Abstract
Background:
Despite evidence supporting telehealth provision in developed countries, there is limited evidence regarding its economic benefits for patients living in areas where access and cost present major barriers to health care, particularly in low- and middle-income countries (LMICs). This study explores the economic benefits of telemedicine for patients, in terms of cost and times savings, and its potential role in improving chronic disease outcomes.
Methods:
This retrospective cross-sectional study compared telemedicine services with hypothetical in-person consultations, with a focus on patient travel time and travel cost savings. A database containing teleconsultation visits (N = 25,182) conducted at health facilities in remote regions of Afghanistan, Pakistan, Tajikistan, and the Kyrgyz Republic, was analyzed. A two-sample homoscedastic t test was used to determine differences between the two groups. A one-way sensitivity analysis was also conducted, presuming in-person teleconsultations at 90%, 75%, and 50%.
Results:
The study extracted data from 25,182 teleconsultation visits (12,814 males; 12,368 females). The cumulative patient savings through the program amounted to USD 9,175,132, and 1,876,146 h, or 213.1 years. A significant difference was seen between the two groups in terms of mean time savings (p-value <0.05), and a nearly significant difference was observed in terms of mean cost savings (p-value = 0.05).
Conclusions:
This study suggests that considerable economic benefits imparted to patients in low-resource settings of LMICs via accessing telemedicine. Telemedicine has great potential to improve chronic disease outcomes in low-resource areas by reducing socioeconomic barriers related to cost and access, and increasing uptake of services, thereby enabling early intervention and long-term management.
Keywords: telemedicine, chronic disease, telemedicine cost savings, telemedicine time savings, teleconsultation network, economic evaluation of telemedicine, telemedicine in LMICs, telemedicine user benefits
Introduction
Poverty and chronic disease are interconnected in a vicious cycle, with poverty being one of the main risk factors for developing chronic disease, and chronic disease augmenting poverty in affected individuals. The poor are more affected for several reasons, such as psychosocial stress and reduced access to health care services.1
Populations living in low- and middle-income countries (LMICs) are more severely affected, with approximately 80% of all deaths due to chronic diseases occurring in LMICs, as per the latest estimates by the World Health Organization.1 Health inequity is, unfortunately, one of the salient features of health systems in these countries, with populations in remote and rural regions often affected with higher rates or morbidity and mortality. Poor infrastructure, security concerns, sociopolitical instability, high poverty rates, and large distances to health centers requiring extensive travel, prevent individuals from accessing health care, leading to missed opportunities of primary prevention, progression of conditions into chronic diseases and poor prognosis of existing chronic diseases.2 Telemedicine provides a viable medium to improve health care access in such areas.
Advancements in Information and Communication Technologies (ICTs) have immense potential to facilitate equitable health care provision.3 One of the major barriers to telehealth provision is the lack of high-quality evidence for its cost-effectiveness, particularly in LMICs.3 Despite considerable research into the effectiveness of teleconsultations and their various benefits, most studies are from an institutional perspective; studies documenting the patient’s perspective have evaluated either small sample sizes or covered a short-period of time.4–6 Furthermore, most studies have been based on subjective survey data.5
The role of teleconsultation as a service line is being explored globally, as a means to address socioeconomic disparities, particularly in remote areas. A literature review was conducted with a focus on studies evaluating patient cost savings through telemedicine and the resulting economic impact.
The majority of studies analyzed results from the health systems perspective. Studies evaluating patient cost savings through the program had employed various criterion to determine the cost. For example, an Arkansas-based study reported savings of US $32 in fuel costs across 92% of sampled patients, and wage savings of $100, in 84% of sampled patients. The study also calculated savings in family expenses and reduced missed time at work, which often presents an additional cost.4 An outpatient telemedicine program in vascular surgery in Michigan estimated the average travel cost saving to be $4.26 per patient, limiting it to gas and parking costs, along with an average roundtrip time savings of 39 min.7 A similar analysis was conducted on the University of Kansas Medical Center child psychiatry telemedicine program, which included a sample size of 132 patients and 257 teleconsultations. The study reported $86.13 in average mileage cost savings.6 The telerehabilitation program at Buffalo Veteran Affairs reported a median saving of 2.09 h in travel time, and $65.29 in travel costs per saving, the study also reported a 24% increase in patient care.8
A review of the teleconsultation database of the University of California Davis Health System program estimated the average time savings at 245 min and average cost savings at $156.5 A similar study in Mali was conducted to determine the economic benefits of telehealth in four districts of Mali, estimating an average of US $25 was saved by each patient.9 Both studies evaluated travel and lodging costs that would have incurred by determining the difference between accessing telehealth at the spoke site to a single designated hub site, that is, University of California Davis in the US, and the capital city in Mali. Following a similar model in our analysis, but minimizing the risk of bias, cost and time savings were calculated between accessing telemedicine at a spoke site and the nearest health facility offering the required specialty, which may not necessarily be the hub providing telemedical care.
Apart from Mali, most of the studies were based in the United States of America and France, both high income countries where the Federal minimum wage is above $7.25 per hour.10,11 In comparison, the minimum wage per hour in Afghanistan is $0.5, in Pakistan $0.68, in Tajikistan $0.17, and in the Kyrgyz Republic $0.10.12–15 These findings, while highlighting the disparity across the socioeconomic spectrum, also signify the immense burden of health care costs in low-resource settings. This study aimed to estimate the average travel-related cost and time savings for patients per each teleconsultation visit, in place of in-person visits to the nearest specialist facility.
The Aga Khan Development Network (AKDN) eHealth Program was established between 30 sites in Afghanistan, Pakistan, Tajikistan and Kyrgyz Republic, with a particular focus on populations living in remote and rural regions. The potential of this service line has not been explored extensively in the region. Based on data collected from a large sample size (i.e. patients accessing teleconsultation services between 2013 and 2017), the research team conducted an analysis of the cost and time savings estimated per each patient and the cumulative savings for the sample population. The study also aimed to explore the following policy question: Does telemedicine have the potential to improve chronic disease outcomes by reducing cost and distance barriers?
Methods
Study site and description
The AKDN eHealth Program was developed with the aim of addressing the three major barriers to health; access, quality, and cost. Through the program, teleconsultation services, which served as a link between the underserved communities and specialist health care services, were established in the participating countries.
Prior to project implementation, a community health needs assessment took place, after which the location of study sites (hub and spoke sites) was determined, which included existing Aga Khan Health Service sites; government health centers managed by AKDN; government health centers managed by other entities; health centers and hospitals owned and managed by the government; and healthcare facilities resulting from public-private partnerships developed between AKDN and Ministry of Health in order to support the local government. The hub and spoke sites along with their connections are tabulated in Appendix 1.
Teleconsultation services included both live and store-and-forward teleconsultations services. The comprehensive list of medical specialties offered in the South and Central Asian countries is tabulated in Appendix 2. The services offered ranged from internal medicine, pediatrics, and cardiology, among several others. Afghanistan, one of the oldest program, offered the most comprehensive set of services (17 services), compared with the Kyrgyz Republic and Pakistan, which offered only 3–4 teleconsultation specialties. The continuity in teleconsultation for these services over the years, suggest the benefits seen by both the providers and patients.
Study model
A ‘hub and spoke’ model was established among primary, secondary, and tertiary level healthcare facilities, which aimed to achieve strategic centralization. Hub sites, which are traditionally tertiary level hospitals, are capable of providing complex medical services and skills-intensive technological support. Through ICTs, they lend support to spoke sites, which are primary or secondary level health facilities that provide basic health care in remote regions, but lack in specialized service provision. The centralized network allows the majority of healthcare needs of the population to be addressed locally.
Study design
The study followed a retrospective cross-sectional study design. Prior to accessing teleconsultation services, a consent form was signed by each patient, ensuring complete confidentiality and privacy of personal health information (PHI). Each teleconsultation session was linked to a unique identification number, which included patient demographics, hub and spoke site information, type of specialty accessed, and clinical data.
Inclusion criteria
Patients who reported to the spoke-site health centers for treatment were offered teleconsultation services in the required specialty. Each participant with a valid identification number, sex, specialty accessed, and hub and spoke site information, was included in the study.
Exclusion criteria
Patients were excluded from the study if there was insufficient data regarding patient’s home address. These patients were excluded as the absence of their local address limited us from calculating the distance they would need to travel to the nearest health facility providing services in the required specialty, thereby precluding calculation of travel time and cost.
Data constraints
At the program’s initiation, teleconsultation was introduced as a service line as opposed to a research study. Recording of detailed patient information is a rare practice in these countries due to inefficient health systems, health policies, and health databases. As a result, there were constraints during data collection regarding patient demographics, such as age, socioeconomic status, education, and occupation.
Outcome measures
The study had the following outcome measures.
Projected cost savings
The projected cost savings were the round trip cost savings achieved through the use of teleconsultations, or the difference between the travel costs associated with accessing a teleconsultation at the spoke site, and costs associated with traveling to the nearest next-level health facility. The major costs associated with travel were recorded as follows: transport, accommodation, and three meals each day for two people; the patient and their attendant. Transport costs were calculated as an average of public and private transport cost in areas where the next-level facility could easily be reached by road. In Pakistan, it was calculated as a mean value of road and air travel costs, as both modes of traveling are availed. In Afghanistan, security concerns limit traveling to next-level health facilities by road, leading to most of health-care related travel being undertaken through United Nation (UN) chartered flights. Most of the travel in Tajikistan and Kyrgyz Republic was done by road. These factors were taken into account during calculation of transport-related costs.
Accommodation costs were calculated by the application of the lowest cost local hotel, after consultation by the local site head.
Costs for each teleconsultation were recorded by converting the local currency into USD, with the application of the average USD conversion rate for the year the teleconsultation took place.
Projected time savings
The projected time savings were the round trip time savings achieved through the use of teleconsultations, or the difference between the travel time associated with accessing teleconsultation at the spoke site, and time associated with traveling to the nearest next-level health facility.
Travel time was calculated using the quickest route on Google maps, and validated by the site head at each health facility. There were no standardized travel routes in most regions due to lack of proper roads, and frequent obstructions and delays due to landslides in the region. The lowest given value was accounted in these instances.
Two sample t test
A two-sample homoscedastic t test was done to compare the means of population accessing telemedicine and hypothetical in-person care.
Sensitivity analysis
A one-way sensitivity analysis was also conducted presuming in-person teleconsultations at 90%, 75%, and 50%. For the initial calculations, it was assumed that teleconsultations replaced all in-person encounters, or that, without it, all consultations would have taken place in-person at the next-level health facility. This suggests an overestimation of results. It is highly plausible that in the absence of telemedical facilities that the patient may not have received an in-person referral by the primary health care provider due to unavailability of a specialist, or that patients may have not travelled for in-person consultations due to cost limitations, travel-related inconvenience, political instability, security concerns, or other reasons.
For primary analyses, all telemedicine consultation encounters were assumed to have replaced in-person consultations, and that, without access to telemedicine, these encounters would have otherwise occurred in-person at the nearest health facility providing the specialty. However, it is likely that not all telemedicine encounters actually replaced in-person encounters due to various reasons, such as not being referred by their primary care provider, or the inconvenience related to travel in the region. A sensitivity analysis was conducted by altering this assumption to determine the corresponding impact on finding. Calculations were repeated assuming in-person encounter rates of 90%, 75%, and 50%.
Statistical analysis
Data was stored in an electronic database server, VirtualDoc, from which it was extracted onto Excel. Descriptive statistics were carried out via IBM SPSS version 19.
Ethical approval
The study did not require ethical approval as it evaluated existing available data retrospectively.
Results
Data description
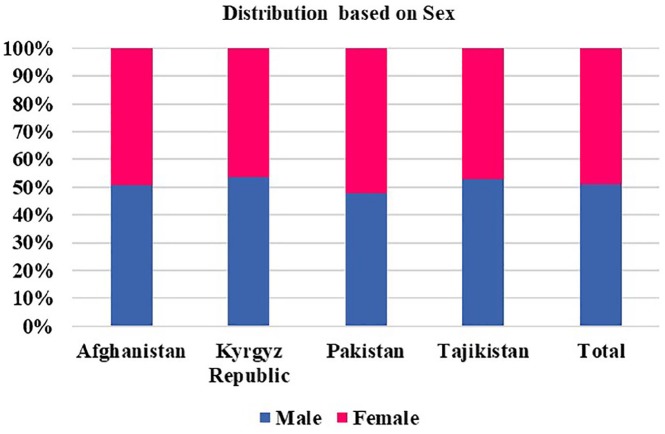
A total of 25,182 teleconsultations were carried out from 2013 to 2017. Patients were based in remote areas of Afghanistan, the Kyrgyz Republic, Pakistan, and Tajikistan. Approximately half of the patients were female. Many more patients were seen in Afghanistan than the other countries. The Kyrgyz Republic had many fewer patients, as the program was initiated in 2015, compared with other countries where it was initiated in 2013–2014. The distribution of teleconsultations according to sex is described in Figure 1 and Table 1.
Figure 1.
Distribution of teleconsultation participants in each country by sex.
Table 1.
Distribution of teleconsultations in each country by sex.
| April 2013–December 2017 | |||
|---|---|---|---|
| Teleconsultations | |||
| Total | Male | Female | |
| Afghanistan | 19,157 | 9707 | 9450 |
| Pakistan | 1,529 | 727 | 802 |
| Tajikistan | 4227 | 2237 | 1990 |
| Kyrgyz Republic | 269 | 144 | 125 |
| Total | 25,182 | 12,814 | 12,368 |
Table 2 depicts the following information for each country: cumulative monetary savings; cumulative time saved in hours, months, and years; total number of teleconsultations; and the date of initiation of the program. The cumulative cost savings by the patients amounted to USD 9,175,132, whereas the cumulative time saved by the patients amounted to 1,867,146 h or 213.1 years.
Table 2.
Cumulative teleconsultations, cost and time savings in each country.
| Initiation of teleconsultation services under CAHSS | No of teleconsultations | Cost saved (USD) | Hours saved | Days saved | Years saved | |
|---|---|---|---|---|---|---|
| Afghanistan | Apr-13 | 19,157 | $8,697,749 | 1,598,625 | 66,609 | 183 |
| Pakistan | Jan-14 | 1529 | $ 292,422 | 57,159 | 2382 | 7 |
| Tajikistan | Apr-13 | 4227 | $ 169,842 | 207,865 | 8661 | 24 |
| Kyrgyz Republic | Nov-15 | 269 | $ 15,119 | 3497 | 146 | 0 |
| Total | 25,182 | $9,175,132 a | 1,867,146 | 77,798 | 213.1 |
For Afghanistan, the exchange rate for 2013–2017 was taken at 1 USD = AFN 54.24 (2013), AFN 56.62 (2014), AFN 61.32 (2015), AFG 67.76 (2016), and AFG 67.65 (2017); for Pakistan, the exchange rate for 2013–2017 was taken at 1 USD = PKR 100.58 (2014), PKR 102.26 (2015), PKR 104.24 (2016), and PKR 105.26 (2017); for Tajikistan, the exchange rate for 2013–2017 was taken at 1 USD = TJS 4.76 (2013), TJS 4.93 (2014), TJS 6.15 (2015), TJS 7.83 (2016), and TJS 8.52 (2017); for the Kyrgyz Republic, the exchange rate for 2013–2017 was taken at 1 USD = KGS 64.46 (2015), KGS 69.91 (2016), and KGS 68.87 (2017).
CAHSS, Central Asia health systems strengthening; USD, United States dollars.
Two sample t test
Results of the two sample homoscedastic t test showed significant difference was seen between the two groups in terms of mean time savings (p value <0.05), and a nearly significant difference was observed in terms of mean cost savings (p value = 0.05).
Sensitivity analysis
Results of the sensitivity analyses of cost and time savings in each country, with replacement thresholds at 100%, 90%, 75%, and 50%, are listed in Table 3.
Table 3.
Sensitivity analysis showing cost and time saved at 90%, 75%, and 50%.
| Cumulative cost saving (USD) | Per capita cost saving (USD) | Cumulative time saving (h) | Per capita time saving (h) | ||
|---|---|---|---|---|---|
| Afghanistan | 100% | $8,697,749 | $ 454 | 1,598,625 | 83 |
| 90% | $7,827,974 | $ 409 | 1,438,763 | 75 | |
| 75% | $6,523,312 | $ 341 | 1,198,969 | 63 | |
| 50% | $4,348,875 | $ 227 | 799,313 | 42 | |
| Pakistan | 100% | $ 292,422 | $ 191 | 57,159 | 37 |
| 90% | $ 263,180 | $ 172 | 51,443 | 34 | |
| 75% | $ 219,317 | $ 143 | 42,869 | 28 | |
| 50% | $ 146,211 | $ 96 | 28,580 | 19 | |
| Tajikistan | 100% | $ 169,842 | $ 40 | 207,865 | 49 |
| 90% | $ 152,858 | $ 36 | 187,079 | 44 | |
| 75% | $ 127,381 | $ 30 | 155,899 | 37 | |
| 50% | $ 84,921 | $ 20 | 103,933 | 25 | |
| Kyrgyz Republic | 100% | $ 15,119 | $ 56 | 3497 | 13 |
| 90% | $ 13,607 | $ 51 | 3147 | 12 | |
| 75% | $ 11,339 | $ 42 | 2623 | 10 | |
| 50% | $ 7559 | $ 28 | 1749 | 7 |
USD, United States dollars.
Table 3 depicts the cumulative and per capita cost and time savings in each country, while varying the assumption for in-person encounters in the hypothetical group at 90%, 75%, and 50%. Findings suggest considerable cost and time savings, even if half the teleconsultations had taken place.
Uptake of teleconsultation services
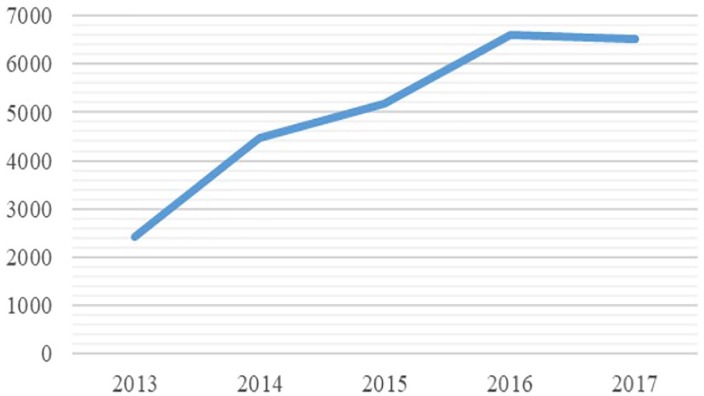
As shown in Figure 2 below, the cumulative uptake of teleconsultation services in all countries increased up to 2016 but showed a slight decrease in 2017, which suggests increased access to healthcare services, and better compliance. The decrease in 2017 is attributed to delay in funds delivery, prolonged and unplanned leave by healthcare personnel in the Kyrgyz Republic, and severe weather conditions such as heavy snow fall in the Kyrgyz Republic and flooding in Booni, Pakistan, leading to the spoke site being temporarily shut down. The decrease was most prominent in Tajikistan due to hiring of a specialist at a main spoke site, leading to reduced demand.
Figure 2.
Uptake of teleconsultation services between 2013 and 2017.
Discussion
The results demonstrated considerable cost and time savings in each of the participating countries.
The highest cumulative cost savings in Afghanistan are attributed to the teleconsultation service line being well-established by 2013, having been initiated in 2007. In contrast, the program was established in April 2013 in Tajikistan, January 2014 in Pakistan, and November 2015 in the Kyrgyz Republic, which is reflected in the difference in cumulative savings in each country. The per capita cost savings per teleconsultation were highest in Afghanistan and lowest in Tajikistan. The high costs in Afghanistan are attributed to the large travel distances. The situation is further aggravated by patients having to resort to air travel due to dire security concerns in terms of prevalent lawlessness, violence and terrorism, poor infrastructure, and dangerous terrain. In contrast, the distances are comparatively and easily covered by road in Afghanistan. Accommodation costs in Tajikistan were nominal compared with other countries in the project, as most patients reported staying at the homes of relatives or acquaintances when traveling to next-level health facilities.
Concurrently, the cumulative and average time savings per teleconsultation were highest in Afghanistan and lowest in the Kyrgyz Republic, attributed to the difference in country size. Assuming patients and their attendants are part of the labor force, and attend 8-h work days, the value of lost time was monetized by applying each country’s minimum wage and employment rate. Through teleconsultations, the following additional savings were achieved in each country: $20,259 in Afghanistan; $12,179 in Pakistan; $11,496 in Tajikistan; and $108 in the Kyrgyz Republic.16–19 The relatively low savings in the Kyrgyz Republic are attributed to the program being established later, leading to fewer teleconsultations and projected time savings; comparatively shorter distances between sites in the Kyrgyz Republic, lower minimum wage, and fewer specialties offered in the program.
The overall net savings are assumed to be an underestimation, and depict a percentage of total cost savings. There are a number of additional elements that were not included in the design of the study such as opportunity costs due to time lost at work, additional costs associated with private transport, parking fees, etc. The lowest possible values for transport and accommodation were included during estimation of costs. Furthermore, greater cost savings would have been estimated if some other hard-to-quantify factors were included in the cost-estimation process, such as a decrease in the number of visits to primary health care provider, better health outcomes due to timely consultation with a specialist, etc.
The research study is unique because it is the first to provide empirical data from a patient perspective through a multi-country program in LMICs on such a large scale. The central database, VirtualDoc, accumulated a large dataset between 2013 and 2017, which led to more accurate mean values, and a smaller margin of error in the results. The retrospective study also allowed standardization, as the sample population is assumed to be a subset of the ‘real world’ population. The main limitation of the study is that it is based on constrained retrospective data. A prospective cohort study planned prior to implementation would have enabled reporting along the Model of Assessment of Telemedicine (MAST) guidelines, or developing a cost-benefit analysis, to draw reliable comparison between studies.20,21 The study is also unable to comment on the resulting savings for healthcare systems.
While this study highlights the benefits attained by consumers in LMICs through an extensive teleconsultation network, a cost–benefit analysis of a prospective cohort study should be carried out to determine the long-term sustainability of teleconsultation programs in chronic disease management.21
Implementation of telemedicine technology in LMICs is associated with a range of barriers. While the initial cost of technology equipment and training technical staff is high, there is sufficient research to suggest that long-term benefits far outweigh the initial investment.22,23 Intersectoral collaborations, such as public private partnerships, established within this program minimize conventional concerns regarding loss or personal connection between doctor and patient, as a primary health care provider within a rural facility can not only guide the consultation, but also develop a patient history form and conduct their physical examinations, which also leads to their capacity building. It is also particularly useful in cases where the doctor does not have access to the patient’s electronic health record, which is presented as another key limitation to telemedicine programs.24,25 Another main limitation is ensuring sufficient connection bandwidth, which was addressed by using satellite connections in the absence of regular internet connectivity.26 Other valid concerns regarding telemedicine implementation is identification and the application of appropriate reimbursement models that were clarified prior to implementation.26 Prior to implementation, a situation analysis was conducted in each country. As a result, the implementation plan was driven and contextualized according to each country’s health system, existing health policies, and limitations. The implementation processes were developed, refined, and modified based on routine feedback and consultations with key stakeholders.
The measures outlined above enabled the telemedicine intervention to present a viable and sustainable solution in regions where distance, time, and costs related to traveling present major barriers to chronic disease prevention and management, which often leads to higher attrition rates, reduced number of physician visits, poorer management of chronic conditions, and unfavorable health outcomes.2
A customized telemedicine framework incorporating a comprehensive approach to effective chronic disease management should include separate components of preventive measures, self-management, quality treatment provision, and effective care coordination mechanisms between health care providers and patients.27 Through teleconsultations, health systems have the capacity to enhance patient involvement, identify early symptoms and manage chronic diseases in a timely manner. Effective telemedicine networks have been evidenced to reduce not only hospital stays but also the number of admissions and readmissions in chronic disease management.28 The evidence base on the cost effectiveness of telemedicine in chronic disease is, however, particularly limited.
This study does not aim to establish an evidence-base on the cost-effectiveness of telemedicine programs. It merely details the auxiliary savings associated with accessing telemedicine as opposed to traditional care, which may perhaps be nominal in high-income countries, but amount to a considerably large number for patients from low socioeconomic backgrounds in LMICs, where low minimal wage and high inflation rates make quality health care provision a precious commodity.
Most public health programs on chronic diseases are focused on prevention and addressing modifiable risk factors. Despite large-scale measures in the majority of WHO Member States, the increasingly high disability-adjusted life-years (DALYs), morbidity and mortality rates associated with chronic diseases continue to be a concern, and suggest research into addressing other seemingly nonmodifiable factors. Results of this study provide policy-makers, government organizations, and other health organizations with empirical evidence related to cost and time reductions for patients accessing telemedicine, addressing two of the major socioeconomic determinants of poor health: poverty and access.
Conclusion
This study suggests significant savings in time and cost for patients receiving chronic as well as infectious disease care through telemedicine in remote regions of LMICs. Policy implications emerging from the study are particularly relevant for countries experiencing similar socioeconomic barriers and shortage of specialists: considerable impact can be achieved in chronic disease management by addressing monetary, time, and access barriers, thereby initiating early intervention and improving prognoses for chronic diseases.
Supplemental Material
Supplemental material, Appendices for Addressing cost and time barriers in chronic disease management through telemedicine: an exploratory research in select low- and middle-income countries by Saleem Sayani, Momina Muzammil, Karima Saleh, Abdul Muqeet, Fabiha Zaidi and Tehniat Shaikh in Therapeutic Advances in Chronic Disease
Acknowledgments
The authors would like to acknowledge the support received from Aga Khan Foundation, Canada and Global Affairs Canada for the project’s implementation. We are also grateful to the implementing agencies for their efforts in ensuring timely data collection and verification.
The authors would like to acknowledge the efforts of all implementing agencies in accurate data collection.
Footnotes
Funding: The author(s) received no financial support for the research, authorship, and publication of this article.
Conflict of interest statement: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Disclaimer: Conclusions drawn from this study are based on the views of its authors and do not necessarily reflect the views of any external agencies. The authors have no conflicting interests to report.
ORCID iD: Momina Muzammil  https://orcid.org/0000-0001-9900-085X
https://orcid.org/0000-0001-9900-085X
Supplemental material: Supplemental material for this article is available online.
Contributor Information
Saleem Sayani, Aga Khan University, Karachi, Pakistan.
Momina Muzammil, Aga Khan Development Network Digital Health Resource Centre, Aga Khan University, National Stadium Road, Karachi City, Sindh 74800, Pakistan.
Karima Saleh, World Bank, Washington, DC, USA.
Abdul Muqeet, Aga Khan University, Karachi, Pakistan.
Fabiha Zaidi, Aga Khan University, Karachi, Pakistan.
Tehniat Shaikh, Aga Khan University, Karachi, Pakistan.
References
- 1. World Health Organization. Chronic diseases and their common risk factors [Internet], 2005. https://www.who.int/chp/chronic_disease_report/media/Factsheet1.pdf
- 2. Smith A, Youngberry K, Christie F, et al. The family costs of attending hospital outpatient appointments via videoconference and in person. J Telemed Telecare 2003; 9(2 Suppl.): 58–61. [DOI] [PubMed] [Google Scholar]
- 3. World Health Organization. Global diffusion of eHealth: making universal health coverage achievable. World Health Organization, 2016. [Google Scholar]
- 4. Bynum A, Irwin C, Cranford C, et al. The impact of telemedicine on patients’ cost savings: some preliminary findings. Telemed J E Health 2003; 9: 361–367. [DOI] [PubMed] [Google Scholar]
- 5. Dullet N, Geraghty E, Kaufman T, et al. Impact of a university-based outpatient telemedicine program on time savings, travel costs, and environmental pollutants. Value Health 2017; 20: 542–546. [DOI] [PubMed] [Google Scholar]
- 6. Kessler E, Sherman A, Becker M. Decreasing patient cost and travel time through pediatric rheumatology telemedicine visits. Pediatr Rheumatol 2016; 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Paquette S, Lin J. Outpatient telemedicine program in vascular surgery reduces patient travel time, cost, and environmental pollutant emissions. Ann Vasc Surg 2019; 59: 167–172. [DOI] [PubMed] [Google Scholar]
- 8. Spaulding R, Belz N, DeLurgio S, et al. Cost savings of telemedicine utilization for child psychiatry in a rural Kansas community. Telemed E Health 2010; 16: 867–871. [DOI] [PubMed] [Google Scholar]
- 9. Bagayoko C, Traoré D, Thevoz L, et al. Medical and economic benefits of telehealth in low- and middle-income countries: results of a study in four district hospitals in Mali. BMC Health Serv Res 2014; 14(S1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. U.S. Department of Labor. Minimum Wage - Wage and Hour Division (WHD). https://www.dol.gov/whd/minimumwage.htm (accessed 3 October 2018).
- 11. Eurostat. Monthly minimum wages, bi-annual data [Internet], 2019. http://appsso.eurostat.ec.europa.eu/nui/show.do?dataset=earn_mw_cur&lang=en (accessed 1 October 2019).
- 12. United States Department of State, Bureau of Democracy, Human Rights and Labor. Afghanistan 2017 Human Rights Report, https://www.state.gov/documents/organization/277519.pdf (accessed 3 October 2018).
- 13. United States Department of State, Bureau of Democracy, Human Rights and Labor. Pakistan 2017 Human Rights Report, http://www.state.gov/j/drl/rls/hrrpt/humanrightsreport/index.htm?year=2017&dlid=277291 (accessed 3 October 2018).
- 14. United States Department of State, Bureau of Democracy, Human Rights and Labor. Tajikistan 2011 Human Rights Report, https://www.state.gov/j/drl/rls/hrrpt/humanrightsreport/index.htm?year=2017&dlid=277291#wrapper (accessed 3 October 2018).
- 15. United States Department of State, Bureau of Democracy, Human Rights and Labor. Kyrgyz Republic 2017 Human Rights Report, https://www.state.gov/documents/organization/277529.pdf (accessed 3 October 2018).
- 16. Central Intelligence Agency. Cia.gov. South Asia: Afghanistan - The World Factbook, https://www.cia.gov/library/publications/the-world-factbook/geos/af.html (accessed 20 December 2018).
- 17. Central Intelligence Agency. Cia.gov. South Asia: Pakistan - The World Factbook, https://www.cia.gov/library/publications/the-world-factbook/geos/pk.html (accessed 20 December 2018).
- 18. Central Intelligence Agency. Cia.gov. Central Asia: Tajikistan - The World Factbook, https://www.cia.gov/library/publications/the-world-factbook/geos/ti.html (accessed 21 December 2018).
- 19. Central Intelligence Agency. Cia.gov. Central Asia: Kyrgyzstan - The World Factbook, https://www.cia.gov/library/publications/the-world-factbook/geos/kg.html (accessed 21 December 2018).
- 20. Kidholm K, Ekeland A, Jensen L, et al. A model for assessment of telemedicine applications: mast. Int J Technol Assess Health Care 2012; 28: 44–51. [DOI] [PubMed] [Google Scholar]
- 21. Dávalos M, French M, Burdick A, et al. Economic evaluation of telemedicine: review of the literature and research guidelines for benefit–cost analysis. Telemed E Health 2009; 15: 933–948. [DOI] [PubMed] [Google Scholar]
- 22. Kouskoukis M, Botsaris C. Cost-benefit analysis of telemedicine systems/units in Greek remote areas. Pharmacoecon Open 2016; 1: 117–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Akiyama M, Yoo B. A systematic review of the economic evaluation of telemedicine in Japan. J Prev Med Public Health 2016; 49: 183–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Patterson V. Teleneurology in Northern Ireland: a success. J Telemed Telecare 2002; 8(3 Suppl.): 46–47. [PubMed] [Google Scholar]
- 25. Brown S. Will teleneurology hit the big time? Lancet Neurol 2004; 3: 517–518. [DOI] [PubMed] [Google Scholar]
- 26. Patel U, Malik P, DeMasi M, et al. Multidisciplinary approach and outcomes of tele-neurology: a review. Cureus 2019; 11: e4410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Salisbury C, Thomas C, O’Cathain A, et al. TElehealth in CHronic disease: mixed-methods study to develop the TECH conceptual model for intervention design and evaluation. BMJ Open 2015; 5: e006448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Bashshur R, Shannon G, Smith B, et al. The empirical foundations of telemedicine interventions for chronic disease management. Telemed E Health 2014; 20: 769–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Appendices for Addressing cost and time barriers in chronic disease management through telemedicine: an exploratory research in select low- and middle-income countries by Saleem Sayani, Momina Muzammil, Karima Saleh, Abdul Muqeet, Fabiha Zaidi and Tehniat Shaikh in Therapeutic Advances in Chronic Disease