Abstract
Objectives:
We examined the association between quality of postpartum contraceptive counseling and changes in contraceptive method preference between delivery and 3-months postpartum.
Study design:
We used data from 1167 postpartum women delivering at eight hospitals in Texas who did not initiate contraception in the hospital. We conducted baseline and 3-month follow-up interviews to ask women about the method they would prefer to use at 6-months postpartum, postpartum contraceptive counseling, reproductive history, and demographic characteristics. We measured quality of postpartum contraceptive counseling with seven items related to satisfaction and information received. High-quality counseling was defined as meeting all seven criteria. We used logistic regression to predict the primary outcome of changes in preferred method by contraceptive counseling and described contraceptive counseling and changes in preferred method by demographic characteristics.
Results:
Receipt of high-quality postpartum contraceptive counseling was reported by 26%. At 3-months postpartum 70% of participants reported the same contraceptive preferences by category of effectiveness that they expressed at the time of delivery. Spanish-speaking, Hispanic foreign-born, and lower socioeconomic status women were less likely to receive high-quality counseling than their counterparts. High-quality counseling was associated with lower odds of preferring a less effective method (OR: 0.31, 95% CI: 0.18–0.52) and changing preference from an IUD or implant (OR: 0.34, 95% CI: 0.17–0.68).
Conclusions:
High-quality postpartum contraceptive counseling is relatively rare and occurs less often among low SES and immigrant women. High quality counseling appears to reinforce preferences for highly effective contraception.
Implications:
Training healthcare providers to provide high-quality contraceptive counseling to all postpartum women may reduce contraceptive disparities related to race/ethnicity and social class.
Keywords: Counseling, contraception, postpartum contraception, patient preferences, Texas, race/ethnicity
1. Introduction
The American College of Obstetricians and Gynecologists recommends contraceptive counseling during prenatal and postpartum care [1]. However, there is limited evidence that counseling actually influences women’s contraceptive choices or leads to greater use of or satisfaction with contraception. This evidence mainly consists of cross-sectional studies that found a positive association between prenatal and postpartum contraceptive counseling and use of effective methods of contraception postpartum, specifically, intrauterine devices (IUDs) and implants [2–4]. It is unclear how much of the observed association between counseling and use may be due to differences in contraceptive access that may vary along with receipt of counseling. A better outcome variable is something that counseling could influence directly, such as contraceptive preferences.
Contraceptive preferences are associated with, but do not determine use. Our recent study in Texas found that among women who preferred an IUD, implant, or sterilization, only half were using them at 6-months postpartum, suggesting that there is a large gap between preferences and use [12]. Nationally, about half of postpartum women are using no method or a less-effective method of contraception, such as condoms or withdrawal, which increases their risk of short inter-pregnancy intervals [5]. Preferences for IUDs and implants are especially important to measure directly because they are often subject to provider misinformation regarding eligibility [6–9], and are more difficult to access than other contraceptive methods [10,11].
In this study, we use data from a prospective cohort study of postpartum women in Texas that assessed the method women would prefer to be using at 6-months postpartum asked just after delivery and then three months later. The study also assessed the content and quality of postpartum contraceptive counseling. We investigate the association between quality of postpartum contraceptive counseling and changes in contraceptive method preference between delivery and 3-months postpartum. We also examine quality of postpartum contraceptive counseling and changes in method preference by social and economic characteristics. Although effectiveness is only one of many method attributes that women may use to form their preferences, we examine contraceptive preference by effectiveness to advance prior research that has suggested contraceptive counseling is associated with the use of more effective contraception [2–4].
2. Materials and method
2.1. Study design
We use data from the Texas Postpartum Contraception Study, a two-year prospective cohort of 1700 women recruited following delivery at eight hospitals across Texas that began October 2014. Eligible women were between the ages of 18 and 44, spoke English or Spanish, delivered a healthy, singleton baby, were covered by public insurance or had no insurance at delivery, and wished to delay childbearing for at least two years. We include data from baseline interviews which were conducted in-person in the hospital soon after delivery and before any postpartum counseling, and telephone follow-up interviews that were carried out 3–4 months postpartum after any postpartum counseling. Full study procedures are reported elsewhere [12]. Overall, 1469 women (86%) completed the 3-month survey. We excluded 232 women who were sterilized by 3-months postpartum, 65 women who received an immediate postpartum IUD or implant, and 4 women who were pregnant by the 3-month survey because none of these women were asked about postpartum contraceptive counseling. Finally, we excluded one participant who was missing data on contraceptive preferences at baseline. The final sample size was 1167 women.
2.2. Measures
To assess participants’ contraceptive preferences at baseline we asked two questions: (1) What method they would like to be using by the time their baby turned 6-months old and, (2) what method they would like to be using at 6-months if they could get any method for free. At the 3-month interview, we asked three questions: (1) what method they would like to be using by the time their baby turned 6-months old, (2) what method they would like to be using at 6-months if they could get any method for free, and (3) among women who attended a postpartum visit, we asked if there was a method they wanted to get at their postpartum visits that they were unable to get. We considered the preferred method to be the most effective method given in each series of questions.
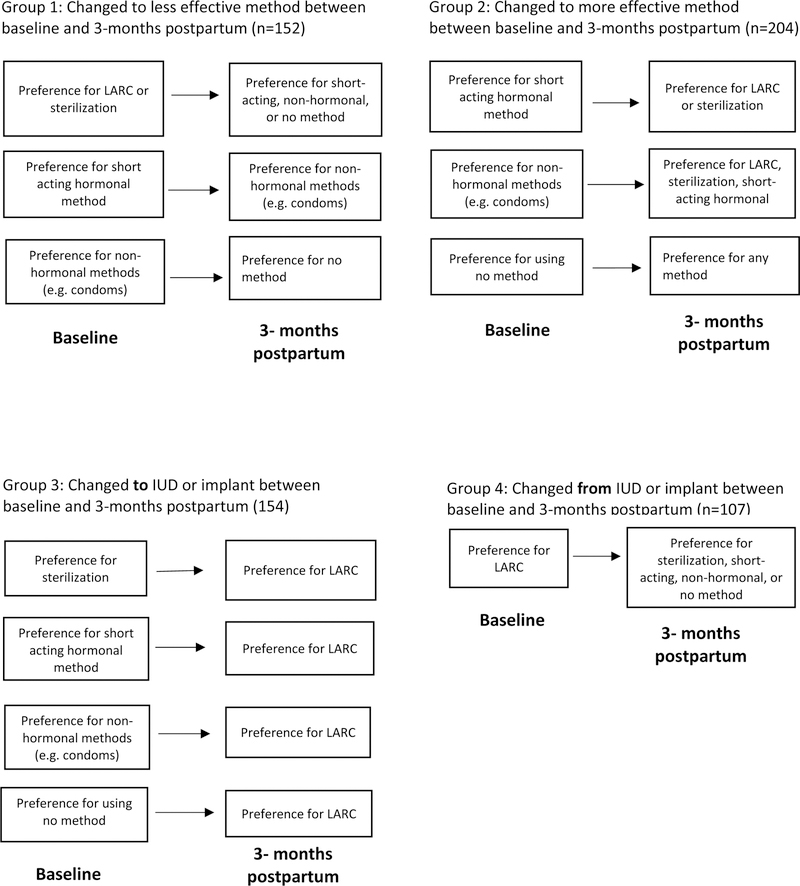
We assessed four outcome variables through comparisons in method preference between baseline and 3-months postpartum (Figure 1). First, we captured a change to a more effective method if the participant preferred a short-acting hormonal method (i.e., injection, contraceptive pill, ring, or patch), a less effective method (e.g., condom, abstinence), or no method at baseline and they preferred a more effective method at 3-months. Women preferring sterilization or an IUD or implant are not eligible to change to a more effective method so they were not included in this variable. Second, we captured a change to a less effective method if the participant preferred sterilization, IUD or implant, a short-acting hormonal, or less effective methods at baseline and preferred a less effective method at 3-months. Women preferring no method or who did not know their preference were not included in the variable because they were not eligible to choose a less effective method. We also created a categorical variable that included the full sample: (1) No change in preferred method; (2) change to more effective method; and (3) change to a less effective method.
Figure 1:
Analytic groups defined according to change in 6-month contraceptive preference between delivery (baseline) and 3-months postpartum among low-income women in Texas who not initiate contraception in prior to hospital discharge, 2014–2018.
Third, we created a variable that included all participants who did not prefer an IUD or implant at baseline. They were coded as having changed to an IUD or implant if they preferred an IUD or implant at 3 months postpartum. Finally, we created a variable that included all participants who preferred an IUD or implant at baseline. They were coded as having changed from an IUD or implant if they did not prefer an IUD or implant at 3 months postpartum. We also created a categorical variable that included all participants: (1) Never preferred IUD or implant; (2) changed from an IUD or implant; (3) changed to an IUD or implant; and (4) always preferred an IUD or implant.
We assessed the type of contraceptive counseling women received at their first postpartum visit with a series of questions at the 3-month survey developed by Dehlendorf and colleagues [13]. We considered the first postpartum visit as a specified postpartum checkup or the first medical visit postpartum where a participant discussed contraception with a provider. We asked if they discussed any method of contraception at their first postpartum visit with a health care provider and if they discussed both the IUD and implant. Women who reported receiving any contraceptive counseling were asked three questions that were answered on a Likert scale: (1) “How well did [provider] do at letting you say what mattered to you about your birth control method?”, (2) “How well did [provider] do at giving you an opportunity to ask questions?”, and (3) “How do you feel about how involved [provider] was with helping you choose a birth control method?” We also asked if the provider discussed four aspects of their preferred method: (1) Possible side effects, (2) effectiveness, (3) patient cost, and (4) method removal for IUDs or implants. Due to skip patterns, participants whose response to the first direct preference question was a less effective methods such as condoms, were only asked about effectiveness. We consider postpartum contraceptive counseling to be “high-quality” if the participant rated their provider as either “excellent” or “very good” on the first two satisfaction questions, “involved the right amount” on the third question, and if they received information on all aspects related to their preferred method. Finally, we created a categorical variable to measure the type of postpartum contraceptive counseling received: (1) No contraceptive counseling; (2) minimal contraceptive counseling (i.e., discussed contraception but did not discuss both the IUD and implant and was not considered “high-quality” counseling; (3) received counseling on IUDs and implants (a proxy for received information on all methods), but not “high-quality” counseling; and (4) women who received “high-quality counseling.” The 37 participants (3%) with missing responses on any of the seven items defaulted into the next highest category. Women who did not have a postpartum checkup or discuss contraception at any visit after delivery (n=199) were considered to not have received any contraceptive counseling.
We included social, economic, and reproductive history variables: Hospital of delivery, age (18–24, 25–29, 30+), number of living biological children (1, 2, 3+), race/ethnicity and nativity (foreign-born Hispanic, U.S.-born Hispanic, non-Hispanic black, non-Hispanic white or other), education (<high school, high school diploma or equivalent, >high school), income (<$10,000, $10,000-$19,000, $20,000-$34,999, $35,000+, don’t know), and language of interview (English or Spanish). Insurance status (has or does not have insurance), relationship status (single, cohabitating, married), and childbearing intentions (wants more, does not want more, unsure) were taken from the 3-month survey.
2.3. Analysis
We calculated proportions for preferred contraceptive methods at baseline and 3-months postpartum and changes in method preference for the full sample. We used χ2 tests to calculate significant differences between the type of contraceptive counseling received and social and demographic characteristics. Finally, we predicted each of the four dichotomous contraceptive preference change outcomes, after adjusting for covariates: Change to a more effective method (Model 1); change to a less effective method (Model 2); change to an IUD or implant (Model 3); and change from an IUD or implant (Model 4). We used logistic regression models that accounted for the clustering of participants within hospitals. We included covariates that improved model fit with a likelihood ratio test χ2 p-value of <0.05. Because of the positive association between parity and age, we included both variables in any model that had a significant likelihood ratio test for either. We used list-wise deletion for missing data (all variables missing < 0.5% of observations). Analyses were conducted with Stata 13.
3. Results
At baseline and 3-months postpartum, almost half of participants wanted to use an IUD or implant at six-months after delivery, and almost one-third had a preference for other hormonal methods; the difference in method preferences between baseline and 3-months was significant (p<0.001) (Table 1). Seventy-percent of participants did not change their method preference by effectiveness tier; 18% changed their preference to a more effective method and 13% to a less effective method. Over three-quarters (78%) did not change their preference to or from an IUD or implant; 9% changed to an IUD or implant and 13% from an IUD or implant (not shown).
Table 1.
Six-month postpartum method preference reported at baseline and 3-months postpartum by low-income women in Texas who not initiate contraception in prior to hospital discharge (N=1,167), 2014–2018
| Baseline (%) | 3-months (%) | |
|---|---|---|
| Sterilization | 8.1 | 7.1 |
| IUD or implant | 46.7 | 50.7 |
| Non-LARC hormonal method | 32.4 | 30.9 |
| Less effective methods | 6.5 | 8.5 |
| None/Don’t know | 6.3 | 2.8 |
Approximately one-quarter of participants received high-quality counseling and 22% did not receive any contraceptive counseling (Table 2). Type of counseling varied by hospital. Women who were Hispanic foreign-born or white and other, Spanish-speaking, without insurance, less educated, or had a household income of less than $10,000, were less likely to receive high-quality counseling and more likely to receive no counseling than women who were Hispanic U.S.-born, English-speaking, insured, had more than a high school education, and a household income of $35,000 or more. Women who received contraceptive counseling at a private practice were more likely to receive minimal counseling but less likely to receive counseling on IUDs and implants than other women.
Table 2:
Social and economic characteristics by type of postpartum contraceptive counseling among low-income women in Texas who not initiate contraception in prior to hospital discharge, 2014–2018
| N | No contraceptive counseling % | Minimal contraceptiv e counseling % | Counseling on IUDs & implants, not high quality % | High quality counseling % | χ2 p-value | |
|---|---|---|---|---|---|---|
| All Hospital | 1167 | 22.4 | 33.9 | 17.3 | 26.5 | |
| Hospital 1 | 224 | 13.4 | 33.5 | 18.8 | 34.4 | |
| Hospital 2 | 156 | 36.5 | 31.4 | 17.3 | 14.7 | |
| Hospital 3 | 65 | 18.5 | 38.5 | 18.5 | 24.6 | |
| Hospital 4 | 207 | 10.1 | 31.4 | 25.6 | 32.9 | |
| Hospital 5 | 64 | 34.4 | 26.6 | 9.4 | 29.7 | |
| Hospital 6 | 227 | 18.9 | 43.6 | 12.8 | 24.7 | |
| Hospital 7 | 153 | 26.6 | 27.9 | 15.6 | 29.9 | |
| Hospital 8 | 71 | 49.3 | 32.4 | 12.7 | 5.6 | <0.001 |
| Age | ||||||
| 18–24 | 605 | 22.4 | 31.9 | 17.0 | 28.7 | |
| 25–29 | 306 | 20.3 | 35.3 | 20.3 | 24.2 | |
| 30+ | 256 | 24.6 | 37.1 | 14.5 | 23.8 | 0.231 |
| Race/ethnicity/nativity | ||||||
| Hispanic Foreign-born | 502 | 26.0 | 32.0 | 19.0 | 24.0 | |
| Hispanic U.S.-born | 439 | 18.0 | 37.0 | 15.0 | 30.0 | |
| Non-Hispanic Black | 161 | 22.0 | 27.0 | 22.0 | 29.0 | |
| White & Other | 65 | 26.1 | 45.0 | 9.0 | 20.3 | 0.003 |
| Language | ||||||
| Spanish | 430 | 27.9 | 30.0 | 20.0 | 22.1 | |
| English | 737 | 19.1 | 36.2 | 15.7 | 29.0 | <0.001 |
| Insurance status (3-months) | ||||||
| Does not have insurance | 874 | 24.1 | 34.1 | 18.1 | 23.7 | |
| Has insurance | 289 | 17.2 | 33.1 | 15.2 | 34.5 | 0.001 |
| Education | ||||||
| <High school | 381 | 25.2 | 35.4 | 15.5 | 23.9 | |
| High school | 486 | 24.9 | 31.1 | 17.7 | 26.3 | |
| >High school | 300 | 14.3 | 36.5 | 18.9 | 29.9 | 0.009 |
| Living children | ||||||
| 1 | 359 | 18.1 | 33.7 | 18.7 | 29.5 | |
| 2 | 402 | 22.4 | 35.2 | 17.9 | 24.3 | |
| 3+ | 406 | 25.9 | 32.8 | 15.5 | 25.9 | 0.188 |
| Relationship status (3-months) | ||||||
| Single | 353 | 24.9 | 31.7 | 17.6 | 25.8 | |
| Cohabitating | 449 | 20.0 | 33.4 | 18.0 | 28.5 | |
| Married | 363 | 22.8 | 36.5 | 16.2 | 24.5 | 0.457 |
| Childbearing intentions (3-months) | ||||||
| Does not want more children | 404 | 26.4 | 32.4 | 17.8 | 23.5 | |
| Wants more children | 647 | 21.2 | 34.3 | 17.2 | 27.4 | |
| Unsure if wants more | 113 | 15.0 | 36.3 | 16.8 | 31.9 | 0.165 |
| Annual Household Income | ||||||
| <$10,000 | 416 | 26.7 | 36.3 | 16.6 | 20.4 | |
| $10,000 – $19,999 | 358 | 19.0 | 32.7 | 17.3 | 31.0 | |
| $20,000 – $34,999 | 238 | 19.3 | 34.9 | 19.8 | 26.1 | |
| $35,000+ | 110 | 23.4 | 29.7 | 13.5 | 33.3 | |
| Don’t know | 45 | 22.2 | 26.7 | 20.0 | 31.1 | 0.045 |
| Postpartum counseling location | ||||||
| Private | 394 | 7.0 | 43.0 | 16.0 | 34.0 | |
| Public/Mexico | 513 | 6.0 | 37.0 | 26.0 | 31.0 | 0.005 |
| Method preference (3-months) | ||||||
| None/Don’t know | 33 | 54.6 | 21.2 | 24.2 | 0.0 | |
| Less effective methods | 83 | 27.3 | 38.4 | 18.2 | 16.2 | |
| Non-LARC hormonal methods | 592 | 21.4 | 40.0 | 16.9 | 21.7 | |
| Implant or IUD | 360 | 19.6 | 29.6 | 16.6 | 34.3 | |
| Male or female sterilization | 99 | 26.5 | 38.6 | 20.5 | 14.5 | <0.001 |
Model 1 in Table 3 shows that women 30 and older were less likely to change their preference to an effective method between delivery and 3-months postpartum than women 18 to 24 years-old. There was no significant association between type of contraceptive counseling and preference for an effective method. In contrast, women who received minimal contraceptive counseling, counseling on IUDs and implants, or high-quality counseling had lower odds of changing their preference to a less effective method than women who received no counseling (Model 2, Table 3). Non-Hispanic black women had higher odds of changing their preference to a less effective method than Hispanic foreign-born women. Among women who did not prefer an IUD or implant at baseline, women 30 and older had lower odds of changing their preference to an IUD or implant than women 18 to 24 years old. Women with two or more children were more likely to change their preference to an IUD or implant than women with one child. Women who received high-quality counseling were more likely to change their preference to an IUD or implant than women who received no counseling (Model 3, Table 3). Among women with a preference for an IUD or implant, non-Hispanic black women were more likely than Hispanic foreign-born women to change their preference from an IUD or implant (Model 4, Table 3). Finally, women who received high-quality counseling were less likely to change their preference from an IUD or implant than women who received no counseling.
Table 3.
Multivariate models (Odds Ratios, 95% confidence intervals) predicting a change in contraceptive method preference between delivery and 3-months postpartum among low-income women in Texas who not initiate contraception in prior to hospital discharge, 2014–2018.α
| To MORE effective method Model 1 | To LESS effective method Model 2 | TO LARC Model 3 | FROM LARC Model 4 | |
|---|---|---|---|---|
| Postpartum contraceptive counseling | ||||
| No contraceptive counseling | Ref. | Ref. | Ref. | Ref. |
| Minimal contraceptive counseling | 1.19 (0.64 – 2.21) | 0.55 (0.41 – 0.72) | 0.91 (0.47 – 1.77) | 0.74 (0.42 – 1.30) |
| Counseling on IUDs & implants but not high quality | 1.21 (0.77 – 1.88) | 0.59 (0.36 – 0.98) | 0.88 (0.62 – 1.24) | 0.63 (0.30 – 1.34) |
| High quality counseling | 1.34 (0.66 – 2.72) | 0.31 (0.18 – 0.53) | 1.76 (1.05 – 2.94) | 0.32 (0.16 – 0.65) |
| Age | ||||
| 18–24 | Ref. | Ref. | ||
| 25–29 | 1.00 (0.55 – 1.79) | 0.83 (0.51 – 1.36) | ||
| 30+ | 0.47 (0.26 – 0.85) | 0.34 (0.17 – 0.66) | ||
| Race/ethnicity/nativity | ||||
| Hispanic Foreign-born | Ref. | Ref. | ||
| Hispanic U.S.-born | 1.30 (0.90 – 1.86) | 1.34 (0.64 – 2.78) | ||
| Non-Hispanic Black | 2.21 (1.21 – 4.04) | 3.30 (2.41 – 4.53) | ||
| White & Other | 1.54 (0.67 – 3.53) | 2.32 (0.96 – 5.60) | ||
| Living children | ||||
| 1 | Ref. | Ref. | ||
| 2 | 0.91 (0.65 – 1.28) | 1.23 (1.05 – 1.43) | ||
| 3+ | 1.44 (0.84 – 2.47) | 1.68 (1.15 – 2.45) | ||
| Constant | 0.59 (0.32 – 1.07) | 0.22 (0.14 – 0.34) | 0.32 (0.17 – 0.60) | 0.28 (0.14 – 0.56) |
| Observations | 527 | 1,094 | 622 | 545 |
Only variables shown were included in the models
4. Discussion
We found that high-quality counseling was not commonly nor equitably received in this setting. It is also concerning that almost one-quarter of participants did not receive any postpartum contraceptive counseling. Perhaps postpartum counseling may not change women’s preferred method to something more effective, but providing high-quality and comprehensive counseling that includes side effects, use, and cost may reinforce women’s preferences and reduce the likelihood of changing to a less effective method. Regarding IUDs and implants, women are generally less knowledgeable about IUDs and implants than other methods [5,14] and may learn about them during their postpartum visit. However, low quality counseling on IUD and implant was not associated with a changing preference to an IUD or implant, suggesting that information alone is not as influential as patient-centered counseling.
We do not argue that counseling should center on effectiveness, indeed our measure of high-quality counseling focused on patient-centeredness. We focus on changes in preferences by effectiveness to challenge prior literature that examined the association between counseling and postpartum use of effective methods [2–4] and find that counseling may have a more indirect effect on contraceptive preferences by reinforcing pre-existing preferences, rather than changing them. By restricting the analysis to preferences rather than use, we are able to limit the confounding that may exist due to an association between counseling and access. It may also be possible to avoid confounding in prospective studies that adjust for variation in clinical context, and in which the assumption that women have actually chosen their preferred method is reasonable [13].
The low frequency of high-quality contraceptive counseling, particularly among immigrant and low SES women is concerning. Spanish-speaking and low-income women of color are often dissatisfied with contraceptive counseling [15–18] or pressured into using certain types of contraception [17,19]. Consistent with prior research showing black women are less likely than white and Hispanic women to prefer and use IUDs and implants, black women were also more likely than Hispanic foreign-born women to change to a less effective method or change from an IUD or implant [12,20]. This could also reflect greater access to and acceptability of postpartum IUDs in Mexico [21].
A lower proportion of women receiving contraceptive counseling at private practices received counseling on IUDs and implants than women from public clinics. Public clinics may be more likely to provide IUDs and implants due to lower costs and their staff may have better knowledge on counseling and medical eligibility criteria [22,23].
Advancing prior research, we measured contraceptive preferences rather than use and used longitudinal data to examine contraceptive preferences both before and after postpartum contraceptive counseling. We also incorporated the quality of counseling. However, limitations include that we cannot assess whether women changed their preference before counseling occurred or as a result of other social and demographic factors, we did not ask why participants preferred a method, and we were unable to assess if participants received counseling while in the hospital for admission. Our design also prevents us from looking for any effects that counseling might have on how women use and continue contraception.
This research suggests that contraceptive counseling may play an important role in maintaining a preference for an effective contraceptive method rather than changing method preference. It also underscores the importance of equitable and high-quality contraceptive counseling.
Acknowledgements:
We would like to thank the following individuals who served as site investigators: Aida Gonzalez, MSN, RN, Moss Hampton, MD, Ted Held, MD, MPH, Nima Patel-Agarwall, MD, Sireesha Reddy, MD, Ruby Taylor, DNP, RN, Cristina Wallace, MD. We also thank Christine Dehlendorf, MD and her team for sharing their contraceptive counseling survey questions.
Funding source: This project was supported by a grant from the Susan Thompson Buffett Foundation, and a center grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (P2CHD042849) awarded to the Population Research Center at the University of Texas at Austin and the University of Colorado Population Center (grant R24 HD066613). The funders played no role in the design and conduct of the study; interpretation of the data; or preparation, review, or approval of this manuscript for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- [1].American Academy of Pediatrics, American College of Obstetricians and Gynecologists, editors. Guidelines for perinatal care 7th ed. Elk Grove Village, IL : Washington, DC: American Academy of Pediatrics ; American College of Obstetricians and Gynecologists; 2012. [Google Scholar]
- [2].Hernandez LE, Sappenfield WM, Goodman D, Pooler J. Is Effective Contraceptive Use Conceived Prenatally in Florida? The Association Between Prenatal Contraceptive Counseling and Postpartum Contraceptive Use. Matern Child Health J 2011;16:423–9. [DOI] [PubMed] [Google Scholar]
- [3].Wilson EK, Fowler CI, Koo HP. Postpartum Contraceptive Use Among Adolescent Mothers in Seven States. J Adolesc Health 2013;52:278–83. [DOI] [PubMed] [Google Scholar]
- [4].Zapata LB, Murtaza S, Whiteman MK, Jamieson DJ, Robbins CL, Marchbanks PA, et al. Contraceptive counseling and postpartum contraceptive use. Am J Obstet Gynecol 2015;212:171.e1–171.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].White K, Teal SB, Potter JE. Contraception After Delivery and Short Interpregnancy Intervals Among Women in the United States. Obstet Gynecol 2015;125:1471–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Zerden ML, Tang JH, Stuart GS, Norton DR, Verbiest SB, Brody S. Barriers to Receiving Long-acting Reversible Contraception in the Postpartum Period. Womens Health Issues 2015. [DOI] [PubMed]
- [7].Biggs MA, Arons A, Turner R, Brindis CD. Same-day LARC insertion attitudes and practices. Contraception 2013;88:629–35. [DOI] [PubMed] [Google Scholar]
- [8].Coleman-Minahan K, Aiken ARA, Potter JE. Prevalence and Predictors of Prenatal and Postpartum Contraceptive Counseling in Two Texas Cities. Womens Health Issues 2017;27:707–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Coleman-Minahan K, Dillaway CH, Canfield C, Kuhn DM, Strandberg KS, Potter JE. Low-Income Texas Women’s Experiences Accessing Their Desired Contraceptive Method at the First Postpartum Visit. Perspect Sex Reprod Health 2018;50:189–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Potter JE, Hopkins K, Aiken ARA, Hubert C, Stevenson AJ, White K, et al. Unmet demand for highly effective postpartum contraception in Texas. Contraception 2014;90:488–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Tang JH, Dominik RC, Zerden ML, Verbiest SB, Brody SC, Stuart GS. Effect of an educational script on postpartum contraceptive use: a randomized controlled trial. Contraception 2014;90:162–7. [DOI] [PubMed] [Google Scholar]
- [12].Potter JE, Coleman-Minahan K, White K, Powers D, Dillaway C, Stevenson AJ, et al. Contraception After Delivery Among Publicly Insured Women in Texas: Use Compared With Preference. Obstet Gynecol 2017;130:393–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Dehlendorf C, Henderson JT, Vittinghoff E, Grumbach K, Levy K, Schmittdiel J, et al. Association of the Quality of Interpersonal Care During Family Planning Counseling with Contraceptive Use. Am J Obstet Gynecol 2016;0. [DOI] [PubMed]
- [14].White K, Hopkins K, Potter JE, Grossman D. Knowledge and Attitudes about Long-Acting Reversible Contraception Among Latina Women Who Desire Sterilization. Womens Health Issues 2013;23:e257–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Dehlendorf C, Krajewski C, Borrero S. Contraceptive Counseling: Best Practices to Ensure Quality Communication and Enable Effective Contraceptive Use. Clin Obstet Gynecol 2014;57:659–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Brown GF, Moskowitz EH. Moral and policy issues in long-acting contraception. Annu Rev Public Health 1997;18:379–400. [DOI] [PubMed] [Google Scholar]
- [17].Becker D, Tsui AO. Reproductive Health Service Preferences And Perceptions of Quality Among Low-Income Women: Racial, Ethnic and Language Group Differences. Perspect Sex Reprod Health 2008;40:202–211. [DOI] [PubMed] [Google Scholar]
- [18].Forrest JD, Frost JJ. The family planning attitudes and experiences of low-income women. Fam Plann Perspect 1996:246–277. [PubMed]
- [19].Dehlendorf C, Ruskin R, Grumbach K, Vittinghoff E, Bibbins-Domingo K, Schillinger D, et al. Recommendations for intrauterine contraception: a randomized trial of the effects of patients’ race/ethnicity and socioeconomic status. Am J Obstet Gynecol 2010;203:319.e1–319.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Kavanaugh ML, Jerman J, Finer LB. Changes in Use of Long-Acting Reversible Contraceptive Methods Among U.S. Women, 2009–2012. Obstet Gynecol 2015:1. [DOI] [PMC free article] [PubMed]
- [21].Potter JE, Hubert C, White K. The availability and use of postpartum LARC in Mexico and among Hispanics in the United States. Matern Child Health J 2017;21:1744–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Thiel de Bocanegra H, Cross Riedel J, Menz M, Darney PD, Brindis CD. Onsite Provision of Specialized Contraceptive Services: Does Title X Funding Enhance Access? J Womens Health 2014;23:428–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Biggs MA, Harper CC, Malvin J, Brindis CD. Factors influencing the provision of long-acting reversible contraception in California. Obstet Gynecol 2014;123:593–602. [DOI] [PubMed] [Google Scholar]