.publhealth.25.050503.153958 [DOI] [PubMed] [Google Scholar]


