Serious conduct problems (CP) affect 4% to 10% of elementary school age children and are a common reason for referral to mental health services (Conduct Problems Prevention Research Group, 1992). Children with CP experience a host of negative developmental outcomes and place a high burden on society (Loeber & Farrington, 2001). Yet not all children with CP experience negative outcomes, spurring research aimed at understanding differences among children with CP. One factor that has proven to be especially useful in this regard is callous-unemotional (CU) traits. Children with CU traits exhibit an interpersonal-affective style that is characterized by a lack of remorse or guilt after misbehavior, a lack of empathy or concern for others, unconcern about their performance in developmentally important areas (school, work), and a shallow or deficient affective style. Over two decades of research demonstrates that children with CP and CU (CPCU) differ in significant and important ways from children with CP without CU (CP-only) (see Frick, Ray, Thornton, & Kahn, 2014 for a review) and CU was introduced as a specifier of conduct disorder (under the rubric “limited prosocial emotions”) in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (American Psychiatric Association, 2013).
There is now considerable (though not entirely consistent) evidence that children with CPCU respond less well to behavior therapy than do children with CP-only whether delivered through a parent intervention (Hawes, Price, & Dadds, 2014) or delivered directly to children (Wilkinson, Waller, & Viding, 2016). What might explain this pattern? One possibility is that children with CPCU have a unique learning style, characterized by decreased sensitivity to punishment especially when first primed by reward (see Byrd, Loeber, & Pardini, 2013; Matthys, Vanderschuren, & Schutter, 2013 for reviews), that impairs their response to behavior therapy. This unique learning style has been observed in behavioral tasks (Budhani & Blair, 2005; Fisher & Blair, 1998; O’Brien & Frick, 1996) and in studies of brain activity (Finger et al., 2011; Finger et al., 2008). Further, animal and human learning (Blair, Peschardt, Budhani, Mitchell, & Pine, 2006; Dadds & Salmon, 2003), criminal justice (Caldwell & Van Rybroek, 2005), and developmental (Kochanska, 1997) research suggests that punishment may serve to increase rates of antisocial behavior in children with CPCU by escalating their frustration, anger and revenge seeking or by impairing their guilt and moral reasoning. Treatment studies also suggest that punishment is less effective or even counter-productive when used to treat children with CPCU. For example, among children with CP, higher CU traits have been associated with decreased effectiveness of Time Out and more disruptive behavior during Time Out (Garcia, Graziano, & Hart, 2018; Haas et al., 2011; Hawes & Dadds, 2005). This research suggests that punishment may be counter-productive when treating children with CPCU and that reward-emphasized treatments may be needed instead (Frick et al., 2014; Kiehl, 2014; Moffitt et al., 2008). As written in one review: “Current treatments may not meet the needs of children with callous-unemotional traits. Specifically, punishment-based approaches may not work optimally. Translational research is needed to develop and evaluate treatments incorporating strict boundaries, consistent rewards, and appeal to self-interest.” (Moffitt et al., 2008, p. 10).
To date, only a handful of such translational studies have been conducted, with several reporting advantages of reward-emphasized or punishment de-emphasized treatments for youth with CU (Caldwell, 2011; Caldwell, Skeem, Salekin, & Van Rybroek, 2006; Datyner, Kimonis, Hunt, & Armstrong, 2015; Kimonis & Armstrong, 2012; Kimonis et al., 2018; Miller et al., 2014). However, other research suggests behavioral treatment is generally effective but youth with CU are neither more nor less responsive to reward and punishment components (Byrd, Hawes, Burke, Loeber, & Pardini, 2018; Ortiz, Hawes, Lorber, Lazer, & Brotman, 2018).
The purpose of this study was to test whether children with CPCU would respond significantly better to modified behavior therapy (MBT), which emphasized rewards and de-emphasized punishments, relative to treatment as usual, which was standard behavior therapy (SBT) that emphasized rewards and punishments equally (see Table 1 and online supplement for details of these treatments). In other words, we tested whether behavior therapy tailored to the specific characteristics of children with CPCU would show advantages over non-tailored behavior therapy, in accordance with recent writings advocating personalized approaches to psychosocial interventions generally (Leijten et al., 2017; Ng & Weisz, 2016; Scott, 2016) and psychopathy specifically (Hecht, Latzman, & Lilienfeld, 2018; Salekin, 2010). It was hypothesized that, within a sample of youth with CP, higher levels of CU would be associated with a more positive response to MBT relative to SBT.
Table 1.
Summary of Treatment Components for Standard Behavior Therapy and Modified Behavior Therapy
| Component | Standard Behavior Therapy | Modified Behavior Therapy |
|---|---|---|
| Point System | • Earn points for exhibiting positive behavior or failing to exhibit negative behavior • Lose points for exhibiting negative behavior |
• Earn points for exhibiting positive behavior or failing to exhibit negative behavior |
| Morning Module | • Awards for High Point Kid, Most Improved Kid • Award for Best Social Skills • Social Skills Training Module |
• Awards for High Point Kid, Most Improved Kid • Award for Best Helper • Emotion Skill Training Module |
| Daily Check In | • None | • Counselor initiated brief positive “check-in” encounter with each child at least twice per day |
| Sit-Out Cards | • None | • Each child is allowed to use up to 3 “I need a break” cards each day |
| Time Out Procedure | • Starts at 10 minutes • Must serve last 2 minutes appropriately • Escalated to 20 minutes for misbehavior during TO • End TO by asking why they were assigned TO |
• Starts at 10 minutes • Must serve last 2 minutes appropriately • Reduced to 5 minutes by serving TO appropriately • End TO by asking how they are feeling and what can be done to help them improve |
| Daily Behavior Consequences | • Positive consequences (recess) for positive daily behavior • Negative consequences (writing sentences, set apart from group) for negative daily behavior |
• Positive consequences (recess) for positive daily behavior • Group-based positive consequences (end of day fun activity chosen by kids) for positive daily behavior exhibited by treatment group |
| Weekly Behavior Consequences | • Positive consequences (field trip) for positive weekly behavior • Negative consequences (chores, boring tasks) for negative weekly behavior |
• Positive consequences (field trip) for positive weekly behavior. Extra incentives added to weekly field trip to make it more rewarding. |
| Intermittent Rewards | • None | • “Caught you being good” ticket system backed up by material rewards (toy store). |
Notes: Differences between conditions highlighted by italic font
Method
Participants
Participants were 46 children (36 boys and 10 girls), ages 7.0 to 12.6 years old (M = 9.3, SD = 1.4), who attended an intensive eight-week summer treatment program (STP) for children with disruptive behavior disorders. Participants were recruited from a large city in the southeastern United States. The majority of participants were Caucasian (n = 30, 65.2%) and Hispanic (n = 25, 54.3%). IQ scores, estimated using the Wechsler Abbreviated Scale of Intelligence 2nd edition (Wechsler, 2011), averaged 102 (SD = 12). All participants met diagnostic criteria for ODD and ADHD, and 29 (63.0%) also met diagnostic criteria for CD. Participants were oversampled for high levels of CU but a range of CU scores were represented (see distribution of CU in online supplement).
Eligibility criteria included: (a) full scale IQ at or above 75; (b) between 7.0 and 12.9 years old on the first day of treatment; (c) diagnosis of ODD and/or CD; (d) at least one custodial parent fluent in English; (e) able to participate in vigorous outdoor activities; and (f) parent agreement to keep the child’s medication treatment constant throughout treatment. One child dropped out after the first block of treatment due to an injury apparently unrelated to participation in the study. Of the 46 children, 11 (23.9%) were on stimulant medication throughout treatment. Two other children (in addition to the 46 participants) were excluded from analyses because their medication changed during treatment (i.e., stimulant medication was initially withheld by parents but restarted when their behavior became dangerous).
Procedure
Assessment and diagnosis.
The study was approved by a university Institutional Review Board, informed consent was obtained from legal guardians, and assent was obtained from children. Participants were recruited using advertisements, postings, fliers, and referrals from health and mental health professionals. Children and parents completed two separate three hour assessments during which children worked with a trained graduate student to complete measures of IQ, academic achievement, information processing abilities, and emotional processing skills, and parents worked with a Ph.D. clinician to complete structured and semi-structured interviews about their child. Rating scales were also completed by parents and teachers. Diagnoses were assigned using all available information (parent and teacher ratings, parent interview) and following criteria specified in the DSM-IV-TR (American Psychiatric Association, 2000).
Treatment.
Treatment was implemented in a STP, which is a manualized treatment for disruptive child behavior that has been incorporated into numerous clinical trials and is in the national registry of evidence-based programs (Pelham et al., 2017). Treatment was delivered as children participated in activities typical of summer school and summer sports camps, including two academic classes and an art class, three recreational activities (softball, soccer, and basketball), lunch, and recess. Children attended treatment for eight weeks (Monday through Friday) from 8:00 AM until 5:00 PM. Children were placed in one of four groups of 12 children, with groups formed by age, and they stayed in these groups throughout treatment. A clinical supervisor, graduate student lead counselor, five undergraduate counselors, a teacher, and a teacher aide implemented the treatments. Standard rules were reviewed at the beginning of each activity. Counselors evaluated and recorded operationally defined positive and negative behaviors displayed by children in real time. Parents attended weekly two-hour parent education groups to learn behavioral techniques for managing their child’s behavior (Cunningham, Davis, Bremner, Dunn, & Rzasa, 1993).
Within this context, two treatments were implemented: MBT, which was a reward-emphasized, punishment-deemphasized intervention designed to match the learning style of children with high CU, and SBT, which was the treatment as usual condition (see Table 1 and online supplement for details). MBT and SBT were delivered using a within-person design; all participants received one treatment for the first four weeks and the other treatment for the last four weeks. A within-person design provided a test of the modified treatment relative to the standard of care (rather than comparing it to an inert treatment condition) which is a more rigorous and ecologically valid standard of comparison (Weisz et al., 2017). A within-person design also provided a more powerful test of the primary contrast of interest (SBT vs. MBT) and ensured that treatment comparisons were not influenced by inter-individual differences (age, sex, etc.). Treatment was delivered at the group level, with order of treatment (standard treatment first vs. modified treatment first) randomly assigned and counterbalanced across groups. Treatments were implemented Monday through Thursday, with Friday activities dependent on the child’s weekly behavior (special events, normal day, or chores). Fidelity of treatment was measured using observations conducted by the supervising clinicians. Approximately 8 hours of treatment fidelity observations (once per week) were completed, with observations sampled across treatment activities and groups. Supervisors rated the overall quality of implementation using seven point Likert ratings that ranged from 1 (“high quality”) to 7 (“low quality”). The overall quality of treatment implementation was high (M = 2.37, SD = 0.77).
Independent Measures
Table 2 summarizes means, standard deviations, and reliability estimates for independent and dependent measures. Correlations between measures are in an online supplement.
Table 2.
Descriptive Statistics for Measures
| Baseline |
SBT |
MBT |
Rel |
||||
|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | ||
| Independent Variables | |||||||
| Callous-Unemotionala | 48.30 | 9.78 | -- | -- | -- | -- | .84 |
| Conduct Problemsb | 1.18 | 0.36 | -- | -- | -- | -- | .86 |
| ADHDb | 2.58 | 0.35 | -- | -- | -- | -- | .83 |
| Dependent Variables | |||||||
| Noncompliancec | -- | -- | 5.15 | 6.19 | 4.95 | 4.37 | .60 |
| Rule Violationsc | -- | -- | 59.34 | 54.68 | 57.66 | 37.73 | .86 |
| Interruptionsc | -- | -- | 26.29 | 26.05 | 24.08 | 14.48 | .86 |
| Complainingc | -- | -- | 6.63 | 9.55 | 8.18 | 9.00 | .98 |
| Conduct Problemsc | -- | -- | 2.78 | 7.40 | 3.10 | 5.66 | .72 |
| Negative Verbalsc | -- | -- | 14.19 | 15.81 | 15.08 | 12.97 | .75 |
| Positive Peer Behaviorsc | -- | -- | 8.26 | 4.90 | 8.85 | 3.21 | .74 |
| Inatt-Impulse-Overactd | -- | -- | 6.83 | 3.12 | 6.09 | 2.74 | .80 |
| Oppositional-Defiantd | -- | -- | 6.87 | 3.75 | 5.69 | 2.95 | .89 |
| Problem Ratingse | 2.95 | 1.14 | 2.66 | 0.96 | .98 | ||
| Callous-Unemotionala | 33.30 | 12.83 | 28.40 | 9.80 | 28.63 | 8.30 | .87 |
| Conduct Problemsb | 0.87 | 0.39 | 0.61 | 0.35 | 0.63 | 0.32 | .81 |
| ADHDb | 2.15 | 0.56 | 1.59 | 0.62 | 1.66 | 0.60 | .89 |
| Impairmentf | 4.68 | 0.87 | 3.85 | 1.44 | 3.79 | 1.38 | .91 |
| Improvementg | -- | -- | 4.91 | 0.73 | 4.89 | 0.68 | .96 |
| Satisfactionh | -- | -- | 2.23 | 0.73 | 2.37 | 0.59 | .78 |
Notes: Independent variables were parent and teacher combined ratings completed before treatment. Dependent variables were point system frequency counts during treatment or parent ratings completed before, during, and/or after treatment. Baseline = pre-treatment. SBT = standard behavior therapy. MBT = modified behavior therapy. Rel = Reliability coefficients, which were inter-rater reliabilities (estimated using Itraclass Correlation Coefficients) for point system measures and internal consistencies (estimated using Cronbach’s alpha) for all other measures.
= Inventory of Callous-Unemotional Traits (Frick, 2004);
= Disruptive Behavior Disorders Rating Scale (Pelham, Gnagy, et al., 1992);
= point system frequency counts as defined in the Summer Treatment Program manual (Pelham, Greiner, & Gnagy, 1998).
= IOWA Conners (Waschbusch & Willoughby, 2008).
= Problem Rating Form (Waschbusch et al., 2013).
= Impairment Rating Scale (Fabiano et al., 2006);
= Improvement Rating Scale (Pelham et al., 2000).
= Parent Treatment Satisfaction Ratings (Pelham et al., 2000).
Inventory of Callous Unemotional Traits (ICU).
The ICU is a 24 item scale that measures callous-unemotional traits using 0 (“not at all true”) to 3 (“definitely true”) Likert scales (Frick, 2004). The reliability and validity of the ICU has been supported in previous research (Kimonis et al., 2008; Ray & Frick, 2018). Ratings were completed before treatment and parent and teacher ratings were combined by taking a max score item-by-item after reverse scoring relevant items. Items were summed to compute a CU score.
Disruptive Behavior Disorder Rating Scale (DBDRS).
The DBDRS is a 45 item scale that measures symptoms of ADHD, ODD and CD using 0 (“not at all”) to 3 (“very much”) Likert scales (Pelham, Gnagy, Greenslade, & Milich, 1992). The reliability and validity of the DBDRS has been supported (Pelham, Evans, Gnagy, & Greenslade, 1992; Pelham, Gnagy, et al., 1992; Wright, Waschbusch, & Frankland, 2007). Ratings were completed before treatment and parent and teacher ratings were combined by taking a max score item-by-item. Inattentive, hyperactive, and impulsive symptoms were averaged to compute an ADHD score and ODD and CD symptoms were averaged to compute a conduct problems (CP) score.
Dependent Measures
Point system behaviors.
Indices of peer-and staff-directed social behavior were frequency counts derived from the STP point system observation code. Consistent with many previous studies (e.g., Pelham et al., 2014), the following behavioral categories were derived from this system: (1) noncompliance; (2) rule violations; (3) interrupting; (4) complaining; (5) conduct problems (lying, stealing, intentional destruction of property, and intentional aggression); (6) negative verbalizations (verbal abuse to staff, teasing peers, and swearing); and (7) positive peer behavior (helping, sharing, ignoring peer provocation).
Weekly Ratings.
At the end of each week parents completed the IOWA Conners Rating Scale (Loney & Milich, 1982; Pelham, Milich, Murphy, & Murphy, 1989) and the Problem Rating Form (Waschbusch, Coles, & Pelham 2013). The IOWA consists of five items to measure inattentive-impulsive-overactive (IO) behaviors and five items to measure oppositional-defiant (OD) behaviors. Item are rated using 0 (not at all) to 3 (very much) Likert scales and summed to compute scores. The reliability, validity, and sensitivity to treatment has been supported (Pelham et al., 2002; Waschbusch & Willoughby, 2008). The Problem Rating Form is a 42 item measure of problems in daily functioning, including peer relationships, defiance, academics, responsibility, self-esteem, problem solving, sport skills, and overall adjustment. Items are evaluated using 1 (not a problem) to 7 (serious problem) Likert scales. The first 39 items study were averaged to compute an overall score.1
End of treatment ratings.
At baseline and after each treatment condition parents completed the DBDRS and the ICU (described earlier) as well as the Impairment Rating Scale, the Improvement Rating Scale, and Parent Satisfaction Ratings. The Impairment Rating Scale measures impairment in getting along with peers, siblings, and parents, academic and classroom functioning, functioning in the family, self-esteem, and overall adjustment (Fabiano et al., 2006). Items are evaluated using a visual analogue scale anchored on the low end by “No Problem, No need for treatment or services” and on the high end by “Extreme Problem, Definitely needs treatment or services”. Items were scored using a 0 to 6 metric and averaged into an overall impairment score. The reliability, validity, and sensitivity to treatment of this measure has been well supported (Fabiano & Pelham, 2009; Pelham et al., 2016). The Improvement Rating Scale (Pelham et al., 2000) consists of 42 items that assess response to treatment in numerous areas, including peer relationships, defiance, academics, responsibility, self-esteem, problem solving, sport skills, and overall adjustment (sample items include “Following home rules” and “Adult directed defiance/noncompliance”). The first 39 items are rated using a 1 (very much worse) to 7 (very much better) Likert scale, with 4 (no change) as the mid-point. Parents could also indicate “no problem” for any item that was not a problem before treatment. Items rated as “no problem” were excluded from analyses and remaining items were averaged into an overall score. The Parent Satisfaction Ratings consists of seven items, including three used in this study: “How much did your child benefit from this treatment?” “How much did you benefit from this treatment?” and “How much did your child enjoy this treatment?”. These items were rated using a 0 (not at all) to 3 (very much) Likert scale. Items were averaged into an overall satisfaction score. The reliability, validity, and sensitivity to treatment of these measures have been supported (Haas et al., 2011; Pelham et al., 2000),
Analytic Plan
Effects of treatment were examined using mixed models (computed using SPSS version 25) with random intercepts and using full information maximum likelihood procedures to account for missing data (Enders, 2013). Restricted maximum likelihood estimation was used to avoid underestimated variance components and biased parameters (Hedeker & Gibbons, 2006; Singer & Willet, 2003). Consistent with the primary purpose of the study, which was to evaluate whether CU was associated with treatment within a sample of children with CP, the primary independent variables of interest were CU, Treatment (SBT = 0, MBT = 1), and their interaction. CU was included as a continuous measure because it was normally distributed in the sample (see normality tests and histogram in online supplement) and because continuous predictors are typically more statistically powerful than categorical predictors (Altman & Royston, 2006). Medication (0 = no, 1 = yes), ADHD, and CP were included as covariates, with ADHD and CP as continuous measures. For end of treatment child behavior ratings, baseline ratings were included as a level within Treatment (Baseline = 0, SBT = 1, MBT = 2). Nonsignificant interactions were trimmed from final models. Significant interactions were followed up by testing simple slopes of Treatment at CU scores of 33 (Low CU) and 60 (high CU) on the ICU, which represent the lower and upper 10% (respectively) of the sample distribution.2 Parameter estimates and standardized mean difference effect sizes are summarized in Tables 3 and 4.
Table 3.
Parameter Estimates and Treatment Effect Sizes for Point System Data, Weekly Parent Ratings and End of Treatment Parent Ratings
| Fixed effects estimates |
Effect Sizes | |||||||
|---|---|---|---|---|---|---|---|---|
| Measure | Intercept | Med | ADHD | CP | CU | Treatment | Treatment*CU | |
| Point Systema | ||||||||
| Noncompliance | 1.49* | 0.17 | 0.08 | 0.39 | −0.01 | 0.06 | 0.01* | 0.13 |
| Rule Violations | 2.68* | 0.06 | 0.18 | 0.15 | −0.01 | −0.03 | 0.01* | 0.06 |
| Interruptions | 2.10* | −0.02 | 0.24 | 0.27 | −0.02 | 0.03 | -- | 0.06 |
| Complaining | 1.58* | 0.12 | 0.05 | 0.56* | −0.02* | 0.07 | -- | 0.15 |
| Conduct Problems | 1.22* | 0.17 | 0.07 | 0.43* | −0.01 | 0.12* | -- | 0.25 |
| Negative Verbalizations | 1.84* | 0.03 | 0.01 | 0.47* | −0.01 | 0.08 | 0.01* | 0.17 |
| Positive Peer Behaviors | 1.68* | −0.04 | 0.04 | 0.04 | −0.001 | 0.06 | -- | 0.31 |
| Weekly Ratings | ||||||||
| Inatt-Impulsive-Overactb | 7.11* | 1.29 | 2.76* | −1.06 | 0.02 | −0.50 | -- | −0.17 |
| Oppositional-Defiantb | 7.06* | 1.62 | 0.20 | 1.19 | −0.01 | −1.04* | -- | −0.30 |
| Problem Rating Formc | 2.90* | 0.28 | 0.32 | 0.48 | 0.003 | −0.26* | -- | −0.25 |
| End of Treatment | ||||||||
| Improvementd | 4.66* | −0.28 | −0.19 | 0.06 | −0.008 | −0.03 | -- | −0.04 |
| Treatment Satisfactione | 2.21* | −0.18 | 0.41 | 0.17 | −0.01 | 0.14 | -- | 0.22 |
Notes: SBT = standard behavior therapy. MBT = modified behavior therapy. Med = medication main effect (0 = no medication, 1 = medication). ADHD = ADHD main effect. CP = conduct problem main effect. CU = CU main effect, Treatment = treatment main effect (SBT = 0, MBT = 1). Treatment*CU = Treatment by CU interaction.
= Summer Treatment Program point system (Pelham et al., 1998).
= IOWA Conners (Loney & Milich, 1982).
= Problem Rating Form (Waschbusch et al., 2013).
= Improvement Rating Scale (Pelham et al., 2000).
= Parent Treatment Satisfaction Ratings (Pelham et al., 2000).
Effect sizes are standardized mean differences computed as: (MMBT - MSBT) / Overall SD.
= p < .05
Table 4.
Parameter Estimates and Treatment Effect Sizes for Parent Ratings Completed Pre-Treatment and Post-Treatment
| Fixed effects estimates |
Effect Sizes |
||||||
|---|---|---|---|---|---|---|---|
| |
Intercept | Med | Treatment |
Base vs. SBT | Base vs. MBT | MBT vs SBT | |
| Measure | Base vs. SBT | Base vs. MBT | |||||
| Callous-Unemotionala | 35.47* | 2.84 | −4.72* | −4.21* | 0.44 | 0.39 | 0.05 |
| Conduct Problemsb | 0.88* | 0.01 | −0.25* | −0.23* | 0.67 | 0.62 | 0.05 |
| ADHDb | 2.19* | 0.06 | −0.55* | −0.47* | 0.86 | 0.74 | 0.12 |
| Impairmentc | 4.88* | 0.26 | −0.84* | −0.88* | 0.64 | 0.67 | −0.04 |
Notes: Base = baseline (pre-treatment). SBT = standard behavior therapy. MBT = modified behavior therapy. Med = medication main effect (0 = no medication, 1 = medication). Treatment = treatment main effect (Baseline = 0, SBT = 1, MBT = 2).
= Inventory of Callous-Unemotional Traits (Frick, 2004).
= Disruptive Behavior Disorders Rating Scale (Pelham, Gnagy, et al., 1992).
= Impairment Rating Scale (Fabiano et al., 2006).
Effect sizes are standard mean differences computed as follows:
Base – SBT = (MBaseline – MSBT) / Overall SD.
Base – MBT = (MBaseline – MMBT) / Overall SD.
MBT – SBT = (MMBT – MSBT) / Overall SD.
= p < .05
Results
Point System Behaviors
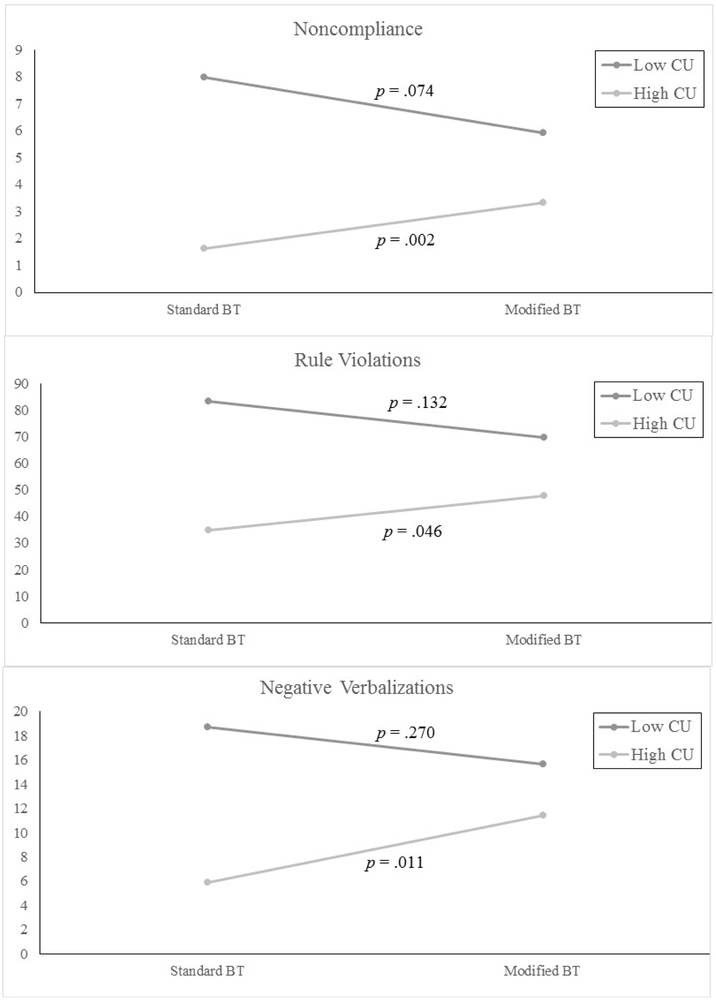
As in past studies (Pelham et al., 2014) fourth-root transformations were applied to point system behaviors to normalize their distributions prior to analyses. There were significant main effects of CP on complaining, conduct problems, and negative verbalizations (see Table 3), with higher CP associated with worse levels of these behaviors. There was a significant main effect of CU on complaining, with higher CU associated with less complaining. There was a significant main effect of Treatment for CP, which showed that children had more conduct problems in MBT than SBT. Finally, there were significant Treatment*CU interactions for noncompliance, rule violations, and negative verbalizations (see Figure 1). Simple slopes tests of Treatment at low and high values of CU showed that MBT versus SBT did not differ at low CU but children had more noncompliance, rule violations, and negative verbalizations in MBT than SBT at high CU.
Figure 1.
Noncompliance (top), rule violations (middle), and negative verbalizations (bottom) as a function of Treatment (standard behavioral treatment vs. modified behavioral treatment) and pre-treatment level of callousness (CU).
Weekly Ratings
There were significant main effects of Treatment for oppositional-defiant behavior and problems in functioning (see Table 3). Examination of means (see Table 2) and effect sizes (see Table 3) showed that children had higher parent rated oppositional-defiant behavior and more problems in functioning in SBT than in MBT.
End of Treatment Ratings
There were no significant effects for parent end of treatment ratings of improvement or treatment satisfaction (see Table 3), with both SBT and MBT rated somewhat improved and with satisfaction rated between much and very much (see Table 2). Parent ratings of CU, CP, ADHD and impairment were collected before treatment as well after SBT and after MBT so analyses of these measures included baseline as part of the Treatment effect (Basline = 0, SBT = 1, MBT = 2). Only Medication and Treatment were included in these models to avoid predictor-outcome contamination. There were significant main effects of Treatment for each measure (see Table 4). Means, post-hoc tests, and effect sizes (see Tables 2 and 4) showed children improved significantly between baseline and SBT and between baseline and MBT, but SBT did not differ from MBT.
After both treatments were complete, parents were asked to select whether their child responded best to the first or second half of the STP, and these responses were coded into treatment conditions (SBT = 0, MBT = 1). Parents selected MBT as the optimal treatment for 60% of children, but pre-treatment CU was not associated treatment choice (r = −.14, p = .380). Likewise, after both treatments were complete each group of counselors discussed each child’s treatment response considering their own observations and data collected during treatment. These discussion were led by the lead counselor. After approximately five minutes of discussion each child was placed into one of four treatment outcome groups based on group consensus: (1) SBT best treatment; (2) MBT best treatment; (3) responded well to both SBT and MBT; or (4) did not respond well to either treatment. Of the 45 children who completed treatment, 26.7% were classified as optimal responders to SBT, 22.2% were optimal responders to MBT, 35.6% responded equally well to both treatments, and 15.6% did not respond to either treatment. These categories were recoded into two variables: (1) recommend SBT (0 = no, 1 = yes) and (2) recommend MBT (0 = no, 1 = yes). Higher pre-treatment CU was significantly associated with counselors recommending SBT (r = .35, p = .019) but not MBT (r = −.20, p = .191).
Discussion
The purpose of this study was to take a first step toward developing personalized treatment for youth with CPCU by modifying behavioral treatment to match the reward-driven, punishment-insensitive learning style that seems to characterize them in at least some research (Byrd et al., 2013). Toward this goal, a modified behavioral treatment (MBT) was developed (based on pilot research) that emphasized rewards and de-emphasized punishments and this was compared to standard behavioral treatment (SBT) that balanced rewards and punishments and is considered an empirically supported treatment for CP. These treatments were implemented with a diverse sample of elementary school age children with ODD and (or many) CD, most of whom were Caucasian and Hispanic, reflecting the community from which they were recruited. It was hypothesized that, within a sample of youth with CP, higher levels of CU would be associated with a more positive response to MBT relative to SBT.
Overall, results provided mixed support for the hypothesis. Arguing against the hypothesis was data from the point system. On three of the seven point system measures (interrupting, complaining, and positive peer behaviors) SBT and MBT did not differ and on the other four point system measures (noncompliance, rule violations, negative verbalizations, conduct problems) MBT was worse than SBT for at least some participants (see Tables 2 and 3 and Figure 1). Also, SBT and MBT did not differ on parent end of treatment ratings of improvement, satisfaction, CU, CP, ADHD, or impairment (see Table 4). In contrast to these findings, however, parent weekly ratings of oppositional-defiant behavior and overall problems were significantly lower during MBT than SBT (see Tables 2 and 3). Global judgements about the treatments also showed a mixed pattern, with similar rates of children showing an optimal response to MBT as compared to SBT, with treatment response judged by parents and counselors. The mixed findings with respect to MBT versus SBT should be interpreted in light of evidence that both treatments were effective. Parent ratings showed significant and moderate to large reductions from before treatment to after treatment for both MBT and SBT (see Table 4), and at the end of treatment counselors judged about 85% of children as having responded positively to at least one treatment. Thus, the results were mixed with respect to whether MBT was superior to SBT, but both were apparently effective.
The pattern of mixed findings regarding the relative value of MBT versus SBT mirrors the larger literature on whether children with CPCU differentially respond to reward-emphasized, punishment-deemphasized treatments. Some studies provide evidence in support of this approach to treating youth with CU (Datyner et al., 2015; Kimonis & Armstrong, 2012; Kimonis et al., 2018; Miller et al., 2014), but other studies suggest reward and punishment sensitivity is not associated with treatment response in youth with CU (Byrd et al., 2018; Ortiz et al., 2018). Of special note, a randomized controlled trial found that parent training in behavior management was generally effective at reducing CP in youth, but treatment response did not differ as a function of CU traits nor was CU differentially influenced by reward versus punishment strategies (Ortiz et al., 2018). It’s worth mentioning that the supportive studies had sample sizes that ranged from 1 to 23, whereas the two studies that failed to support the differential treatment effects of reward and punishment had sample sizes of 64 and 74.
Taken as a whole, the results of our study as well as previous studies seem to indicate that increasing reward and decreasing punishment as a means of personalizing behavioral treatment for youth with CPCU has, at best, inconsistent effects. There are two implications of this tentative conclusion. First, and most obvious, more research is needed to understand these mixed findings. Paraphrasing Paul’s (1967) famous quote, it is time to move beyond questions of whether behavior therapy is effective for children with CPCU and begin to address what type of behavior therapy works for which subset of children and under what conditions. For example, this study reduced both the magnitude and likelihood of punishment during treatment, yet there is evidence that reducing the magnitude of punishment while increasing its likelihood may be a better approach (Waschbusch et al., 2016). This echoes recommendations for deterring crime: “The deterrent impact of punishment depends only weakly on its severity, but strongly on its swiftness and certainty” (Kleiman, 2010). Whether this advice applies to and benefits youth with CPCU has not been directly studied. Relatedly, an assumption of this and most or all other studies on this topic is that measures of CU are adequate for identifying which youth show a differential response to reward and punishment techniques. There is some evidence to support this assumption (Byrd et al., 2013), but it is worth pointing out that measures of CU don’t directly assess children’s response to reward and punishment. It may be that directly measuring how children with CPCU respond to rewards and punishments is more useful for personalizing behavior therapy for them.
Second, the mixed findings in response to treatment in this study suggest that manipulating aspects of behavior therapy may not provide sufficient treatment for youth with CPCU. Instead, it may be necessary to develop and implement treatments that can be used as adjuncts to behavior therapy. Possible targets of adjunctive treatments include the emotional (Blair, Leibenluft, & Pine, 2014), motivational (Salekin, 2010), interpersonal (Pasalich, Dadds, Hawes, & Brennan, 2012; Pasalich, Waschbusch, Dadds, & Hawes, 2014), or information processing (Baskin-Sommers, Waller, Fish, & Hyde, 2015; Waller, Hyde, Baskin-Sommers, & Olson, 2017) deficits associated with CU. Recent studies have begun to investigate this approach, with some but not all studies finding positive effects (Dadds, Cauchi, Wimalaweera, Hawes, & Brennan, 2012; Dadds, English, Wimalaweera, Schollar-Root, & Hawes, 2019; Datyner et al., 2015; Kimonis et al., 2018; Salekin, Tippey, & Allen, 2012). Medication treatment may also be a useful adjunct to behavioral treatment of children with CU traits (Blader et al., 2013; Waschbusch, Carrey, Willoughby, King, & Andrade, 2007).
Several other points about this study are also worth making. First, it was surprising that pre-treatment ratings of CU were generally not associated with measures of antisocial behavior during or after treatment (see Table 3 and online supplement). This runs counter to several other studies, including studies conducted in STP settings (Graziano et al., 2015; Waschbusch et al., 2007). Furthermore, higher CU was associated with less negative behavior in standard behavior therapy for some measures (see Figure 1), which also runs counter to previous studies (see Frick et al., 2014; Hawes et al., 2014; Wilkinson et al., 2016 for reviews). It is not clear what explains these surprising findings, but the fact that there was a somewhat restricted range for CU in this sample may be implicated. Although the CU score used in analyses was normally distributed (see online supplement), the entire distribution was shifted to the right relative to the general population. This is apparent by comparing the CU scores in the present study to the same scores from a large sample of adolescents (Docherty et al., 2017) using one-sample t-tests. These comparisons show that the average parent-teacher CU score in the present study (48.30) was significantly higher (p < .001) than the same score in a community sample of adolescents (which had an average parent-teacher CU score of 30.60) and higher than in adolescent delinquents (which had an average parent-teacher CU mean score of 41.64). Most children in this sample also exceed cutoffs for identifying high CU, with rates of high CU in this sample varying from 73.9% to 100% depending on which informant ratings are used and which proposed cutoffs are applied (Docherty et al., 2017; Kimonis, Fanti, & Singh, 2014). As such, the sample used in this study largely consisted of children with high CU relative to the general population. Findings regarding the CU scores may have changed had children with lower levels of CU been included.
Second, the fact that both counselor and parent ratings showed similar rates of optimal response to SBT versus MBT illustrates an important point: even among a sample of children who were selected to be relatively homogeneous (all had ADHD and ODD and most had high CU), there was large variance in response to treatment. We are far from the first to note that children with CP vary in their response to treatment, but it is nonetheless an important point because attending to individual differences when delivering treatment is likely to be a critical determinant of whether children with CPCU show a positive treatment response. Indeed, one consistent feature across published studies that have reported positive treatment effects with samples of children with CPCU is they each used less prescriptive and more individualized, adaptive treatments (Hyde et al., 2013; Kimonis et al., 2018; Kolko & Pardini, 2010; White, Frick, Lawing, & Bauer, 2012). The effectiveness of treating children with CPCU could be accelerated by incorporating methods for quantifying individual differences into analyses of treatment response (Ridenour, Wittenborn, Raiff, Benedict, & Kane-Gill, 2016).
The findings of this study must be considered in light of several limitations. First, the study had a modest sample size. Small to modest samples are common in treatment studies, especially when testing novel treatments and in studies of seriously antisocial children who require intensive (and costly) treatment and staffing. The modest sample size was partly accommodated by using a within-subjects design, but the results should be considered preliminary. Second, the modest sample size precluded examination of moderators. It may be that the results differ as a function of demographic or other characteristics such as anxiety, history of trauma, or both, given that they have been shown to moderate CU (Humayun, Kahn, Frick, & Viding, 2014; Kimonis, Fanti, Goulter, & Hall, 2017). Third, staff members were necessarily aware of the two treatment conditions and it is possible that this knowledge influenced results. However, the point system behaviors were operationally defined and implemented with reliability and validity suggesting bias was not a major factor. Fourth, the treatments included not only behavior therapy, but also social skills (in SBT) or emotional skills (in MBT) interventions. Other adjunctive treatment components were also used in MBT (see online supplement for description and rationale). The impact of these components cannot be separated from the behavior therapy manipulations. Results should be interpreted as effects of behavior therapy plus these adjuncts.
These limitations are balanced by noteworthy strengths. First, the study relied on a translational research strategy that has been suggested as a key to advancing knowledge of psychopathology and treatment (Cuthbert, 2014). Second, the study included a treatment as usual condition, which is rare in studies of youth with CU traits (Reidy, Kearns, & DeGue, 2013). Third, the study enrolled a clinically important sample who had severe and impairing behavior problems that were apparent during treatment. For example, during one week of treatment the most extreme child averaged four hours per day in Time Out due to intentional aggression (directed exclusively at counselors) and 22 minutes per day being physically managed to prevent dangerous behaviors. Fourth the point system represents 288 hours of observed child behavior. Fifth, the multi-measure approach aligns with recommendations for optimally evaluating youth mental health treatments (Bakker, Greven, Buitelaar, & Glennon, 2017; Weisz et al., 2017). Sixth, treatment was delivered in an ecologically valid setting, making the results (arguably) directly applicable to “real life” settings of children.
Finally, it is important emphasize that we do not mean to downplay the crucial role of behavior therapy in treatment. Effective behavior therapy will almost certainly be a necessary part of treatment for any child with CP; if misbehavior can’t be managed, then focusing on other deficits is not likely to be effective or even possible. Yet even if behavior can be managed with behavior therapy, additional treatment approaches may be needed to address deficits associated with CPCU that are not directly targeted by behavior therapy. Research that develops and evaluates these new treatments should continue to be a high priority.
Supplementary Material
Footnotes
For this measure, as well as for the Improvement Rating Scale and the Parent Satisfaction Ratings, other items were not used because they are evaluated with different Likert scales and anchors.
The value selected to represent low CU in this sample (33) approximates the average CU score (31) of typically developing adolescents in a recent study (Docherty, Boxer, Huesmann, O'Brien, & Bushman, 2017).
Contributor Information
Daniel A. Waschbusch, Penn State Health Milton S Hershey Medical Center - Department of Psychiatry, 500 University Drive, Hershey, Pennsylvania 17033
Michael T. Willoughby, RTI International, Research Triangle Park, North Carolina 27709-2194
Sarah M. Haas, Penn State Health Milton S Hershey Medical Center - Psychiatry, Hershey, Pennsylvania 17033-0850
Ty Ridenour, RTI International, Research Triangle Park, North Carolina 27709-2194.
Sarah Helseth, Florida International University, Department of Psychology and the Center for Children and Families, Miami, Florida 33199-2156.
Kathleen I. Crum, Florida International University, Department of Psychology and the Center for Children and Families, Miami, Florida 33199-2156
Amy R. Altszuler, Florida International University, Department of Psychology and the Center for Children and Families, Miami, Florida 33199-2156
J. Megan Ross, Florida International University, Department of Psychology and the Center for Children and Families, Miami, Florida 33199-2156.
Erika K. Coles, Florida International University, Department of Psychology and the Center for Children and Families, Miami, Florida 33199-2156
William E. Pelham, Jr, Florida International University, Department of Psychology and the Center for Children and Families, Miami, Florida 33199-2156.
References
- Altman DG, & Royston P (2006). The cost of dichotomising continuous variables. BMJ, 332(7549), 1080. doi: 10.1136/bmj.332.7549.1080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th text revision ed.). Washington, DC: American Psychiatric Association. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Association. [Google Scholar]
- Bakker MJ, Greven CU, Buitelaar JK, & Glennon JC (2017). Practitioner Review: Psychological treatments for children and adolescents with conduct disorder problems–a systematic review and meta‐analysis. Journal of Child Psychology and Psychiatry and Allied Disciplines, 58(1), 4–18. doi: 10.1111/jcpp.12590 [DOI] [PubMed] [Google Scholar]
- Baskin-Sommers AR, Waller R, Fish AM, & Hyde LW (2015). Callous-unemotional traits trajectories interact with earlier conduct problems and executive control to predict violence and substance use among high risk male adolescents. Journal of Abnormal Child Psychology. Advance online publication. doi: 10.1007/s10802-015-0041-8 [DOI] [PubMed] [Google Scholar]
- Blader JC, Pliszka SR, Kafantaris V, Foley CA, Crowell JA, Carlson GA, . . . Daviss WB (2013). Callous-unemotional traits, proactive aggression, and treatment outcomes of aggressive children with attention-deficit/hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 52(12), 1281–1293. doi: 10.1016/j.jaac.2013.08.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blair RJR, Leibenluft E, & Pine DS (2014). Conduct disorder and callous-unemotional traits in youth. New England Journal of Medicine, 371(23), 2207–2216. doi: 10.1056/NEJMra1315612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blair RJR, Peschardt KS, Budhani S, Mitchell DGV, & Pine DS (2006). The development of psychopathy. Journal of Child Psychology and Psychiatry, 47(3–4), 262–275. doi: 10.1111/j.1469-7610.2006.01596.x [DOI] [PubMed] [Google Scholar]
- Budhani S, & Blair RJR (2005). Response reversal and children with psychopathic tendencies: Success is a function of salience of contingency change. Journal of Child Psychology and Psychiatry, 46(9), 972–981. doi: 10.1111/j.1469-7610.2004.00398.x [DOI] [PubMed] [Google Scholar]
- Byrd AL, Hawes SW, Burke JD, Loeber R, & Pardini DA (2018). Boys with conduct problems and callous-unemotional traits: Neural response to reward and punishment and associations with treatment response. Developmental Cognitive Neuroscience, 30, 51–59. doi: 10.1016/j.dcn.2017.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrd AL, Loeber R, & Pardini DA (2013). Antisocial behavior, psychopathic features and abnormalities in reward and punishment processing in youth. Clinical Child and Family Psychology Review, 17(2), 125–156. doi: 10.1007/s10567-013-0159-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caldwell MF (2011). Treatment-related changes in behavioral outcomes of psychopathy facets in adolescent offenders. Law and Human Behavior, 35(4), 275–287. doi: 10.1007/s10979-010-9239-z [DOI] [PubMed] [Google Scholar]
- Caldwell MF, Skeem JL, Salekin RT, & Van Rybroek GJ (2006). Treatment response of adolescent offenders with psychopathy features: A 2-year follow up. Criminal Justice and Behavior, 33(5), 571–596. [Google Scholar]
- Caldwell MF, & Van Rybroek GJ (2005). Reducing violence in serious juvenile offenders using intensive treatment. International Journal of Law and Psychiatry, 28(6), 622–636. doi: 10.1016/j.ijlp.2004.07.001 [DOI] [PubMed] [Google Scholar]
- Conduct Problems Prevention Research Group. (1992). A developmental and clinical model for the prevention of conduct disorder: The FAST Track Program. Development and Psychopathology, 4(4), 509–527. doi: 10.1017/S0954579400004855 [DOI] [Google Scholar]
- Cunningham CE, Davis JR, Bremner R, Dunn KW, & Rzasa T (1993). Coping modeling problems solving versus master modeling: Effects on adherence, in-session process, and skill acquisition in a residential treatment parent-training program. Journal of Consulting and Clinical Psychology, 61(5), 871–877. [DOI] [PubMed] [Google Scholar]
- Cuthbert BN (2014). Keeping an open attitude towards the RDoC project. World Psychiatry, 13(1), 28–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dadds MR, Cauchi AJ, Wimalaweera S, Hawes DJ, & Brennan J (2012). Outcomes, moderators, and mediators of empathic-emotion recognition training for complex conduct problems in childhood. Psychiatry Research, 199(3), 201–207. doi: 10.1016/j.psychres.2012.04.033 [DOI] [PubMed] [Google Scholar]
- Dadds MR, English T, Wimalaweera S, Schollar-Root O, & Hawes DJ (2019). Can reciprocated parent-child eye gaze and emotional engagement enhance treatment for children with conduct problems and callous-unemotional traits: a proof-of-concept trial. Journal of Child Psychology and Psychiatry and Allied Disciplines. doi: 10.1111/jcpp.13023 [DOI] [PubMed] [Google Scholar]
- Dadds MR, & Salmon K (2003). Punishment insensitivity and parenting: Temperament and learning as interacting risks for antisocial behavior. Clinical Child and Family Psychology Review, 6(2), 69–86. doi: 10.1023/a:1023762009877 [DOI] [PubMed] [Google Scholar]
- Datyner A, Kimonis ER, Hunt E, & Armstrong K (2015). Using a novel emotional skills module to enhance empathic responding for a child with conduct disorder and limited prosocial emotions. Clinical Case Studies. Advance online publication. doi: 10.1177/1534650115588978 [DOI] [Google Scholar]
- Docherty M, Boxer P, Huesmann LR, O’Brien M, & Bushman B (2017). Assessing callous-unemotional traits in adolescents: Determining cutoff scores for the inventory of callous and unemotional traits. Journal of Clinical Psychology, 73(3), 257–278. doi: 10.1002/jclp.22313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enders CK (2013). Dealing with missing data in developmental research. Child Development Perspectives, 7(1), 27–31. doi: 10.1111/cdep.12008 [DOI] [Google Scholar]
- Fabiano GA, & Pelham WE Jr. (2009). Impairment in Children In Naglieri J & Goldstein S (Eds.), Assessing Impairment: From Theory to Practice (pp. 105–119). Boston, MA: Springer US. [Google Scholar]
- Fabiano GA, Pelham WE Jr., Waschbusch DA, Gnagy EM, Lahey BB, Chronis AM, . . . Burrows-MacLean L (2006). A practical impairment measure: Psychometric properties of the Impairment Rating Scale in samples of children with attention-deficit/hyperactivity disorder and two school-based samples. Journal of Clinical Child and Adolescent Psychology, 35(3), 369–385. doi: 10.1207/s15374424jccp3503_3 [DOI] [PubMed] [Google Scholar]
- Finger EC, Marsh AA, Blair KS, Reid ME, Sims C, Ng P, . . . Blair RJR (2011). Disrupted reinforcement signaling in the orbitofrontal cortex and caudate in youths with conduct disorder or oppositional defiant disorder and a high level of psychopathic traits. American Journal of Psychiatry, 168(2), 152–162. doi: 10.1176/appi.ajp.2010.10010129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finger EC, Marsh AA, Mitchell DG, Reid ME, Sims C, Budhani S, . . . Blair JR (2008). Abnormal ventromedial prefrontal cortex function in children with psychopathic traits during reversal learning. Archives of General Psychiatry, 65(5), 586–594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher L, & Blair RJR (1998). Cognitive impairment and its relationship to psychopathic tendencies in children with emotional and behavioral difficulties. Journal of Abnormal Child Psychology, 26(6), 511–519. doi: 10.1023/a:1022655919743 [DOI] [PubMed] [Google Scholar]
- Frick PJ (2004). Inventory of Callous-Unemotional Traits. Retrieved from http://labs.uno.edu/developmental-psychopathology/ICU.html
- Frick PJ, Ray JV, Thornton LC, & Kahn RE (2014). Can callous-unemotional traits enhance the understanding, diagnosis, and treatment of serious conduct problems in children and adolescents? A comprehensive review. Psychological Bulletin, 140(1), 1–57. doi: 10.1037/a0033076 [DOI] [PubMed] [Google Scholar]
- Garcia AM, Graziano PA, & Hart KC (2018). Response to time-out among preschoolers with externalizing behavior problems: The role of callous-unemotional traits. Child Psychiatry and Human Development. Advance online publication. doi: 10.1007/s10578-018-0788-6 [DOI] [PubMed] [Google Scholar]
- Graziano PA, Ros R, Haas S, Hart K, Slavec J, Waschbusch D, & Garcia A (2015). Assessing callous-unemotional traits in preschool children with disruptive behavior problems using peer reports. Journal of Clinical Child and Adolescent Psychology(ahead-of-print), 1–14. [DOI] [PubMed] [Google Scholar]
- Haas SM, Waschbusch DA, Pelham WE Jr., King S, Andrade BF, & Carrey NJ (2011). Treatment response in CP/ADHD children with callous/unemotional traits. Journal of Abnormal Child Psychology, 39(4), 541–552. doi: 10.1007/s10802-010-9480-4 [DOI] [PubMed] [Google Scholar]
- Hawes DJ, & Dadds MR (2005). The treatment of conduct problems in children with callous-unemotional traits. Journal of Consulting and Clinical Psychology, 73(4), 737–741. doi: 10.1037/0022-006x.73.4.737 [DOI] [PubMed] [Google Scholar]
- Hawes DJ, Price MJ, & Dadds MR (2014). Callous-unemotional traits and the treatment of conduct problems in childhood and adolescence: A comprehensive review. Clinical Child and Family Psychology Review, 17(3), 248–267. doi: 10.1007/s10567-014-0167-1 [DOI] [PubMed] [Google Scholar]
- Hecht LK, Latzman RD, & Lilienfeld SO (2018). The psychological treatment of psychopathy: Theory and research In David D, Lynn SJ, & Montgomery GH (Eds.), Evidence-based psychotherapy: The state of science and practice. Hoboken, NJ: Wiley-Blackwell. [Google Scholar]
- Hedeker D, & Gibbons RD (2006). Longitudinal data analysis. Hoboken, NJ: John Wiley & Sons. [Google Scholar]
- Humayun S, Kahn RE, Frick PJ, & Viding E (2014). Callous-unemotional traits and anxiety in a community sample of 7-year-olds. Journal of Clinical Child and Adolescent Psychology, 43(1), 36–42. doi: 10.1080/15374416.2013.814539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyde LW, Shaw DS, Gardner F, Cheong J, Dishion TJ, & Wilson M (2013). Dimensions of callousness in early childhood: Links to problem behavior and family intervention effectiveness. Development and Psychopathology, 25(02), 347–363. doi: 10.1017/S0954579412001101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiehl KA (2014). What it’s like to spend 20 years listening to psychopaths for science. Retrieved from http://www.wired.com/2014/04/psychopath-brains-kiehl/
- Kimonis ER, & Armstrong K (2012). Adapting Parent Child Interaction Therapy to treat severe conduct problems with callous-unemotional traits: A case study. Clinical Case Studies, 11(3), 234–252. doi: 10.1177/1534650112448835 [DOI] [Google Scholar]
- Kimonis ER, Fanti KA, Goulter N, & Hall J (2017). Affective startle potentiation differentiates primary and secondary variants of juvenile psychopathy. Development and Psychopathology, 29(4), 1149–1160. [DOI] [PubMed] [Google Scholar]
- Kimonis ER, Fanti KA, & Singh JP (2014). Establishing cut-off scores for the Parent-Reported Inventory of Callous-Unemotional Traits. Archives of Forensic Psychology, 1(1), 27–48. [Google Scholar]
- Kimonis ER, Fleming G, Briggs N, Brouwer-French L, Frick PJ, Hawes DJ, . . . Dadds M (2018). Parent-Child Interaction Therapy adapted for preschoolers with Callous-Unemotional Traits: An open trial pilot study. Journal of Clinical Child and Adolescent Psychology. Advance online publication. doi: 10.1080/15374416.2018.1479966 [DOI] [PubMed] [Google Scholar]
- Kimonis ER, Frick PJ, Skeem JL, Marsee MA, Cruise K, Munoz LC, . . . Morris, A. S. (2008). Assessing callous-unemotional traits in adolescent offenders: validation of the Inventory of Callous-Unemotional Traits. International Journal of Law and Psychiatry, 31(3), 241–252. doi: 10.1016/j.ijlp.2008.04.002 [DOI] [PubMed] [Google Scholar]
- Kleiman MAR (2010). The outpatient prison: How to lower both the prison population and crime - at the same time. The American Interest, 5(3). http://www.the-american-interest.com/2010/03/01/the-outpatient-prison/ [Google Scholar]
- Kochanska G (1997). Multiple pathways to conscience for children with different temperaments: From toddlerhood to age 5. Developmental Psychology, 33(2), 228–240. [DOI] [PubMed] [Google Scholar]
- Kolko DJ, & Pardini DA (2010). ODD dimensions, ADHD, and callous-unemotional traits as predictors of treatment response in children with disruptive behavior disorders. Journal of Abnormal Psychology, 119(4), 713–725. doi: 10.1037/a0020910 [DOI] [PubMed] [Google Scholar]
- Leijten P, Gardner F, Landau S, Harris V, Mann J, Hutchings J, . . . Scott S (2017). Research Review: Harnessing the power of individual participant data in a meta‐analysis of the benefits and harms of the Incredible Years parenting program. Journal of Child Psychology and Psychiatry. Advance online publication. doi: 10.1111/jcpp.12781 [DOI] [PubMed] [Google Scholar]
- Loeber R, & Farrington DP (2001). The significance of child delinquency In Loeber R & Farrington DP (Eds.), Child delinquents: Development, intervention, and service needs (pp. 1–22). Thousand Oaks, CA: Sage. [Google Scholar]
- Loney J, & Milich R (1982). Hyperactivity, inattention, and aggression in clinical practice In Wolraich M & Routh DK (Eds.), Advances in developmental and behavioral pediatrics (Vol. 3, pp. 113–147). Greenwich, CT: JAI. [Google Scholar]
- Matthys W, Vanderschuren LJ, & Schutter DJ (2013). The neurobiology of oppositional defiant disorder and conduct disorder: Altered functioning in three mental domains. Development and Psychopathology, 25(1), 193–207. doi: 10.1017/S0954579412000272 [DOI] [PubMed] [Google Scholar]
- Miller NV, Haas SM, Waschbusch DA, Willoughby MT, Helseth SA, Crum KI, . . . Pelham WE Jr. (2014). Behavior therapy and callous-unemotional traits: Effects of a pilot study examining modified behavioral contingencies on child behavior. Behavior Therapy, 45(5), 606–618. doi: 10.1016/j.beth.2013.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moffitt TE, Arseneault L, Jaffee SR, Kim-Cohen J, Koenen KC, Odgers CL, . . . Viding E (2008). Research Review: DSM-IV conduct disorder: Research needs for an evidence base. Journal of Child Psychology and Psychiatry, 49(1), 3–33. doi: 10.1111/j.1469-7610.2007.01823.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng MY, & Weisz JR (2016). Annual Research Review: Building a science of personalized intervention for youth mental health. Journal of Child Psychology and Psychiatry and Allied Disciplines, 57(3), 216–236. doi: 10.1111/jcpp.12470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Brien BS, & Frick PJ (1996). Reward dominance: Associations with anxiety, conduct problems, and psychopathy in children. Journal of Abnormal Child Psychology, 24(2), 223–240. doi: 10.1007/bf01441486 [DOI] [PubMed] [Google Scholar]
- Ortiz C, Hawes DJ, Lorber M, Lazer S, & Brotman LM (2018). Are callous-unemotional traits associated with differential response to reward versus punishment components of parent-training? A randomized trial. Evidence-Based Practice in Child and Adolescent Mental Health. doi: 10.1080/23794925.2018.1450689 [DOI] [Google Scholar]
- Pasalich DS, Dadds MR, Hawes DJ, & Brennan J (2012). Attachment and callous-unemotional traits in children with early-onset conduct problems. Journal of Child Psychology and Psychiatry and Allied Disciplines, 53(8), 838–845. doi: 10.1111/j.1469-7610.2012.02544.x [DOI] [PubMed] [Google Scholar]
- Pasalich DS, Waschbusch DA, Dadds MR, & Hawes DJ (2014). Emotion socialization style in parents of children with callous-unemotional traits. Child Psychiatry and Human Development, 45(2), 229–242. doi: 10.1007/s10578-013-0395-5 [DOI] [PubMed] [Google Scholar]
- Paul GL (1967). Strategy of outcome research in psychotherapy. Journal of Consulting Psychology, 31(2), 109–118. doi: 10.1037/h0024436 [DOI] [PubMed] [Google Scholar]
- Pelham WE Jr., Burrows-MacLean L, Gnagy EM, Fabiano GA, Coles EK, Wymbs BT, . . . Waschbusch DA (2014). A dose-ranging study of behavioral and pharmacological treatment in social settings for children with ADHD. Journal of Abnormal Child Psychology, 42(6), 1019–1031. doi: 10.1007/s10802-013-9843-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelham WE Jr., Evans SW, Gnagy EM, & Greenslade KE (1992). Teacher Ratings of Dsm-Iii-R Symptoms for the Disruptive Behavior Disorders - Prevalence, Factor-Analyses, and Conditional Probabilities in a Special-Education Sample. School Psychology Review, 21(2), 285–299. [Google Scholar]
- Pelham WE Jr., Fabiano GA, Waxmonsky JG, Greiner AR, Gnagy EM, Pelham WE 3rd, . . . Murphy SA (2016). Treatment sequencing for childhood ADHD: A multiple-randomization study of adaptive medication and behavioral interventions. Journal of Clinical Child and Adolescent Psychology, 45(4), 396–415. doi: 10.1080/15374416.2015.1105138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelham WE Jr., Gnagy EM, Greenslade KE, & Milich R (1992). Teacher ratings of DSM-III-R symptoms for the disruptive behavior disorders. Journal of the American Academy of Child and Adolescent Psychiatry, 31(2), 210–218. doi: 10.1097/00004583-199203000-00006 [DOI] [PubMed] [Google Scholar]
- Pelham WE Jr., Gnagy EM, Greiner AR, Fabiano GA, Waschbusch DA, & Coles EK (2017). Summer treatment programs for Attention-Deficit/Hyperactivity Disorder In Weisz JR & Kazdin AE (Eds.), Evidence-based psychotherapies for children and adolescents (3rd ed., pp. 215–234). New York: Guilford Press. [Google Scholar]
- Pelham WE Jr., Gnagy EM, Greiner AR, Hoza B, Hinshaw SP, Swanson JM, . . . Baron-Mayak C (2000). Behavioral vs. behavioral and pharmacological treatment in ADHD children attending a summer treatment program. Journal of Abnormal Child Psychology, 28(6), 507–525. [DOI] [PubMed] [Google Scholar]
- Pelham WE Jr., Greiner AR, & Gnagy EM (1998). Children’s summer day treatment program manual. Buffalo, NY: CTADD. [Google Scholar]
- Pelham WE Jr., Hoza B, Pillow DR, Gnagy EM, Kipp HL, Greiner AR, . . . Fitzpatrick E (2002). Effects of methylphenidate and expectancy on children with ADHD: Behavior, academic performance, and attributions in a Summer Treatment Program and regular classroom setting. Journal of Consulting and Clinical Psychology, 70(2), 320–335. [PubMed] [Google Scholar]
- Pelham WE Jr., Milich R, Murphy DA, & Murphy HA (1989). Normative data on the IOWA Conners teacher rating scale. Journal of Clinical Child Psychology, 18(3), 259–262. doi: 10.1207/s15374424jccp1803_9 [DOI] [Google Scholar]
- Ray JV, & Frick PJ (2018). Assessing callous-unemotional traits using the total score from the Inventory of Callous-Unemotional Traits: A meta-analysis. Journal of Clinical Child and Adolescent Psychology, 1–10. doi: 10.1080/15374416.2018.1504297 [DOI] [PubMed] [Google Scholar]
- Reidy DE, Kearns MC, & DeGue S (2013). Reducing psychopathic violence: A review of the treatment literature. Aggression and Violent Behavior, 18(5), 527–538. doi: 10.1016/j.avb.2013.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ridenour TA, Wittenborn AK, Raiff BR, Benedict N, & Kane-Gill S (2016). Illustrating idiographic methods for translational research: Moderation effects, natural clinical experiments, and complex treatment-by-subgroup interactions. Translational Behavioral Medicine, 6(1), 125–134. doi: 10.1007/s13142-015-0357-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salekin RT (2010). Treatment of child and adolescent psychopathy: Focusing on change In Salekin RT & Lynam DT (Eds.), Handbook of child and adolescent psychopathy (pp. 343–373). New York: Guilford Press. [Google Scholar]
- Salekin RT, Tippey JG, & Allen AD (2012). Treatment of conduct problem youth with interpersonal callous traits using mental models: Measurement of risk and change. Behavioral Sciences and the Law, 30(4), 470–486. doi:Doi 10.1002/Bsl.2025 [DOI] [PubMed] [Google Scholar]
- Scott S (2016). Commentary: Finding out the best way to tailor psychological interventions for children and families--a commentary on Ng and Weisz (2016). Journal of Child Psychology and Psychiatry and Allied Disciplines, 57(3), 237–240. doi: 10.1111/jcpp.12543 [DOI] [PubMed] [Google Scholar]
- Singer JD, & Willet JB (2003). Applied longitudinal data analysis. New York: Oxford University Press. [Google Scholar]
- Waller R, Hyde LW, Baskin-Sommers AR, & Olson SL (2017). Interactions between Callous Unemotional Behaviors and Executive Function in Early Childhood Predict later Aggression and Lower Peer-liking in Late-childhood. Journal of Abnormal Child Psychology, 45(3), 597–609. doi: 10.1007/s10802-016-0184-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waschbusch DA, Bernstein MD, Robb Mazzant J, Willoughby MT, Haas SM, Coles EK, & Pelham WE Jr. (2016). A case study examining fixed versus randomized criteria for treating a child with conduct problems and callous-unemotional traits. Evidence-Based Practice in Child and Adolescent Mental Health, 1(2–3), 73–85. doi: 10.1080/23794925.2016.1227946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waschbusch DA, Carrey NJ, Willoughby MT, King S, & Andrade BF (2007). Effects of methylphenidate and behavior modification on the social and academic behavior of children with disruptive behavior disorders: The moderating role of callous/unemotional traits. Journal of Clinical Child and Adolescent Psychology, 36(4), 629–644. doi: 10.1080/15374410701662766 [DOI] [PubMed] [Google Scholar]
- Waschbusch DA, Coles EK, & Pelham WE Jr. (2013). Problem Rating Form. Penn State Hershey. [Google Scholar]
- Waschbusch DA, & Willoughby MT (2008). Parent and teacher ratings on the IOWA Conners Rating Scale. Journal of Psychopathology and Behavioral Assessment, 30(3), 180–192. doi: 10.1007/s10862-007-9064-y [DOI] [Google Scholar]
- Wechsler D (2011). Wechsler Abbreviated Scale of Intelligence - Second Edition. New York: Harcourt. [Google Scholar]
- Weisz JR, Kuppens S, Ng MY, Eckshtain D, Ugueto AM, Vaughn-Coaxum R, . . . Fordwood SR (2017). What five decades of research tells us about the effects of youth psychological therapy: A multilevel meta-analysis and implications for science and practice. American Psychologist, 72(2), 79–117. doi: 10.1037/a0040360 [DOI] [PubMed] [Google Scholar]
- White SF, Frick PJ, Lawing K, & Bauer D (2012). Callous–Unemotional traits and response to functional family therapy in adolescent offenders. Poster presented at the Behavioral Sciences and the Law. [DOI] [PubMed] [Google Scholar]
- Wilkinson S, Waller R, & Viding E (2016). Practitioner Review: Involving young people with callous unemotional traits in treatment - does it work? A systematic review. Journal of Child Psychology and Psychiatry and Allied Disciplines, 57(5), 552–565. doi: 10.1111/jcpp.12494 [DOI] [PubMed] [Google Scholar]
- Wright KD, Waschbusch DA, & Frankland BW (2007). Combining data from parent ratings and parent interview when assessing ADHD. Journal of Psychopathology and Behavioral Assessment, 29(3), 141–148. doi: 10.1007/s10862-006-9039-4 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.