Abstract
[Purpose] The purposes of this case study are to: (1) report the immediate effects of knee flexion range of motion following manual therapy (MT) and self-stretching/AROM following a total knee arthroplasty (TKA). (2) contribute empirical evidence to the literature through reports within this case study. [Participant and Methods] For 6 days, the authors utilized a different MT technique and 1 day of self-stretching and active range of motion for an 85-year-old male who was 3 days status post right TKA. [Results] The greatest gains for AROM/PROM for knee flexion were achieved while performing typical arthrokinematic motion joint mobilizations, for AROM and PROM, resulting in a gain of 10 degrees and 10 degrees, respectfully. [Conclusion] We theorize that performing typical arthrokinematic motion joint mobilizations stimulates a greater response from the mechanoreceptors and therefore a greater stimulation response to the central and peripheral nervous systems. This greater stimulation may explain the greatest immediate gain in knee flexion range of motion being performed by typical arthrokinematic motion joint mobilizations. The outcomes of this study demonstrate the start of some empirical evidence while exploring the immediate effects of knee flexion range of motion following manual therapy and self-stretching/AROM following a TKA.
Key words: Manual therapy, Knee
INTRODUCTION
Osteoarthritis (OA) is the most frequent cause of disability among adults in the United States (U.S.) and is the leading indication for joint replacement procedures1). The joints most commonly affected are the knees, hips, hands and spine1). Data that has been reviewed from 2013 to 2015, reports that there are over 54 million people over the age of 18 that have self reported doctor diagnosed arthritis and over 23 million who have activity limitations due to arthritis2). Symptomatic knee OA is expected to be a risk for almost 1 in 2 people over the age of 85, as reported by the Johnston County Osteoarthritis project1). The number of adults in the U.S. with arthritis is expected to reach 67 million by the year 20303).
Total Knee Arthroplasties (TKAs) were first widely performed in the 1970s and 1980s and are now regarded as an effective treatment for end-stage knee arthritis3). More than 650,000 TKA surgeries were performed in the U.S. in 2008 and have been increasing every year3). In 2009 over 900,000 knee and hip replacements were performed accounting for more than 42 billion dollars4). Following a TKA patients often report knee stiffness, limited range of motion (ROM), pain, and decreased function4).
Manual therapy (MT) has been reported to likely work through biomechanical and/or neurophysiological mechanisms5). MT techniques include joint mobilizations, myofascial releases (MFR), stretching, scar mobilizations, soft tissue mobilizations (STM), and muscle energy techniques (METs)6). Joint mobilizations are most commonly used to treat joint hypomobility6). MFR is a graded stretch to tissue by the therapist that is guided by feedback from the patient’s body to determine stretch direction, force, and duration to address soft tissue restrictions6, 7). Stretching, specifically static stretching, is performed for a period of 15–20 seconds to increase flexibility and to improve the range of motion of joints8). Scar mobilizations helps reorganize scar tissue so that collagen fibers are softened and flattened which ultimately assists with the prevention of hypertropic scarring9). STMs are also used to promote changes in the myofascial network by the use of manual forces6, 10). METs are used as a direct treatment in which a patient’s muscles are actively contracting, in a specific position, against a Physical Therapist’s counter force6).
There is currently no evidence found by the authors, from an extended literature review, that reports the immediate effects of knee flexion range of motion following MT or self-stretching/active range of motion (AROM) 3 days following a TKA. The purposes of this case study are to: (1) report the immediate effects of knee flexion range of motion following MT and self-stretching/AROM following a TKA. (2) contribute empirical evidence to the literature through reports within this case study.
PARTICIPANT AND METHODS
This case study included an 85-year-old male participant who was admitted to the hospital for a right elective TKA secondary to degenerative OA. The participant was transferred to the transitional care unit 3 days later for sub-acute rehabilitation and was weight bearing as tolerated on the right lower extremity. The participant’s past medical history was remarkable for hypertension, benign prostatic hyperplasia, atrial fibrillation, mitral valve prolapse, and a left TKA.
The participant (N=1) was taken from a sample of convenience from the transitional care unit. Interventions that were selected and performed were randomized. The independent variable was the type of intervention performed and the dependent variable is the outcome of knee flexion range of motion. Written informed consent from the participant was obtained prior to the study.
The participant received pain medication approximately 30 minutes prior to the scheduled session each day. The participant ambulated the same distance each day to our gymnasium where he was instructed to lie supine on the standard Hi Lo table. Each intervention was performed at the barrier of motion (end range of joint motion). Each intervention was performed for the first 15 minutes of the participant’s treatment session that was monitored with a digital timer by the Physical Therapist.
A 12 inch hand held goniometer was used to measure active range of motion (AROM) and passive range of motion (PROM) before and after each intervention. Mild pressure was applied to the lateral knee to palpate and identify the lateral femoral condyle through the participant’s pitting edema. A black washable marker was used to mark the lateral femoral condyle to maintain consistent placement of the fulcum for the measurements of knee flexion for before and after each intervention. A sterile, 70% isopropyl alcohol prep pad was used at the end of session to clean the black mark from the skin. This process was repeated in the same manner each day.
This study was conducted in accordance with the Declaration of Helsinki 1964 and sufficient informed consent was obtained from the patient, paying attention to the Health Insurance Portability and Accountability Act (HIPAA) of 1996.
RESULTS
The results of AROM before, AROM after, and AROM gains are displayed in Table 1. The results of PROM before, PROM after, and PROM gains are displayed in Table 2. The greatest gains for AROM/PROM for knee flexion were achieved while performing typical arthrokinematic motion joint mobilizations, for AROM and PROM, resulting in a gain of 10 degrees and 10 degrees, respectfully.
Table 1. Results of AROM before/after intervention and AROM gains (measured in degrees).
| Day of intervention | Technique | AROM before | AROM after | Gain |
| 1 | Direct STM | 80 | 88 | 8 |
| 2 | Joint mobilization – Typical arthro | 85 | 95 | 10 |
| 3 | Superficial MFR | 88 | 94 | 6 |
| 4 | Joint mobilization - Atypical-arthro | 87 | 95 | 8 |
| 5 | Peri-scar mobilization | 87 | 92 | 5 |
| 6 | MET | 94 | 100 | 6 |
| 7 | Self-stretch/AROM | 100 | 104 | 4 |
Table 2. Results of PROM before/after intervention and PROM gains (measured in degrees).
| Day of intervention | Technique | PROM before | PROM after | Gain |
| 1 | Direct STM | 88 | 94 | 6 |
| 2 | Joint mobilization – Typical arthro | 89 | 99 | 10 |
| 3 | Superficial MFR | 93 | 97 | 4 |
| 4 | Joint mobilization - Atypical-arthro | 92 | 99 | 7 |
| 5 | Peri-scar mobilization | 92 | 100 | 8 |
| 6 | MET | 98 | 104 | 6 |
| 7 | Self-stretch/AROM | 104 | 107 | 3 |
DISCUSSION
The greatest gains for AROM/PROM for knee flexion were achieved while performing typical arthrokinematic motion joint mobilizations, for AROM and PROM, resulting in a gain of 10 degrees and 10 degrees, respectfully. Since there was only a sample size of 1 (N=1), no other statistical tests were performed.
Joint mobilization is one of the techniques that is used in manual therapy that may be used to mechanically elongate connective tissues and to fire muscle and joint receptors6). The significance of using joint mobilization is to modulate pain and increase range of motion (ROM)11, 12). This is done by the stimulation of mechanoreceptor activation for modification of nociceptor-generated pain impulse transmission12). This stimulation therefore inhibits the nociceptive input to the central nervous system12).
In a synovial joint, there are four types of afferent nerve that sends signals into the central nervous system; Ruffini endings (REs), Pacinian corpuscles (PCs), Golgi ligament endings (GLEs), and free nerve endings12, 15). REs, PCs, and GLEs are mechanoreceptors where they carry different signals to the brain12). REs are slow afferent fibers that generate impulses at rest and during movement12, 15). Their role is to maintain muscle tone and awareness while the joint is in a static position and are located in the superficial layers of all joint capsule12, 15). PCs are activated by the “velocity of joint motion at the beginning and end of displacement” and are known to be a high velocity mechanoreceptors12, 15). PCs located in the inner layers of fibrous capsules and fat pads and are inactive when the joint is immobilized12, 15). GLEs convey information about ligament tension and proprioception12, 15). Free nerve endings are nociceptors that are in the joint capsules, ligament, fat pads, and walls of the blood vessels which are not active during joint mobilizations12, 15).
In our case study we will recognize that all interventions that were performed increased mechanoreceptors responses due to an increase in knee flexion AROM/PROM. We theorize that since the joint capsule of the knee is removed surgery this will result in a compensatory increase in responses from the REs and GLEs into the nervous system. We theorize that performing typical arthrokinematic motion joint mobilizations stimulates a greater response from the mechanoreceptors, specifically the REs and GLEs, and therefore a greater stimulation response to the central and peripheral nervous systems. This greater stimulation may explain the greatest immediate gain in knee flexion range of motion being performed by typical arthrokinematic motion joint mobilizations.
To minimize potential error in regards to range of motion testing, the same Physical Therapist measured knee flexion before and after each intervention. In a study by Pandya et al., they reported when goniometric measurements are performed by the same examiner, they provide a good objective measure to document progression of disease and evaluate results of treatment to reduce tightness, as evidenced by an intra-tester reliability values of ICC= 0.81 to 0.9413).
Three limitations were identified in this study. First, the skill of the therapist applying the techniques will affect the results of the treatment1). Second, due to our low sample size (N=1), the authors cannot generalize the results for populations following a TKA. Lastly, this study did not control for rater bias. The Physical Therapist who was the rater knew the purpose of the study, performed the interventions, and measured ROM every day for the participant.
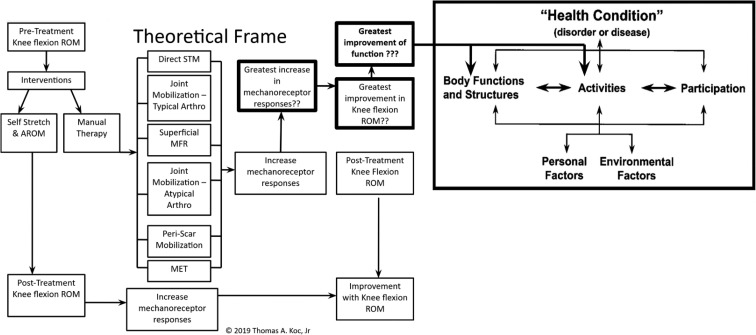
It has been reported by Xu et al., that joint mobilizations for TKAs are important to promote the fast and efficient recovery for patients and to reduce economic expenditures11). The conclusions by these authors and our study may also be integrated into the International Classification of Functioning, Disability, and Health (ICF) model14) (Fig. 1). By utilizing joint mobilizations for a participant with a TKA may assist with improving range of motion and improving activities such as bed mobility, transfers and ambulation as linked to the ICF’s Body Functions and Structures and Activities categories, respectfully.
Fig. 1.
Knee intervention theoretical framework with integration with International Classification of Functioning, Disability, and Health (ICF) model14).
The outcomes of this study demonstrate the start of some empirical evidence while exploring the immediate effects of knee flexion range of motion following manual therapy and self-stretching/AROM following a TKA. While the findings in the present study do not demonstrate treatment efficacy due to the case study design, the findings are encouraging and supportive of future investigation of the immediate effects of knee flexion range of motion following manual therapy and self-stretching/AROM following a TKA. Further studies are needed to test this methodology on a larger sample size to determine whether or not these techniques may be used on a similar population.
Funding
There was no funding provided for this study.
Conflict of interest
The authors declare that there is no conflict of interest.
REFERENCES
- 1.Murphy L, Helmick CG: The impact of osteoarthritis in the United States: a population-health perspective: a population-based review of the fourth most common cause of hospitalization in U.S. adults. Orthop Nurs, 2012, 31: 85–91. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. https://www.cdc.gov/arthritis/data_statistics/national-statistics.html Updated February 7, 2018. Accessed Nov. 13, 2018.
- 3.Van Manen MD, Nace J, Mont MA: Management of primary knee osteoarthritis and indications for total knee arthroplasty for general practitioners. J Am Osteopath Assoc, 2012, 112: 709–715. [PubMed] [Google Scholar]
- 4.Kim J, Nelson CL, Lotke PA: Stiffness after total knee arthroplasty. Prevalence of the complication and outcomes of revision. J Bone Joint Surg Am, 2004, 86: 1479–1484. [PubMed] [Google Scholar]
- 5.Bialosky JE, Bishop MD, Price DD, et al. : The mechanisms of manual therapy in the treatment of musculoskeletal pain: a comprehensive model. Man Ther, 2009, 14: 531–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wise CH: Orthopaedic manual physical therapy: from art to evidence. Philadelphia: F.A. Davis Company, 2015. [Google Scholar]
- 7.McKenney K, Elder AS, Elder C, et al. : Myofascial release as a treatment for orthopaedic conditions: a systematic review. J Athl Train, 2013, 48: 522–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Page P: Current concepts in muscle stretching for exercise and rehabilitation. Int J Sports Phys Ther, 2012, 7: 109–119. [PMC free article] [PubMed] [Google Scholar]
- 9.Edwards J: Scar management. Nurs Stand, 2003, 17: 39–42. [DOI] [PubMed] [Google Scholar]
- 10.Godges JJ, Mattson-Bell M, Thorpe D, et al. : The immediate effects of soft tissue mobilization with proprioceptive neuromuscular facilitation on glenohumeral external rotation and overhead reach. J Orthop Sports Phys Ther, 2003, 33: 713–718. [DOI] [PubMed] [Google Scholar]
- 11.Xu J, Zhang J, Wang XQ, et al. : Effect of joint mobilization techniques for primary total knee arthroplasty: study protocol for a randomized controlled trial. Medicine (Baltimore), 2017, 96: e8827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kaminski TW, Kahanov L, Kato M: Therapeutic effect of joint mobilization: joint mechanoreceptors and nociceptors. Athl Ther Today, 2007, 12: 28–31. [Google Scholar]
- 13.Pandya S, Florence JM, King WM, et al. : Reliability of goniometric measurements in patients with Duchenne muscular dystrophy. Phys Ther, 1985, 65: 1339–1342. [DOI] [PubMed] [Google Scholar]
- 14.International Classification of Functioning: Disability and Health (ICF) framework to facilitate Interprofessional education and collaborative practice. World Health Organization. http://www.who.int/hrh/news/2014/hrh_icf_framework/en/. Published Oct. 13, 2014. Accessed Nov. 13, 2018.
- 15.Wyke B. Neurol Joints, 1967, 41: 25–50. [PMC free article] [PubMed] [Google Scholar]