Abstract
The early initiation of breastfeeding (EIBF) within one hour after birth enhanced mother–newborn bonding and protection against infectious diseases. This paper aimed to examine factors associated with EIBF in 13 Economic Community of West African States (ECOWAS). A weighted sample of 76,934 children aged 0–23 months from the recent Demographic and Health Survey dataset in the ECOWAS for the period 2010 to 2018 was pooled. Survey logistic regression analyses, adjusting for country-specific cluster and population-level weights, were used to determine the factors associated with EIBF. The overall combined rate of EIBF in ECOWAS was 43%. After adjusting for potential confounding factors, EIBF was significantly lower in Burkina Faso, Cote d’Ivoire, Guinea, Niger, Nigeria, and Senegal. Mothers who perceived their babies to be average and large at birth were significantly more likely to initiate breastfeeding within one hour of birth than those mothers who perceived their babies to be small at birth. Mothers who had a caesarean delivery (AOR = 0.28, 95%CI = 0.22–0.36), who did not attend antenatal visits (ANC) during pregnancy, and delivered by non-health professionals were more likely to delay initiation of breastfeeding beyond one hour after birth. Male children and mothers from poorer households were more likely to delay introduction of breastfeeding. Infant and young child feeding nutrition programs aimed at improving EIBF in ECOWAS need to target mothers who underutilize healthcare services, especially mothers from lower socioeconomic groups.
Keywords: breastfeeding, infants, ECOWAS, antenatal care, pregnancy, infant mortality
1. Introduction
Globally, about 75% of all under-five deaths occur within the first year of life, and sub-Saharan African countries remain the hub of the world burden of all under-five deaths [1,2]. Early initiation of breastfeeding (EIBF) within one hour of birth remains a significant public health challenge, particularly in sub-Saharan African (SSA) countries, including the Economic Community of West African States (ECOWAS). In keeping with the Sustainable Development Goals, developing countries have committed to reducing under-five mortality by 25 deaths per 1000 live births by 2030 [3]. Global strategies, including the Baby-Friendly Hospital Initiative (BFHI), Community Integrated Management of Childhood Illness (C-IMCI), and Infant and Young Child Feeding (IYCF) guidelines have been developed by United Nations Children’s Fund (UNICEF) and the World Health Organization (WHO). These aim to substantially reduce child mortality, morbidity, and undernutrition [4,5]. They have succeeded in some parts of the world but remain refractory in Africa. In addition, there is a strong epidemiological evidence to suggest that the nutritional benefits of EIBF may include a reduced risk of hypoglycemia in at-risk infants (e.g., small for gestational age and macrosomia infants), which can cause significant morbidity and mortality [6]. This is due to EIBF containing antibodies for natural immunity, which provide protection against infectious diseases (such as diarrheal and pneumonia) and other potentially life-threatening ailments [7,8]. ECOWAS is a regional political and economic union of 15 countries in West Africa, founded in 1975 with members including Benin, Burkina Faso, Cabo Verde, Cote d’Ivoire, The Gambia, Ghana, Guinea, Guinea-Bissau, Liberia, Mali, Niger, Nigeria, Senegal, Sierra Leone, and Togo. The main aim of this alliance is to promote socioeconomic integration among member states to raise living standards and promote economic development, with wider implications for judicial and health service cooperation [9].
There are numerous recognized advantages of EIBF, however, the rates of EIBF in ECOWAS are typically low and still suboptimal, ranging from 17% to 62% [10,11]. These low rates mean a substantial proportion of newborn babies are deprived of mother–newborn bonding, resistance against infection, and the early breastfeeding needed to fight disease [7,8]. Studies highlight that infants initiated to breastfeeding within an hour of birth have a reduced incidence of life-threatening conditions, such as serious systemic bacterial infections, diarrhea, respiratory infections, as well as less severe infections of the middle ear and urinary tract, and allergic conditions [12,13,14]. A cohort study conducted in rural Ghana indicated that 22% of neonatal deaths could be prevented if breastfeeding started within the first hour of birth [15]. Similarly, a community-based randomized trial conducted in southern Nepal revealed that approximately 8–19% of newborn deaths could be averted annually in developing countries if all newborns were breastfed within an hour of delivery [16]. EIBF is not only beneficial to neonates but also to mothers, as it reduces the risk of postpartum hemorrhage [17].
Published studies conducted on EIBF in SSA, including ECOWAS countries, have indicated that EIBF is associated with demographic, socioeconomic, and obstetric characteristics. A nationwide cross-sectional study on trends and factors associated with EIBF in Nigeria found that mothers who had four or more antenatal visits (ANC) visits during pregnancy, mothers from wealthier households, and mothers who delivered their babies at the health facility are more likely to initiate breastfeeding within one hour of birth [18,19]. Another population-based study conducted in Nigeria that examined urban–rural differences in the rates of EIBF concluded that EIBF rates were significantly lower in rural areas than urban areas [20]. The perception of a lack of breastmilk, perception that the mother and the baby need rest after birth, performing post-birth activities (such as bathing), and the baby not crying for milk were observed as barriers to EIBF among mothers in Ghana [11]. In that study, delivery in a health facility was a facilitator to EIBF, as health practitioners encouraged early breastfeeding [11]. A nationwide cross-sectional study in Zimbabwe found that skilled delivery assistants, multiparity, and postpartum skin to skin contact between mother and newborn babies immediately after birth were significantly related to EIBF [21]. Similarly, in a community-based cross-sectional study on EIBF conducted in Ethiopia, maternal education, delivery at a health facility and visiting antenatal care services during pregnancy were also significantly associated with EIBF within one hour of delivery [22]. The low rate of EIBF practice in ECOWAS could have potentially contributed to nearly half of all under-five deaths, such as those due to prematurity or malnutrition in sub-Saharan Africa region in the year 2017 [1]. Prior to the current study, no studies have used combined country-specific local data across ECOWAS countries to examine factors associated with EIBF within one hour of birth. Evidence based on collective data will provide region-specific targeted interventions to scale up EIBF practices to reduce morbidity and mortality.
Hence, this study aims to investigate the possible characteristics influencing EIBF in 13 of the ECOWAS member countries using the most recent Demographic and Health Survey (DHS) survey datasets conducted between 2010 and 2018. Recognition of factors associated with EIBF in ECOWAS countries is essential for building effective nutrition education and behavior change communication interventions in targeting women at heightened risk of sub-optimal feeding behaviors. In addition, the identification of modifiable associated factors will help public health nutrition program managers and policymakers develop strategies to support these contributory factors. ECOWAS would gain enormous health and economic benefits by improving EIBF. Thus, the findings from this study could assist in the planning and monitoring of effective infant and breastfeeding promotion programs in each ECOWAS country, which may contribute to achieving the child survival sustainable development goal.
2. Materials and Methods
The most recent ECOWAS DHS datasets between 2010 and 2018 were used for this study. Cabo Verde and Guinea-Bissau were not included in the study because their last DHS surveys were not within the study period. As a result, the most recent DHS datasets from 13 ECOWAS countries were used for this study. These data sets were obtained from standardized population-based cross-sectional surveys with a high response rate and trained interviewers [10]. The DHS surveys are publicly available for download [10,23]. Each ECOWAS National Bureau of Statistics collects the DHS Data in collaboration with the United States Agency for International Development [10]. The DHS surveys use identical questionnaires in all countries to collect information on diverse topics, including fertility, reproductive health, maternal and child health, mortality, nutrition, and self-reported health behaviors among adults [5]. In this study and to reduce recall bias, we restricted the analysis to the last born child at 23 months and living with the respondent. This yielded a weighted total of 76,934 children.
2.1. Outcome and Confounding Factors
The outcome variable was EIBF. Women were asked how long after birth the baby was put to the breast for the first time. Responses were recorded in minutes and/or hours. EIBF within one hour of birth was estimated using the World Health Organization recommendation [24,25]. This indicator includes the EIBF rate (the proportion of children born aged 0–23 months who were put to the breast within one hour of birth). EIBF was categorized into a binary form of the outcome variables: “Yes” (1 = if a child was given EIBF) and “No” (0 = if a child was not given EIBF). The potential confounding factors were organised into four distinct groups: demographic factors (countries, place of residence, mother’s age, marital status, combined birth rank and birth interval, sex of baby, child’s age in category, perceived size of the baby); socio-economic factors (household wealth index, maternal work in the last 12 months, maternal education, and maternal literacy); access to media factors (frequency of reading newspapers/magazine, frequency of listening to radio, and frequency of watching television); and healthcare utilization factors (place of delivery, mode of delivery, type of delivery assistance, and antenatal clinic visits). For the pooled dataset, the household wealth index was constructed using the ‘hv271’ variable. The hv271 is a household’s wealth index value generated by the product of standardized scores (z-scores) and factor coefficient scores (factor loadings) of wealth indicators [26]. In the household wealth index categories, the bottom 20% of households was arbitrarily referred to as the poorest households and the top 20% as richest households, and they were divided into poorest, poor, middle, rich, and richest.
2.2. Statistical Analysis
For the combined 13 ECOWAS datasets, a population-level weight, unique country-specific clustering, and strata were created. This was to manage large country weights being greater than small country weights and also because clusters were different in each country. Population-level weights were used for survey (SVY) tabulation that adjusted for a unique country-specific stratum, and clustering was used to determine the percentage, frequency count, and univariate analysis of all selected characteristics. Country-specific weights were used for the Taylor series linearization method [27] in the surveys when estimating the rates and 95% confidence intervals of EIBF in each country.
Population-level weights were used in the multivariate analyses. In the multivariate analyses, a four-stage hierarchical model was carried out. In the first stage model, demographic factors were entered into the model. In the second stage model, demographic factors were added to the socio-economic factors. A similar procedure was employed for the third stage model, which included the demographic and socio-economic level factors, as well as access to media factors. The fourth and final stage model, healthcare utilization factors, were added to demographic, socio-economic, and media factors. All statistical analyses were conducted using (statistics and data) STATA/MP Version.14.1 (StataCorp, College Station, TX, USA) and adjusted odds ratios (AORs) and their 95% confidence intervals (CIs) obtained from the adjusted multivariate logistic regression model were used to measure the factors associated with EIBF.
3. Results
3.1. Characteristics of the Sample and Univariate Analyses for EIBF
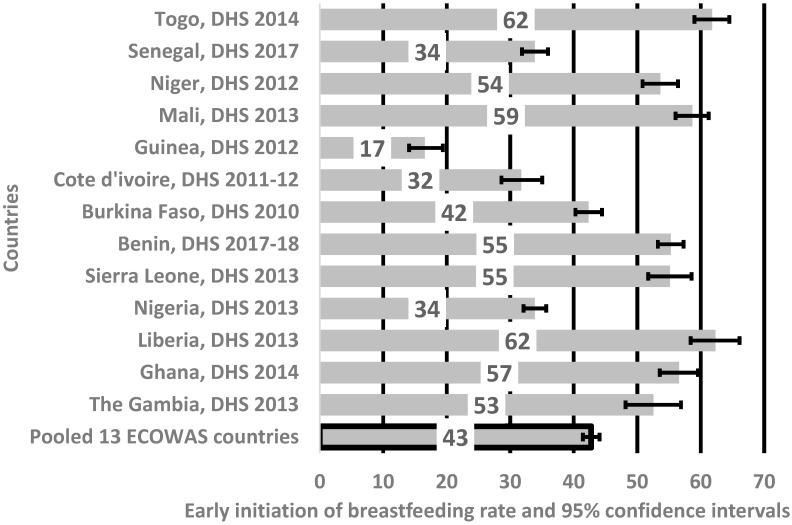
The pooled rate of EIBF in the 13 ECOWAS was 43% and EIBF lay between 52% and 62% in Togo, Niger, Mali, Benin, Sierra Leone, Liberia, Ghana, and Gambia, as indicated in Figure 1. The highest rates of EIBF were observed in Togo and Liberia, and the lowest was in Guinea (17%).
Figure 1.
Rates of early initiation of breastfeeding in thirteen Economic Community of West African States. DHS = Demographic and Health Survey.
Table 1 illustrates the characteristics of the sample of children aged 0–23 months and the unadjusted odd ratios of EIBF in children aged 0–23 months. Overall, 21% of children aged 0–23 months were from Nigeria, and compared to Benin (7.7%), the odds of EIBF in Nigeria was reduced significantly, by 58% (OR = 0.42, 95% CI:0.36, 0.48). About 42% of EIBF babies were perceived by their mothers to be of average birth size compared to the 18% of EIBF babies perceived to be small at birth. The unadjusted odd ratios of EIBF were significant with babies perceived by their mothers to be the average birth size at birth, combined birth rank and birth interval, household wealth, frequency of listening to the radio, and watching television.
Table 1.
Individual, household, and community level characteristics and unadjusted odds ratios (OR) (95% CI) of early initiation of breastfeeding (EIBF) among children aged 0–23 months in 13 Economic Community of West African States (ECOWAS).
| Characteristic | n * | % * | % | EIBF | |||
|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-Value | |||||
| Demographic factors | |||||||
| Country | |||||||
| Benin | 5937 | 7.7 | 9.2 | 1.00 | |||
| Burkina Faso | 6887 | 9.0 | 10.0 | 0.58 | 0.50 | 0.67 | <0.001 |
| Cote d’ivoire | 4554 | 5.9 | 5.2 | 0.43 | 0.33 | 0.56 | <0.001 |
| The Gambia | 5387 | 7.0 | 6.0 | 0.76 | 0.52 | 1.11 | 0.151 |
| Ghana | 3412 | 4.4 | 4.0 | 1.07 | 0.88 | 1.31 | 0.483 |
| Guinea | 3574 | 4.6 | 4.7 | 0.17 | 0.13 | 0.22 | <0.001 |
| Liberia | 4241 | 5.5 | 5.1 | 1.30 | 0.96 | 1.77 | 0.093 |
| 4843 | 6.3 | 6.7 | 1.11 | 0.93 | 1.32 | 0.242 | |
| Niger | 7044 | 9.2 | 8.1 | 0.90 | 0.75 | 1.08 | 0.262 |
| Nigeria | 15,993 | 20.8 | 20.7 | 0.42 | 0.36 | 0.48 | <0.001 |
| Senegal | 5790 | 7.5 | 8.1 | 0.35 | 0.29 | 0.41 | <0.001 |
| Sierra Leone | 6230 | 8.1 | 7.4 | 0.85 | 0.67 | 1.08 | 0.173 |
| Togo | 3042 | 4.0 | 4.8 | 1.49 | 1.23 | 1.79 | <0.001 |
| Residence | |||||||
| Urban | 27,769 | 36.1 | 31.0 | 1.00 | |||
| Rural | 49,165 | 63.9 | 69.0 | 0.96 | 0.85 | 1.08 | 0.468 |
| Mothers’ age in years | |||||||
| 15–19 | 25,575 | 33.2 | 33.4 | 1.00 | |||
| 20–34 | 36,855 | 47.9 | 46.9 | 1.09 | 1.02 | 1.17 | 0.012 |
| 35–49 | 14,503 | 18.9 | 19.8 | 1.08 | 0.99 | 1.17 | 0.084 |
| Marital status | |||||||
| Currently married | 70,916 | 92.2 | 92.7 | 1.00 | |||
| Formerly married ^ | 1875 | 2.4 | 2.5 | 1.13 | 0.91 | 1.39 | 0.269 |
| Never married | 4142 | 5.4 | 4.8 | 0.98 | 0.83 | 1.17 | 0.863 |
| Age of child (months) | |||||||
| 0–5 | 19,736 | 25.7 | 25.8 | 1.00 | |||
| 6–11 | 20,308 | 26.4 | 26.9 | 1.02 | 0.93 | 1.12 | 0.657 |
| 12–17 | 20,402 | 26.5 | 26.0 | 1.07 | 0.98 | 1.16 | 0.138 |
| 18–23 | 16,488 | 21.4 | 21.3 | 1.10 | 1.00 | 1.21 | 0.047 |
| Birth order or birth rank | |||||||
| First-born | 15,935 | 20.7 | 20.0 | 1.00 | |||
| Second–fourth | 36,840 | 47.9 | 46.6 | 1.26 | 1.16 | 1.36 | <0.001 |
| Fifth or more | 24,159 | 31.4 | 33.4 | 1.19 | 1.09 | 1.31 | <0.001 |
| Preceding birth interval (n = 76,748) | |||||||
| No previous birth | 15,935 | 20.7 | 20.0 | 1.00 | |||
| <24 months | 8163 | 10.6 | 10.6 | 1.13 | 1.00 | 1.28 | 0.042 |
| ≥24 months | 52,650 | 68.4 | 69.2 | 1.25 | 1.16 | 1.35 | <0.001 |
| Combined birth rank and birth interval | |||||||
| Second/third birth rank, more than two years interval | 30,717 | 39.9 | 39.0 | 1.00 | |||
| First birth rank | 15,935 | 20.7 | 20.0 | 0.78 | 0.72 | 0.85 | <0.001 |
| Second/third birth rank, less than or equal to two years interval | 6123 | 8.0 | 7.7 | 0.90 | 0.79 | 1.02 | 0.097 |
| Fourth birth rank, more than two years interval | 20,520 | 26.7 | 28.4 | 0.94 | 0.87 | 1.02 | 0.120 |
| Fourth birth rank, less than or equal to two years interval | 3638 | 4.7 | 5.0 | 0.89 | 0.77 | 1.02 | 0.103 |
| Sex of baby | |||||||
| Male | 38,723 | 50.3 | 50.6 | 1.00 | |||
| Female | 38,211 | 49.7 | 49.4 | 1.05 | 0.99 | 1.11 | 0.120 |
| Size of baby (n = 76,255) | |||||||
| Small | 13,689 | 17.8 | 17.5 | 1.00 | |||
| Average | 32,517 | 42.3 | 42.6 | 1.22 | 1.11 | 1.34 | <0.001 |
| Large | 30,049 | 39.1 | 38.9 | 1.19 | 1.07 | 1.31 | 0.001 |
| Socio-economic factors | |||||||
| Household Wealth Index | |||||||
| Poorest | 12,753 | 16.6 | 20.1 | 1.00 | |||
| Poorer | 13,520 | 17.6 | 19.7 | 1.35 | 1.19 | 1.54 | <0.001 |
| Middle | 15,088 | 19.6 | 19.8 | 1.55 | 1.36 | 1.78 | <0.001 |
| Richer | 14,854 | 19.3 | 20.1 | 1.33 | 1.16 | 1.52 | <0.001 |
| Richest | 20,719 | 26.9 | 20.5 | 1.25 | 1.07 | 1.46 | 0.005 |
| Work in the last 12 months (n = 76,918) | |||||||
| Not working | 30,637 | 39.8 | 38.2 | 1.00 | |||
| Working | 46,281 | 60.2 | 61.8 | 0.94 | 0.86 | 1.02 | 0.150 |
| Maternal education (n = 76,926) | |||||||
| No education | 45,527 | 59.2 | 61.6 | 1.00 | |||
| Primary | 13,319 | 17.3 | 18.1 | 1.06 | 0.96 | 1.17 | 0.239 |
| Secondary and above | 18,080 | 23.5 | 20.4 | 1.03 | 0.93 | 1.14 | 0.549 |
| Maternal Literacy (n = 76,549) | |||||||
| Cannot read at all | 57,292 | 74.5 | 77.4 | 1.00 | |||
| Able to read only part of sentences | 19,257 | 25.0 | 22.1 | 0.96 | 0.88 | 1.04 | 0.341 |
| Access to media | |||||||
| Frequency of reading newspaper or magazine (n = 76,736) | |||||||
| Not at all | 68,490 | 89.0 | 91.5 | 1.00 | |||
| Less than once a week | 4575 | 5.9 | 4.8 | 0.93 | 0.81 | 1.08 | 0.356 |
| At least once a week | 3644 | 4.7 | 3.7 | 1.10 | 0.92 | 1.32 | 0.281 |
| Almost every day | 27 | 0.0 | 0.0 | 2.13 | 0.80 | 5.69 | 0.132 |
| Frequency of listening to radio (n = 76,808) | |||||||
| Not at all | 25,977 | 33.8 | 36.0 | 1.00 | |||
| Less than once a week | 19,798 | 25.7 | 25.0 | 0.95 | 0.87 | 1.04 | 0.300 |
| At least once a week | 30,250 | 39.3 | 37.8 | 0.97 | 0.88 | 1.06 | 0.466 |
| Almost every day | 783 | 1.0 | 1.1 | 3.27 | 2.49 | 4.29 | <0.001 |
| Frequency of watching Television (n = 76,760) | |||||||
| Not at all | 42,468 | 55.2 | 59.8 | 1.00 | |||
| Less than once a week | 12,287 | 16.0 | 15.1 | 1.01 | 0.90 | 1.13 | 0.861 |
| At least once a week | 21,294 | 27.7 | 24.1 | 0.84 | 0.76 | 0.93 | 0.001 |
| Almost every day | 711 | 0.9 | 0.8 | 2.60 | 1.97 | 3.44 | <0.001 |
| Healthcare utilization factors | |||||||
| Place of delivery | |||||||
| Home | 31,183 | 40.5 | 41.3 | 1.00 | |||
| Health facility | 45,751 | 59.5 | 58.7 | 1.34 | 1.23 | 1.47 | <0.001 |
| Mode of delivery (n = 76,729) | |||||||
| Non-caesarean | 73,763 | 95.9 | 96.3 | 1.00 | |||
| Caesarean section ⱡ | 2966 | 3.9 | 3.5 | 0.39 | 0.32 | 0.49 | <0.001 |
| Type of delivery assistance (n = 63,553) | |||||||
| Health professional | 49,991 | 65.0 | 62.8 | 1.00 | |||
| Traditional birth attendant | 1884 | 2.4 | 2.8 | 0.73 | 0.61 | 0.88 | 0.001 |
| Other untrained | 6959 | 9.0 | 10.7 | 0.76 | 0.64 | 0.90 | 0.001 |
| No one | 4699 | 6.1 | 6.0 | 0.61 | 0.51 | 0.72 | <0.001 |
| Antenatal clinic visits (n = 74,550) | |||||||
| None | 9478 | 12.3 | 12.6 | 1.00 | |||
| 1–3 | 23,314 | 30.3 | 31.9 | 1.55 | 1.36 | 1.77 | <0.001 |
| 4+ | 41,758 | 54.3 | 52.7 | 1.67 | 1.45 | 1.91 | <0.001 |
^ divorce/separated/widowed; * Weighted sample sizes and percentages; ⱡ Caesarean section is a combination of both general and regional anesthesia.
3.2. Factors Associated with Early Initiation of Breastfeeding
As shown in Table 2, EIBF within one hour of birth was significantly lower among children living in Nigeria, Cote d’Ivoire, Burkina Faso, Guinea, and Senegal. Mothers from poorest households, mothers’ first birth, and delivery by non-health professionals were significantly associated with delayed initiation of breastfeeding. Mothers who underwent caesarean delivery were significantly more likely to delay the initiation of breastfeeding (adjusted OR = 0.28, 95% CI:0.22, 0.36; p < 0.001) than those who had non-caesarean delivery.
Table 2.
Adjusted odds ratio (AOR) (95% confidence intervals (CI)) of factors associated with the early initiation of breastfeeding (EIBF) among children aged 0–23 months in 13 Economic Community of West African States (ECOWAS).
| Characteristic | Model 1 | Model 2 | Model 3 | Model 4 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AOR | 95% CI | p-Value | AOR | 95% CI | p-Value | AOR | 95% CI | p-Value | AOR | 95% CI | p-Value | |||||
| Demographic factors | ||||||||||||||||
| Benin | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||||||
| Burkina Faso | 0.58 | 0.50 | 0.67 | <0.001 | 0.56 | 0.48 | 0.65 | <0.001 | 0.56 | 0.48 | 0.66 | <0.001 | 0.58 | 0.48 | 0.69 | <0.001 |
| Cote d’ivoire | 0.42 | 0.32 | 0.54 | <0.001 | 0.43 | 0.33 | 0.56 | <0.001 | 0.43 | 0.33 | 0.56 | <0.001 | 0.43 | 0.33 | 0.55 | <0.001 |
| The Gambia | 0.75 | 0.51 | 1.09 | 0.134 | 0.73 | 0.50 | 1.07 | 0.109 | 0.75 | 0.51 | 1.11 | 0.148 | 0.67 | 0.44 | 1.02 | 0.062 |
| Ghana | 1.08 | 0.88 | 1.34 | 0.460 | 1.11 | 0.89 | 1.38 | 0.351 | 1.15 | 0.92 | 1.43 | 0.212 | 1.33 | 1.03 | 1.72 | 0.028 |
| Guinea | 0.17 | 0.13 | 0.22 | <0.001 | 0.17 | 0.13 | 0.23 | <0.001 | 0.17 | 0.13 | 0.23 | <0.001 | 0.19 | 0.14 | 0.25 | <0.001 |
| Liberia | 1.30 | 0.95 | 1.79 | 0.106 | 1.34 | 0.96 | 1.87 | 0.081 | 1.34 | 0.96 | 1.87 | 0.085 | 1.44 | 1.04 | 1.98 | 0.028 |
| Mali | 1.10 | 0.93 | 1.32 | 0.271 | 1.30 | 1.07 | 1.58 | 0.009 | 1.34 | 1.09 | 1.63 | 0.005 | 1.36 | 1.09 | 1.71 | 0.006 |
| Niger | 0.94 | 0.78 | 1.13 | 0.520 | 0.86 | 0.71 | 1.04 | 0.132 | 0.87 | 0.72 | 1.05 | 0.144 | 0.98 | 0.80 | 1.22 | 0.882 |
| Nigeria | 0.41 | 0.36 | 0.48 | <0.001 | 0.44 | 0.38 | 0.51 | <0.001 | 0.44 | 0.38 | 0.52 | <0.001 | 0.51 | 0.43 | 0.61 | <0.001 |
| Senegal | 0.36 | 0.30 | 0.43 | <0.001 | 0.37 | 0.31 | 0.45 | <0.001 | 0.38 | 0.32 | 0.46 | <0.001 | 0.40 | 0.33 | 0.48 | <0.001 |
| Sierra Leone | 0.86 | 0.67 | 1.10 | 0.230 | 0.84 | 0.65 | 1.07 | 0.151 | 0.83 | 0.65 | 1.07 | 0.147 | 0.78 | 0.60 | 1.03 | 0.075 |
| Togo | 1.50 | 1.25 | 1.81 | 0.000 | 1.50 | 1.24 | 1.81 | <0.001 | 1.29 | 1.05 | 1.59 | 0.015 | 1.56 | 1.25 | 1.94 | <0.001 |
| Residence | ||||||||||||||||
| Urban | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||||||
| Rural | 0.95 | 0.84 | 1.06 | 0.335 | 0.94 | 0.83 | 1.07 | 0.373 | 0.94 | 0.82 | 1.07 | 0.355 | 0.92 | 0.81 | 1.04 | 0.200 |
| Mothers’ age in years | ||||||||||||||||
| 15–19 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||||||
| 20–34 | 0.98 | 0.90 | 1.07 | 0.732 | 0.99 | 0.91 | 1.08 | 0.777 | 0.98 | 0.90 | 1.07 | 0.605 | 0.98 | 0.90 | 1.08 | 0.731 |
| 35–49 | 0.98 | 0.86 | 1.11 | 0.725 | 0.98 | 0.86 | 1.11 | 0.727 | 0.96 | 0.85 | 1.09 | 0.538 | 0.94 | 0.82 | 1.08 | 0.372 |
| Marital status | ||||||||||||||||
| Currently married | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||||||
| Formerly married ^ | 0.99 | 0.79 | 1.26 | 0.957 | 0.99 | 0.78 | 1.26 | 0.940 | 0.99 | 0.78 | 1.26 | 0.952 | 0.98 | 0.76 | 1.26 | 0.894 |
| Never married | 0.96 | 0.78 | 1.18 | 0.692 | 0.93 | 0.76 | 1.14 | 0.501 | 0.95 | 0.77 | 1.17 | 0.610 | 0.98 | 0.79 | 1.21 | 0.843 |
| Birth rank and birth interval | ||||||||||||||||
| Second/third birth rank, more than two years interval | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||||||
| First birth rank | 0.78 | 0.71 | 0.86 | <0.001 | 0.78 | 0.70 | 0.86 | <0.001 | 0.77 | 0.70 | 0.85 | <0.001 | 0.78 | 0.69 | 0.87 | <0.001 |
| Second/third birth rank, less than or equal to two years interval | 0.89 | 0.78 | 1.03 | 0.123 | 0.89 | 0.77 | 1.02 | 0.098 | 0.89 | 0.77 | 1.03 | 0.105 | 0.91 | 0.78 | 1.07 | 0.268 |
| Fourth birth rank, more than two years interval | 0.98 | 0.89 | 1.08 | 0.699 | 0.99 | 0.89 | 1.09 | 0.791 | 1.00 | 0.90 | 1.11 | 0.978 | 1.03 | 0.93 | 1.15 | 0.551 |
| Fourth birth rank, less than or equal to two years interval | 0.92 | 0.79 | 1.07 | 0.268 | 0.92 | 0.78 | 1.07 | 0.288 | 0.93 | 0.79 | 1.09 | 0.359 | 0.98 | 0.82 | 1.17 | 0.808 |
| Sex of baby | ||||||||||||||||
| Male | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||||||
| Female | 1.07 | 1.01 | 1.13 | 0.027 | 1.07 | 1.01 | 1.13 | 0.024 | 1.07 | 1.01 | 1.13 | 0.025 | 1.08 | 1.01 | 1.16 | 0.021 |
| Age of child (months) | ||||||||||||||||
| 0–5 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||||||
| 6–11 | 1.03 | 0.94 | 1.13 | 0.546 | 1.03 | 0.94 | 1.13 | 0.538 | 1.03 | 0.93 | 1.13 | 0.570 | 1.02 | 0.92 | 1.14 | 0.664 |
| 12–17 | 1.09 | 1.00 | 1.20 | 0.056 | 1.10 | 1.00 | 1.20 | 0.045 | 1.09 | 0.99 | 1.19 | 0.071 | 1.10 | 0.98 | 1.22 | 0.096 |
| 18–23 | 1.10 | 1.00 | 1.21 | 0.048 | 1.10 | 1.00 | 1.21 | 0.047 | 1.10 | 1.00 | 1.21 | 0.052 | 1.10 | 0.99 | 1.23 | 0.075 |
| Size of baby | ||||||||||||||||
| Small | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||||||
| Average | 1.21 | 1.09 | 1.33 | <0.001 | 1.20 | 1.08 | 1.32 | <0.001 | 1.20 | 1.09 | 1.32 | <0.001 | 1.19 | 1.07 | 1.32 | 0.002 |
| Large | 1.23 | 1.11 | 1.37 | <0.001 | 1.22 | 1.10 | 1.36 | <0.001 | 1.22 | 1.10 | 1.36 | <0.001 | 1.20 | 1.07 | 1.36 | 0.002 |
| Socio-economic factors | ||||||||||||||||
| Household Wealth Index | ||||||||||||||||
| Poorest | 1.00 | 1.00 | 1.00 | |||||||||||||
| Poorer | 1.29 | 1.13 | 1.48 | <0.001 | 1.32 | 1.15 | 1.51 | <0.001 | 1.19 | 1.02 | 1.38 | 0.028 | ||||
| Middle | 1.38 | 1.20 | 1.59 | <0.001 | 1.42 | 1.23 | 1.63 | <0.001 | 1.22 | 1.03 | 1.43 | 0.018 | ||||
| Richer | 1.34 | 1.17 | 1.55 | <0.001 | 1.39 | 1.20 | 1.60 | <0.001 | 1.17 | 0.98 | 1.39 | 0.077 | ||||
| Richest | 1.16 | 0.98 | 1.36 | 0.083 | 1.19 | 1.00 | 1.43 | 0.052 | 1.03 | 0.84 | 1.26 | 0.782 | ||||
| Work in the last 12 months | ||||||||||||||||
| Not working | 1.00 | 1.00 | 1.00 | |||||||||||||
| Working | 0.95 | 0.86 | 1.04 | 0.243 | 0.95 | 0.87 | 1.04 | 0.291 | 0.95 | 0.87 | 1.05 | 0.329 | ||||
| Maternal education | ||||||||||||||||
| No education | 1.00 | 1.00 | 1.00 | |||||||||||||
| Primary | 1.02 | 0.92 | 1.13 | 0.732 | 1.03 | 0.92 | 1.14 | 0.627 | 1.00 | 0.90 | 1.12 | 0.992 | ||||
| Secondary and above | 0.98 | 0.80 | 1.21 | 0.860 | 0.96 | 0.78 | 1.19 | 0.717 | 0.89 | 0.73 | 1.10 | 0.291 | ||||
| Maternal Literacy | ||||||||||||||||
| Cannot read at all | 1.00 | 1.00 | 1.00 | |||||||||||||
| Able to read only part of sentences | 1.04 | 0.87 | 1.24 | 0.690 | 1.00 | 0.82 | 1.21 | 0.985 | 1.02 | 0.85 | 1.23 | 0.811 | ||||
| Access to media | ||||||||||||||||
| Frequency of reading newspaper or magazine | ||||||||||||||||
| Not at all | 1.00 | 1.00 | ||||||||||||||
| Less than once a week | 1.11 | 0.93 | 1.32 | 0.255 | 1.06 | 0.89 | 1.27 | 0.508 | ||||||||
| At least once a week | 1.33 | 1.09 | 1.63 | 0.006 | 1.36 | 1.10 | 1.67 | 0.004 | ||||||||
| Almost every day | 0.91 | 0.33 | 2.51 | 0.856 | 1.01 | 0.40 | 2.50 | 0.990 | ||||||||
| Frequency of listening to Radio | ||||||||||||||||
| Not at all | 1.00 | 1.00 | ||||||||||||||
| Less than once a week | 0.90 | 0.82 | 0.99 | 0.037 | 0.86 | 0.78 | 0.95 | 0.002 | ||||||||
| At least once a week | 0.92 | 0.83 | 1.01 | 0.089 | 0.92 | 0.83 | 1.02 | 0.099 | ||||||||
| Almost every day | 1.47 | 1.11 | 1.95 | 0.007 | 1.45 | 1.07 | 1.95 | 0.016 | ||||||||
| Frequency of watching Television | ||||||||||||||||
| Not at all | 1.00 | 1.00 | ||||||||||||||
| Less than once a week | 1.03 | 0.90 | 1.18 | 0.660 | 1.00 | 0.86 | 1.17 | 0.967 | ||||||||
| At least once a week | 0.95 | 0.84 | 1.06 | 0.333 | 0.90 | 0.80 | 1.02 | 0.104 | ||||||||
| Almost every day | 1.17 | 0.85 | 1.60 | 0.335 | 1.14 | 0.82 | 1.60 | 0.438 | ||||||||
| Healthcare utilization factors | ||||||||||||||||
| Place of delivery | ||||||||||||||||
| Home | 1.00 | |||||||||||||||
| Health facility | 1.38 | 1.21 | 1.57 | <0.001 | ||||||||||||
| Mode of delivery | ||||||||||||||||
| Non-caesarean | 1.00 | |||||||||||||||
| Caesarean section ⱡ | 0.28 | 0.22 | 0.36 | <0.001 | ||||||||||||
| Type of delivery assistance | ||||||||||||||||
| Health professional | 1.00 | |||||||||||||||
| Traditional birth attendant. | 0.77 | 0.60 | 0.98 | 0.037 | ||||||||||||
| Other untrained | 0.96 | 0.79 | 1.16 | 0.663 | ||||||||||||
| No one | 0.76 | 0.62 | 0.92 | 0.005 | ||||||||||||
| Antenatal Clinic visits | ||||||||||||||||
| None | 1.00 | |||||||||||||||
| 1–3 | 1.17 | 1.00 | 1.37 | 0.052 | ||||||||||||
| 4+ | 1.20 | 1.01 | 1.41 | 0.034 | ||||||||||||
^ divorce/separated/widowed.; ⱡ Caesarean section is a combination of both general and regional anesthesia.
Mothers who perceived their babies to be average or larger at birth were more likely to initiate breastfeeding within one hour of delivery than mothers who perceived their babies to be small. EIBF was significantly higher among mothers who frequently listened to the radio, who delivered their babies at the health facilities, and those mothers who had four or more antenatal clinic visits. EIBF was significantly higher with female births (adjusted OR = 1.17, 95% CI:1.00, 1.37; p = 0.046) than male births.
4. Discussion
Our results indicate that EIBF rates in the 13 ECOWAS are at a sub-optimum level, and need further improvement to fulfil the goal of optimal infant feeding in this subregion and the related Sustainable Development Goals (SDGs) of reducing neonatal mortality. During the study period (2010–2018), we noted the uneven prevalence of EIBF among infants aged between 0 and 23 months of age across the ECOWAS countries, ranging from a low of 17% (Guinea) to the highest of 61% (Togo). The reported rates of EIBF in this study are still well below the expected target of ≥70% recommended by the WHO [1] to further reduce infant mortality and morbidity in the sub-region by 25 deaths per 1000 live births by 2030. The wide variation in the rates of EIBF within the 13 ECOWAS countries may be due to socio-cultural, geographical location, and health inequalities, as well as economic issues among different populations. The study indicated that place of delivery (health institution), mode of delivery (vaginal delivery), ANC visits (≥4), and household wealth index (poorer or middle-class household) were significantly associated with EIBF within one hour of birth. Media exposure (newspaper/magazine or radio), baby size at birth (average and large), child’s sex (female), and first birth order were also found to be positively related to EIBF. Delayed introduction to breastfeeding was significant in six ECOWAS member states (Gambia, Nigeria, Senegal, Guinea, Burkina Faso, and Cote d’Ivoire).
Child delivery at health facilities predicts EIBF practices within one hour of the birth. This finding is consistent with previous studies conducted in Nepal [28], Nigeria [29], Namibia [30], and Ethiopia [31]. However, this is not unexpected given that the majority of health institutions across ECOWAS countries have adopted BFHI, which is overseen by skilled health providers (midwife, nurse, or doctor) whose core aim is to encourage and assist mothers in achieving optimal breastfeeding practices, including EIBF. It has been suggested that the presence of trained breastfeeding and delivery assistants in health institutions improved mothers’ EIBF practice [32]. This may have contributed to the substantial proportion (60%) of EIBF among mothers who gave birth at a hospital, as observed in the current study.
Similar to reports from earlier studies [22,29,30], the present study found that vaginal delivery was strongly correlated with EIBF practice when compared with caesarean birth. A plausible reason for this difference may be related to the adverse physical effects mothers and newborns often experience after CS surgery. Factors such as excruciating pain, anesthesia, prolonged labor, and related respiratory distress among newborns [33,34] may result in healthcare providers being preoccupied with helping both babies and mothers to stabilize rather than initiating breastfeeding [35,36].
Previously published studies indicated that pregnant women being unable to access or attend ANC services during pregnancy poses a significant barrier in initiating breastfeeding within one-hour post-birth [37,38]. However, in the present study, we found that mothers who had four or more ANC visits to a health institution prior to childbirth showed a greater likelihood of EIBF practice than those who had none or less than four ANC visits. This result is similar to that reported in past studies carried out in India [39] and Nepal [40]. Breastfeeding counseling and health messages received through the Baby-Friendly Hospital Initiative (BFHI) may have contributed to the increased likelihood of EIBF noted in the study. It has been suggested in previous work that breastfeeding counseling during ANC visits is positively related to the mother’s adherence to the WHO optimal breastfeeding practices [41,42]. Therefore, promoting and supporting ANC uptake in ECOWAS countries could ensure remarkable improvement in EIBF practices.
Newborn babies whose mother perceived their size to be average or larger had an increased likelihood of EIBF within one hour of birth compared with those who were perceived to be small or smaller size. This finding is consistent with a cross-sectional study carried out in Nigeria in 2016, which indicated that newborn babies perceived by their mothers as average or larger size at birth were more likely to be EIBF [29]. Also, a cross-sectional study done in Nepal in 2014 reported that newborn babies whose size was large at birth were significantly more likely to receive EIBF within one hour of birth in comparison with babies whose size was small [28]. The significantly increased odds of EIBF practice among newborn babies perceived to be of average or larger size in ECOWAS countries may be attributed to their physical maturity and associated proper coordination of the suction–deglutination–respiratory cycle and breast-seeking reflex [28]. Conversely, the immaturity of small babies often hinders the abilities required to initiate breastfeeding within one hour of delivery due to poor breast-seeking reflex and sucking inability [43]. Additionally, illness often leads to newborn babies being kept away from their mothers [44], resulting in the early introduction of complementary drinks. Notably, female births were found to be associated with EIBF within one hour of delivery. This outcome is similar to earlier reports in Sri Lanka [45] and Ethiopia [46], which found that male babies were less likely to receive early breastfeeding than their female counterparts. This gender difference in EIBF practice may be influenced by socio-cultural beliefs and require further assessment. However, previous studies have suggested that the practice of prelacteal feeds (or the act of given foods to newborn babies before initiating breastfeeding) in male babies is common and acceptable in African [8,47] and Asian countries [47,48].
Newborn babies born to mothers from a poor household had significantly higher odds of initiating breastfeeding within one hour of birth compared with those from a wealthy household. This finding contradicts previous reports, which indicated that mothers from wealthy households were more likely to initiate breastfeeding in the first hour of delivery [28,35]. Nevertheless, our finding is similar to those reported from Nepal [49] and Namibia [30]. The significantly higher odds of EIBF practice among poor mothers noted in the current study may be attributed to lack of access to infant formula or inability to buy costly complementary substitutes to breast milk, which may result in poor mothers depending solely on breastfeeding. It has also been suggested that mothers from wealthy households were more likely have an elective caesarean section, resulting in delayed initiation of breastfeeding within one hour of birth [50]. It was not unexpected that mothers who frequently watch television or listen to radio were more likely to initiate breastfeeding within one hour of delivery. This finding is consistent with previous studies [51,52]. Apart from health facilities, exposure to other information sources regarding breastfeeding practices during antenatal and postnatal care can also play a key role in encouraging women to practice early initiation of breastfeeding.
Similar to previous reports [30,46], we found that mothers who were having their first child were less likely to initiate breastfeeding within one hour of birth compared with those with two or more deliveries. This may be related to inexperience regarding breastfeeding and relatively poor use of maternal health services by first time mothers. As shown in a past study, earlier breastfeeding experience is correlated with both intention and timely breastfeeding initiation [53].
5. Limitations and Strengths
The following limitations of this study should be considered when making specific conclusions about its findings: (a) the study was unable to establish a causal relationship between the study characteristics and EIBF, as cross-sectional data was used to identify the predictors of EIBF; (b) recall and measurement errors may have overestimated or underestimated the findings of this study, as data regarding some of the study factors was obtained from mothers up to five years after childbirth; (c) there were some unmeasured coexisting factors, such as instrumental vaginal birth, cultural beliefs, and health professionals’ prior knowledge of EIBF or family dynamics, which may have also impacted the study findings. Additionally, detailed information concerning infant formula advertising via electronic or print media was not available at the time of the DHS survey. Despite the highlighted weaknesses, there are a number of strengths that should also be noted regarding this study. Firstly, the rate of EIBF was based on nationally representative data of 13 countries, and hence findings could be generalized across the subregion. Secondly, the results are comparable across the ECOWAS countries because all the variables used were similarly described across countries. Thirdly, the study used a combined nationally representative large sample size across the 13 ECOWAS, which meant that the potential impact of selection bias was minimal and unlikely to affect the estimates.
6. Conclusions
The findings of this study suggest that delivery in a hospital or health facility, vaginal delivery, frequent ANC visits (≥4), middle income household, access to electronic media (television or radio), average or larger baby size at birth, child’s sex (female), and first birth order were significantly associated with EIBF within one hour of birth in the 13 ECOWAS countries. In the ECOWAS subregion, it is crucial that integrated nutritional health promotion campaigns be conducted both at the community and individual levels. At the community level, the role of midwives and community health officers (CHO) in promoting breastfeeding practices appeared evident, with CHO antenatal home visits contributing to the early initiation of breastfeeding and empowering the community with greater knowledge of the nutrition and health requirements of children under two years of age. At the individual level, interventions to promote the involvement of family members during pregnancy and child birth are needed in ECOWAS and should particularly target young mothers and families from lower socioeconomic groups with lower rates of EIBF.
Acknowledgments
The authors are grateful to Measure DHS, ICF International, Rockville, Marylands, USA for providing the data for this study. GloMACH: Members are Kingsley E Agho, Felix A Ogbo, Thierno Diallo, Osita E Ezeh, Osuagwu L Uchechukwu, Pramesh R Ghimire, Blessing Akombi, Paschal Ogeleka, Tanvir Abir, Abukari I Issaka, Kedir Yimam Ahmed, Rose Victor, Deborah Charwe, Abdon Gregory Rwabilimbo, Daarwin Subramanee, Mehak Mehak, Nilu Nagdev and Mansi Dhami.
Author Contributions
Conceptualization, K.E.A. and F.A.O.; methodology, K.E.A. and O.K.E.; software, K.E.A.; validation, O.L.U., F.A.O. and O.K.E.; formal analysis, K.E.A. and P.R.G.; investigation, O.K.E., P.R.G.; resources, W.K.T.; data curation, F.A.O., P.R.G. and O.L.U.; writing—original draft preparation, K.E.A. and O.K.E.; writing—review and editing, O.L.U., W.K.T., G.J.S.; visualization, G.J.S., O.L.U.; supervision, K.E.A., W.K.T. and G.J.S.; project administration, O.K.E., P.R.G. and K.E.A.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest. K.E.A is a Guest Editor for the Nutrients Special Issue on “Breastfeeding: Short and Long-Term Benefits to Baby and Mother” and did not have any role in the journal review and decision-making process for this manuscript.
References
- 1.Collective G.B., UNICEF. World Health Organization . Global Breastfeeding Scorecard, 2017: Tracking Progress for Breastfeeding Policies and Programmes. World Health Organization; Geneva, Switzerland: 2017. [Google Scholar]
- 2.UNICEF . Levels and Trends in Child Mortality: Report 2011. WHO Estimates Developed by the UN Inter-Agency Group for Child Mortality Estimation; New York, NY, USA: 2011. [Google Scholar]
- 3.United Nations . Population Facts. Vol. 6. United Nations, Department of Economic and Social Affairs, Population Division; New York, NY, USA: 2017. pp. 1–2. [Google Scholar]
- 4.WHO. UNICEF . Planning Guide for National Implementation of the Global Strategy for Infant and Young Child Feeding. World Health Organization; Geneva, Switzerland: 2007. [Google Scholar]
- 5.WHO. UNICEF. Health WHODoCA . Handbook IMCI: Integrated Management of Childhood Illness. World Health Organization; Geneva, Switzerland: 2005. [Google Scholar]
- 6.Smith E.R., Hurt L., Chowdhury R., Sinha B., Fawzi W., Edmond K.M., Neovita Study Group Delayed breastfeeding initiation and infant survival: A systematic review and meta-analysis. PLoS ONE. 2017;12:e0180722. doi: 10.1371/journal.pone.0180722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Horta B.L., Victora C.G. Long-Term Effects of Breastfeeding. Volume 74 World Health Organization; Geneva, Switzerland: 2013. [Google Scholar]
- 8.Agho K.E., Ogeleka P., Ogbo F.A., Ezeh O.K., Eastwood J., Page A. Trends and Predictors of Prelacteal Feeding Practices in Nigeria (2003–2013) Nutrients. 2016;8:462. doi: 10.3390/nu8080462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Turner B. The Statesman’s Yearbook. Springer; Berlin, Germany: 2012. Economic Community of West African States (ECOWAS) pp. 59–60. [Google Scholar]
- 10.DHS . The Demographic and Health Survey Program. 2016 ed. United States Agency for International Development; Washington, DC, USA: 2016. [Google Scholar]
- 11.Tawiah-Agyemang C., Kirkwood B., Edmond K., Bazzano A., Hill Z. Early initiation of breast-feeding in Ghana: Barriers and facilitators. J. Perinatol. 2008;28:S46–S52. doi: 10.1038/jp.2008.173. [DOI] [PubMed] [Google Scholar]
- 12.Leung A.K.C., Sauve R.S. Breast is best for babies. J. Nat. Med. Assoc. 2005;97:1010–1019. [PMC free article] [PubMed] [Google Scholar]
- 13.Hanieh S., Ha T.T., Simpson J.A., Thuy T.T., Khuong N.C., Thoang D.D., Tran T.D., Tuan T., Fisher J., Biggs B.-A. Exclusive breast feeding in early infancy reduces the risk of inpatient admission for diarrhea and suspected pneumonia in rural Vietnam: A prospective cohort study. BMC Public Health. 2015;15:1166. doi: 10.1186/s12889-015-2431-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Arifeen S., Black R.E., Antelman G., Baqui A., Caulfield L., Becker S. Exclusive breastfeeding reduces acute respiratory infection and diarrhea deaths among infants in Dhaka slums. Pediatrics. 2001;108:e67. doi: 10.1542/peds.108.4.e67. [DOI] [PubMed] [Google Scholar]
- 15.Edmond K.M., Zandoh C., Quigley M.A., Amenga-Etego S., Owusu-Agyei S., Kirkwood B.R. Delayed breastfeeding initiation increases risk of neonatal mortality. Pediatrics. 2006;117:e380–e386. doi: 10.1542/peds.2005-1496. [DOI] [PubMed] [Google Scholar]
- 16.Mullany L.C., Katz J., Li Y.M., Khatry S.K., LeClerq S.C., Darmstadt G.L., Tielsch J.M. Breast-feeding patterns, time to initiation, and mortality risk among newborns in southern Nepal. J. Nutr. 2008;138:599–603. doi: 10.1093/jn/138.3.599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Exavery A., Kanté A.M., Hingora A., Phillips J.F. Determinants of early initiation of breastfeeding in rural Tanzania. Int. Breastfeed. J. 2015;10:27. doi: 10.1186/s13006-015-0052-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ogbo F.A., Page A., Agho K.E., Claudio F. Determinants of trends in breast-feeding indicators in Nigeria, 1999–2013. Public Health Nutr. 2015;18:3287–3299. doi: 10.1017/S136898001500052X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ogbo F.A., Agho K.E., Page A. Determinants of suboptimal breastfeeding practices in Nigeria: Evidence from the 2008 demographic and health survey. BMC Public Health. 2015;15:259. doi: 10.1186/s12889-015-1595-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Adewuyi E.O., Zhao Y., Khanal V., Auta A., Bulndi L.B. Rural-urban differences on the rates and factors associated with early initiation of breastfeeding in Nigeria: Further analysis of the Nigeria demographic and health survey, 2013. Int. Breastfeed. J. 2017;12:51. doi: 10.1186/s13006-017-0141-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mukora-Mutseyekwa F., Gunguwo H., Mandigo R.G., Mundagowa P. Predictors of early initiation of breastfeeding among Zimbabwean women: Secondary analysis of ZDHS 2015. Matern. Health Neonatol. Perinatol. 2019;5:2. doi: 10.1186/s40748-018-0097-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bisrat Z., Kenzudine A., Bossena T. Factors associated with early initiation and exclusive breastfeeding practices among mothers of infant’s age less than 6 months. J. Pediatr. Neonatal Care. 2017;7:00292. [Google Scholar]
- 23.Corsi D.J., Neuman M., Finlay J.E., Subramanian S. Demographic and health surveys: A profile. Int. J. Epidemiol. 2012;41:1602–1613. doi: 10.1093/ije/dys184. [DOI] [PubMed] [Google Scholar]
- 24.UNICEF. World Health Organization . Capture the Moment: Early Initiation of Breastfeeding: The Best Start for Every Newborn. UNICEF; New York, NY, USA: World Health Organization; Geneva, Switzerland: 2018. [Google Scholar]
- 25.Bortz K. WHO, UNICEF: 78 million newborns not breastfed within first hour after birth. Infect. Dis. Child. 2018;31:19. [Google Scholar]
- 26.Rutstein S.O., Johnson K. The DHS Wealth Index. DHS Comparative Reports No. 6. (ORC Macro, Calverton, MD, 2004) [(accessed on 20 August 2019)]; Available online: https://dhsprogram.com/pubs/pdf/CR6/CR6.pdf.
- 27.Rutstein S.O., Rojas G. Guide to DHS Statistics. ORC Macro; Calverton, MD, USA: 2006. [Google Scholar]
- 28.Adhikari M., Khanal V., Karkee R., Gavidia T. Factors associated with early initiation of breastfeeding among Nepalese mothers: Further analysis of Nepal Demographic and Health Survey, 2011. Int. Breastfeed. J. 2014;9:21. doi: 10.1186/s13006-014-0021-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Berde A.S., Yalcin S.S. Determinants of early initiation of breastfeeding in Nigeria: A population-based study using the 2013 demograhic and health survey data. BMC Pregnancy Childbirth. 2016;16:32. doi: 10.1186/s12884-016-0818-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ndirangu M., Gatimu S., Mwinyi H., Kibiwott D. Trends and factors associated with early initiation of breastfeeding in Namibia: Analysis of the demographic and health surveys 2000–2013. BMC Pregnancy Childbirth. 2018;18:171. doi: 10.1186/s12884-018-1811-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liben M.L., Gemechu Y.B., Adugnew M., Asrade A., Adamie B., Gebremedin E., Melak Y. Factors associated with exclusive breastfeeding practices among mothers in dubti town, afar regional state, northeast Ethiopia: A community based cross-sectional study. Int. Breastfeed. J. 2016;11:4. doi: 10.1186/s13006-016-0064-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Okafor I., Olatona F., Olufemi O. Breastfeeding practices of mothers of young children in Lagos, Nigeria. Niger. J. Paediatr. 2014;41:43–47. doi: 10.4314/njp.v41i1.8. [DOI] [Google Scholar]
- 33.Awi D., Alikor E. Barriers to timely initiation of breastfeeding among mothers of healthy full-term babies who deliver at the University of Port Harcourt Teaching Hospital. Niger. J. Clin. Pract. 2006;9:57–64. [PubMed] [Google Scholar]
- 34.Liben M.L., Yesuf E.M. Determinants of early initiation of breastfeeding in Amibara district, Northeastern Ethiopia: A community based cross-sectional study. Int. Breastfeed. J. 2016;11:7. doi: 10.1186/s13006-016-0067-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tilahun G., Degu G., Azale T., Tigabu A. Prevalence and associated factors of timely initiation of breastfeeding among mothers at Debre Berhan town, Ethiopia: A cross-sectional study. Int. Breastfeed. J. 2016;11:27. doi: 10.1186/s13006-016-0086-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hobbs A.J., Mannion C.A., McDonald S.W., Brockway M., Tough S.C. The impact of caesarean section on breastfeeding initiation, duration and difficulties in the first four months postpartum. BMC Pregnancy Childbirth. 2016;16:90. doi: 10.1186/s12884-016-0876-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Goldie S.J., Sweet S., Carvalho N., Natchu U.C.M., Hu D. Alternative strategies to reduce maternal mortality in India: A cost-effectiveness analysis. PLoS Med. 2010;7:e1000264. doi: 10.1371/journal.pmed.1000264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Darmstadt G.L., Bhutta Z.A., Cousens S., Adam T., Walker N., De Bernis L. Evidence-based, cost-effective interventions: How many newborn babies can we save? Lancet Neonatal Survival Steering Team. Lancet. 2005;365:977–988. doi: 10.1016/S0140-6736(05)71088-6. [DOI] [PubMed] [Google Scholar]
- 39.Senanayake P., O’Connor E., Ogbo F.A. National and rural-urban prevalence and determinants of early initiation of breastfeeding in India. BMC Public Health. 2019;19:896. doi: 10.1186/s12889-019-7246-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Subedi N., Paudel S., Rana T., Poudyal A. Infant and young child feeding practices in Chepang communities. J. Nepal Health Res. Counc. 2012;10:141–146. [PubMed] [Google Scholar]
- 41.El Shafei A.M.H., Labib J.R. Determinants of exclusive breastfeeding and introduction of complementary foods in rural Egyptian communities. Glob. J. Health Sci. 2014;6:236–244. doi: 10.5539/gjhs.v6n4p236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mekuria G., Edris M. Exclusive breastfeeding and associated factors among mothers in Debre Markos, Northwest Ethiopia: A cross-sectional study. Int. Breastfeed. J. 2015;10:1. doi: 10.1186/s13006-014-0027-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Walker M. Breastfeeding the late preterm infant. J. Obstet. Gynecol. Neonatal Nurs. 2008;37:692–701. doi: 10.1111/j.1552-6909.2008.00293.x. [DOI] [PubMed] [Google Scholar]
- 44.Mulready-Ward C., Sackoff J. Outcomes and factors associated with breastfeeding for <8 weeks among preterm infants: Findings from 6 states and NYC, 2004–2007. Matern. Child Health J. 2013;17:1648–1657. doi: 10.1007/s10995-012-1178-5. [DOI] [PubMed] [Google Scholar]
- 45.Senarath U., Siriwardena I., Godakandage S.S., Jayawickrama H., Fernando D.N., Dibley M.J. Determinants of breastfeeding practices: An analysis of the Sri Lanka Demographic and Health Survey 2006–2007. Matern. Child Nutr. 2012;8:315–329. doi: 10.1111/j.1740-8709.2011.00321.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.John J.R., Mistry S.K., Kebede G., Manohar N., Arora A. Determinants of early initiation of breastfeeding in Ethiopia: A population-based study using the 2016 demographic and health survey data. BMC Pregnancy Childbirth. 2019;19:69. doi: 10.1186/s12884-019-2211-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nguyen P.H., Keithly S.C., Nguyen N.T., Nguyen T.T., Tran L.M., Hajeebhoy N. Prelacteal feeding practices in Vietnam: Challenges and associated factors. BMC Public Health. 2013;13:932. doi: 10.1186/1471-2458-13-932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Khanal V., Adhikari M., Sauer K., Zhao Y. Factors associated with the introduction of prelacteal feeds in Nepal: Findings from the Nepal demographic and health survey 2011. Int. Breastfeed. J. 2013;8:9. doi: 10.1186/1746-4358-8-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Khanal V., Scott J., Lee A., Karkee R., Binns C. Factors associated with early initiation of breastfeeding in Western Nepal. Int. J. Environ. Res. Public Health Nutr. 2015;12:9562–9574. doi: 10.3390/ijerph120809562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rowe-Murray H.J., Fisher J.R. Baby friendly hospital practices: Cesarean section is a persistent barrier to early initiation of breastfeeding. Birth. 2002;29:124–131. doi: 10.1046/j.1523-536X.2002.00172.x. [DOI] [PubMed] [Google Scholar]
- 51.Tamiru D., Mohammed S. Maternal knowledge of optimal breastfeeding practices and associated factors in rural communities of Arba Minch Zuria. Int. J. Nutr. Food Sci. 2013;2:122–129. doi: 10.11648/j.ijnfs.20130203.15. [DOI] [Google Scholar]
- 52.Hailemariam T.W., Adeba E., Sufa A. Predictors of early breastfeeding initiation among mothers of children under 24 months of age in rural part of West Ethiopia. BMC Public Health. 2015;15:1076. doi: 10.1186/s12889-015-2420-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lessen R., Crivelli-Kovach A. Prediction of initiation and duration of breast-feeding for neonates admitted to the neonatal intensive care unit. J. Perinat. Neonatal Nurs. 2007;21:256–266. doi: 10.1097/01.JPN.0000285817.51645.73. [DOI] [PubMed] [Google Scholar]