Abstract
Objectives. To contrast the geographic distribution of fentanyl-involved and non–fentanyl-involved fatal overdoses between 2014 and 2018 in Cook County, Illinois.
Methods. We conducted a spatial analysis using locations of fentanyl-involved fatal overdoses (n = 1433) compared with nonfentanyl opioid and polydrug fatal overdoses (n = 1838) collected through the Cook County Medical Examiner’s Office from 2014 to 2018. We also used logistic regression to test significant individual- and neighborhood-level covariates.
Results. Fentanyl overdoses geographically clustered more than nonfentanyl overdoses, and this difference was statistically significant. One area in particular showed significantly elevated risk for fentanyl overdoses (P < .05) located in 2 specific neighborhoods of Chicago. The odds of a fentanyl-involved overdose were significantly increased for men, Blacks, Latinos/as, and younger individuals. Neighborhood deprivation score was the only significant neighborhood-level predictor (odds ratio = 1.11; 95% confidence interval = 1.07, 1.17).
Conclusions. Fentanyl-involved fatal overdoses follow a distinct geographic distribution associated with resource deprivation in neighborhoods where they occur. This suggests an evolving bifurcated drug market, with drug markets in resource-deprived neighborhoods disproportionately likely to include fentanyl.
Illicitly manufactured fentanyl and fentanyl analogs have become increasingly prevalent in the US drug market. The Drug Enforcement Administration’s National Forensic Laboratory Information System reported that the number of seized drug samples testing positive for fentanyl more than doubled from 2015 to 2016, rising from 14 440 to 34 119; this increase continued into 2017, with an estimated 25 460 reports in the first 6 months of 2017 alone.1,2 Potency of fentanyl and fentanyl analogs has also increased.3 Much of this illicit fentanyl has been mixed with heroin as fentanyl powder is similar in appearance to white powder heroin.4 Fentanyl has also been combined increasingly with illicit drugs other than heroin, including cocaine; Drug Enforcement Administration laboratories in Pennsylvania detected a 112% increase in fentanyl-adulterated cocaine samples from 2016 to 2017.4,5 Fentanyl is increasingly found in counterfeit medications: fentanyl was present in 89% of seized counterfeit OxyContin tablets in Canada, and fentanyl has been found in counterfeit Xanax (alprazolam), Norco (acetaminophen–hydrocodone), and other medications in the United States.4,6
This influx of illicitly produced fentanyl in the US drug market has contributed to a significant increase in the number of overdose deaths attributable to synthetic opioids since 2013.7,8 Synthetic opioid-involved deaths in 2016 accounted for 30.5% of all drug overdose deaths and 45.9% of all opioid-involved deaths, with a 100% increase in the rate of these deaths from 2015.9 More than 55% of opioid overdose deaths occurring nationally in 2017 involved synthetic opioids, accounting for more than 27 000 overdose deaths and exceeding the total number of all opioid overdose deaths in 2013, when deaths involving synthetic opioids first began to rise.4
While some people who use drugs seek out fentanyl and fentanyl-adulterated drugs, there is evidence that many people who consume fentanyl may be unaware they are consuming fentanyl or may prefer not to use fentanyl but find it unavoidable.10,11 There is a lack of consensus as to why fentanyl is being incorporated into illicit street drugs at such high rates, especially considering that fentanyl is lethal at much lower doses than other opioids and is significantly more potent by weight compared with heroin.12 One theory is that fentanyl is significantly cheaper to produce than heroin as heroin costs approximately $65 000 per kilogram wholesale whereas illicit fentanyl is available at roughly $3500 per kilogram.6 As a consequence, drug dealers may be incentivized to incorporate fentanyl into their products to reduce costs and increase profits despite the public health risks. Fentanyl also increases the addictiveness of the drugs with which it is combined, including nonopioids such as cocaine, resulting in increasing drug usage frequency.13 There is some speculation that these market forces could result in 2 drug markets analogous to the crack and cocaine drug markets of the 1980s,14 with poorer people who use drugs priced out of access to pure heroin or cocaine.
Examining trends in the geographic distribution of fentanyl-involved overdoses may shed light on any patterns in fentanyl availability and the evolving bifurcation of different opioid markets. If fentanyl and fentanyl-adulterated drugs are targeted to areas where people who use drugs are unable to afford higher drug prices or larger drug quantities of unadulterated drugs, then we would expect to see more fentanyl in poorer or more resource-deprived neighborhoods. There has been little discussion on the pattern of fentanyl distribution—whether it follows a similar distribution to other drugs, particularly drugs it is mixed with, or if a unique set of geographic and social factors influence fentanyl use and related overdoses. Identifying areas with more fentanyl may also target areas for lay naloxone administration15 and fentanyl test strip availability,12 as well as identify new harm-reduction strategies. The purpose of this study was to examine geographic trends in the distribution of fentanyl-involved overdose deaths and discern if fentanyl-involved overdoses follow a bifurcated geographic distribution independent of other overdose deaths.
METHODS
The Columbia University Medical Center institutional review board waived review of this study.
Data Sources
The Cook County Medical Examiner’s Office provides information on all deaths that fall under the jurisdiction of the medical examiner or are reported to the medical examiner in Cook County, Illinois, and qualify for further investigation. Cook County is the second most populous county in the United States (population: 5 180 493) and includes Chicago and the surrounding suburbs.16 These data include full toxicology reports and Global Positioning System (GPS) coordinates for where the overdose occurred (the location of injury). Data are publicly available for download and updated regularly.17 Data included in this analysis were from August 1, 2014, to August 15, 2018.
We grouped all records indicating a derivative of fentanyl or fentanyl metabolite (e.g., fentanyl, carfentanil, 4-ANPP,3 U-477008) as the primary cause of death (n = 1433; Table 1) using text-based identification of drug involvement.18 Records that listed an illicit or prescription opioid (e.g., heroin, oxycodone, codeine, morphine) or a substance that was listed as part of a fentanyl-involved overdose (e.g., cocaine, LSD, methamphetamine, MDMA) but that did not include fentanyl as part of a polydrug overdose served as a comparison group (n = 1838; see Figure A for overdose categorization available as a supplement to the online version of this article at http://www.ajph.org).
TABLE 1—
Description of Fentanyl-Involved Fatal Overdoses and Nonfentanyl Opioid and Polydrug Fatal Overdose Comparisons: Cook County, Illinois, August 1, 2014, to August 15, 2018
| Fentanyl-Involveda Fatal Overdoses (n = 1433) | Nonfentanyl Opioid and Polydrugb Fatal Overdoses (n = 1838) | |
| Individual-level covariates | ||
| Age, y, mean ±SD | 43.1 ±12.5 | 44.2 ±12.6 |
| Race/ethnicity, no. (%) | ||
| Non-Latino/a Black | 619 (43.2) | 666 (36.2) |
| Non-Latino/a White | 616 (43.0) | 966 (52.6) |
| Latino/a | 185 (12.9) | 170 (9.2) |
| Other | 13 (0.9) | 36 (2.0) |
| Gender, no. (%) | ||
| Male | 1114 (77.7) | 1343 (73.1) |
| Female | 319 (22.3) | 495 (26.9) |
| Neighborhood-level covariates | ||
| Household income in $10 000s, median ±SD | 4.79 ±2.76 | 5.08 ±2.82 |
| Neighborhood deprivation score | ||
| Mean ±SD | −0.04 ±1.84 | −0.45 ±1.81 |
| Low (range = −5.00–0.00), no. (%) | 715 (49.9) | 1123 (61.1) |
| Moderate (range = 0.01–1.00), no. (%) | 252 (17.6) | 266 (14.5) |
| High (range = 1.01–5.00), no. (%) | 466 (32.5) | 449 (24.4) |
| Index of Concentration at the Extremes, range = −1 to +1, mean ±SD | −0.11 ±0.74 | 0.07 ±0.73 |
| Population density per square mile in 1000s, mean ±SD | 16.4 ±23.0 | 15.3 ±13.1 |
Substances used, identified in medical examiner toxicity screen as primary cause of death, were fentanyl and fentanyl metabolites, carfentanil, 4-ANPP, and U-47700, alone or in combination with drugs listed in footnote b.
Substances used, identified in medical examiner toxicity screen as primary cause of death, were opioids (heroin, codeine, methadone, morphine, hydrocodone, tramadol, oxycodone, oxymorphone, buprenorphine, mitragynine, opioid, opiate) and nonopioids (cocaine, amphetamine, methamphetamine, lysergic acid diethylamide [LSD], 3-fluorophenmetrazine [3-FPM], methylenedioxyamphetamine [MDA], methylenedioxymethamphetamine [MDMA], 7-aminoclonazepam, clonazepam [Klonopin], delorazepam, diazepam [Valium], diclazepam, etizolam, lorazepam [Ativan], midazolam [Versed], nordiazepam, and temazepam [Restoril]).
We excluded suicides and homicides from this analysis, as well as deaths in which opioid use was a secondary contributing factor (e.g., a person who died of chronic obstructive pulmonary disease but also had opioids in his or her system would be excluded because the primary cause of death was not accidental drug overdose). Demographic information included age, gender, and 2 racial/ethnic categories with a separate designation for Latino/a. We recoded race/ethnicity into 1 racial/ethnic category with non-Latino/a White, non-Latino/a Black, Latino/a, and other (combining Asian, American Indian, “other,” and “unknown”).
We took neighborhood demographic variables for each census block group in Cook County, including population totals and median household income, from 5-year American Community Survey (ACS) estimates for each year of overdose data (e.g., we paired 2014 ACS estimates with 2014 fatal overdoses).16 Because 2018 ACS estimates were not yet available at the time of data analysis, we assigned overdoses 2017 ACS values. We calculated population density by taking the total population of each census block group and dividing by the area of the census block group in square miles.
Measures
Previous research has demonstrated the importance of neighborhood context in risk for drug use19 and drug overdose.20 To provide a window into the broader neighborhood context not fully explained by demographics, we calculated the neighborhood disadvantage score by using census block group-level items from ACS as described previously. The items used to create the index included the percentages of (1) adults aged 25 years or older with a college degree, (2) owner-occupied housing, (3) households with incomes below the federal poverty threshold, and (4) female-headed households with children. We used Ross and Mirowsky’s21 formula to generate the index: {[(c/10+d/10)–(a/10+b/10)]/4} (percentages are entered as whole numbers, not decimals). Each 1-unit increase in the neighborhood disadvantage score is equivalent to an increase of 10 percentage points for each component item of the index.21 The total score has a possible range from −5 to +5, where −5 is very low or little disadvantage, and +5 is very severe disadvantage. This metric has been used in previous investigations examining the relationships between neighborhoods, mental health, and risk factors for heavy drinking and violent crime.22,23
We assessed the level of Black–White segregation in Cook County census block groups by using the Index of Concentration at the Extremes (ICE).24 We subtracted the number of Blacks from the number of Whites in a block group, and then divided by the entire population of the block group. The values range from −1 to +1, where −1 is 100% Black, 0 is 50% Black and 50% White, and +1 is 100% White. Whereas other measures of community-level racial segregation only give information about whether segregation exists, the ICE measure quantifies the polarization by group and considers majority-White and majority-Black communities to be qualitatively different.24
Data Analyses
We imported all overdoses with GPS coordinates (n = 3271) into ArcGIS 10.6 (ESRI, Redlands, CA) and mapped them. We used the spatial join tool in ArcGIS to identify the census block group where each overdose took place and assigned the corresponding census block group measures (e.g., neighborhood disadvantage score, population density) to the overdose.
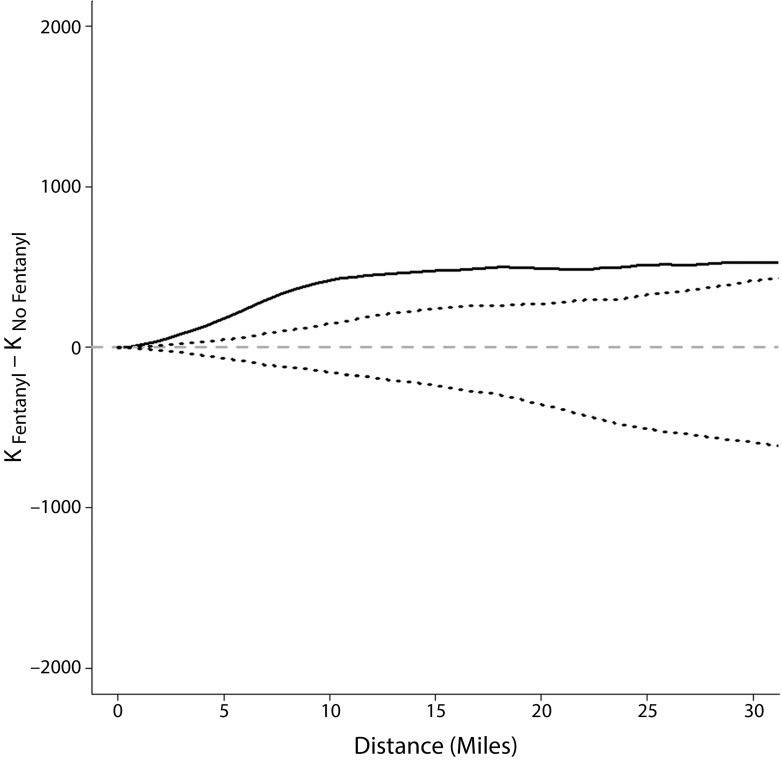
To evaluate the global property of clustering in the data, we compared the K functions for the 2 groups in R 3.4.1 (R Foundation for Statistical Computing, Vienna, Austria; see Appendix A for sample R code). Clustering occurs when event locations tend to be near other event locations. If there was no difference in where fatal fentanyl overdoses occurred compared with fatal opioid overdoses in general, we would expect to see no significant difference when we compared the K functions for the 2 groups.25 If the difference is within the banded region (similar to a confidence interval, designated by dashed lines in Figure 1), we would fail to reject the null hypothesis of no significant difference between where fentanyl and nonfentanyl fatal overdoses occur. When the difference function is above the upper limit, fentanyl overdoses exhibit more clustering than nonfentanyl overdoses, and if the function is under the lower limit, the nonfentanyl overdoses are more clustered than fentanyl overdoses. We calculated the difference in K functions for all study years combined (2014–2018) and each year individually to assess temporal shifts in clustering related to the recent introduction of fentanyl into the drug marketplace.
FIGURE 1—
Difference in Fentanyl and Nonfentanyl Overdoses K Functions With Confidence Bands (Dashed) and Distance in Miles: Cook County, Illinois, 2014–2018
Note. Solid line indicates differences; dashed lines indicate confidence intervals, within which the null hypothesis would not be rejected.
We mapped kernel intensity estimates to assess geographic variability in fentanyl overdoses and nonfentanyl opioid overdoses and then mapped the kernel ratio function to assess the spatial variation in risk—the property that the risk or “odds” of an event occurring varies geographically.25 This is a nonparametric tool that maps the ratio of intensity of fentanyl overdoses to intensity of nonfentanyl overdoses and may identify areas of elevated risk for fentanyl overdose.25 We then calculated a log ratio of kernel intensity functions for fentanyl and nonfentanyl overdoses to get a log relative risk surface and used Monte Carlo randomization of the fentanyl group labels (i.e., we randomized which location was designated a fentanyl overdose vs a nonfentanyl overdose) to detect significant local differences in fentanyl and nonfentanyl overdose intensities. This method maps the significant areas of log relative risk at a P level of less than .05.25 We mapped all years combined and each year individually to assess temporal changes in relative risk for fentanyl-involved overdoses.
Finally, we used logistic regression to assess possible individual- and neighborhood-level correlates of fentanyl-involved overdose. We first assessed the univariable relationship between odds of a fentanyl-involved overdose and each covariate of interest separately. We then assessed covariates that were significant in univariable analysis (at P < .05) in the multivariable model. As this method does not account for spatial variation in fentanyl and nonfentanyl overdoses, we calculated spatial semivariograms to detect residual spatial variation not accounted for by the covariates for each model.25 To select the best fitting and most parsimonious model, we calculated Akaike’s information criterion and checked for multicollinearity by using variance inflation factors.25 The final multivariable model presented here represents the most parsimonious model according to these criteria.
We then used geographically weighted regression (GWR) to further investigate the spatial variation of covariates at overdose locations. Unlike logistic regression, GWR does not assume that the relationship between covariates and the outcome of interest is consistent—or stationary—across the study area. Rather, GWR assesses whether the relationships between a set of covariates and an outcome vary by geographic location as the fitted coefficient values of a global logistic regression model may not represent detailed local variations in the data sufficiently.26 GWR constructs a separate logistic regression equation for every location in the data set, which incorporates the dependent and independent variables of locations falling within the bandwidth of each overdose location. While GWR has some limitations, such as multicollinearity27 and approaches to calculating goodness-of-fit statistics,28 it is a useful tool for investigating spatial nonstationarity and is used here as a sensitivity analysis to determine if further inquiry into spatial variation of fentanyl overdose deaths is warranted.
RESULTS
Table 1 presents a description of fentanyl-involved fatal overdoses and nonfentanyl opioid fatal overdoses, including substances used by both groups. A larger proportion of nonfentanyl overdoses were White (nonfentanyl: n = 966; 52.6% vs fentanyl: n = 616; 43.0%) while a larger proportion of fentanyl overdoses were men (fentanyl: n = 1114; 77.7% vs nonfentanyl: n = 1343; 73.1%). Age distribution was similar for both groups. A larger proportion of nonfentanyl overdoses occurred in neighborhoods with low neighborhood deprivation (nonfentanyl: n = 1123; 61.1% vs fentanyl: n = 715; 49.9%; see Table A, available as a supplement to the online version of this article at http://www.ajph.org, for substances commonly reported in polydrug overdoses).
The difference in the K functions for fentanyl and nonfentanyl overdoses for all years combined show that fentanyl overdoses cluster more than nonfentanyl overdoses, and this difference is significant (Figure 1). When we examined the K functions by year, much of this difference occurred starting in 2016 and may be related to the influx of fentanyl in the drug market at that time (Figure B, available as a supplement to the online version of this article at http://www.ajph.org). In 2014 and 2015, fentanyl overdoses clustered more than nonfentanyl overdoses, but this difference was not significant. Starting in 2016, the clustering of fentanyl overdoses was significantly greater than clustering among nonfentanyl overdoses.
The overall kernel intensity ratio maps identified several areas of elevated fentanyl overdoses compared with nonfentanyl overdoses (designated in yellow in Figure C, available as a supplement to the online version of this article at http://www.ajph.org), but one area in particular showed significantly elevated risk for fentanyl overdoses (P < .05; Figure 2). This area was located in the western neighborhoods of Chicago around Humboldt Park and Garfield Park (Figure D, available as a supplement to the online version of this article at http://www.ajph.org). Kernel intensity maps by year showed temporal variation in fentanyl risk. The 2014 map showed multiple areas of significantly elevated risk (Figure E, available as a supplement to the online version of this article at http://www.ajph.org). After 2015, maps were similar to the map for all years combined and showed 1 area of significantly elevated risk; this area changed in size but centered around the Humboldt Park and Garfield Park neighborhoods. In 2017, there were 2 additional areas of significantly elevated risk southwest of Chicago near Tinley Park and Harvey, but these regions were not significant for any other year.
FIGURE 2—
Map of Kernel Intensity Ratio Estimates Showing Significant Local Differences in Fentanyl and Nonfentanyl Overdose Intensities: Cook County, Illinois, 2014–2018
Note. Lighter grays indicate areas of elevated fentanyl overdoses compared with nonfentanyl overdoses. Dashed line represents the significant areas of log relative risk at P < .05. See Figure D, available as a supplement to the online version of this article at http://www.ajph.org, for color version.
Results from univariable logistic regression showed that several individual- and neighborhood-level risk factors were significantly associated with fentanyl overdoses (Table 2). In univariable analysis, the odds of a fentanyl-involved overdose were significantly increased for men, Blacks, Latinos/as, and younger individuals, and these covariates were assessed in multivariable analysis. Median household income (odds ratio [OR] = 0.963; 95% confidence interval [CI] = 0.938, 0.987; P = .003), neighborhood deprivation score (OR = 1.128; 95% CI = 1.086, 1.172; P < .001), and ICE (OR = 0.720; 95% CI = 0.661, 0.794; P < .001) were also significant and assessed in multivariable analysis. Population density was not significant (OR = 1.004; 95% CI = 0.999, 1.008; P = .092) and was not included in multivariable analysis.
TABLE 2—
Univariable and Multivariable Logistic Regression Results for Odds of Fentanyl Overdose: Cook County, Illinois, August 1, 2014, to August 15, 2018
| Variable | Univariable OR (95% CI) | Multivariable OR (95% CI)a |
| Age | 0.993 (0.988, 0.999) | 0.984 (0.977, 0.990) |
| Race/ethnicity | ||
| Non-Latino/a White (Ref) | 1.458 (1.256, 1.692) | 1.448 (1.205, 1.742) |
| Non-Latino/a Black | 1.707 (1.354, 2.152) | 1.570 (1.239, 1.989) |
| Latino/a | 0.566 (0.287, 1.049) | 0.511 (0.258, 0.954) |
| Other | ||
| Sex (Ref: female) | 1.287 (1.096, 1.514) | 1.327 (1.126, 1.565) |
| Neighborhood deprivation score (–5 to +5)b | 1.128 (1.086, 1.172) | 1.114 (1.066, 1.165) |
| Index of Concentration at the Extremes (–1 to +1) | 0.720 (0.661, 0.794) | |
| Median household income (in $10 000s) | 0.952 (0.928, 0.977) | |
| Population density (in 1000s) | 1.004 (0.999, 1.008) |
Note. CI = confidence interval; OR = odds ratio. Sample size n = 3271. For adjusted model, Akaike’s information criterion = 4400.
Adjusted for other covariates in the column.
OR denotes a 1.00-unit change in the score over the −5 to +5 scale.
In the multivariable logistic regression, median household income was not significant when we controlled for individual age, gender, and race/ethnicity (OR = 0.98; 95% CI = 0.95, 1.01; P = .128) and was significantly correlated with neighborhood deprivation index (r = −0.639; P < .001). ICE showed multicollinearity (variance inflation factor > 3) with race/ethnicity of individual overdose cases and with neighborhood deprivation score. ICE was also significantly correlated with individual race/ethnicity (r = −0.490; P < .001) and neighborhood deprivation score (r = −0.500; P < .001). The model containing age, gender, and ICE showed poorer fit compared with the model containing age, gender, race/ethnicity, and neighborhood deprivation score (Akaike’s information criterion = 4410 vs 4400; Table B, available as a supplement to the online version of this article at http://www.ajph.org).
The odds of a fentanyl-involved overdose increased 11.4% with each unit increase in neighborhood deprivation (95% CI = 1.066, 1.165; P < .001) when we controlled for age, race/ethnicity, and gender. Residual semivariograms for models with neighborhood deprivation score indicated no unexplained spatial variation. GWR models supported this finding (Figure F and Table C, available as supplements to the online version of this article at http://www.ajph.org); there was no variation in the relationship between neighborhood deprivation score and the odds of a fentanyl overdose across the study region.
DISCUSSION
This study describes the geographic distribution of fatal fentanyl-involved overdoses compared with other fatal opioid and polydrug overdoses and examines neighborhood-level correlates of overdose fatality. Few studies have examined the local geographic distribution of drug overdoses and associated neighborhood-level risk factors. Much of this work has been ecological, using large geographic units such as zip codes or counties on a national scale.29 This study provides a unique perspective on the geographic distribution of overdose locations by using point-level data, allowing for a more localized investigation of overdose risk factors, and supports the hypothesis that fentanyl may be targeted to more resource-deprived neighborhoods.
We employed a variety of parametric and nonparametric tests to assess if fentanyl-involved overdoses follow a bifurcated geographic distribution independent of other overdose deaths. The difference in K functions showed that fentanyl overdoses clustered more than other overdoses, suggesting that fentanyl does not follow the same geographic distribution as that of the general drug-using population. This finding was supported by the lack of significance of population density in logistic regression. Kernel intensity ratio maps identified several areas of elevated risk for fentanyl-involved overdose, indicating that the odds of a fentanyl-involved overdose occurring varies geographically. We also assessed temporal variations in these trends by looking at all study years combined (2014–2018) and each year individually to make sure that overall trends could not be attributed to the sudden influx of fentanyl into the drug market after 2014. All analyses conducted after 2014 found significant sustained spatial variation in fentanyl-involved overdoses compared with opioid and polydrug overdoses.
Our findings suggest that fentanyl-involved overdoses are concentrated in resource-deprived neighborhoods over and above what we see for opioid and polydrug overdoses. This supports the hypothesis of an evolving bifurcated drug market, with people who use drugs in resource-deprived neighborhoods potentially unable to access drugs free of fentanyl. In addition, the odds of a fentanyl-involved overdose were significantly increased for men, Blacks, Latinos/as, and younger individuals. These findings echo previous studies of risk for crack cocaine use, which identified socioeconomic disadvantage as a fundamental cause of racial disparities in crack use.14
The physical and social characteristics of disadvantaged neighborhoods can undermine residents’ mental health, increasing risk for drug use.19,20,23 Neighborhood risk factors for drug use may be modifiable through targeted infrastructure improvements or other community development strategies, such as park-making or building renovation,30–32 but this research has not been extended to overdose prevention to date. For example, vacant lot remediation has been shown to significantly reduce gun violence31 and improve residents’ mental health in cities30; this presents a possible strategy for reducing drug use in resource-deprived neighborhoods. Further inquiry into specific, modifiable aspects of neighborhood deprivation that can be used to create actionable policy and interventions for harm reduction and overdose prevention is warranted.
Limitations
This study was limited to fatal overdoses only and does not account for possible geographic variability in nonfatal overdoses. We could not explore geographic factors that might reduce risk for fatal overdose, such as access to health services or naloxone distribution. It is possible that nonfatal fentanyl-involved overdoses differ from fatal overdoses in significant and meaningful ways; future research should include nonfatal overdoses in place-based inquiry.
The Cook County Medical Examiner’s Office began routinely testing for fentanyl in June 201533; there is potential for misclassification bias for overdoses before this date. Generalizability of findings may be limited to urban areas where fentanyl is readily combined with opioids such as white powder heroin. For example, black tar heroin is more difficult to mix with fentanyl and is primarily sold in areas west of the Mississippi River—areas that have not experienced the same influx of fentanyl into the drug supply.4
GPS coordinates indicated where an overdose occurred (location of injury); we do not have data on locations where drugs were purchased or consumed. It is possible that people who use drugs may travel to certain neighborhoods to purchase and consume drugs,34 but mobility among people who use drugs and variation in activity centers has not been widely studied. As we did not have access to home addresses, interpretation of findings is limited to where the overdose occurred and cannot be expanded to include neighborhoods where people who use drugs lived or purchased drugs. However, previous research has shown that more than 70% of people who use drugs purchase drugs in their neighborhood of residence,35 and a San Francisco, California, study found that opioid users traveled on average 1.5 miles between locations where they lived, hung out, and used drugs.34 Although our data do not directly record the location where drugs were purchased, these data provide a proxy location to explore the characteristics of neighborhoods where drugs were purchased and consumed.
Conclusions
Fentanyl-involved fatal overdoses follow a unique geographic distribution compared with fatal nonfentanyl opioid and polydrug overdoses associated with resource deprivation in neighborhoods where they occur. This suggests an evolving bifurcated drug market, with drug markets in resource-deprived neighborhoods disproportionately likely to include fentanyl. Future research should explore modifiable aspects of neighborhood deprivation that can be used to create actionable policy and interventions for prevention of fentanyl-involved overdoses.
ACKNOWLEDGMENTS
This work was supported by the National Institute on Drug Abuse (grant T32DA031099).
The authors thank Alex Freed for his help in preparing this article.
CONFLICTS OF INTEREST
All authors have no possible conflicts of interest to disclose.
HUMAN PARTICIPANT PROTECTION
This research used publicly available data disseminated such that participants cannot be identified and was deemed non–human participant research by the Columbia University Medical Center institutional review board.
REFERENCES
- 1.US Drug Enforcement Administration Diversion Control Division. National Forensic Laboratory Information System: year 2016 annual report. 2017. Available at: https://www.nflis.deadiversion.usdoj.gov/DesktopModules/ReportDownloads/Reports/NFLIS2016AR_Rev2018.pdf. Accessed September 6, 2018.
- 2.US Drug Enforcement Administration Diversion Control Division. National Forensic Laboratory Information System: NFLIS-drug midyear report 2017. 2018. Available at: https://www.nflis.deadiversion.usdoj.gov/DesktopModules/ReportDownloads/Reports/11674r1NFLISMidyear2017.pdf. Accessed September 6, 2018.
- 3.Schueler HE. Emerging synthetic fentanyl analogs. Acad Forensic Pathol. 2017;7(1):36–40. doi: 10.23907/2017.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Rising numbers of deaths involving fentanyl and fentanyl analogs, including carfentanil, and increased usage and mixing with non-opioids. 2018. Available at: https://emergency.cdc.gov/han/HAN00413.asp. Accessed September 6, 2018.
- 5.US Drug Enforcement Administration. 2017. national drug threat assessment. 2017. Available at: https://www.dea.gov/documents/2017/10/01/2017-national-drug-threat-assessment. Accessed September 7, 2018.
- 6.Frank RG, Pollack HA. Addressing the fentanyl threat to public health. N Engl J Med. 2017;376(7):605–607. doi: 10.1056/NEJMp1615145. [DOI] [PubMed] [Google Scholar]
- 7.O’Donnell JK, Gladden R, Seth P. Trends in deaths involving heroin and synthetic opioids excluding methadone, and law enforcement drug product reports, by census region—United States, 2006–2015. MMWR Morb Mortal Wkly Rep. 2017;66(34):897–903. doi: 10.15585/mmwr.mm6634a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.O’Donnell JK, Halpin J, Mattson C, Goldberger B, Gladden R. Deaths involving fentanyl, fentanyl analogs, and U-47700—10 states, July–December 2016. MMWR Morb Mortal Wkly Rep. 2017;66:1197–1202. doi: 10.15585/mmwr.mm6643e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Seth P, Scholl L, Rudd R, Bacon S. Overdose deaths involving opioids, cocaine, and psychostimulants—United States, 2015–2016. MMWR Morb Mortal Wkly Rep. 2018;67(12):349–358. doi: 10.15585/mmwr.mm6712a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mars SG, Ondocsin J, Ma E, Ciccarone D. Sold as heroin: perceptions and use of an evolving drug in Baltimore, MD. J Psychoactive Drugs. 2018;50(2):167–176. doi: 10.1080/02791072.2017.1394508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ciccarone D, Ondocsin J, Mars S. Heroin uncertainties: exploring users’ perceptions of fentanyl-adulterated and-substituted “heroin. Int J Drug Policy. 2017;46:146–155. doi: 10.1016/j.drugpo.2017.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McGowan CR, Harris M, Platt L, Hope V, Rhodes T. Fentanyl self-testing outside supervised injection settings to prevent opioid overdose: do we know enough to promote it? Int J Drug Policy. 2018;58:31–36. doi: 10.1016/j.drugpo.2018.04.017. [DOI] [PubMed] [Google Scholar]
- 13.Bebinger M. Fentanyl-laced cocaine becoming a deadly problem among drug users. NPR. March 29, 2018. Available at: https://www.npr.org/sections/health-shots/2018/03/29/597717402/fentanyl-laced-cocaine-becoming-a-deadly-problem-among-drug-users. Accessed September 6, 2018.
- 14.Palamar JJ, Davies S, Ompad DC, Cleland CM, Weitzman M. Powder cocaine and crack use in the United States: an examination of risk for arrest and socioeconomic disparities in use. Drug Alcohol Depend. 2015;149:108–116. doi: 10.1016/j.drugalcdep.2015.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fairbairn N, Coffin PO, Walley AY. Naloxone for heroin, prescription opioid, and illicitly made fentanyl overdoses: challenges and innovations responding to a dynamic epidemic. Int J Drug Policy. 2017;46:172–179. doi: 10.1016/j.drugpo.2017.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.US Census Bureau. American Fact Finder. Available at: https://factfinder.census.gov/faces/nav/jsf/pages/index.xhtml. Accessed March 29, 2019.
- 17.Cook County Open Data. Medical examiner case archive. 2018. Available at: https://datacatalog.cookcountyil.gov/Public-Safety/Medical-Examiner-Case-Archive/cjeq-bs86. Accessed August 31, 2018.
- 18.Trinidad JP, Warner M, Bastian BA, Minino AM, Hedegaard H. Using literal text from the death certificate to enhance mortality statistics: characterizing drug involvement in deaths. Natl Vital Stat Rep. 2016;65(9):1–15. [PubMed] [Google Scholar]
- 19.Latkin CA, Williams CT, Wang J, Curry AD. Neighborhood social disorder as a determinant of drug injection behaviors: a structural equation modeling approach. Health Psychol. 2005;24(1):96–100. doi: 10.1037/0278-6133.24.1.96. [DOI] [PubMed] [Google Scholar]
- 20.Cerdá M, Ransome Y, Keyes KM et al. Revisiting the role of the urban environment in substance use: the case of analgesic overdose fatalities. Am J Public Health. 2013;103(12):2252–2260. doi: 10.2105/AJPH.2013.301347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ross CE, Mirowsky J. Neighborhood disadvantage, disorder, and health. J Health Soc Behav. 2001;42(3):258–276. [PubMed] [Google Scholar]
- 22.Furr-Holden CDM, Milam AJ, Nesoff ED et al. Not in my back yard: a comparative analysis of crime around publicly funded drug treatment centers, liquor stores, convenience stores, and corner stores in one mid-Atlantic city. J Stud Alcohol Drugs. 2016;77(1):17–24. doi: 10.15288/jsad.2016.77.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Diez Roux AV, Mair C. Neighborhoods and health. Ann N Y Acad Sci. 2010;1186(1):125–145. doi: 10.1111/j.1749-6632.2009.05333.x. [DOI] [PubMed] [Google Scholar]
- 24.Krieger N, Waterman P, Spasojevic J, Li W, Maduro G, Van Wye G. Public health monitoring of privilege and deprivation with the index of concentration at the extremes. Am J Public Health. 2016;106(2):256–263. doi: 10.2105/AJPH.2015.302955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Waller LA, Gotway CA. Applied Spatial Statistics for Public Health Data. Hoboken, NJ: Wiley; 2004. [Google Scholar]
- 26.Fotheringham A, Brunsdon C, Charlton M. Geographically Weighted Regression: The Analysis of Spatially Varying Relationships. Chichester, UK: Wiley; 2002. [Google Scholar]
- 27.Wheeler D, Tiefelsdorf M. Multicollinearity and correlation among local regression coefficients in geographically weighted regression. J Geogr Syst. 2005;7(2):161–187. [Google Scholar]
- 28.Leung Y, Mei C, Zhang W. Statistical tests for spatial nonstationarity based on the geographically weighted regression model. Environ Plann A. 2000;32(1):9–32. [Google Scholar]
- 29.Jalal H, Buchanich JM, Roberts MS, Balmert LC, Zhang K, Burke DS. Changing dynamics of the drug overdose epidemic in the United States from 1979 through 2016. Science. 2018;361:eaau1184. doi: 10.1126/science.aau1184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.South EC, Hohl BC, Kondo MC, MacDonald JM, Branas CC. Effect of greening vacant land on mental health of community-dwelling adults. JAMA Netw Open. 2018;1(3):e180298. doi: 10.1001/jamanetworkopen.2018.0298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Branas CC, South E, Kondo MC et al. Citywide cluster randomized trial to restore blighted vacant land and its effects on violence, crime, and fear. Proc Natl Acad Sci USA. 2018;115(12):2946–2951. doi: 10.1073/pnas.1718503115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kondo MC, Keene D, Hohl BC, MacDonald JM, Branas CC. A difference-in-differences study of the effects of a new abandoned building remediation strategy on safety [erratum: PLoS One. 2015;10(8):e0136595. doi: 10.1371/journal.pone.0129582. PLoS One. 2015;10(7):e0129582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rushovich T, Salisbury-Afshar E, Arunkumar P Epidemiology report: increase in overdose deaths involving opioids—Chicago, 2015–2016. Chicago Department of Public Health. October 2017. Available at: https://www.chicago.gov/content/dam/city/depts/cdph/tobacco_alchohol_and_drug_abuse/2016ChicagoOpioidReport.pdf. Accessed October 4, 2019. [DOI] [PubMed]
- 34.Martinez AN, Lorvick J, Kral AH. Activity spaces among injection drug users in San Francisco. Int J Drug Policy. 2014;25(3):516–524. doi: 10.1016/j.drugpo.2013.11.008. [DOI] [PubMed] [Google Scholar]
- 35.Latkin CA, Edwards C, Davey-Rothwell MA, Yang C, Tobin KE. The relationship between drug use settings, roles in the drug economy, and witnessing a drug overdose in Baltimore, Maryland. Subst Abus. 2018;39(3):384–389. doi: 10.1080/08897077.2018.1439801. [DOI] [PMC free article] [PubMed] [Google Scholar]