Abstract
Purpose of Review
The goal of this review is to provide updates on the safety and efficacy of long-term sulfonylurea use in patients with KCNJ11-related diabetes. Publications from 2004 to the present were reviewed with an emphasis on literature since 2014.
Recent Findings
Sulfonylureas, often taken at high doses, have now been utilized effectively in KCNJ11 patients for over 10 years. Mild-moderate hypoglycemia can occur, but in two studies with a combined 975 patient-years on sulfonylureas, no severe hypoglycemic events were reported. Improvements in neurodevelopment and motor function after transition to sulfonylureas continue to be described.
Summary
Sulfonylureas continue to be an effective, sustainable, and safe treatment for KCNJ11-related diabetes. Ongoing follow-up of patients in research registries will allow for deeper understanding of the facilitators and barriers to long-term sustainability. Further understanding of the effect of sulfonylurea on long-term neurodevelopmental outcomes, and the potential for adjunctive therapies, is needed.
Keywords: KCNJ11, Sulfonylurea, Glyburide, Neonatal diabetes, Monogenic diabetes, DEND syndrome
Introduction
Using sulfonylureas (SU) to treat KCNJ11-related diabetes is arguably the best example of personalized genetic medicine in diabetes. Mutations in KCNJ11 are the most common cause of permanent neonatal diabetes and were initially found to be responsive to SU about 15 years ago. Since that time, numerous KCNJ11 patients have successfully transitioned from insulin to these oral medications, often with improvements in glycemia, decrease in healthcare costs, and increases in quality of life. SU have been used for the treatment of type 2 diabetes worldwide for many years, although the rates of secondary failure and side effects such as hypoglycemia and cardiovascular risk have been notable concerns [1–3]. Questions have remained regarding the long-term efficacy and safety of these medications in patients with KCNJ11 mutations, particlarly in those taking high doses and off-label use for children. This review will focus on literature surrounding SU use in patients with KCNJ11 mutations, particularly those related to efficacy, sustainability, and safety with a focus on publications from the last 5 years.
Overview of KCNJ11 Neonatal Diabetes
Mechanism of Mutations
KCNJ11 encodes the protein Kir6.2, which forms the inner membrane, or pore, of the ATP-dependent potassium channel (KATP channel). The other subunit is an outer regulatory complex formed by SUR1 proteins, encoded by the ABCC8 gene. Mutations in ABCC8 can be clinically similar to mutations in KCNJ11, but they will not be focused on in this review. KATP channels are critically important for insulin release in beta cells. Heterozygous activating mutations in KCNJ11 cause the channel to stay in the open, active position by reducing the sensitivity of the channel to inhibition [4, 5]. This dysfunction ultimately prevents cell membrane depolarization and calcium influx, thus inhibiting the release of insulin from the beta cell. Severity of the clinical phenotype and level of channel dysfunction are directly related [4, 6]. Some KCNJ11 mutations cause a transient diabetes phenotype, due to a less severe reduction in sensitivity to inhibition [7].
Initial Identification and Diabetes Presentation
KCNJ11 mutations were first identified as a cause of permanent neonatal diabetes (PNDM) in 2004 and transient neonatal diabetes (TNDM) in 2005; they remain the most common cause of PNDM 15 years after their initial discovery [7, 8]. Clinically, patients are most often diagnosed with diabetes in the first 6 months of life, with occasional cases diagnosed beyond 6 months [9–11]. Diabetes onset characteristics can be variable but are frequently severe and may include long-lasting complications [12]. A study of 41 patients with KCNJ11 or ABCC8 mutations (median age at diabetes diagnosis 9.6 weeks) indicated 79% were in diabetic ketoacidosis (DKA) at diagnosis with median initial blood glucose levels of 717 mg/dL [13•].
Neurodevelopmental and Behavioral Difficulties
Because KATP channels are widely expressed within the brain, patients with KCNJ11 mutations may also have a range of neurodevelopmental and behavioral difficulties. The severity of difficulties is directly related to the functional severity of the mutations [6, 14]. Central nervous system features of any severity appear to be relatively common, with one study describing such problems in 64% of permanent diabetes cases with KCNJ11 mutations (n = 52/81) [15••]. Studies of cells expressing mutations suggest that the most damaging mutations are more likely to cause the most severe phenotype, termed DEND (developmental delay, epilepsy, and neonatal diabetes) syndrome, with patients often being unable to ambulate or speak [8, 16–18, 19•, 20]. Other mutations such as V59M are associated with a slightly less severe phenotype sometimes called “intermediate DEND” characterized by global developmental delay and severe cognitive dysfunction but often without seizures [16, 18, 19•, 20]. Compared with siblings without KCNJ11-related diabetes, even children with “mild” mutations (such as R201H) may still display significant differences on measures including IQ, academic achievement, and executive function [19•, 20]. Children with KCNJ11 were reported to have difficulties with inattention and attention-deficit/hyperactivity disorder (ADHD), anxiety, autism spectrum disorder, behavior challenges, and sleep issues, which were often significantly different than sibling controls [21•, 22]. Examination of adults with KCNJ11 mutations revealed similar features, such as autism spectrum disorder, as well as difficulties in coordination, motor sequencing, inattention, and lower IQ [23•].
Sulfonylurea Responsiveness and Efficacy
SU responsiveness in patients with KCNJ11 mutations was first demonstrated in 2004, in the first report of KCNJ11 mutations as a cause of PNDM [8]. These drugs increase the sensitivity of the KATP channels to inhibition, allowing them to close, and thus permitting insulin secretion. Both inpatient and outpatient transitions have been successful [24, 25]. Published protocols and expert centers are available to help guide healthcare providers in most appropriate use of SU medications and the process of reducing insulin doses [24] (monogenicdiabetes.org, diabetesgenes.org).
Transition from Insulin to Sulfonylurea
Large cohort studies have found that up to 90% of patients will be able to fully transition onto SU and discontinue insulin [24, 26•, 27]. These patients often require higher SU doses than are typically used in type 2 diabetes. Significant initial reductions in glycated hemoglobin (HbA1c) after transition to SU ranging from 1.3 to 2.5% have been reported in several cohorts [15••, 24, 28–32].
Barriers to Transition
While most patients will be able to fully transition off of insulin therapy, some will not. Some cases may be entirely unable to transition due to severely activating mutations that have minimal to no responsiveness to SU, such as two KCNJ11 patients (G334D and C166Y) that were completely unresponsive to SU trial [27]. In the case of the patient with G334D mutation, C-peptide levels before and after treatment with SU therapy as high as 1.8 mg/kg/day were barely detectable [33]. Others may respond to SU but have difficulty achieving sufficient glycemic control on SU monotherapy. Target glycemia may be achievable with additional glucose-lowering medications.
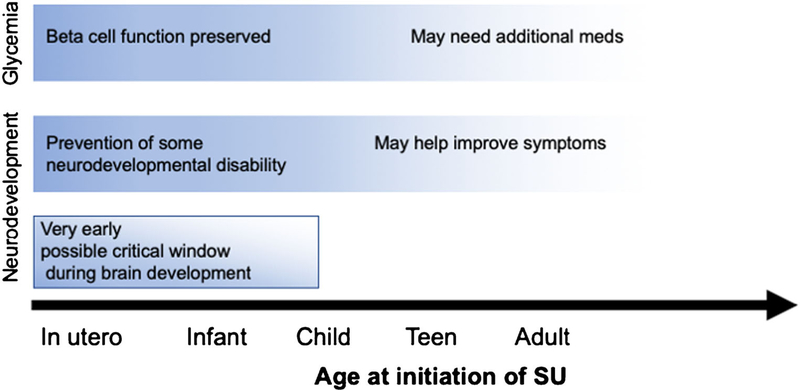
In vitro functional studies that include tests of SU responsiveness by mutated channels have generally correlated well to clinical responsiveness to SU therapy [4, 5, 8]. However, among patients with the same mutation, differences in responsivity to SU exist. Age at transition to SU has emerged as a potential barrier to complete transition to SU monotherapy without the need for insulin or other medications (Fig. 1). Of 58 patients studied in our US cohort, 10 (17%) required additional glucose-lowering medications beyond SU, and they had all been transitioned at age 13 years old or later (metformin: n = 5, sitagliptin: n = 6, exenatide: n =1, insulin: n = 2). Age of SU initiation was also significantly correlated with dose required at long-term follow-up [27]. Similarly, in a separate study of 127 patients with KCNJ11 mutations, 15 (12%) were unable to fully discontinue insulin, although several were able to decrease their insulin dose. There was a significant difference in age at the time of SU initiation for those who required additional medications [26•]. In a single case report of a mother and child who carried the R201C mutation, the child was able to successfully transition at age 8.5 years while the mother was unable to fully transition and remained on short-acting insulin with high-dose SU [34]. An 18-year-old patient with H46Y mutation was able to discontinue insulin and continue on SU after adding sitagliptin [35]. Some older patients may exhibit at least partial SU response only after being treated over several months [36], which may relate to a delayed effect of SU on cellular channel function, but may also be due to adverse effects of hyperglycemia on beta-cell function (such as altering gene expression, increasing glycogen accumulation, and increasing beta-cell apoptosis), as suggested in mouse models ofKCNJ11 diabetes [37, 38]. These adverse effects were modifiable with glucose-lowering medications, and improvements occurred faster with SU therapy than with insulin therapy [37, 38].
Fig. 1.
Age at initiation of sulfonylurea therapy impacts both glycemia and neurodevelopment
Impact of Sulfonylurea Treatment on Neurodevelopmental Outcomes
Neurodevelopment
Several case studies highlighting improvements for individual patients in either parent/caregiver-reported measures or standardized assessments have been reported (Fig. 1). Improvements in motor function [11, 39–41], cognition [11, 41, 42], communication [41], attention [10, 41], and behavior [10] have been attributed to SU transitions. A study by Beltrand and colleagues included several pre- and post-SU transfer measures for 16 children with KCNJ11 mutations. Significant improvements were noted in hyperactivity and motor skills, whereas sociability, language, and intelligence scores did not improve [31]. In a recent study of 81 KCNJ11 participants on long-term SU therapy, 47% of those with central nervous system (CNS) features reported improvements after transfer to SU in areas such as muscle tone and strength, concentration and attention, motor function, and speech [15••].
Early SU treatment appears to impact neurodevelopmental outcomes more strongly, perhaps due to treatment timing during critical windows of brain development. A cohort of 19 children with varying KCNJ11 mutations found that age of SU initiation was inversely correlated with visual-motor integration (VMI) scores for participants carrying the V59M or V59A mutation [43].
Imaging
Changes in neuroimaging before and after transition to SU were assessed for five participants with varying KCNJ11 mutations using single-photon emission computed tomography (SPECT). Significant improvements in cerebellar perfusion were noted after SU transfer in both hemispheres [44], and concurrent improvements in motor skills, attention, coordination, hyperactivity-impulsivity, and cognition (IQ) were noted in a previous description of one participant [45].
Limitations
While significant improvements have been noted through both parent/caregiver report and by standardized assessments, most patients with notable neurological dysfunction will continue to exhibit significant struggles after switching to SU therapy. Noticeable improvement in symptoms such as attention, motor coordination, and behavior are often seen, but complete reversal of physical challenges or full resolution of neurodevelopment difficulties is not common. Out of 18 participants who reported improvements in CNS features after SU treatment, 94% reported incomplete improvements with challenges remaining [15••]. Earlier treatment with SU leads to better neurodevelopmental outcomes, and so identifying patients with KCNJ11 mutations very early on, such as through standardized newborn screening programs or prenatal screening, would allow for earlier treatment and increased potential for improvements before brain development is complete. Limitations of SU treatment exist. A recent animal study sought to quantify the concentration of SU in plasma, cerebrospinal fluid, and brain tissue of treated and control rats and mice. While the plasma concentration of SU was high in the treated animals, SU was not detectable in either the cerebrospinal fluid (CSF) or brain tissue, suggesting that SU may be rapidly removed from CSF [46]. This highlights the need for additional medications that may more directly impact brain tissue and could have additional positive impacts on neurodevelopment.
Clinical Use of Sulfonylurea for KCNJ11 Diabetes
Sulfonylurea Dosing and Other Medications
As a result of the above factors, there is a wide range of SU dose requirements for KCNJ11 patients and it may take weeks before the effectiveness of any dose (especially the initial dose) is fully apparent. We thus recommend careful blood sugar monitoring during any periods of SU dose initiation or escalation, as well as monitoring of adherence, while utilizing published protocols for transition to SU [24] (monogenicdiabetes.org, diabetesgenes.org). Some patients have found continuous glucose monitoring to be helpful, although this may also reveal relative hypoglycemia that does not appear to be dependent on SU dose [47•]. The goals for SU dosing in these patients are distinct from more common forms of diabetes, in that they require a much higher dose for effective insulin secretion, but they subsequently may have some lower blood sugar numbers similar to individuals without diabetes [48, 49]. A dose of at least 1.0 mg/kg/day is typically required for most patients, but doses up to 2 mg/kg/day or more may be needed in some cases. Patients who are older at the time of transition may have had more time for beta-cell destruction or dedifferentiation, and thus less ability to respond to SU. For patients that are unable to fully transition onto SU after a trial with sufficiently high SU dose, the addition of other glucose-lowering medications may assist with lowering HbA1c, reducing insulin requirements, decreasing risk for hypoglycemia, and even improving hypoglycemic awareness [50]. It is imperative to continue SU at a maximal dose even after other medications are utilized to help achieve glycemic targets, as the endogenous insulin secretion is only possible through high-dose SU and the resulting benefits include reducing the dose of any exogenous insulin that may still be required, as well as possible beneficial effects on brain function (such as those discussed above) [34, 51, 52].
Consideration of Sulfonylurea Trial Before Genetic Testing Results Are Available
Some countries experience significant difficulty and/or delay in obtaining genetic testing. It may therefore be appropriate to consider trialing SU before genetic testing results are available in patients diagnosed with diabetes under 6 months of age who have no other ongoing medical difficulties, have no evidence for consanguinity, and have imaging evidence of normal pancreatic tissue [53, 54•]. However, it is imperative that comprehensive genetic testing be performed in all cases to confirm the underlying defect, whether SU was effective or not. If financial limitations to genetic testing exist, connecting with centers who may have resources to support testing is recommended (monogenicdiabetes.org, diabetesgenes.org, and additional local research groups in many different countries).
Choice of Sulfonylurea
Several different SU drugs are available for clinical use; however, glyburide—also called glibenclamide in some countries—has been the primary SU used in this patient population. Differences in efficacy based on SU drug choice have been described in a few instances that support the specific use of glyburide both for diabetes and potential neurological benefit. A patient with G53D mutation experienced no change in C-peptide levels (undetectable) with the addition of gliclazide, while restoration of C-peptide occurred with glyburide treatment. Motor function improved with the addition of gliclazide, with a slightly additional improvement seen after switching from gliclazide to glyburide [40]. Because glyburide is the most commonly used medication in patients with KCNJ11 mutations, it remains unclear how important differences between medications may be for glycemic and developmental improvements.
Safety
SU use in patients with KCNJ11 mutations is generally safe and imparts less risk than insulin use.
Hypoglycemia
Some cases require high-dose SU therapy, and therefore, questions about the potential for hypoglycemia are frequently raised by both families and clinicians. Mild and moderate hypoglycemia can occur in these patients, but severe hypoglycemia has not been reported. In one study of 166 patient-years on SU across 30 participants, 89% reported hypoglycemia (< 70 mg/dl) once per month or less frequently [47•]. However, three participants reported hypoglycemia once weekly or more frequently. Mild-moderate hypoglycemia does not appear to be dose-dependent; SU dose of the three participants reporting frequent hypoglycemia ranged from 0.386 to 2.354 mg/kg/day. No hypoglycemic episodes met criteria for severe hypoglycemia (involving seizures or unconsciousness) [47•]. In a 10-year multicenter follow-up study, data from 81 patients were examined. Across 809 patients-years, there were no reports of severe hypoglycemia [15••]. While any concern for hypoglycemia should be closely monitored, decreasing SU dose does not appear to eliminate mild-moderate hypoglycemia. Anecdotal reports of decreasing SU dose to avoid any blood sugar levels below 70 mg/dL have in some cases resulted in significant worsening of glycemic control, whereas with a sufficient dose, most patients will achieve HbA1c levels well within goal.
Other Side Effects
In general, other reported side effects from SU therapy are mild. The most commonly reported side effects include gastrointestinal issues including diarrhea [15••, 27, 30], initial hepatic steatosis [15••], and tooth discoloration (particularly in those who chewed glyburide tablets or used a concentrated solution instead of swallowing the tablets whole) [15••, 27, 55]. No cardiac side effects have been reported, and it is important to recognize that this unique patient population carrying mutations whose defect is directly addressed by high-dose SU treatment is completely distinct from those with type 2 diabetes who have extremely high baseline cardiovascular risk likely related to insulin resistance and other factors, regardless of which diabetes medications they are treated with. Indeed, most studies suggesting increased cardiovascular risk in type 2 diabetes treated with SU have been in comparison with met-formin and may reflect the benefit of year-long reduction of insulin exposure that would not be applicable to the KCNJ11 diabetes patient population [56].
Long-Term Sustainability
Since the initial discovery of KCNJ11 mutations causing diabetes in 2004, there have now been several longer term outcome studies of a relatively large number of patients who have been treated with SU for many years (Table 1). Eleven patients in a 2010 report who had transitioned to SU a median of 34 months prior were noted to have an initial reduction in HbA1c of 1.68%, as well as an overall decrease in SU dose of 0.24 mg/kg/day from initial transfer to follow-up. A case report of 30-month follow-up on a patient with G53D mutation similarly noted HbA1c reduction and SU dose reduction over the follow-up period [57]. Iafusco and colleagues reported on 11 patients in 2011 that had been followed for a median of 68 months after SU transfer [30]. Mean HbA1c decreased from 8.4% prior to transition, to 5.9% after 3 months of glyburide, to 6.0% after a median of 68 months after transition, suggesting excellent sustainability of SU. The longest follow-up study reported outcomes for 81 participants over a median duration of 10.2 years of SU treatment [15••]. At follow-up, 93% of the cohort remained on SU alone with a median HbA1c of 6.4%. The six patients who still required daily insulin in addition to SU also reported a higher HbA1c at follow-up (8.5%). These patients had similar ages at SU initiation and similar current ages. Oral and intravenous glucose tolerance tests on a small subset of participants (n = 6) suggested preservation of insulin response to oral glucose that may depend at least in part on the incretin effect.
Table 1.
Longitudinal studies on sulfonylurea use in KCNJ11 patients
| Author | Year published |
Number of KCNJ11 cases |
Years of SU f/up |
SU monotherapy at f/up |
Glycemic impact for SU monotherapy |
SU dose change |
Needed addt meds |
Unable to transition, non- responsive to SU |
Hypoglycemia | Other side effects | Complications |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Bowman | 2018 | 81 | Median f/up duration: 10.2 years | 93% (75/81) | Pre-transfer: median A1c 8.1% 1 year after: 5.9% Most recent f/up: 6.4% |
SU dose fell over | 7% (6/81) req. daily insulin | NR | No severe hypoglycemia reported in 809 pt-years of f/up | Reported in 14% (11/81)—diarrhea, nausea, abdominal pain, reduced appetite, hepatic steatosis, tooth discoloration | 9% (7/81)—retinopathy, microalbuminuria, proteinuria, neuropathy |
| Iatusco | 2011 | 11 | Median f/up duration: 68 months | 100% (11/11) | Pre-transfer: mean Alc 8.4% 3 months after: 5.9% Most recent f/up: 6% |
SU dose fell over time | NR | NR | NR | Diarrhea | NR |
| Li | 2018 | 5 PNDM KCNJ11 with SU trial | Mean f/up duration 3.6 years | 5/5 (100%) | “More stable glucose” | SU dose over time | 2 additional KCNJ11 participants chose not to trial SU so remained on insulin | 0% | NR | Transient diarrhea, poor feeding | NR |
| Laiming | 2016 | 30 | Age at SU initiation: median 1.2 years. Age at assessment: median 8 years |
97% (29/30) | NR | NR | 3% (1/30)—sitagliptin, metformin, insulin | NR | Mild to moderate hypoglycemia reported once per month or less frequently in 89.3% No severe hypoglycemia in 166 pt-years of f/up |
NR | NR |
Defined as reports with follow-up sulfonylurea data on at least five cases followed for a median or mean of least 3 years
SU sulfonylurea, NR not reported, PNDM permanent neonatal diabetes mellitus
Diabetes-Related Complications
Diabetes-related complications in patients with KCNJ11 mutations have been reported only rarely. Examinations for retinopathy were conducted in 11 participants in a Polish cohort prior to SU transfer [58]. Two participants had retinopathy at baseline. One was non-proliferative, did not progress during the 3-year follow-up period, and did not require laser therapy. The other participant, who was known to have proliferative retinopathy at baseline, also exhibited microalbuminuria, peripheral polyneuropathy, and cardiovascular autonomic neuropathy and hypertension. Of the cohort, she had been exposed to the highest HbAlc values (some > 13%) for many years while on insulin and had preexisting hypertension. Transfer to SU resulted in rapid improvement of glycemic control, and when the retinopathy also rapidly progressed, she required several rounds of laser therapy. She did achieve stabilization [59], and the rapid progression was not shown to be associated with her SU therapy. One patient out of 58 (7%) in a US cohort was found to have retinopathy, which was thought to be influenced by his later age of transition to SU and years of suboptimal HbAlc [27]. In a recent long-term follow-up study by Bowman and colleagues, after a median of 10 years on SU therapy, 9% of patients (n = 7/81) had microvascular complications, including retinopathy, microalbuminuria, proteinuria, and neuropathy [15••]. These patients were significantly older at the time of SU transfer, and likely had been exposed to non-optimal blood sugars for longer periods of time than those without complications. No macrovascular complications were reported.
Conclusions
Several studies demonstrate that high-dose SU treatment is a sustainable and safe treatment for patients with KCNJ11-related diabetes. SU treatment specifically corrects the molecular defect in these patients, and the majority will exhibit significant restoration of endogenous insulin production that results in vastly improved and excellent glycemic control for most patients. Initiating SU therapy as early as possible is critical for optimizing both glycemic and neurodevelopmental outcomes. Additional studies are needed to better understand the potential for additional therapies to improve neurodevelopmental outcomes. Systematic efforts are needed to more consistently identify patients with neonatal diabetes as early as possible. Possible approaches such as broad newborn screening programs, easier access to affordable genetic testing, as well as better implementation of genomic information into clinical practice will be crucial for optimizing patient outcomes.
Acknowledgments
We would like to acknowledge the international group of scientists and families who contribute to monogenic diabetes research. We would especially like to thank the families who participate in the Monogenic Diabetes Registry at the University of Chicago, and the healthcare teams providing care for them.
Funding Information This work was supported by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health [grant numbers R01 DK104942, P30 DK020595, and K23 DK094866], the CTSA [grant number UL1 TR002389], as well as by grants from the American Diabetes Association [grant numbers 1–11-CT-41 and 1–17-JDF-008], and gifts from the Kovler Family Foundation.
Abbreviations
- KATP channel
ATP-dependent potassium channel
- SU
Sulfonylurea
- PNDM
Permanent neonatal diabetes
- TNDM
Transient neonatal diabetes
- DKA
Diabetic ketoacidosis
- DEND
Developmental delay, epilepsy, and neonatal diabetes
- CNS
Central nervous system
- SPECT
Single-photon emission computed tomography
- CSF
Cerebrospinal fluid
Footnotes
Compliance with Ethical Standards
Conflict of Interest The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Publisher’s Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
•• Of major importance
- 1.Matthews DR, Cull CA, Stratton IM, Holman RR, Turner RC. UKPDS 26: sulphonylurea failure in non-insulin-dependent diabetic patients over six years. UK Prospective Diabetes Study (UKPDS) Group. Diabet Med. 1998;15:297–303. [DOI] [PubMed] [Google Scholar]
- 2.Gangji AS, Cukierman T, Gerstein HC, Goldsmith CH, Clase CM. A systematic review and meta-analysis of hypoglycemia and cardiovascular events: a comparison of glyburide with other secretagogues and with insulin. Diabetes Care. 2007;30:389–94. [DOI] [PubMed] [Google Scholar]
- 3.Sola D, Rossi L, Schianca GPC, Maffioli P, Bigliocca M, Mella R, et al. Sulfonylureas and their use in clinical practice. Arch Med Sci. 2015;11:840–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Proks P, Girard C, Ashcroft FM. Functional effects of KCNJ11 mutations causing neonatal diabetes: enhanced activation by MgATP. Hum Mol Genet. 2005;14:2717–26. [DOI] [PubMed] [Google Scholar]
- 5.Girard CAJ, Shimomura K, Proks P, Absalom N, Castaño L, Perez de Nanclares G, et al. Functional analysis of six Kir6.2 (KCNJ11) mutations causing neonatal diabetes. Pflugers Arch. 2006;453:323–32. [DOI] [PubMed] [Google Scholar]
- 6.Proks P, Antcliff JF, Lippiat J, Gloyn AL, Hattersley AT, Ashcroft FM. Molecular basis of Kir6.2 mutations associated with neonatal diabetes or neonatal diabetes plus neurological features. Proc Natl Acad Sci USA. 2004;101:17539–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gloyn AL, Reimann F, Girard C, Edghill EL, Proks P, Pearson ER, et al. Relapsing diabetes can result from moderately activating mutations in KCNJ11. Hum Mol Genet. 2005;14:925–34. [DOI] [PubMed] [Google Scholar]
- 8.Gloyn AL, Pearson ER, Antcliff JF, Proks P, Bruining GJ, Slingerland AS, et al. Activating mutations in the gene encoding the ATP-sensitive potassium-channel subunit Kir6.2 and permanent neonatal diabetes. N Engl J Med. 2004;350:1838–49. [DOI] [PubMed] [Google Scholar]
- 9.Rubio-Cabezas O, Flanagan SE, Damhuis A, Hattersley AT, Ellard S. KATP channel mutations in infants with permanent diabetes diagnosed after 6 months of life. Pediatr Diabetes. 2012;13:322–5. [DOI] [PubMed] [Google Scholar]
- 10.Mohamadi A, Clark LM, Lipkin PH, Mahone EM, Wodka EL, Plotnick LP. Medical and developmental impact of transition from subcutaneous insulin to oral glyburide in a 15-yr-old boy with neonatal diabetes mellitus and intermediate DEND syndrome: extending the age of KCNJ11 mutation testing in neonatal DM. Pediatr Diabetes. 2010;11:203–7. [DOI] [PubMed] [Google Scholar]
- 11.Battaglia D, Lin Y-W, Brogna C, Crinó A, Grasso V, Mozzi AF, et al. Glyburide ameliorates motor coordination and glucose homeostasis in a child with diabetes associated with the KCNJ11/S225T, del226–232 mutation. Pediatr Diabetes. 2012;13:656–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Day JO, Flanagan SE, Shepherd MH, Patrick AW, Abid N, torrens L, et al. Hyperglycaemia-related complications at the time of diagnosis can cause permanent neurological disability in children with neonatal diabetes. Diabet Med. 2017;34:1000–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.•.Letourneau LR, Carmody D, Wroblewski K, Denson AM, Sanyoura M, Naylor RN, et al. Diabetes presentation in infancy: high risk of diabetic ketoacidosis. Diabetes Care. 2017;40:e147–8This paper examined medical records from 88 infancy-onset diabetes cases and found that a staggering 66% presented in DKA at the time of diagnosis. This supports the need for systematic and early identification of all forms of infancy-onset diabetes.
- 14.Flanagan SE, Edghill EL, Gloyn AL, Ellard S, Hattersley AT. Mutations in KCNJ11, which encodes Kir6.2, are a common cause of diabetes diagnosed in the first 6 months of life, with the pheno-type determined by genotype. Diabetologia. 2006;49:1190–7. [DOI] [PubMed] [Google Scholar]
- 15.••.Bowman P, Sulen Å, Barbetti F, Beltrand J, Svalastoga P, Codner E, et al. Effectiveness and safety of long-term treatment with sulfonylureas in patients with neonatal diabetes due to KCNJ11 mutations: an international cohort study. Lancet Diabetes Endocrinol. 2018;6: 637–46This impressive paper is the longest follow-up study of patients with KCNJ11 mutations. Overall, this work suggests that sulfonylurea therapy is sustainable, effective, and safe.
- 16.Hattersley AT, Ashcroft FM. Activating mutations in Kir6.2 and neonatal diabetes: new clinical syndromes, new scientific insights, and new therapy. Diabetes. 2005;54:2503–13. [DOI] [PubMed] [Google Scholar]
- 17.Gloyn AL, Diatloff-Zito C, Edghill EL, Bellanne-Chantelot C, Nivot S, Coutant R, et al. KCNJ11 activating mutations are associated with developmental delay, epilepsy and neonatal diabetes syndrome and other neurological features. Eur J Hum Genet. 2006;14: 824–30. [DOI] [PubMed] [Google Scholar]
- 18.Busiah K, Drunat S, Vaivre-Douret L, Bonnefond A, Simon A, Flechtner I, et al. Neuropsychological dysfunction and developmental defects associated with genetic changes in infants with neo-natal diabetes mellitus: a prospective cohort study [corrected]. Lancet Diabetes Endocrinol. 2013;1:199–207. [DOI] [PubMed] [Google Scholar]
- 19.•.Carmody D, Pastore AN, Landmeier KA, Letourneau LR, Martin R, Hwang JL, et al. Patients with KCNJ11-related diabetes frequently have neuropsychological impairments compared with sibling controls. Diabet Med. 2016;33:1380–6Sibling controls and children affected with KCNJ11 diabetes were analyzed in this study, which uncovered that even patients with ‘mild’ KCNJ11 mutations may still have developmental struggles compared to their healthy siblings.
- 20.Bowman P, Hattersley AT, Knight BA, Broadbridge E, Pettit L, Reville M, et al. Neuropsychological impairments in children with KCNJ11 neonatal diabetes. Diabet Med. 2017;34:1171–3. [DOI] [PubMed] [Google Scholar]
- 21.•.Bowman P, Broadbridge E, Knight BA, Pettit L, Flanagan SE, Reville M, et al. Psychiatric morbidity in children with KCNJ11neonatal diabetes. Diabet Med. 2016;33:1387–91Six out of ten KCNJ11 participants were noted to have a psychiatric disorder (most commonly autism, anxiety, or ADHD) in this study, which was the first to specifically examine psychiatric morbidity.
- 22.Landmeier KA, Lanning M, Carmody D, Greeley SAW, Msall ME. ADHD, learning difficulties and sleep disturbances associated with KCNJ11-related neonatal diabetes. Pediatr Diabetes. 2017;18:518–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.•.Bowman P, day J, torrens L, shepherd M, knight B, ford T, et al. Cognitive, neurological, and behavioral features in adults with KCNJ11 neonatal diabetes. Diabetes Care. 2019;42:215–24The majority of adults with KCNJ11 mutations from this study (7/8) had abnormal neurological examinations, including difficulties such as impaired attention and reduced IQ.
- 24.Pearson ER, Flechtner I, Njølstad PR, Malecki MT, Flanagan SE, Larkin B, et al. Switching from insulin to oral sulfonylureas in patients with diabetes due to Kir6.2 mutations. N Engl J Med. 2006;355:467–77. [DOI] [PubMed] [Google Scholar]
- 25.Bremer AA, Ranadive S, Lustig RH. Outpatient transition of an infant with permanent neonatal diabetes due to a KCNJ11 activating mutation from subcutaneous insulin to oral glyburide. Pediatr Diabetes. 2008;9:236–9. [DOI] [PubMed] [Google Scholar]
- 26.•.Babiker T, Vedovato N, Patel K, Thomas N, Finn R, Männikkö R, et al. Successful transfer to sulfonylureas in KCNJ11 neonatal diabetes is determined by the mutation and duration of diabetes. Diabetologia. 2016;59:1162–6Babiker and colleagues analyzed data from 127 participants with KCNJ11 mutations and found that 88% were able to transfer fully onto SU and reach target HbA1c levels. They noted that participants who had a shorter duration of diabetes prior to SU transfer were more likely to have a successful transfer, highlighting the need for early initiation of SU.
- 27.Thurber BW, Carmody D, Tadie EC, Pastore AN, Dickens JT, Wroblewski KE, et al. Age at the time of sulfonylurea initiation influences treatment outcomes in KCNJ11-related neonatal diabetes. Diabetologia. 2015;58:1430–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sagen JV, Ræder H, Hathout E, et al. Permanent neonatal diabetes due to mutations in KCNJ11 encoding Kir6.2: patient characteristics and initial response to sulfonylurea therapy. Diabetes. 2004;53: 2713–8. [DOI] [PubMed] [Google Scholar]
- 29.Tonini G, Bizzarri C, Bonfanti R, Vanelli M, Cerutti F, Faleschini E, et al. Sulfonylurea treatment outweighs insulin therapy in short-term metabolic control of patients with permanent neonatal diabetes mellitus due to activating mutations of the KCNJ11 (KIR6.2) gene. Diabetologia. 2006;49:2210–3. [DOI] [PubMed] [Google Scholar]
- 30.Iafusco D, Bizzarri C, Cadario F, Pesavento R, Tonini G, Tumini S, et al. No beta cell desensitisation after a median of 68 months on glibenclamide therapy in patients with KCNJ11-associated permanent neonatal diabetes. Diabetologia. 2011;54:2736–8. [DOI] [PubMed] [Google Scholar]
- 31.Beltrand J, Elie C, Busiah K, Fournier E, Boddaert N, Bahi-Buisson N, et al. Sulfonylurea therapy benefits neurological and psychomotor functions in patients with neonatal diabetes owing to potassium channel mutations. Diabetes Care. 2015;38:2033–41. [DOI] [PubMed] [Google Scholar]
- 32.Støy J, Greeley SAW, Paz VP, Ye H, Pastore AN, Skowron KB, et al. Diagnosis and treatment of neonatal diabetes: an United States experience†. Pediatr Diabetes. 2008;9:450–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Greeley SAW, Zielinski MC, Poudel A, Ye H, Berry S, Taxy JB, et al. Preservation of reduced numbers of insulin-positive cells in sulfonylurea-unresponsive KCNJ11-related diabetes. J Clin Endocrinol Metabol. 2017;102:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Russo C, Salina A, Aloi C, Iafusco D, Lorini R, d’Annunzio G. Mother and daughter carrying the same KCNJ11 mutation but with a different response to switching from insulin to sulfonylurea. Diabetes Res Clin Pract. 2011;94:e50–2. [DOI] [PubMed] [Google Scholar]
- 35.Sastre J, Luque A, del Val F, Aragonés A, López J. Long-term efficacy of glibenclamide and sitagliptin therapy in adult patients with KCNJ11 permanent diabetes. Diabetes Care. 2014;37:e55–6. [DOI] [PubMed] [Google Scholar]
- 36.Malecki MT, Skupien J, Klupa T, Wanic K, Mlynarski W, Gach A, et al. Transfer to sulphonylurea therapy in adult subjects with permanent neonatal diabetes due to KCNJ11-activating [corrected] mutations: evidence for improvement in insulin sensitivity. Diabetes Care. 2007;30:147–9. [DOI] [PubMed] [Google Scholar]
- 37.Brereton MF, Iberl M, Shimomura K, Zhang Q, Adriaenssens AE, Proks P, et al. Reversible changes in pancreatic islet structure and function produced by elevated blood glucose. Nat Commun. 2014;5:4639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Brereton MF, Rohm M, Shimomura K, Holland C, Tornovsky-Babeay S, Dadon D, et al. Hyperglycaemia induces metabolic dys-function and glycogen accumulation in pancreatic β-cells. Nat Commun. 2016;7:13496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Slingerland AS, Nuboer R, Hadders-Algra M, Hattersley AT, Bruining GJ. Improved motor development and good long-term glycaemic control with sulfonylurea treatment in a patient with the syndrome of intermediate developmental delay, early-onset generalised epilepsy and neonatal diabetes associated with the V59M mutation in the KCNJ11 gene. Diabetologia. 2006;49:2559–63. [DOI] [PubMed] [Google Scholar]
- 40.Koster JC, Cadario F, Peruzzi C, Colombo C, Nichols CG, Barbetti F. The G53D mutation in Kir6.2 (KCNJ11) is associated with neo-natal diabetes and motor dysfunction in adulthood that is improved with sulfonylurea therapy. J Clin Endocrinol Metabol. 2008;93: 1054–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Slingerland AS, Hurkx W, Noordam K, Flanagan SE, Jukema JW, Meiners LC, et al. Sulphonylurea therapy improves cognition in a patient with the V59M KCNJ11 mutation. Diabet Med. 2008;25: 277–81. [DOI] [PubMed] [Google Scholar]
- 42.Gurgel LC, Crispim F, Noffs MHS, Belzunces E, Rahal MA, Moises RS. Sulfonylrea treatment in permanent neonatal diabetes due to G53D mutation in the KCNJ11 gene: improvement in glycemic control and neurological function. Diabetes Care. 2007;30: e108–8. [DOI] [PubMed] [Google Scholar]
- 43.Shah RP, Spruyt K, Kragie BC, Greeley SAW, Msall ME. Visuomotor performance in KCNJ11-related neonatal diabetes is impaired in children with DEND-associated mutations and may be improved by early treatment with sulfonylureas. Diabetes Care. 2012;35:2086–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fendler W, Pietrzak I, Brereton MF, Lahmann C, Gadzicki M, Bienkiewicz M, et al. Switching to sulphonylureas in children with iDEND syndrome caused by KCNJ11 mutations results in improved cerebellar perfusion. Diabetes Care. 2013;36:2311–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mlynarski W, Tarasov AI, Gach A, Girard CA, Pietrzak I, Zubcevic L, et al. Sulfonylurea improves CNS function in a case of intermediate DEND syndrome caused by a mutation in KCNJ11. Nat Clin Pract Neurol. 2007;3:640–5. [DOI] [PubMed] [Google Scholar]
- 46.Lahmann C, Kramer HB, Ashcroft FM. Systemic Administration of glibenclamide fails to achieve therapeutic levels in the brain and cerebrospinal fluid of rodents. PLoS One. 2015;10:e0134476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.••.Lanning MS, Carmody D, Szczerbiński Ł, Letourneau LR, Naylor RN, Greeley SAW. Hypoglycemia in sulfonylurea-treated KCNJ11-neonatal diabetes: mild-moderate symptomatic episodes occur infrequently but none involving unconsciousness or seizures. Pediatr Diabetes. 2017;19:393–7Frequency of hypoglycemia was analyzed in 30 participants with KCNJ11-related diabetes. Mild-moderate hypoglycemia was reported, although infrequently, and no episodes of hypoglycemia were noted to be severe.
- 48.Mazze RS, Strock E, Wesley D, Borgman S, Morgan B, Bergenstal R, et al. Characterizing glucose exposure for individuals with normal glucose tolerance using continuous glucose monitoring and ambulatory glucose profile analysis. Diabetes Technol Ther. 2008;10:149–59. [DOI] [PubMed] [Google Scholar]
- 49.Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group. Variation of interstitial glucose measurements assessed by continuous glucose monitors in healthy, nondiabetic individuals. Diabetes Care. 2010;33:1297–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Misra S, Vedovato N, Cliff E, De Franco E, Hattersley AT, Ashcroft FM, et al. Permanent neonatal diabetes: combining sulfonylureas with insulin may be an effective treatment. Diabet Med. 2018;35: 1291–6. [DOI] [PubMed] [Google Scholar]
- 51.Stanik J, Dankovcikova A, Barak L, Skopkova M, Palko M, Divinec J, et al. Sulfonylurea vs insulin therapy in individuals with sulfonylurea-sensitive permanent neonatal diabetes mellitus, attributable to a KCNJ11 mutation, and poor glycaemic control. Diabet Med. 2018;35:386–91. [DOI] [PubMed] [Google Scholar]
- 52.Babiker T, Shepherd MH, Hattersley AT. Continue with long term sulfonylureas in patients with mutations in the KCNJ11 gene when there is evidence of response even if insulin treatment is still required. Diabetes Res Clin Pract. 2013;100:e63. [DOI] [PubMed] [Google Scholar]
- 53.Carmody D, Bell CD, Hwang JL, Dickens JT, Sima DI, Felipe DL, et al. Sulfonylurea treatment before genetic testing in neonatal diabetes: pros and cons. J Clin Endocrinol Metabol. 2014;99:E2709–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.•.Li X, Xu A, Sheng H, Ting TH, Mao X, Huang X, et al. Early transition from insulin to sulfonylureas in neonatal diabetes and follow-up: experience from China. Pediatr Diabetes. 2018;19: 251–8Li and colleagues report on their experience trialing SU before genetic testing results were available in 16 cases with neonatal diabetes in China.
- 55.Kumaraguru J, Flanagan SE, Greeley SAW, Nuboer R, Støy J, Philipson LH, et al. Tooth discoloration in patients with neonatal diabetes after transfer onto glibenclamide: a previously unreported side effect. Diabetes Care. 2009;32:1428–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Roumie CL, Min JY, DAgostino McGowan L, Presley C, Grijalva CG, Hackstadt AJ, Hung AM, Greevy RA, Elasy T, Griffin MR (2017) Comparative safety of sulfonylurea and metformin monotherapy on the risk of heart failure: a cohort study. J Am Heart Assoc 6:696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Vendramini MF, Gurgel LC, Moisés RS. Long-term response to sulfonylurea in a patient with diabetes due to mutation in the KCNJ11 gene. Arq Bras Endocrinol Metabol. 2010;54:682–4. [DOI] [PubMed] [Google Scholar]
- 58.Klupa T, Skupien J, Mirkiewicz-Sieradzka B, Gach A, Noczynska A, Szalecki M, et al. Diabetic retinopathy in permanent neonatal diabetes due to Kir6.2 gene mutations: the results of a minimum 2-year follow-up after the transfer from insulin to sulphonylurea. Diabet Med. 2009;26:663–4. [DOI] [PubMed] [Google Scholar]
- 59.Klupa T, Skupien J, Mirkiewicz-Sieradzka B, Gach A, Noczynska A, Zubkiewicz-Kucharska A, et al. Efficacy and safety of sulfonylurea use in permanent neonatal diabetes due to KCNJ11 gene mutations: 34-month median follow-up. Diabetes Technol Ther. 2010;12:387–91. [DOI] [PubMed] [Google Scholar]