Abstract
Globally, there is increasing usage and legalization of cannabis. In addition to its reported therapeutic effects, cannabis has several health risks which are not clearly defined. Erectile dysfunction (ED) is the most common male sexual disorder and there are plausible mechanisms linking cannabis use to ED. No attempt has been made to collate the literature on this topic. The aim of this review was to summarize the prevalence and risk of ED in cannabis users compared to controls.
A systematic review of major databases from inception to January 1, 2019, without language restriction, was undertaken to identify studies investigating cannabis use and presence of ED. The analysis compared the prevalence of ED in cannabis users versus controls. Consequently, the odds ratio (OR) with 95% confidence intervals (CI) was calculated, applying a random-effect model.
Five case–control studies were included with data from 3,395 healthy men, 1,035 using cannabis (smoking) and 2,360 nonusers. The overall prevalence of ED in cannabis users was 69.1% (95% CI: 38.0–89.1), whilst the correspondent figure in controls was 34.7% (95% CI: 20.3–52.7). The OR of ED in cannabis users was almost four times that of controls (OR = 3.83; 95% CI: 1.30–11.28; p = .02), even if characterized by high heterogeneity (I2 = 90%) and the prediction intervals overlapped 1.00 (95% CI: 0.35–7.26).
Data suggest that ED is twice as high in cannabis users compared to controls. Future longitudinal research is needed to confirm/refute this and explore if a dose–response relationship between cannabis and ED may be evident.
Keywords: Cannabis, erectile dysfunction, prevalence, meta-analysis, systematic review
The term cannabis is used to denote several psychoactive preparations of the Cannabis sativa plant, of which the major psychoactive constituent is ∆-9 tetrahydrocannabinol (THC) (Pertwee, 2008). It is the most widely cultivated, trafficked and consumed substance, with approximately 147 million people, 2.5% of the world population, consuming cannabis annually (Cohen et al., 2019). Cannabinoids, which are compounds present in the Cannabis sativa and structurally similar to THC, are commonly used in medicine.
There is emerging evidence in the scientific literature about the potential therapeutic benefits of cannabis for conditions such as pain, multiple sclerosis, epilepsy, cancer and weight loss, and moderate-quality evidence for Parkinson disease, Alzheimer disease, Huntington’s disease, glaucoma, anxiety, and depressive symptoms (Fraguas-Sanchez & Torres-Suarez, 2018; Scherma et al., 2018; Zuardi, 2006). Although cannabis has been used for therapeutic purposes and has wide-ranging potential uses in medicine, with increasing legalization, the psychoactive properties limit its adoption. In some countries, cannabis is illegal (most of Europe), in others, it is considered a “soft narcotic” (UK and USA) or legal (mainly countries in South America, Asia, Africa) (Nestoros et al., 2017). The main concerns about legalization are due to the uncertain consequences it could have on public health (Kilmer, 2017). In fact, cannabis use can result in several adverse health outcomes. Cannabis intoxication seems to impair cognitive and psychomotor function and can increase the risk of psychotic symptoms, including addiction and cannabis use disorder (Volkow et al., 2014). Moreover, smoking cannabis can negatively impact the respiratory system, from the trachea epithelium to lung function impairment (Cohen et al., 2019). Finally, when cannabis is used during pregnancy, it has been reported to be associated with harmful effects on fetal development and reduction in birth weight (Fried, 1993). Moreover, there has been limited emerging evidence that cannabis use may be associated with erectile dysfunction (ED) (Shamloul & Bella, 2011). There are two main mechanisms hypothesized to explain this link: a central pathway via the hypothalamus and a peripheral pathway on the corpus cavernosum (Argiolas & Melis, 2005; Gratzke et al., 2010). ED is the most common sexual health issue in men and is associated with a substantial range of mental, physical, and psychological adverse effects, including anxiety, low mood, and reductions in couple’s quality of life (Wiltink et al., 2010; Yafi et al., 2016). Thus, understanding emerging risk factors for ED, particularly in relation to the increasing legalization of cannabis, is highly important. Given this background, we aimed to summarize the prevalence of ED in cannabis users compared to controls through a meta-analytic approach.
Methods
Data Sources and Literature Search Strategy
This systematic review adhered to the PRISMA (Liberati et al., 2009) and MOOSE (Stroup et al., 2000) statements and followed a structured but unpublished protocol. Two investigators (NV and DP) independently conducted a literature search using PubMed, EMBASE, SCOPUS, Cochrane Central Register of Controlled Trials and Clinicaltrials.gov, without language restriction, from database inception to January 18, 2019 for studies investigating cannabis use and presence of ED. Any inconsistencies were resolved by consensus with a third author (MS).
In PubMed, the following search strategy was used: “(cannabis OR cannabi* OR Marihuana OR Marihuanas OR Marijuana OR Marijuanas OR Ganja OR Hashish OR 9tetrahydrocannabinol* OR delta3-thc OR sp-104 OR sp104 OR 1972-08-3 OR Dronabinol OR Marinol OR dronabinolum OR deltanyne OR tetrahydrocann* OR cannabinoid* OR canabinoid*) AND (ED OR erectile function OR sexual dysfunction OR sexual function)”. Similar search strategies were used in the other databases. Conference abstracts and reference lists of included articles were hand-searched to identify and potential additional relevant articles.
Study Selection
Inclusion criteria for this meta-analysis were: (i) observational studies (case–control, cross-sectional and prospective) reporting the prevalence/incidence of ED in people using cannabis versus nonusers; (ii) using a validated tool for the detection of ED (e.g., the International Index of Erectile Function, IIEF-5) (Namazi et al., 2018) and (iii) reporting the use of cannabis, also through self-reported information. Studies were excluded if (i) they did not include humans and (ii) a control group of cannabis users was not included.
Data Extraction
Two independent investigators (NV and DP) extracted key data from the included articles in a standardized excel sheet. A third independent investigator (MS) checked the extracted data. For each article, data were extracted regarding study authors, year of publication, country in which the study was conducted, condition, number of participants, participant demographics (mean age), and type of cannabis used.
Outcomes
The primary outcome was the prevalence of ED in cannabis users compared to controls.
Assessment of Study Quality
Study quality was assessed by two investigators (DP and MS) using the Newcastle-Ottawa Scale (NOS) (Luchini et al., 2017; Wells et al., 2012). A third reviewer was available for mediation (NV). The NOS assigns a maximum of nine points based on three quality parameters: selection, comparability and outcome.
Data Synthesis and Statistical Analysis
All analyses were performed using Comprehensive Meta-Analysis (CMA) 2.
The analysis compared the prevalence of ED in cannabis users versus controls. Consequently, the odds ratio (OR) with its 95% confidence intervals (CIs) was calculated, applying a random-effect model (Higgins & Green, 2008).
Heterogeneity across studies was assessed by the I2 metric. Given significant heterogeneity (I2 ≥ 50% and/or p < .05) (Higgins et al., 2011) and having at least 10 studies for each outcome, we planned to run some meta-regression analyses. However, the primary outcome included only five studies and so these analyses were not possible. The prediction interval (PIs) and its 95% CI was also estimated, which further accounts for between-study effects and estimates the certainty of the association if a new study addresses that same association (Higgins et al., 2009; IntHout et al., 2016).
Publication bias was assessed by a visual inspection of funnel plots and calculating the Egger bias test (Egger et al., 1997). In case of publication bias (p < .10), the trim and fill-analysis (Duval & Tweedie, 2000) was applied for overcoming this bias. Finally, the fail-safe number (i.e., the number of studies for nullifying a significant result) (Boikos et al., 2014) was reported.
For all analyses, a p-value < .05 was considered statistically significant.
Results
Search Results
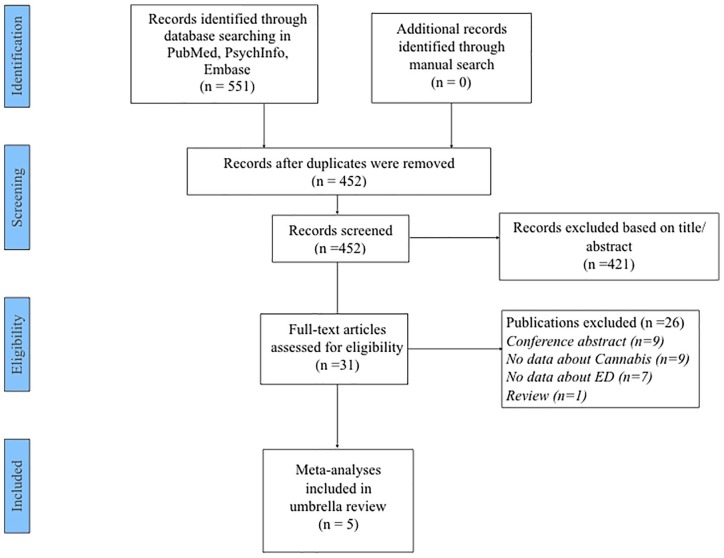
As presented in Figure 1, the searches yielded 452 nonduplicated articles. After excluding 421 articles based on title/abstract review, 31 articles were retrieved for full text review and 5 articles (Aldemir et al., 2017; Aversa et al., 2008; Elbendary et al, 2009; Kumsar et al., 2016; Mialon et al., 2012) were included in the qualitative/quantitative synthesis.
Figure 1.
PRISMA flow-chart.
Study and Patient Characteristics
The five case–control studies included a total of 3,395 healthy men (1,035 using cannabis in the form of smoking and 2,360 nonusers). Three studies were carried out in the Middle East and two in Europe. The IIEF5 was used as a tool for the detection of ED in all the five studies. Four studies compared healthy subjects with patients with ED, whilst Aversa et al. (2008) compared patients affected by organic and nonorganic ED. The mean age of the participants was 20.1 (SD = 1.5). In all studies, the consumption of cannabis has been through smoking. Only one study assessed the duration of cannabis use in months (Aldemir et al., 2017).
The median quality of the studies was six (range: 5–7), indicating a good quality of the studies, according to the NOS (Table 1).
Table 1.
Descriptive Characteristics of the Studies Included.
| Author (year) | Country | Type of cannabis used | Total population (cannabis; controls) | Mean age of the population (standard deviation) | NOS |
|---|---|---|---|---|---|
| Aldemir et al. (2017) | Turkey | Smoking | 80 (47; 33) | NA | 6 |
| Aversa et al. (2008) | Italy | Smoking | 64 (24; 40) | 30 (2) | 6 |
| Elbendary et al. (2009) | Egypt | Smoking | 686 (66; 620) | NA | 7 |
| Kumsar et al. (2016) | Turkey | Smoking | 80 (47; 33) | NA | 5 |
| Mialon et al. (2012) | Switzerland | Smoking | 2485 (845; 1640) | 19.6 (1.3) | 5 |
| Total | 3395 (1035; 2360) | 20.1 (1.5) |
NOS: Newcastle Ottawa Scale.
Prevalence and Odds Ratio of ED in Cannabis Users Versus Controls
The overall prevalence of ED in cannabis users was 69.1% (95% CI: 38.0–89.1), whilst the correspondent figure in controls was 34.7% (95% CI: 20.3–52.7).
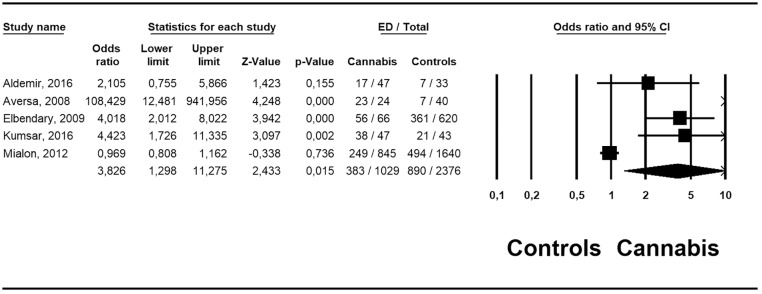
Figure 2 presents the odds ratio of ED in cannabis users versus controls. The odds ratio of ED in cannabis users was almost four times than controls (OR = 3.83; 95% CI: 1.30–11.28; p = .02). This outcome was characterized by a high heterogeneity (I2 = 90%). In a sensitivity analysis, after removing a study that was an outlier (Aversa et al., 2008), the recalculated OR was 2.34 (95% CI: 1.04–5.94; p = .03; I2 = 88%. The prediction intervals overlapped 1.00 (95% CI: 0.35–7.26).
Figure 2.
Odds ratio of erectile dysfunction in people using cannabis compared to controls.
The presence of a possible publication bias (Egger’s test: 3.92 ± 0.81; p = .02) was observed. However, the trim and fill analysis did not change this estimate. The fail-safe number was 35, indicating a low number of studies for bringing the p-value over the alpha.
Discussion
This is the first systematic review and meta-analysis to assess cannabis use and the prevalence of ED. This meta-analysis included five case–control studies with a total of 3,395 men, demonstrating a higher prevalence of ED in cannabis users (more than two-thirds) and leading to four times increased odds ratio of ED in cannabis users compared to controls. These results were characterized by high heterogeneity as shown by the I2 and the prediction intervals, suggesting that some differences in the association between cannabis use and ED exist.
Considering that the causes of ED may be psychological, organic or most commonly a mix of both, different hypotheses can explain this outcome. One of the possible mechanisms is attributed to the endocannabinoid system through the binding of receptors in the paraventricular nucleus of the hypothalamus which regulates erectile function and sexual behavior of males (Argiolas et al., 2005). This mechanism could also explain why cannabis can improve sexual function in some patients affected by conditions or symptoms such as depression, anxiety disorder and pain (Gobbi et al., 2019; Huang et al., 2016). Growing evidence, both in animal and human studies, reported a peripheral effect of cannabis on ED, specifically on corpus cavernosum where cannabinoid receptors are present (Gratzke et al., 2010; Melis et al., 2006). Future longitudinal studies are necessary to confirm/refute this and explore the potential differing effects based on the type, potency and frequency of cannabis used.
The effects of cannabis on male health are, to date, poorly investigated both in terms of fertility and sexual health. Regarding fertility, contrasting data have been reported on testicular function and, whereas some authors highlight that smoking cannabis once per week is enough to impair the testicular function (Gundersen et al., 2015), Nassan et al. (2019) recently observed no sperm quality differences between cannabis user and controls. Cannabis seems to be clearly related to multiple adverse sexual health outcomes, but scientific evidence is limited. Cannabis use is associated with earlier and more frequent sexual activity, having multiple and causal sexual partners, inconsistent contraceptive use and being diagnosed with a sexually transmissible infection (Smith et al., 2010). Surprisingly, only a few studies reported the association between cannabis and ED using validated tools. At a time when there is increasing legalization of cannabis, these results suggest that cannabis use may be associated with ED, a particularly undesirable outcome in males (McCabe & Matic, 2008). Given that ED is associated with a range of adverse health outcomes in males, understanding this potential relationship could be a considerable public health issue (Rajanahally et al., 2019).
The main limitation of the present study is that few studies were available and those were contained small samples. Only one article reported information on duration (mean 87.7 months) of cannabis use identifying a slight negative correlation between sexual intercourse satisfaction and duration of cannabis use (Aldemir et al., 2017). The sample characterization of the study by Aversa et al., different from others, did not compare healthy participants with individuals experiencing ED, rather participants affected by organic and nonorganic ED. Finally, there were only case–control studies that could be affected by reverse causality, that is people with ED more frequently used cannabis. Despite limitations, this study has strengths. In fact, as well as being the first systematic review and meta-analysis on this topic, this study has considered objective validated tools to asses ED. This study is focused on two emerging conditions that represent an important public health concern: ED which is one of the most common worldwide male sexual disorders and is projected to affect 322 million men in 2025 (Shamloul et al., 2011) and cannabis use, which estimates suggest between 2.7% to 4.9% of the population have at least tried (Anthony et al., 2017).
In conclusion, considering the high prevalence of ED and cannabis use and the potential harmful effects of cannabis use on male sexual and general health, it is necessary to increase and improve the knowledge on this topic in order to achieve a general consensus on the best clinical and public health strategies.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: BS is supported by the Health Education England and the National Institute for Health Research HEE/ NIHR ICA Programme Clinical Lectureship (ICA-CL-2017-03-001). The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the National Institute for Health Research, the Department of Health and Social Care or the Italian Agency for Development Cooperation.
ORCID iD: Damiano Pizzol  https://orcid.org/0000-0003-4122-0774
https://orcid.org/0000-0003-4122-0774
References
- Aldemir E., Akyel B., Keskin Gokcelli D., Celikay H., Altintoprak A. E., Coskunol H. (2017). A controlled study of sexual function in men with cannabis use disorder: A brief report. Journal of Substance Use, 22(5), 490–493. [Google Scholar]
- Anthony J. C., Lopez-Quintero C., Alshaarawy O. (2017). Cannabis epidemiology: A selective review. Current Pharmaceutical Design, 22(42), 6340–6352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Argiolas A., Melis M. R. (2005). Central control of penile erection: Role of the paraventricular nucleus of the hypothalamus. Progress Neurobiology, 76(1), 1–21. [DOI] [PubMed] [Google Scholar]
- Aversa A., Rossi F., Francomano D., Bruzziches R., Bertone C., Santiemma V., Spera G. (2008). Early endothelial dysfunction as a marker of vasculogenic erectile dysfunction in young habitual cannabis users. International Journal of Impotence Research, 20(6), 566–573. [DOI] [PubMed] [Google Scholar]
- Boikos C., De Serres G., Lands L. C., Boucher F. D., Tapiéro B., Daigneault P., Quach C. (2014). Safety of live-attenuated influenza vaccination in cystic fibrosis. Pediatrics, 134(4), e983–e991. [DOI] [PubMed] [Google Scholar]
- Cohen K., Weizman A., Weinstein A. (2019). Positive and negative effects of cannabis and cannabinoids on health. Clinical Pharmacology & Therapeutics, 105(5), 1139–1147. [DOI] [PubMed] [Google Scholar]
- Duval S., Tweedie R. (2000). Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics, 56(2), 455–463. [DOI] [PubMed] [Google Scholar]
- Egger M., Davey Smith G., Schneider M., Minder C. (1997). Bias in meta-analysis detected by a simple, graphical test. British Medical Journal, 315(7109), 629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elbendary M. A., El-Gamal O. M., Salem K. A. (2009). Analysis of risk factors for organic erectile dysfunction in Egyptian patients under the age of 40 years. Journal of Andrology, 30(5), 520–524. [DOI] [PubMed] [Google Scholar]
- Fraguas-Sanchez A. I., Torres-Suarez A. I. (2018). Medical use of cannabinoids. Drugs, 78(16), 1665–1703. [DOI] [PubMed] [Google Scholar]
- Fried P. A. (1993). Prenatal exposure to tobacco and marijuana: Effects during pregnancy, infancy, and early childhood. Clinical Obstetrics and Gynecolology, 36(2), 319–337. [DOI] [PubMed] [Google Scholar]
- Gobbi G., Atkin T., Zytynski T., Wang S., Askari S., Boruff J., Ware M., Marmorstein N., Cipriani A., Dendukuri N., Mayo N. (2019). Association of cannabis use in adolescence and risk of depression, anxiety, and suicidality in young adulthood: A systematic review and meta-analysis. JAMA Psychiatry, 76(4), 426–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratzke C., Christ G. J., Stief C. G., Andersson K. E., Hedlund P. (2010). Localization and function of cannabinoid receptors in the corpus cavernosum: Basis for modulation of nitric oxide synthase nerve activity. European Urolology, 57(2), 342–348. [DOI] [PubMed] [Google Scholar]
- Gundersen T. D., Jorgensen N., Andersson A. M., Bang A. K., Nordkap L., Skakkebæk N. E., Priskorn L., Juul A., Jensen T. K. (2015). Association between use of marijuana and male reproductive hormones and semen quality: A study Among 1,215 healthy young men. American Journal of Epidemiology, 182(6), 473–481. [DOI] [PubMed] [Google Scholar]
- Higgins J. P., Altman D. G., Gøtzsche P. C., Jüni P., Moher D., Oxman A. D., Savovic J., Schulz K. F., Weeks L., Sterne J. A; Cochrane Bias Methods Group; Cochrane Statistical Methods Group. (2011). The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. British Medical Journal, 34(3), d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins J. P., Green S. (Eds.). (2008). Cochrane Handbook for Systematic Reviews of Interventions. Version 5. Cochrane Book Series. The Cochrane Collaboration and John Wiley & Sons Ltd, England. [Google Scholar]
- Higgins J. P., Thompson S. G., Spiegelhalter D. J. (2009). A re-evaluation of random-effects meta-analysis. Journal of the Royal Statistical Society. Series A (Statics in Society), 172(1), 137–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang W. J., Chen W. W., Zhang X. (2016). Endocannabinoid system: Role in depression, reward and pain control. Molecular Medicine Reports, 14(4), 2899–2903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IntHout J., Ioannidis J. P. A., Rovers M. M., Goeman J. J. (2016). Plea for routinely presenting prediction intervals in meta-analysis. British Medical Journal, 6(7), e010247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilmer B. (2017). Recreational cannabis: Minimizing the health risks from legalization. The New England Journal of Medicine, 376(8), 705–707. [DOI] [PubMed] [Google Scholar]
- Kumsar N. A., Kumsar S., Dilbaz N. (2016). Sexual dysfunction in men diagnosed as substance use disorder. Andrologia, 48(10), 1229–1235. [DOI] [PubMed] [Google Scholar]
- Liberati A., Altman D. G., Tetzlaff J., Mulrow C., Gøtzsche P. C., Ioannidis J. P., Clarke M., Devereaux P. J., Kleijnen J., Moher D. (2009). The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Medicine, 6(7), e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luchini C., Brendon S., Solmi M., Veronese N. (2017). Assessing the quality of studies in meta-analyses: Advantages and limitations of the Newcastle Ottawa Scale. World Journal of Meta-Analysis, 5(4), 80–84. [Google Scholar]
- McCabe M. P., Matic H. (2008). Erectile dysfunction and relationships: Views of men with erectile dysfunction and their partners. Sexual and Relationship Therapy, 23(1), 51–60. [Google Scholar]
- Melis M. R., Succu S., Mascia M. S., Sanna F., Melis T., Castelli M. P., Argiolas A. (2006). The cannabinoid receptor antagonist SR-141716A induces penile erection in male rats: Involvement of paraventricular glutamic acid and nitric oxide. Neuropharmacology, 50(2), 219–228. [DOI] [PubMed] [Google Scholar]
- Mialon A., Berchtold A., Michaud P. A., Gmel G., Suris J. C. (2012). Sexual dysfunctions among young men: Prevalence and associated factors. Journal of Adolescent Health, 51(1), 25–31. [DOI] [PubMed] [Google Scholar]
- Namazi N., Larijani B., Azadbakht L. (2018). Dietary inflammatory index and its association with the risk of cardiovascular diseases, metabolic syndrome, and mortality: A systematic review and meta-analysis. Hormone and Metabolic Research, 50(5), 345–358. [DOI] [PubMed] [Google Scholar]
- Nassan F. L., Arvizu M., Minguez-Alarcon L., Williams P. L., Attaman J., Petrozza J., Hauser R., Chavarro J.; EARTH Study Team. (2019). Marijuana smoking and markers of testicular function among men from a fertility centre. Human Reproduction, 34(4), 715–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nestoros J. N., Vakonaki E., Tzatzarakis M. N., Alegakis A., Skondras M. D., Tsatsakis A. M. (2017). Long lasting effects of chronic heavy cannabis abuse. American Journal of Addiction, 26(4), 335–342. [DOI] [PubMed] [Google Scholar]
- Pertwee R. G. (2008). The diverse CB1 and CB2 receptor pharmacology of three plant cannabinoids: Delta9-tetrahydrocannabinol, cannabidiol and delta9-tetrahydrocannabivarin. British Journal of Pharmacology, 153(2), 199–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajanahally S., Raheem O., Rogers M., Brisbane W., Ostrowski K., Lendvay T., Walsh T. (2019). The relationship between cannabis and male infertility, sexual health, and neoplasm: A systematic review. Andrology, 7(2), 139–147. [DOI] [PubMed] [Google Scholar]
- Scherma M., Masia P., Deidda M., Fratta W., Tanda G., Fadda P. (2018). New perspectives on the use of cannabis in the treatment of psychiatric disorders. Medicines (Basel), 5(4), E107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shamloul R., Bella A. J. (2011). Impact of cannabis use on male sexual health. The Journal of Sexual Medicine, 8(4), 971–975. [DOI] [PubMed] [Google Scholar]
- Smith A. M., Ferris J. A., Simpson J. M., Shelley J., Pitts M. K., Richters J. (2010). Cannabis use and sexual health. The Journal of Sexual Medicine, 7(2 Pt 1), 787–793. [DOI] [PubMed] [Google Scholar]
- Stroup D. F., Berlin J. A., Morton S. C., Olkin I., Williamson G. D., Rennie D., Moher D., Becker B. J., Sipe T. A., Thacker S. B. (2000). Meta-analysis of observational studies in epidemiology: A proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. Journal of American Medical Association, 283(15), 2008–2012. [DOI] [PubMed] [Google Scholar]
- Volkow N. D., Baler R. D., Compton W. M., Weiss S. R. (2014). Adverse health effects of marijuana use. The New England Journal of Medicine, 370(23), 2219–2227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells G. A., Shea B., O’Connell D., Peterson J., Welch V., Losos M., Tugwell P. (2012). The Newcastle-Ottawa Scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses. Available July 2019, from http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
- Wiltink J., Subic-Wrana C., Tuin I., Weidner W., Beutel M. E. (2010). Repressive coping style and its relation to psychosocial distress in males with erectile dysfunction. The Journal of Sexual Medicine, 7(6), 2120–2129. [DOI] [PubMed] [Google Scholar]
- Yafi F. A., Jenkins L., Albersen M., Corona G., Isidori A. M., Goldfarb S., Maggi M., Nelson C. J., Parish S., Salonia A., Tan R., Mulhall J. P., Hellstrom W. J. (2016). Erectile dysfunction. Nature Reviews Disease Primers, 2, 16003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuardi A. W. (2006). History of cannabis as a medicine: A review. Brazilian Journal of Psychiatry, 28(2), 153–157. [DOI] [PubMed] [Google Scholar]