Abstract
The cancer incidence burden is expected to rise to over 85% in sub-Saharan Africa by 2030.1 This alarming trend underscores the need to develop evidence-based interventions that can effectively handle this volatile epidemic. The evidence generation entails the collection of adequate information on burden, pattern, and prevalence of cancer relative to capacity to promote effective decision-making. Accordingly, this study documents the prevalence and types of cancer in Kenya (demand side) and to determine the diagnostic and treatment capacity of the various health facilities to handle cancer cases (supply side). To investigate demand and supply factors for cancer control, the study surveyed 7 of the 47 counties in Kenya during 2013 to 2014. It sampled 1048 patients with cancer records and 12 health-care facilities. The study found that the most frequent age for female patients was at age 52, while for men was at age 62. The most prevalent cancer in women was breast cancer and cancer of the cervix, while for men was cancer of the esophagus and prostate. It was also found that children and rural populations were more vulnerable than it was thought, hence defying the local perception that cancer inflicts only adults and those in urban areas. Accessing cancer screening and treatment was one of the major hurdles as most cancer care services in Kenya were concentrated within a 5-km radius of each other in Nairobi. The limited capacity with respect to diagnosis and treatment has implications to issues of access, proximity, and availability. It is critical that policy makers and practitioners closely review the current public and individual perceptions about the cancer problems and mitigation strategies.
Keywords: cancer detection, cancer prevalence, cancer prevention, cancer risk, cancer screening, cancer treatment
Introduction
Although developing countries bear 80% of the cancer burden, only about 5% of global resources devoted to cancer are found in these countries yet the burden of cancer incidences in sub-Saharan Africa is expected to grow to over 85% by 2030.1,2 Cancer is the third leading cause of death in Africa, after infectious and cardiovascular diseases. According to the World Health Organization, only 50% of low- and middle-income countries have operational National Cancer Control Plans.3 The annual incidence of cancer in Kenya is about 28 000 new cases with an annual mortality of 22 000 cases, that is, 78.5% of the victims do not survive.4 Like the African experience, cancer is also said to be the third leading cause of death in Kenya, after infectious diseases and cardiovascular diseases. In 2005, cancer deaths were estimated at 18 000 people and by 2014, it was estimated at 22 000. Cancer contributed 7% of the total national mortality each year. The annual incidence of cancer was about 28 000 new cases with an annual mortality of 22 000 cases (ie, 78.5% of the victims did not survive).4 Most of these data are captured by respective cancer registries.5 For example, the Eldoret Cancer registry was established in 1999 in the Faculty of Medical Sciences, Department of Hematology and Blood Transfusion of Moi University’s Teaching and Referral Hospital. The registry records details of all patients with cancer diagnosed and treated in hospitals of Eldoret town. Another cancer registry is the Nairobi Cancer Registry, established in 2001 in partnership with the Ministry of Health (MOH) and Kenya Medical Research Institute (KEMRI). Although the Nairobi Cancer Registry has attempted to collect data with respect to the prevalence of types of cancer based on participating facilities in Nairobi, there is still a large gap for such coordinated data at national level. Hence, there is a need for documentation of demographic distribution of cancer cases and to determine the specific types and nature of cancers in Kenya.6 There has also not been any substantive research done to establish the capacity of cancer diagnostics and treatment in the country, including identifying existing capacities for institutions dealing with cancer. Accordingly, this study fills these gaps in the cancer research literature in Kenya by investigating demand-side and supply-side issues for cancer control. The purpose of the study is 2-fold: to document the prevalence and types of cancer in Kenya (demand side) and to determine the diagnostic and treatment capacity of the various health facilities to handle cancer cases (supply side).
Kenya is facing the growing high demand for cancer treatments, but the nation’s very limited supply capacity with respect to diagnosis and treatment poses serious health-care policy challenges to the government. The problem is that on the demand side, the number of patients has been progressively growing and expected to continue, especially cancers of the cervix, breast, esophagus, and prostate. However, on the supply side, the availability of facilities, equipment, and experts appear not to be growing at a commensurate rate.7 Therefore, the availability problem is a resource problem that would require sourcing and equipping of medical facilities with screening and treatment services. This study documents the extent to which the demand-side and supply-side issues are being incorporated into the cancer intervention strategies in Kenya. It documents the demographic distribution of cancer cases and determines the specific types and nature of cancers in 10 selected counties. It also examines the capacity of cancer diagnostics and treatment in the selected counties. It concludes with demand-side and supply-side recommended strategies for earlier detection, prevention, and treatment, with respect to accessibility, proximity, and resource availability.
Methods
Research Design and Population
The study used a descriptive research design to examine the following demand- and supply-side objectives. On the demand side, objective 1 was to document demographic distribution of cancer cases in 10 selected counties and objective 2 was to determine the specific types and nature of cancers in 10 selected counties. On the supply side, the objective was to establish the capacity of cancer diagnosis and treatment in the selected counties, including identifying existing institutions dealing with cancer. To operationalize these objectives, the study used a descriptive research method for assessment of prevalence and types of cancer as well as the capacity for diagnosis and treatment of cancer.
On the demand side, “cancer prevalence” was assessed by identifying the types of treatment being sought. On the supply side, the “capacity” of cancer diagnosis and treatment was assessed by data from practitioners who provided information about the infrastructure, equipment, and types of testing and treatment available at their facility.
The study sought to retrospectively collate population-based data on cancer in Kenya captured in respective cancer registries to supplement primary data. The population comprised of health facilities, patients with cancer records, and cancer survivors in selected counties as identified by the Africa Cancer Foundation. This study used this framework to elicit the classification, frequency, and pattern of distribution of the cases of cancer. The typology was to include various types of hematological and nonhematological malignancies.
Data Collection
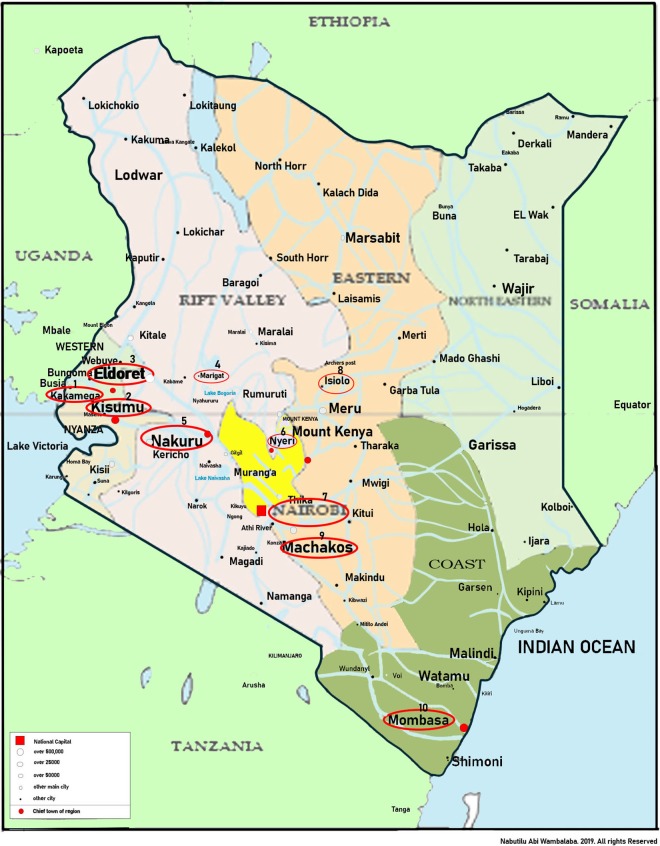
The study targeted 10 but carried out the survey in 7 of the 47 counties in Kenya between November 2013 and February 2014. The counties were suggested by the African Cancer Foundation which funded the study to ensure representation of each of the former 7 provinces. Unfortunately, we were not able to cover North Eastern province which is close to Somalia due to security issues. See the map in Figure 1. The research made an effort to cover at least one facility from each of the 10 targeted counties but was able to cover 9 of 10 as follows: (1) Kakamega General Hospital (Kakamega); (2) Jaramogi Oginga Odinga Teaching and Referral Hospital (Kisumu); (3) Rift Valley General Hospital (Nakuru); (4) Moi Teaching and Referral Hospital (Uasin Gishu); (5) Marigat District Hospital (Baringo); (6) Kenyatta National Hospital, Coptic Hospital, Texas Cancer Centre, and Karen Hospitals (Nairobi); (7) Nyeri General Hospital (Nyeri); (8) Machakos District Hospital (Machakos); and (9) Pandya Hospital (Mombasa). Because of the logistical problems and medical practitioners’ strikes, higher level facilities were targeted hoping that they were better placed to provide more information on cancer diagnosis and treatment issues and were ultimate recipients of patients with cancer referred by lower level facilities.
Figure 1.
Map of study area (http://auctiontheglobe.com/ke). Key: 1 = Kakamega, 2 = Kisumu, 3 = Eldoret, 4 = Marigat, 5 = Nakuru, 6 = Nyeri, 7 = Nairobi, 8 = Isiolo, 9 = Machakos, and 10 = Mombasa.
Data were collected from medical administrators with knowledge about the capacity of their facilities with respect to types of services provided, availability of equipment, and other related resources. We sampled records of 1048 patients with cancer and 12 health-care facilities and conducted at least one patient interview from each facility. Due to health workers strikes, scheduling problems and lack of response from some of the targeted facilities, or their delayed internal approvals, convenience sampling was used to collect data from those who were ready. The study took cognizance of access for the poor and therefore sought to ensure that vulnerable populations were included in the sampling frame to enhance representativeness in the data collection. The critical segments of the data were the demographic distribution of cancer cases, the medical capacity to handle cancer cases, and the equipment currently available to diagnose and treat cancer cases.
Professor Nicholas K. Gikonyo, Chairman of Ethics Review Committee at Kenyatta University approved our interviews (Approval: KU/R/COMM/52/214). Since the institutional review board (IRB) was anonymous, we only have the name of the chairman of the Review Committee. Kenyatta University’s IRB is duly authorized by the National Council for Science and Technology to review proposals. A written consent form was furnished to respondents for review and signature before starting interviews. The form included the following statement: “This study requires respondents to answer interview questions that will take approximately 20 to 30 minutes. Please respond to all the questions for the purpose of completeness. However, if you feel uncomfortable answering any of the questions, you may opt not to answer it. You may also decide to stop being a part of the research study at any time without explanation. You have the right to ask that any data you have supplied to that point be withdrawn or destroyed. If you have any further questions regarding the purpose of the study or with regard to the questions, please feel free to ask now or as you answer the questions.”
This study covered 3 groups of data, that is, patient data from records, interviews with volunteer patients, and survey data from hospital medical officers. For purposes of qualitative data, it was agreed that interviews be done with 1 to 2 patients per participating facility to provide a human face. An interview guide covering demographic, cancer history, and lifestyle practices was used for consistency and completeness. The study faced several key challenges in data collection which included long time frame for IRB approval process, staff turnover, logistical constraints, and respective financial implications.8 To mitigate them, the research team made some adjustments on the plans as follows: First, the study set out to cover 10 counties with the aim of covering at least one facility per county. The 10 counties were identified jointly between the research team and the African Cancer Foundation based on a purposeful sampling approach, focusing on representativeness of 8 former provinces, a mix of private and public providers, and willingness to participate in the study. Northeastern did not participate. Secondly, the study targeted larger facilities such as district or national referral hospitals since they would typically be the ones receiving patients with cancer as the majority of lower level facilities were not likely to have the expertise to diagnose and treat cancer and most had also been affected by the health workers strikes. Thirdly, because of lack of response from some of the targeted facilities or their delayed internal approvals, the study used convenience sampling to collect data from those who were ready. Fourthly, the study tried as much as possible to do trip chaining to combine several sites in one trip to reduce expenses.
To accomplish this, we agreed with responsible officers to leave facility data collection instruments with medical officers to fill out as we ran to the next facility so that we could pick them up on our way back, to avoid spending an extra night at the site while waiting for the forms to be filled up. The study relied on medical records managers who were the initial contacts to follow-up on their behalf. For medical records data collection and for confidentiality, the study paid a stipend to an internal records clerk at each facility to fill out the data collection forms. Potential for conflicting documentation could not be ascertained. However, a medical student intern from University of Nairobi was on hand to help with record interpretations. Finally, these challenges were taken as positive lessons learned from the research and therefore treated as part of the findings.
Data Analysis
The research process systematically divided respondents into 2 categories with focus on the demand and supply side. Although the demand-side analysis focused on number of current patients with cancer, vulnerable populations, and respective types of cancers, the supply-side analysis focused on availability of facilities, equipment, and experts for diagnosis and treatment of cancer. The demand-side process involved the data from existing records and thus identifying the numbers for the different types of treatment being sought and respective assessment of prevalence. The supply side entailed data from medical administrators to provide information about the infrastructure including the numbers of equipment, number of types of testing, and number of treatment types available at their facility and thus assessment of the capacity available. The analysis therefore was to compare the 2 sides to assess areas of adequacy and areas of need. A concurrent mixed-method analysis was used in the triangulation.
Quantitative data analysis was informed by the normality tests that portray the trends in the data distribution. Quantitative data were modeled for cancer prevalence by typology and geographically as well as for best practices. Reliability tests like the confirmatory tests helped in validating the findings. The typology qualitative technique was used for classification. The typology methodology was informed by patterns and themes. Single cases were analyzed more consistently before general statements were made. This entailed a lot of reconstruction of cases. Qualitative analysis was informed by the discourse analysis method. This approach focuses on the words, texts, and nuances during the data collection period. This helps in the reconstruction of the responses.
Results
From the demand side, it seemed that most of the patients were women at 57% compared to men at 43%. The most frequent age for female patients was at age 52 compared to men who constituted 43%, with cancer frequency peaking at age 62. Although the age distribution of the occurrence of the breast and cervix cancers was mainly spread between 25 and 74 years, they were most common among those in the ages between 40 and 55 years, that is, perimenopause. The most frequent type of cancer across the population was breast and cervical, followed by prostate, esophagus, and types of lymphoma. By gender, the most prevalent cancer in women was breast cancer followed by cancer of the cervix, while among men; top on the list was cancer of the esophagus followed by prostate cancer as reflected in Table 1. It is estimated that 3000 women in Kenya were diagnosed with cervical cancer and it is projected that by the year 2025, the number of new cervical cancer cases in Kenya will reach 4261 annually if proper measures are not put in place to prevent, control, or even create awareness among women in Kenya.9 In addition, at facility 4 Teaching and Referral Hospital, the cancer distribution had a bipolar distribution with one peak among children and another among adults.
Table 1.
Top Cancer Type by Facility and by Gender.a
| S. No. | Facility | Top 2 Overall in Percentages | Top 2 for Female in Percentages | Top 2 for Male in Percentages | % of Pop | Age | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| First | Second | First | Second | First | Second | M | F | M | F | ||
| 1 | Facility 1 | Breast 27 | Prost 20 | Breast 40 | Thorax 20; Leukm20 | Prost 60 | Lung 20; esoph 20 | 33 | 67 | 56 | 47 |
| 2 | Facility 2 | Cervix 13 | Cervix/ut 12 | Cervix, 18 | Cervix/ut 17 | Esoph 15 | Neopl 10 | 31 | 69 | 65 | 50 |
| 3 | Facility 3 | Esoph 7 | Breast, Leukm rectum, liver5 | Breast 9 | Colon 8 | Esoph 12 | Leukm and colon 6 | 48 | 52 | 61 | 53 |
| 4 | Facility 4 | Cervix 13 | Lympho 12 | Cervix 20 | Lympho 9 | Lympho 17 | Esoph, prost, pancr 5 | 36 | 64 | 65 | 65 |
| 5 | Facility 5 | Cervix 19 | Esoph 12 | Cervix 28 | Breast 16 | Esoph 25 | Prost 21 | 32 | 68 | 70 | 40 |
| 6 | Facility 6 | Leukm 10 | Cervix & Ovary 8 | Cervix 13 | Breast 11 | colon/leukm rectum 10 | Esopha 10 | 40 | 60 | 70 | 50 |
| 7 | Facility 7 | Breast 17 | Prost 11 | Breast 30 | Cervix/Colon 7 | Prost 25 | Lympho 13 | 44 | 56 | 44 | 56 |
| 8 | Facility 8 | No data available | |||||||||
| 9 | Facility 9 | Prost 20 | Breast 13 | Breast 35 | Ovary 15 | Prost 35 | Bladr 10 | 58 | 42 | 42 | 52 |
| 10 | Facility 10 | Breast 15 | Cervix and esoph 13 | Breast 24 | Cervix 21 | Esoph 16 | Colon 14 | 37 | 63 | 57 | 54 |
| 11 | Facility 11 | Cervix 28 | Breast/esoph 6 | Cervix 38 | Ovary 7 | Esoph 18 | Bladr/lympho 7 | 27 | 73 | 54 | 47 |
| 12 | Facility 12 | Colon 15 | Breast 12; Stomach 12 | Breast 27 | Carcino 20 | Stomac 21 | Colon 16 | 56 | 44 | 62 | 52 |
| Most Common/average | Breast 7 Cervix 7 | Prost 3 esoph 4 | Leukm 2; Rectum 1 | Liver 1; Lympho 1 | Ovary 1; Colon 1 | Stomac 1 | 42 | 58 | 62 | 52 | |
| Top 2 by gender | Breast 8 | Cervix 8 | Esoph 8 | Prost 5 | |||||||
Abbreviations: Bladr, bladder; Carcino, carcinoma; Cervix/ut, cervix uterus; esoph, esophagus; Leukm, leukemia; Lympho, lymphoma; Neopl, neoplasm; Pancr, pancreas; Prost, prostate; Stomac, stomach.
a Top 2 Overall represents percentage of type of cancer prevalent at the facility, for example, at facility 1, breast cancer came in at the top constituting 27% of recorded cases followed by prostate with 20%. With respect to gender, column on top 2 female represents percentage of type of cancer prevalent among female patients only at the facility, for example, at facility 1, breast cancer came in at the top constituting 40% of recorded cases followed by thorax and leukemia with 20%. Same applies for column for male. Finally, next columns are for percentage population which shows gender distribution of patients per facility and age distribution per facility.
From the supply-side perspective, the study examined types of cancers that the different facilities were handling. As demonstrated in Table 2, most of the facilities dealt with cervical, breast, esophagus, and prostate cancer and in most cases did more of the screening than treatment. Table 3 shows the status of treatment services available or outsourced at the respective facilities. The most common treatment services were surgery, chemotherapy, and existence of support groups, especially through palliative or hospice care services. The facilities that seem to offer most of the services were facility 8, facility 6, facility 7, facility12, and facility 9. It is worth noting that except for facility 6, the rest were private, and except for facility 9 which was in Mombasa (second largest city), the rest were from Nairobi (the capital city). Although not captured in the data, it was also clear from discussions with medical administrators that they were receiving patients with cancer toward the final stages. This picture is shared with the regional cancer registry at KEMRI, showing 80% of reported cancer cases were diagnosed at advanced stages, when very little could be done for curative treatment. This is largely due to low awareness of cancer signs and symptoms, inadequate screening services, inadequate diagnostic facilities, and a poorly structured referral system. The report also points out that the country had few cancer specialists concentrated in a few health facilities in Nairobi resulting in long waiting times and thus causing some previously curable tumors to progress to incurable stages.10
Table 2.
Type of Cancer by Facility.a,b
| S. No. | Indicate Type of Cancer You Deal With in This Facility…Screen (S) or Treat (T)? | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Facility | S/T | F1 | F2 | F3 | F4 | F5 | F6 | F7 | F8 | F9 | F10 | F11 | F12 | Total | |
| Type of Cancer | |||||||||||||||
| 1 | Cervical | S | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 7 | ||||
| T | 0 | 0 | 1 | 0 | 1 | 1 | 0 | 0 | 3 | ||||||
| 2 | Breast | S | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 9 | |||
| T | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 5 | |||||
| 3 | Esophagus | S | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 5 | |||||
| T | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 5 | |||||||
| 4 | Prostate | S | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 6 | ||||
| T | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 4 | ||||||
| 5 | Ovary | S | 0 | 0 | 0 | ||||||||||
| T | 0 | 1 | 1 | ||||||||||||
| 6 | Colon | S | 0 | 1 | 1 | 1 | 3 | ||||||||
| T | 0 | 0 | 1 | 0 | 2 | ||||||||||
| 7 | Thyroid | S | 1 | 1 | |||||||||||
| T | 1 | 1 | |||||||||||||
| 8 | Pancreatic | S | 1 | 1 | 2 | ||||||||||
| T | 1 | 0 | 1 | ||||||||||||
| 9 | Lung | S | 1 | 1 | |||||||||||
| T | 1 | 1 | |||||||||||||
| 10 | Liver | S | 0 | 0 | |||||||||||
| T | 0 | 0 | |||||||||||||
a Medical officials listed type of cancer and service provided where 1 means they provide the service and 0 means they don’t while empty slot means they did not list it. For example, facility 1 listed cervical, breast, and prostate indicating they screen cervical and breast cancer but no treatment while no screening nor treatment of prostate even though they have seen prostate patients. All cancers listed here were at least listed by one or more of the facilities. Last column shows frequency of screening or treatment across all facilities combined.
b Type of facility label key: F1 = Facility 1 District Hospital; F2 = Facility 2 General Hospital; F3 = Facility 3 Teaching and Referral Hospital; F4 = Facility 4 Teaching and Referral Hospital; F5 = Facility 5 General Hospital; F6 = Facility 6 National Hospital; F7 = Facility 7 Private Hospital; F8 = Facility 8 Cancer Center; F9 = Facility 9 Private Hospital; F10 = Facility 10 General Hospital; F11 = Facility 11 District Hospital; F12 = Facility 12 Private Hospital.
Table 3.
Treatment-Related Services by Facility.a
| Use the Codes Provided to Indicate the Status of the Following Services in Your Health Facility | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| S. No. | Facility | Y/O/N | F1 | F2 | F3 | F4 | F5 | F6 | F7 | F8 | F9 | F10 | F11 | F12 | Total |
| Type of Health Services | |||||||||||||||
| 1 | Surgery | Y | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 7 | |||||
| O | 1 | 1 | |||||||||||||
| N | 0 | 0 | 0 | ||||||||||||
| 2 | Radiology | Y | 1 | 1 | 2 | ||||||||||
| O | 1 | 1 | 1 | 3 | |||||||||||
| N | 0 | 0 | 0 | 0 | 0 | ||||||||||
| 3 | Chemotherapy | Y | 1 | 1 | 1 | 1 | 1 | 1 | 6 | ||||||
| O | 1 | 1 | |||||||||||||
| N | 0 | 0 | 0 | 0 | |||||||||||
| 4 | Immunotherapy | Y | 1 | 1 | |||||||||||
| O | 1 | 1 | 1 | 3 | |||||||||||
| N | 0 | 0 | 0 | 0 | 0 | 0 | |||||||||
| 5 | Hormonotherapy | Y | 1 | 1 | 2 | ||||||||||
| O | 1 | 1 | 2 | ||||||||||||
| N | 0 | 0 | 0 | 0 | 0 | 0 | |||||||||
| 6 | Gene therapy | Y | 1 | 1 | |||||||||||
| O | 1 | 1 | 1 | 3 | |||||||||||
| N | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||||||||
| 7 | Targeted therapy | Y | 1 | 1 | 1 | 3 | |||||||||
| O | 0 | ||||||||||||||
| N | 0 | 0 | 0 | 0 | |||||||||||
| 8 | Stem cell transplant | Y | 1 | 1 | 1 | 3 | |||||||||
| O | 1 | 1 | |||||||||||||
| N | 0 | 0 | 0 | 0 | 0 | 0 | |||||||||
| 9 | Laser technology | Y | 1 | 1 | 2 | ||||||||||
| O | 1 | 1 | 2 | ||||||||||||
| N | 0 | 0 | 0 | 0 | |||||||||||
| 10 | Cryotherapy | Y | 1 | 1 | 1 | 3 | |||||||||
| O | 1 | 1 | 1 | 3 | |||||||||||
| N | 0 | 0 | 0 | ||||||||||||
| 11 | Existence of support groups | Y | 1 | 1 | 1 | 1 | 1 | 1 | 6 | ||||||
| O | 0 | ||||||||||||||
| N | 0 | 0 | 0 | ||||||||||||
| 12 | Other/specify | 0 | |||||||||||||
| Totals | 0 | 0 | 0 | 4 | 0 | 10 | 9 | 11 | 6 | 3 | 3 | 9 | 55 | ||
a Medical officers were to specify from given service options whether they were available or outsourced as indicated by a “Y” for available, “O” for outsourced, and “N” for not available or blank if they did not specify either because they did not have information or it did not apply or for some other reason. The last column reflects the total frequency of provided services across all facilities, while the bottom reflects total services provided by a specific facility.
As illustrated in Table 4, available preventive services were very limited at the respective facilities with only preventive vaccinations, breast self-examination, and Pap smear. Although these services are modestly offered by facility 6 and facility 12, the overall mean for preventive services across all facilities was 1.9 on a scale of 1 to 4, indicating a small extent of services.
Table 4.
Preventive Services by Facility.a
| Score the Status of the Services Below Using the Codes Provided: 1 = Not Done; 2 = Small Extent; 3 = Moderate Extent; 4 = Large Extent | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| S.No. | Facility | F1 | F2 | F3 | F4 | F5 | F6 | F7 | F8 | F9 | F10 | F11 | F12 | Total, Mean |
| Type of Services Provided | ||||||||||||||
| 1 | Educating people on dangerous lifestyles | 1 | 2 | 3 | 2 | 1 | 2 | 2 | 2 | 3 | 2 | |||
| 2 | Protective strategies (protecting the skin) | 0 | 1 | 3 | 0 | 1 | 1 | 1 | 0 | 2 | 1 | |||
| 3 | Dietary plans (eat fish, fruits, low fats) | 0 | 2 | 3 | 2 | 2 | 2 | 3 | 0 | 3 | 1.9 | |||
| 4 | Preventive vaccinations (papillomavirus, hepatitis B) | 1 | 3 | 2 | 3 | 2 | 1 | 2 | 3 | 2.1 | ||||
| 5 | Systematic screening for early detection | 0 | 1 | 2 | 3 | 1 | 3 | 2 | 2 | 3 | 1.9 | |||
| 6 | Breast self-examination | 3 | 3 | 3 | 3 | 1 | 3 | 2 | 2 | 3 | 2.6 | |||
| 7 | Monographs | 0 | 2 | 3 | 0 | 3 | 1 | 0 | 3 | 1.5 | ||||
| 8 | Testicular self-examination | 0 | 1 | 3 | 3 | 1 | 3 | 1 | 1 | 2 | 1.7 | |||
| 9 | Pap smears (VIA) | 2 | 3 | 3 | 2 | 1 | 3 | 3 | 3 | 3 | 1.6 | |||
| Means | 0.8 | 0.0 | 0.0 | 2.0 | 0.0 | 2.8 | 2.3 | 1.0 | 2.4 | 1.8 | 1.3 | 2.9 | 1.9 | |
Abbreviation: VIA, Visual Inspection with Acetic Acid.
a Medical officers were to rate from given service options on a scale of 1 (not done) to 4 (large extent) or blank whether they did not specify, either because they did not respond, did not have information, or it did not apply or for some other reason. The last column reflects the mean score for provided services across all facilities, while the bottom reflects mean score for services provided by a specific facility.
The status of screening services as to whether they were available or not, and if not available, whether they were outsourced was analyzed. Data from facility 2, facility 3, and facility 5 were not available. Based on the feedback from participating administrators, a quick analysis shows that only one-third of the services are being provided (calculating the mean for all services provided). The most common services provided were Pap smears and X-rays. Most of these services were being provided or outsourced by facility 7, facility 8, facility 9, and facility 12 hospitals with a score of 15 of the possible score of 34, all of which are private. Next in line were facility 6 in Nairobi and facility 4 in Kisumu with a score of 13 of the possible 34, which are public as presented in Table 5.
Table 5.
Screening Services by Facility.a
| Use the Codes Provided to Indicate the Status of the Following Services in Your Health Facility | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| F1 | F2 | F3 | F4 | F5 | F6 | F7 | F8 | F9 | F10 | F11 | F12 | Total | |
| (a) Biopsy | |||||||||||||
| Available | 1 | 1 | 1 | 1 | 4 | ||||||||
| Outsource | 1 | 1 | 1 | 1 | 4 | ||||||||
| No service | 0 | 0 | 0 | ||||||||||
| (b) Sentinel node biopsy | 0 | ||||||||||||
| Available | 1 | 1 | 2 | ||||||||||
| Outsource | 1 | 1 | 1 | 3 | |||||||||
| No service | 0 | 0 | 0 | 0 | |||||||||
| (c) Endoscopy | 0 | ||||||||||||
| Available | 1 | 1 | 1 | 1 | 4 | ||||||||
| Outsource | 1 | 1 | 2 | ||||||||||
| No service | 0 | 0 | 0 | 0 | |||||||||
| (d) Blood tests | 0 | ||||||||||||
| Available | 1 | 1 | 1 | 1 | 1 | 1 | 6 | ||||||
| Outsource | 0 | ||||||||||||
| No service | 0 | 0 | 0 | 0 | |||||||||
| (e) Bone marrow aspiration | 0 | ||||||||||||
| Available | 1 | 1 | 1 | 1 | 1 | 1 | 6 | ||||||
| Outsource | 1 | 1 | 2 | ||||||||||
| No service | 0 | 0 | |||||||||||
| (f) Pap smear tests/cervical screening | 0 | ||||||||||||
| Available | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 | ||||
| Outsource | 1 | 1 | |||||||||||
| No service | 0 | ||||||||||||
| (g) Sputum analysis/bronchial washing analysis | 0 | ||||||||||||
| Available | 1 | 1 | 1 | 1 | 1 | 5 | |||||||
| Outsource | 1 | 1 | 2 | ||||||||||
| No service | 0 | 0 | 0 | ||||||||||
| (h) Urinalysis | 0 | ||||||||||||
| Available | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 7 | |||||
| Outsource | 0 | ||||||||||||
| No service | 0 | 0 | 0 | ||||||||||
| (i) Imaging studies: | 0 | ||||||||||||
| (i) X-rays | 0 | ||||||||||||
| Available | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 | ||||
| Outsource | 1 | 1 | |||||||||||
| No service | 0 | 0 | |||||||||||
| (ii) CT scans | 0 | ||||||||||||
| Available | 1 | 1 | 1 | 1 | 1 | 1 | 6 | ||||||
| Outsource | 1 | 1 | 2 | ||||||||||
| No service | 0 | 0 | |||||||||||
| (iii) MRI scans | 0 | ||||||||||||
| Available | 1 | 1 | 2 | ||||||||||
| Outsource | 1 | 1 | 1 | 1 | 4 | ||||||||
| No service | 0 | 0 | 0 | 0 | |||||||||
| (iv) Any other (specify) | 0 | ||||||||||||
| Available | 0 | ||||||||||||
| Outsource | 0 | ||||||||||||
| No service | 0 | 0 | 0 | ||||||||||
| (j) Immunohistochemistry | 0 | ||||||||||||
| Available | 1 | 1 | 2 | ||||||||||
| Outsource | 1 | 1 | 2 | ||||||||||
| No service | 0 | 0 | 0 | 0 | 0 | 0 | |||||||
| (k) Hormone analysis | 0 | ||||||||||||
| Available | 1 | 1 | 1 | 1 | 1 | 5 | |||||||
| Outsource | 1 | 1 | 2 | ||||||||||
| No service | 0 | 0 | 0 | ||||||||||
| (l) Mammography/mammogram | 0 | ||||||||||||
| Available | 1 | 1 | 1 | 1 | 4 | ||||||||
| Outsource | 1 | 1 | 2 | ||||||||||
| No service | 0 | 0 | 0 | ||||||||||
| (m) PET scan | 0 | ||||||||||||
| Available | 0 | ||||||||||||
| Outsource | 1 | 1 | 1 | 1 | 4 | ||||||||
| No service | 0 | 0 | 0 | 0 | 0 | ||||||||
| (n) Any other | 0 | 0 | |||||||||||
| Total | 2 | 0 | 0 | 13 | 0 | 13 | 15 | 15 | 15 | 7 | 5 | 15 | |
Abbreviations: CT, computed tomography; MRI, magnetic resonance imaging; PET, positron emission tomography.
a Medical officers were to specify from given service options whether they were available or outsourced as indicated by a “1” or blank if they did not specify, either because they did not have information or it did not apply or for some other reason. The last column reflects the total frequency of provided services across all facilities, while the bottom reflects total services provided by a specific facility.
Also, the research wanted to assess the status of treatment-related services available or outsourced at the respective facilities. The data collected is summarized in Table 6. Medical officers were to specify from given service options if they were available or outsourced as indicated by a “1,” a “0” for not available, or blank if they did not specify, either because they did not have information or they did not apply for some other reason. The last column reflects the total frequency of provided services across all facilities, while the bottom reflects total services provided by a specific facility.
Table 6.
Treatment-Related Services by Facility.a
| Use the Codes Provided to Indicate the Status of the Following Services in Your Health Facility | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| F1 | F2 | F3 | F4 | F5 | F6 | F7 | F8 | F9 | F10 | F11 | F12 | Total | ||
| (a) Surgery | Y | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 7 | |||||
| O | 1 | 1 | ||||||||||||
| N | 0 | 0 | 0 | |||||||||||
| (b) Radiotherapy | Y | 1 | 1 | 2 | ||||||||||
| O | 1 | 1 | 1 | 3 | ||||||||||
| N | 0 | 0 | 0 | 0 | 0 | |||||||||
| (c) Chemotherapy | Y | 1 | 1 | 1 | 1 | 1 | 1 | 6 | ||||||
| O | 1 | 1 | ||||||||||||
| N | 0 | 0 | 0 | 0 | ||||||||||
| (d) Immunotherapy | Y | 1 | 1 | |||||||||||
| O | 1 | 1 | 1 | 3 | ||||||||||
| N | 0 | 0 | 0 | 0 | 0 | 0 | ||||||||
| (e) Hormone therapy | Y | 1 | 1 | 2 | ||||||||||
| O | 1 | 1 | 2 | |||||||||||
| N | 0 | 0 | 0 | 0 | 0 | 0 | ||||||||
| (f) Gene therapy | Y | 1 | 1 | |||||||||||
| O | 1 | 1 | 1 | 3 | ||||||||||
| N | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||||||
| (g) Targeted therapy (uses drugs) | Y | 1 | 1 | 1 | 3 | |||||||||
| O | 0 | |||||||||||||
| N | 0 | 0 | 0 | 0 | ||||||||||
| (h) Stem cell transplant (peripheral blood, bone marrow) | Y | 1 | 1 | 1 | 3 | |||||||||
| O | 1 | 1 | ||||||||||||
| N | 0 | 0 | 0 | 0 | 0 | 0 | ||||||||
| (i) Laser technologies (light beams) | Y | 1 | 1 | 2 | ||||||||||
| O | 1 | 1 | 2 | |||||||||||
| N | 0 | 0 | 0 | 0 | ||||||||||
| (j) Cryotherapy | Y | 1 | 1 | 1 | 3 | |||||||||
| O | 1 | 1 | 1 | 3 | ||||||||||
| N | 0 | 0 | 0 | |||||||||||
| (k) Existence of support groups | Y | 1 | 1 | 1 | 1 | 1 | 1 | 6 | ||||||
| O | 0 | |||||||||||||
| N | 0 | 0 | 0 | |||||||||||
| (l) Other (specify) | Y | 0 | ||||||||||||
| 0 | 0 | 0 | 4 | 0 | 10 | 9 | 11 | 6 | 3 | 3 | 9 | |||
a Medical officers were to specify from given service options whether they were available or outsourced as indicated by a “Y” for available, “O” for outsourced, and “N” for not available or blank if they did not specify, either because they did not have information or it did not apply or for some other reason. The last column reflects the total frequency of provided services across all facilities, while the bottom reflects total services provided by a specific facility.
From the table, the mean score of treatment services is approximately 7 of 16 which is a little below halfway. The most common treatment services were surgery, chemotherapy, and existence of support groups especially through palliative or hospice care services. The facilities that seem to offer most of the services were Texas Cancer Center with a score of 11 of 16, followed by facility 6 with a score of 10, facility 7 and facility 12 hospitals each with a score of 6, and facility 9 in Mombasa with a score of 6. It is worth noting that except for facility 6, the rest were private, and except for facility 9, the rest were from Nairobi.
Discussion
As revealed in results, there are demand-side versus supply-side cancer control issues in Kenya. It is very clear that the prevalence of cancer is very high especially among women at a much young age (average 52 years compared to men at 62 years) and that children and the rural populations are as much of a concern as are adults and those in urban areas. Hence, the demand for cancer services is in very large numbers and will continue to grow. It was also clear that among the patients with cancer, awareness is very critical. Widespread lack of awareness and accurate information about cancer is another reason why screening is rare and many cancers are detected when it is too late to treat effectively.11 Several cultural myths, such as “cancer is caused by curses from ancestors,” exist, which are critical obstacles to expanded cancer control and care in Kenya, especially when it comes to early detection. According to the Regional Cancer Registry at KEMRI, about 80% of reported cases of cancer are diagnosed at advanced stages, when very little can be achieved in terms of curative treatment.12 This is largely due to the low awareness of cancer signs and symptoms, inadequate screening services, inadequate diagnostic facilities, and poorly structured referral facilities. Given the heavy demand in the face of limited capacity, it is critical that policy makers and practitioners closely review the cancer problems and mitigation strategies. Coupled with the growing demand-side cancer issues, Kenya’s supply capacity is crippled with physical, human, and fiscal resource constraints. The limited capacity with respect to diagnosis and treatment has implications to issues of access, proximity, and availability.
Accessing cancer screening and treatment is one of the major hurdles Kenyan patients with cancer face. Most cancer care services in Kenya are concentrated within a 5-km radius of each other in Nairobi.13 This leads to very limited access to care for most patients with cancer since 78% of Kenyans are rural residents, resulting in long waiting times causing some previously curable tumors to progress to incurable stages.14 There are only 4 cancer screening centers in Kenya with over 40 million people (or 39 000 new cancer cases annually)—all based in Nairobi—and 3 of them are privately owned. The cost of 1 week of radiation treatment at facility 6 is 2000 shillings ($24), while at private hospitals, patients pay 40 000 shillings ($475) for the same treatment. Facility 6 is the only public facility with an oncology unit that is affordable to many patients, making it difficult to meet the demand from the high number of patients. The wait time for treatment at facility 6 is extremely long, and this is a problem, as there is a narrow window of opportunity to treat cancer effectively. The other option of private cancer care is not actually an option for the majority of Kenyans, as treatment costs in these hospitals are so astronomical that many patients travel to India for cancer treatment and some patients from Western Kenya seek treatments in Uganda.15 To improve accessibility, it is recommended that subsidy programs, including donor appeals, be made similar to the AIDS/HIV initiatives to available screening and treatment services to those without means. These could be channeled through cancer foundations which would target risk sites and vulnerable populations for assistance.
The proximity problem arises from the concentration of cancer screening and treatment facilities primarily in Nairobi which is a long way from most of the patients across the country where 78% of the Kenyans reside. This problem could be addressed by directing resources to rural areas at community clinic levels with the help of cancer foundations. This would especially be also suited for awareness and preventive programs and yet reduce the treatment cost resulting from late diagnosis.
The resources availability problem is a resource problem that would require sourcing and equipping of medical facilities with screening and treatment services. Given the performance of private hospitals using outsourced resources, it is recommended that such a model be encouraged among public facilities so as to benefit from economies of scale, especially for smaller facilities. The cancer foundations can play a critical role enhancing awareness of such facilities for outsourcing. The Cobalt-60 machines used by facility 6 are of an old generation and are equipped with limited capability to optimally treat complex cases. Kenya Cancer Statistics estimates the human capacity for cancer treatment in Kenya in the public sector to include 4 radiation oncologists, 6 medical oncologists, 4 pediatric oncologists, 5 radiation therapy technologists, 3 oncology nurses, and 2 medical physicists.16 This falls far way below the capacity to manage and treat the 39 000 new cancer cases countrywide effectively. Most medical personnel, especially those trained in blood diseases and surgery, have been involved in treating cancer. This is as a result of increased numbers of patients with cancer who overwhelm the limited number of medical personnel in Kenyan hospitals. Facility 6 which is the largest hospital in the country had only one pediatric oncology unit (with only 28 beds) that catered for only 25% of pediatric cancer cases—the rest were accommodated in other wards. To improve the diagnostic facilities and treatment of cancer, there is a need for more pathologists and oncologists in peripheral hospitals to facilitate early detection and prompt treatment of cancer. In addition, government, public, and private teaching hospitals should commit themselves to widening the scope of learning about cancer in basic medical and nursing training programs. Policy guidelines would help in preventing cancer and minimize treatment interventions and hospital stays that increase individual suffering. Governmental and nongovernmental organizations should collaborate in drug dispensing, distribution and payment mechanisms, and support for poor patients.
Given the scarce supply of health-care resources, most cancer cases in Kenya are undetected or misdiagnosed, and prevention and early detection services are not available to most populations in Kenya. The Kenyan government has made marginal efforts to alleviate this growing problem. However, cancer screening coverage remained negligible because the national screening program had not been implemented as a fully fledged national program. Also, awareness of prevention and cancer management was low despite the ongoing cancer awareness campaigns.17 The government’s long-term measures have been captured in the cancer control initiatives at the MOH level in the Kenya Policy. The new policy framework for the next 20 years includes halting the rise of noncommunicable diseases as a strategic objective. The Kenyan household demographic survey in 2014 included questions about incidence of cancer—Kenya Demographic Health Survey.18
One of the implications of the study is that unlike the typical longer life expectancy of women, life expectancy among patients with cancer for women may become lower than for men given that women with cancer are 10 years younger than for men, and most patients with cancer in Kenya are dragonized in their late stage and ultimately die. Another implication is that the prevalence of cancer among children meant that cancer was no longer simply an exclusive problem among the adults, hence need to pay attention to the children as well. However, subsequent feedback indicated that the large numbers of children had to do with a special program for children with cancer at facility 4 resulting from the Medical Superintendent’s keen interest. Nevertheless, cancer among children should be of concern to policy makers and medical facilities that do not have a pertinent program. Thirdly, among the top 2 types of cancer, the second most frequent occurrence was the response for “other” which was representative of different multiple types of cancer other than the top 5, that is, breast, cervical, prostate, esophagus, and lymphoma. This has implications on the diversity and magnitude of other types of cancer that should not be overlooked. Thus, a comprehensive rather than a selective approach should be considered.
Conclusion
From screening to diagnosis to treatment, best practices in Kenya are impeded at every stage. Limited fiscal resources affect both the availability of physical and human capacity resources. This is more so because cancer treatment is protracted and expensive, especially due to the intensive procedures required for the advanced cancer cases. More so, delayed and futile multiple referrals pave the way for the most intensive and expensive hospital treatment, which entail catastrophic disruption of the livelihood. Cancer treatment is therefore a process of hope, fraught with daily life struggles.19 The findings point to a situation where the demand for cancer treatment services is growing from diverse directions, including the rural poor, the young, and most importantly the female gender being affected at a very young age compared to the male gender. From the supply side, there is a big problem of accessibility with respect to cost, proximity, and service availability. In Africa, patients with cancer face serious supply-side huddles due to very limited access to and availability of cancer screening and treatment services.20 In Kenya, the problem is becoming more pronounced particularly among the children patients.21 Notably, the Kenyan health-care system lacks sufficient financing and infrastructure to provide appropriate prompt treatment to most patients. A deeper examination of these findings reveals the rising gap between the growing demand for affordable care and the limited affordable supply due to the poorly resourced national health insurance system. Additional physical, human, and fiscal resources are desperately needed to narrow this gap. Comprehensive resource mobilization strategies should be undertaken to pool additional resources together, including augmentation of cancer foundations for enhancing awareness. The rising gap between the limited supply of resources and the growing demand for cancer treatment lead to rising economic costs of cancer care in Kenya.22 This alarming trend makes the Kenyan government’s inadequate cancer care policy further unsustainable. The Kenyan government has to tackle supply-side and demand-side challenges simultaneously.
From the demand side, it is recommended that cancer services be widely spread into the rural areas, especially at community and clinic levels which tend to be first points of contact, and where most of awareness is lacking. It is also emphasized that more attention be paid to children with cancer as was done at facility 4. More preventive attention must be paid to females, especially at a much younger age including initiation of programs in primary and secondary schools. More attention needs to be paid on the supply side to provide adequate cancer treatment and preventive services. On the treatment side, the issue of access with respect to cost management, proximity of facilities to patients, and availability of screening and treatment services are very highly recommended. On the preventive side, the issues of awareness in terms of symptoms and lifestyle practices are going to be very critical.23 To improve accessibility of care, the government must collaborate with cancer foundations and launch joint cancer AIDS/HIV initiatives and subsidy programs to assist patients without means. The government also needs to shift its focus from concentrated health resources in large cities to rural areas where almost 80% of the nation’s patients live.
Since this was a pilot study, it is not premature to recommend that a more comprehensive study be done to provide a much more definitive picture that would fully capture the prevalence and capacity of cancer diagnostics and treatment in Kenya. This study was limited to the 10 facilities that participated. Although most of the facilities largely catered for the local populations, referral facilities such as facility 6, facility 3, and facility 4 served populations from outside the region. Moreover, the facility 4 children cancer facility served the whole country. Hence, there is no inference of regional prevalence from the study.
Bearing these limitations in mind, the results of this study help understand the unbalanced cancer care policies and capacity which inadequately tackle the challenge of growing demand for affordable cancer care, while producing unsuccessful outcomes through insufficient supply-side interventions. Demand-side and supply-side cancer care issues should be carefully integrated into a balanced cancer care policy and capacity enhancement.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by Rockefeller Foundation through the Africa Cancer Foundation.
ORCID iD: Barbara Son, PhD  https://orcid.org/0000-0001-8523-759X
https://orcid.org/0000-0001-8523-759X
References
- 1. Morhason-Bello IO, Odedina F, Rebbeck TR, et al. Challenges and opportunities in cancer control in Africa: a perspective from the African organisation for research and training in cancer. Lancet Oncol. 2013;14(4):e142–151. [DOI] [PubMed] [Google Scholar]
- 2. Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095–2128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. World Health Organization. 1 in 2 Countries Unprepared to Prevent and Manage Cancers. Geneva, Switzerland: World Health Organization; 2013. [Google Scholar]
- 4. Kenya Medical Research Institute. Cancer Incidence Report. 2012. Geneva, Switzerland: Nairobi Cancer Registry. [Google Scholar]
- 5. Korir A, Mutuma GZ. Trends in adult cancers in Nairobi—Kenya (Nairobi Cancer Registry 2003-2006). AFR J Health Sci. 2011:19(3-4):104–105. [Google Scholar]
- 6. Korir A, Gakunga R, Subramanian S, et al. Economic analysis of the Nairobi Cancer Registry: implications for expanding and enhancing cancer registration in Kenya. Cancer Epidemiol. 2016;45(suppl 1):S20–S29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Tenge CN, Kuremu RT, Buziba NG, Patel K, Were PA. Burden and pattern of cancer in Western Kenya. East Afr Med J. 2009;86(1):7–10. [DOI] [PubMed] [Google Scholar]
- 8. Mills EJ, Seely D, Rachlis B, et al. Barriers to participation in clinical trials of cancer: a meta-analysis and systematic review of patient-reported factors. Lancet Oncol. 2006;7(2):141–148. [DOI] [PubMed] [Google Scholar]
- 9. Muraya JN. Direct asset recovery framework in Kenya. Paper Presented at: September 12, 2014; The Ethics and Anticorruption Commission, Nairobi, Kenya. [Google Scholar]
- 10. Worldwide Palliative Care Alliance and World Health Organization. Global Atlas of Palliative Care at End of Life. London, United Kingdom: World Health Organization; 2014. [Google Scholar]
- 11. Connor SR, Gwyther E. The worldwide hospice palliative care alliance. J Pain Symptom Manage. 2018;55(2S):S112–S116. [DOI] [PubMed] [Google Scholar]
- 12. National Cancer Control Strategy 2011-2016. Kenya Ministry of Public Health and Sanitation and Ministry of Medical Service. Nairobi, Kenya: National Cancer Control Strategy. [Google Scholar]
- 13. Mulemi BA. Coping With Cancer and Adversity: Hospital Ethnography in Kenya. Leiden, the Netherlands: African Studies Centre; 2010. [Google Scholar]
- 14. Friedrich MJ. Rates of noncommunicable diseases increasing in developing countries. JAMA. 2015;313(3):235. [Google Scholar]
- 15. Lesiew K, Alal M, Mghenyi C. Kenyan Women Flock to Uganda for Cancer Treatment. The STAR; 2013. [Google Scholar]
- 16. Kenya Cancer Statistics & National Strategies. Kenyan Network of Cancer Organizations. Nairobi, Kenya: Kenyan Network of Cancer Organizations; 2013. [Google Scholar]
- 17. Kenya Cancer Prevention and Control Act. National Council for Law Reporting With the Authority of the Attorney-General. Nairobi, Kenya: National Council for Law Reporting; 2012. [Google Scholar]
- 18. World Bank Open Data. Washington, DC: The World Bank; 2014. [Google Scholar]
- 19. Makumi D. Cancer nurses in Africa finding their footing. Asia Pac J Oncol Nurs. 2017;4(1):4–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kingham TP, Alatise OI, Vanderpuye V, et al. Treatment of cancer in sub-Saharan Africa. Lancet Oncol. 2013;14(4):e158–167. [DOI] [PubMed] [Google Scholar]
- 21. Marquez PV, Farrington JL. The Challenge of Noncommunicable Diseases and Road Traffic Injuries in Sub-Saharan Africa: An Overview. Washington, DC: The World Bank; 2013. [Google Scholar]
- 22. Huchko MJ, Bukusi EA, Cohen CR. Building capacity for cervical cancer screening in outpatient HIV clinics in the Nyanza province of western Kenya. Int J Gynaecol Obstet. 2011;114(2):106–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Stefan DC, Elzawawy AM, Khaled HM, et al. Developing cancer control plans in Africa: examples from five countries. Lancet Oncol. 2013;14(4):e189–195. [DOI] [PubMed] [Google Scholar]