Abstract
[Purpose] Specific exercises and brace treatment are the two evidence-based modes of treatment for patients with scoliosis. The purpose of this paper is to present the first end-results from a prospective cohort that commenced treatment in 2011 with a CAD based Chêneau derivate and is then compared to the published results achieved with the Boston Brace. [Participants and Methods] Inclusion criteria for the study, refers to the SRS inclusion criteria on bracing, except the range of Cobb angles which was extended to curvatures of up to 45°. Twenty-eight patients were weaned from their CAD Chêneau style brace. The results of this cohort have been compared with the BRAIST study by Weinstein et al. with the help of the Z-test. [Results] A success rate of 92.9% has been achieved. This was compared to the success rate of 72% in the BRAIST study. The differences were highly significant in the Z-test. [Conclusion] The results achieved with the GBW are significantly and better than the results achieved with the Boston brace. Therefore, the standards for bracing should be reviewed with the results that symmetric compression with Boston bracing is not as successful, when compared to asymmetric high correction bracing results, which allow a standardized classification-based corrective approach.
Key words: Scoliosis, Physiotherapy, Brace treatment
INTRODUCTION
Scoliosis is a 3D deformity of the spine and trunk. Numerous causes of scoliosis have been described; the most common scoliosis presentation is adolescent idiopathic scoliosis (AIS)1,2,3,4). AIS is defined as a lateral curve of the spine in an otherwise healthy child4). The cause of AIS, as the term ‘idiopathic’ indicates, has not yet been found, although recent papers support the hypothesis that the origin of AIS lies in a functional tethering of the spinal cord5, 6).
It is now generally accepted that scoliosis is a 3D deformity but the Cobb angle (measured in the frontal plane)7) continues to be the most important parameter used by researchers in the medical field and in subsequent guidelines.
Treatments of AIS and other forms of scoliosis in the main consists of; exercise; brace treatment and spinal fusion surgery. While there is high quality evidence supporting exercises8,9,10) and brace treatment11) during growth, no high-quality evidence exists to support spinal fusion surgery12,13,14,15,16,17). Because evidence for spinal fusion is still lacking, Ward et al. suggest including those patients with curves exceeding 40° conservatively, a threshold which historically was seen as being an indication for surgery17).
Today there are numerous studies on brace treatment of patients with AIS18,19,20,21,22,23,24). In the US, UK, Scandinavia and some countries in Asia, the Boston brace is widely used. Boston brace treatment is supported by several cohort studies19), a multicenter controlled prospective study22) as well as by a randomized study11) and a Meta-analysis24).
Part-time bracing is not supported by high quality evidence24). We now know that in-brace correction and brace wearing time (compliance) directly correlate and therefore determine the end-result of bracing18). This fact has been confirmed in a recent review25).
The Chêneau brace was introduced in Muenster, Germany and historically is the most important evolution in brace design in central Europe. The first end-results of the cast based Chêneau brace have been published 198526). When compared to the first end-results with the Milwaukee brace27) the Chêneau sample was shown to be more effective. There are also studies demonstrating better results found for Chêneau style braces than found in the studies on the Boston brace23, 28,29,30,31).
Like the Boston braces, Chêneau braces initially have been made by casting the patient and by using the plaster positive as the basis for modelling the final brace form32). This form is then wrapped with a heated polyethylene sheet which is vacuumed to the form and finally cut from the mould32). Some studies exist to support cast based Chêneau style bracing33,34,35,36,37,38) including one prospective controlled paper23).
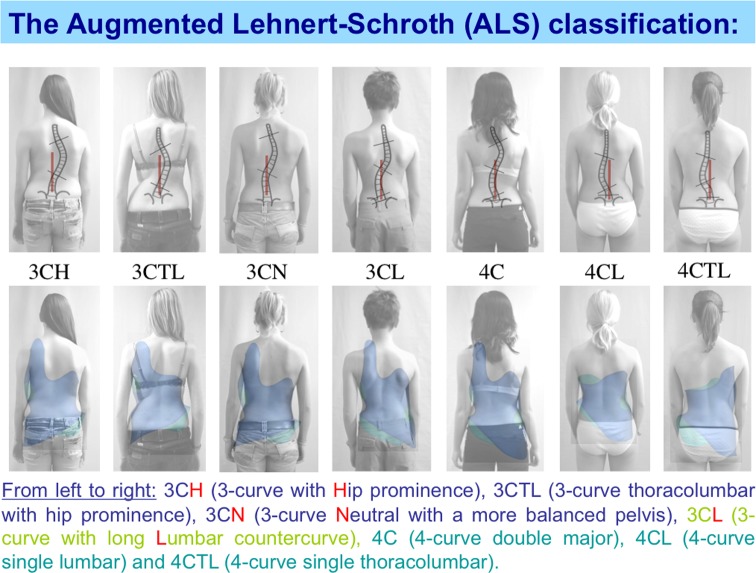
CAD/CAM technology (Computer Aided Design/Computer Aided Manufacturing) has been introduced since the end of the last century but is increasingly used in the last 10 to 15 years. All the Chêneau style CAD braces in use today were originally developed in Germany (Regnier brace, Rigo-Chêneau brace, Gensingen brace [GBW]). The advantage of these CAD Chêneau braces is that bracing can be standardized29). All the existing Chêneau based CAD systems use certain classifications and provide a library of braces in order to address different patterns of curvature appropriately29). The GBW application31, 39) as used in this study, is based upon the patterns of the Augmented Lehnert-Schroth (ALS) classification (Fig. 1). This brace has been described in international literature since 201039) and the CAD approach to assessment for bracing has been described in more depth recently40).
Fig. 1.
The ALS Classification (With kind permission Schroth Best Practice Academy).
The purpose of this paper is to present the first end-results from a prospective cohort started in 2011 treated with GBW and to compare the results to those achieved with the Boston Brace from another publication with a prospective design11).
PARTICIPANTS AND METHODS
The treatment group: We included all patients into our prospective database complying with the SRS inclusion criteria for studies on bracing (Girls only, Age 10−14 years, Risser 0–2, Cobb angle 25−40°, no other treatment than physiotherapy prior to bracing). With the exception of the range of Cobb angles, which was then extended to curvatures of up to 45° in order to increase the number of patients in the study.
One hundred five patients treated with the Gensingen brace (GBW), complying with the inclusion criteria, within our prospective database. Fifty five of these have a minimum follow-up of 18 months (a preliminary cohort). End-results have been obtained in 28 patients from this cohort as of December 2018 (end result cohort).
Twenty eight patients from our prospective cohort were weaned from their CAD Chêneau style brace initially with an average age of 12.5 years (SD 0.96); an average Risser sign of 0.8 (SD 0.9), average Cobb angle of 32.6° (SD 6.24) and were one to 24 months without brace at the final investigation. Average angle of trunk rotation (ATR) in the thoracic region was 8.5° (SD 4.5) and lumbar 6.4 (SD 4.0). There were 12 primary thoracic (3CH, 3CN, 3CTL), 4 lumbar (4CL), 3 thoracolumbar (4CTL) and 9 double major curves (4C, 3CL). Patients were excluded if they received previous treatment for adolescent idiopathic scoliosis other than physiotherapy.
The results of this cohort have been compared to the BRAIST (Bracing in Adolescent Idiopathic Scoliosis Trial) study by Weinstein et al.11) with the help of the Z-test. Failure in both studies was defined as a Cobb angle reaching or exceeding 50° Cobb.
When the clinical parameters were met at the last consultation and compared to the consultation of the last X-Ray at the end of the weaning phase, this X-Ray was used, and no new X-Ray was made.
The brace applied in this study: The patients in the treatment group have received a CAD (computer aided design) Chêneau style brace. This brace design is the Gensingen brace (GBW) which today is the most used asymmetric CAD designed Chêneau style brace worldwide28, 29, 31, 39, 40). A brace library of different brace forms is available in order to address different patterns of curvature29). The choice of brace depends on the Augmented Lehnert Schroth (ALS) classification system29,30,31). With this approach we may gain a consistent quality as the pathway of brace choice and individual CAD adjustment relies on standardized algorithms. The GBW has been described in more depth as early as 201039), however this brace has been largely developed over the last ten years, therefore some of these early braces look different compared to the more modern examples31, 40). As the GBW has been developed with the aim to address different patterns of curvature specifically, a series of different brace forms has been established. Examples of different Gensingen braces for different curve patterns and some of the results achieved can be found in the Figs. 2 , 3 , 4 , 5 , 6.
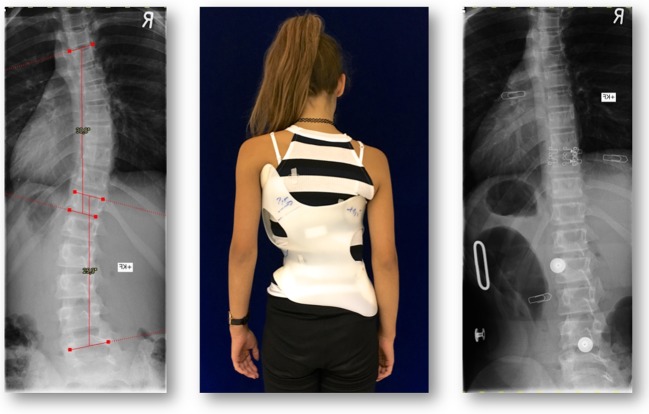
Fig. 2.
Thirteen-years-old girl with a combined curve fully corrected in a GBW. On the left X-Ray before bracing, middle picture Patient from the rear in the brace and on the right x-ray in the brace. The drawings on the brace are the suggestions made by the first author in order to improve brace fit. The metal markers as seen on the in-brace X-Ray on the right indicate the height of the peak pressure areas of the brace.
Fig. 3.

In small single curve patterns overcorrections are possible with the GBW in case the patient is still immature (13 year-old girl, one-year postmenarchial).
Fig. 4.

More than 50% correction in a 12 year-old girl with AIS of single lumbar characteristics treated with a Gensingen CAD/CAM brace (GBW). On the upper right the ventral aspect of the brace is visible, on the lower right the CAD scene with the scan of the patient and the final brace file ready for being carved.
Fig. 5.
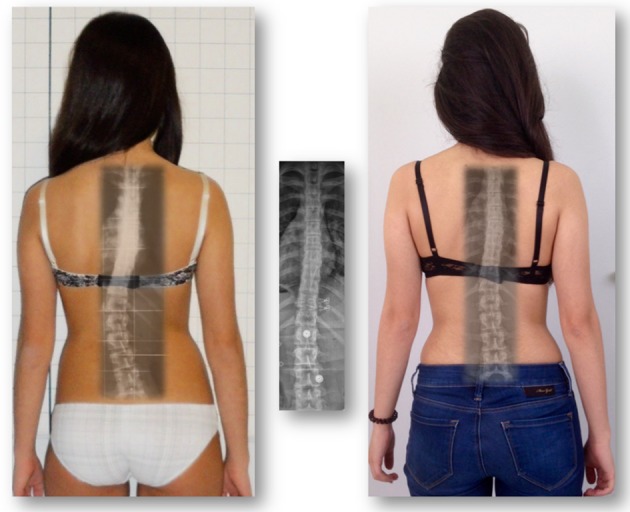
Left: 12 year-old girl with a 30° thoracolumbar curve corrected to 6° in the Gensingen brace (middle). Right: The same patient at the age of 15.6 years with 12° one year without the brace. The pelvis has been rebalanced.
Fig. 6.

Left: 27° single thoracic curve with an ATR (angle of trunk rotation) of 10° at the start of treatment at the age of 13.0 years. Middle: Result 5 months without brace at the age of 15.0 years and with 20° Cobb and ATR 3°. Right: Final result >2 years without brace 22° Cobb and ATR 4°. Rib hump has been reduced significantly after treatment with the GBW. The initial ATR was 10°, the final value was 4°. Trunk symmetry is also improved when focusing on the initial pelvic prominence after treatment being rebalanced. Both clinical parameters seem relatively stable more than two years after brace weaning as is the Cobb angle improvement.
The control group: Since it has been found that brace treatment is effective in prospective controlled19,20,21) and randomized controlled11) studies it would have been unethical to establish an untreated control group in patient samples at risk for being progressive. Therefore, it seems reasonable to use a published group from a study with similar inclusion criteria as a control group.
The BRAIST study11) contains a sample of patients treated with a Boston style brace with comparable characteristics. Inclusion criteria for the BRAIST study were as follows:
Patients with AIS, age 10−15 years, Risser 0–2, Cobb angle 20−40°. One hundred forty six patients were included with an average age of 12.7 years, Cobb angle 30.5 years and the majority of curves were thoracic or combined like in our sample treated with the GBW. The average follow-up time was 24.2 months. Rate of treatment success was 72%. In-brace correction in the control cohort has not been reported11).
The brace applied within the control group: The only information about the braces as used within the control group was the following: The majority of patients assigned to bracing (68%) were treated with a customized Boston-type thoracolumbosacral orthosis11). No picture or description of the brace was provided within the study, which would have provided more depth of understanding. The typical Boston brace is a more symmetric brace with a soft padded area of the apical areas of the curves. As there are no voids (spaces) opposite to the pressure areas like in the Chêneau style braces, the Boston braces tend to lead to compression, which may cause discomfort.
Statistical Analysis: A Z-test to compare cohorts of different sizes was performed as proposed by Goldberg41), to compare the success rate of this cohort, to the success rate of patients from the BRAIST cohort, a study which predominately used the Boston-type brace11). The Z-test is to compare two different proportions to each other, when the raw data of one group is not available. The Z-test within this paper has been performed by the last author (AK).
In the BRAIST study11), 146 patients were braced and followed through skeletal maturity. In this sample 28 patients have been treated and followed until the completion of the treatment at skeletal maturity.
The success rate of 92.9% from this study has been compared to the success rate of the BRAIST study, which was 72%. Additionally, also the success rate from our preliminary cohort (n=55; 94.5%) has been compared to the success rate of the BRAIST study using the Z-test. The study has been approved by the ethics committee of the Ärztekammer Rheinland-Pfalz (Chamber of physicians of Rhineland-Palatinate). The chair has stated that by using this study design according to German laws not official approval is necessary.
Written informed consent has been obtained from all patients and their parents to be included in this study.
RESULTS
End-result (ER) cohort: The average in brace correction (GBW brace group) was 51.4%. Two of the 28 patients (7.1%) from this group reached or exceeded 50° at final follow-up making a success rate 92.9%. This was compared to the success rate of 72% in the BRAIST study. The differences were highly significant in the Z-test (z=2,58, t=−3.42, p=0.01). Final Cobb angle was 29.2° (SD 10.4). ATR (angle of trunk rotation as measured with the Scoliometer™) thoracic was reduced from 8.5 to 7.8°, ATR lumbar from 6.4 to 3.9°.
Average brace wearing time as reported was 20.3 hrs per day (SD 3.5), average clinical follow-up was 32.1 months (SD 10.9) and the average radiological follow-up time 25.3 months (SD 13.9).
One patient with a curve of 25° dropped out of this study for other serious non-related health issues and left the study after the in-brace results. This patient returned in October 2018, more than two years without the brace with a final Cobb angle measuring 28°.
Preliminary (PR) cohort: The PR cohort (n=55) contains the 28 patients from the end-results cohort; The patients had a Cobb angle of 33.9° (SD 6.6), Risser 0.7 (SD 0.9), age 12.4 years (SD 0.97). The characteristics were comparable to the end-result group alone.
Twenty three patients from this sample of 55 patients (41.8%) improved (>5°) while 3 patients (5.5%) reached or exceeded 50°. The Cobb angle was reduced to 30.6° after the follow-up period, the ATR had also reduced. Thoracic ATR reduced from 9.1° (SD 4.83) to 7° (SD 4.3) while the lumbar ATR was reduced from 5.9° (SD 4.2) to 3.2° (SD 3.1). Average brace wearing time as reported was 20.9 hrs/day (SD 2.8).
In-brace correction within this cohort was from 33.9 to 15.9° which makes an average correction of 52.7% (p<0.001). The results of both groups are summarized in Tables 1 and 2.
Table 1. Distribution of the results of the end-result cohort (ER) and the preliminary cohort (PR) with the success rate compared to the controls (BRAIST)11). As can be seen the result distribution of ER and PR are quite similar, as are the characteristics of the materials of both groups.
| Improved >5° | Stabilized | Progressed >5° | Reaching 50° | Success rate | |
| ER (n=28) | 11 | 13 | 4 | 2 | 92.9 % |
| PR (n=55) | 23 | 25 | 7 | 3 | 94.5% |
| BRAIST | 72% |
Table 2. The success rate of the end-result cohort (ER) and the preliminary cohort (PR) compared to the controls (BRAIST)11) with the help of the z-test. The differences were significant on p=0.01 level.
| Success rate | BRAIST (n=146) | t | Z | p | |
| ER (n=28) | 92.9 % | 72% | −3.42 | 2.58 | 0.01 |
| PR (n=55) | 94.5% | 72% | −4.67 | 2.58 | 0.01 |
DISCUSSION
Chêneau style braces seem to be effective in several cohorts, however, the results seem to vary significantly28,29,30,31,32,33,34,35,36,37,38). The first end-results study on Chêneau style bracing26) seems more effective than a later study from Germany33) and a more recent study from Poland35), the latter with a success rate of only 56%. This indicates that plaster based Chêneau braces vary in quality, possibly depending upon the skills of the present orthotist.
Differentiation in inclusion criteria may lead to variable results. In a study from Italy using the plaster based Chêneau brace a success rate of 100% has been reported20). In this study the average Cobb angle was less than 25° and only single curve patterns have been included, correcting much easier than combined curvatures (Lenke B and C type patterns)42).
A prospective controlled study with a homogenous patient group (Girls only, first signs of maturation, Risser 0, premenarchial) has been published comparing plaster based Chêneau braces with a soft brace23). In this study the success rate of the Chêneau brace was 80%.
In a retrospective paper including more recent Chêneau developments (Chêneau light, Gensingen brace), a success rate of 95% was reported28) while in another recent publication on the CAD/CAM Gensingen brace with a prospective design the success rate was around 90%31). When comparing the more recent results of Chêneau style braces with the Boston success rates, (72/70%)11, 22) the Chêneau style braces report better results than Boston braces. This fact has been confirmed in a recent study directly comparing both designs (Rigo-Chêneau)30).
In-brace correction and brace wearing time (compliance) directly determine the end-result18, 25). Historically in-brace correction has always been lower in the Boston braces than the correction as described for Chêneau derivates43). In a recent paper comparing a CAD Boston bracing with a CAD Chêneau design bracing, the in-brace correction using the Boston derivate was lower29).
Studies with low to moderate in-brace corrections show that at average, there might be a progression after weaning from the brace38), whilst in studies with higher in-brace corrections there may be improvements after brace weaning18, 44).
Aulisa and coworkers concluded43): Scoliotic curves did not deteriorate beyond their original curve size after bracing in both groups at the 15 year follow-up. These results are in contrast with the history of this pathology that normally shows a progressive and lowly increment of the curve at skeletal maturity. Bracing is an effective treatment method characterized by positive long-term outcomes, including for patients demonstrating moderate curves.
The in-brace correction in the preliminary, as well as in the end-result cohort, from this study using the GBW at average was >50%, while in the recent study with the Rigo-Chêneau brace correction was 31.5%, which was not different to the in-brace correction in the Boston brace sample from the same paper30). Despite this, the Rigo-Chêneau brace had better end-results. This fact might indicate that not only in-brace correction, but also other factors may influence the final result.
The success rate in the PR as well as in the ER cohort from this paper is exceeding 90% (Table 1). As the preliminary results are similar to end-results we can assume that at the end of growth there is no longer a great risk for progression, while patients are at reduced brace wearing times. This fact might influence the bracing strategy in a way that mild to moderate curves, the patient might not need to even be braced until their full skeletal maturity.
Interestingly, the results from a prospective cohort with curves of 40° and more was also significantly better than the results as achieved within the BRAIST trial31). Considering that there is little advantage of surgery over conservative treatment17) and in view of the lack of evidence for spinal fusion surgery12,13,14,15,16,17), the GBW offers a real advantage for those patients with curves beyond the historical surgical threshold31), who wish to avoid surgery.
Within the clinic of the first author, the location of the present study, between 200 and 250 patients have been provided braces every year. So, one might assume that there must be more than the relatively small number of patients in our study meeting the inclusion criteria. However, we have had many patients presenting after being braced elsewhere before, patients coming with curves exceeding 50°, patients with Risser stages >2, early onset scoliosis and patients with scoliosis of other cause. The third author was in charge to submit all patients complying with the inclusion criteria and eligible for the study to our prospective database. No patient or parent declined inclusion to the study. This shows that it is not easy to obtain big numbers of patients complying with the inclusion criteria as described.
When we look at outcomes of brace treatment the success mainly relies on the Cobb angle, which is a measure for the deviation of the spine in frontal plane, only. However, the Cobb angle alone in patients with AIS does not determine any severe health problems2,3,4, 45). This also has been confirmed in a more recent review46). Therefore, in modern brace treatment we should focus more on the cosmetic aspects of the deformity than on the Cobb angle. There is some evidence that even without a significant improvement of the Cobb angle, cosmetic changes are possible with modern Chêneau derivates31, 43, 47, 48). In a review focusing on clinical outcome parameters few papers have been found addressing cosmetic aspects48). In that paper it has been shown that trunk symmetry can be improved significantly48). In order to demonstrate the impact of bracing on clinical or cosmetic signs and symptoms of a scoliosis we would recommend an area of future research would be observing the ATR alongside the Cobb angle results (Figs. 5 and 6) as the radiologic development is not always the automatically most important clinical outcome for patients48, 49). It has been shown that even with an increase of the Cobb angle, an improvement of trunk symmetry has been achieved with an asymmetric Chêneau derivate49).
Within GBW cohorts there is a good compliance rate in patients initially with an average brace wearing time exceeding 20 hours per day, as reported by the patients and parents. Although the average brace wearing time in the control group (BRAIST study11)) has not been reported, it appears that brace wearing time was less in the controls than in GBW cohorts. As the compliance has been detected electronically in the BRAIST study11) this might be more precise than the reports of patients and parents in our groups. It is therefore possible that the brace wearing time is lower than reported in the present study. Nevertheless, the reduced brace wearing time when using the Boston brace may also be due to the lack of comfort. Also, the individual approach of the managing physician or orthotist may influence the brace compliance of the patient50).
The number of patients within our ER cohort (n=28) seems low which might be a shortcoming of the study. However, when adding the patients with a minimum follow-up of 18 months, a group of 55 patients remained, with similar results to the ER cohort alone. The PR cohort contains the ER cohort, but even though both groups are not significantly different, with respect to the success rate. This may strengthen the value of the results achieved to some extent, however a further larger number of patients with end-results would be required to determine this.
As the prospective cohort is followed up for a longer period, we would hope to explore this.
A shortcoming of this study is the relatively small cohort of patients with end-results and the study design (retrospective chart review of a prospective cohort). However, the promising results as obtained with this study suggest that the implementation of future studies with a higher level of evidence are indicated.
In conclusion: Preliminary and end-results as achieved with the GBW are significantly better than the results as achieved with the Boston brace. Other determinants; such as the quality and experience of the orthotist and the outcome of Cobb angle may also affect compliance and success of reported treatment. As outcomes are more successful with the GBW, general standards of bracing should be reviewed, to move from using symmetric compression, to asymmetric high correction braces allowing a standardized classification based corrective movement for most of the possible curve patterns.
Conflict of interest
HRW is receiving financial support for attending symposia and has received royalties from Koob GmbH & Co KG. The company is held by the spouse of HR Weiss. DT is employed with The London Orthotic Consultancy Ltd.—an orthotic company that manufacture and supply brace and orthotic products. None of the other authors report any competing interest or potential conflict of interest.
Acknowledgments
HRW provided the first draft and made the literature review. DT contributed to the improvement of the first draft and copyedited the final version. SS is responsible for the database and provided the XLS sheet in preparation of the statistical tests. AK (PhD in Mathematics) oversaw statistical testing. Parts of this paper have been presented previously: Weiss HR, Turnbull D, Seibel S, Kleban A, Tournavitis N. First end-result of a prospective cohort with AIS treated with the Gensingen brace. Proceedings of the 1st. International Conference on Scoliosis Management on behalf of the Turkish Scoliosis Society, April 12–13, 2019, Istanbul, Turkey.
REFERENCES
- 1.Winter RB: Classification and terminology. In: Lonstein JE, Bradford DS, Winter RB, Ogilvie JW, ed. Moe’s textbook of scoliosis and other spinal deformities, 3rd ed. hiladelphia: WB Saunders, 1995, pp 39–44. [Google Scholar]
- 2.Goldberg CJ, Moore DP, Fogarty EE, et al. : Adolescent idiopathic scoliosis: natural history and prognosis. Stud Health Technol Inform, 2002, 91: 59–63. [PubMed] [Google Scholar]
- 3.Asher MA, Burton DC: Adolescent idiopathic scoliosis: natural history and long term treatment effects. Scoliosis, 2006, 1: 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lonstein JE: Idiopathic scoliosis. In: Lonstein JE, Bradford DS, Winter RB, Ogilvie JW, ed. Moe’s textbook of scoliosis and other spinal deformities, 3rd ed. Philadelphia: WB Saunders, 1995, pp 219–256. [Google Scholar]
- 5.Deng M, Hui SC, Yu FW, et al. : MRI-based morphological evidence of spinal cord tethering predicts curve progression in adolescent idiopathic scoliosis. Spine J, 2015, 15: 1391–1401. [DOI] [PubMed] [Google Scholar]
- 6.Chu WC, Lam WW, Chan YL, et al. : Relative shortening and functional tethering of spinal cord in adolescent idiopathic scoliosis?: study with multiplanar reformat magnetic resonance imaging and somatosensory evoked potential. Spine, 2006, 31: E19–E25. [DOI] [PubMed] [Google Scholar]
- 7.Cobb J: Outline for the study of scoliosis. AAOS. Instr Course Lect, 1948, 5: 261–275. [Google Scholar]
- 8.Weiss HR, Weiss G, Petermann F: Incidence of curvature progression in idiopathic scoliosis patients treated with scoliosis in-patient rehabilitation (SIR): an age- and sex-matched controlled study. Pediatr Rehabil, 2003, 6: 23–30. [DOI] [PubMed] [Google Scholar]
- 9.Monticone M, Ambrosini E, Cazzaniga D, et al. : Active self-correction and task-oriented exercises reduce spinal deformity and improve quality of life in subjects with mild adolescent idiopathic scoliosis. Results of a randomised controlled trial. Eur Spine J, 2014, 23: 1204–1214. [DOI] [PubMed] [Google Scholar]
- 10.Kuru T, Yeldan İ, Dereli EE, et al. : The efficacy of three-dimensional Schroth exercises in adolescent idiopathic scoliosis: a randomised controlled clinical trial. Clin Rehabil, 2016, 30: 181–190. [DOI] [PubMed] [Google Scholar]
- 11.Weinstein SL, Dolan LA, Wright JG, et al. : Effects of bracing in adolescents with idiopathic scoliosis. N Engl J Med, 2013, 369: 1512–1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weiss HR, Goodall D: The treatment of adolescent idiopathic scoliosis (AIS) according to present evidence. A systematic review. Eur J Phys Rehabil Med, 2008, 44: 177–193. [PubMed] [Google Scholar]
- 13.Weiss HR, Moramarco M: Indication for surgical treatment in patients with adolescent Idiopathic Scoliosis—a critical appraisal. Patient Saf Surg, 2013, 7: 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bettany-Saltikov J, Weiss HR, Chockalingam N, et al. : A comparison of patient-reported outcome measures following different treatment approaches for adolescents with severe idiopathic scoliosis: a systematic review. Asian Spine J, 2016, 10: 1170–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cheuk DK, Wong V, Wraige E, et al. : Surgery for scoliosis in Duchenne muscular dystrophy. Cochrane Database Syst Rev, 2015, 10: CD005375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bettany-Saltikov J, Weiss HR, Chockalingam N, et al. : Surgical versus non-surgical interventions in people with adolescent idiopathic scoliosis. Cochrane Database Syst Rev, 2015, 4: CD010663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ward WT, Friel NA, Kenkre TS, et al. : SRS-22r scores in nonoperated adolescent idiopathic scoliosis patients with curves greater than forty degrees. Spine, 2017, 42: 1233–1240. [DOI] [PubMed] [Google Scholar]
- 18.Landauer F, Wimmer C, Behensky H: Estimating the final outcome of brace treatment for idiopathic thoracic scoliosis at 6-month follow-up. Pediatr Rehabil, 2003, 6: 201–207. [DOI] [PubMed] [Google Scholar]
- 19.Danielsson AJ, Hasserius R, Ohlin A, et al. : A prospective study of brace treatment versus observation alone in adolescent idiopathic scoliosis: a follow-up mean of 16 years after maturity. Spine, 2007, 32: 2198–2207. [DOI] [PubMed] [Google Scholar]
- 20.De Giorgi S, Piazzolla A, Tafuri S, et al. : Chêneau brace for adolescent idiopathic scoliosis: long-term results. Can it prevent surgery? Eur Spine J, 2013, 22: S815–S822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fang MQ, Wang C, Xiang GH, et al. : Long-term effects of the Chêneau brace on coronal and sagittal alignment in adolescent idiopathic scoliosis. J Neurosurg Spine, 2015, 23: 505–509. [DOI] [PubMed] [Google Scholar]
- 22.Nachemson AL, Peterson LE: Effectiveness of treatment with a brace in girls who have adolescent idiopathic scoliosis. A prospective, controlled study based on data from the Brace Study of the Scoliosis Research Society. J Bone Joint Surg Am, 1995, 77: 815–822. [DOI] [PubMed] [Google Scholar]
- 23.Weiss HR, Weiss GM: Brace treatment during pubertal growth spurt in girls with idiopathic scoliosis (IS): a prospective trial comparing two different concepts. Pediatr Rehabil, 2005, 8: 199–206. [DOI] [PubMed] [Google Scholar]
- 24.Rowe DE, Bernstein SM, Riddick MF, et al. : A meta-analysis of the efficacy of non-operative treatments for idiopathic scoliosis. J Bone Joint Surg Am, 1997, 79: 664–674. [DOI] [PubMed] [Google Scholar]
- 25.van den Bogaart M, van Royen BJ, Haanstra TM, et al. : Predictive factors for brace treatment outcome in adolescent idiopathic scoliosis: a best-evidence synthesis. Eur Spine J, 2019, 28: 511–525. [DOI] [PubMed] [Google Scholar]
- 26.Hopf C, Heine J: [Long-term results of the conservative treatment of scoliosis using the Chêneau brace]. Z Orthop Ihre Grenzgeb, 1985, 123: 312–322 (in German). [DOI] [PubMed] [Google Scholar]
- 27.Heine J, Götze HG: [Final results of the conservative treatment of scoliosis using the Milwaukee brace]. Z Orthop Ihre Grenzgeb, 1985, 123: 323–337 (in German). [DOI] [PubMed] [Google Scholar]
- 28.Weiss HR, Werkmann M: Rate of surgery in a sample of patients fulfilling the SRS inclusion criteria treated with a Chêneau brace of actual standard. Stud Health Technol Inform, 2012, 176: 407–410. [PubMed] [Google Scholar]
- 29.Weiss HR, Kleban A: Development of CAD/CAM based brace models for the treatment of patients with scoliosis-classification based approach versus finite element modelling. Asian Spine J, 2015, 9: 661–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Minsk MK, Venuti KD, Daumit GL, et al. : Effectiveness of the Rigo Chêneau versus Boston-style orthoses for adolescent idiopathic scoliosis: a retrospective study. Scoliosis Spinal Disord, 2017, 12: 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Weiss HR, Tournavitis N, Seibel S, et al. : A prospective cohort study of AIS patients with 40° and more treated with a Gensingen Brace (GBW): preliminary results. Open Orthop J, 2017, 11: 1558–1567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Weiss HR, Rigo M, Chêneau J: Praxis der Chêneau-Korsettversorgung in der Skoliosetherapie. Georg Thieme Verlag, Stuttgart, 2000. [Google Scholar]
- 33.Bullmann V, Halm HF, Lerner T, et al. : [Prospective evaluation of braces as treatment in idiopathic scoliosis]. Z Orthop Ihre Grenzgeb, 2004, 142: 403–409. [DOI] [PubMed] [Google Scholar]
- 34.Pham VM, Herbaux B, Schill A, et al. : [Evaluation of the Cheneau brace in adolescent idiopathic scoliosis]. Annales de readaptation et de medecine physique: revue scientifique de la Societe francaise de reeducation fonctionnelle de readaptation et de medecine physique. 2007, 50: 125–133. [DOI] [PubMed] [Google Scholar]
- 35.Zaborowska-Sapeta K, Kowalski IM, Kotwicki T, et al. : Effectiveness of Chêneau brace treatment for idiopathic scoliosis: prospective study in 79 patients followed to skeletal maturity. Scoliosis, 2011, 6: 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Matussek J, Dingeldey E, Benditz A, et al. : [Conservative treatment of idiopathic scoliosis: influence of archetypical Cheneau-Corsets on trunk asymmetry]. Orthopade, 2015, 44: 869–878. [DOI] [PubMed] [Google Scholar]
- 37.Taghi Karimi M, Rabczuk T, Kavyani M: Evaluation of the efficiency of the Chêneau brace on scoliosis deformity: a systematic review of the literature. Orthopade, 2018, 47: 198–204. [DOI] [PubMed] [Google Scholar]
- 38.Korovessis P, Syrimpeis V, Tsekouras V, et al. : Effect of the Chêneau brace in the natural history of moderate adolescent idiopathic scoliosis in girls: cohort analysis of a selected homogenous population of 100 consecutive skeletally immature patients. Spine Deform, 2018, 6: 514–522. [DOI] [PubMed] [Google Scholar]
- 39.Weiss HR: “Brace technology” thematic series—The Gensingen brace (TM) in the treatment of scoliosis. Scoliosis, 2010, 5: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Weiss HR, Tournavitis N, Nan X, et al. : Workflow of CAD / CAM scoliosis brace adjustment in preparation using 3D printing. Open Med Inform J, 2017, 11: 44–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Goldberg CJ, Moore DP, Fogarty EE, et al. : Adolescent idiopathic scoliosis: the effect of brace treatment on the incidence of surgery. Spine, 2001, 26: 42–47. [DOI] [PubMed] [Google Scholar]
- 42.Lenke LG, Betz RR, Harms J, et al. : Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am, 2001, 83: 1169–1181. [PubMed] [Google Scholar]
- 43.Weiss HR, Lehnert-Schroth C, Moramarco M, et al. : Advancements in conservative scoliosis treatment. Saarbruecken: Lambert Academic Publishing, 2015. [Google Scholar]
- 44.Aulisa AG, Guzzanti V, Falciglia F, et al. : Curve progression after long-term brace treatment in adolescent idiopathic scoliosis: comparative results between over and under 30 Cobb degrees—SOSORT 2017 award winner. Scoliosis Spinal Disord, 2017, 12: 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Weinstein SL, Dolan LA, Spratt KF, et al. : Health and function of patients with untreated idiopathic scoliosis: a 50-year natural history study. JAMA, 2003, 289: 559–567. [DOI] [PubMed] [Google Scholar]
- 46.Weiss HR, Karavidas N, Moramarco M, et al. : Long-term effects of untreated adolescent idiopathic scoliosis: a review of the literature. Asian Spine J, 2016, 10: 1163–1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Weiss HR: Bracing can lead to a persistent correction in the treatment of adolescent idiopathic scoliosis: a case report. Hard Tissue, 2014, 3: 8. [Google Scholar]
- 48.Weiss HR, Moramarco M: Remodelling of trunk and backshape deformities in patients with scoliosis using standardized asymmetric computer-aided design/computer-aided manufacturing braces. Hard Tissue, 2013, 2: 14. [Google Scholar]
- 49.Weiss HR: Clinical improvement and radiological progression in a girl with early onset scoliosis (EOS) treated conservatively–a case report. Scoliosis. 2006, 1: 07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Freidel K, Reichel D, Steiner A, et al. : Idiopathic scoliosis and quality of life. Stud Health Technol Inform, 2002, 88: 24–29. [PubMed] [Google Scholar]